Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


BURNS
747
this may represent a potentially beneficial active interven-
tion as opposed to supportive care and good pulmonary
toilet that represents the mainstay of current care of smoke
inhalation injury.
Infection
The immune dysfunction following burns, for which a specific
cause is unknown, also may be a potential site of pharmaco-
logic intervention. Granulocyte-macrophage colony-stimulat-
ing factor (GM-CSF; sargramostim), in addition to
stimulating proliferation of granulocyte and macrophage pro-
genitor cells, increases macrophage phagocytic and cytocidal
activity, granulocyte RNA and protein synthesis, granulocyte
oxidative metabolism, and antibody-dependent cytotoxic
killing in mature cells in vitro. In a small cohort of burn
patients, sargramostim therapy increased granulocyte counts
by 50%. Administration of sargramostim reduced granulocyte
cytosolic oxidative function and myeloperoxidase activity to
control levels without changing superoxide production.
However, following cessation of treatment, superoxide activity
was subsequently increased compared with untreated burn
patients. These findings caution against clinical extrapolation
of in vitro results. A reduction in myeloperoxidase activity
actually may be detrimental because bactericidal capability
may be compromised. Increased superoxide production could
potentiate endothelial cell damage leading to increased capil-
lary permeability. The inability of immunomodulatory drugs
to significantly alter the postburn changes in immune func-
tion simply may represent the inability of single agents to alter
the complex cascade of pathophysiologic events occurring in
extensively burned patients.
The concept that the gut plays a central role in mainte-
nance of a persistent catabolic state in severely injured
patients has gained substantial popularity. Many animal stud-
ies support this hypothesis; however, the lack of clinically sig-
nificant bacteremia and endotoxemia in humans makes the
meaning of these findings unclear. Intestinal permeability is
increased preceding and during episodes of sepsis in burn
patients. Whether alterations in intestinal permeability result
in infection or represent only an epiphenomenon remains to
be proved. In a recent clinical study, the administration of
prophylactic enteral polymyxin B to burn patients resulted in
a decrease in endotoxemia; however, no correlation with ill-
ness severity score or outcome was observed.
Wound Closure
Excision of the burn wound with subsequent split-thickness
skin grafting is now common practice in most institutions.
Some clinicians advocate complete excision of the burn
wound within the first several days of hospitalization. The
postulated benefits of this treatment include decreasing the
extent and duration of hypermetabolism and immunosup-
pression, shortening the length of the hospital stay, and
improving survival. Prompt excision and closure of the burn
wound has been shown to ameliorate the hypermetabolic
response in laboratory animals, provided that the entirety of
the excised wound is closed by grafting. Similar reversal of
the immunosuppressive effects of burning also has been
documented. Such findings have yet to be observed in
humans probably because the entirety of the full-thickness
wound is seldom removed, partial-thickness wounds are not
excised, and definitive closure of large wounds cannot be
accomplished in a single operation. In several reports dealing
exclusively with early wound excision in burned children, the
duration of hospital stay was clearly shortened, intraopera-
tive blood loss was decreased, and survival was reported to be
improved. The duration of hospitalization has decreased for
adult burn patients in many centers because excisional ther-
apy is employed routinely, but a favorable impact of early
complete excision of the burn wound on pathophysiologic
changes and outcome has not been documented. Moreover,
the deleterious hemodynamic and pulmonary effects of gen-
eral anesthesia during the early postburn period speak for
cautious use of such procedures during the resuscitation
period in the severely burned patient. Such excisions should
be performed on carefully selected patients and only by expe-
rienced operating teams and anesthesiologists.
The identification and availability of various growth fac-
tors have stimulated interest in the potential for accelerating
the healing of burns, skin grafts, and skin graft donor sites.
An effective agent could produce more rapid healing of
burns (hastening return to work), permit more frequent har-
vesting of donor sites in massive burns, and shorten healing
time of skin grafts (reducing periods of immobility). The
topical application of epidermal growth factor has been
shown to enhance healing of split-thickness skin graft donor
sites by reducing the time to complete healing by 1.5 days.
Although the decrease in healing time was statistically signif-
icant, the clinical benefit would be minimal. A 50% reduc-
tion in skin graft donor-site healing time would be required
to be clinically effective. The systemic administration of
human growth hormone also has been reported to decrease
the time of skin graft donor-site healing in children, but the
same effect was not observed routinely in adult patients. The
ability of growth factors to improve healing in burn patients
continues to be an area of active research and debate.
Hypermetabolism
The hypermetabolic response to thermal injury is well
described, and in addition to the classic hormonal mediators,
cytokines may play an important role in maintenance of the
hyperdynamic state. Circulating levels of tumor necrosis fac-
tor, IL-1, and IL-6 are increased at various times following
thermal injury and sepsis; however, the effect of pharmaco-
logic or immunologic blockade of these cytokines is not
clearly established following burn injury. In a series of exten-
sively burned patients, blood levels of TNF-α, IL-1, and IL-6,
although frequently elevated, had no correlation with the
patients’ clinical courses.
CHAPTER 35
748
The hypermetabolic response to thermal injury can be
attenuated by β-adrenergic blockade. Administration of pro-
pranolol has been effective in decreasing metabolic rate and
cardiac work in burned children and adults; however,
increased nitrogen loss was induced presumably from periph-
eral β-receptor blockade. Cardioselective β-adrenergic block-
ers are currently being studied that may circumvent the
nitrogen-wasting effects of nonselective agents. Attempts to
decrease catabolism and protein wasting also have been stud-
ied. The selective β
2
-adrenergic agonist clenbuterol increased
resting energy expenditure and normalized muscle protein
content, muscle mass, and body weight gain in burned rats.
Administration of insulin-like growth factor 1 (IGF-1) to
burn patients, decreased protein oxidation and protein break-
down only in patients in whom an insulin-like effect also
occurred. Similar responses in burn patients were demon-
strated with the administration of low-dose exogenous
insulin and glucose. Testosterone analogues also have been
used to reduce postinjury catabolism. Oxandrolone, a weakly
androgenic testosterone analogue, has been shown recently to
decrease net daily nitrogen loss and weight loss in seriously
burned patients. This study also described a decrease in heal-
ing time of standarized donor sites from 13 ± 3 days to 9 ± 2
days. Complications were similar between groups, and no side
effects directly attributed to the drug were identified.
Herndon and colleagues evaluated the effect of β-adrenergic
blockade using orally administered propranolol on resting
energy expenditure and muscle-protein catabolism in
severely burned children. After 2 weeks of treatment, a dose
sufficient to decrease the resting heart rate by 20% resulted in
a 24% decrease in resting energy expenditure in the propra-
nolol group compared with a 5% increase in a matched con-
trol group. The net muscle-protein balance increased by 82%
over baseline values in the propranolol group, whereas it
decreased by 27% in the control group.
Further studies are required to determine if the apparent
benefits of blockade of the hypermetabolic response result in
decreased morbidity and mortality for the severely burned
patient or whether they merely reflect short-term changes in
protein metabolism.
Basadre JO et al: The effect of leukocyte depletion on smoke
inhalation injury in sheep. Surgery 1988;104:208–15.
Baxter CR: Future perspectives in trauma and burn care. J Trauma
1990;30:S208–9.
Brown GL et al: Enhancement of wound healing by topical treat-
ment with epidermal growth factor. N Engl J Med 1989;321:
76–9. [PMID: 2659995]
Chance WT et al: Clenbuterol decreases catabolism and increases
hypermetabolism in burned rats. J Trauma 1991;31:365–70.
[PMID: 2002523]
Cioffi WG Jr et al: Effects of granulocyte-macrophage colony-
stimulating factor in burn patients. Arch Surg 1991;126:74–9.
[PMID: 1845929]
Davis CF et al: Neutrophil activation after burn injury:
Contributions of the classic complement pathway and of endo-
toxin. Surgery 1987;102:477–84.
Demling RH, Lalonde C: Early burn excision attenuates the post-
burn lung and systemic response to endotoxin. Surgery
1990;108:28–35. [PMID: 2360187]
Demling RH, Lalonde C: Effect of partial burn excision and clo-
sure on postburn oxygen consumption. Surgery 1988;104:
846–52. [PMID: 3187900]
Demling RH et al: Fluid resuscitation with deferoxamine prevents
systemic burn-induced oxidant injury. J Trauma 1991;31:
538–43. [PMID: 1708429]
Demling RH, Orgill DP: The anticatabolic and wound healing
effects of the testosterone analog oxandrolone after severe burn
injury. J Crit Care 2000;15:12–7. [PMID: 10757193]
Desai MH et al: Reduction in mortality in pediatric patients with
inhalation injury with aerosolized heparin/N-acetylcystine
therapy. J Burn Care Rehabil 1988;19:210–2. [PMID: 9622463]
Desai MH et al: Early burn wound excision significantly reduces
blood loss. Ann Surg 1990;211:753–9. [PMID: 2357138]
Gore DC et al: Effect of exogenous growth hormone on whole-
body and isolated-limb protein kinetics in burned patients.
Arch Surg 1991;126:38–43. [PMID: 1898697]
Herndon DN et al: Determinants of mortality in pediatric patients
with greater than 70% full-thickness total body surface area
thermal injury treated by early total excision and grafting.
J Trauma 1987;27:208–12. [PMID: 3546714]
Herndon DN et al: Effect of propranolol administration on hemo-
dynamic and metabolic responses of burned pediatric patients.
Ann Surg 1988;208:484–92. [PMID: 3052328]
Herndon DN et al: Effects of recombinant human growth hor-
mone on donor-site healing in severely burned children. Ann
Surg 1990;212:424–49. [PMID: 2121109]
Herndon DN et al: The pathophysiology of smoke inhalation injury
in a sheep model. J Trauma 1984;24;1044–51. [PMID: 6512897]
Herndon DN et al: Reversal of catabolism by beta-blockade after
severe burns. N Engl J Med 2001;345:1223–9. [PMID: 11680441]
Ireton-Jones CS, Turner WW Jr, Baxter CR: The effect of burn
wound excision on measured energy expenditure and urinary
nitrogen excretion. J Trauma 1987;27:217–20. [PMID: 3820355]
Lalonde C, Demling RH: The effect of complete burn wound exci-
sion and closure on postburn oxygen consumption. Surgery
1987;102:862–8. [PMID: 3672326]
Sartorelli KH, Silver GM, Gamelli RL: The effect of granulocyte
colony-stimulating factor (G-CSF) upon burn-induced defec-
tive neutrophil chemotaxis. J Trauma 1991;31:523–39. [PMID:
2020039]
Schirmer WJ et al: Complement-mediated hemodynamic depres-
sion in the early postburn period. J Trauma 1989;29:932–8.
[PMID: 2746703]
Strock LL et al: The effect of insulin-like growth factor I on post-
burn hypermetabolism. Surgery 1990;108:161–4.
Tanaka H et al: Reduction of resuscitation fluid volumes in severely
burned patients using ascorbic acid administration. Arch Surg
2000;135:326–31. [PMID: 10722036]
Tchervenkov JI et al: Early burn wound excision and skin grafting
postburn trauma restores in vivo neutrophil delivery to inflam-
matory lesions. Arch Surg 1988;123:1477–81. [PMID: 3056334]
Thompson P et al: Effect of early excision on patients with major
thermal injury. J Trauma 1987;27:205–7. [PMID: 3820353]
Waxman K et al: Hemodynamic and oxygen transport effects of
pentastarch in burn resuscitation. Ann Surg 1989;209:341–5.
[PMID: 2466449]

BURNS
749
II. CHEMICAL BURN INJURY
The severity of injury caused by chemical exposure is related
to the amount and concentration of the agent and the dura-
tion of contact with the tissues. Strong alkalis and acids
found in common household cleaners are responsible for
the majority of minor chemical injuries. More extensive
injuries often result from industrial and laboratory acci-
dents or from assaults. The amount of tissue damage
incurred also depends on the nature of the specific agent.
Strong alkalis react with tissues to produce saponification
and liquefaction necrosis. Acids are water-soluble and pene-
trate easily into subcutaneous tissue and cause coagulation
necrosis soon after contact. The exothermic reaction pro-
duced by contact with strong acids or bases also contributes
to the depth of injury. Organic solvents and petroleum
products, which are highly lipid-soluble, injure tissues by
delipidation. Cutaneous absorption of certain chemical
agents may cause systemic toxicity, which complicates sub-
sequent therapy and makes identification of the causative
agent imperative.
Initial Care of Chemical Burns
Chemical injuries, unlike other thermal injuries, require
immediate care of the burn wound. The caustic agent must
be washed from the skin surface as soon as possible. All
clothing, including shoes and gloves, must be removed and
the wounds copiously irrigated with water. If possible,
lavage of chemical injuries should continue for at least 30
minutes. In the case of alkali burns, this treatment should
continue for a minimum of 1 hour. If ocular injury is sus-
pected, prompt and prolonged irrigation with saline or
water should begin. A search for specific antidotes is unnec-
essary and may only delay the initiation of adequate water
lavage. Assessing the depth of injury in chemical burns is
difficult because many agents may produce a tanned or
bronzed appearance of the skin, which remains pliable to
the touch but may represent extensive full-thickness tissue
necrosis. With the exception of the initial attention given to
the burn wound, the resuscitation and later treatment of
skin injury follow that of thermal burns.
Specific Chemical Agents & Systemic
Toxicities
In general, the use of antidotes for specific chemicals is con-
demned, and copious water lavage is considered the appro-
priate form of initial therapy. However, several specific
chemical agents exist for which treatment with a specific
antidote has proved beneficial. Injury owing to hydrofluo-
ric acid exposure is an occupational hazard of petroleum
refinery workers, etchers, and those employed in the clean-
ing of air-conditioning equipment. Following contact with
this agent, there is usually a pain-free interval followed by
pallor in the area of contact in association with severe tis-
sue pain. Fluoride ion continues to penetrate the tissues
until inactivated by calcium salt formation. Immediately
after exposure, the area should be copiously irrigated with
water. Topical treatment with a calcium gluconate gel
should be instituted, and if the pain does not subside, local
injection of 10% calcium gluconate into the damaged tissue
may provide prompt pain relief. Intraarterial infusion of
calcium gluconate also has been used to limit tissue damage
and relieve pain, but surgical excision of the damaged tissue
may be necessary for complete pain control. Hypocalcemia
may occur following extensive hydrofluoric acid burns.
Phenol
Phenol is an aromatic acid alcohol with high lipid solubility.
Initial treatment consists of copious water lavage; however,
owing to the poor water solubility of phenol, a lipophilic sol-
vent such as polyethylene glycol (50% solution in water) may
be more effective at removing the residual agent. Sufficient
systemic absorption of phenol produces CNS depression,
hypothermia, hemolysis, renal failure, and hypotension.
Maximal ICU support may be required. No specific antidote
is available.
Hydrocarbons
Cutaneous injury from immersion in gasoline and other
hydrocarbons is often overlooked in victims of motor vehicle
accidents who sustain prolonged exposure during extrica-
tion. Skin necrosis results from lipid dissolution. Partial- and
full-thickness injuries have been described, and systemic tox-
icity, similar to that produced by ingestion or inhalation, may
occur. The pulmonary excretion of hydrocarbons may pro-
duce chemical pneumonitis and bronchitis. Systemic lead
poisoning from cutaneous absorption of leaded gasoline also
has been described.
Inhalation of Aerosolized Chemicals
Inhalation of aerosolized chemicals may produce pulmonary
injury and systemic toxicity, thus requiring accurate diagno-
sis and aggressive treatment. Varying degrees of pulmonary
insufficiency may be agent-specific and manifested by severe
airway edema formation, mucosal sloughing, and bron-
chospasm. Systemic toxicity through pulmonary absorption
may occur; thus the causative agents must be clearly identi-
fied to ensure appropriate diagnostic and treatment strate-
gies. The degree of pulmonary support required is
determined by the severity of pulmonary insufficiency.
Ocular Injury
If chemical eye injury is suspected, prompt and prolonged
irrigation of the eye with water or saline should ensue. A spe-
cially designed scleral contact lens with an irrigating sidearm
CHAPTER 35
750
is useful when prolonged irrigation is necessary. Epithelial
defects may be identified by fluorescein stain.
Ophthalmology consultation should be obtained on all sus-
pected chemical eye injuries.
Mozingo DW et al: Chemical burns. J Trauma 1988;28:642–7.
[PMID: 3367407]
III. ELECTRICAL BURN INJURY
Tissue damage from electrical injury results from heat gener-
ated by the passage of electric current through the body as
well as direct thermal injury caused by the ignition of cloth-
ing. The severity of the injury depends on the voltage, the
type of current (alternating or direct), the path of the current
through the body, and the duration of contact. High- and
low-voltage injuries are arbitrarily defined as those above
and below 1000 V.
Tissue damage from electrical injury may be obvious at
the cutaneous contact site or sites but also may involve
underlying tissues and organs along the path of the current.
The amount of heat generated is proportionate to tissue
resistance; however, the differences in tissue resistance (eg,
bone, fat, nerve, etc.) are so small that the body acts as a
volume conductor. Current density then predominates as
the main determinant of tissue damage, with severity of
injury being inversely proportional to the cross-sectional
area traversed by current. Thus severe injuries to the
extremities are often encountered, and significant injuries
to the torso are rare. Superficial tissues in a limb may be
normal, whereas tissues near bone may be nonviable owing
to longer duration of heating because of the slower heat
dissipation from bone. Alternating current injuries may ini-
tiate ventricular fibrillation, whereas high-voltage injury
and lightning injury are associated with asystolic cardiopul-
monary arrest.
Treatment
Cardiac arrest often occurs following an electrical contact
and requires immediate cardiopulmonary resuscitation.
Patients with electric injury are more likely to have associ-
ated injuries owing to falls or tetanic skeletal muscle con-
tractions from the electric current; therefore, the patient’s
spine should be immobilized until cervical, thoracic, and
lumbar radiographs exclude the presence of spinal frac-
tures. In patients not sustaining an initial cardiac arrest,
cardiac dysrhythmias occur in a small percentage of
patients. All patients should have continuous electrocar-
diographic monitoring for at least 24 hours, and function-
ally significant dysrhythmias should be treated promptly if
they occur.
The estimation of resuscitation fluid requirements in
patients sustaining electrical injury is difficult owing to
extensive subcutaneous or deep tissue involvement with only
limited areas of cutaneous injury. This “iceberg” effect may
require the performance of fasciotomy—rather than
escharotomy—to ensure adequate perfusion of the distal
extremity and to evaluate the viability of the underlying sub-
cutaneous tissue and muscle. With extensive muscle necrosis,
hemochromogens may be liberated, resulting in the appear-
ance of those pigments in the urine. Intravenous fluids are
administered to achieve a urine output of 100 mL/h in
adults. If the hemochromogenuria does not clear with an
adequate urine output, 50 meq sodium bicarbonate should
be added to each liter of intravenous fluid to promote alkalin-
ization of the urine and prevent pigment precipitation in the
renal tubules. If after aggressive fluid resuscitation the renal
output does not reach 100 mL/h, an osmotic diuretic such as
mannitol also may be administered (a bolus dose of 25 g with
12.5 g added to each liter of IV fluid until pigment clearing
occurs) to force an increased urine output. When urine pro-
duction is increased by the use of diuretics, invasive hemody-
namic monitoring with a pulmonary artery catheter should
be considered because urine output is no longer a reliable
measure of intravascular volume and organ perfusion.
Complications
Associated injuries are more common in patients sustaining
electrical injury than those injured by thermal burns. Owing
to the titanic contractions of the paraspinal musculature
induced by the electric current, compression fractures of the
lumbar and thoracic spine may occur. Furthermore, many
electrical injuries involve workers who fall from heights.
Blunt traumatic injuries should be suspected and appropri-
ate diagnostic measures initiated.
A complete neurologic examination must be performed
on admission and at scheduled intervals in all patients sus-
taining electrical injury. Neurologic changes may be of early
or late onset. Immediate peripheral deficits owing to the
damaging effects of electric current may be irreversible; how-
ever, early deficits in a distribution where there is no clear tis-
sue damage are likely to resolve. Neurologic symptoms of
delayed onset, often mimicking upper motor neuron disease,
tend to be progressive and permanent. Progressive thrombo-
sis of nutrient vessels of the spinal cord or nerve trunks may
play a role in the pathogenesis of the late-occurring upper
motor neuron deficits.
Direct electrical injury to the viscera is rare; however, liver
necrosis, intestinal perforation, focal pancreatic necrosis, and
gallbladder necrosis have been reported in patients with
high-voltage electric injury and truncal contact points. An
increased occurrence of cholelithiasis has been reported in
convalescent patients following electric injury.
Delayed hemorrhage from moderate-sized to large blood
vessels has been described following electrical injury and
attributed by some to an “arteritis” produced by the electric
current. The actual mechanism of this complication is unclear,
but inadequate initial wound debridement and subsequent

BURNS
751
exposure and desiccation of the involved vessel appear to be
causative factors.
In patients in whom the electrical contact point involved
the head or neck, the development of cataracts up to 3 years
or more following injury has been described.
Ophthalmologic slit-lamp examination should document
the presence or absence of cataracts during the initial hospi-
talization. Additional information on electrical injuries is
presented in Chapter 37.
Grube BJ et al: Neurologic consequences of electrical burns. J
Trauma 1990;30:254–8.
Pruitt BA Jr, Mason AD: Lightning and electric shock. In
Weatherall DJ, Ledinghan JGG, Warrell DA (eds), Oxford
Textbook of Medicine, 2nd ed. New York: Oxford University
Press, 1987.
REFERENCES
Advances in understanding trauma and burn injury. J Trauma
1990;30:S1–211.
Demling RH: Burns. In Wilmore DW et al (eds), Care of the Surgical
Patient, Vol 1: Critical Care. New York: Scientific American, 1991.
McManus WF, Pruitt BA Jr: Thermal injuries. In Mattox KL, Moore
EV, Feliciano DV (eds), Trauma. Stanford, CT: Appleton & Lange,
1988.
Pruitt BA Jr, Goodwin CW Jr: Burns: Including cold, chemical and
electrical injuries. In Sabiston DC Jr (ed), Textbook of Surger y,
13th ed. Philadelphia: Saunders, 1986.
Pruitt BA Jr, Goodwin CW: Burn injury. In Moore EE (ed), Early
Care of the Injured Patient. New York: BC Decker, 1990.
Pruitt BA Jr: The universal trauma model. Bull Am Coll Surg
1985;70:2.

752
00
An integral part of the practice of critical care is treating the
patient who either intentionally or inadvertently ingests or is
exposed to a potentially toxic substance. The magnitude of this
problem is staggering. In 2002, the American Association of
Poison Control Centers documented 2,112,774 episodes of
toxin exposure resulting in poison center notification. This
number actually underrepresents the true number of poison-
ings because 70% are never reported to poison control centers.
Treating these patients requires a working understanding
of the principles of stabilization and supportive care, decon-
tamination, drug elimination, use of antidotes, and the
pathophysiologic features specific to the poisons or toxins
involved. This chapter will cover the general principles
involved in caring for these patients and will discuss the
details of treating the specific poisons typically encountered
in the practice of critical care.
EVALUATION OF POISONING IN THE ACUTE
CARE SETTING OR ICU
The pathophysiologic consequences following an exposure
are poison-specific, and adequate treatment requires an
understanding of these individual differences. However, there
are several general guidelines for the evaluation and treat-
ment of a patient with a potential ingestion or toxic exposure.
Diagnosis of Poisoning
History
Obtaining a history from a patient with a potential ingestion
or toxic exposure may be difficult if the patient is too young
to communicate, is obtunded, or is reluctant to cooperate. It
may be helpful to question the patient’s relatives, friends, or
coworkers to obtain additional historical information in
these cases. When getting the patient’s history, several points
require particular attention: the drugs or toxins involved, the
route of exposure (ie, oral, dermal, inhalation, etc.), and the
time of the exposure or ingestion. It is important to remem-
ber, however, that the history may be unreliable in patients
who intentionally ingest toxins. Careful physical examina-
tion is key, and laboratory evaluation and close observation
are frequently required.
Symptoms and Signs
The physical examination can provide a wealth of informa-
tion, even in patients unable to provide a useful history. An
abbreviated physical examination, which could be called the
toxidrome-oriented physical examination, focuses on the phys-
ical findings observed in patients exposed to particular types
of poisons and offers rapid assessment and guides testing and
treatment. This physical examination should include vital
signs, a brief neurologic examination emphasizing level of
consciousness and pupillary and motor responses, palpa-
tion of the skin for moisture and inspection for cyanosis
and rashes, auscultation and percussion of the lungs, and
auscultation of bowel sounds (Table 36–1). Table 36–2 sum-
marizes the physical findings associated with the major
groups of poisons and lists several examples of each.
Laboratory Studies
A rapid bedside serum glucose concentration should be checked
in all patients with altered mental status, and if it is found to be
low, intravenous glucose should be administered. Serum elec-
trolytes, blood urea nitrogen (BUN), serum creatinine, arterial
blood gas, serum osmolality, calculated osmolar gap, and a uri-
nalysis (ie, crystals, myoglobinuria or hemoglobinuria) are the
basic laboratory tests in the evaluation of patients with over-
doses (Table 36–3). Other tests (eg, drug levels, methemoglobin
level, and carboxyhemoglobin level) may be helpful in specific
patients and will be discussed later in this chapter.
As a general rule, toxicology screens are of limited value
in evaluation of these patients and are expensive and
36
Poisonings & Ingestions
∗
Diane Birnbaumer, MD
∗
Envenomation (snakebite, etc.) is discussed in Chapter 37.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
POISONINGS & INGESTIONS
753
time-consuming. In some specific situations, however,
screening may be helpful. These tests can be useful in nar-
rowing the differential diagnosis in patients who present
with altered mental status or abnormal vital signs; in such
cases, a directed toxicology screen should be ordered that
tests for agents consistent with the patient’s presentation and
physical findings. A toxicology screen also may be helpful in
patients with mixed-drug ingestions or those who present
with signs of major toxicity. Finally, a sample of blood may
be saved for future toxicology evaluation in patients in whom
the diagnosis is unclear.
Serum concentrations of some drugs are helpful in guid-
ing management decisions (Table 36–4). Salicylate, aceta-
minophen, barbiturates, digoxin, ethanol, iron, lithium, and
theophylline serum levels are available in most hospital lab-
oratories on an urgent basis. (Methanol and ethylene glycol
levels often need to be sent out; positive tests are often used
to confirm a suspected case, but management must begin
before levels are available.) Salicylate serum drug levels are
not necessary in all ingestion cases, an acetaminophen level
should be sent in virtually all cases. This drug is found in
many prescription and over-the-counter medications, and
patients may ingest potentially lethal amounts but show
minimal or nonspecific signs of toxicity.
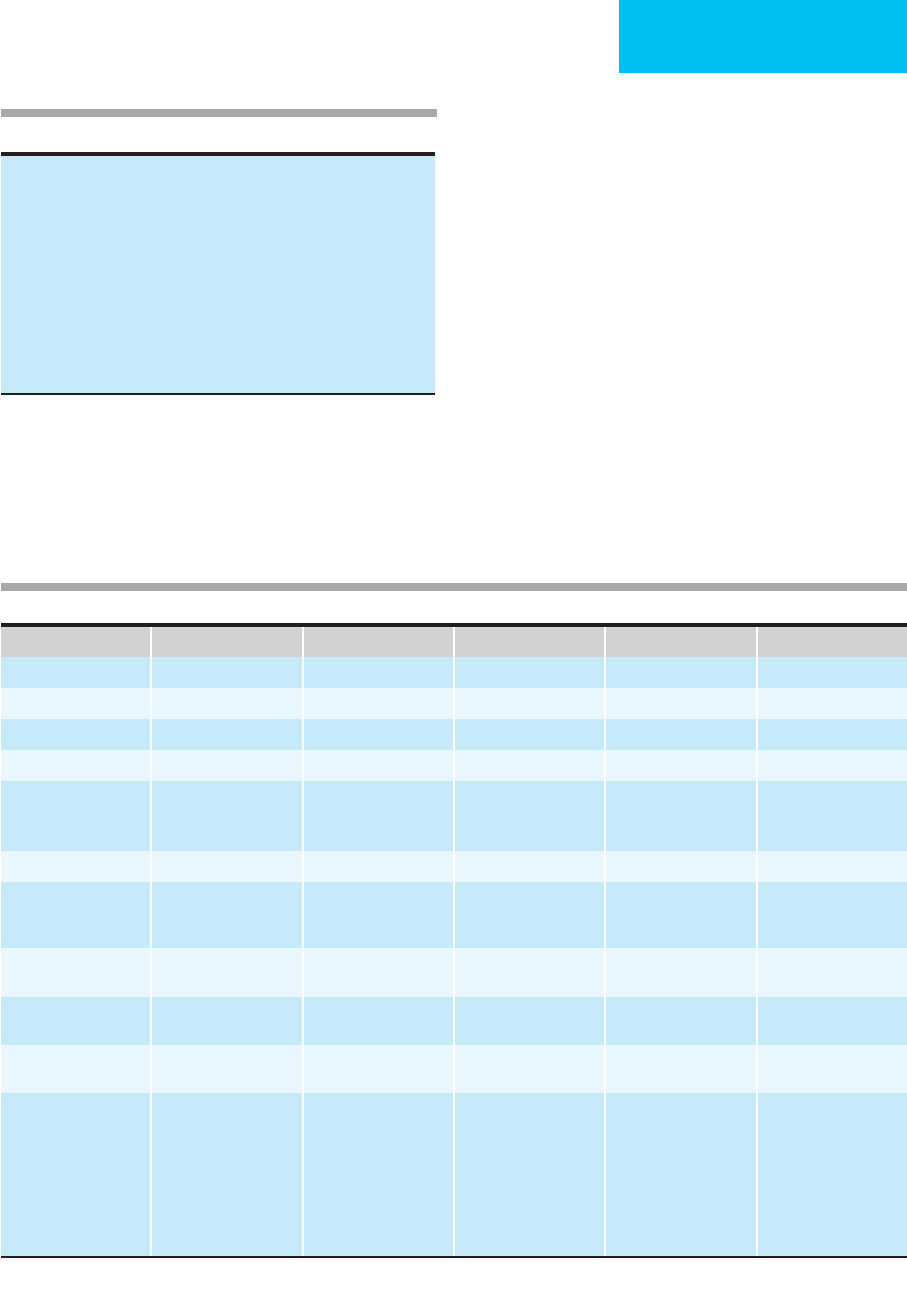
Physical Examination Sedative– Hypnotic Cholinergic Anticholinergic Sympathomimetic Sympatholytic
Temperature N/– N N/+ N/+/++ N/–
Respiratory rate N/–/– – +/– N/– +/– –
Heart rate N/– + or – +/++ ++ N/–
Blood pressure N/– + N/+ ++ N/–
Level of consciousness Normal
Obtunded
Comatose
Normal
Confusion
Coma
Delirium
Coma
Normal
Agitated
Paranoid, delusional
Normal
Lethargy, coma
Pupillary examination Miosis Miosis Mydriasis Mydriasis N or miosis
Motor responses N/– Weakness
Paralysis
Fasciculations
N N N
Skin, moisture N ++
Diaphoresis
Dry, hot Diaphoresis Dry
Lung examination N Bronchospasm
Bronchorrhea
N N N
Bowel sounds N/– ++
(SLUD)
–– N/– N/–
Examples Opioids
Benzodiazepines
Alcohols
Barbiturates
Organophosphates
Carbamates
Physostigmine
Edrophonium
Some mushrooms
Tricyclics
Phenothiazines
Antihistamines
Scopolamine
Amantadine
Cocaine
Amphetamine
Methamphetamines
Phenylpropanolamine
Ephedrine
Caffeine
Theophylline
Phencyclidine
Clonidine
SLUD = salivation, lacrimation, urination, defecation; N = no effect; + = increased; ++ = markedly increased; – = decreased; – – = markedly decreased.
Vital signs
Temperature
Blood pressure
Respiratory rate
Heart rate
Brief neurologic examination
Level of consciousness
Pupillary examination
Motor responses
Skin examination: moisture, rash, cyanosis
Lung examination
Auscultation for bowel sounds
Table 36–1. The toxidrome-oriented physical examination.
Table 36–2. Toxidromes.

CHAPTER 36
754
Electrocardiography
An ECG should be ordered in all patients with potential drug
ingestions. The heart rate, evidence of dysrhythmias, vector
axes, and interval measurements are helpful in determining
the presence or severity of several ingestions, and serial elec-
trocardiographic evaluation can, in some cases, help to fol-
low the progression of toxicity.
Imaging Studies
A plain abdominal film may be helpful in patients who ingest
radiopaque medications such as iron tablets or some enteric-
coated medications. These films also may be helpful in visu-
alizing drug packets in “body packers”—individuals who
ingest wrapped packets of illicit drugs to transport them.
Although the packages themselves are often not radiopaque,
they still may be visualized by the changes caused in bowel
gas patterns by their presence.
Differential Diagnosis of Poisoning
The differential diagnosis of the toxin-exposed patient is
extensive and varies with the agent involved. In general, how-
ever, infectious processes (eg, meningitis, encephalitis, and sep-
sis), metabolic disorders (eg, hypo- or hyperthyroidism, hypo-
or hyperglycemia, hypo- or hypercalcemia, and hypo- or
hypernatremia), and environmental disorders (eg, heat
stroke) are the most common other causes of the clinical
syndromes found in toxic exposures. Head trauma or hypox-
emia also may cause findings similar to those observed fol-
lowing toxin exposure.
Erickson TB et al: The approach to the patient with an unknown
overdose. Emerg Med Clin North Am 2007;25:249–81. [PMID:
17482020]
Mokhlesi B et al: Adult toxicology in critical care: I. General
approach to the intoxicated patient. Chest 2003;123:577–92.
[PMID: 12576382]
Lai MW et al: 2005 Annual Report of the American Association of
Poison Control Centers’ national poisoning and exposure data-
base. Clin Toxicol (Phila) 2006;44:803–932. [PMID: 17015284]
TREATMENT OF POISONING IN THE ICU
General Measures
The first priority in treating any patient with a toxic exposure
is resuscitation and stabilization; assessing the patient’s air-
way, breathing, and circulation are the initial goals. This may
require establishing an airway, ventilating and oxygenating
the patient, and supporting circulation by normalizing and
maintaining an adequate heart rate and blood pressure. These
measures should be taken regardless of the toxin involved;
more specific interventions can be made after stabilization is
completed. All overdose or toxin-exposed patients should be
placed on a cardiac monitor and given supplemental oxygen
if hypoxic. Intravenous access should be established.
Airway Management
Endotracheal or nasotracheal intubation is indicated in all
patients who are inadequately ventilating, those who have
significant hypoxemia, those who cannot protect their airway
because of obtundation or a poor gag reflex, or those with an
anticipated clinical course of deterioration. Intubation for
airway protection also should be considered in patients who
need gastric lavage, although this once frequently used prac-
tice is now indicated in only rare instances.
There are two potential situations where an obtunded
patient may not need intubation. Altered patients whose
rapid blood glucose is low may respond sufficiently to intra-
venous dextrose to obviate the need for intubation. (In
patients with suspected alcohol abuse or those who appear
significantly malnourished, administration of dextrose
should be preceded by a 100-mg dose of thiamine intra-
venously or intramuscularly.) Obtunded patients taking nar-
cotics or benzodiazepines may respond to administration of
naloxone or flumazenil (see “Antidotes” below).
Hemodynamic Support
Abnormal blood pressure, heart rate, and temperature should
be managed in the usual fashion; more specific interventions
Electrolytes
Serum glucose and rapid bedside glucose level
Blood urea nitrogen
Serum creatinine
Arterial blood gases
Serum osmolality
Calculated osmolal gap
Urinalysis
Electrocardiogram
Acetaminophen level
Other laboratory test (methemoglobin level, carboxyhemoglobin
level, etc) as indicated
Specific drug levels (as indicated)
Abdominal x-ray (as indicated)
Table 36–3. Screening evaluation of the poison-exposed
patient.
Salicylates Ethylene glycol
Acetaminophen Iron
Barbiturates Isopropyl alcohol
Digoxin Lithium
Ethanol Theophylline
Methanol
Table 36–4. Drug levels helpful in guiding management.

POISONINGS & INGESTIONS
755
or modifications of treatment can be addressed when more
information regarding the toxin involved is available.
Control of Seizures
Benzodiazepines should be used initially for the manage-
ment of seizures; phenytoin or barbiturates may be needed if
benzodiazepines are not effective. In cases of refractory
seizures, general anesthesia or the use of paralytic agents may
be required; in this case, electroencephalographic monitor-
ing should be instituted to determine if the patient continues
to have electrical seizure activity. It is important to note that
normalization of vital signs and control of seizures may
require interventions specific to the toxin involved (eg, pyri-
doxine for treating isoniazid ingestion).
Opioid and Benzodiazepine Antagonists
Comatose patients should receive naloxone, particularly if
they are hypoventilating and have miotic pupils. The usual
dose is 0.8 mg intravenously in both adults and children; if
there is a suspicion that the patient may be narcotic-
addicted, the dose should be titrated in increments of
0.2–0.4 mg to prevent abrupt withdrawal symptoms. Certain
opioid ingestions, particularly propoxyphene, may require
larger doses of naloxone to be effective. If this ingestion is
suspected, 2 mg naloxone should be administered.
Flumazenil—a benzodiazepine antagonist—may be indi-
cated in patients who present with obtundation or coma sus-
pected to be due to benzodiazepine ingestion. Since use of
this agent in the benzodiazepine-dependent patient may pre-
cipitate withdrawal seizures, this agent should be used with
extreme care in these patients if it is used at all. The initial
dose of flumazenil is 0.2 mg intravenously given over
30 seconds; if, after observation for 30 seconds, the patient
does not respond, an additional dose of 0.3 mg should be
given over 30 seconds. If additional doses are needed, 0.5 mg
should be given over 30 seconds at 1-minute intervals to a
total dose of 3–5 mg; if the patient does not respond to this
maximum dose, the primary cause of altered mental status is
unlikely to be due to benzodiazepines. Because the half-life of
flumazenil is approximately 1 hour (shorter than the half-life
of all currently available benzodiazepines), resedation occurs
in 50–65% of patients with benzodiazepine overdose. When
it occurs, the resedation is usually within 1–3 hours of
flumazenil administration; this necessitates close observation
of these patients.
Decontamination
After stabilization and initial basic therapeutic interventions
have been completed, decontamination should be addressed.
A. External Exposures—Patients who have dermal expo-
sure to a toxin should be undressed and copiously irrigated
with tepid water. Health care personnel must take appropri-
ate measures to ensure that they are not exposed to the agent
while caring for the patient. Irrigation also should be used in
patients with eye contamination, particularly with alkali or
acid substances.
B. Ingestions—Since the vast majority of poisonings occur
by ingestion, gastric emptying and gut decontamination have
been a mainstay of management. Studies have shown, how-
ever, that these interventions are of little benefit in most cases.
1. Syrup of ipecac—In the past, syrup of ipecac was used
extensively to induce gastric emptying in patients with toxic
ingestions, particularly children, but studies question the role
of ipecac in these situations. Ipecac is no longer recom-
mended for the treatment of most ingestions (see “Current
Controversies and Unresolved Issues” below).
2. Gastric lavage—Gastric lavage is a relatively effective
means of accomplishing gastric emptying, decreasing drug
absorption by as much as 50%. Studies of its impact on clin-
ical outcome in poisoned patients, however, have reported
conflicting results. Gastric lavage should not be used routinely
in all poisoned patients but may have a role in specific clini-
cal situations. Gastric lavage should be considered in patients
who present within 1 hour of ingesting a potentially lethal
amount of a toxin. Another possible indication is in poison-
ings with agents that decrease gastric motility (eg, anticholin-
ergic agents), although utility in these cases is questionable.
Gastric lavage may be useful when patients ingest agents that
bind poorly to activated charcoal and in life-threatening poi-
sonings with agents such as theophylline, tricyclic antidepres-
sants, and cyanide. Table 36–5 summarizes these indications.
When gastric lavage is performed, the patient should be
placed in the head-down lateral position. Owing to the risk
of aspiration, gastric lavage never should be performed with
the patient supine, particularly if the patient is in restraints
and cannot be turned quickly if emesis occurs. Suction
equipment should be available at all times. A large-bore gav-
age tube (ie, 36–42F in adults and 16–32F in children) should
be used to remove large pill fragments and whole pills. Some
authors recommend that extra holes be cut along the sides of
the distal end of the tube to facilitate pill removal. Since these
tubes are large, they should not be passed through the nose;
oral passage is better tolerated and has fewer complications.
Once gastric tube position is confirmed, aspiration of the
stomach should be performed to remove as much of the
Recent ingestion (<1 hour) of a potentially life-threatening poison
Ingestion of a substance that slows gastric emptying (eg, anticholinergic
medications)
Ingestion of a poison that is slowly absorbed from the gastrointestinal
tract
Ingestion of a substance that does not bind well to activated charcoal
(eg, iron, lithium)
Ingestion of specific life-threatening poisons (eg, tricyclic antidepres-
sants, theophylline, cyanide)
Table 36–5. Indications for gastric lavage.
CHAPTER 36
756
poison as possible before irrigation is instituted. Once aspi-
ration is complete, tepid tap water should be used for gastric
lavage. In patients under age 5, normal saline should be used
to prevent electrolyte disturbances. Using 150–300-mL
aliquots (50–150 mL in children), the fluid should be alter-
natively instilled down the tube and then allowed to efflux
from the stomach by gravity; amounts in excess of 300 mL
increase the risk of emesis and aspiration. Lavage should be
continued until the effluent fluid is clear of pill fragments. If
activated charcoal and a cathartic is to be used, it can be
placed down the lavage tube before it is withdrawn.
Several complications are associated with gastric lavage.
Aspiration and subsequent pneumonitis can occur; there-
fore, it is critical that patients who cannot protect their air-
ways be intubated prior to gastric lavage. Esophageal
perforation has been reported, as has inadvertent tracheal
tube placement (with subsequent instillation of lavage fluid
into the lungs). Children under the age of 5 years may
develop electrolyte imbalances if normal saline is not used as
the lavage fluid. Laryngospasm and cardiac dysrhythmias
also have been described.
Gastric lavage has only one absolute contraindication—it
should not be used in caustic ingestions because it may cause
the patient to vomit, leading to more extensive esophageal
and oral burns.
3. Charcoal—Activated charcoal is an odorless, tasteless
powder that is beneficial in many types of ingestions and is
the cornerstone of therapy for most cases. In the gut, it binds
the toxin and prevents its absorption. Although it binds
many compounds, there are several potentially life-
threatening poisons that do not bind well to charcoal
(Table 36–6). When used in repeated doses, activated char-
coal can both interrupt enterohepatic circulation and
enhance the elimination of some drugs that have already
been absorbed from the GI tract (Table 36–7); this is referred
to as gastrointestinal dialysis. When used in this fashion, the
dose of activated charcoal should be 25–50 g orally every 2–4
hours; in children, it is 0.25–1 g/kg every 2–4 hours.
Activated charcoal is administered as a slurry of water
and charcoal. Although the initial dose is 50–100 g orally in
adults and 1–2 g/kg in children, when the amount of ingested
agent is known, the optimal dosing of activated charcoal is in
a ratio of 10:1, charcoal to ingested agent.
The only relative contraindication to giving charcoal is in
patients with caustic ingestions; the charcoal accumulates in
burned areas of the GI tract and interferes with endoscopy.
The most common complication of charcoal administration
is constipation. This problem can be addressed by adding a
cathartic to the charcoal. If repeat-dose activated charcoal
therapy is to be used, the cathartic should be added only to
the first dose of charcoal because the every 2–4-hour dosing
of the repeat-dose activated charcoal regimen can lead to
excessive cathartic administration and possible electrolyte
imbalances from the resulting diarrhea. In addition, some
children have become hypermagnesemic when magnesium
citrate was used as the cathartic. The most common cathartics
used in this situation are 70% sorbitol (1 g/kg), magnesium
citrate (4 mL/kg), and 10% magnesium sulfate (250 mg/kg).
4. Bowel irrigation—Whole bowel irrigation is a method
of removing ingested toxins from the gut by forcing the toxin
rapidly through the GI tract. Indications for whole bowel
irrigation are limited; the most common use of this tech-
nique is in patients who intentionally ingest packets of illicit
compounds such as cocaine or heroin in order to transport
them without detection. The other indication for this ther-
apy is in patients who ingest potentially lethal toxins that are
difficult to remove from the stomach and do not bind well to
charcoal (eg, iron).
The technique for whole bowel irrigation involves admin-
istration of 1–2 L of polyethylene glycol electrolyte solution
per hour, either orally or via a nasogastric tube. In children
under the age of 5 years, the solution should be given at a rate
of 150–500 mL/h. The goal is to produce a rectal discharge
with the same appearance as the administered oral solution,
which indicates complete cleansing of the gut. Effective
whole bowel irrigation usually takes 6–12 hours. The patient
must be able to cooperate and sit either on a toilet or a bed-
side commode during the procedure.
The only contraindications to this procedure are the pres-
ence of ileus, GI perforation, and bleeding. It should not be
used in patients who are uncooperative or combative or in
those with CNS depression or respiratory distress. The compli-
cations associated with whole bowel irrigation are abdominal
Bromides
Caustics
Cyanide
Ethylene glycol
Heavy metals
Iron
Isopropyl alcohol
Lithium
Methanol
Table 36–6. Poisons not well bound by activated charcoal.
Carbamazepine
Diazepam
Digitalis
Phenobarbital
Phenytoin
Salicylates
Theophylline
Tricyclic antidepressants
Table 36–7. Some drugs amenable to repeat-dose
activated charcoal therapy.
