Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

GASTROINTESTINAL BLEEDING
707
decrease in incidence is probably due to wide use of stress-
ulceration prophylaxis in ICU patients.
B. Portal Hypertension—Varices are a hallmark of portal
hypertension, most commonly caused by liver cirrhosis. The
lifelong risk of variceal bleeding is about 50% in cirrhotic
patients. For patients with variceal bleeding, prognosis is
poor. Without treatment, the risk of rebleeding is 70%. Each
episode of variceal bleeding carries 30% mortality rate.
The size, location, and endoscopic appearance of varices
and the Child-Pugh score are the most important independent
predictors of variceal bleeding. Varices that are larger than 6
mm or that occupy more than a third of the lumen portend
the highest risk of bleeding. Esophageal varices are responsible
for most cases of variceal bleedings, whereas gastric varices
account for fewer than 30%. Usually, gastric varices are found
in combination with esophageal varices, but isolated gastric
varices should prompt evaluation for splenic vein thrombosis.
If isolated splenic vein thrombosis is present, splenectomy is
the therapy of choice. Gastric varices, and in particular, iso-
lated fundic varices, tend to produce severe and difficult-to-
control bleeding. Endoscopic appearance of varices is also a
bleeding risk predictor. Red streaks or “cherry” or cystic spots
(“blood blisters”) are high bleeding risk endoscopic stigmata.
Development of varices parallels the progression of liver
disease. Thus patients with higher Child-Pugh scores are more
likely to have varices and are at higher risk for variceal bleed-
ing. As an example of these factors put together, a Child’s C
cirrhotic patient with large varices and endoscopic red streaks
has a 76% yearly risk of variceal bleeding, whereas the risk
drops to 10% for a Child’s A patient without other risk factors.
UGI Bleeding Diagnosis and Treatment
Over the past decade, significant advances have been made in
the diagnosis and treatment of UGI bleeding. Endoscopy has
evolved from a merely diagnostic technique into a com-
monly used therapeutic modality. Endoscopic therapy
decreases mortality and the need for surgery and reduces
rebleeding rates, length of hospital stay, and transfusion
requirements. Endoscopy also plays an important role in
patient risk stratification, allowing for significant cost savings.
The armamentarium of available diagnostic techniques has
further expanded with the invention of capsule endoscopy. A
small camera/capsule is swallowed by the patient and trans-
mits 360-degree pictures throughout the UGI tract. In par-
ticular, capsule endoscopy significantly improves localization
of small bowel bleeding lesions. Another new endoscopic
technique is double-balloon enteroscopy, which allows for
endoscopic examination of the entire small bowel. It is still
under development and has limited availability.
A combination of endoscopic and pharmacologic therapies
is successful in great majority of UGI bleeding patients.
Currently, 95% of UGI bleeding patients respond to combined
endoscopic and pharmacologic therapy. Therefore, surgery and
interventional radiology techniques are reserved for patients
who fail endoscopic management. Below we focus on endo-
scopic and pharmacologic approaches to the two main types of
UGI bleeding: peptic ulcer and variceal bleeding.
Peptic Ulcer Disease
A. Endoscopic Diagnosis and Treatment of Peptic Ulcer
Bleeding—Endoscopic findings determine the need for endo-
scopic therapy and guide further decisions on hospitalization
and the extent of follow up (Table 33–4). Active bleeding, a vis-
ible vessel, and adherent clot are considered high-risk endo-
scopic signs. Endoscopic therapy is recommended for such
patients, and they need to be monitored closely for signs of
rebleeding. Indeed, without endoscopic therapy, an ulcer
found to be actively bleeding during the endoscopy has a 90%
rebleeding rate after bleeding stops spontaneously. On the
other hand, no endoscopic therapy is indicated for clean base
ulcers (low-risk finding). Such patients can be discharged
safely after endoscopy with close outpatient follow-up.
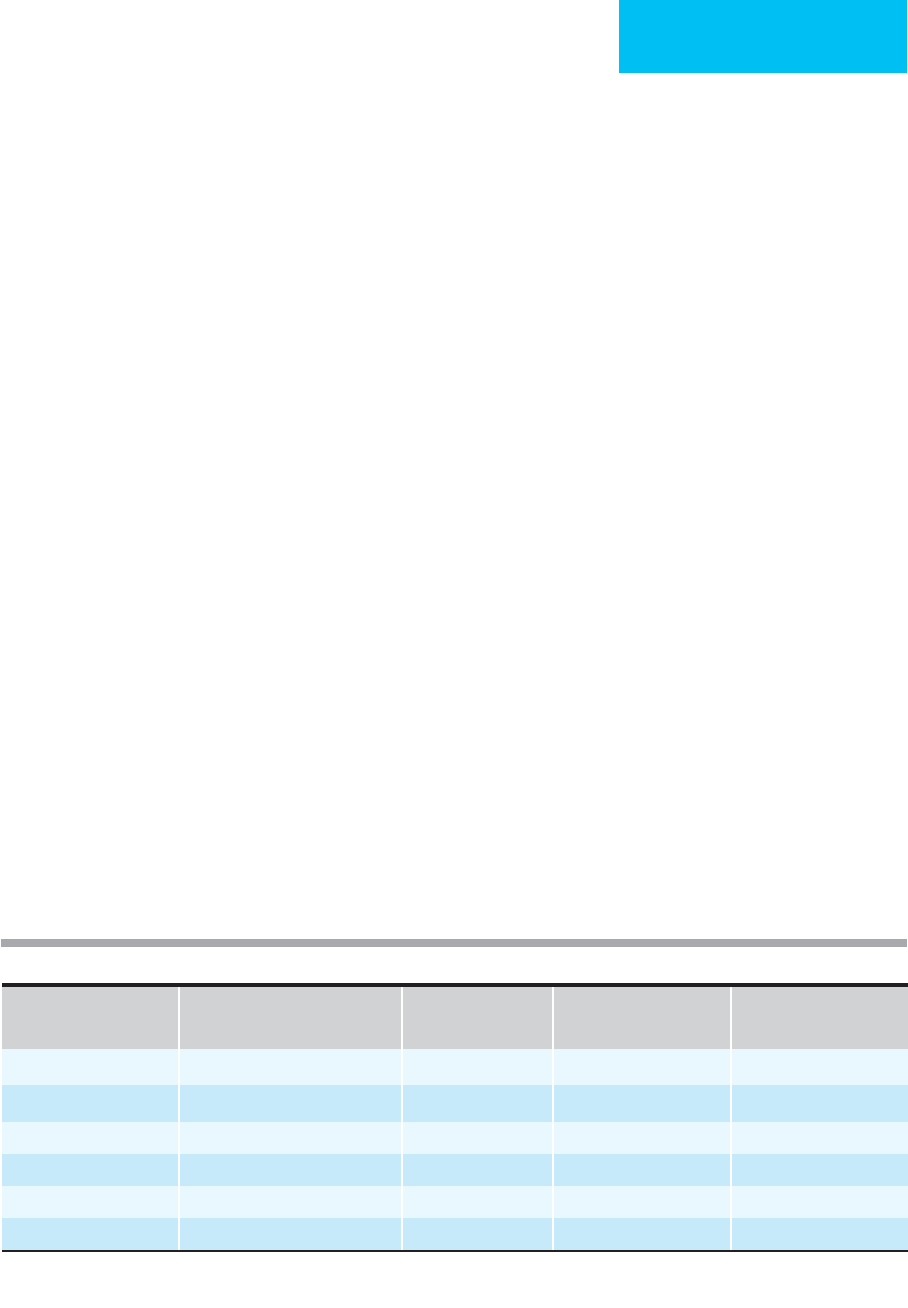
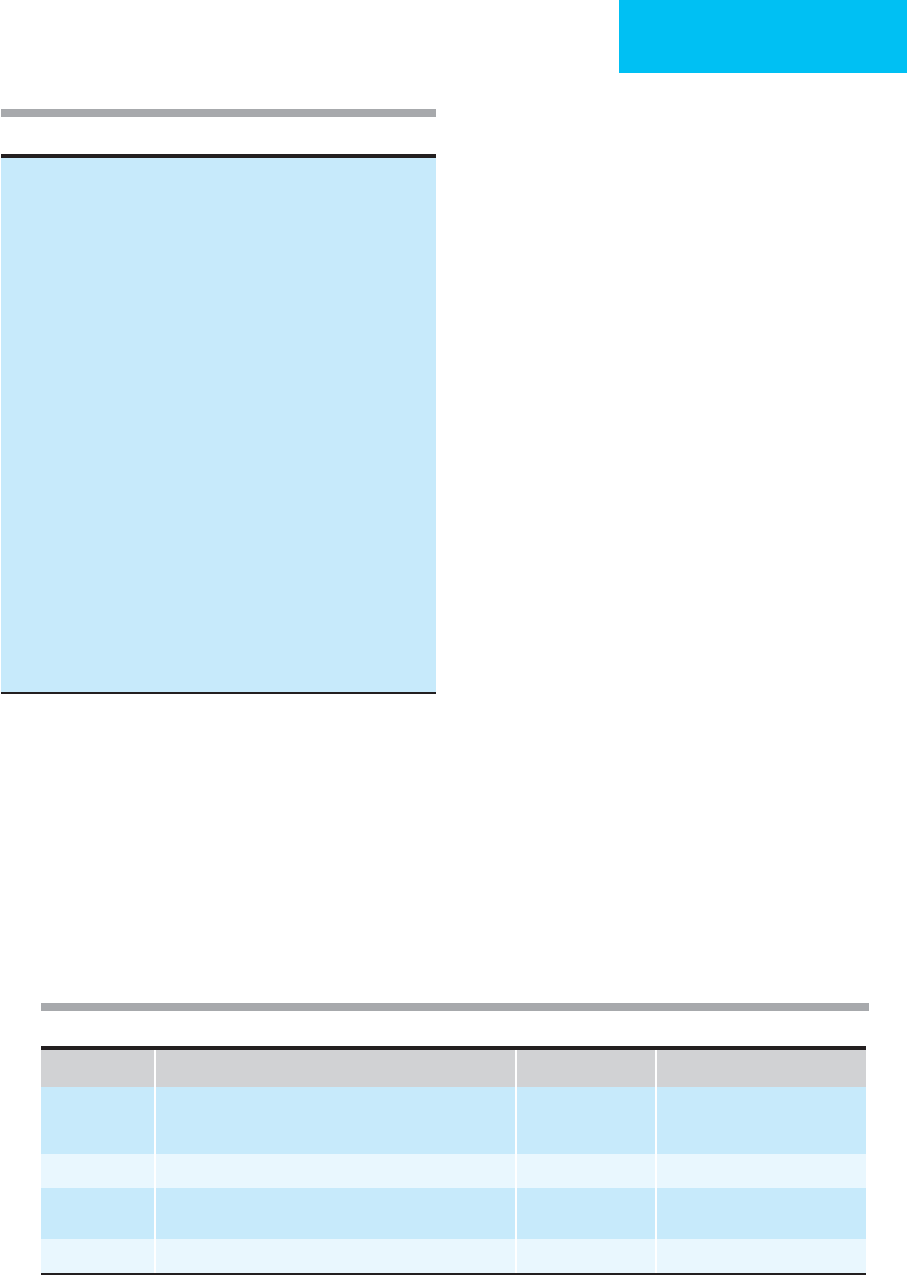
Endoscopic Stigmata Prevalence
Rebleeding Risk without
Endoscopic Therapy
Rebleeding Risk after
Endoscopic Therapy
High risk Active arterial bleeding 10% 90% 18%
Nonbleeding visible vessel 25% 40–50% 10–15%
Adherent clot 10–14% 25–35% 0–5%
Oozing without visible vessel 10% 10–20% <1%
Low risk Flat spot 10% 7% N/A
Clean-base ulcer 35% 3–5% N/A
Modified from Katschinski B et al: Dig Dis Sci 1994;39:706; and from Center for Ulcer Research and Education: Digestive Disease Research
Center, Hemostasis Research Group, UCLA School of Medicine and the West Los Angeles VA Medical Center.
Table 33–4. UGI bleeding: endoscopic stigmata and risk of rebleeding without and with endoscopic therapy.
CHAPTER 33
708
Modern endoscopic therapeutic techniques include injec-
tion of vasoconstrictive agents, thermal therapy, and use of
mechanical devices. Injection therapy employs a needle with
retractable tip, with epinephrine the most commonly used
agent. Injections are frequently combined with thermal ther-
apy. A bipolar coagulation or heater probe is physically com-
pressed against the bleeding vessel, and thermal energy then
seals the vessel wall. More recently, mechanical devices, in
particular endoscopic clips, are being used increasingly in
ulcer hemostasis. A number of studies have shown signifi-
cantly decreased rebleeding rates with the combination of
endoscopic clips and injection therapy compared with injec-
tion therapy alone. However, clips are difficult to place in a
scarred-down ulcer, and they also are more likely to fall off in
this situation. Overall, clip application is more operator- and
position-dependent than other modalities.
B. Pharmacologic Therapy for Peptic Ulcer Bleeding—
Pharmacologic therapy by acid suppression is the cornerstone
of peptic ulcer bleeding management. Indeed, clot lysis occurs
at pH less than 6, and platelet aggregation is enhanced at pH
greater than 6. Proton pump inhibitors (PPIs) are the main
acid suppressive agents. A high-dose PPI bolus followed by
continuous infusion is particularly efficacious after endo-
scopic therapy. A recent large double-blind, randomized trial
showed 6.7% versus 22.5% rebleeding rates in patients on con-
tinuous intravenous PPIs after endoscopic therapy compared
with placebo. PPIs also decreased rebleeding and surgery rates
compared with histamine-2 (H
2
) blockers. Data also support
the use of empirical high-dose PPI therapy prior to endoscopy.
H. pylori eradication is important in peptic ulcer bleeding
management, in particular for prevention of ulcer recur-
rence. H. pylori serology and antral biopsy are the preferred
tests in acute bleeding. H. pylori eradication should be con-
firmed after treatment with a urea breath test.
Intravenous octreotide has been studied in nonvariceal acute
UGI bleeding, but its effectiveness remains undetermined.
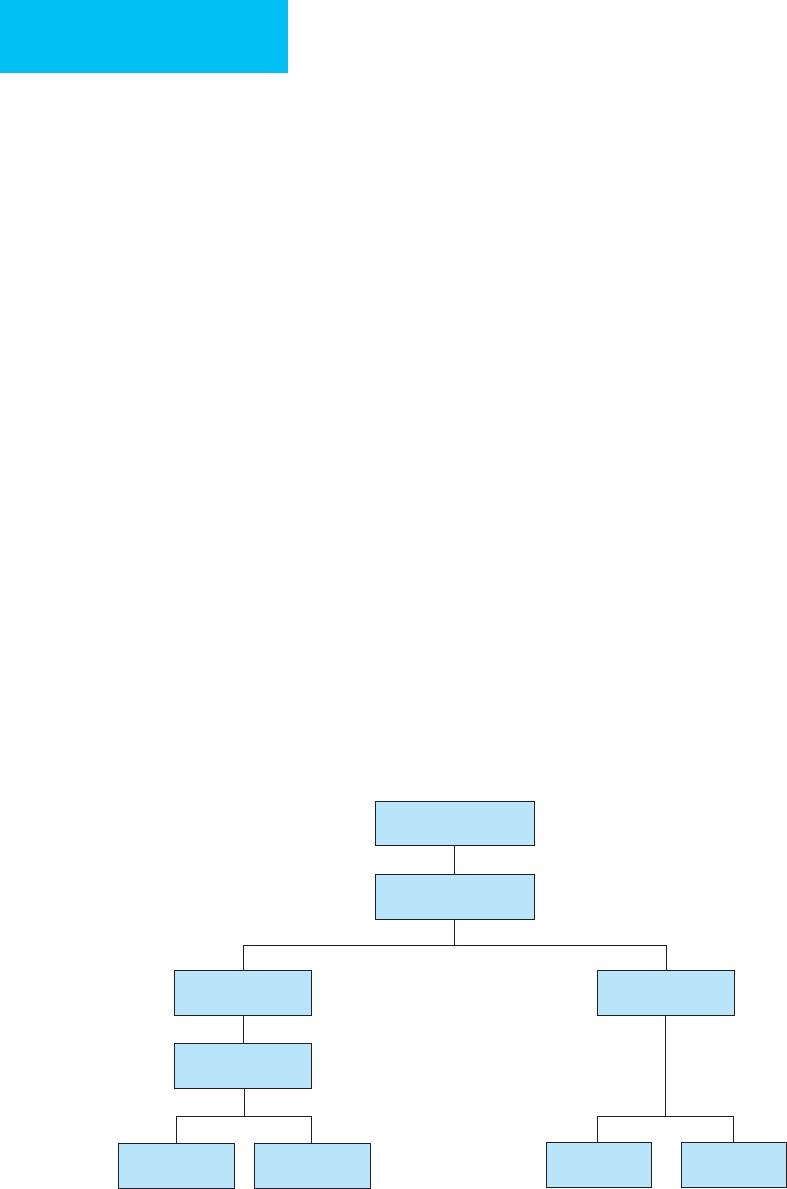
C. Recurrent Peptic Ulcer Bleeding and Endoscopic
Therapy Failures—Effective hemostasis is attained endo-
scopically in more than 95% of ulcers that are actively bleed-
ing or have high-risk endoscopic stigmata. However,
high-risk ulcers have a 15% risk of rebleeding, usually in the
first 72 hours after index bleed. Active spurting of blood and
large (>2 cm) ulcers were independent risk factors for endo-
scopic therapy failure in a recent prospective study.
Therefore, a “second look” endoscopy is usually indicated in
case of rebleeding, with a 73% rate of long-term hemostasis.
Failure of the second endoscopic therapy attempt should
initiate consideration for alternative treatments, in particular
surgery (Figure 33–2). According to a recent large registry of
UGI bleeding cases, 6.5% of patients with bleeding peptic
ulcers underwent surgery for continued bleeding or rebleed-
ing. With the effective medical therapies available, the goal of
surgery is no longer ulcer cure but control of hemorrhage in
these patients. The choice of surgical procedure includes
simple oversewing of the ulcer (with or without vessel liga-
tion), ulcer excision, or radical surgery (ie, depending on
ulcer location, vagotomy with antrectomy or gastrectomy).
In a recent review of surgical options, conservative therapy
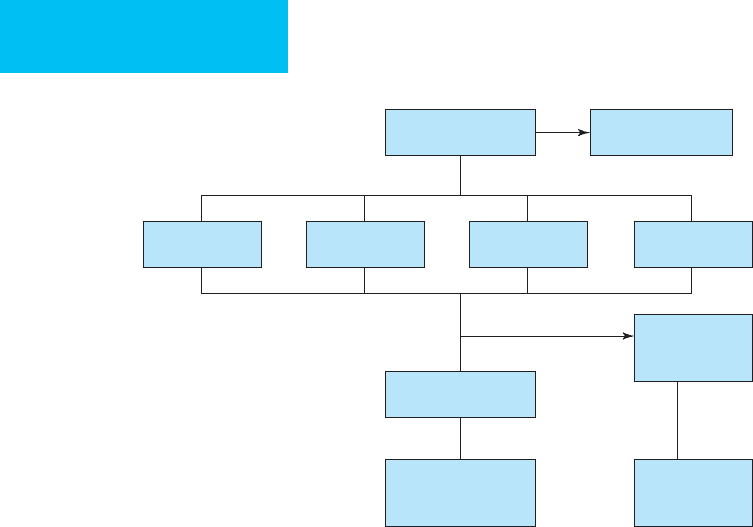
Continued bleeding
or early recurrence
Failed
repeat endoscopy
TIPS
1
Splenectomy
2
Shunt surgery
Surgery Angiography
Variceal bleeding
Nonvariceal
bleeding
Balloon
tamponade
1
Treatement of choice for gastric varices
2
Treatment of choice for isolated splenic vein thrombosis & gastric varices
Figure 33–2. Upper gastrointestinal bleeding: failures of endoscopic therapy.

GASTROINTESTINAL BLEEDING
709
with oversewing of the ulcer had rates of morbidity and mor-
tality comparable with those of more radical surgery.
However, rebleeding rate was somewhat higher. Current rec-
ommendations are for ulcer excision in patients with a bleed-
ing gastric ulcer, but gastric resection should be performed
for a large penetrating ulcer. Duodenal ulcers should be over-
sewn and vessel ligation performed.
Patients who are not surgical candidates can be considered
for a third endoscopic therapy attempt or for therapeutic
angiography. The latter showed a 50–90% success rate in
management of large gastroduodenal ulcers. Intraarterial
vasopressin infusion and embolization with microcoils, gela-
tin, or polyvinyl alcohol particles are the main angiographic
techniques in ulcer hemostasis. With selective catheterization,
complications of embolization such as bowel ischemia, perfo-
ration, abscess formation, and hepatic infarction are rare.
Variceal Bleeding
A. Endoscopic Diagnosis and Treatment of Variceal
Bleeding—Endoscopy is critical in all aspects of variceal
bleeding management: to identify the patients at risk, to pre-
vent a first bleed, to treat active bleeding, and to decrease the
risk of rebleeding. Both esophageal and gastric (near the car-
dia) varices can be treated endoscopically, with overall suc-
cess rates of about 90% (see Figure 33-1). However, gastric
varices often require additional treatment modalities to pre-
vent rebleeding.
Two endoscopic techniques are applied most often for
variceal bleeding hemostasis: sclerotherapy, which has been
in use for 60 years, and more recently, band ligation. In scle-
rotherapy, a sclerosant (routinely 5% ethanolamine) is
injected via a retractable-tip needle into the varix and/or sur-
rounding tissues, leading to coagulation necrosis and variceal
thrombosis. Repeated sclerotherapy can be performed until
there is complete eradication of esophageal varices. However,
sclerotherapy has been associated with 2–5% mortality and
up to a 20% major complication rate. Major complications
include deep ulcerations, stricture formation, esophageal
perforation, and mediastinitis. Transient bacteremia is com-
mon during sclerotherapy, and antibiotics should be given to
at-risk patients prior to sclerotherapy.
In recent years, band ligation has replaced sclerotherapy
as the primary endoscopic treatment of variceal bleeding,
and it is equally efficacious but much safer. In this procedure,
a rubber band is placed on the varix via a device attached to
the endoscope. The band effectively strangulates the varix,
resulting in varix thrombosis. Multiple bands can be
deployed in one setting. The effect of the band is local, and
systemic complications are rare. In several studies, band lig-
ation was compared with sclerotherapy for the prevention of
esophageal varices recurrence. Rebleeding rate and number
of sessions needed for variceal obliteration were significantly
lower with band ligation (6% and four sessions compared
with 21% and five sessions for sclerotherapy). On the other
hand, recurrence of varices at 1 year was less with sclerotherapy
(8% versus 29% for band ligation). Some experts recom-
mend combining band ligation and sclerotherapy at the final
therapy session to improve long-term eradication of varices.
B. Pharmacologic Therapy of Variceal Bleeding—
Pharmacologic therapy is a necessary component of variceal
bleeding management. Octreotide, a long-acting analogue of
somatostatin, is used most commonly owing to its safety and
ease of administration. Octreotide is thought to work, at least
in part, by decreasing splanchnic blood flow. Octreotide typ-
ically is given as a bolus followed by continuous infusion.
Optimal duration of therapy is not well defined, but 3–5 days
of administration after the bleeding episode is typically rec-
ommended. Octreotide, used in combination with endo-
scopic therapy, has been shown to significantly improve
short-term hemostasis rate (66% versus 55% for band liga-
tion alone).
Prophylactic use of antibiotics in cirrhotic patients with
UGI bleeding is another important aspect of variceal bleed-
ing management. Indeed, bacterial infections are found in up
to 20% of cirrhotic patients with UGI bleeding. Antibiotic
prophylaxis not only reduces infectious complications but
also has shown a trend toward improved mortality. The
choice of antibiotic and duration of therapy are not well
established. An oral quinolone is used commonly for 7–10
days after the bleeding episode.
Several uncontrolled studies suggest that acid suppres-
sion (ie, with a PPI) might be another useful addition to
endoscopic therapy, in particular in healing of postscle-
rotherapy or post–band ligation ulcers. Nonselective β-
blockers and nitrates have a limited role in acute variceal
bleeding setting and should be reserved for outpatient
rebleeding prevention.
C. Recurrent Variceal Bleeding and Endoscopic Therapy
Failures—In 10–20% of patients, combined endoscopic and
pharmacologic therapy fails to achieve long-term hemosta-
sis. The highest risk for rebleeding is in the first 48 hours, as
well as up to 6 weeks after the index bleed. Generally, repeat
endoscopy is recommended in early hemostasis failure.
Alternative endoscopic therapeutic modality should be
applied in these cases, such as sclerotherapy if initial band
ligation was unsuccessful.
Surgery and transjugular intrahepatic portosystemic
shunting (TIPS) are the two main treatment options for patients
who have failed endoscopic therapy (see Figure 33-2).
Balloon tamponade usually is attempted to address acute
severe bleeding until one of these options is chosen. The
Sengstaken-Blakemore tube, with both esophageal and gastric
balloons, is used most commonly for tamponade. Short-term
hemostasis rates vary from 30–90%, and rebleeding usually
occurs after balloon deflation. Balloon tamponade is associ-
ated with a number of significant complications, in particular
esophageal rupture and aspiration. To prevent these compli-
cations, the esophageal balloon should not be inflated for
more than 24 hours, and tamponade should be performed
only in patients with an endotracheal tube in place.
CHAPTER 33
710
Surgery is effective in variceal bleeding. Unfortunately,
most variceal bleeding patients present with decompensated
cirrhosis, making them poor surgical candidates. Nowadays,
both nonselective (ie, portocaval) and selective (ie, splenore-
nal) shunts are used for variceal bleeding control.
Nonshunting operations, such as gastroesophageal devascu-
larization (Sugiura procedure), are performed rarely.
Perioperative morbidity and mortality are quite high for
emergent shunt operations, and management is further com-
plicated by a 40–50% incidence of encephalopathy. Surgical
shunting also significantly alters vascular anatomy, making
future liver transplantation more challenging.
In recent years, TIPS has emerged as a safer and easier-
to-perform alternative to surgical shunting. TIPS is done
by an interventional radiologist and requires only local
anesthesia or light sedation. The stent is passed via the
transjugular route and connects the hepatic vein with an
intrahepatic portion of the portal vein, thus creating a por-
tosystemic shunt. TIPS is effective in more than 90% of
variceal bleeds. It is the treatment of choice for gastric
variceal bleeding because endoscopic therapy usually does
not prevent rebleeding of gastric varices. As with surgical
shunts, post-TIPS encephalopathy is common (~30% inci-
dence). Another limitation of TIPS is frequent stent
restenosis or thrombosis leading to multiple revisions and
restenting.
Baradarian R et al: Early intensive resuscitation of patients with
upper gastrointestinal bleeding decreases mortality. Am J
Gastroenterol 2004;99:619–22. [PMID: 15089891]
Barkun A et al: Consensus recommendations for managing
patients with nonvariceal upper gastrointestinal bleeding. Ann
Intern Med 2003;139:843–57. [PMID: 14623622]
Barkun A et al: The Canadian registry on nonvariceal upper gas-
trointestinal bleeding and endoscopy (RUGBE): Endoscopic
hemostasis and proton pump inhibition are associated with
improved outcomes in real-life setting. Am J Gastroenterol
2004;99:1238–46. [PMID: 15233660]
Chung IK et al: Endoscopic factors predisposing to rebleeding fol-
lowing endoscopic hemostasis in bleeding peptic ulcers.
Endoscopy 2001;33:969–75. [PMID: 11668406]
El-Serag HB, Everhart JE: Improved survival after variceal hemor-
rhage over an 11-year period in the Department of Veterans
Affairs. Am J Gastroenterol 2000;95:3566–73. [PMID: 11151893]
Imperiale TF et al: Predicting poor outcome from acute upper gas-
trointestinal hemorrhage. Arch Intern Med 2007;167:1291–6.
[PMID: 17592103]
Jensen DM et al: Randomized trial of medical or endoscopic ther-
apy to prevent recurrent ulcer hemorrhage in patients with
adherent clots. Gastroenterology 2002;123:407–13. [PMID:
12145792]
Kahi CJ et al: Endoscopic therapy versus medical therapy for
bleeding peptic ulcer with adherent clot: A meta-analysis.
Gastroenterology 2005;129:855–62. [PMID: 16143125]
Lau JY et al: Omeprazole before endoscopy in patients with gas-
trointestinal bleeding. N Engl J Med 2007;356:1631–40. [PMID:
17442905]
Ohmann C, Imhof M, Roher HD: Trends in peptic ulcer bleeding
and surgical treatment. World J Surg 2000;24:284–93. [PMID:
10658062]
Orozco H, Mercado MA: The evolution of portal hypertension
surgery: Lessons from 1000 operations and 50 Years’ experience.
Arch Surg 2000;135:1389–93. [PMID: 11115336]
Qureshi W et al: ASGE guideline: The role of endoscopy in the
management of variceal hemorrhage, updated July 2005.
Gastrointest Endosc 2005;62:651–5. [PMID: 16246673]
Soares-Weiser K et al: Antibiotic prophylaxis of bacterial infections
in cirrhotic inpatients: A meta-analysis of randomized, con-
trolled trials. Scand J Gastroenterol 2003;38:193–200. [PMID:
12678337]
Stabile BE, Stamos MJ: Surgical management of gastrointestinal
bleeding. Gastroenterol Clin North Am 2000;29:189–222.
[PMID: 10752022]
Lower Gastrointestinal Bleeding
ESSENTIALS OF DIAGNOSIS
Hematochezia (bright red or maroon stools).
Initial evaluation is similar for lower and upper GI
bleeding patients.
Patients younger than 50 years of age with self-limited
mild lower intestinal bleeding (most likely owing to
internal hemorrhoids) can be further evaluated with
colonoscopy or flexible sigmoidoscopy as outpatients.
Urgent colonoscopy is indicated in the presence of
unstable vital signs, continued bleeding, or more than
two comorbid conditions.
Life-threatening lower intestinal bleeding require con-
sideration of emergent angiography or surgery without
delaying for bowel preparation/colonoscopy.
General Considerations
Lower intestinal bleeding is characterized by a lesion location
distal to ligament of Treitz. Most often the source of bleeding
is colonic. Hematochezia (ie, bright red or maroon colored
stools) is the classic clinical presentation. Although severe
lower intestinal bleeding is less common than UGI bleeding,
it is a frequent GI emergency. On average, a full-time gas-
troenterologist sees more than 10 severe lower intestinal
bleeding cases per year.
Initial Approach, Resuscitation, and Risk
Stratification
The main principles of initial evaluation and resuscitation of
UGI bleeding apply equally to lower intestinal bleeding. The
goals are the same: to assess bleeding severity based on the
degree of hemodynamic compromise, to evaluate comorbid
illnesses, and to optimize the patient’s condition prior to
treatment. Syncope or postural hypotension is indicative of
GASTROINTESTINAL BLEEDING
711
potentially massive bleeding. In such cases, NG aspiration
should be performed to exclude an upper bleeding source. In
hematochezia without hemodynamic compromise, severe
UGI bleeding is unlikely, and NG tube placement might not
be necessary. After assessing bleeding severity, attention
should be paid to exacerbation of comorbid illnesses. In par-
ticular, evaluation for cardiac ischemia is important because
lower intestinal bleeding is frequent in elderly patients.
Resuscitation of lower and upper GI bleeding patients
involves similar approaches. As described earlier for UGI
bleeding, resuscitation aims to quickly restore intravascular
volume with crystalloids, colloids, and blood and to correct
hemostatic abnormalities, if present. Patients with severe
bleeding should be admitted to an ICU, and surgical consulta-
tion should be obtained early in the course of hospitalization.
In most patients, lower intestinal bleeding stops sponta-
neously. Thus it is crucial to identify patients who are at high
risk for continued bleeding. Commonly reported clinical
predictors are hypotension and tachycardia, continued rectal
bleeding during the first 4 hours of hospitalization, absence
of abdominal pain, use of aspirin, and presence of at least
two comorbid conditions. Prospective validation of this risk
stratification scheme showed 0% rebleeding in a low-risk
group compared with 77% in a high-risk group.
Causes of Lower Intestinal Bleeding
Diverticulosis, colitis (ie, ischemic, infectious, or postradia-
tion), cancer, and angiodysplasia are the main causes of
severe lower intestinal bleeding (Table 33–5). Hemorrhoids
are a frequent cause of rectal bleeding, especially in patients
younger than 50 years. However, hemorrhoidal bleeding is
rarely severe.
Diverticulosis is responsible for more than 30% of lower
intestinal bleeding. Colonic diverticula are mucosal and sub-
mucosal herniations through the muscle layer, thought to
develop owing to increased intraluminal pressure or
decreased colonic wall muscle tone. They are found in half the
adult population in the Western hemisphere, and the inci-
dence increases with age. Bleeding occurs in only 5–15% of
patients with diverticular disease. However, lower GI bleeding
can be massive in a third of those patients. Painless hema-
tochezia is the classic clinical presentation of diverticular
bleeding. In 75%, diverticular bleeding stops spontaneously,
but the risk of rebleeding is 25–38% in the following 4 years.
Colitis (inflammation of the colon) is another common
cause of severe lower intestinal bleeding. Of note, mortality
rates as high as 20–50% have been reported in hospitalized
patients with ischemic colitis bleeding. Hematochezia in
ischemic colitis is typically accompanied by mild abdominal
pain, differentiating it from painless diverticular bleeding.
The mechanism of mucosal ischemia is thought to be hypo-
perfusion of small intramural vessels rather than large vessel
occlusion. Ischemic colitis can occur throughout the colon,
but watershed areas such as at the splenic flexure or rectosig-
moid junction are affected most frequently. Ischemic colitis
sometimes occurs after extensive surgical procedures or as a
result of systemic hypotension.
Infectious and inflammatory colitis rarely cause severe
lower intestinal bleeding. However, infectious colitis, in par-
ticular secondary to Clostridium difficile, can mimic ischemic
colitis and should be excluded as part of the workup for
hematochezia and colitis.
Angiodysplasias (arteriovenous malformations) account
for about 8% of severe lower intestinal bleeding, but its inci-
dence has been decreasing in recent years. Angiodysplasia is
associated with renal failure and hereditary hemorrhagic
telangiectasia syndrome (Osler-Weber-Rendu syndrome).
An association with aortic stenosis is less clear.
Colon cancer typically presents with occult blood loss
rather than overt hematochezia. Severe lower intestinal
bleeding usually is caused by cancer ulceration, signifying an
advanced stage.
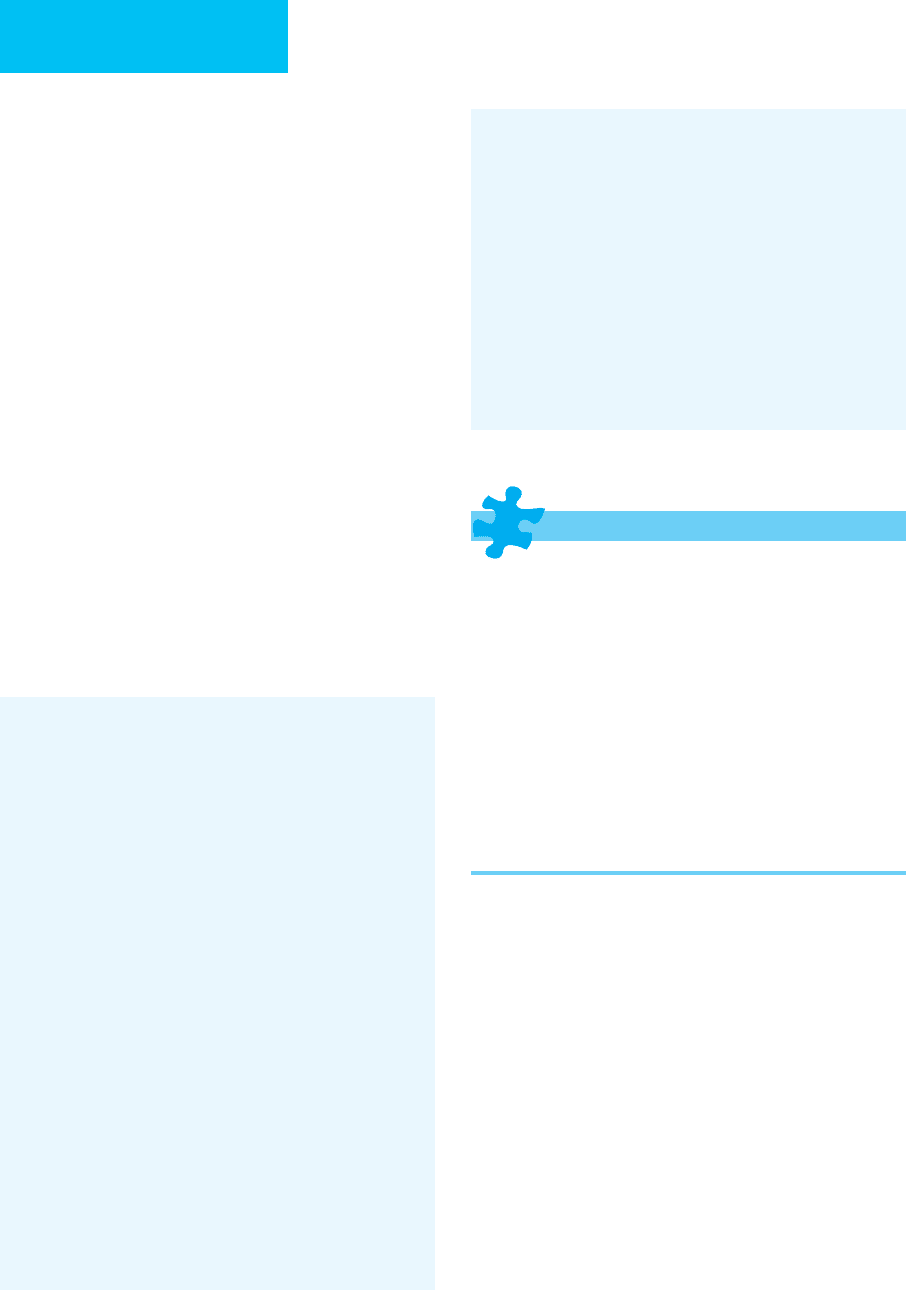
Diagnosis of Lower Intestinal Bleeding
Colonoscopy is typically the first step in evaluation of
lower intestinal bleeding (Figure 33–3). Its main advantage
is that both diagnosis and treatment can be accomplished
in one procedure. However, downsides are the requirement
for bowel preparation and the small, albeit identifiable,
risk of sedation. Notably, management of severe life-
threatening lower intestinal bleeding (ie, angiography or
surgery) should not be delayed for bowel preparation/
colonoscopy. Some gastroenterologists perform colonoscopy
on unprepared bowel because blood is cathartic.
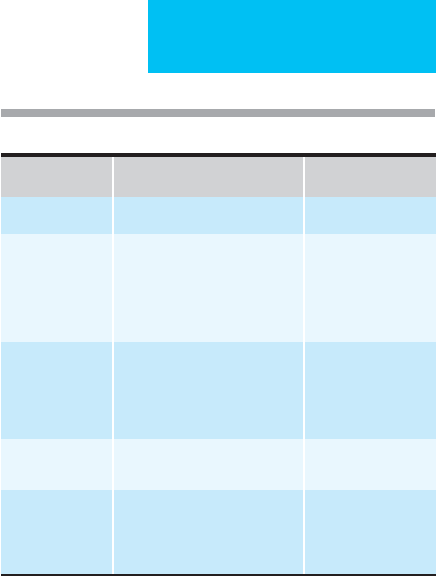
Table 33–5. Severe lower gastrointestinal bleeding: causes.
Relative Frequency
Anatomic Diverticulosis 33%
Vascular
malformations
Arteriovenous malformations
Idiopathic angiomas
Osler-Weber-Rendu syndrome
Radiation-induced
telangiectasia
Angiodysplasia, 8%
Inflammatory Ischemic colitis
Infectious colitis
Inflammatory bowel disease
Radiation colitis
18%
Neoplasm Polyps
Carcinoma
19%
Other Hemorrhoids
Ulcer
Postbiopsy, postpolypectomy
18%
CHAPTER 33
712
Occasionally, flexible sigmoidoscopy on unprepared bowel
is sufficient, in particular as a quick check for ischemic or
infectious colitis. In most cases, we recommend urgent
bowel purge with polyethylene glycol (4–6 L) over 3–5
hours via NG tube or orally. Metoclopramide can be used
in conjunction with the purge to improve gastric emptying
and decrease nausea. Sodium phosphate preparations
should not be used in the acute setting because of high
phosphate and sodium loads. Radiographic studies should
be obtained prior to the bowel preparation to rule out per-
foration or intestinal obstruction.
The overall diagnostic yield of colonoscopy in lower intes-
tinal bleeding is between 48% and 90% (mean 68%). There
are conflicting data on the optimal timing for colonoscopy.
One recent report suggests that diagnostic yield improves with
urgent colonoscopy. We usually perform colonoscopy for
severe lower intestinal bleeding within 6–12 hours of hospital-
ization, after resuscitation and bowel preparation.
Treatment of Lower Intestinal Bleeding
Although surgery is the most common treatment modality
for lower intestinal bleeding, endoscopic therapeutic options
have been expanding in recent years. In particular, bipolar
coagulation is used successfully for angiodysplasia bleeding.
In diverticular hemorrhage, a visible bleeding vessel or clot
(high-risk stigmata) can be treated with sclerotherapy and
bipolar coagulation similar to peptic ulcer bleeding. Use of
endoscopic clips in diverticular bleeding is currently under
investigation. Significantly decreased short- and long-term
rebleeding rates have been reported for endoscopic therapy
of diverticular bleeding. However, urgent colonoscopy and
experience in advanced endoscopic techniques are needed to
achieve high hemostasis success rates.
Failure of Endoscopic Diagnosis and Treatment
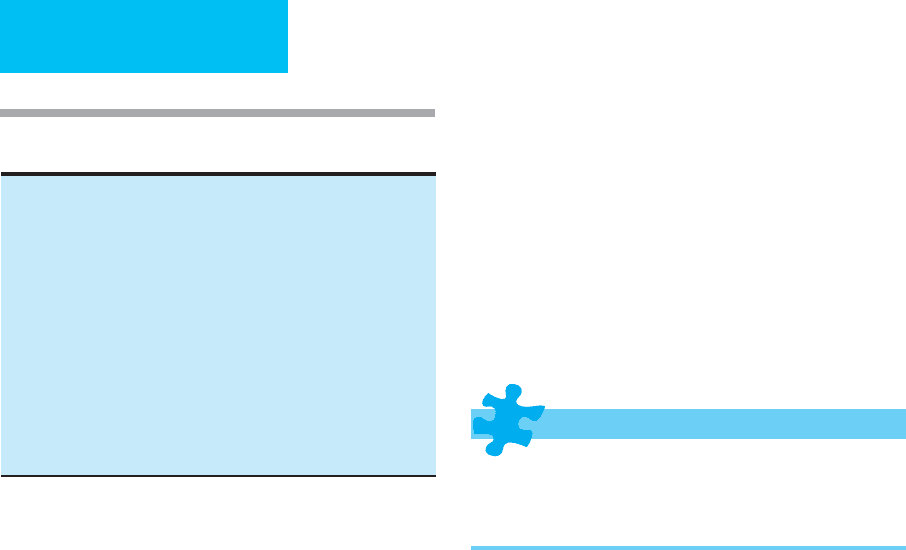
Radionuclide imaging typically is the next step in the local-
ization of a bleeding site after unsuccessful colonoscopy
(Figure 33–4). Radiolabeled red blood cells are injected
intravenously, and focal collections of radiolabeled material
are detected by scintigraphy. A 78% accuracy rate has been
reported, and bleeding as slow as 0.1–0.5 mL/min can be
identified. However, confirmatory colonoscopy is recom-
mended in the case of a positive radionuclide test owing to
rather high false-positive rates, typically a result of blood
from a UGI source collecting in the right colon.
Angiography is another diagnostic and therapeutic
modality used in case of colonoscopic failure. Angiography is
highly specific, but its sensitivity is significantly lower than
that of radionuclide imaging or colonoscopy. For angiogra-
phy to be positive, bleeding must be brisk, at a rate of more
than 1–1.5 mL/min. Since most lower GI bleeding stops
spontaneously, the timing of the angiography procedure is
particularly important. The overall diagnostic yield varies
widely from 12–69%. Some experts recommend radionu-
clide imaging prior to angiography to increase sensitivity.
However, this would further delay angiography and poten-
tially decrease its diagnostic yield.
After the bleeding site is identified angiographically, vaso-
pressin can be infused or a vessel can be selectively embolized
to stop the bleeding. Hemostasis rates of 91% have been
reported after intraarterial vasopressin in diverticular and
angiodysplasia bleeding. However, the rebleeding rate can be
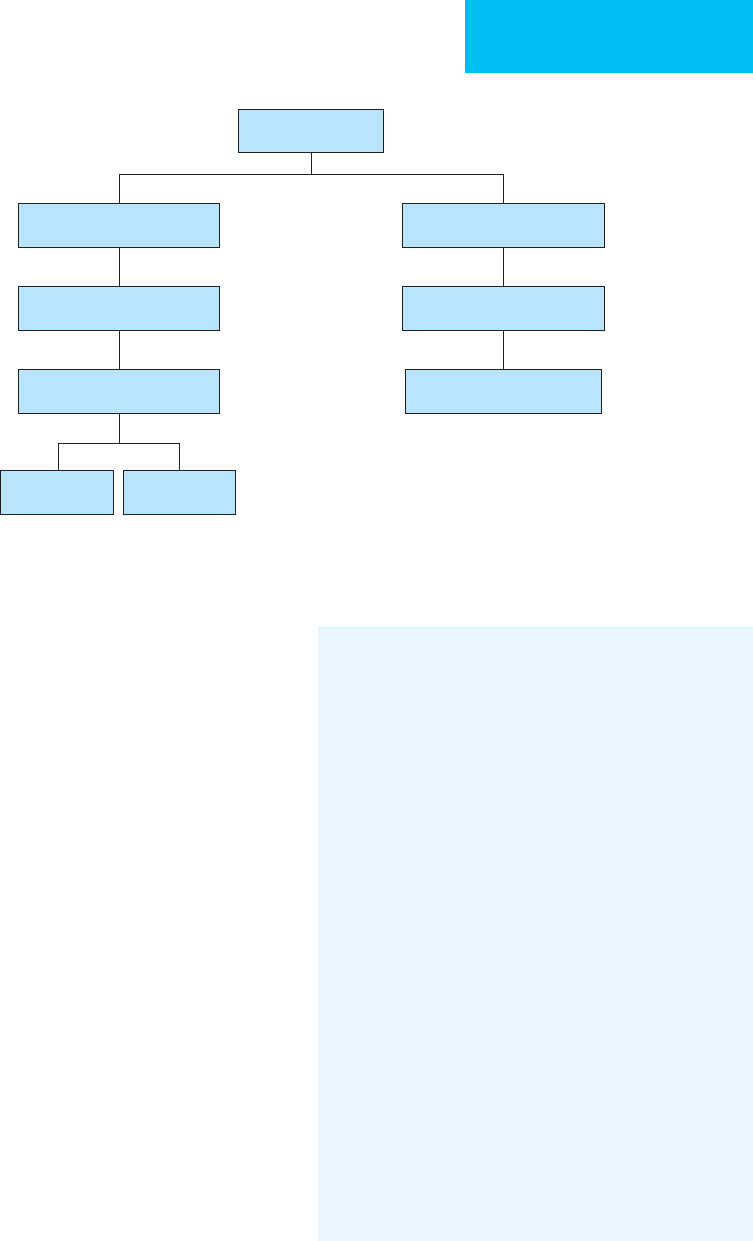
Hematochezia
NG lavage
R/O upper source
>2
comorbidities
Continued
bleeding
Syncope
low SBP
Older
age
Urgent
purge
Urgent
colonoscopy
(within 6–12 hours)
Urgent
angiography/
surgery
Life-
threatening
bleeding
Figure 33–3. Management of lower gastrointestinal bleeding.
GASTROINTESTINAL BLEEDING
713
as high as 50%. Angiography also has a fairly significant (up
to 9%) rate of major complications, including intestinal
ischemia, contrast-induced renal failure, femoral artery
thrombosis, and transient ischemic attack.
Surgical Treatment
Surgery is recommended for continued bleeding (~10% of
all patients presenting with lower intestinal bleeding; see
Figure 33-4). If bleeding has been localized preoperatively,
segmental resection is performed with or without a stoma.
Reported surgical mortality is about 10%, mostly because of
comorbid conditions.
In the case of bleeding that cannot be localized, enteroscopy
and, if available, capsule endoscopy should be performed as a
final attempt to identify the bleeding site. If the bleeding lesion
is still not identified, a thorough surgical exploration is per-
formed, with examination and palpation of the entire small
intestine. If there is a significant amount of blood in the small
intestine, intraoperative endoscopy can be performed.
Exploratory laparotomy leads to localization of the bleeding
site in 78% of patients without preoperative diagnosis.
In the absence of an identified source of bleeding, subto-
tal colectomy is undertaken with ileorectal anastomosis or
ileostomy with Hartmann’s pouch. Emergent subtotal colec-
tomy carries significant morbidity (37%) and mortality
(11%). However, segmental colectomy without a definitive
source of bleeding is associated with an unacceptably high
30% rebleeding rate.
Bloomfeld RS, Rockey DC, Shetzline MA: Endoscopic therapy of
acute diverticular hemorrhage. Am J Gastroenterol 2001;96:
2367–72. [PMID: 11513176]
Brandt LJ, Boley SJ: AGA technical review on intestinal ischemia.
American Gastrointestinal Association. Gastroenterology
2000;118:954–68. [PMID: 10784596]
Green BT et al: Urgent colonoscopy for evaluation and manage-
ment of acute lower gastrointestinal hemorrhage: A random-
ized, controlled trial. Am J Gastroenterol 2005;100:2395–402.
[PMID: 16279891]
Green BT, Rockey DC: Lower gastrointestinal bleeding:
Management. Gastroenterol Clin North Am 2005;34:665–78.
[PMID: 16303576]
Hammond KL et al: Implications of negative technetium
99m–labeled red blood cell scintigraphy in patients presenting
with lower gastrointestinal bleeding. Am J Surg 2007;193:404–7.
[PMID: 17320544]
Heil U, Jung M: The patient with recidivent obscure gastrointesti-
nal bleeding. Best Pract Res Clin Gastroenterol 2007;21:
393–407. [PMID: 17544107]
Jensen DM et al: Urgent colonoscopy for the diagnosis and treat-
ment of severe diverticular hemorrhage. N Engl J Med
2000;342:78–82. [PMID: 10631275]
Strate LL et al: Validation of a clinical prediction rule for severe
acute lower intestinal bleeding. Am J Gastroenterol 2005;100:
1821–7. [PMID: 16086720]
Strate LL, Syngal S: Predictors of utilization of early colonoscopy
vs radiography for severe lower intestinal bleeding. Gastrointest
Endosc 2005;61:46–52. [PMID: 15672055]
Strate LL: Lower GI bleeding: Epidemiology and diagnosis.
Gastroenterol Clin North Am 2005;34:643–64. [PMID:
16303575]
Failed endoscopic
diagnosis
Radionuclide imaging
identifies site
Failed endoscopic
therapy
Angiography
Segmental
colectomy
Subtotal
colectomy
1
Radionuclide imaging
fails to identify site
Confirmatory colonoscopy
endoscopic therapy
Enteroscopy
± capsule endoscopy
1
With intraoperative endoscopy
to exclude small bowel source
Figure 33–4. Lower gastrointestinal bleeding: failures of endoscopic diagnosis.

714
34
Hepatobiliary Disease
Hernan I. Vargas, MD
Liver disease is the ninth leading cause of death in the United
States, resulting in approximately 30,000 deaths each year.
Cirrhosis represents the final common pathway for a wide
variety of chronic liver diseases. Cirrhosis is defined as a dif-
fuse fibrotic process in the liver. Grossly abnormal nodules
replace the normally smooth hepatic parenchyma.
Patients with cirrhosis often develop complications from
their underlying liver disease such as upper GI bleeding,
renal insufficiency, ascites, or encephalopathy and require
critical care. In other circumstances, cirrhotic patients may
require critical care owing to unrelated problems such as
trauma, cancer, or major surgery. The physician caring for
patients in the ICU therefore should be knowledgeable about
disorders of liver function.
Acute Hepatic Failure
ESSENTIALS OF DIAGNOSIS
Acute onset.
Jaundice.
Encephalopathy.
General Considerations
Acute hepatic failure is a rapid-onset, severe impairment of
liver function. The natural history is that of progressive dete-
rioration with multiple-system organ failure. Prior to the
availability of liver transplantation, the mortality was as high
as 80%.
The interval between the development of jaundice and
the onset of encephalopathy has been used to classify hepatic
failure as hyperacute (0–7 days), acute (8–28 days), and sub-
acute (28 days–12 weeks).
Acute viral hepatitis (ie, hepatitis B [HVB], and hepatitis A
[HVA]) and acetaminophen toxicity are the most common
causes of acute hepatic failure in the United States. Other
causes are as listed in Table 34–1.
Clinical Features
A. Symptoms and Signs—The onset of symptoms is usu-
ally abrupt, characterized by malaise, fatigue, and loss of
appetite. Less frequently, patients complain of abdominal
pain and fever. The physical examination is significant for the
presence of jaundice, hepatomegaly, and right upper quad-
rant tenderness.
Signs of developing encephalopathy range from mild per-
sonality change to confusion and deep coma. The presence of
encephalopathy is a precondition for a diagnosis of acute
hepatic failure. The severity of encephalopathy is measured
in four stages (Table 34–2).
Patients with encephalopathy stage III or stage IV com-
monly suffer from cerebral edema and increased intracra-
nial pressure. Cerebral edema is a common finding in
patients who die from acute hepatic failure. The pathogene-
sis of cerebral edema has not been clearly elucidated.
However, investigators have proposed a breakdown of the
blood-brain barrier as an important mechanism. Sodium
accumulation in the brain cells secondary to inhibition of
Na
+
,K
+
-ATPase also has been proposed. Cerebral edema
causes an acute rise in the intracranial pressure that
decreases perfusion pressure and cerebral blood flow.
Autoregulation of cerebral blood flow is lost.
Oliguria and generalized edema occur commonly and
are associated with higher mortality. They are typically
caused by hypovolemia, acute tubular necrosis, or hepatore-
nal syndrome.
Late in the course, patients may develop upper GI bleed-
ing and blood loss from the airways, puncture sites, and soft
tissues.
The clinical course of acute hepatic failure is frequently
complicated by bacterial and fungal infections. Infectious
complications are a major contributor to increased morbid-
ity and are the immediate cause of death in nearly half of
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
HEPATOBILIARY DISEASE
715
fatal cases. The immune system is impaired by decreased
function of the reticuloendothelial system and complement
deficiency.
Coagulopathy may occur as a consequence of decreased
production of coagulation factors by the liver, as a conse-
quence of increased fibrinolysis, and from consumption, as in
disseminated intravascular coagulation. Thrombocytopenia
and platelet dysfunction are common.
Predictors of poor outcome are summarized in the King’s
College criteria (Table 34–3).
Treatment
Acute liver failure constitutes a medical emergency given the
high incidence of multisystem organ failure and the high
mortality. Patients with mild hepatic injury require mainte-
nance therapy with adequate hydration, euglycemia, and
electrolyte balance. Because the condition of patients with
more severe liver damage may deteriorate rapidly, respira-
tory support is often needed—particularly when cerebral
edema ensues.
A. Support Measures—
1. Encephalopathy and intracranial hypertension—
Cerebral herniation is a major cause of death if cerebral
edema and hypertension are untreated. Intracranial pressure
measurement is used for diagnosis of intracranial hyperten-
sion and monitoring of intracranial pressure dynamics. The
techniques for intracranial pressure monitoring are dis-
cussed in Chapter 31. Other monitoring techniques are
measurements of cerebral blood flow (with xenon) and cere-
bral oxygen consumption (by calculating the arterial-jugular
venous oxygen content difference).
The head of the bed is typically elevated 20–30 degrees to
reduce intracranial pressure, although the cerebral perfusion
pressure should be monitored to avoid an adverse impact
from a decrease in systemic pressure. Patients being main-
tained on ventilatory support are subjected to mild hyper-
ventilation to decrease cerebral hyperemia. Patient
stimulation must be minimized by premedication prior to
suctioning or postural changes in patients with severe
intracranial hypertension. A number of other measures may
decrease cerebral edema, such as mannitol (1 g/kg). Serum
osmolarity should be monitored. Mannitol is contraindi-
cated if the serum osmolarity is greater than 320 mOsm/L.
The use of barbiturates has been proposed as a means of
lowering intracranial pressure in combination with hypother-
mia. Barbiturates decrease cerebral metabolism and further
Table 34–1. Causes of acute hepatic failure.
Most common causes in USA
Acute viral hepatitis (HBV, HAV, HC)
Acetaminophen toxicity
Less common causes
Hepatitis D and E
Herpes simplex virus
Epstein-Barr virus
Drug toxicity
Antimicrobials (eg, ampicillin-clavulanate, ciprofloxacin,
erythromycin, isoniazid, tetracycline)
Sodium valproate
Lovastatin
Phenytoin
Tricyclic antidepressants
Halothane
Other toxins
Ecstasy (methylenedioxymethamphetamine)
Amanita phalloides (mushrooms)
Organic solvents
Herbal medicines (eg, ginseng, pennyroyal oil,
Teucrium polium
).
Miscellaneous causes
Acute fatty liver of pregnancy
Autoimmune hepatitis
Budd-Chiari syndrome
Reye’s syndrome
Wilson’s disease
Indeterminate
Stage Mental Status Tremor Electroencephalography
I Euphoria, occasionally depression; fluctuating mild confu-
sion; slowness of mentation and affect; slurred speech;
disorder in sleep rhythm
Slight Normal
II Drowsiness; inappropriate behavior. Present Generalized slowing
III Sleeps most of the time but is arousable, confused;
incoherent speech.
Present Abnormal
IV Unarousable Absent Abnormal
Table 34–2. Stages of encephalopathy.
CHAPTER 34
716
decrease cerebral blood flow and pressure. They also prevent
seizures. Barbiturate use is controversial, however, because of
their delayed metabolism owing to liver insufficiency.
2. Cardiovascular support—Patients with acute liver
insufficiency experience arteriovenous shunting and vasodi-
lation that causes tachycardia and hypotension. The
decreased clearance of vasoactive metabolites causes
decreased systemic vascular resistance and increased cardiac
output. Therefore, volume resuscitation and vasoactive drugs
may be necessary as support measures. With this hemody-
namic profile, an important differential diagnosis is sepsis.
3. Coagulopathy—Transfusion therapy is in general
reserved for patients with active bleeding. It is indicated also
prior to invasive procedures such as the placement of
intracranial pressure monitoring.
4. Renal failure—Renal failure is common in patients with
acute liver insufficiency. Maintenance of euvolemia is critical.
Avoidance of nephrotoxic drugs (ie, aminoglycosides) is
important. If renal azotemia ensues, dialysis may be needed.
Continuous venovenous dialysis or arteriovenous dialysis
methods are preferred to avoid hemodynamic changes and
hypotension associated with standard hemodialysis.
5. Respiratory failure—Airway intubation and mechani-
cal ventilation are frequently used as the encephalopathy
progresses to stage III. Acute respiratory distress syndrome
(ARDS) occurs in one-third of patients, causing hypoxemia.
B. Liver Transplantation—The mortality of severe acute
liver insufficiency in the absence of liver transplantation
approaches 80%. Survival after orthotopic liver transplanta-
tion has improved in recent years from 50% to more than
80% in selected series. Unfortunately, only 40–60% of
patients actually undergo transplantation owing to the short-
age of available organ donors.
Contraindications to liver transplantation are malig-
nancy, extrahepatic sepsis, irreversible brain injury from
intracranial hemorrhage, and unresponsive cerebral edema.
Bioartificial liver support is being investigated in selected
centers as a bridge to transplantation. Reports of hemoperfu-
sion, plasmapheresis, and extracorporeal perfusion exist, but
there has been limited success. Most recently, the develop-
ment of hybrid bioartificial support systems using hepato-
cytes from human or xenogeneic sources has shown some
promise.
Acute Gastrointestinal Bleeding
from Portal Hypertension
ESSENTIALS OF DIAGNOSIS
Hematemesis, melena.
Stigmata of chronic liver disease.
Endoscopic evidence of bleeding varices.
General Considerations
Esophagogastric varices occur in 90% of patients with cir-
rhosis. Approximately one-third of these patients will experi-
ence GI bleeding, and between 30% and 50% of them will die
during each episode. It is not unexpected that bleeding from
esophagogastric varices accounts for one-third of all deaths
in patients with cirrhosis.
Esophagogastric varices are dilated intramural veins asso-
ciated with an extensive and tortuous capillary network.
They are alternative pathways of venous flow around the
increased vascular resistance in the intrahepatic and portal
system. They occur as a consequence of portal hypertension.
The development of varices is facilitated by systemic vasodi-
lation and decreased vascular resistance present in cirrhotics.
Clinical Features
A. Symptoms and Signs—Patients with acute bleeding
present with hematemesis. Patients with more chronic
bleeding present with melena and symptoms of anemia,
such as fatigue and weakness. Anemia may cause pallor and
tachycardia.
B. Laboratory Findings—Anemia occurs frequently.
Decreases in hemoglobin levels may not be detectable in an
early assessment of the bleeding. Evidence of chronic hepatic
dysfunction such as elevated serum aminotransferases,
bilirubin, and alkaline phosphatase is commonly present.
Differential Diagnosis
Patients with cirrhosis may experience an upper GI bleed
from other causes such as gastritis, peptic ulcer disease,
esophageal ulceration, or mucosal tears (Mallory-Weiss syn-
drome). Endoscopy is essential for diagnosis.
Table 34–3. Predictors of poor outcome in patients with
acute hepatic failure (King’s College criteria).
Acetaminophen toxic patients
Blood pH <7.30 (irrespective of grade of encephalopathy) or–
A combination of: encephalopathy stage III or IV, prothrombin time
>100 s (INR >6.5), and serum creatinine >3.4 mg/dL
Nonacetaminophen toxic patients
Prothrombin time >100 s (INR >6.5) (irrespective of stage of
encephalopathy) or–
Any three of the following five variables (irrespective of stage of
encephalopathy):
1. Age <10 years or >40 years
2. Etiology: hepatitis C, halothane hepatitis, idiosyncratic drug
reactions
3. Duration of jaundice before onset of encephalopathy of >7 days
4. Prothrombin time >50 s (INR >3.5)
5. Serum bilirubin level of >17.5 mg/dL
