Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

BURNS
737
(eg, collagenase, protease, etc.), bacterial motility, and antibi-
otic resistance may be important in the pathogenesis of
eschar penetration and invasion of viable tissues.
Although the use of topical chemotherapeutic agents and
the timely excision and grafting of the burn wound have
decreased the incidence of invasive burn wound infection in
most U.S. burn centers, this problem has not been eliminated
entirely. Invasive burn wound infection is uncommon in sec-
ond-degree burns and in patients with burns of less than
30% of the body surface. Extremes of age and increasing size
of burn strongly influence the risk of developing invasive
burn wound infection.
Clinical Features
A. Symptoms and Signs—Clinical signs of invasive burn
wound infection are often indistinguishable from those
observed in uninfected hypermetabolic burn patients or
burn patients with other sources of sepsis and include
hyper- or hypothermia, tachycardia, tachypnea, ileus, glu-
cose intolerance, and disorientation. Tinctorial and physical
changes in the appearance of the burn wound are more reli-
able signs of invasive burn wound infection (Table 35–5).
The development of clinical signs and symptoms of sepsis in
the thermally injured patient should prompt a thorough
examination of the burn wound to identify areas suspicious
for invasive infection.
B. Laboratory Findings—Surface cultures of the eschar can-
not distinguish colonization from invasive infection.
Quantitative bacteriologic cultures of burn wound tissue
correlate poorly with the presence of invasive burn wound
infection. Quantitative bacteriologic counts less than 10
5
per
gram of biopsy tissue correlate with absence of invasive burn
wound infection; however, even when quantitative counts
exceed 10
5
organisms per gram of biopsy tissue, histologic
examination confirms invasive infection in less than half of
biopsy specimens.
Histologic examination of a biopsy of the burn wound
and underlying viable tissue is the most rapid and reliable
method for differentiating microbial colonization of nonvi-
able eschar from microbial invasion of viable subeschar tis-
sue. The latter defines invasive burn wound infection. A burn
wound biopsy is performed as an ICU procedure. A 500-mg
elliptical biopsy (0.5 × 1.0 cm) including subjacent unburned
tissue is obtained by scalpel dissection from the area of the
burn wound identified as suspicious for infection. Hemostasis
is achieved by application of direct pressure or by electroco-
agulation. Half the specimen is cultured for organism identi-
fication and antibiotic sensitivities, and the other half is
submitted for histologic analysis. The presence of microor-
ganisms in viable tissue confirms the diagnosis of invasive
burn wound infection. The histologic staging scheme for
burn wound colonization and infection is presented in
Table 35–6. If only colonization (stage 1A to stage 1C) is pres-
ent, no specific change in antimicrobial therapy is indicated
unless serially obtained specimens document a progression of
colonization stage. If stage 2 (invasion) is reported, prompt
treatment for invasive burn wound infection should begin.
Treatment
When the diagnosis of invasive burn wound infection is
made, local and systemic antimicrobial therapy is initiated.
In the case of bacterial burn wound invasion, topical
chemotherapy should be in the form of twice-daily applica-
tions of mafenide acetate because of its superior eschar pen-
etration. Systemic antibiotic therapy is initiated based on
prior surface cultures or burn center organism prevalence.
Further refinements in therapy are based on biopsy, culture,
and sensitivity results. Customary critical care supportive
measures are employed to maintain hemodynamic and res-
piratory stability. Subeschar antibiotic clysis of the infected
area with a broad-spectrum penicillin is recommended at
12 hours and immediately prior to operation to minimize
the risk of hematogenous seeding and florid septic shock at
the time of eschar excision. Half the daily dose of a broad-
spectrum penicillin (eg, piperacillin or ticarcillin) delivered
in 1 L of normal saline is infused into the subeschar tissues
by means of a no. 20 spinal needle. Excision of the burn
wound to the level of the investing fascia is employed to
ensure removal of all nonviable tissue. The wound is usually
treated with moist dressings of 5% mafenide acetate, 0.5%
silver nitrate, or a biologic dressing. The patient is returned
to the operating room in 24–48 hours for wound inspection
and redebridement or split-thickness skin grafting as needed.
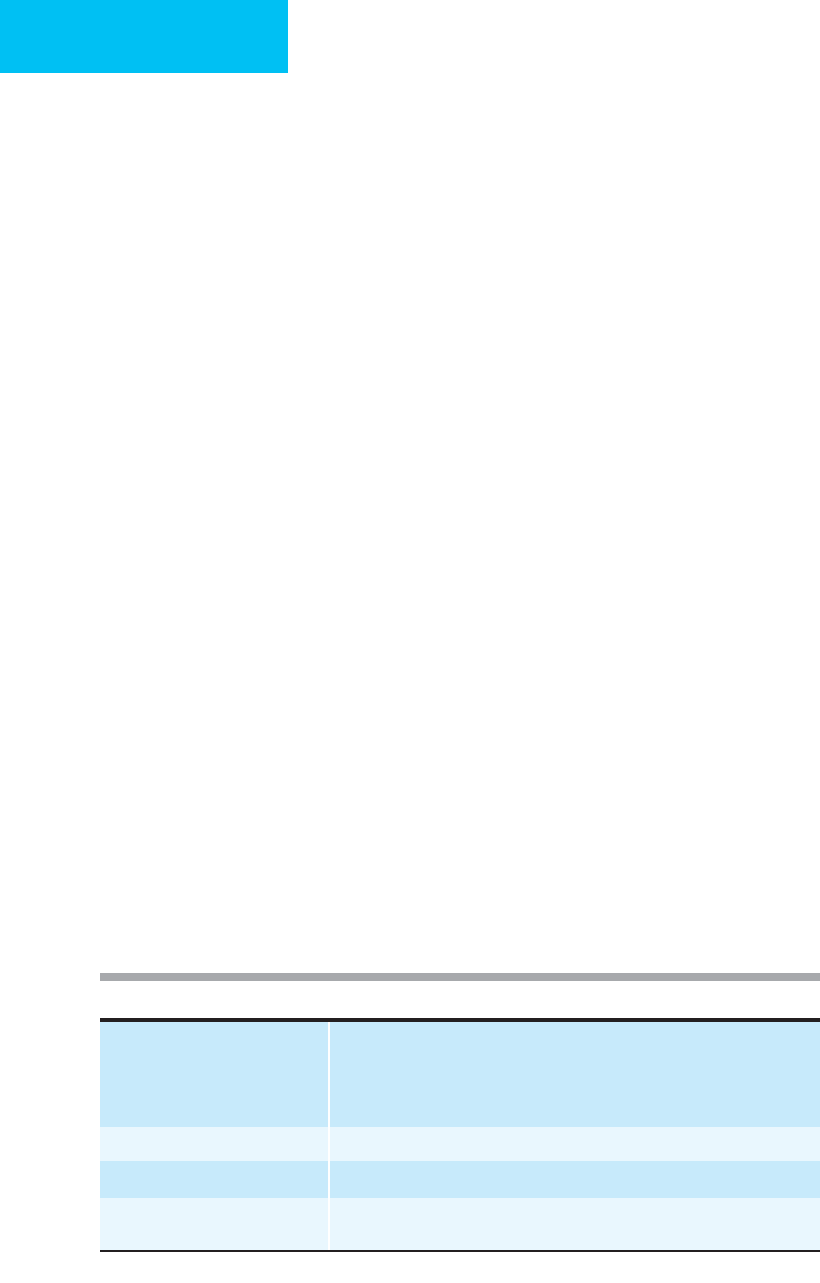
Stage I: Colonization
A. Superficial: Sparse microbial population on burn wound surface.
B. Penetration: Microorganisms present in variable thickness of eschar.
C. Proliferation: Dense population of microorganisms at interface of
nonviable and viable tissue.
Stage II: Invasion
A. Microinvasion: Microscopic foci of microorganisms in viable tissue
immediately subjacent to subeschar space.
B. Generalized: Widespread penetration of microorganisms deep into
viable subcutaneous tissues.
C. Microvascular: Involvement of lymphatics and microvasculature.
Table 35–6. Histologic staging of burn wound infection.
Table 35–5. Clinical signs of burn wound infection.
Conversion of second-degree burn to full-thickness necrosis
Focal dark brown or black discoloration of wound
Degeneration of wound with “neoeschar” formation
Unexpectedly rapid eschar separation
Hemorrhagic discoloration of subeschar fat
Erythematous or violaceous, edematous wound margin
Metastatic septic lesions in unburned tissue

CHAPTER 35
738
In addition to bacteria, fungi and yeasts also cause inva-
sive burn wound infection and have become the predomi-
nant organisms causing burn wound infection because
topical therapy and early excision have reduced the incidence
of bacterial infection. Candida species commonly colonize
wounds but rarely cause invasive burn wound infection.
Aspergillus, the most common filamentous fungus that
causes invasive burn wound infection, usually remains con-
fined to subcutaneous tissues and seldom transverses fascial
planes. Wounds colonized by Candida or Aspergillus can be
treated with topical application of clotrimazole, but histo-
logic evidence of invasion requires surgical burn wound exci-
sion and initiation of systemic amphotericin B therapy. The
Phycomycetes often behave in a manner similar to
Aspergillus; however, these organisms may spread rapidly
along tissue plains, invade blood vessels, and penetrate fascia.
Aggressive wide debridement, including amputation, may be
necessary to control these infections.
Becker WK et al: Fungal burn wound infection: A 10-year experi-
ence. Arch Surg 1991;126:44–8. [PMID: 1985634]
McManus AT: Pseudomonas aeruginosa: A controlled burn
pathogen? Antibiot Chemother 1989;42:103–8. [PMID: 2512832]
McManus WF, Goodwin CW Jr, Pruitt BA Jr: Subeschar treatment
of burn-wound infection. Arch Surg 1983;118:291–4. [PMID:
6824429]
Pruitt BA Jr: The diagnosis and treatment of infection in the burn
patient. Burns Incl Ther Inj 1984;11:79–91. [PMID: 6525539]
Waymack J, Pruitt BA Jr: Burn wound care. Adv Surg 1990;23:
261–89. [PMID: 2403460]
Burn Wound Excision & Grafting
Technique
The current operative management of burns employs tan-
gential excision of eschar to viable dermis or fat and scalpel
excision to the level of the investing fascia for burn wound
removal. Burn wound excision may be performed early in
the postburn course once the patient is hemodynamically
stable and resuscitation is complete.
The operative procedure should be limited to excision of
20% of the body surface area, an area of excision producing
a blood loss equal to the patient’s blood volume, or 2 hours
of operative time. Careful anesthetic management is impera-
tive to avoid hypotension and hypothermia. Hypotension
may impair blood flow to areas of second-degree burn,
resulting in ischemia of the wound and conversion to full-
thickness injury. The depth of excision in tangential and
sequential burn wound removal is governed by the appear-
ance of healthy tissue and punctate bleeding from dermal
beds. Scalpel excision of burns involves removal of the
wound and underlying subcutaneous tissue to the level of the
investing muscle fascia. This may be accomplished more rap-
idly and with significantly less blood loss than tangential or
sequential wound excisions. Once a viable wound surface is
obtained, wound coverage is accomplished with autograft or
biologic dressings.
Conventional skin grafting is achieved with cutaneous
autografts 0.008–0.012 inches thick. These grafts may be
employed as a sheet graft or meshed to provide expansion
ratios ranging from 1.5:1 to 9:1. Expansion ratios of 4:1 or
greater require a prolonged time for interstitial closure, have a
greater propensity for scar formation, and are used only in
patients with massive burns and limited donor sites. Following
grafting, occlusive dressings moistened with topical antibiotic
agents are applied. The wounds are kept moist to prevent des-
iccation until the interstices of the graft have epithelialized.
Skin Substitutes and Biologic Dressings
In massively burned patients, the disparity between donor-
site area and burn-wound area requires the use of temporary
skin substitutes or biologic dressings to effect wound closure
while awaiting donor-site availability. Biologic dressings pre-
vent desiccation of the wound bed, decrease protein and
fluid losses, promote angiogenesis of granulation tissue, and
reduce pain. Viable cadaver allograft currently provides the
best temporary wound coverage. Allograft becomes vascular-
ized from the underlying wound bed and usually remains
adherent until surgically excised or immunologically rejected
by the patient. As a result of the immunosuppression associ-
ated with thermal injury, the allograft may remain intact,
vascularized, and viable for several weeks following applica-
tion. The same theoretical risks of disease transmission (eg,
hepatitis, HIV infection, etc.) associated with organ donation
apply to the use of cadaveric allografts. Appropriate tissue
banking measures are imperative. In addition to fresh
cadaver allograft, frozen and lyophilized allograft is available
from many sources.
Porcine xenograft is also available as a fresh, frozen, or
lyophilized preparation. Advantages include an abundant
supply and lower cost. This biologic dressing, however, does
not become vascularized and adheres to the wound bed by
fibrin bonding. The underside of the graft is nourished by
the plasma circulation, and desiccation and necrosis of the
outer surface usually occur within 1 week. Application of
porcine cutaneous xenografts to superficial partial-thickness
wounds facilitates healing and decreases pain. Porcine
xenografts are of limited usefulness in the coverage of excised
wounds because of their lack of vascularization and the lim-
ited time until desiccation and necrosis occur.
Several synthetic skin substitutes have been developed in
an attempt to avoid the problems of disease transmission and
storage requirements common to biologic dressings. The
most successful materials have been of a bilaminated config-
uration with an outer layer mimicking epidermis that allows
water vapor transmission and prevents bacterial contamina-
tion. The inner dermal layer is designed to promote adher-
ence and fibrovascular ingrowth from the wound bed.
Biobrane is currently the most commonly used synthetic skin
BURNS
739
substitute. The epidermal layer is composed of pliable Silastic,
and the dermal component is derived from porcine collagen.
This product is available with a variety of pore sizes, and its
elastic nature allows freedom of motion and is well adapted to
body contours. Biobrane promotes healing of second-degree
burns and usually provides adequate short-term coverage for
excised wounds, although submembrane suppuration and
lack of adherence cause difficulties. Integra is a synthetic der-
mal substitute that is unique in that a neodermis is formed by
fibrovascular ingrowth into a glycosaminoglycan matrix der-
mal analogue. The epidermal component is Silastic and is
removed once the dermal analogue is vascularized, allowing
definitive closure of the wound with ultrathin split-thickness
autografts. This permits more rapid healing of donor sites for
repeated autograft harvesting. Incomplete adherence, sub-
membrane suppuration, and technical problems with the
application of ultrathin autografts have been observed.
TransCyte is a bilaminated biosynthetic skin substitute
used as a temporary dressing on second-degree burns or
excised full-thickness burns. This product is composed of
Biobrane on which human foreskin-derived neonatal dermal
fibroblasts are seeded and grown to confluence in culture.
The fibroblasts secrete matrix proteins and growth factors
that remain active after the product is frozen. Application of
TransCyte to the wound surface is similar to that of
Biobrane. It also carries the same limitations.
The availability of commercial laboratories capable of
carrying out skin culture techniques has led to the recent
evaluation of cultured autologous keratinocytes for coverage
of wounds in massively burned patients. Current culture
techniques require 3 or more weeks of preparation for a
product six to eight epidermal cells in thickness. These grafts
are quite fragile and susceptible to bacterial colonization of
the recipient wound bed and minimal shear forces. The use
of cultured autologous keratinocytes to effect wound closure
in massively burned patients was studied recently. In a series
of 16 patients with an average burn size greater than 60% of
BSA, definitive final engraftment covered only 4.7% of the
body surface area at a cost of over $9000 per percent of BSA
closed. Wound bed microbial colonization, lack of dermal
elements, and patient age may be significant factors relating
to the failure of culture-derived cells as a definitive form of
burn wound coverage. This technology has the potential for
providing timely coverage of large surface areas but is
presently limited by the aforementioned problems.
Caruso DM et al: Randomized clinical study of Hydrofiber dressing
with silver or silver sulfadiazine in the management of partial-
thickness burns. Burn Care Res 2006;27:298–309. [PMID:
16679897]
Hansbrough JF: Current status of skin replacements for coverage
of extensive burn wounds. J Trauma 1990;30:S155–60. [PMID:
2254975]
Hansbrough JF et al: Burn wound closure with cultured autolo-
gous keratinocytes and fibroblasts attached to a collagen-
glycosaminoglycan substrate. JAMA 1989;262:2125–30.
Heimbach D et al: Artificial dermis for major burns: A multicenter
randomized clinical trial. Ann Surg 1988;208:313–20.
Pruitt BA Jr, Levine NS: Characteristics and uses of biologic dress-
ings and skin substitutes. Arch Surg 1984;119:312–22. [PMID:
6365034]
Pruitt BA Jr, McManus WF, McDougal WS: Surgical management
of burns. In Nora FP (ed), Operative Surgery: Principles and
Techniques. Philadelphia: Saunders, 1990.
Inhalation Injury
ESSENTIALS OF DIAGNOSIS
Facial burns.
Intraoral burns or carbonaceous sputum.
Edema, erythema, mucosal ulcerations on laryngoscopy.
Increased
133
Xe retention.
Decreased Pao
2
and expiratory flow rates.
General Considerations
Pulmonary injury from smoke inhalation is frequently
observed in patients with thermal injury who require admis-
sion to a burn center. In a recent series, 33% of patients had
concomitant inhalation injury. The injury caused by the
inhalation of smoke or toxic gases may include chemical
damage to the respiratory system, carbon monoxide toxicity,
and infrequently, direct thermal injury to the tracheo-
bronchial tree. Patients most likely to have inhalation injury
are those with burns sustained in a closed space and those
who were burned during a period of depressed conscious-
ness secondary to head trauma or drug intoxication.
Direct thermal injury to the airway is encountered rarely
in patients who survive a fire and are hospitalized for treat-
ment. However, autopsy series of patients dying at the scene
of a fire frequently reveal devastating direct thermal injury to
the airways. The effective cooling capabilities of the
nasopharynx and oropharynx prevent significant heat expo-
sure of the lower respiratory system; however, direct thermal
injury to the supraglottic airway does occur and may lead to
upper airway obstruction. An exception is burns caused by
exposure to steam because water has a heat-carrying capac-
ity 4000 times greater than that of air.
Smoke inhalation—particularly when the injury occurred
in a closed space—may be associated with carbon monoxide
poisoning, which may impair tissue oxygenation. The pres-
ence of carboxyhemoglobin or the chemical alteration of the
cytochrome system by carbon monoxide does not affect the
amount of dissolved oxygen in the blood; thus the Pa
O
2
will
remain normal. However, saturation of hemoglobin by oxy-
gen may be markedly reduced, impairing oxygen delivery.
The inhalation of smoke (incomplete products of combus-
tion) is manifest by deleterious effects on both the airway and

CHAPTER 35
740
the pulmonary vasculature. The anatomic location of pul-
monary injury depends on the size of the inhaled particle.
When the particle diameter is less than 0.05 μm, the larger,
endoscopically visible airways may appear normal in the pres-
ence of severe alveolar and terminal bronchiolar inflammatory
damage. Alternatively, the larger airways may be severely
inflamed, leading to mucosal ulceration or necrosis in the pres-
ence of relatively normal gas exchange and alveolar function.
In various animal models of inhalation injury, increased
pulmonary microvascular permeability and peribronchial
edema have been reproduced. Thromboxane A
2
levels have
been found to increase within 5 minutes of inhalation injury,
with levels correlating with increases in lung lymph flow and
extravascular lung water. The role of the neutrophil in the
pathophysiology of smoke inhalation is currently under
investigation. Both the preinjury induction of a neutropenic
state by administration of mechlorethamine and postinjury
treatment with pentoxifylline have been reported to attenu-
ate pulmonary artery hypertension, reduce pulmonary vas-
cular resistance, and decrease the severity of pulmonary
insufficiency following smoke exposure in animals. Although
alterations in surfactant function have been described fol-
lowing smoke inhalation, surfactant replacement has not
been shown to improve pulmonary function in animal mod-
els of inhalation injury.
Clinical Features
A. Symptoms and Signs—Smoke inhalation should be sus-
pected in patients with facial burns, singed facial hair and
nasal fibrissae, intraoral burns or carbonaceous deposits in the
oropharynx, or a history of being burned in a closed space.
B. Bronchoscopy—The diagnosis of inhalation injury is
made by examination of the upper airway and tracheo-
bronchial tree by fiberoptic bronchoscopy. Direct laryn-
goscopy also may be used to visualize the upper airway. The
presence of carbonaceous material, edema, erythema, or
mucosal ulcerations below the vocal cords confirms the diag-
nosis. An endotracheal tube of appropriate size should be
placed over the fiberoptic bronchoscope before the examina-
tion so that intubation may be readily achieved if the appear-
ance of upper airway edema threatens airway patency.
False-negative bronchoscopic examinations occur occasion-
ally and usually are secondary to the failure to observe
inflammation and erythema in the hypovolemic patient with
impaired tracheal mucosa perfusion.
C. Radionuclide Studies—
133
Xe ventilation-perfusion lung
scans may be performed in patients in whom the clinical sus-
picion of inhalation injury is high yet the bronchoscopic
examination appears relatively normal. After intravenous
injection of 10 μCi of
133
Xe, serial chest scintigraphs are
obtained. Retention of the gas in the lungs for over 90 seconds
following injection or an unequal distribution of radiation
density is considered diagnostic of inhalation injury. The false-
negative and false-positive rates from this study are 5% and 8%,
respectively. False-negatives result from marked hyperventila-
tion and false-positives from preexisting chronic obstructive
pulmonary disease (COPD), bronchitis, or atelectasis.
D. Respiratory Function Studies—Measurements of pul-
monary function also may be helpful in establishing the
diagnosis of inhalation injury. Burn patients with inhalation
injury may have a decreased Pa
CO
2
and peak expiratory flow
and an increased ventilation-perfusion gradient, airway
resistance, and nitrogen washout slope. Static and dynamic
compliance tends to be normal in the early phase of inhala-
tion injury. The complexity of some pulmonary function
tests and the requirement for full patient cooperation often
limit their clinical usefulness as aids to the early diagnosis of
inhalation injury.
The diagnosis of inhalation injury can be made with 96%
accuracy when the results of fiberoptic bronchoscopy, venti-
lation-perfusion scanning, and pulmonary function testing
are combined. Overdiagnosis of inhalation injury accounts
for the 4% error.
Treatment
A. General Measures—The current treatment of inhalation
injury is primarily supportive because no specific agent has
been identified that minimizes the severity of the insult. The
aim of treatment, therefore, is to correct the underlying pul-
monary insufficiency while minimizing further iatrogenic
pulmonary insults. The amount of intervention required is
guided by the severity of pulmonary insufficiency.
B. Respiratory Support—Patients with mild disease require
only administration of humidified oxygen-enriched air (usu-
ally 40%) and noninvasive pulmonary physiotherapy. Severe
injury may require maximal mechanical ventilatory support
and frequent flexible fiberoptic or rigid bronchoscopy to
clear the airways of sloughed mucosal debris and secretions.
Small-airways disease may produce significant atelectasis
requiring increased oxygen administration and institution of
positive end-expiratory pressure. Systemic administration of
steroids has not decreased morbidity or mortality rates in
patients with inhalation injury, and such treatment has been
reported to increase infectious complications.
A recent clinical trial of the prophylactic use of high-fre-
quency percussive ventilation in patients with inhalation
injury demonstrated significant improvements in morbid-
ity and mortality rates compared with conventional volume
ventilation. Fifty-four burn patients with documented
inhalation injury were managed by this type of ventilation
within 24 hours of intubation. Fourteen patients (25.9%)
developed pneumonia, compared with a predicted histori-
cal frequency of 45.8%. The observed mortality rate was
18.5% compared with a historical frequency of 35%. Only
4 of the 10 deaths were attributable to pulmonary failure.
Although the exact mechanism by which high-frequency
percussive ventilation improves outcome is not known, the
ability to maintain ventilation and oxygenation at lower peak

BURNS
741
airway pressures and inspired oxygen concentrations may
reduce the iatrogenic injury associated with the use of
volume-controlled ventilators. The high frequency percussive
breaths also improve clearance of secretions—similar to results
obtained with high-frequency oscillators and jet ventilators.
C. Antimicrobial Therapy—Bronchopneumonia is the most
common cause of morbidity and death in patients with
inhalation injury. The daily chest roentgenograph should be
examined carefully. Appropriate antimicrobial therapy is ini-
tiated based on the presence of pulmonary infiltrates and
sputum leukocytosis. Pneumonia occurring after inhalation
injury usually is caused by gram-positive organisms. Gram-
negative pneumonias, which now occur infrequently, usually
develop later in the hospital course. Therapy is initiated
based on the results of the sputum Gram stain, with refine-
ments of antibiotic choice depending on endobronchial cul-
ture and microbial sensitivity testing.
Prognosis
Smoke inhalation, in the absence of cutaneous thermal
injury, is almost always treated successfully by supportive
measures. The tracheobronchial mucosa typically heals com-
pletely in 2–3 weeks. However, when smoke inhalation
occurs in the presence of moderate to severe cutaneous burn,
mortality rates are increased by as much as 20% over those
predicted by the age of the patient and the extent of injury.
When pneumonia complicates inhalation, the mortality rate
may rise to 60% above the predicted level.
Cioffi WG et al: High-frequency percussive ventilation in patients
with inhalation injury. J Trauma 1989;29:350–4. [PMID:
2926848]
Cioffi WG et al: Prophylactic use of high-frequency percussive ven-
tilation in patients with inhalation injury. Ann Surg
1991;213:575–80. [PMID: 2039288]
Huang Y, Li A,Yang Z: Effect of smoke inhalation injury on throm-
boxane levels and platelet counts. Burns Incl Therm Inj
1988;14:440–6. [PMID: 3250716]
Pruitt BA Jr et al: Evaluation and management of patients with
inhalation injury. J Trauma 1990;30:S63–8. [PMID: 2254994]
Shirani KZ, Moylan JA Jr, Pruitt BA Jr: Diagnosis and treatment of
inhalation injury. In Loke J (ed), Pathophysiology and Treatment
of Inhalation Injuries. New York: Marcel Dekker, 1988.
Shirani KZ, Pruitt BA Jr, Mason AD Jr: The influence of inhalation
injury and pneumonia in burn mortality. Ann Surg
1987;205:82–7. [PMID: 3800465]
POSTRESUSCITATION PERIOD
Prevention & Treatment of Complications
1. Infection Control
Infectious complications always have been the predominant
determinant of outcome in thermally injured patients.
Improved care of critically ill patients and the control of
burn wound sepsis through effective topical antimicrobial
agents and timely excision and grafting have resulted in the
salvage of more burn patients who previously would have
died in the early postburn period. The hospital course of
nonsurvivors also has been prolonged. Since infection con-
tinues as the leading cause of morbidity and death in burn
patients, prolonged hospitalization increases the risk of col-
onization and infection by nosocomial organisms that are
predominantly true fungi, yeasts, and multiply-antibiotic-
resistant bacteria.
A strict infection control program can minimize the clin-
ical impact of exposure to nosocomial pathogens during a
prolonged hospital stay in an immunocompromised patient.
Such a program might employ scheduled microbial surveil-
lance, an actively functioning infection control committee,
environmental monitoring procedures, biopsy monitoring of
the burn wound, and cohort patient care as deemed neces-
sary. The surveillance program includes thrice-weekly cul-
tures of sputum and the burn wound surface and
twice-weekly culturing of urine and stool. Multiple antibiotic
sensitivities are determined for all staphylococci as well as all
Pseudomonas species and other gram-negative organisms
recovered from routine cultures. Reports are provided on a
daily basis, enabling initial empirical selection of antibiotics
to be made more precisely should an infection be diagnosed.
Cohort patient care is initiated if a patient is admitted
and found to be colonized or infected with an organism of
broad antibiotic resistance or if this resistance pattern devel-
ops during broad-spectrum antibiotic therapy.
Cross-contamination is minimized by strict enforce-
ment of hand washing, gowning, and gloving policies. The
establishment of patient care teams to provide care for
only one specific patient or a limited number of patients
and restriction of the traffic of convalescing patients (often
colonized with resistant organisms) are imperative in
reducing cross-contamination and eradicating endemic
microorganisms.
The infection control committee monitors infections
occurring in the burn unit to identify changes in microbial
prevalence, the incidence of infection, and evidence of cross-
contamination. Strict criteria for the definition and identifi-
cation of infections that occur in burn patients are necessary
to avoid unnecessary and inappropriate antibiotic adminis-
tration. Antibiotics are used only for specific indications to
minimize the emergence of microbial resistance. Effective
infection control policies require continual reevaluation of
surveillance culture results and correlation with the sites and
treatment of infections.
2. Infectious Complications: Prevention,
Diagnosis, & Treatment
With the decrease in fatal burn wound sepsis and improved
survival of patients with massive burns, infections in other
sites have shown a relative increase as principal causes of

CHAPTER 35
742
death. Dense bacterial colonization of the burn wound and
the presence of immunosuppression associated with burn
injury increase the likelihood of development of infectious
complications.
Pneumonia
Pneumonia is the most frequent septic complication follow-
ing thermal injury. As the occurrence of invasive burn
wound infection has decreased, bronchopneumonia has
surpassed hematogenous pneumonia as the predominant
form. The increase in airborne pneumonia also may be
attributable to improved survival in patients with severe
inhalation injury. Atelectasis is often present prior to the
development of infection. The appearance of an ill-defined
irregular infiltrate on chest x-ray mandates Gram stain, cul-
ture, and sensitivity testing of endobronchial secretions.
Empirical antibiotic treatment is begun as determined by
microbiologic surveillance and Gram stain of the secretions.
Subsequent antibiotic therapy is adjusted on the basis of
sensitivity testing.
Compared with bronchopneumonia, hematogenous
pneumonia usually occurs later in the hospital course.
Remote septic foci such as invasive wound infection,
endocarditis, and suppurative thrombophlebitis are com-
mon causes. The radiographic hallmark is a solitary nodu-
lar pulmonary infiltrate, but progression to multiple
nodular infiltrates throughout the lungs may occur. All
possible sites of infection must be evaluated if a character-
istic nodular pulmonary infiltrate appears. The primary
infection must be identified and treated. The pneumonic
process is treated by systemic administration of antibi-
otics directed against the causative organism and ventila-
tory support as needed. Aggressive pulmonary toilet
to prevent atelectasis may help to decrease the occurrence
of pneumonia, although most routine measures have little
proved benefit.
Suppurative Thrombophlebitis
The loss of skin integrity, the presence of dense bacterial col-
onization of the burn wound, and the frequent need for
long-term venous access increase the likelihood that suppu-
rative thrombophlebitis will develop in burn patients.
Limiting the duration of cannulation of a vein to 3 days or
less in patients with thermal injury has reduced the inci-
dence of this complication from 4.3% to less than 1.4% in
recent years. Local signs of thrombophlebitis are present in
less than half of patients with this complication because of
the presence of the overlying burn wound and the systemic
immunosuppression accompanying burn injury. With the
increased use of central venous cannulation, these patients
are also at risk for development of central vein suppurative
thrombophlebitis.
The diagnosis of peripheral vein suppurative throm-
bophlebitis is made by operative exploration, excision, histologic
analysis, and culture of the suspected phlebitic vein.
Identification of bacteria within the vein necessitates excision
of the entire length of involved vein to a level of patent normal
vein and the administration of systemic antibiotics to which
the causative microorganism is sensitive. The diagnosis of cen-
tral venous thrombophlebitis is more difficult. Indium-
111–labeled leukocyte scanning, CT scanning, and contrast
venography may help to establish the diagnosis. This rare com-
plication is treated with systemic antibiotics directed against
the organism isolated by blood culture and anticoagulation
with heparin. The efficacy of thrombolytic therapy in the treat-
ment of central venous thrombosis is unclear. The failure of
antibiotics and anticoagulation to eradicate the infectious focus
mandates surgical exploration and vein excision.
The true incidence of intravascular catheter–related bac-
teremia in thermally injured patients is unknown. Vascular
access through a densely colonized wound in those with
extensive surface area burns limits the use and effectiveness
of standard catheter care policies employed for other criti-
cally ill patients. Presumably, as a result of contamination by
removal through colonized eschar and skin, catheter tip cul-
tures frequently are positive even in the absence of sepsis or
bacteremia. Exchanging catheters over guidewires, an
accepted practice in most ICUs, is discouraged because the
catheters and guidewires often transverse heavily contami-
nated open wounds or intact eschar. Consequently, central
venous and pulmonary artery catheters are removed and a
new catheter inserted at a different site every 3 days. This pol-
icy has resulted in a low incidence of bacteremia and sepsis
clinically attributable to catheter-related infections.
Endocarditis
Acute infective endocarditis is an infrequent but consistent
source of morbidity and mortality in burn patients (1.3%)
owing to the bacteremias associated with wound manipula-
tion, prolonged intravenous cannulation, and septic throm-
bophlebitis. Preventive measures include effective topical
antimicrobial therapy, timely excision and closure of the
burn wound, and early discontinuation or frequent replace-
ment of intravenous cannulas.
Staphylococcus aureus is the most common causative
organism, and the right side of the heart is affected most fre-
quently. Recurrent staphylococcal bacteremia in a burn
patient with sepsis and no other apparent identifiable source
of infection should suggest the diagnosis. Heart murmurs
are difficult to detect in hyperdynamic, tachycardiac
patients. Transesophageal echocardiography is the pre-
ferred examination to detect valvular lesions, but small veg-
etations may remain undetected. On occasion, cardiac
catheterization—to identify valvular vegetations or valvular
incompetence—may be required for definitive diagnosis if
echocardiographic findings are equivocal. Systemic maximal-
dose antibiotic therapy is directed against the causative
organism. Antibiotic therapy is continued for 6 weeks after
the last positive blood culture.

BURNS
743
Sinusitis
The true incidence of sinusitis in burn patients is unclear, but
patients requiring prolonged transnasal intubation of both
the airway and stomach are at increased risk. One study
reported an incidence of 36% in transnasally intubated ICU
burn patients. Sinusitis is most often clinically undetectable
and requires radiographic examination by plain films or CT
scanning to establish the diagnosis. These studies help to
direct sinus aspiration to differentiate between congestion
and infection. Treatment involves topical mucosal vasocon-
strictors to improve patency of the sinus ostia and removal of
transnasal tubes. Appropriate systemic antibiotic therapy
should be initiated. Surgical drainage is required in cases not
responsive to these procedures. Tracheostomy or gastros-
tomy may be necessary if prolonged ventilatory support and
enteral nutrition are required.
Other Complications
A. Ocular—Thermal injury of the ocular adnexa is common
in patients sustaining facial burns, but actual injury to the
cornea and globe is uncommon because of the ble-
pharospasm induced by heat, noxious gases, and smoke.
Exceptions occur in patients with altered sensoria at the
time of burning and incomplete protection of the globe.
Shortly after admission, fluorescein staining of the cornea
and examination with a Wood’s lamp should be performed
to detect loss of epithelial integrity. If epithelial defects are
noted, prophylactic topical antibiotic therapy, for example,
bacitracin zinc–neomycin sulfate–polymyxin B sulfate oph-
thalmic ointment, should be initiated. Ophthalmologic con-
sultation should be obtained and the defects examined daily
to document resolution or progression of the epithelial
defects, the major hazard of which is bacterial infection.
Minor corneal abrasions that become infected may progress
rapidly to corneal ulceration and globe perforation.
Infections caused by Pseudomonas species are particularly
prone to this complication.
Frequent ocular examination, adequate eye lubrication,
prophylactic and therapeutic use of topical antibiotics, and
timely performance of eyelid releases are paramount in the
prevention of ocular complications. With severe burns of the
eyelids, ectropion or loss of lid margin may occur. If the
cornea is no longer protected, operation is indicated in the
form of an eyelid release with split-thickness skin grafting.
Release of one or both lids may be required, and in severe
cases, repeated release of the same lid may be made necessary
by progressive skin graft contracture. A temporary tarsorrha-
phy is sometimes useful to protect the cornea from exposure,
but severe ectropion or loss of the lid margin limits the use-
fulness of this technique.
B. Gastrointestinal—Many GI complications have been
documented following thermal injury and include pancreati-
tis, acalculous cholecystitis, gastroduodenal stress ulceration,
and Ogilvie’s syndrome. Stress ulceration of the upper GI
tract has been controlled effectively by prophylactic antacid
or H
2
-receptor antagonist therapy. Hemorrhage or perfora-
tion requiring operative management occurred in only five
patients (0.1%) during a 14-year series. In a recent study, the
prophylactic administration of sucralfate has been found
equally effective in stress ulcer prevention. Gastric colonization
with gram-negative organisms occurred later among patients
receiving sucralfate than among those receiving antacids, but
this did not change the incidence or type of pneumonia
occurring following burn injury.
Superior mesenteric artery syndrome may occur in
patients who sustain profound weight loss during their hos-
pital course. This condition results in compression and
obstruction of the transverse duodenum by the superior
mesenteric artery from weight loss–induced changes in the
anatomic position of this vessel. Current nutritional prac-
tices have nearly eliminated this complication. If diagnosed,
initial management should be directed toward nutritional
repletion and nasogastric decompression. Nasoenteral feed-
ing tubes may be guided past the obstruction under fluoro-
scopic guidance and are preferred over parenteral alimentation.
Operation is rarely necessary.
The management of GI complications in thermally
injured patients is the same as in other critically ill patients.
If operation is required, retention sutures should be used in
closing any abdominal incision in burn patients owing to the
increased risk of postoperative wound infection and fascial
dehiscence.
Bowers BL, Purdue GF, Hunt JL: Paranasal sinusitis in burn
patients following nasotracheal intubation. Arch Surg
1991;126:1411–12. [PMID: 1747055]
Pruitt BA Jr: The diagnosis and treatment of infection in the burn
patient. Burns Incl Therm Inj 1984;11:79–91. [PMID: 6525539]
Pruitt BA Jr, McManus AT, Kim SH: Burns. In Gorbach SL, Bartlet
JG, Blacklow HR (eds), Infectious Diseases in Medicine and
Surgery. Philadelphia: Saunders, 1992.
Shirani KZ et al: Effects of environment on infection in burn
patients. Arch Surg 1986;121:31–36. [PMID: 3942497]
NUTRITION
Postburn Hypermetabolism
Extensive thermal injury may cause metabolic rates to rise
to levels one and one-half to two times normal, far exceed-
ing the hypermetabolism observed in other critically ill
patients. The hypermetabolic response is linearly related to
the extent of burn, and the actual physiologic response is
influenced by environmental temperature, the patient’s age,
physical activity, pain and anxiety, and the presence of
infection. The hypermetabolic response to burn injury,
common to other forms of critical illness and trauma, is
partially driven by the neurohumoral milieu produced by
CHAPTER 35
744
the hypothalamic-pituitary and autonomic nervous system
responses. Activation of the former results in increased release
of antidiuretic hormone, adrenocorticotropic hormone
(ACTH), and β-endorphins, whereas stimulation of the latter
results in the release of catecholamines, glucagon, and corti-
sol. Postburn hypermetabolism is manifested by increased
oxygen consumption, a hyperdynamic circulation, increased
core temperature, wasting of lean body mass, and increased
urinary nitrogen excretion. An increase in CO
2
production
follows that parallels oxygen consumption. Hypermetabolism
is temperature-sensitive in patients with burns involving over
50% of the BSA, and a 10% decrease in metabolic rate may be
achieved by maintaining ambient temperatures above 30°C.
Blood flow to the burn wound is markedly increased com-
pared with the blood flow to other organs and tissues. This
explains to some extent the relationship of extent of burn to
hypermetabolism.
Substrate Utilization
Glucose metabolism is altered following thermal injury.
Hepatic gluconeogenesis and total glucose flow increase.
However, owing to relative insulin insensitivity, glucose uptake
by insulin-dependent tissues is decreased.An exaggerated frac-
tion of nutrient flow is directed to the burn wound. Through
anaerobic, insulin-independent means, large quantities of glu-
cose are required to support the immune cellular functions of
necrotic tissue removal and microbial containment and
destruction. Cellular proliferation and wound healing are also
glucose-dependent. The predominance of anaerobic metabo-
lism in the burn wound results in increased lactate production
with subsequent hepatic conversion of lactate to glucose via
the Cori cycle.
Marked catabolism resulting in muscle protein breakdown
and loss of lean body mass is observed following thermal
injury. Catabolism of muscle protein provides amino acid glu-
coneogenic precursors (converted to glucose by liver and gut)
and supplies amino acid substrates for synthesis of acute-phase
proteins. Significant nitrogen loss occurs, with 80–90%
excreted as urea. The metabolism of glutamine, a preferred
substrate for gut metabolism and a precursor for renal ammo-
nia production, is also increased during the hypermetabolic
phase. Glutamine is converted by the gut into alanine, which
subsequently enters the gluconeogenic pathway.
The ability to oxidize fat as a source of nonprotein calo-
ries depends on the extent of injury and the degree of
hypermetabolism. In patients with relatively small burns,
carbohydrate and fat may be used interchangeably as effec-
tive nonprotein calorie sources. In patients with larger
burns, carbohydrate is more effective than fat in maintain-
ing body protein stores when each is used as a sole energy
source.
Estimation of Caloric Needs
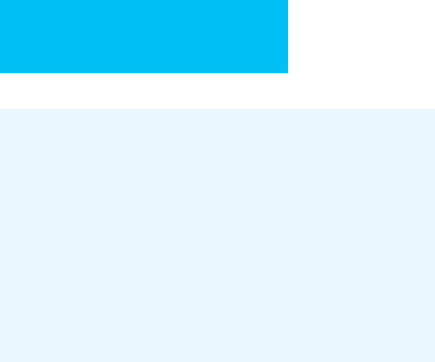
Many formulas exist for the estimation of caloric needs in
thermally injured patients. Some of the more common ones
based on body size, age, and sex are presented in Table 35–7.
The increase in calories required to support the metabolic
demand following burn injury is computed by either adding
predetermined stress or injury factors to standard formulas or
by incorporating the measured extent of burn into those for-
mulas specifically derived for burn patients. The use of for-
mulas to predict caloric requirements in individual patients
may result in overestimation or underestimation of caloric
needs. Since most formulas are derived by patient measure-
ments in the resting state, activity factors are customarily
applied and range from 10–50%. Serial measurements by
indirect calorimetry provide the most accurate determination
of energy requirements for patients with major burns; how-
ever, there is no current consensus regarding the most appro-
priate formula to use when requirements must be estimated.
The best method to calculate the protein requirements of
thermally injured patients remains controversial; however,
supplying 12–18 g of nitrogen per square meter of body sur-
face area or 1.5–2 g of protein per kilogram of body weight
Based on Harris-Benedict equation Basal metabolic rate × Activity factor × Injury factor
BMR male = 66.47 + 13.75 (kg BW) + 5.00 (cm ht) – 6.76 (age yr)
BMR female = 65.51 + 9.56 (kg BW) + 1.85 (cm ht) – 4.68 (age yr)
Activity factor = 1.2 bed rest, 1.3 out of bed
Injury factor = 2.1 for severe burn
Curreri (25 kcal × kg BW) + 40 kcal × % burn
Shriner’s (Galveston)
1800 kcal/m
2
BSA + 2200 kcal/m
2
of burn
USAISR
Basal in kcal/m
2
BSA per hour x Factor
Factor = 2.33764 – (1.33764
[–0.0286 × % burn]
)
USAISR = U.S. Army Institute of Surgical Research.
Table 35–7. Formulas for estimating energy requirements in thermally injured patients.

BURNS
745
has been recommended. Nonprotein kilocalorie-to-nitrogen
ratios of 100:1 to 150:1 are acceptable. Only enough fat to
prevent essential fatty acid deficiency is required. Some burn
patients may tolerate up to 9 mg/kg per minute of carbohy-
drate administration. However, carbohydrate delivery
exceeding 5 mg/kg per minute occasionally results in hepatic
fat deposition and excessive CO
2
production. This may cause
CO
2
retention in patients unable to compensate by increas-
ing minute ventilation.
Once the optimal delivery rate of carbohydrates is deter-
mined, balancing the remainder of the caloric requirements
with fat may be achieved safely if the fraction of calories
delivered as fat does not exceed one-third of the total.
Triglyceride clearance usually is increased following thermal
injury, but triglyceride levels should be followed weekly in
patients whose nutritional regimens contain a significant
percentage of calories supplied as fat. Hypertriglyceridemia,
usually from parenteral infusion of fat emulsions, may result
in coagulation abnormalities, hepatic dysfunction, and
altered pulmonary diffusion capacity. Triglyceride levels
above 200 mg/dL should prompt a decrease in lipid admin-
istration. The combination of medium- and long-chain
triglycerides provided in most enteral formulas is the pre-
ferred form of dietary fat supplementation and rarely results
in hypertriglyceridemia.
Delivery of Nutritional Support
Administration of nutrition by the enteral route is pre-
ferred to preserve enterohepatic delivery of substrates and
maintain mucosal function and integrity. Enteral intake
may be initiated safely when the ileus associated with ther-
mal injury has resolved. Patients with burns exceeding
30–40% of BSA may not be capable of meeting nutritional
goals by oral intake alone, and supplementation with any of
the commercially available enteral formulas with an appro-
priate calorie-to-nitrogen ratio may be used. Nasogastric
and nasojejunal feedings are commonly employed based on
institutional preference. Nasojejunal feedings have the
added advantage of providing continuous nutrition
throughout the perioperative and intraoperative periods
with a low risk of aspiration.
Parenteral nutrition is reserved for patients with pro-
longed ileus or conditions prohibiting effective GI motility
or absorption. Glucose intolerance is a more common com-
plication of parenteral nutrition and necessitates frequent
monitoring of blood glucose levels.
Monitoring Nutritional Therapy
Careful monitoring of nutritional therapy is imperative if the
high metabolic demand associated with thermal injury is to
be met and adequate nutrition maintained throughout the
hospital course. Useful indices include body weights, calo-
rie counts, nitrogen balance studies, and measurement of
respiratory quotients. In other critically ill patients, measure-
ment of serum albumin, transferrin, prealbumin, and
retinol-binding protein are commonly employed to monitor
the adequacy of nutritional support; however, these bio-
chemical markers have been shown to be poor predictors of
temporal changes in nitrogen balance in thermally injured
patients, and their use is not recommended. Nitrogen bal-
ance calculations based on urinary urea nitrogen (UUN)
excretion measurements should be modified to include
wound losses and other nonurea protein losses. Wound
losses, in grams per day, may be estimated as 0.1 × BSA in m
2
× percent BSA of unhealed burn wound. Total urinary nitro-
gen excretion exceeds UUN in thermally injured patients.
Increasing the measured 24-hour UUN by 25% will provide
an accurate estimate of total urinary nitrogen losses. The
daily nitrogen loss is increased by adding 2 g to account for
stool and normal integumentary losses. The formula derived
for daily nitrogen loss following thermal injury is as follows:
Total nitrogen loss (g/day) = 24-hour UUN
× 1.25 + [0.1 × BSA (m
2
)] + 2
If indirect calorimetric measurements are available, mon-
itoring the respiratory quotient (RQ) provides useful infor-
mation regarding substrate utilization. An RQ of greater than
1.0 indicates carbohydrate oxidation and overfeeding, which
may result in hepatic fat deposition. An RQ of less than 0.7
indicates fat oxidation and is consistent with the delivery of
insufficient carbohydrate calories. Routine serum chemistries,
liver function tests, and serum calcium, phosphorus, magne-
sium, and triglyceride determinations should be monitored
once or twice a week during nutritional therapy. Most meta-
bolic complications can be avoided by appropriate adjust-
ment of the elemental and nutrient composition of the
formula administered.
Complications
The mechanical, septic, and metabolic complications associ-
ated with enteral and parenteral nutrition in thermally
injured patients are the same as those common to all critically
ill patients. However, the quantity and duration of nutritional
supplementation required in thermally injured patients are
such that strict attention to the amount, composition, and
safe delivery of nutrition is required to avoid complications.
Burke JF et al: Glucose requirements following burn injury:
Parameters of optimal glucose infusion and possible hepatic
and respiratory abnormalities following excessive glucose
intake. Ann Surg 1979;190:274–85. [PMID: 485602]
Carlson DE, Jordan BS: Implementing nutritional therapy in the
thermally injured patient. Crit Care Nurs Clin North Am
1991;3:221–35. [PMID: 1905139]
Carlson DE et al: Resting energy expenditure in patients with ther-
mal injuries. Surg Gynecol Obstet 1992;174:270–76. [PMID:
1553604]
CHAPTER 35
746
Demling RH, Lalonde C: Nutritional support. In Blaisdell FW,
Trunkey DD (eds), Burn Trauma. New York: Thieme, 1989.
Saffle JR et al: Use of indirect calorimetry in the nutritional man-
agement of burned patients. J Trauma 1985;25:32–9. [PMID:
3965736]
Waxman K et al: Protein loss across burn wounds. J Trauma
1987;27:136–40. [PMID: 3820350]
Wilmore DW et al: Catecholamines: Mediator of the hypermeta-
bolic response to thermal injury. Ann Surg 1974;180:653–69.
[PMID: 4412350]
Wilmore DW: Pathophysiology of the hypermetabolic response to
burn injury. J Trauma 1990;30:S4–6. [PMID: 2254989 ]
Current Controversies & Unresolved Issues
Postburn Hemodynamics
Resuscitation of patients to provide supranormal levels of
oxygen delivery in states of severe illness or injury has been
popularized recently. At present, this goal is impractical in
the acute resuscitation of thermally injured patients. Even
though large volumes of fluid may be required to maintain
urine output, burned patients have decreased oxygen deliv-
ery and consumption during the initial phase of resuscita-
tion. Attempts to improve oxygen delivery would result in
massive fluid administration leading to excessive edema for-
mation and subsequent morbidity. The goal of fluid resusci-
tation in thermally injured patients is to maintain vital organ
function at the lowest physiologic cost. A more physiologic
restoration of intravascular volume and oxygen delivery
would seem beneficial.
Several approaches to reduction of edema formation and
restoration of circulatory integrity are under investigation.
Early intervention to block production of or to scavenge
superoxide and oxygen free radicals has been shown to
decrease edema formation. Administration of a soluble com-
plement receptor that blocks the classic and alternative com-
plement pathways has attenuated postburn edema formation
in animals. Fluid resuscitation with deferoxamine has been
shown to diminish the systemic effects of burn-induced oxi-
dant injury, and an inositol phosphate derivative, 1,2,6-
D
-
myoinositol triphosphate, has been shown to decrease burn
wound edema and resuscitation fluid requirements by an
unknown mechanism. Vitamin C, which has been shown in
various animal models to reduce burn wound edema and
resuscitation volume, was administered to burn patients in a
prospective, randomized, controlled manner. The patients
were resuscitated according to the Parkland formula. The 24-
hour total fluid infusion volumes were 5.5 mL/kg per percent
burn in the control group and 3.0 mL/kg per percent burn in
the vitamin C group. The vitamin C group had an initial
weight gain of 9.2% of pretreatment weight compared with a
17.8% weight increase in controls. The results of this initial
small study are encouraging. Urinary outputs were main-
tained between 0.5 and 1.0 mL/kg per hour during the first
24 hours postburn, and total 24-hour urine volumes were
not different between groups. Inhibition of lipid peroxida-
tion accomplished by antioxidant administration may be an
important adjunct in limiting fluid resuscitation volume and
edema formation following burn injury.
The inclusion of osmotically active macromolecules,
such as pentafraction, that have a decreased propensity for
transcapillary leakage during resuscitation also could improve
early circulatory integrity. Until mechanisms of edema forma-
tion are better understood and means of limiting transvascu-
lar fluid loss are developed, “supranormal” resuscitation is
neither appropriate nor feasible for burn patients.
Inhalation Injury
The mechanism by which inhalation of smoke and products of
incomplete combustion injure the tracheobronchial mucosa,
distal airways, and lung parenchyma is not completely under-
stood. In part, injury is governed by particle size, which deter-
mines the anatomic region where injury will occur. Toxicities
of noxious gases produced by combustion of synthetic and
natural materials also contribute to the tissue injury of
smoke inhalation but are at present impossible to quantify in
patients following exposure. Most animal models used to
study the effects of smoke inhalation fail to reproduce the
clinical and histologic changes associated with inhalation
injury in humans. Problems with smoke composition, car-
bon monoxide poisoning, and smoke delivery systems are
common. In a recent study of smoke inhalation injury in non-
human primates, high-frequency percussive ventilation was
found to be superior to conventional volume ventilation and
high-frequency oscillatory ventilation in decreasing baro-
trauma and the histopathologic severity of injury.
Pharmacologic intervention to modulate the response to
smoke inhalation may prove beneficial in decreasing pul-
monary vascular changes and improving lung aeration.
Recent studies in sheep have shown improved alveolar venti-
lation and diminished inflammatory response to smoke
inhalation following postexposure treatment with pentoxi-
fylline. The use of inhaled nitric oxide—which does not alter
the normal inflammatory response—to ameliorate pul-
monary artery hypertension following smoke inhalation is
also being studied. Other treatments, including complement
depletion and antioxidant therapy, are being investigated and
may prove beneficial. Any attempt to modulate the host
response to inhalation injury must proceed with caution to
avoid impairing the normal mechanisms of cellular repair
and immunologic defense.
A nebulized cocktail of heparin and a mucolytic agent,
N-acetylcystine, has been shown to reduce pulmonary failure
and ameliorate airway cast formation in both an animal
model and a case-controlled human study in 47 children. A
blinded, randomized study or studies in adults have not
been reported; however, decreases in reintubation rates
and mortality rates for patients treated with this regimen
were noted when compared with historical controls.
Further information is also needed in this arena; however,
