Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


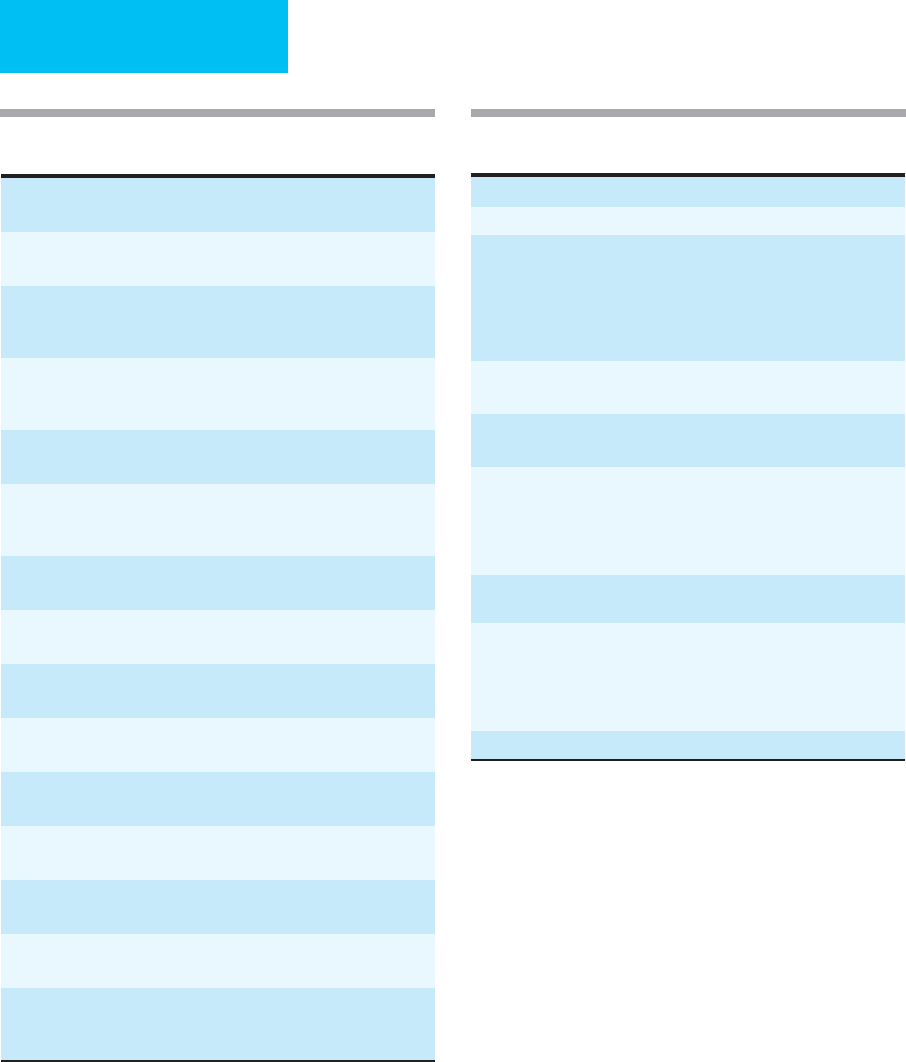
AUTHORS
ix
Bruce L. Miller, MD
Clausen Distinguished Professor of Neurology, University
of California, San Francisco; Memory and Aging Center,
San Francisco, California
bruce@email.his.ucsf.edu
Critical Care of Neurologic Disease
David W. Mozingo, MD
Professor of Surgery and Anesthesiology, University of
Florida; Chief, Division of Acute Care Surgery, Director,
Shands Burn Center, Gainesville, Florida
mozindw@surgery.ufl.edu
Burns
Kenneth A. Narahara, MD
Professor of Medicine, David Geffen School of Medicine,
University of California, Los Angeles, School of
Medicine; Assistant Chair for Clinical Affairs,
Department of Medicine, Director, Coronary Care,
Division of Cardiology, Harbor-UCLA Medical Center,
Torrance, California
knarahara@labiomed.org
Coronary Heart Disease
Gideon P. Naudé, MD
Chairman, Department of Surgery, Tuolumne General
Hospital, Sonora, California
gpnaude@aol.com
Gastrointestinal Failure in the ICU
Dean C. Norman, MD
Chief of Staff, Veterans Administration Greater Los Angeles
Healthcare System; Professor of Medicine, University of
Southern California, Los Angeles, California
Dean.Norman@med.va.gov
Care of the Elderly Patient
Basil A. Pruitt, Jr., MD, FACS, FCCM
Clinical Professor, Department of Surgery, University of
Texas Health Science Center at San Antonio; Consultant,
U.S. Army Institute of Surgical Research, San Antonio,
Texas
pruitt@uthscsa.edu
Burns
Steven S. Raman, MD
Associate Professor, Department of Radiology, David Geffen
School of Medicine, University of California,
Los Angeles, California
SRaman@mednet.ucla.edu
Imaging Procedures
Sofiya Reicher, MD
Assistant Clinical Professor of Medicine, David Geffen
School of Medicine, University of California, Los Angeles,
California
sreicher@sbcglobal.net
Gastrointestinal Bleeding
William P. Schecter, MD
Professor of Clinical Surgery and Vice Chair, University
of California, San Francisco, San Francisco, California;
Chief of Surgery, San Francisco General Hospital, San
Francisco, California
bschect@sfghsurg.ucsf.edu
Care of Patients with Environmental Injuries
Paul A. Selecky, MD
Clinical Professor of Medicine, David Geffen School of
Medicine, University of California, Los Angeles,
California; Medical Director, Pulmonary Department,
Hoag Hospital, Newport Beach, California
pselecky@hoaghospital.org
Ethical, Legal, & Palliative/End-of-Life Care Considerations
Shelley Shapiro, MD, PhD
Clinical Professor of Medicine, David Geffen School of
Medicine, University of California, Los Angeles,
California
sshapiro@ucla.edu
Cardiac Problems in Critical Care
Elizabeth D. Simmons, MD
Partner, Southern California Permanente Medical Group,
Los Angeles, California
Elizabeth.D.Simmons@kp.org
Transfusion Therapy; Bleeding & Hemostasis; Antithrombotic
Therapy
Michael J. Stamos, MD
Professor of Surgery and Chief, Division of Colon and Rectal
Surgery, University of California, Irvine, Orange, California
mstamos@uci.edu
Acute Abdomen
Samuel J. Stratton, MD, MPH
Professor of Emergency Medicine, University of California
Irvine, Orange, California
sstratton@att.net
Transport

AUTHORS
x
Darryl Y. Sue, MD
Professor of Clinical Medicine, David Geffen School
of Medicine, University of California, Los Angeles,
California; Director, Medical-Respiratory Intensive Care
Unit, Division of Respiratory and Critical Care
Physiology and Medicine, Associate Chair
and Program Director, Department of Medicine,
Harbor-UCLA Medical Center, Torrance, California
dsue@ucla.edu
Philosophy & Principles of Critical Care; Fluids, Electrolytes,
& Acid-Base; Pharmacotherapy; Intensive Care
Monitoring; Respiratory Failure; Critical Care
of the Oncology Patient; Pulmonary Disease; HIV
Infection in the Critically Ill Patient
John A. Tayek, MD
Associate Professor of Medicine-in-Residence, David Geffen
School of Medicine, University of California, Los Angeles,
Harbor-UCLA Medical Center, Torrance, California
jtayek@ladhs.org
Nutrition
Timothy L. Van Natta, MD
Associate Professor of Surgery, David Geffen School of
Medicine, University of California, Los Angeles,
Harbor-UCLA Medical Center, Torrance, California
timothy.vannatta@gmail.com
Surgical Infections
Hernan I. Vargas, MD
Associate Professor of Surgery, David Geffen School
of Medicine, University of California, Los Angeles,
California; Chief, Division of Surgical Oncology, Harbor-
UCLA Medical Center, Torrance, California
hvargas@ucla.edu
Hepatobiliary Disease
Edward D. Verrier, MD
William K. Edmark Professor of Cardiovascular Surgery,
Vice Chairman, Department of Surgery, University
of Washington, Seattle, Washington; Chief, Division
of Cardiothoracic Surgery, University of Washington,
Seattle, Washington
edver@u.washington.edu
Cardiothoracic Surgery
Janine R. E. Vintch, MD
Associate Clinical Professor of Medicine, David Geffen
School of Medicine, University of California, Los
Angeles, Divisions of General Internal Medicine and
Respiratory and Critical Care Physiology and Medicine,
Harbor-UCLA Medical Center, Torrance, California
jvintch@ladhs.org
Respiratory Failure; Pulmonary Disease
Kenneth Waxman, MD
Director of Surgical Education, Santa Barbara Cottage
Hospital, Santa Barbara, California
kwaxman@sbch.org
Intensive Care Monitoring
Mallory D. Witt, MD
Professor of Medicine, David Geffen School of Medicine,
University of California, Los Angeles, California;
Associate Chief, Division of HIV Medicine, Harbor-
UCLA Medical Center, Torrance, California
mwitt@labiomed.org
Infections in the Critically Ill; HIV Infection in the
Critically Ill Patient
Nam C. Yu, MD
Resident Physician, Department of Radiology, David Geffen
School of Medicine, University of California,
Los Angeles, California
nyu@mednet.ucla.edu
Imaging Procedures
Kory J. Zipperstein, MD
Chief, Department of Dermatology, Kaiser-Permanente
Medical Center, San Francisco, California
Kory.Zipperstein@kp.org
Dermatologic Problems in the Intensive Care Unit
xi
Preface
The third edition of Current Diagnosis & Treatment: Critical Care is designed to serve as a single-source reference for the adult
critical care practitioner. The diversity of illnesses encountered in the critical care population necessitates a well-rounded and
thorough knowledge of the manifestations and mechanisms of disease. In addition, unique to the discipline of critical care is
the integration of an extensive body of medical knowledge that crosses traditional specialty boundaries. This approach is
readily apparent to intensivists, whose primary background may be in internal medicine or one of its subspecialties, surgery,
or anesthesiology. Thus a central feature of this book is a unified and integrated approach to the problems encountered in
critical care practice. Like other books with the Lange imprint, this book emphasizes recall of major diagnostic features,
concise descriptions of disease processes, and practical management strategies based on often recently acquired evidence.
INTENDED AUDIENCE
Planned by two internists and a surgeon to meet the need for a concise but thorough source of information, Current Diagnosis
& Treatment: Critical Care is intended to facilitate both teaching and practice of critical care. Students will find its consid-
eration of basic science and clinical application useful during clerkships on medicine, surgery, and intensive care unit electives.
House officers will appreciate its descriptions of disease processes and organized approach to diagnosis and treatment. Fellows
and those preparing for critical care specialty examinations will find those sections outside their primary disciplines particu-
larly useful. Clinicians will recognize this succinct reference on critical care as a valuable asset in their daily practice.
Because this book is intended as a reference on various aspects of adult critical care, it does not contain chapters on
pediatric or neonatal critical care. These areas are highly specialized and require entire monographs of their own. Further, we
have not included detailed information on performing bedside procedures such as central venous catheterization or arterial line
insertion. Well-illustrated pocket manuals are available for readers who require basic technical information. Finally, we have
chosen not to include a chapter on nursing or administrative topics, details of which can be found in other works.
ORGANIZATION
Current Diagnosis & Treatment: Critical Care is conceptually organized into three major sections: (1) fundamentals of crit-
ical care applicable to all patients, (2) topics related primarily to critical care of patients with medical diseases, and (3) essentials of
care for patients requiring care for surgical problems. Early chapters provide information about the general physiology and
pathophysiology of critical illness. The later chapters discuss pathophysiology using an organ system– or disease-specific
approach. Where appropriate, we have placed the medical and surgical chapters in succession to facilitate access to information.
OUTSTANDING FEATURES
Concise, readable format, providing efficient use in a variety of clinical and academic settings
Edited by both surgical and medical intensivists, with contributors from multiple subspecialties
Illustrations chosen to clarify basic and clinical concepts
Careful evaluation of new diagnostic procedures and their usefulness in specific diagnostic problems
Updated information on the management of severe sepsis and septic shock, including hydrocortisone therapy
New information on the serotonin syndrome
Carefully selected key references in Index Medicus format, providing all information necessary to allow electronic retrieval
ACKNOWLEDGMENTS
The editors wish to thank Robert Pancotti and Ruth W. Weinberg at McGraw-Hill for unceasing efforts to motivate us and keep
us on track. We are also very grateful to our families for their support.
Frederic S. Bongard, MD
Darryl Y. Sue, MD
Janine R. E. Vintch, MD
July 2008
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
This page intentionally left blank
1
1
Philosophy & Principles
of Critical Care
Darryl Y. Sue, MD
Frederic S. Bongard, MD
Critical care is unique among the specialties of medicine.
While other specialties narrow the focus of interest to a sin-
gle body system or a particular therapy, critical care is
directed toward patients with a wide spectrum of illnesses.
These have the common denominators of marked exacerba-
tion of an existing disease, severe acute new problems, or
severe complications from disease or treatment. The range
of illnesses seen in a critically ill population necessitates
well-rounded and thorough knowledge of the manifesta-
tions and mechanisms of disease. Assessing the severity of
the patient’s problem demands a simultaneously global and
focused approach, depends on accumulation of accurate
data, and requires integration of these data. Although prac-
titioners of critical care medicine—sometimes called
intensivists—are often specialists in pulmonary medicine,
cardiology, nephrology, anesthesiology, surgery, or critical
care, the ability to provide critical care depends on the basic
principles of internal medicine and surgery. Critical care
might be considered not so much a specialty as a “philoso-
phy” of patient care.
The most important development in recent years has
been an explosion of evidence-based critical care medicine
studies. For the first time, we have evidence for many of the
things that we do for patients in the ICU. Examples include
low tidal volume strategies for acute respiratory distress
syndrome, tight glycemic control, prevention of ventilator-
associated pneumonia, and use of corticosteroids in septic
shock (Table 1–1). The resulting improvement in outcome
is gratifying, but even more surprising is how often evi-
dence contradicts long-held beliefs and assumptions.
Probably the best example is recent studies that conclude
that the routine use of pulmonary artery catheters in ICU
patients adds little or nothing to management. Much more
needs to be studied, of course, to address other unresolved
issues and controversies.
Do intensivists make a difference in patient outcome?
Several studies have shown that management of patients by
full-time intensivists does improve patient survival. In fact,
several national organizations recommend strongly that full-
time intensivists provide patient care in all ICUs. It can be
argued, however, that local physician staffing practices;
interactions among primary care clinicians, subspecial-
ists, and intensivists; patient factors; and nursing and
ancillary support play large roles in determining out-
comes. In addition, recent studies show that patients do
better if an ICU uses protocols and guidelines for routine
care, controls nosocomial infections, and provides feed-
back to practitioners.
The general principles of critical care are presented in this
chapter, as well as some guidelines for those who are respon-
sible for leadership of ICUs.
GENERAL PRINCIPLES OF CRITICAL CARE
Early Identification of Problems
Because critically ill patients are at high risk for developing
complications, the ICU practitioner must remain alert to
early manifestations of organ system dysfunction, complica-
tions of therapy, potential drug interactions, and other pre-
monitory data (Table 1–2). Patients with life-threatening
illness in the ICU commonly develop failure of other
organs because of hemodynamic compromise, side effects
of therapy, and decreased organ function reserve, espe-
cially those who are elderly or chronically debilitated. For
example, positive-pressure mechanical ventilation is asso-
ciated with decreased perfusion of organs. Many valuable
drugs are nephro- or hepatotoxic, especially in the face of
preexisting renal or hepatic insufficiency. Older patients
are more prone to drug toxicity, and polypharmacy pres-
ents a higher likelihood of adverse drug interactions. Just as
patients with acute coronary syndrome and stroke benefit
from early intervention, an exciting finding is the evidence
that the first 6 hours of management of septic shock are very
important.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 1
2
Identifying and acting on new problems and complica-
tions in the ICU demands frequent and regular review of all
information available, including changes in symptoms, phys-
ical findings, and laboratory data and information from mon-
itors. In some facilities, early identification and treatment are
provided by rapid-response teams. Once notified that a patient
outside the ICU may be deteriorating, the team is mobilized
to provide a mini-ICU environment in which critical care can
be delivered early, even before the patient is actually
transferred.
Effective Use of the Problem-Oriented
Medical Record
The special importance of finding, tracking, and being aware
of ICU issues demands an effective problem-oriented med-
ical record. In order to define and follow problems effec-
tively, each problem should be reviewed regularly and
characterized at its current state of understanding. For exam-
ple, if the general problem of “renal failure” subsequently has
been determined to be due to aminoglycoside toxicity, it
should be described in that way in an updated problem list.
However, even the satisfaction of identifying a cause of the
renal failure may be short-lived. The same patient subse-
quently may develop other related or unrelated renal prob-
lems, thereby forcing reassessment.
In our opinion, ICU problems must not be restricted to
“diagnoses.” We list intravascular catheters and the date they
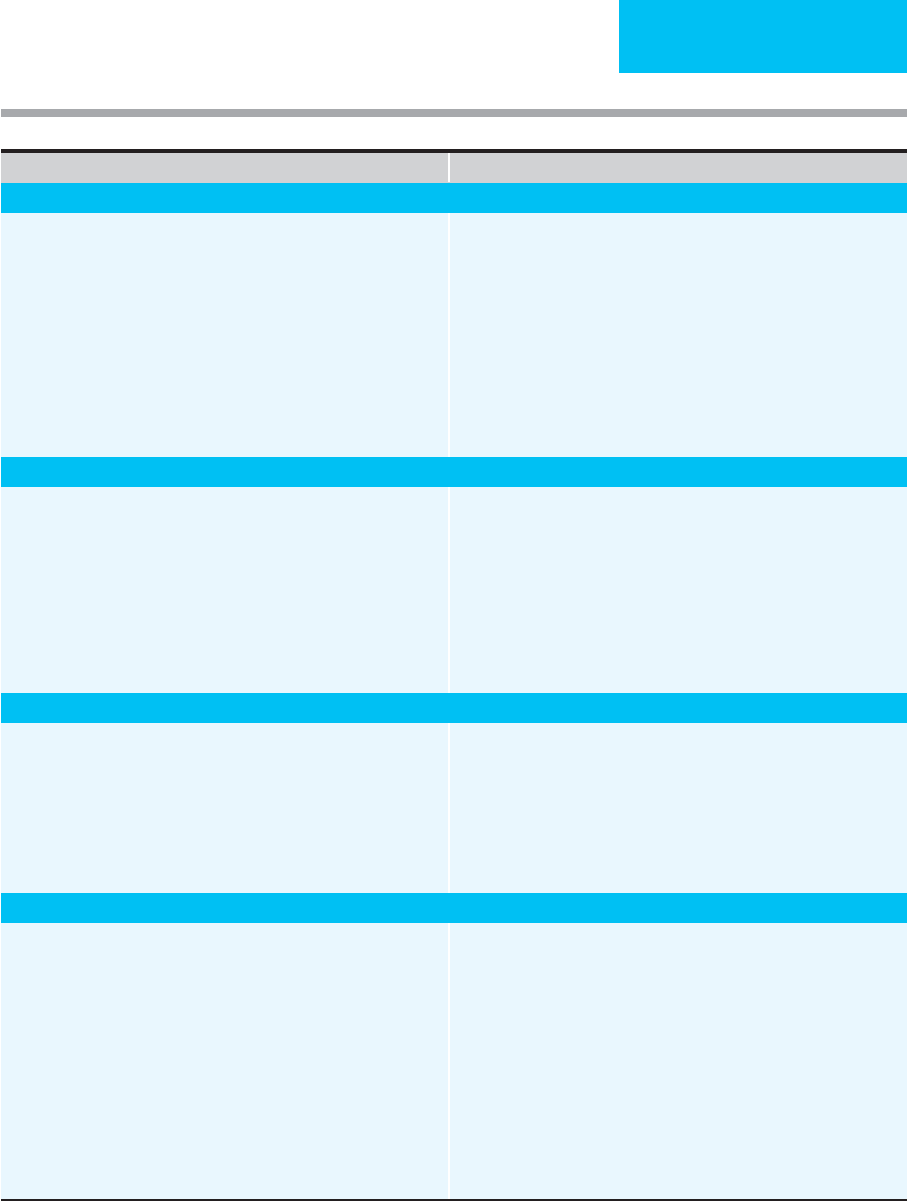
Table 1–1. Recent developments in evidence-based
critical care medicine.
Table 1–2. Recommendations for routine patient care in
the ICU.
• Assess current status, interval history, and examination.
• Review vital signs for interval period (since last review).
• Review medication record, including continuous infusions:
Duration and dose
Changes in dose or frequency based on changes in renal, hepatic,
or other pharmacokinetic function
Changes in route of administration
Potential drug interactions
• Correlate changes in vital signs with medication administration and
other changes by use of chronologic charting.
• Integrate nursing, respiratory therapists, patient, family, and other
observations.
• Review, if indicated:
Respiratory therapy flow chart
Hemodynamics records
Laboratory flowsheets
Other continuous monitoring
• Review all problems, including adding, updating, consolidating, or
removing problems as indicated.
• Periodically, review supportive care:
Intravenous fluids
Nutritional status and support
Prophylactic treatment and support
Duration of catheters and other invasive devices
• Review and contrast risks and benefits of intensive care.
• Corticosteroids improve outcome in exacerbations of chronic obstruc-
tive respiratory disease (COPD).
• A low tidal volume strategy decreases mortality in acute respiratory
distress syndrome (ARDS).
• A lower hemoglobin decision point for transfusion of red blood cells
in many ICU patients results in similar outcome and greatly reduced
use of blood products.
• Tight glycemic control in postoperative surgical patients, most of
whom did not have diabetes, resulted in less mortality and fewer
complications.
• Elevating the head of the bed to 30–45 degrees in ICU patients
reduces the incidence of nosocomial pneumonia.
• Daily withholding of sedation in the ICU decreases the number of
ICU days and results in fewer evaluations for altered level of
consciousness.
• Daily spontaneous breathing trials lead to faster weaning from
mechanical ventilation and shorter duration of ICU stay.
• Low-dose (physiologic) vasopressin may reduce the need for pres-
sors in septic shock.
• Fluid resuscitation using colloid-containing solutions is not more ben-
eficial than crystalloid fluids.
• Low-dose dopamine does not improve renal function or diuresis and
does not protect against renal dysfunction.
• Acetylcysteine or sodium bicarbonate protect against radiocontrast
material–induced acute renal failure.
• Patients with bleeding esophageal varices have a higher rebleeding
risk if they have infection, especially spontaneous bacterial peritonitis.
• Noninvasive positive-pressure ventilation decreases the need for
intubation in patients with COPD exacerbation.
• Noninvasive positive-pressure ventilation is associated with fewer
respiratory infections than conventional ventilation.
• Early goal-directed therapy for sepsis (specific targets for central
venous pressure, hemoglobin, and central venous oxygen content
during the first 6 hours of care) decreases mortality.

PHILOSOPHY & PRINCIPLES OF CRITICAL CARE
3
were inserted on the problem list. This helps us to remember
to consider the catheter as a site of infection if the patient
has a fever. Other “nondiagnoses” on our problem list
include nutritional support, prevention of deep vein
thrombosis and decubitus ulcers, drug allergies, patient
positioning, and prevention of stress ulcers. It may be use-
ful to include nonmedical issues as well so that they can be
discussed routinely. Examples are psychosocial difficul-
ties, unresolved end-of-life decisions, and other questions
about patient comfort. Finally, we share the patient’s
problem-oriented record with nonphysicians caring for the
patient, a process that enhances communication, simplifies
interactions between staff members, and furthers the goals
of patient care.
Monitoring & Data Display
A tremendous amount of patient data is acquired in the
ICU. Although ICU monitoring is often thought of as
electrocardiography, blood pressure measurements, and
pulse oximetry, ICU data include serial plasma glucose
and electrolyte determinations, arterial blood gas deter-
minations, documentation of ventilator settings and
parameters, and body temperature determinations. Taking
a daily weight is invaluable in determining the net fluid
balance of a patient.
Flowcharts of laboratory data and mechanical ventilator
activity, 24-hour vital signs, graphs of hemodynamic data, and
lists of medications are indispensable tools for good patient
care, and efforts should be made to find the most effective and
efficient ways of displaying such information in the ICU.
Methods that integrate the records of physicians, nurses, respi-
ratory therapists, and others are particularly useful.
Computer-assisted data collection and display systems
are found increasingly in ICUs. Some of these systems
import data directly from bedside monitors, mechanical
ventilators, intravenous infusion pumps, fluid collection
devices, clinical laboratory instruments, and other devices.
ICU practitioners may enter progress notes, medications
administered, and patient observations. Advantages of these
systems include decreased time for data collection and the
ability to display data in a variety of formats, including flow-
charts, graphs, and problem-oriented records. Such data can
be sent to remote sites for consultation, if necessary.
Computerized access to data facilitates research and quality
assurance studies, including the use of a variety of prognos-
tic indicators, severity scores, and ICU decision-making
tools. Computerized information systems have the potential
for improving patient care in the ICU, and their benefit to
patient outcome continues to be studied.
The next step is to integrate ICU data with treatment,
directly and indirectly. One excellent example is glycemic
control so that up-to-date blood glucose measurements
will be linked closely to insulin protocols—at first with
the nurse and physician “in the loop” but potentially with
real-time feedback and automated adjustment of insulin
infusions.
Supportive & Preventive Care
Many studies have pointed out the high prevalence of gas-
trointestinal hemorrhage, deep venous thrombosis, decu-
bitus ulcers, inadequate nutritional support, nosocomial
and ventilator-associated pneumonias, urinary tract infec-
tions, psychological problems, sleep disorders, and other
untoward effects of critical care. Efforts have been made to
prevent, treat, or otherwise identify the risks for these
complications. As outlined in subsequent chapters, effec-
tive prevention is available for some of these risks (Table 1–3);
for other complications, early identification and aggres-
sive intervention may be of value. For example, aggressive
nutritional support for critically ill patients is often indi-
cated both because of the presence of chronic illness and
malnutrition and because of the rapid depletion of
nutritional reserves in the presence of severe illness.
Nutritional support, prevention of upper gastrointestinal
bleeding and deep venous thrombosis, skin care, and other
supportive therapy should be included on the ICU
patient’s problem list. To these, we have added glycemic
control because of recent data indicating reduced morbid-
ity and mortality in medical and surgical patients whose
plasma glucose concentration is maintained in a relatively
narrow range.
Because of expense and questions of effectiveness and
safety, studies of preventive treatment of ICU patients con-
tinue. For example, a multicenter study reported that clini-
cally important gastrointestinal bleeding in critically ill
patients was seen most often only in those with respiratory
failure or coagulopathy (3.7% for one or both factors).
Otherwise, the risk for significant bleeding was only 0.1%.
The authors suggested that prophylaxis against stress ulcer
could be withheld safely from critically ill patients unless
they had one of these two risk factors. On the other hand,
about half the patients in this study were post–cardiac sur-
gery patients, and the majority of patients in many ICUs have
one of the identified risk factors. Thus there may not be suf-
ficient compelling evidence to discontinue the practice of
providing routine prophylaxis for gastrointestinal bleeding
in all ICU patients.
Other routine practices have been challenged. For exam-
ple, several studies show that routine transfusion of red
blood cells in ICU patients who reached an arbitrary hemo-
globin level did not change outcome when compared with
allowing hemoglobin to fall to a lower value. Further studies
are needed to define the role of other preventive strategies.
Important questions include differences in the need for
glycemic control, critical differences in the intensity and type
of therapy needed to prevent thrombosis, the optimal hemo-
globin for patients with myocardial infarction, and the bene-
fit of tailored nutritional support.

CHAPTER 1
4
(
continued
)
Things To Think About Reminders
General ICU Care
1. Nosocomial infections, especially line- and catheter-related.
2. Stress gastritis.
3. Deep venous thrombosis and pulmonary embolism.
4. Exacerbation of malnourished state.
5. Decubitus ulcers.
6. Psychosocial needs and adjustments.
7. Toxicity of drugs (renal, pulmonary, hepatic, CNS).
8. Development of antibiotic-resistant organisms.
9. Complications of diagnostic tests.
10. Correct placement of catheters and tubes.
11. Need for vitamins (thiamine, C, K).
12. Tuberculosis, pericardial disease, adrenal insufficiency, fungal sepsis,
rule out myocardial infarction, pneumothorax, volume overload or
volume depletion, decreased renal function with normal serum crea-
tinine, errors in drug administration or charting, pulmonary vascular
disease, HIV-related disease.
1. Discontinue infected or possibly infected lines.
2. Need for H2 blockers, antacids, or sucralfate.
3. Provide enteral or parenteral nutrition.
4. Change antibiotics?
5. Chest x-ray for line placement.
6. Review known drug allergies (including contrast agents).
7. Check for drug dosage adjustments (new liver failure or renal failure).
8. Need for deep venous thrombosis prophylaxis?
9. Pain medication and sedation.
10. Weigh patient.
11. Give medications orally, if possible.
12. Does patient really need an arterial catheter?
13. Give thiamine early.
Nurition
1. Set goals for appropriate nutrition support.
2. Avoid or minimize catabolic state.
3. Acquired vitamin K deficiency while in ICU.
4. Avoidance of excessive fluid intake.
5. Diarrhea (lactose intolerance, low serum protein, hyperosmolarity,
drug-induced, infectious).
6. Minimize and anticipate hyperglycemia during parenteral nutritional
support.
7. Adjustment of rate or formula in patients with renal failure or liver
failure.
8. Early complications of refeeding.
9. Acute vitamin insufficiency.
1. Calculate estimated basic caloric and protein needs. Use 30 kcal/kg
and 1.5 g protein/kg for starting amount.
2. Regular food preferred over enteral feeding; enteral feeding preferred
over parenteral in most patients.
3. Increased caloric and protein requirements if febrile, infected, agitated,
any inflammatory process ongoing, some drugs.
4. Adjust protein if renal or liver failure is present. Adjust again if dialysis
is used.
5. Measure serum albumin as primary marker of nutritional status.
6. Give vitamin K, especially if malnourished and receiving antibiotics.
7. Consider volume restriction formulas (both enteral and parenteral).
8. Give phosphate early during refeeding.
9. Control hyperglycemia (glucose <110–120 mg/dL).
Acute Renal Failure
1. Volume depletion, hypoperfusion, low cardiac output, shock.
2. Nephrotoxic drugs.
3. Obstruction of urine outflow.
4. Interstitial nephritis.
5. Manifestation of systemic disease, multiorgan system failure.
6. Degree of preexisting chronic renal failure.
1. Measure urine Na
+
, Cl
–
, creatinine, and osmolality.
2. Volume challenge, if indicated.
3. Discontinue nephrotoxic drugs if possible.
4. Adjust all renally excreted drugs.
5. Renal medicine consultation for dialysis, other management.
6. Renal ultrasound if indicated for obstruction.
7. Check catheter and replace if indicated.
8. Stop potassium supplementation if necessary.
9. Adjust diet (Na
+
, protein, etc.).
10. If dialytic therapy is begun, adjust drugs if necessary.
11. Weigh patient daily.
Table 1–3. Things to think about and reminders for ICU patient care.
PHILOSOPHY & PRINCIPLES OF CRITICAL CARE
5
Things To Think About Reminders
Acute Respiratory Failure, COPD
1. Adequacy of oxygenation.
2. Exacerbation due to infection, malnutrition, congestive heart failure.
3. Airway secretions.
4. Other medical problems (coexisting heart failure).
5. Hypotension and low cardiac output response to positive-pressure
ventilation.
6. Hyponatremia, SIADH.
7. Severe pulmonary hypertension.
8. Sleep deprivation.
9. Coexisting metabolic alkalosis.
1. Should patient be intubated or mechanically ventilated?
Noninvasive mechanical ventilation?
2. Bronchodilators.
3. Consider corticosteroids, ipratropium.
4. Sufficient supplemental oxygen.
5. Antibiotic coverage for common bacterial causes of exacerbations.
Evaluate for pneumonia as well as acute bronchitis.
6. Early nutrition support.
7. Check theophylline level, if indicated.
8. Ventilator management: low tidal volume, long expiratory time, high
inspiratory flow, watch for auto-PEEP.
9. Think about weaning early.
Acute Respiratory Failure, ARDS
1. Sepsis as cause, from pulmonary or nonpulmonary site (abdominal,
urinary).
2. Possible aspiration of gastric contents.
3. Fluid overload or contribution form congestive heart failure.
4. Anticipate potential multiorgan system failure.
5. Assess the risks of oxygen toxicity versus complications of PEEP.
6. Consider the complications of high airway pressure or large tidal vol-
ume in selection of type of mechanical ventilatory support.
7. Low serum albumin (contribution from hypo-oncotic pulmonary
edema).
1. Early therapeutic goal of Fi0
2
<0.50 and lowest PEEP (<5–10 cm H
2
O),
resulting in acceptable O
2
delivery.
2. Directed (if possible) or broad-spectrum antibiotics.
3. Evaluate for soft tissue or intra-abdominal infection source.
4. Diuretics, if necessary. Assess need for fluid intake to support O
2
delivery.
5. Evaluate intake and output daily; weigh patient daily.
6. Use low tidal volume, ≤6 ml/kg to keep plateau pressure
<30 cm H
2
O.
7. Follow renal function, electrolytes, liver function, mental status to
assess organ system function.
Asthma
1. Airway inflammation is the primary cause of status asthmaticus.
2. Auto-PEEP or hyperinflation dominates gas exchange when using
mechanical ventilation.
3. Potentially increased complication rate of mechanical ventilation.
1 High-dose corticosteroids are primary treatment.
2. Aggressive inhaled aerosolized β
2
agonists (hourly, if needed).
3. Early intubation if necessary.
4. Adequate oxygen to inhibit respiratory drive.
5. Use low tidal volume, high inspiratory flow, low respiratory frequency
with mechanical ventilation to avoid barotrauma and auto-PEEP.
6. May need to sedate or paralyze to reduce hyperinflation.
7. Measure peak flow or FEV, as a guide to therapeutic response.
Diabetic Ketoacidosis
1. Evaluate degree of volume depletion and relationship of water to
solute balance (hyperosmolar component).
2. Avoid excessive volume replacement.
3. Look for a trigger for diabetic ketoacidosis (infection, poor compliance,
mucormycosis, other).
4. Avoid hypoglycemia during correction phase.
5. Identify features of hyperosmolar complications.
6. Calculate water and volume deficits.
7. Evaluate presence of coexisting acid-base disturbances (lactic acidosis,
metabolic alkalosis).
8. Avoid hypokalemia and hypophosphatemia during correction phase.
1. Give adequate insulin to lower glucose at appropriate rate (increase
aggressively if no response). Use continuous insulin infusion.
2. Give adequate volume replacement (normal saline) and water replace-
ment, if needed (half normal saline, glucose in water).
3. Follow glucose and electrolytes frequently.
4. Consider stopping insulin infusion when glucose is about 250 mg/dL
and HCO
3
–
is >18 meq/L.
5. Avoid hypoglycemia; if you continue insulin drip with glucose <250mg/dL,
then give D
5
W. If glucose continues to fall, lower insulin drip rate.
6. Monitor serum potassium, phosphorus.
7. Calculate water deficit, if any.
8. Urine osmolality, glucose, etc.
9. Check sinuses, nose, mouth, soft tissue, urine, chest x-ray, abdomen for
infection.
(
continued
)
Table 1–3. Things to think about and reminders for ICU patient care. (continued)
CHAPTER 1
6
Table 1–3. Things to think about and reminders for ICU patient care. (continued)
(
continued
)
Things To Think About Reminders
Hyponatremia
1. Consider volume depletion (nonosmolar stimulus for ADH secretion).
2. Consider edematous state with hyponatremia (cirrhosis, nephrotic
syndrome, congestive heart failure).
3. SIADH with nonsuppressed ADH.
4. Drugs (thiazide diuretics).
5. Adrenal insuffieiency, hypothyroidism.
1. Measure urine Na
+
, Cl
–
, creatinine, and osmolality.
2. Calculate or measure serum osmolality.
3. Volume depletion? Give volume challenge?
4. Ask if patient is thirsty (may be volume-depleted).
5. Review medication list.
6. Primary treatment may be water restriction.
7. Consider need for hypertonic saline (carefully calculate amount)
and furosemide.
8. Other treatment (demeclocycline).
Hypernatremia
1. Diabetes insipidus (CNS or renal disease, lithium?)
2. Diabetes mellitus.
3. Has patient been water-depleted for a long-time?
4. Concomitant volume depletion?
5. Is the urine continuing to be poorly concentrated?
1. Calculate water deficit and ongoing water loss.
2. Replace with hypotonic fluids (0.45% NaCl, D
5
W) at calculated rate.
3. Replace volume deficit, if any, with normal saline.
4. Measure urine osmolality, Na
+
, Cl
–
, creatinine.
5. Does patient need desmopressin acetate (central diabetes insipidus)?
Hypotension
1. Volume depletion.
2. Sepsis. (Consider potential sources; may need to treat empirically.)
3. Cardiogenic. (Any reason to suspect?)
4. Drugs or medications (prescribed or not).
5. Adrenal insufficiency.
6. Pneumothorax, pericardial effusion or tamponade, fungal sepsis,
tricyclic overdose, amyloidosis.
1. Volume challenge; decide how and what to give and how to monitor.
2. If volume-depleted, correct cause.
3. Gram-positive or gram-negative sepsis (or candidemia) may also cause
hypotension and shock.
4. Give naloxone if clinically indicated.
5. Echocardiogram (left ventricular and right ventricular function, pericardial
disease, acute valvular disease) may be helpful.
6. Does the patient need a Swan-Ganz catheter?
7. Cosyntropin stimulation test or empiric corticosteroids.
Swan-Ganz Catheters
1. Site of placement (safety, risk, experience of operator).
2. Coagulation times, platelet count, bleeding time, other
bleeding risks.
3. Document in medical record.
4. Estimate need for monitoring therapy.
5. Predict whether interpretation of data may be difficult (mechanical
ventilation, valvular insufficiency, pulmonary hypertension).
1. Check for contraindications.
2. Write a procedure note.
3. Make measurements and document immediately after placement.
4. Obtain chest x-ray afterward.
5. Level transducer with patient before making measurement; eliminate
bubbles in lines or transducer.
6. Discontinue as soon as possible.
7. Use Fick calculated cardiac output to confirm thermodilution
measurements.
8. Send mixed venous blood for O
2
saturation.
Upper Gastrointestinal Bleeding
1. Rapid stabilization of patient (hemoglobin and hemodynamics).
2. Identification of bleeding site.
3. Does patient have a nonupper GI bleeding site?
4. Consider need for early operation.
5. Review for bleeding, coagulation problems.
6. Determine when “excessive” amounts of blood products given.
7. Do antacids, H
2
blockers, PPIs play a role?
8. Reversible causes or contributing causes.
1. Monitor vital signs at frequent intervals.
2. Monitor hematocrit at frequent intervals.
3. Choose hematocrit to maintain.
4. Consider need and timing of endoscopy.
5. Consult surgery.
6. Patients with abnormally long coagulation time may benefit from fresh-
frozen plasma (calculate volume of replacement needed).
7. Platelet transfusions needed?
8. Desmopressin acetate (renal failure).
