Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CRITICAL CARE OF NEUROLOGIC DISEASE
677
General Considerations
The initial patient examination should lead to an etiologic
diagnosis and selection of appropriate therapy. Infectious
disease consultation may be necessary in the process. Beyond
this, the critical care physician should be alert to certain
aspects and complications of CNS infections. Viral, granulo-
matous, parasitic, and bacterial infections each have special
features requiring consideration, and all have some common
features.
Clinical Features
A. Viral Infections—Meninges and neurons are the site of
most CNS viral infections; human immunodeficiency virus
(HIV), which infects microglia and leads to the formation of
multinucleated cells in the brain, is a notable exception. Viral
meningitis usually runs a self-limited course with supportive
therapy only, and the specific virus usually is not identified,
no more than headache, fever, neck stiffness, and abnormal
CSF findings are expected clinical features. On the other
hand, viral encephalitis reflects neuronal dysfunction. Altered
mental status, seizures, and even focal neurologic signs are
common. Early recognition is especially important in herpes
simplex type I (HSV) encephalitis because early and prompt
treatment with acyclovir improves outcome. This virus has a
predilection for temporal lobes; thus presenting features
commonly are confusion, change of usual behavior patterns,
memory disturbance, and complex partial seizures, which
may secondarily generalized (see section on seizures).
Inflammation, sometimes with a hemorrhagic component,
and edema may be enough to affect nearby cortex, giving rise
to additional focal features such as hemiparesis, sensory
deficit, or language disturbance. If HSV encephalitis is sus-
pected, acyclovir should be started immediately and not
postponed awaiting confirmatory workup.
HIV infection of the CNS may result in mental and motor
slowing (AIDS dementia complex) by mechanisms not yet
understood, but aside from the acute phase of infection, the
occurrence of seizures, focal neurologic symptoms, and find-
ings or symptoms and signs of meningitis indicate a super-
imposed complication such as infection with Toxoplasma,
Cryptococcus, fungus, or mycobacteria or an intracerebral
lymphoma.
B. Parasitic Infections—Cysticercosis is the most common
parasitic CNS infection encountered in the United States. It
is most common in states bordering Mexico and is seen
most often in Mexican immigrants. It is a major public
health problem in other parts of the world as well. It is
acquired by ingestion of eggs of the tapeworm Taenia, which
are shed in the feces of human carriers. Three forms of the
disease exist. The most common site of infection is the
parenchyma of the cerebral hemispheres, and the natural
course of this form of the disease is eventual death of the
organisms and subsequent calcification of the lesion, which
is readily identified as punctate calcifications on CT scans.
This process often is entirely asymptomatic, but sometimes
the tissue reaction and associated edema caused by the
organisms’ death produce focal neurologic symptoms and
signs, and imaging studies may not clearly distinguish such
a lesion from a primary or metastatic neoplasm. In this
instance, neurologic consultation is indicated. The charac-
teristic locus of parenchymal cysticercosis is at the gray-
white junction, and the usual clinical manifestation is a
seizure disorder, which sometimes is limited in time and
sometimes chronic. The seizures are partial, often with sec-
ondary generalization, which may be so rapid that the par-
tial onset is unrecognizable. Treatment with antiepileptic
medication is indicated.
Another form of this disease is intraventricular cysticer-
cosis, in which the organism remains cystic and is located
within the ventricular system. It is asymptomatic unless it
causes obstructive hydrocephalus with headaches as the ini-
tial symptom. This is a very dangerous situation because the
cysts often are free to move within a ventricle and thus can
cause acute hydrocephalus and relatively sudden and unex-
pected death of the patient. A high degree of suspicion is nec-
essary and should lead to brain imaging studies, which could
include CT brain scan, intraventricular positive-contrast CT
brain scan to outline a cyst, and MRI of the brain.
Neurosurgical intervention for shunting of CSF or cyst
removal is required.
Finally, the organism may reside in the subarachnoid
space, where it exists in the racemose form and can cause
meningeal inflammation. This is an indolent and chronic
form, and racemose membrane formation with cystic locula-
tions usually is slowly progressive. If this occurs around the
base of the brain, it also may result in obstructive hydro-
cephalus and require placement of a CSF shunt. Nonsteroidal
anti-inflammatory medication is indicated for relief of
headache owing to the meningeal reaction and may decrease
the inflammatory response.
Praziquantel or albendazole will kill the organism in the
parenchymal form and perhaps the racemose form, but no
controlled evidence exists that treatment with these agents
changes the natural outcome of the disease. Furthermore, the
increased rate of organism death and the subsequent brain
tissue reaction have increased patient morbidity and in some
instances, particularly when the disease was present in the
posterior fossa and around the brain stem, have contributed
to death of the patient.
Amebic meningoencephalitis occurs but is rare in the
United States. Usually it is acquired from swimming or
bathing in infected fresh warm water springs. Fever,
headache, and seizures are the presenting signs. Amphotericin
B has been recommended for treatment.
Toxoplasmosis—infection with Toxoplasma gondii, an
obligate intracellular parasite—is one of the most frequent
opportunistic infections in patients with AIDS and as a con-
sequence is encountered much more frequently than it used

CHAPTER 30
678
to be. Symptoms are those of meningoencephalitis and often
include headache, confusion, delirium, obtundation, and less
often, seizure. Brain imaging studies and CSF examination,
including serum Toxoplasma IgG antibody titer, are useful in
diagnosis, but sometimes a favorable response to treatment
with pyrimethamine and sulfadiazine (usually judged by
reduction of lesions seen on imaging studies) is necessary for
diagnostic confirmation. Brain biopsy will be diagnostic if
response to treatment is uncertain or fails.
C. Granulomatous Infections—Among fungi and yeast
infections, coccidioidomycosis and cryptococcosis are
encountered most frequently. While their infectious agents
and mycobacteria may form parenchymal lesions, a chronic
progressive meningitis is the rule, and it has a predilection
for meninges at the base of the brain. A common complica-
tion is the development of hydrocephalus owing to blockage
of CSF flow from the foramina of Luschka and Magendie. It
is usually a relatively slow and progressive process, occurring
in the middle to later stages of these diseases, and it often
requires placement of a CSF shunt. Brain CT scan or MRI
will show the presence and progression of hydrocephalus.
With contrast material, those studies also show the presence
of the inflammatory basilar meningitis. Other complications
are cranial nerve deficits and infarctions caused by inflam-
mation and constriction from the proliferative meningitis
around arteries. Fluconazole and intravenous amphotericin B
are the primary drugs for treatment of coccidioidomycosis
and cryptococcosis, but sometimes the response is insuffi-
cient, and intrathecal administration of amphotericin B is
necessary. One must be aware that if the drug is delivered
into a lateral ventricle in the presence of hydrocephalus and
a shunt, it will not reach the site of infection but rather be
diverted away. Under these circumstances, placement of a
reservoir for delivery into the foramen magnum or lumbar
subarachnoid space may be possible. This will require neuro-
surgical consultation.
D. Bacterial Infections—CNS infection with Listeria mono-
cytogenes is singled out here because it is unusual in that it
can cause a rhombencephalitis with prominent brain stem
findings, and it also may cause meningitis. Persons with
chronic illness are predisposed to this disease. In general,
prompt diagnosis and appropriate therapy of bacterial infec-
tions can prevent or reduce complications.
When seizures or focal neurologic deficits occur in the
course of bacterial meningitis, one should suspect cortical
vein thrombosis, which can be demonstrated by brain imag-
ing studies. In the case of seizures, an antiepileptic drug such
as phenytoin or phenobarbital should be administered and
probably will have to be given intravenously (see section on
seizures). Acute sagittal sinus thrombosis is a life-threatening
complication because of brain swelling and bleeding into the
parenchyma; neurologic findings can include obtundation
and signs of increased intracranial pressure, seizures, and
perhaps focal neurologic deficits—typically paresis of the
legs because of the functional localization of the area of brain
drained by the sinus. CT scan or MRI will confirm the diag-
nosis. Administration of an anticoagulant may diminish
clotting but may serve to increase bleeding from veins feed-
ing the sinus. Seizures should be treated with an antiepilep-
tic drug. As prompt a resolution as possible of the underlying
infection will improve outcome.
Hydrocephalus can be an early or late complication of
bacterial meningitis. Impairment of CSF absorption at the
arachnoid granulations caused by purulent accumulation,
inflammation, and adhesions is a significant factor in this
case. CSF shunting may be necessary.
Neurologic features of bacterial brain abscesses characteris-
tically are focal neurologic findings and seizures. These
abscesses often develop because of cardiac or pulmonary right-
to-left shunting or extension of a sinus infection. In addition to
antibiotic therapy, neurosurgical drainage and excision may be
necessary. The dreaded complication is rupture of an abscess
into the ventricles; this results in an acute ventriculitis, which
almost always is fatal. Because of postinfectious scarring and
gliosis, a chronic seizure disorder can develop.
Lastly, it is notable that a partially treated bacterial
meningitis can mimic viral meningitis.
E. Laboratory Findings—The EEG should be normal in
viral meningitis, but it is highly likely to be abnormal in viral
encephalitis, showing generalized slowing and, sometimes,
epileptiform events. Characteristic of herpes encephalitis are
periodic seizure discharges, predominant over the affected
temporal area; absence of this finding does not rule out her-
pes encephalitis. Hydrocephalus, especially from disease in
the posterior fossa, can show background disorganization
and slowing with intermittent runs of high-voltage slow
waves. Any focal brain disease may result in focal slow activ-
ity in the EEG, and often it is especially prominent in brain
abscesses. The presence of epileptiform discharges will con-
firm the diagnosis of seizures and, if focal, indicate the site of
the epileptogenic process.
The CSF examination will show an increased cellular con-
tent in all active meningeal infections, although rarely the
specimen may be obtained just preceding the cellular
response; in this case, another specimen after a day or so
should show increased cells. In general, bacterial infections
will show polymorphonuclear leukocytes (PMNs) and the
other infections predominantly mononuclear cells. Some
viral infections, notably herpes simplex, may show a signifi-
cant proportion of PMNs early in the course of the disease.
It is typical in herpes encephalitis for the CSF to contain red
blood cells, but their absence does not rule it out. Partially
treated bacterial meningitis can show predominantly
mononuclear cells. Eosinophils are found occasionally in
cases of cysticercosis. The organism can be demonstrated by
India ink preparation in cryptococcosis and by wet prepara-
tion in amebic infection, but not finding them does not rule
out either one. The Gram stain may find bacteria and the
acid-fast stain mycobacteria. Low CSF glucose results from
infections interfering with its transport into the CSF, and it is

CRITICAL CARE OF NEUROLOGIC DISEASE
679
characteristically quite low in bacterial, fungal, and tubercu-
lous meningitis. It is usually little altered in viral meningitis.
Since the CSF glucose level is normally close to half the blood
glucose level, significantly high or low blood glucose can
confuse the issue. CSF glucose concentration lags behind
blood glucose 1–2 hours, but a blood glucose measured near
the time of obtaining the CSF specimen is usually satisfac-
tory for judging the CSF level. In viral infections, the CSF
protein content, like the glucose, is little altered, whereas it is
elevated in the other infections. If the protein content is very
high, blockage and impairment of CSF flow should be sus-
pected. Culture of CSF can provide a definitive diagnosis in
most infections other than viral, in which it is unusual to
recover the agent. Anaerobic organisms are common in brain
abscesses. Frequently the best management is to initiate
appropriate therapy while awaiting the results of culture.
Serologic tests of CSF include latex agglutination or other
techniques for detection of bacteria-specific antigens (usu-
ally available as a panel), measurement of cryptococcal anti-
gen, and assay of coccidioidal antibody titer—the latter two
are useful to follow as an index of response to treatment.
False-negative immunologic tests frequently are encountered
in neurocysticercosis, and a positive test may be found in
extraneural cysticercosis, so the practical value of such test-
ing is limited. Serum-specific HSV antibody titers rising over
the course of the illness can confirm the diagnosis, but usu-
ally in retrospect. Polymerase chain reaction (PCR) testing
for CSF herpes simplex antigen has rarely been helpful in the
authors’ experience. Toxoplasma IgM titer is helpful if posi-
tive; a negative result does not exclude the disease in AIDS.
HIV infection of the CNS can be accurately followed by
assaying the CSF viral load.
REFERENCES
Adams HP Jr et al: Guidelines for the early management of patients
with ischemic stroke. Stroke 2003;34:1056–83. [PMID: 12677087]
Antithrombotic Trialists’ Collaboration: Collaborative meta-analysis
of randomised trials of antiplatelet therapy for prevention of
death, myocardial infarction, and stroke in high risk patients. Br
Med J 2002;324:71–86. [Note: The last sentence of this article has
been corrected to read “for most healthy individuals, however, for
whom a risk of a vascular event is likely to be substantially less
than 1% a year, daily aspirin may well be inappropriate” (rather
than appropriate).]
Barohn RJ: Approach to peripheral neuropathy and neuronopathy.
Semin Neurol 1998;18:7–18. [PMID: 9562663]
Broderick JP et al: Guidelines for the management of spontaneous
intracerebral hemorrhage. Stroke 1999;30:905–15. [PMID:
10187901]
Drachman DB: Myasthenia gravis (medical progress). N Engl J Med
1994;330:1797–1810. [PMID: 8190158]
Hamel MB et al: Identification of comatose patients at high risk for
death or severe disability. JAMA 1995;273:1842–8. [PMID:
7776500]
Keys PA, Blume RP: Therapeutic strategies for myasthenia gravis.
DICP 1991;25:1101–8. [PMID: 1803801]
Medical Consultants to the President’s Commission for the Study of
Ethical Problems in Medicine and Biomedical and Behavioral
Research: Guidelines for the determination of death. Neurology
1982;32:395–99.
Plum F, Posner JB: The Diagnosis of Stupor and Coma, 3rd ed. New
York: Davis, 1982.
Qureshi AI: Endovascular treatment of cerebrovascular diseases and
intracranial neoplasms. Lancet 2004;363:804–13. [PMID: 15016492]
Van Ness PC: Pentobarbital and EEG burst suppression in treatment
of status epilepticus refractory to benzodiazepines and phenytoin.
Epilepsia 1990;31:61–67. [PMID: 2303014]
680
00
Neurosurgical critical care covers a wide array of disorders
with varying pathophysiologic features. These conditions
also may be associated with unique complications that must
be recognized and treated promptly. Physicians involved in
the ICU management of neurosurgical patients therefore
must be familiar with the clinical features, complications,
and treatment of CSN disorders.
This chapter focuses on the management of patients with
head injury, aneurysmal subarachnoid hemorrhage, brain
tumor, and cervical spinal cord injury. These disorders com-
prise the majority of neurosurgical ICU admissions.
Following injury, the CNS is vulnerable to a variety of sec-
ondary insults that can occur minutes, hours, or days following
the primary injury. Systemic conditions such as hypoxia,
hypotension, and electrolyte disorders may result in morbidity in
severely injured patients. Cerebral complications such as elevated
intracranial pressure, seizure, hemorrhage, and ischemia also
have the potential to cause neurologic impairment. The main
focus of current intensive care is to avoid or quickly reverse con-
ditions that can lead to secondary injury. Therefore, meticulous
management of all aspects of critical care is required to prevent
increased neurologic damage and improve patient outcome.
Head Injuries
ESSENTIALS OF DIAGNOSIS
Signs depend on severity and anatomic location.
Concussion: transient loss of consciousness, memory
loss, headache, autonomic dysfunction.
Herniation: depressed level of consciousness, anisocoria,
abnormal motor findings.
General Considerations
Injuries to the brain remain the most common cause of
trauma-related death and disability. More than 500,000 peo-
ple suffer some degree of head trauma annually in the United
States. In the past, patients with traumatic brain injuries were
viewed with pessimism because both surgical and medical
therapeutic resources were limited. However, with recent
advances, including prompt, intensive management of head-
injured patients, the outcome has improved. One of the
major reasons for the better results has been improved criti-
cal care management, particularly the recognition and pre-
vention of disorders that cause secondary brain injury.
Classification
A. Primary Injuries—By definition, primary traumatic brain
injury occurs at the time of impact. This may lead to irre-
versible damage from cell disruption depending on the mech-
anism and severity of the inciting event. Head trauma may
cause damage to the scalp, skull, and underlying brain. Scalp
lacerations can cause significant hemorrhage, but in most
cases hemostasis can be achieved easily. Fractures are classi-
fied as linear, depressed, compound, or involving the skull
base. Linear or simple skull fractures require no specific treat-
ment. Depressed skull fracture occurs when the outer table of
the skull is depressed below the inner table and may result in
tearing of the dura or laceration of the brain. Operative repair
may be required, especially if the depressed fracture involves
the posterior wall of the frontal sinus or is associated with
intracranial hematoma. Compound depressed fractures are
defined as those associated with laceration of the overlying
scalp and are treated by surgical wound debridement and
fracture elevation, if severe. Basal skull fractures, which may
be diagnosed by the clinical findings of periorbital ecchymo-
sis (“raccoon eyes”), ecchymosis of the postauricular area
(Battle’s sign), hemotympanum, or cerebrospinal fluid (CSF)
leak, may be complicated by meningitis or brain abscess.
Patients suffering from skull fractures have an increased risk
31
Neurosurgical Critical Care
∗
Duncan Q. McBride, MD
∗
Chris A. Lycette, MD, Curtis Doberstein, MD, Gerald E. Rodts, Jr.,
MD, and Duncan Q. McBride, MD, were the authors of this chapter
in the second edition.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
NEUROSURGICAL CRITICAL CARE
681
of delayed intracranial hematoma and should be observed for
12–24 hours after the initial injury.
Brain injury can occur directly under the injury site (coup
injury), but because the brain may move relative to the skull
and dura, compression of the brain remote from the site of
impact also can occur. This explains why brain injury can occur
in intracranial regions opposite the point of impact (contrecoup
injury). Craniocerebral trauma can cause concussion, cerebral
contusion, intracranial hemorrhage, or diffuse axonal injury.
1. Concussion—Concussion is an episode of transient loss
of consciousness following craniocerebral trauma. There is
no evidence of pathologic brain damage. Patients may suffer
from variable degrees of memory loss, autonomic dysfunc-
tion, headaches, tinnitus, and irritability.
2. Cerebral contusions—Cerebral contusions are hetero-
geneous areas of hemorrhage into the brain parenchyma and
may produce neurologic deficits depending on their anatomic
location. The anterior portions of the frontal and temporal
lobes are particularly vulnerable because of the rough contour
of the skull in these regions. Contusions are often associated
with disruption of the blood-brain barrier and may be com-
plicated by extension of the hemorrhage, edema formation, or
seizure. Large contusions can cause a mass effect resulting in
elevation of intracranial pressure or brain herniation.
3. Intracranial hematomas—Head injury may cause hem-
orrhage into the epidural, subdural, or subarachnoid spaces.
This bleeding, which may require surgical evacuation depend-
ing on its size and location, is usually diagnosed prior to admis-
sion to the ICU. However, delayed intracranial hematomas or
postoperative hematomas are not uncommon following cran-
iocerebral trauma and can develop and progress during ICU
observation. Intracranial bleeding may result in mass effect that
can cause intracranial pressure elevation (see below) and brain
herniation with compression of vital cerebral structures.
a. Epidural hematoma—This lesion is typically associated
with skull fracture and laceration of a meningeal vessel, most
commonly the posterior branch of the middle meningeal
artery. This may occur following low-velocity impact
injuries. Because the dura is firmly tethered to the inner table
of the skull, the hematoma usually takes on a homogeneous
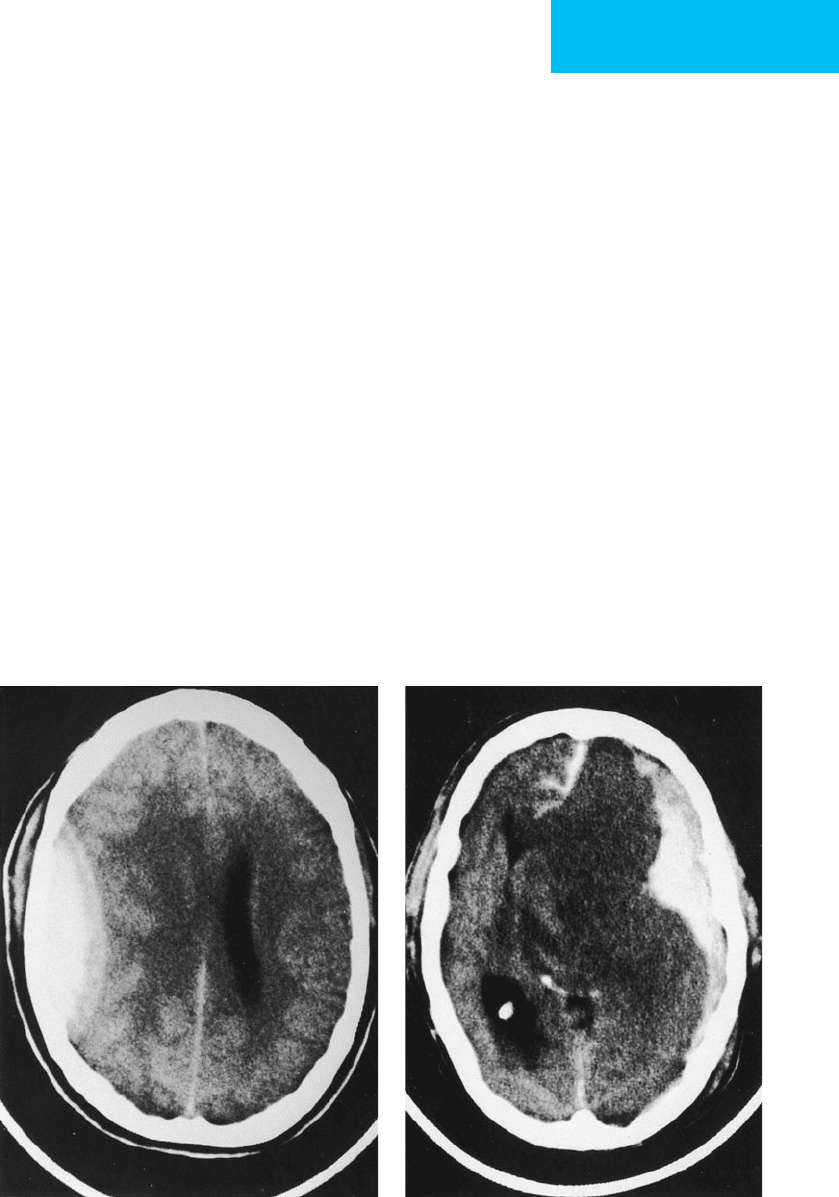
lentiform configuration (Figure 31–1A).
b. Subdural hematoma—Subdural hematoma can be sec-
ondary to tearing of the cortical vessels, such as the bridging
veins that drain from the cortex to the dura and superior sagittal
sinus. It is commonly associated with other injuries such as cere-
bral contusions and has a worse prognosis than epidural
hematoma. Because it is not contained by dural attachments, the
hemorrhage often spreads diffusely across the cortical surface
resulting in a crescent-shaped image on CT scan (Figure 31–1B).
AB
Figure 31–1.
A.
Left temporoparietal epidural hematoma with obliteration of the left lateral ventricle and midline
shift.
B.
Right frontoparietal and interhemispheric subdural hematoma with massive right-to-left midline shift.
CHAPTER 31
682
c. Subarachnoid hemorrhage—Subarachnoid hemor-
rhage is caused most commonly by craniocerebral trauma.
The subarachnoid bleeding itself does not usually cause neu-
rologic damage, but hydrocephalus and cerebral vasospasm,
which are delayed complications, can lead to neurologic
impairment. Subarachnoid hemorrhage as a result of a rup-
tured intracranial aneurysm always should be considered as
a possible causative factor in trauma and needs to be ruled
out with an angiogram if there is reasonable concern.
4. Diffuse axonal injury—Diffuse axonal injury is shear-
ing of brain tissue with disruption of neuronal axon projec-
tions in the cerebral white matter resulting from rotational
deceleration of the brain. This diffuse injury to axons occurs
microscopically and can result in severe neurologic impair-
ment. Evidence of diffuse axonal injury is often not demonstra-
ble on CT scan. However, macroscopic hemorrhagic lesions
can be seen in deep brain structures such as the corpus callo-
sum or brain stem in association with diffuse axonal injury.
B. Secondary Injuries—Many studies have observed that
cerebral autoregulation is impaired after traumatic brain
injury. This causes patients with head injuries to be unusu-
ally vulnerable to secondary ischemic insults such as
hypotension, intracranial hypertension, and hypoxia.
Further ischemic damage often can be prevented with an
understanding of the pathophysiology of these secondary
insults and an aggressive targeted management protocol.
These conditions can be conveniently divided into intracra-
nial and systemic disorders (Table 31–1). Following traumatic
brain injury, some cells are directly and irreversibly damaged.
However, other cells may be functionally compromised and
not mechanically disrupted. These may recover if provided
with an optimal environment for survival. Compromised
cells are vulnerable to the pathophysiologic challenges
imposed by secondary insults. Prevention or rapid recogni-
tion and treatment of secondary insults is the primary focus
of modern critical care management of head-injured patients.
1. Secondary intracranial insults (raised intracra-
nial pressure)—Intracranial hypertension following cran-
iocerebral trauma may be caused by intracranial hematomas,
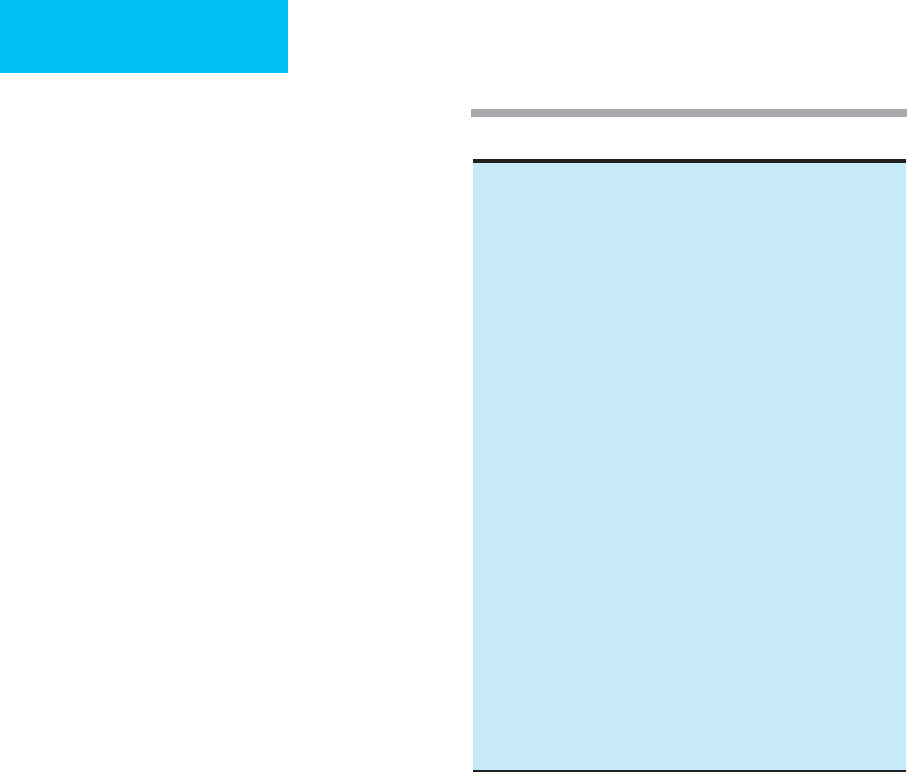
cerebral edema, or cerebral hyperemia. The Monro-Kellie
doctrine proposes that small increments in intracranial vol-
ume ultimately may cause intracranial pressure (ICP) to rise
because of the rigid and inelastic properties of the skull.
Under normal circumstances, intracranial volume is com-
posed of roughly 80% brain tissue, 10% CSF, and 10% blood.
An increase in volume of one of these compartments—or the
addition of a new pathologic compartment (eg, intracranial
hematoma)—must be compensated for by a reduction in the
volume of another compartment to maintain pressure.
Compensatory mechanisms that buffer such volume changes
include increased CSF absorption, redistribution of CSF
from the intracranial cavity into the spinal subarachnoid
space, and a reduction in cerebral blood volume. Cerebral
compliance relates the change in intracranial volume to the
resulting change in ICP (Figure 31–2). High compliance
signifies a system that can use buffering mechanisms to keep
ICP stable with changes in intracranial volume. However,
when the buffering becomes saturated, large pressure eleva-
tions result from small volume changes (poor compliance;
arrow in Figure 31–2). Therefore, although ICP may lie
within a relatively normal range (up to 20 mm Hg), a low-
compliance state may exist, and rapid elevations in ICP may
result from small increases in intracranial volume.
The falx cerebri, tentorium cerebelli, and foramen mag-
num are relatively rigid structures that compartmentalize
regions of the brain. Because many pathologic processes are
focal, pressure gradients can be generated between the
intracranial compartments. Elevated ICP may exert its delete-
rious effect by causing pressure gradients between different
brain compartments. If this pressure gradient is of sufficient
magnitude, shifting or herniation of brain tissue occurs and
can result in compression of vital structures. For example,
transtentorial herniation occurs when increased supratentorial
volume and pressure are sufficient to shift the uncus and the
medial portion of the temporal lobe through the tentorial
notch, causing compression and dysfunction of the midbrain
and oculomotor nerve. Compression of the medulla occurs
Table 31–1. Secondary insults.
Intracranial
Raised intracranial pressure
Delayed intracerebral hematoma
Edema
Hyperemia
Carotid artery dissection
Seizures
Vasospasm
Systemic
Hypoxia
Respiratory arrest
Airway obstruction
ARDS
Aspiration pneumonia
Pneumonia and hemothorax
Pulmonary contusion
Hypotension
Shock
Excessive bleeding
Myocardial infarction
Cardiac contusion or tamponade
Spinal cord injury
Tension pneumothorax
Electrolyte imbalance
Diabetes insipidus
SIADH
Others
Anemia
Hyperthermia
Hypercapnia
Hypoglycemia
NEUROSURGICAL CRITICAL CARE
683
when ICP is elevated and the cerebellar tonsils herniate through
the foramen magnum. This condition, known as tonsillar herni-
ation, can prove fatal because of the location of vital respiratory
and vasomotor centers in this area of the brain stem.
Alternatively, since cerebral perfusion pressure (CPP) is
inversely related to ICP,
∗
elevations in pressure may cause
impaired cerebral perfusion. If CPP is greatly reduced
(<40–50 mm Hg), cerebral ischemia or infarction can occur.
Therefore, maintenance of systemic blood pressure is of
paramount importance when ICP is elevated.
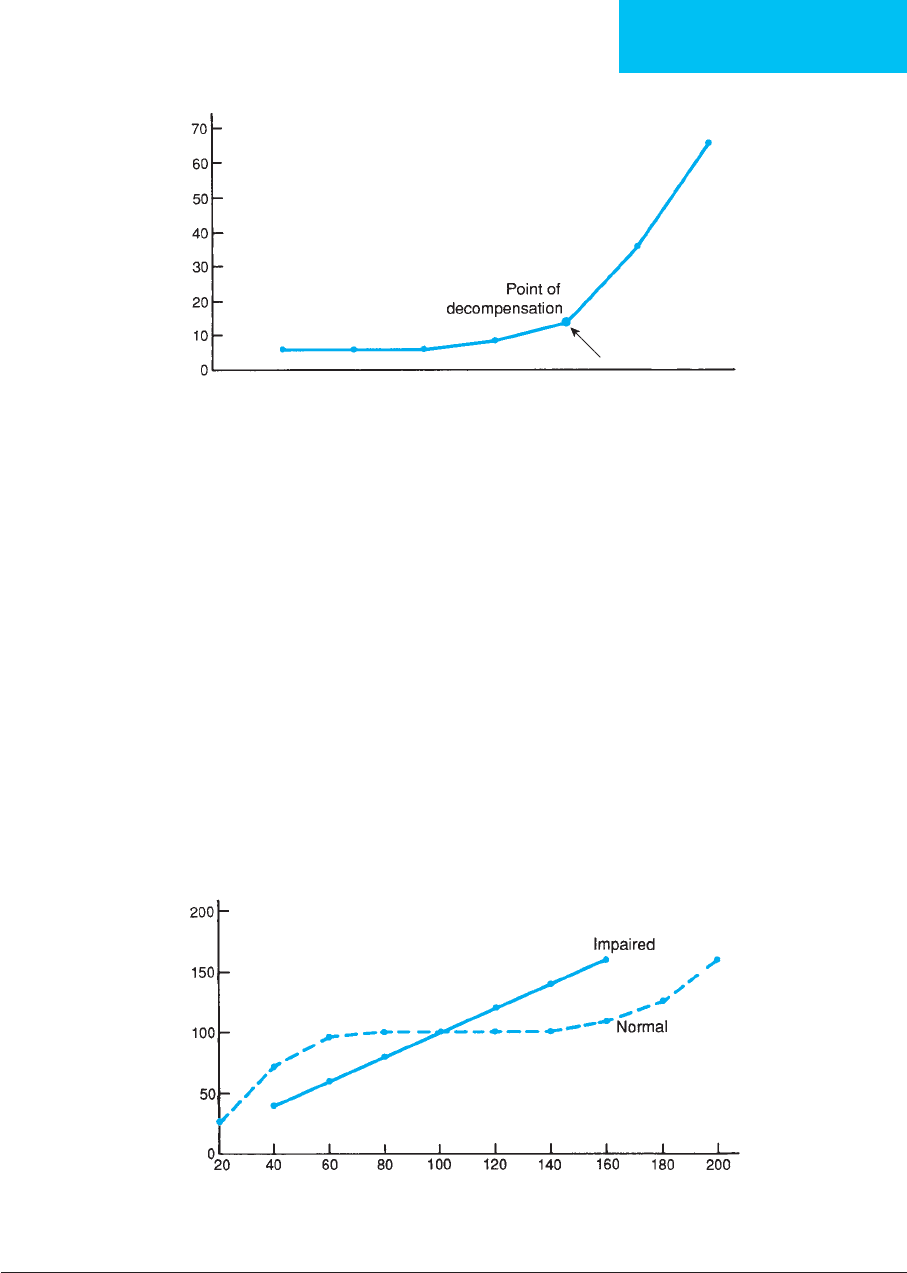
2. Secondary systemic insults—Of the various systemic
secondary insults, hypoxia and hypotension are the most
significant. Prospective clinical studies have demonstrated
that these two variables independently have a deleterious
influence on the outcome in severe head injury. Hypotension
alone is associated with a 150% increase in mortality rate. In
patients with significant head injuries, hypoxemia may be due
to upper airway obstruction, pneumothorax, hemothorax,
pulmonary edema, or hypoventilation. Whatever the cause,
hypoxemia must be corrected rapidly to avoid potential
damage to neural tissues. Hypotension reduces cerebral
perfusion, which promotes cerebral ischemia and infarc-
tion. This is particularly harmful in the face of elevated ICP.
In addition, impaired cerebral autoregulation can occur
after brain injury. With normal autoregulation, cerebral
blood flow remains constant despite fluctuation in mean
arterial pressure between 60 and 180 mm Hg (Figure 31–3).
Rapid arteriolar constriction or dilation occurs in response
to pressure changes. However, when this normal response is
Volume
ICP (mm Hg)
Figure 31–2. Intracranial pressure (ICP) remains normal with increased volume until the point of decompensation is
reached. Above this critical volume, ICP increases quickly.
Figure 31–3. Cerebral blood flow (CBF) remains normal over a wide range of cerebral perfusion pressures in nor-
mal patients. Under pathologic conditions, CBF varies directly with cerebral perfusion pressure (CPP).
CCP (mm Hg)
CBF (percent)
∗
Cranial perfusion pressure (CPP) = Mean arterial pressure (MAP) – Intracranial pressure (ICP)
CHAPTER 31
684
impaired, cerebral blood flow becomes directly related to
systemic arterial pressure. Thus, if hypotension occurs,
reduced tissue perfusion and ischemia may result. Elective
surgery for extracranial injuries should be delayed as long as
possible because of this issue. Surgery-related hypotensive
episodes can have correspondingly negative impact on brain
perfusion and ultimately the quality of overall outcome.
Other treatable or preventable systemic causes of secondary
brain injury include electrolyte disturbances, anemia, hypo-
glycemia, hyperthermia, coagulopathies, and seizures.
Clinical Features
A. Symptoms and Signs—Clinical examination remains
the best method for rapidly identifying neurologic deteriora-
tion. The Glasgow Coma Scale, which is based on eye open-
ing as well as verbal and motor responses, is used widely to
assess head injury patients (Table 31–2). Other important
components of the initial neurologic examination include
assessment of brain stem function, including level of con-
sciousness, respiratory pattern, pupillary size and reactivity,
as well as oculocephalic, oculovestibular, and gag reflexes. Eye
movements, extremity motor and sensory function, and lan-
guage and speech also should be evaluated. Following this
initial brief examination, a more thorough neurologic assess-
ment can be performed.
Transtentorial herniation, usually secondary to an
expanding supratentorial mass, produces a classic triad of
clinical signs: (1) depressed level of consciousness owing to
compression of the midbrain reticular activating system,
(2) anisocoria and loss of the pupillary light reflex owing to
ipsilateral third nerve compression, and (3) abnormal motor
findings from compression of the midbrain. In the early
stages of herniation, the ipsilateral third nerve is compressed;
however, if pressure on the brain stem increases, both pupils
may become dilated and unreactive. Contralateral hemipare-
sis owing to direct compression of the ipsilateral cerebral
peduncle is the most frequent abnormal motor response.
However, in about 25% of patients, hemiparesis may occur
on the same side as the mass lesion because the brain stem is
displaced away from the mass, compressing the opposite
cerebral peduncle against the free edge of the tentorium
(Kernohan’s notch phenomenon). The posterior cerebral
artery can be occluded during transtentorial herniation and
result in infarction of the occipital lobe it supplies.
Signs of tonsillar herniation include respiratory irregular-
ities, Cushing’s response (ie, elevated blood pressure associ-
ated with bradycardia), nuchal rigidity, and abnormal gag
and cough reflexes owing to medullary compression. During
early herniation, the patient’s level of consciousness may be
normal because the upper brain stem and reticular activating
system remain intact.
Neurologic deterioration in the ICU warrants immediate
and thorough evaluation in an effort to elucidate the cause.
Vital signs, serum electrolytes, O
2
saturation, and arterial
blood gas values should be determined if the deterioration is
global in nature. However, if the examination suggests a focal
lesion, an intracranial hematoma, elevated intracranial pres-
sure with a herniation syndrome, cerebral edema, or cerebral
ischemia is probably present. Studies validate that aggressive
medical management can reverse herniation and improve
outcome.
B. Imaging Studies—
1. CT scan—CT scanning is significantly more accurate than
conventional radiographs and has replaced them in the eval-
uation of head injuries. CT scanning can delineate parenchy-
mal hemorrhages and contusions, epidural and subdural
hematomas, cerebral edema, hydrocephalus, and cerebral
infarction. An intracranial lesion is said to exert a “mass
effect” on the brain when there is CT evidence of effacement
of the cerebral ventricles, subarachnoid cisterns, or cortical
sulci signifying redistribution of CSF. Further CT evidence of
a mass effect includes a shift of midline structures away from
the lesion and herniation of tissues. The outlet of the con-
tralateral ventricle can become “trapped” as a result of mid-
line shifting, and this can further increase ICP. Because MRI
is slower and generally not available emergently, especially in
intubated patients, it is not used commonly to assess acute
neurologic deteriorations. The availability of portable CT
scanners enables the diagnostic study to be performed with-
out transporting an unstable patient and risking harmful res-
piratory or cardiovascular events.
2. Cerebral angiography—Prior to the advent of CT
scanning, angiography was the primary diagnostic study for
evaluating head-injured patients because it detects the mass
effect from intracranial lesions. Currently, however, the main
role for angiography is the assessment of vascular disorders
Table 31–2. Glasgow Coma Scale.
Eye opening (E)
Spontaneous 4
To voice 3
To pain 2
None 1
Motor responses (M)
Obeys commands 6
Localizes pain 5
Withdraws 4
Abnormal flexion 3
Abnormal extension 2
None 1
Verbal responses (V)
Oriented 5
Confused 4
Inappropriate words 3
Incomprehensible sounds 2
None 1
TOTAL SCORE (3 to 15)

NEUROSURGICAL CRITICAL CARE
685
such as dissection or traumatic pseudoaneurysm of the
internal carotid or vertebral arteries and cerebral vasospasm.
Both MRI- and CT-based noncatheter angiography have sup-
planted invasive techniques for most emergency indications.
3. Transcranial Doppler ultrasonography—Transcranial
Doppler ultrasonography is a noninvasive technique that
measures blood flow velocity in the basal cerebral arteries.
It can be performed serially at the bedside in the ICU and
can reliably detect arterial narrowing owing to vasospasm,
which causes increased flow velocity. It also can aid in the
confirmation of absent blood flow owing to brain death.
C. Monitoring of Intracranial Pressure—Measurement of
ICP through an open catheter placed in the lateral ventricle
(ventriculostomy) is the standard with which all other meth-
ods of ICP measurement must be compared. Additionally,
CSF may be drained via the ventriculostomy to treat elevated
pressures, if present. Ventricular catheters may be placed in
the operating room during surgery or can be inserted at the
bedside in the emergency room or ICU. Because of the risk
of infection, patients with ventriculostomies should be given
prophylactic antibiotics with gram-positive coverage such as
cefazolin or vancomycin, and the catheters must be changed
periodically. Measurement of ICP also can be done using a
fiberoptic or strain-gauge device. These monitors are usually
more expensive, have a tendency to drift, and are unable to
drain CSF.
D. Lumbar Puncture—Lumbar puncture should not be per-
formed in the initial evaluation of head trauma patients
because of the risk of tonsillar herniation. The only role for
lumbar puncture is to examine CSF in patients who may
have meningitis. In such cases, ICP must be thought to lie
within the normal range prior to the procedure, or patients
should receive mannitol to induce diuresis prior to a small-
volume tap with a thin (eg, 22-gauge) spinal needle.
Treatment
A. Surgery—Patients who show neurologic deterioration
require rapid intervention to prevent irreversible tissue dam-
age. Cerebral contusions, intracranial hematomas, and for-
eign bodies may require emergent evacuation depending on
their size and location.
B. Reduction of Intracranial Pressure—Raised ICP should
be treated using the following measures:
1. Removal of CSF by ventricular drainage.
2. The use of mannitol prior to ICP monitoring should be
reserved for signs of transtentorial herniation or progres-
sive neurologic deterioration not attributable to systemic
extracranial explanations. Serum osmolarity should be
maintained below 320 mOsm/L to avoid renal failure, and
volume should be replaced with colloid agents or blood if
necessary to avoid hypotension or reduced cerebral per-
fusion. A Foley catheter is essential.
3. Hyperventilation results in cerebral vasoconstriction and
can help to reduce ICP for brief and specific periods. The
vasoconstrictive effects assist in the management of an
intracranial hypertensive crisis; however, the long-term
influence can produce permanent injury by reducing
blood flow below critical levels in an already injured
brain. Therefore, in the absence of high ICP, chronic
hyperventilation (Pa
CO
2
<25 mm Hg) should be avoided
in the first 24 hours after traumatic brain injury. In addi-
tion, the use of prophylactic hyperventilation (Pa
CO
2
<
35 mm Hg) during the first 24 hours should be limited
because it can compromise cerebral perfusion during a
time of reduced cerebral blood flow (CBF).
4. Head elevation should be maintained to promote cerebral
venous drainage. The head should be kept straight, and
tape from the endotracheal tube should not cross the
jugular area.
5. Sedation and neuromuscular paralysis are recommended
in intubated patients. Noxious stimuli may increase ICP,
which can be alleviated by sedation. Narcotics are useful
because they can be reversed rapidly. Neuromuscular
paralysis can reduce ICP in intubated patients by prevent-
ing increases in venous pressure associated with the Valsalva
maneuver during ventilatory support. Benzodiazepines and
propofol can be used as first-line agents for the sedation
of head-injured patients.
6. Anticonvulsant therapy (eg, IV keppra or phenytoin) can
be used to prevent or control seizure activity that
increases cerebral blood flow and subsequently ICP.
Available evidence does not indicate that the prevention
of early posttraumatic seizures improves outcome follow-
ing head injury, so these agents should be used with dis-
cretion. Bedside electroencephalography should be
obtained in patients with suspicious movements, pos-
tures, or eye movements and in those with unexplained
depression of consciousness. One week of prophylactic
anticonvulsant medication generally is sufficient in a
patient without evidence of seizure activity.
7. Fever increases ICP and should be prevented when possi-
ble. Chilled intravenous fluids or cooling blankets are
helpful for the management of refractory temperature
elevations.
8. Barbiturate (eg, pentobarbital) coma is useful if all other
medical therapies fail because it reduces ICP by decreas-
ing cerebral metabolism and therefore cerebral blood
flow. Care must be taken to prevent hypotension.
9. In selected patients in whom maximum medical therapy has
failed to reduce ICP, bony decompression or temporal lobec-
tomy can be performed surgically. Hemicraniectomy with
duraplasty can be performed in severe, refractory cases.
C. Electrolytes—Cerebral salt wasting is a recognized phe-
nomenon following brain injury and is caused by release of
cerebral natriuretic factors. It is defined as renal loss of
CHAPTER 31
686
sodium during intracranial disease leading to hyponatremia
and a decrease in extracellular fluid volume. Hyponatremia
produces increased brain swelling, and the volume depletion
that accompanies cerebral salt wasting must be treated
aggressively to avoid hypotension and reduced cerebral per-
fusion. Therefore, cerebral salt wasting should be recognized
promptly and treated with hypertonic saline solutions.
Traumatic brain injury also can result in a number of
other electrolyte disturbances requiring treatment, including
hypomagnesemia, hypophosphotemia, and hypokalemia.
Becker DP, Gudeman SK (eds): Textbook of Head Injury.
Philadelphia: Saunders, 1989.
Chesnut RM, Marshall LF: Treatment of abnormal intracranial
pressure. Neurosurg Clin North Am 1991;2:267–84.
Cooper PR: Delayed brain injury: Secondary insults. In Becker DP,
Povlishock JT (eds), Central Nervous System Trauma Status
Report—1985. Prepared for the National Institute of
Neurological and Communicative Disorders and Stroke.
Washington: National Institutes of Health, 1986.
Guidelines for the Management of Severe Head Injury, 2d ed.
Washington: Brain Tumor Foundation, 2000.
Marshall LF, Smith RW, Shapiro HM: The outcome with aggressive
treatment in severe head injuries. J Neurosurg 1979;50:20–5.
[PMID: 758374]
Seelig JM et al: Traumatic acute subdural hematoma: Major mor-
tality reduction in comatose patients treated under four hours.
N Engl J Med 1981;304:1511–8. [PMID: 7231489]
Temkin NR et al: A randomized double-blind study of phenytoin
for prevention of post-traumatic seizures. N Engl J Med
1990;323:497–502. [PMID: 2115976]
Aneurysmal Subarachnoid Hemorrhage
ESSENTIALS OF DIAGNOSIS
Headache.
Nausea and vomiting.
Photophobia.
Nuchal rigidity.
Depressed level of consciousness.
Cranial nerve palsies, motor abnormalities.
General Considerations
Rupture of an intracranial aneurysm is a devastating event
because roughly half of these patients die. Of the remainder,
almost half are left with significant neurologic deficits as a
result of their initial hemorrhage or owing to delayed com-
plications such as rebleeding, vasospasm, or hydrocephalus.
In order to optimize outcome following subarachnoid hem-
orrhage, successful surgical or radiologic intervention and
meticulous ICU care are required.
Intracranial aneurysms typically occur at bifurcation sites
of major arteries at the base of the brain and usually point in
the direction of blood flow. It is believed that a defect in the
medial elastic lamina is present that predisposes to aneurysm
formation. Aneurysms are associated with a variety of condi-
tions, including hypertension, polycystic kidney disease,
coarctation of the aorta, Ehlers-Danlos syndrome, pseudoxan-
thoma elasticum, and cerebral arteriovenous malformations.
Approximately 85% are located in the anterior circulation,
with the most common sites being the junction of the anterior
cerebral and anterior communicating arteries, the junction of
the internal carotid and posterior communicating arteries, the
bifurcation or trifurcation of the middle cerebral artery, and
the bifurcation of the internal carotid artery. Fifteen percent of
aneurysms lie within the posterior circulation; the basilar
artery apex is the most common site. Multiple aneurysms can
be identified in 15–20% of patients. Since the cerebral arteries
course within the subarachnoid space, rupture typically pro-
duces subarachnoid hemorrhage. However, intraparenchymal
and intraventricular bleeding may occur depending on the
location of the aneurysm and the extent of bleeding.
The three major complications following aneurysmal sub-
arachnoid hemorrhage are rebleeding, vasospasm, and hydro-
cephalus. Rebleeding from a ruptured intracranial aneurysm
occurs in 20% of patients during the first 2 weeks after the
initial hemorrhage if the aneurysm is untreated. The highest
risk is in the first 24 hours, and occlusive treatment with sur-
gery or interventional embolization is required. Cerebral
vasospasm is a common delayed complication of subarach-
noid hemorrhage and is related to the amount of blood
located within the subarachnoid space. Vasospasm typically
occurs between 3 and 14 days postbleed. Arterial narrowing is
thought to result from degradation of subarachnoid blood,
which produces breakdown products that cause smooth mus-
cle constriction. If this smooth muscle constriction is pro-
longed, morphologic alterations such as fibrosis can occur in
the vessel wall, further enhancing arterial narrowing.
Communicating hydrocephalus is another complication that
can occur after subarachnoid hemorrhage and is secondary to
blockage of CSF reabsorption by platelets, erythrocytes, and
their breakdown products. Hydrocephalus may present in an
acute, subacute, or delayed fashion.
In addition to the previously described neurologic com-
plications, several systemic medical disorders can occur fol-
lowing subarachnoid hemorrhage. Cardiac arrhythmias and
myocardial ischemia are observed often. Respiratory compli-
cations such as pulmonary edema, acute respiratory distress
syndrome (ARDS), and pneumonia are common. Other dis-
orders such as anemia, GI bleeding, deep vein thrombosis,
and hyponatremia occur with varying frequency.
Clinical Features
A. Symptoms and Signs—Subarachnoid hemorrhage is
described most often as the sudden onset of the worst
headache of the patient’s life. Other symptoms such as nausea
