Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

BURNS
727
production by peripheral blood lymphocytes. Septic compli-
cations result in a further decrement in IL-2 production.
Serum IgG levels are decreased following burn injury and
gradually return to normal over 2–4 weeks as the patient
recovers. Restoration of IgG levels to normal by exogenous
administration has not been shown to affect morbidity or
mortality. Many investigators, using a number of experimen-
tal approaches, have demonstrated immunosuppressive fac-
tors present in the serum of thermally injured patients.
Similar immunosuppressive properties have been detected in
burn blister fluid. Immunosuppressive polypeptides have
been the most commonly invoked agents; however, other fac-
tors, including complement degradation products,
immunoglobulin fragments, prostaglandins, and endocrine
secretions, occur in the serum following thermal injury.
Alterations in granulocyte chemotaxis, degranulation,
adherence, oxygen free-radical production, and complement
receptor expression have been observed following thermal
injury. Granulocytes from burned patients exhibit an
increase in cytosolic oxidase activity, suggesting in vivo acti-
vation. They also exhibit greater than normal oxidase activ-
ity after in vitro stimulation. This increase suggests that
neutrophils from burned patients have an increased oxida-
tive burst potential that, if activated, could cause increased
tissue and organ injury. A marked and sustained increase in
neutrophil expression of the complement opsonin receptors
CRT and CR3 has been described following burn injury. The
increase in receptor expression correlated with decreased
chemotaxis in response to zymosan-activated serum, sug-
gesting that C5A was responsible for inducing systemic neu-
trophil activation. Recent investigations have demonstrated
significant elevation of F-actin content and decreased ability
to polymerize and depolymerize F-actin in the granulocytes
of burn patients when compared with controls. These alter-
ations may be partly responsible for the observed changes in
chemotaxis and migration following thermal injury.
Almost every aspect of immunoregulation is affected fol-
lowing burn injury. At present, no effective immunomodula-
tory treatment has been identified; however, the development
of new immunomodulatory drugs and recombinant lym-
phokines and their antagonists may prove beneficial in cor-
recting immune dysfunction following burn injury.
Aulick LH et al: Influence of the burn wound on peripheral circu-
lation in thermally injured patients. Am J Physiol
1977;233:H520. [PMID: 910969]
Bowen BD et al: Microvascular exchange during burn injury: III.
Implications of the model. Circ Shock 1989;28:221–33. [PMID:
2766478]
Burleson DG et al: Flow cytometric measurement of rat lympho-
cyte subpopulations after burn injury and burn injury with
infection. Arch Surg 1987;122:216–20. [PMID: 3813870]
Cioffi WG et al: Dissociation of blood volume and flow in regula-
tion of salt and water balance in burn patients. Ann Surg
1991;214:213–8. [PMID: 1656902]
Cioffi WG et al: Granulocyte oxidative activity after thermal injury.
Surgery 1992;112:860–5.
Demling RH et al: Early lung dysfunction after major burns: Role
of edema and vasoactive mediators. J Trauma 1985;25:959–66.
[PMID: 2413227]
Demling RH, Kramer G, Harms B: Role of thermal injury-induced
hypoproteinemia on fluid flux and protein permeability in
burned and non-burned tissue. Surgery 1984;95:136–44.
Ferrara JJ et al: The suppressive effect of subeschar tissue fluid
upon in vitro cell-mediated immunologic function. J Burn Care
Rehabil 1988;9:584–8. [PMID: 3220864]
Fleming RY et al: The effect of erythropoietin in normal healthy
volunteers and pediatric patients with burn injuries. Surgery
1992;112:424–31.
Fukuzuka K et al: Glucocorticoid-induced, caspase-dependent
organ apoptosis early after burn injury. Am J Physiol Regul
Integr Comp Physiol 2000;278:R1005–18. [PMID: 10749790]
Gadd MA et al: Defective T-cell surface antigen expression after
mitogen stimulation: An index of lymphocyte dysfunction after
controlled murine injury. Ann Surg 1989;209:112–18. [PMID:
2783362]
Harms BA et al: Microvascular fluid and protein flux in pulmonary
and systemic circulations after thermal injury. Microvasc Res
1982;23:77–86. [PMID: 7099009]
Jones WG II et al: Differential pathophysiology of bacterial translo-
cation after thermal injury and sepsis. Ann Surg 1991;214:
24–30. [PMID: 2064468]
LeVoyer T et al: Alterations in intestinal permeability after thermal
injury. Arch Surg 1992;127:26–9. [PMID: 1734847]
Lund T, Reed RK: Microvascular fluid exchange following thermal
skin injury in the rat: Changes in extravascular colloid osmotic
pressure, albumin mass, and water content. Circ Shock
1986;20:91–104. [PMID: 3779907]
Ozkan AN, Hoyt DB, Ninnemann JL: Generation and activity of
suppressor peptides following traumatic injury. J Burn Care
Rehabil 1987;8:527–30. [PMID: 3325512]
Pruitt BA Jr, Goodwin CW, Mason AD Jr: Epidemiological, demo-
graphic, and outcome characteristics of burn injury. In
Herndon DN (ed), Total Burn Care, 2nd ed. Philadelphia:
Saunders, 2002.
Pruitt BA Jr, Mason AD Jr, Moncrief JA: Hemodynamic changes in
the early postburn patient: The influence of fluid administra-
tion and of a vasodilator (hydralazine). J Trauma 1971;11:
36–46. [PMID: 5099912]
Pruitt BA Jr: The universal trauma model. Bull Am Coll Surg
1985;70:2.
Solomkin JS: Neutrophil disorders in burn injury: Complement,
cytokines, and organ injury. J Trauma 1990;30:S80–85. [PMID:
2254997]
Till GO et al: Oxygen radical dependent lung damage following
thermal injury of rat skin. J Trauma 1983;23:269–77. [PMID:
6842628]
INITIAL CARE OF THE BURN PATIENT
Prehospital Treatment
The primary concern at the accident scene is to stop the
burning process. Burning and smoldering clothing should be
extinguished. Patients with electrical injury should be sepa-
rated from points of electric contact, taking all necessary care
CHAPTER 35
728
to avoid injuring oneself. If the burn was caused by a chemi-
cal agent, all contaminated clothing should be removed and
copious water lavage initiated.
As with all trauma patients, the primary concern during
initial assessment is maintenance of cardiopulmonary func-
tion. Airway patency and adequacy of ventilation must be
maintained and supplemental oxygen administered as neces-
sary. In the absence of associated mechanical trauma or need
for cardiopulmonary resuscitation, placement of an intra-
venous cannula is not necessary if transport to a treatment
facility can be accomplished in less than 45 minutes. The
application of ice or cold water soaks will relieve pain in areas
of second-degree burn. If the cold therapy is initiated within
10 minutes of burning, tissue heat content is also reduced,
and the depth of thermal injury may be lessened. If cold ther-
apy is used, care must be taken to avoid causing hypother-
mia. Cold soaks or ice should only be used on patients with
burns of less than 10% of the body surface and only for the
time required to produce analgesia. After the ice or cold soak
is removed, the patient should be covered with a clean sheet
and blanket to conserve body heat and minimize contamina-
tion of the burn wounds during transport to the hospital.
Emergency Management
On arrival at the hospital, the patency of the airway and ade-
quacy of breathing should be reassessed and endotracheal
intubation performed if necessary. Intravenous fluid resusci-
tation is initiated by infusing a physiologic salt solution, for
example, lactated Ringer’s solution, through a large-bore
intravenous cannula. The order of preference for the site of
intravenous cannulation is a peripheral vein underlying
unburned skin, a peripheral vein underlying burned skin,
and lastly, a central vein.
A history should be obtained, paying special attention to
the circumstances of the injury, the presence of preexisting
disease, allergies and medications, and the use of illicit drugs
or alcohol prior to injury. A complete physical examination
should be performed and associated injuries identified.
Baseline laboratory data should include an arterial blood gas
and pH analysis, serum electrolytes, urea nitrogen, creati-
nine, and glucose, and a complete blood count. If available,
continuous transcutaneous pulse oximetry determination of
oxygen saturation should be initiated in patients with sus-
pected inhalation injury or extensive burns.
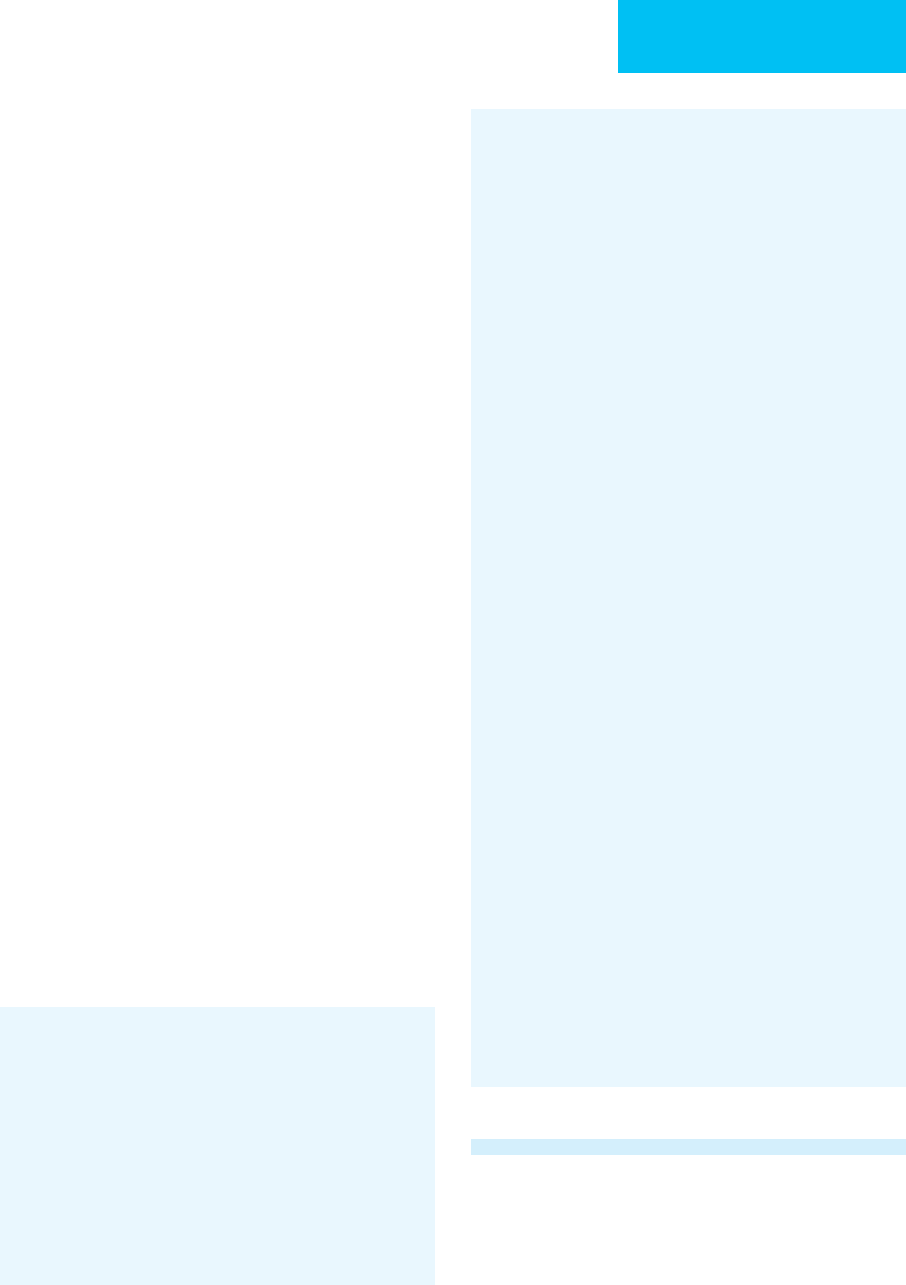
Since all currently used resuscitation formulas are based on
body weight and the percentage of total body surface area
burned (TBSB), the patient should be weighed and the depth
and extent of burn estimated. The extent of body surface area
burned can be estimated easily using the “rule of nines,” which
recognizes that specific anatomic regions represent 9% or 18%
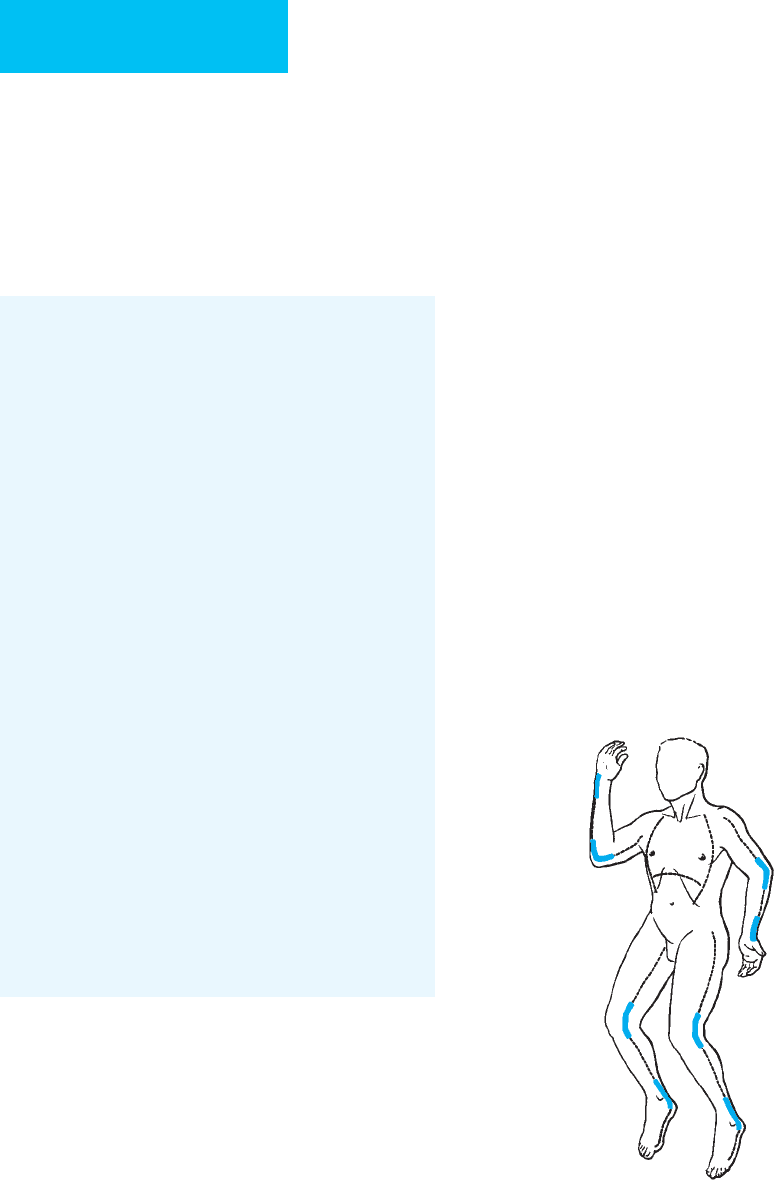
of the total body surface area (Figure 35–1). Since the area of
one surface of the patient’s hand (palm and digits) represents
1% of that person’s total body surface, one can use that rela-
tionship in estimating the extent of irregularly distributed
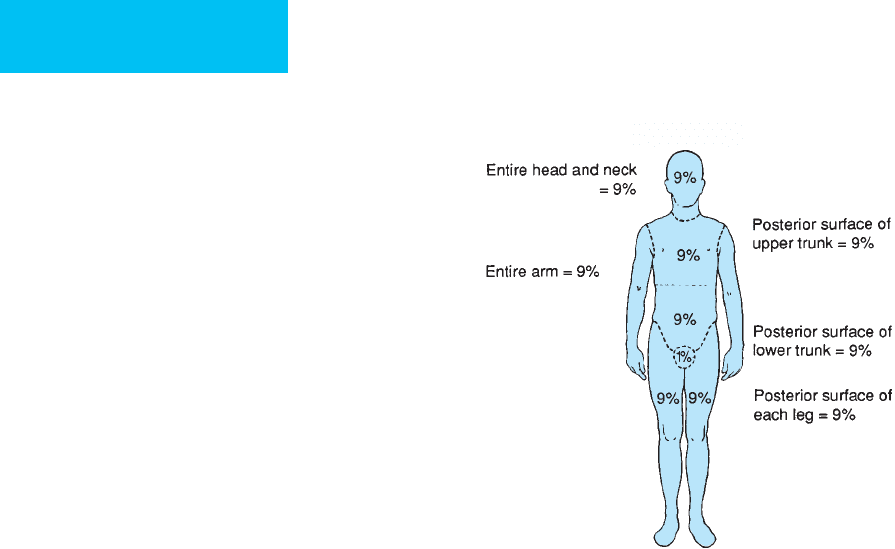
burns. Infants and children have a different body surface area
distribution, with relatively larger heads and smaller lower
extremities. When estimating the body surface burn area for
children under age 10, the Lund and Browder burn diagram
(Figure 35–2) or other similar diagram should be used to deter-
mine the body surface area burned with greater precision.
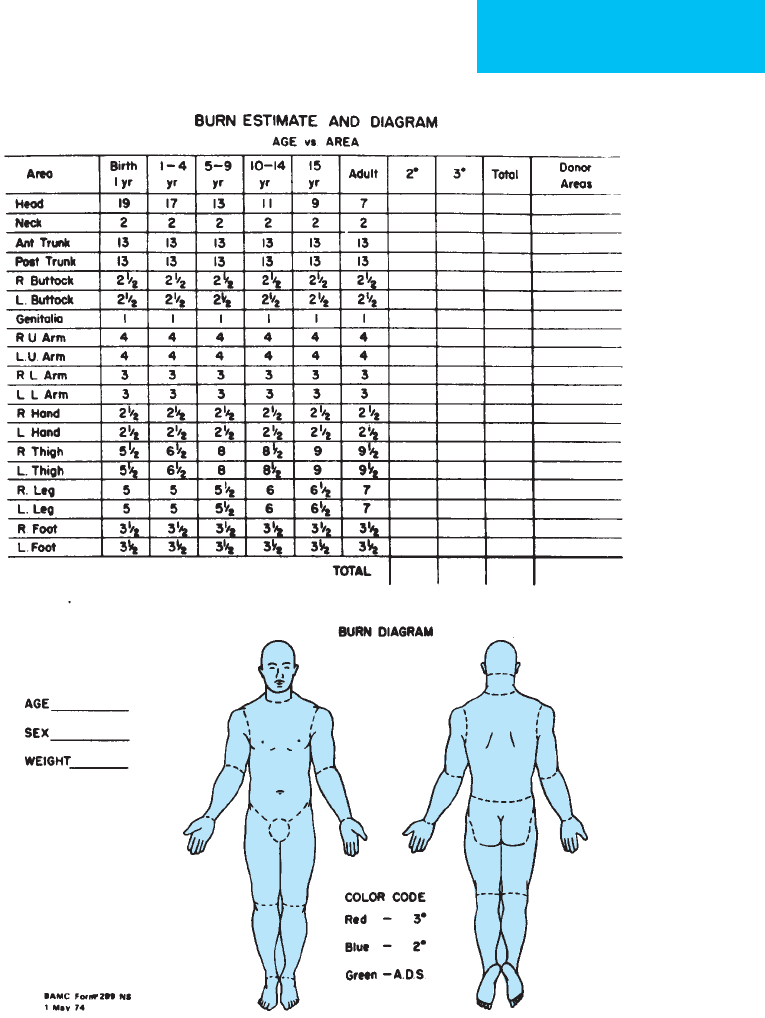
The depth of burn is classified as partial- or full-thickness
with respect to the extent of dermal destruction by coagula-
tion necrosis (Figure 35–3). First- and second-degree burns
are considered partial-thickness injuries and third-degree
burns full-thickness injuries. Superficial partial-thickness
burns heal spontaneously by epithelial migration from pre-
served dermal appendages. Full-thickness injuries have com-
plete destruction of all epithelial elements and require skin
grafting for wound closure. Deep partial-thickness burns
may heal over a long period of time, but grafting is frequently
performed to decrease time to wound closure, reduce scar
formation, improve functional outcome, and shorten the
hospital stay. The clinical criteria in Table 35–2 permit initial
differentiation among the different depths of burn injury.
Only the total percentage of skin surface area involved in
second- and third-degree burns is calculated or estimated for
resuscitation purposes. First-degree burns do not cause sig-
nificant edema formation or metabolic alteration and are not
considered in the calculation of burn size for estimation of
resuscitation requirements. Differentiation between second-
and third-degree burns is more important in the later post-
burn course because it has implications for the duration of
hypermetabolism, the need for autograft closure of the burn
wound, and the anticipated functional result.
ADULT
“Rule of Nines”
Figure 35–1. Rule of nines showing distribution of
body surface area (BSA) by anatomic parts in the adult.
BURNS
729
The presence of associated mechanical trauma may affect
the resuscitation requirements of the thermally injured
patient. Soft tissue trauma and bleeding from any injury will
increase the fluid required to establish adequate urine out-
put. The presence of thermal injury should not delay or alter
the evaluation and subsequent treatment, including opera-
tive intervention, of mechanical trauma. An indwelling
urethral catheter should be inserted in all patients requiring
intravenous fluid therapy, and the urinary output should be
measured and recorded hourly. Vital signs and the patient’s
general condition should be monitored and recorded fre-
quently on a flowsheet. The rectal temperature should be
measured hourly, providing a guide for maintenance of core
temperature. In patients with high-voltage electrical injury,
Figure 35–2. The use of a burn diagram permits a more exact estimation of the extent of burn. Note that the sur-
face areas of the head and lower extremities change significantly with age.
CHAPTER 35
730
electrocardiographic monitoring should be initiated in the
emergency department.
The tetanus immunization status of the patient should be
determined in the emergency department. The burn patient
who has been immunized against tetanus previously should
be given a booster dose of tetanus toxoid if the last dose was
administered more than 5 years previously. Patients with no
history of active immunization should receive tetanus
immune globulin in addition to an initial dose of tetanus
toxoid. Active immunization is completed subsequently
according to the routine dosage schedule.
PRINCIPLES OF BURN TREATMENT
Fluid Resuscitation
Fluid resuscitation should be started as soon as possible fol-
lowing thermal injury. Generally, burns involving more than
25% of the body surface area require intravenous fluid resus-
citation because ileus precludes oral resuscitation. Patients
with smaller burns in whom ileus does not develop should
have liberal access to electrolyte-containing fluids such as
fruit juices or milk, but excessive intake of electrolyte-free
water should be avoided to prevent hyponatremia. Many for-
mulas have been proposed for calculation of intravenous
fluid resuscitation of thermally injured patients (Table 35–3).
The central theme is that the volume of fluid required
depends on the patient’s weight and the extent of burn. Most
often it is recommended that half the calculated requirement
be infused over the first 8 hours following injury, that is, at
the time of maximal vascular permeability; the remainder of
the first 24-hour resuscitation volume is delivered over
the next 16 hours. Certain subgroups of patients require a
significantly greater resuscitation volume than that estimated
by the formulas. A delay in starting fluid resuscitation,
inhalation injury, and ethanol intoxication frequently are
associated with greater than predicted fluid requirements.
Patients with high-voltage electrical injuries frequently
require more resuscitation fluid than that predicted based on
the extent of cutaneous injury. One must recognize that any
resuscitation formula serves only to guide the initiation of
fluid therapy. The actual amount of resuscitation fluid is tai-
lored to each patient’s physiologic responses, with frequent
reassessment and adjustment of infusion rates as needed to
preserve vital organ perfusion.
The various burn formulas in Table 35–3 differ consider-
ably with respect to the volume and composition of the
resuscitation fluids; however, each formula has been found to
be clinically effective. The general use of burn formulas has
decreased the frequency of burn-induced hypovolemic shock
and organ dysfunction, which were secondary to inadequate
Figure 35–3. Diagram of the skin and subcutaneous
tissues demonstrating the depth of burn and relationship
to the location of the cutaneous adnexa. First- and sec-
ond-degree burns are considered partial-thickness.
Preservation of the hair follicles and sweat glands per-
mits spontaneous healing by epithelial cell migration.
Full-thickness (third-degree) burns will not reepithelialize
and require skin grafting for closure.
First-Degree Second-Degree Third-Degree
Cause Exposure to sunlight, very brief expo-
sure to hot liquid, flash, flame, or
chemical agent.
Limited exposure to hot liquid, flash,
flame, or chemical agent.
Prolonged exposure to flame, hot object, or chem-
ical agent. Contact with high-voltage electricity.
Color Red Pink or mottled red Pearly white, charred, translucent, or parchment-
like. Thrombosed vessels may be visible.
Surface Dry or very small blisters Bullae or moist, weeping surface Dry and inelastic
Sensation Painful Painful Insensate surface
Table 35–2. Characteristics of first-, second-, and third-degree burns.
BURNS
731
resuscitation. Failure to reevaluate the patient’s response to
resuscitation frequently on a scheduled basis may lead to
over- or underresuscitation. This is frequently observed
when the volume of fluid administered is based solely on the
initial estimate. With overzealous administration of intra-
venous fluids, pulmonary, cerebral, and excessive burn
wound edema may result. These complications are most evi-
dent from the third to sixth postburn days, when vascular
permeability has returned to “normal,” vascular resistance
has decreased, and burn wound edema is being resorbed.
Laboratory and clinical studies evaluating transcapillary
fluid movement and the physiologic response to resuscita-
tion have failed to demonstrate a benefit from the use of col-
loid-containing solutions during the first 24 hours of
resuscitation. Extravascular lung water has been shown to
remain essentially unchanged during the first postburn week
in patients who received only crystalloid-containing fluids in
the first 24 hours following injury. However, extravascular
lung water increased progressively in patients who received
colloid-containing fluids as part of the initial resuscitation.
During the latter half of the first week following injury, cap-
illary permeability normalizes and fluid requirements
decrease. As this occurs, the use of colloid-containing fluids
repletes the intravascular volume deficit more efficiently and
with a lesser volume than with crystalloid fluids alone.
The use of hypertonic saline has been proposed as a
means of reducing resuscitation fluid volume requirements.
Although the initial volume of fluid administered when
using hypertonic fluid is clearly less, the proposed benefits of
a decreased need for escharotomy, decreased incidence and
duration of ileus, and decreased fractional sodium retention
have not been found in all studies. Potential problems with
hypertonic saline resuscitation include hypernatremia,
which, if of sufficient magnitude to require infusion of hypo-
tonic fluid, negates the potential benefits of this resuscitation
strategy. The cellular dehydration induced by hypertonic
saline infusion of sufficient magnitude (15%) may cause cel-
lular and organ dysfunction necessitating correction with
hypotonic fluid administration. Subsequent evaporative
water loss from the burn wound may worsen the expected
hypernatremia from hypertonic saline resuscitation, requir-
ing additional hypotonic fluid infusion. Occasionally, some
patients with markedly reduced cardiac reserve may benefit
from resuscitation protocols employing hypertonic saline;
however, isotonic fluid resuscitation formulas provide ade-
quate resuscitation in most patients. Caution should be
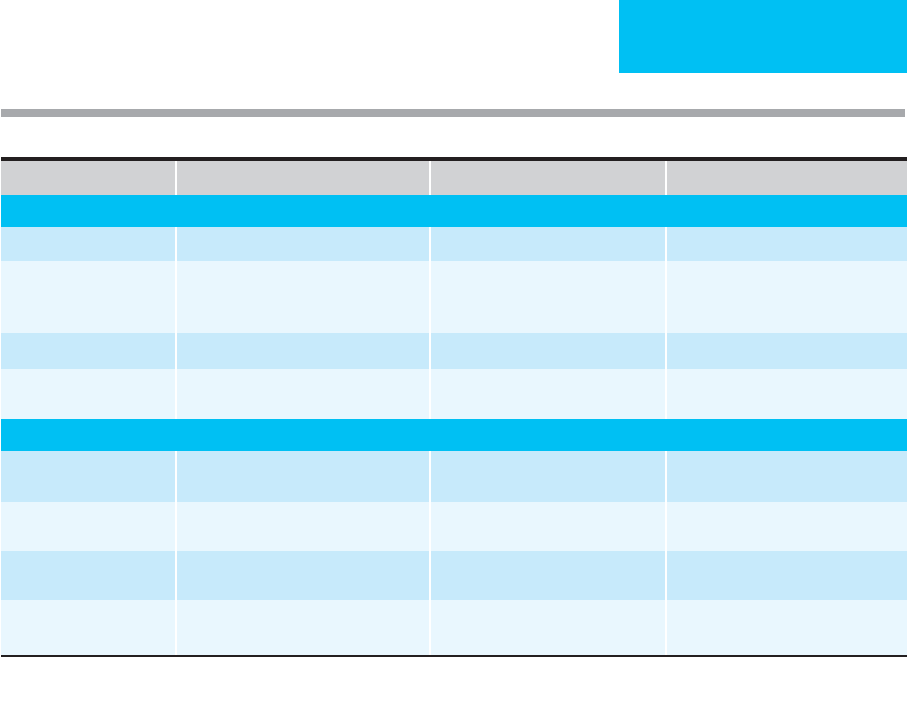
Formula Electrolyte-Containing Solution Colloid-Containing Solution 5% Glucose in Water
First 24 Hours Postburn
Parkland Lactated Ringer’s, 4 mL/kg per % burn.
Hypertonic sodium
resuscitation
Volume of fluid containing 250 meq of
sodium/L to maintain hourly urinary
output of 30 mL.
Modified Brooke Lactated Ringer’s, 2 mL/kg per % burn.
Consensus
∗
Lactated Ringer’s, 2–4 mL/kg per %
burn.
Second 24 Hours Postburn
Parkland 20–60% of calculated plasma volume. As necessary to maintain urinary
output.
Hypertonic sodium
resuscitation
33% isotonic salt solution up to
3500 mL limit.
Modified Brooke
0.3–0.5 mL/kg per % burn
†
As necessary to maintain urinary
output.
Consensus
∗
0.3–0.5 mL/kg per % burn
†
As necessary to maintain urinary
output.
∗
American Burn Association: Advanced Burn Life Support Course.
†
Administered as a plasma equivalent (eg, 5% albumin in 0.9% sodium chloride solution.)
Table 35–3. Commonly used resuscitation formulas.

CHAPTER 35
732
observed when implementing hypertonic saline resuscitation
because increases in early acute renal failure and mortality
have been reported.
Adjuvant administration of high-dose ascorbic acid dur-
ing the first 24 hours after thermal injury has been shown to
reduce the resuscitation fluid volume required significantly
during this period in burn patients. Wound edema and body
weight gain also were decreased. Infusion of ascorbic acid has
been shown to attenuate postburn lipid peroxidation as a
known antioxidant. It is uncertain as to the exact mechanism
by which vitamin C seems to confer these benefits during
burn resuscitation. Additional study of this treatment should
be performed.
The modified Brooke formula (see Table 35–3), which is
recommended by the authors, employs a physiologic salt
solution during the first 24 hours without the addition of
colloid or electrolyte-free crystalloid solutions. Lactated
Ringer’s is the preferred solution because of its more nearly
physiologic concentration of chloride ions than normal
saline. Fluid needs are estimated as 3 mL (children) or 2 mL
(adults) per kilogram body weight per percent TBSA of lac-
tated Ringer’s solution. Children have a greater body surface
area per unit of body mass and require more resuscitation
fluid than adults. One-half the calculated estimate is admin-
istered in the first 8 hours and the second half over the sub-
sequent 16 hours postburn. If initiation of fluid resuscitation
is delayed, that amount of fluid calculated to be administered
in the first 8 hours should be infused at a rate such that half
the estimated 24-hour fluid requirement will be delivered by
8 hours postburn.
In the second 24 hours following burn injury, 5% albumin
solution in physiologic saline is administered in an amount
proportional to body weight and the extent of burn to aid in
correction of the plasma volume deficit (Table 35–4). During
the second 24 hours, lactated Ringer’s infusion is stopped,
and 5% dextrose and water is delivered to maintain adequate
urine output.
Monitoring Resuscitation
The objective of fluid resuscitation following thermal injury
is maintenance of organ perfusion and function. The ade-
quacy of resuscitation may be assessed by the hemodynamic
response, the status of mental function, indicating the ade-
quacy of cerebral perfusion, and the volume of urine output,
indicating effective renal perfusion.
Patient disorientation, anxiety, and restlessness may be
early signs of hypovolemia or hypoxemia that require imme-
diate assessment and correction. Sphygmomanometric mon-
itoring of blood pressure in patients with extensive burns can
be misleading. In a burned limb—or in an unburned
extremity in which massive edema develops—Korotkoff
sounds may be progressively attenuated, falsely implying
hypoperfusion. Blood pressure measurements, even when
obtained by use of an indwelling peripheral arterial cannula,
may not reflect true hydration status because markedly ele-
vated circulating levels of catecholamines and other vasoac-
tive materials may cause severe vasospasm. A resting
tachycardia between 100 and 120 beats/min is common fol-
lowing thermal injury. Rates above this level may reflect
inadequate pain control or inadequate fluid resuscitation. A
more objective indication of the adequacy of resuscitation is
the rate of production of urine, which reflects the adequacy
of renal perfusion. In the absence of osmotically driven
diuresis, a urinary output of 30–50 mL/h indicates adequate
resuscitation in most adult patients, and 1 mL/kg per hour
indicates adequate resuscitation in patients weighing less
than 30 kg.
Routine use of flow-directed pulmonary artery catheters
during burn resuscitation is unnecessary. Even with extensive
injury, healthy young adults usually respond to fluid resusci-
tation in a predictable manner. The previously discussed
indicators of adequacy of resuscitation may be used to guide
fluid infusion rates. Fluid infusion rates should be adjusted if
the hourly urine output is below or above the desired urinary
output by more than 33% for 2 consecutive hours. Only
patients who do not respond to fluid resuscitation as
expected—or whose fluid administration in the first 6 hours
exceeds that volume which will result in a 6 mL/kg per
percent burn resuscitation—should be monitored with a
flow-directed pulmonary artery catheter. If the pulmonary
artery occlusion pressure or measurements of right ventricu-
lar end-diastolic volume indicate an adequate intravascular
volume, this type of patient may benefit from the use of a
cardiac inotropic agent to augment cardiac output.
Occasionally, patients manifest a diminished cardiac out-
put with a markedly elevated systemic vascular resistance
when pulmonary artery wedge pressures indicate adequate
fluid resuscitation. In these patients, administration of a
short-acting afterload-reducing agent may result in a
decrease in the systemic vascular resistance and an increase
in the hourly urinary output. Administration of small doses
of hydralazine (0.5 mg/kg) has been shown to be effective
when used in this manner. In animal models of burn injury,
sodium nitroprusside and verapamil administered during
the resuscitation period reduced peripheral vascular resist-
ance and increased cardiac output. This therapy should be
administered cautiously and only to patients who have
received adequate fluid loading. If used inappropriately, the
resulting vasodilation will exacerbate the hypovolemia and
further depress cardiac output and organ perfusion.
Table 35–4. Estimation of colloid replacement during
second 24 hours postburn.
30–50% burn: 0.3 mL/kg body weight per % burn
50–70% burn: 0.4 mL/kg body weight per % burn
>70% burn: 0.5 mL/kg body weight per % burn

BURNS
733
Excessive fluid administration during resuscitation may
result in pulmonary edema, increased need for escharotomy,
and even the need for fasciotomy in unburned limbs.
Recently, the occurrence of intraabdominal compartment
syndrome has been recognized as a complication of excessive
fluid resuscitation. An increase in intraabdominal pressure to
greater than 25 mm Hg may impair venous return and
decrease cardiac output. This is often associated with elevated
peak and mean airway pressures and high pulmonary artery
wedge and central venous pressures. It is prudent to monitor
intraabdominal pressure routinely using an indwelling blad-
der catheter in patients with extensive burns who receive fluid
volumes of more than 25% of preburn total body weight dur-
ing the resuscitation phase. More important, strict attention
to the rate of fluid administration and reduction of excessive
resuscitation fluid volumes should be emphasized.
Continuous monitoring of arterial blood pressure with
indwelling arterial cannulas is not required in uncomplicated
burn resuscitations. In patients with inhalation injury or
those who do not respond as expected to fluid resuscitation,
frequent monitoring of arterial blood gases should be per-
formed, and a distal extremity artery should be cannulated to
decrease the risk of complications associated with repetitive
arterial puncture. Femoral arterial cannulation also has a low
complication rate and may be employed if distal arterial can-
nulation is not possible.
Other measures of perfusion such as serum lactate, base
deficit, and intramucosal pH, commonly followed during
resuscitation of various shock states, may be difficult to
interpret when used to monitor burn resuscitation. An eleva-
tion of plasma lactate concentration is observed frequently in
severely burned patients and may in part reflect increased
circulating levels of catecholamines. Glucose administration
increases the rate of glucose oxidation with a subsequent
increase in plasma lactate and pyruvate concentrations fol-
lowing thermal injury. Thus caution must be used in inter-
preting elevated serum lactate levels as related to the
adequacy of burn resuscitation and systemic oxygen delivery.
Similarly, measurement of the arterial base deficit during
burn resuscitation often will yield values as low as –6 even
though other measures of resuscitation, such as urinary out-
put, are at normal levels. This may reflect a relative deficit in
systemic oxygen delivery; however, the excessive fluid admin-
istration required to reverse the base deficit will result in
complications of overresuscitation. Measurement of gastric
intramucosal P
CO
2
changes using a gastric tonometer may be
used to detect intestinal ischemia during burn resuscitation.
Patients with significant gastric acidosis have a mortality rate
twice that of patients without acidosis. The deaths in this
group were predominantly from multiple-organ dysfunction
occurring several weeks after injury. This suggests that intes-
tinal ischemia still may occur in some patients despite appar-
ently adequate fluid resuscitation after thermal injury,
inflicting persistent deleterious effects on distant organ func-
tion. Conversely, Venkatesh and colleagues have reported
depression of gastric mucosal pH in the presence of “nor-
mal” indices of systemic circulation and attributed this dis-
parity to selective GI vasoconstriction and the development
of tissue edema.
At the beginning of the second postburn day, when col-
loid replacement is initiated and infusion of lactated Ringer’s
solution is discontinued, the volume of 5% dextrose in water
infused per hour should be equal to 25–50% of the preced-
ing hour’s volume of lactated Ringer’s solution. If the urinary
output remains greater than 30 mL/h, that infusion rate
should be maintained for the next 3 hours, at which time the
rate of infusion of 5% dextrose in water should be further
reduced in a similar manner.
Pulmonary function must be reassessed continually
throughout the resuscitative phase. Tachypnea may indicate
metabolic acidosis from underresuscitation, hypoxemia, or
restriction of chest wall motion owing to circumferential
burns or massive edema. Evaluation must include ausculta-
tion, chest x-rays, and arterial blood gas analyses if a signifi-
cant tachypnea occurs. Thermally injured patients in the ICU
should be monitored with a pulse oximeter. In most patients,
hemoglobin saturation by arterial blood gas analysis matches
that obtained by pulse oximetry; however, patients with
severely burned digits may be difficult to monitor using this
method. In addition, a decrease in intensity of the pulsed sig-
nal detected in an extremity monitored by pulse oximetry
may reflect inadequate distal perfusion from underresuscita-
tion, constricting circumferential burn wounds, or arterial
spasm owing to high levels of circulating catecholamines.
Low oxygen saturation, as measured by pulse oximetry, also
may indicate circulating levels of carboxyhemoglobin or
methemoglobin as a consequence of the inhalation of carbon
monoxide or cyanide, respectively.
In thermally injured patients requiring endotracheal
intubation and mechanical ventilation, end-tidal CO
2
moni-
toring should be used to detect early changes in ventilation
owing to inhalation injury or restriction of chest wall
motion. This method of monitoring is particularly useful in
pressure-controlled modes of mechanical ventilation. Chest
radiographs should be obtained at least daily during resusci-
tation and the period of edema absorption. Subsequent x-
rays are ordered as clinically indicated.
Serum chemistry profiles, complete blood count, arterial
blood gases, and other baseline blood studies are obtained on
admission, with further tests depending on the clinical situa-
tion. The patient’s weight should be measured on admission
and followed daily as an indicator of fluid balance.
Evaporative water loss from the wound typically peaks on
the third postburn day and persists until the burn wound is
healed or grafted. Insensible water losses may be estimated
according to the following formula:
Insensible water loss (mL/h) = (25% + % BSA
burned) × total BSA (m
2
)
CHAPTER 35
734
This formula, like the initial resuscitation formulas, is
only an estimate, and replacement of evaporative water loss
should be guided by assessing the adequacy of hydration by
monitoring the patient’s weight, serum osmolality, and
serum sodium concentrations. Following elimination of the
resuscitation-related salt and water load, salt-containing flu-
ids should be administered in the amount needed to main-
tain a normal serum sodium concentration.
Goodwin CW et al: Randomized trial of efficacy of crystalloid and
colloid resuscitation on hemodynamic response and lung water
following thermal injury. Ann Surg 1983;197:520–31. [PMID:
6342554]
Gore DC et al: Influence of glucose kinetics on plasma lactate con-
centrations and energy expenditure in severely burned patients.
J Trauma Inj Infect Crit Care 2000;49:673–8.
Gunn ML et al: Prospective randomized trial of hypertonic sodium
lactate versus lactated Ringer’s solution for burn shock resusci-
tation. J Trauma 1989;29:1261–7. [PMID: 2671402]
Huang PP et al: Hypertonic sodium resuscitation is associated with
renal failure and death. Ann Surg 1995;221:543–54. [PMID:
7748036]
Ivy ME et al: Intra-abdominal hypertension and abdominal com-
partment syndrome in burn patients. J Trauma Inj Infect Crit
Care 2000;49:387–91.
Lorente JA et al: Systemic hemodynamics, gastric intramucosal
P
CO
2
changes and outcome in critically ill burn patients. Crit
Care Med 2000;28:1728–35. [PMID: 10890610]
Onarheim H et al: Effectiveness of hypertonic saline–dextran 70
for initial fluid resuscitation of major burns. J Trauma
1990;30:597–603.
Pruitt BA Jr, Mason AD Jr, Moncrief JA: Hemodynamic changes in
the early postburn patient: The influence of fluid administra-
tion and of a vasodilator (hydralazine). J Trauma 1971;11:
36–46. [PMID: 5099912]
Pruitt BA Jr: Discussion of Caldwell FT and Bowser BH: Critical
evaluation of hypertonic and hypotonic solutions to resuscitate
severely burned children: A prospective study. Ann Surg
1979;189:551–2.
Tanaka H et al: Reduction of resuscitation fluid volumes in severely
burned patients using ascorbic acid administration: A random-
ized, prospective study. Arch Surg 2000;135:326–31. [PMID:
10722036]
Venkatesh B et al: Monitoring tissue oxygenation during resuscita-
tion of major burns. J Trauma 2001;50:485–94.
Escharotomy & Fasciotomy
Edema formation beneath the inelastic eschar of circumfer-
ential full-thickness burns of the extremities may impair the
circulation to the distal and underlying tissues. To prevent
secondary ischemic necrosis of those tissues, an escharotomy
may be necessary to reduce the elevated tissue pressure. To
identify the need for escharotomy, the adequacy of circula-
tion must be assessed at no less than hourly intervals. The
most reliable determination is made with a Doppler flowme-
ter to detect pulsatile blood flow in the palmar arch, digital
vessels in the upper limbs, and pedal vessels in the lower
limbs. Absence or progressive decrease of pulsatile flow on
sequential examination is an indication for escharotomy.
Clinical indicators of impaired extremity perfusion, includ-
ing distal cyanosis, impaired capillary refilling, neurologic
deficits, and deep tissue pain, are less precise in determining
true impairment of blood flow and should be used only as
indications for escharotomy when a Doppler flowmeter is
unavailable. Fascial compartment pressure monitoring also
has been described following thermal injury. Fascial com-
partment pressures often exceed 30 mm Hg following cir-
cumferential extremity burns, and escharotomy based on
compartment pressures has been proposed. A greater sensi-
tivity of direct compartment pressure measurements in
detecting critically low-flow states and preserving threatened
tissues has not been confirmed by direct comparison with
Doppler flowmeter assessments. This technique is associated
with a risk of infection arising in the pressure cannula tract,
but the magnitude of the risk is undefined.
The escharotomy procedure may be performed in the
ICU without the use of general or local anesthesia. Since only
insensate, full-thickness burn is incised, the use of anesthetic
agents is unnecessary. The first escharotomy incision is
placed in the midlateral line of the involved extremity. If this
does not improve distal blood flow, a second escharotomy
incision is made in the mid-medial line of that limb
(Figure 35–4). The escharotomy incision should be per-
formed along the entire length of the full-thickness burn to
Figure 35–4. The dashed lines show the preferred
sites for escharotomy incisions. The solid segments of
the lines demonstrate the importance of extending the
incisions across joints with full-thickness burns.
BURNS
735
ensure adequate release of vascular and neural compression.
The incision must cross involved joints because the relative
lack of subcutaneous tissue in these areas permits ready com-
pression of vessels and nerves. The escharotomy incision
should only penetrate the eschar and immediately subjacent
thin connective tissue to permit expansion of the edematous
subcutis. When performed at this level, loss of blood from
the escharotomy incision is minimal and readily controlled
by electrocoagulation or application of pressure. When inci-
sions are carried into the subcutaneous tissues, excessive
bleeding often occurs. The consumptive coagulopathy that
may occur in the early postburn period may contribute to
excessive blood loss when escharotomy incisions are made
too deep.
Fasciotomy is rarely required to restore circulation in a
thermally injured limb. However, in patients with high-
voltage electrical injury, fasciotomy is often necessary.
Patients with very deep burns involving fascia and muscle or
patients with associated traumatic injuries may require
fasciotomies to restore adequate limb circulation.
Escharotomies also may be required in patients with cir-
cumferential truncal burns to relieve restriction of chest wall
movement by the unyielding eschar and restore more effec-
tive ventilation. The escharotomy incision is made in the
anterior axillary line in the area of full-thickness burn. An
incision along the lower margin of the rib cage may be nec-
essary in patients with deep burns extending onto the upper
abdominal wall (see Figure 35–4). Patients may become rest-
less, agitated, and tachypneic despite having an adequate air-
way, indicating the need for chest escharotomy. In
mechanically ventilated patients, the need for escharotomy is
manifested by a progressive increase in peak inspiratory pres-
sure, decreased tidal volumes in pressure-controlled ventila-
tion, and an increase in the end-tidal CO
2
fraction. Once
chest escharotomy is performed, these changes promptly
revert toward normal.
Saffle JR, Zeluff GR, Warden GD: Intramuscular pressure in the
burned arm: Measurement and response to escharotomy. Am J
Surg 1980;140:825–31. [PMID: 7457708]
CARE OF THE BURN WOUND
Debridement
Only after respiratory and hemodynamic stability have been
achieved should care of the burn wound be addressed.
During transport of the patient from the accident scene or
from the initial care facility to a burn center, the burns
should be covered with clean sheets or blankets and no
attempt made to debride or dress them. In the absence of
gross contamination, burn wounds may be managed safely
without topical antimicrobial agents for the first 24–48
hours. When the patient arrives at the definitive care facility,
general anesthesia is not necessary for initial burn wound
debridement; intravenous analgesia is sufficient for pain
control during this procedure. The burns are gently cleansed
with a surgical soap solution, and nonviable epidermis is
debrided. Bullae are excised, and body hair is shaved from
the area of thermal injury beyond the margin of normal skin.
The patient is placed in a clean bed, and bulky dressings may
be placed beneath the burned parts to absorb the serous exu-
date. These dressings should be changed as they become sat-
urated. Patients should be turned frequently to prevent
maceration of burned and unburned skin.
Topical Antimicrobial Therapy
The development and clinical use of effective topical antimi-
crobial agents has decreased the incidence of invasive burn
wound infection and subsequent sepsis significantly. This has
been associated with improved survival of burn patients and
nearly eliminated invasive bacterial burn wound infection as
a cause of death. Mafenide (Sulfamylon), silver sulfadiazine
(Silvadene), and silver nitrate are the three topical antimicro-
bial agents employed most commonly for burn wound care.
Each agent has specific advantages and limitations with
which the physician must be familiar to ensure optimal ben-
efit and patient safety. Mafenide acetate and silver sulfadi-
azine are available as topical creams to be applied directly to
the burn wound. Silver nitrate is applied as a 0.5% solution
in occlusive dressings.
Mafenide burn cream is an 8.5% by weight suspension of
mafenide acetate in a water-soluble base. Mafenide is very
water-soluble and diffuses freely into the eschar. Mafenide is
the preferred agent if the patient has heavily contaminated
burn wounds or has had burn wound care delayed by several
days. Mafenide has the added advantage of being highly
effective against gram-negative organisms. The limitations of
mafenide burn cream include hypersensitivity reactions in
7% of patients, pain or discomfort of 20–30 minutes’ dura-
tion when applied to partial-thickness burns, and carbonic
anhydrase inhibition. The latter may produce an early bicar-
bonate diuresis and increase postburn hyperventilation.
This metabolic acidosis may develop into significant
acidemia if respiratory complications occur and the com-
pensatory hyperventilation is impaired. Carbonic anhydrase
inhibition rarely persists for more than 7–10 days, and the
severity of acidosis can be minimized if mafenide is applied
once per day followed by an application of silver sulfadiazine
cream 12 hours later.
Silver sulfadiazine burn cream is a 1% suspension of sil-
ver sulfadiazine in a water-miscible base. Unlike mafenide
acetate, silver sulfadiazine has limited solubility in water and
thus limited penetration into the eschar. The agent is most
effective when applied to burns immediately after injury to
minimize bacterial proliferation on the wound’s surface. This
agent has the advantage of being painless on application and
has no effect on serum electrolytes or acid-base balance.
Silver sulfadiazine burn cream may induce neutropenia,
which usually subsides after discontinuation of the agent.
CHAPTER 35
736
Hypersensitivity is uncommon and is manifested by an ery-
thematous maculopapular rash on unburned skin. The sulfa-
diazine component of silver sulfadiazine is ineffective against
certain strains of Pseudomonas and virtually all Enterobacter
species; however, the sensitivity of microorganisms coloniz-
ing burn wounds to the silver ion of this compound main-
tains its effectiveness as a topical antimicrobial agent.
Either cream is applied in an
1
/
8
-inch layer to the entire
burn wound in an aseptic manner following initial debride-
ment and is reapplied at 12-hour intervals to ensure contin-
uous topical chemotherapy. Once each day, all the topical
agent should be cleansed from the patient using a surgical
detergent or disinfectant solution and the wounds inspected
by the attending physician.
Silver nitrate solution (0.5%) delivered in multilayered
occlusive gauze dressings may provide an effective antimicro-
bial barrier to the burn wound surface. This agent is employed
most commonly when a history of allergy to sulfonamide
drugs is elicited or when the patient develops a hypersensitiv-
ity reaction to one of the burn creams. The dressings are
changed two or three times daily and moistened every 2 hours
to prevent evaporation from increasing the silver nitrate con-
centration to cytotoxic levels within the dressings. Transeschar
leaching of sodium, potassium, chloride, and calcium should
be anticipated and replaced appropriately. Because silver
nitrate precipitates on contact with the proteinaceous exudate
of the burn wound and does not penetrate the eschar, it is not
effective for treatment of burn wound infection or for prophy-
lactic treatment of heavily contaminated wounds. A common
use of silver nitrate is for topical antimicrobial prophylaxis in
patients with toxic epidermal necrolysis syndrome, a disorder
caused by idiosyncratic drug reactions resulting in significant
epidermal sloughing. Hypersensitivity to silver nitrate has not
been described.
Acticoat is a new burn wound dressing. It consists of a
urethane film onto which nanocrystalline elemental silver is
deposited. When moistened, application of this dressing to
the wound results in a sustained release of elemental silver,
which is bactericidal and fungicidal. The mechanism of
action is probably much like that of silver nitrate dressings;
however, Acticoat does not cause transeschar leaching of
electrolytes. The silver does not penetrate the eschar, limiting
its use on infected or heavily contaminated wounds.
Transient mild pain may be noted occasionally after applica-
tion. The use of Acticoat is currently limited to partial-thick-
ness burns.
Aquacel Ag hydrofiber (ConvaTec, a Bristol-Myers Squibb
Company, Skillman, NJ) is another dressing containing ele-
mental silver, although at a much lower concentration. When
compared with silver sulfadiazine on partial-thickness burns,
this dressing was associated with an increased rate of reep-
ithelization and was a slightly more cost-effective. This study
was limited owing to sample size; however, the replacement
of burn cream pharmaceuticals with silver-containing bar-
rier dressings is occurring in certain settings, namely, those
of superficial burns.
All these agents are effective in the prevention of inva-
sive burn wound infection. However, because of their lack
of eschar penetration, silver nitrate soaks and silver sulfa-
diazine burn cream are most effective in the treatment of
full-thickness burns when applied immediately following
burn injury.
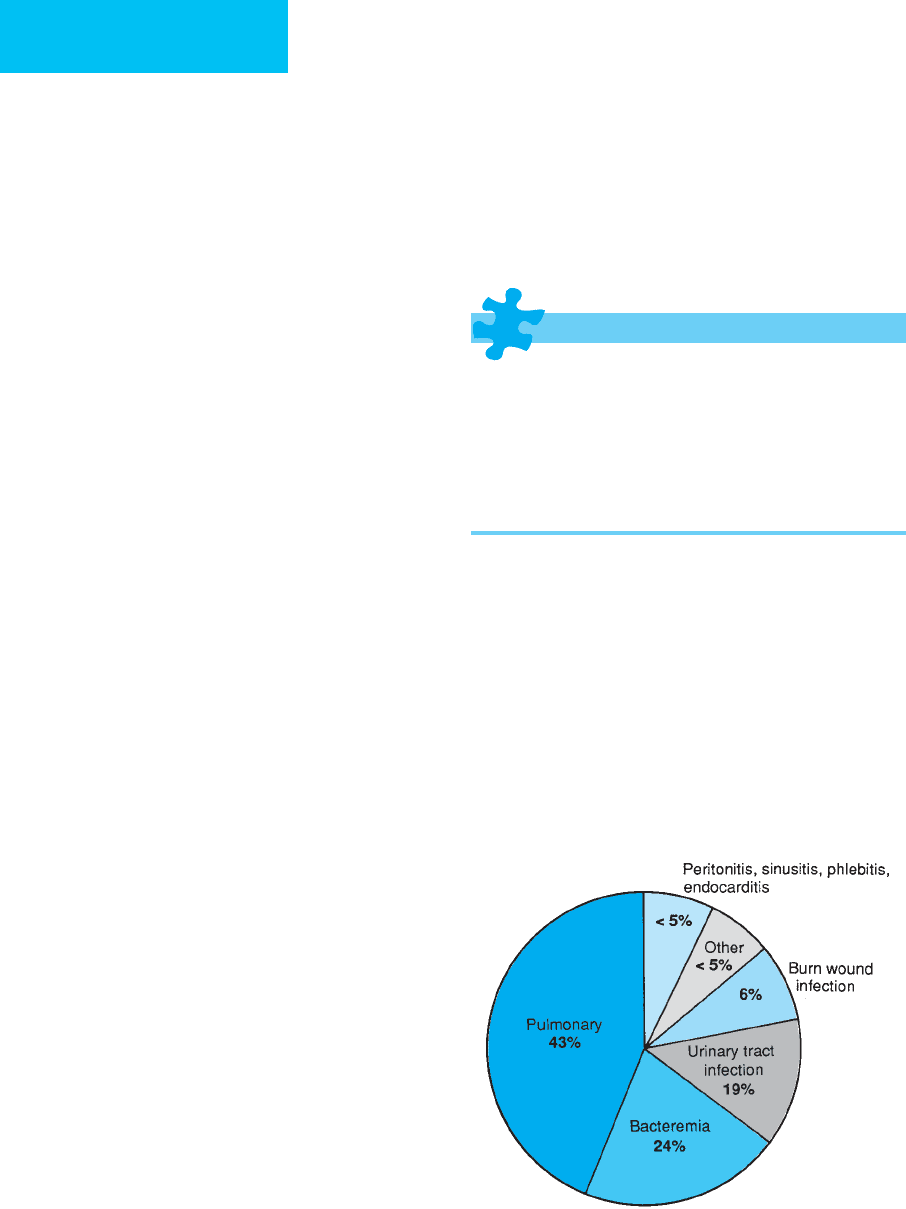
Burn Wound Infection (See Figure 35–5)
ESSENTIALS OF DIAGNOSIS
Hypo- or hyperthermia.
Tachycardia and tachypnea.
Glucose intolerance.
Disorientation.
Ileus.
Change in appearance of the burn wound.
General Considerations
Inherent characteristics of the microorganisms and the burn
wound they colonize influence the rate of microbial penetra-
tion of and proliferation in the eschar. The moist, protein-
rich, avascular eschar serves as an excellent culture medium
from which white blood cells and systemically administered
antibiotics are excluded. The density of bacterial coloniza-
tion of the eschar influences the likelihood of burn wound
infection. Bacterial invasion is uncommon unless the num-
ber of microorganisms exceeds 10
5
per gram of tissue.
Bacterial strain–specific factors such as enzyme production
Figure 35–5. The frequency of infection by site
expressed as a percentage of all infections complicating
thermal injury.
