Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

CRITICAL CARE OF VASCULAR DISEASE & EMERGENCIES
657
Poldermans D et al: The effect of bisoprolol on perioperative mor-
tality and myocardial infarction in high-risk patients undergo-
ing vascular surgery. N Engl J Med 1999;341:1789–94. [PMID:
10588963]
Powell RJ et al: Effect of renal insufficiency on outcome following
infrarenal aortic surgery. Am J Surg 1997;174:126–30. [PMID:
9293827]
Raby KE et al: Correlation between preoperative ischemia and
major cardiac events after peripheral vascular surgery. N Engl J
Med 1989;321:1296–300. [PMID: 2797102]
Tepel M et al: Prevention of radiographic-contrast-agent-induced
reductions in renal function by acetylcysteine. N Engl J Med
2000;343:180–184. [PMID: 10900277]
Samson RH et al: A modified classification and approach to the
management of infections involving peripheral arterial pros-
thetic grafts. J Vasc Surg 1988;8:147–53. [PMID: 3398172]
Yusuf S et al: Effects of an angiotensin-converting-enzyme inhibitor,
ramipril, on cardiovascular events in high-risk patients. The
Heart Outcomes Prevention Evaluation Study Investigators.
N Engl J Med 2000;342:145–53. [PMID: 10639539]

658
00
Alterations of consciousness including coma, seizures, and
neuromuscular disorders account for many of the neurologic
problems in patients admitted to ICUs. Therefore, this chap-
ter emphasizes encephalopathy and coma, seizures and status
epilepticus, and problems associated with neuromuscular
disorders. A comprehensive review of cerebrovascular disease
and stroke syndromes is beyond the scope of this book, but
since the critical care physician undoubtedly will have to deal
with cerebrovascular diseases, some fundamental aspects of
these disorders are described. In addition, certain aspects and
complications of CNS infectious diseases are included.
ENCEPHALOPATHY & COMA
Coma
The brain controls the individual’s ability to breathe, obtain
food and water, and avoid noxious stimuli in the environment.
When the individual slips into coma, the ability to perform
these functions is lost, and the patient will not survive unless
coma is reversed. In this sense, coma represents a global failure
of brain function. There are many causes of coma, some of
them reversible. The first responsibility of the physician caring
for a patient in coma is to ensure that breathing, circulation,
and nutrition are maintained. The cause of coma then must be
determined and reversible causes treated appropriately.
Normal consciousness has two main components: con-
tent and arousal. They have different anatomic substrates,
with the former localized largely in the cerebral cortex and
the latter depending on the brain stem reticular activating
system. Injury to the dominant cortical hemisphere leads to
impairment or loss of language function, but bilateral corti-
cal injury is required for complete loss of consciousness.
Furthermore, the cortex is responsible for interpreting
incoming signals. This includes encoding and assigning
“meaning” to emotional and sensory inputs. When the cor-
tex is diffusely injured, the ability to reflect on and interpret
experience is lost, and for this reason, the content of con-
sciousness is lost as well.
The major role of the brain stem reticular activating sys-
tem is to arouse and alert the cortex so that the organism can
reflect on and react to stimuli from the environment. A
patient can lose consciousness by two different mechanisms:
diffuse dysfunction of the cerebral cortex or injury to the
reticular activating system. Coma often develops as a result of
injury to both areas. However, cortical neurons are extremely
sensitive to a variety of metabolic and toxic injuries, includ-
ing hypoxia, hypercapnia, hyponatremia, hypernatremia,
hypoglycemia, hyperglycemia, and many drugs, whereas the
brain stem is more resistant to these injuries. Thus toxic and
metabolic injuries first cause dysfunction in cortical neu-
rons, and only with increasing severity influence the brain
stem. In contrast, coma owing to primary brain injury affects
the reticular activating system. These major anatomic differ-
ences allow the clinician to distinguish metabolic from struc-
tural causes of coma.
Neuroimaging techniques suggest that there may be a
fundamental pathophysiologic basis for many of the meta-
bolic causes of coma, perhaps explaining why so many
patients with different causes present with such similar clin-
ical profiles. In comas owing to metabolic encephalopathy, a
profound and diffuse decrease in cerebral glucose metabo-
lism has been shown using positron-emission tomography.
Similarly, severe and diffuse cerebral hypoperfusion as meas-
ured with
133
Xe appears in patients in coma owing to sepsis,
hepatic encephalopathy, hypoxia, head trauma, and cocaine
intoxication. Studies in comatose patients using
31
P magnetic
resonance spectroscopy have shown dramatic decreases in
the brain’s energy-containing phosphorus compounds,
including ATP and phosphocreatine. This work suggests that
any process that compromises cortical neuronal energy pro-
duction may lead to a comatose state.
Clinical Features
One key issue in the evaluation of any unconscious patient
is whether the unconscious state is due to metabolic,
toxic, or structural brain injury. Because there are only
30
Critical Care of Neurologic
Disease
Hugh B. McIntyre, MD, PhD
Linda Chang, MD
Bruce L. Miller, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CRITICAL CARE OF NEUROLOGIC DISEASE
659
minor differences in the clinical characteristics of comatose
states owing to varying types of metabolic and toxic insults,
the clinical examination cannot definitively distinguish one
metabolic cause from another; thus the cause must be sought
or confirmed with laboratory investigations. In contrast, if
the clinical examination suggests structural brain injury,
emergency imaging tests must be performed to determine
the cause so that appropriate treatment can be initiated.
Simultaneously with the assessment of the neurologic
examination, it is critical that the physician obtain an accu-
rate history. Although a comatose patient cannot give a his-
tory, relatives, housemates, and others often describe the
onset of coma and provide information regarding medica-
tions and preexisting illnesses. Even when information from
these sources is not available, paramedics usually can provide
details about the circumstances in which the patient was
found. In all cases, a check of the patient’s pockets and purse
or wallet may help to elicit important medical data, and some
patients wear medical bracelets or necklaces, which will alert
the examiner to potential causes of coma.
Rapidity of onset is an important clue to the cause of
coma. Certain metabolic insults such as hypoxia, ischemia, or
hypoglycemia may come on suddenly, whereas others such as
hyponatremia, hypernatremia, and hyperglycemia develop
subacutely. Similarly, subarachnoid hemorrhage or brain
stem ischemic stroke can lead to sudden coma, whereas coma
related to chronic subdural hematoma, cortical ischemic
stroke, or brain tumor usually develops slowly.
The five main areas that need to be assessed in the evalu-
ation of a patient in coma are (1) level of consciousness,
(2) pupillary responses and ophthalmoscopic examination,
(3) oculomotor system, (4) motor system, and (5) respira-
tory and circulatory systems.
Based on the findings in these domains, usually it is pos-
sible to localize accurately the specific regions in the brain
that are impaired. Table 30–1 lists changes that occur with
injury in different anatomic areas of the brain. A precise
anatomic localization of the area of dysfunction in the brain
often helps to elucidate the cause of coma. Although coma
scales are helpful in assessing prognosis, they are not a sub-
stitute for neurologic examination because they neither
localize the area of dysfunction nor help in determination of
the cause.
A. Level of Consciousness—Many terms such as stuporous,
lethargic, drowsy, and semicomatose have been used to char-
acterize degrees of altered consciousness. However, it is bet-
ter to describe the patient’s spontaneous activity, response to
verbal stimuli, and reaction to painful stimuli in precise
terms that do not have different meanings to different
observers. A carefully recorded description of the patient’s
level of consciousness on entry into the hospital will be
invaluable in following the progression of the comatose state.
With herniation from a large unilateral cerebral hemisphere
mass, drowsiness occurs when the reticular activating system
in the thalamus is compressed; coma ensues when injury to
the reticular activating system reaches the midbrain.
The best places to apply painful stimuli to determine
arousability are over the sternum or the nail beds; these
maneuvers also help to determine whether the patient
responds with evidence of focality, for example, if there is no
movement of one side while the other hand attempts to
remove the painful stimulus.
B. Pupillary and Ophthalmoscopic Evaluation—Perhaps
no component of the neurologic examination is as valuable
for differentiating metabolic or toxic coma from coma owing
to structural brain disease as inspection of the pupils.
Pupillary size is determined by the relative contributions of
the parasympathetic and sympathetic autonomic fibers.
Coma associated with brain injury usually exhibits changes
in the pupillary response. These changes occur because most
structural comas are associated with injury to the reticular
activating system in the brain stem where the Edinger-
Westphal and sympathetic autonomic fibers are located.
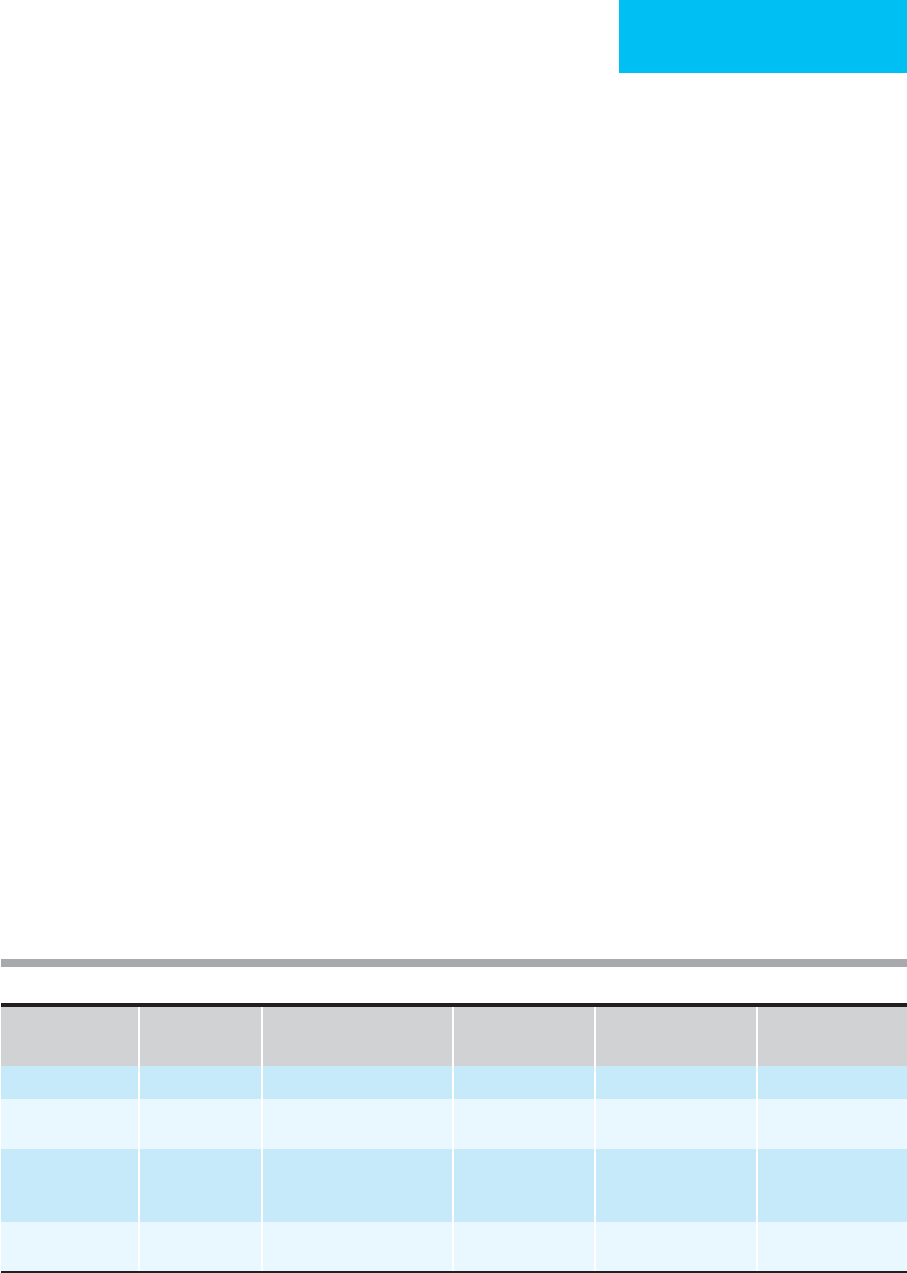
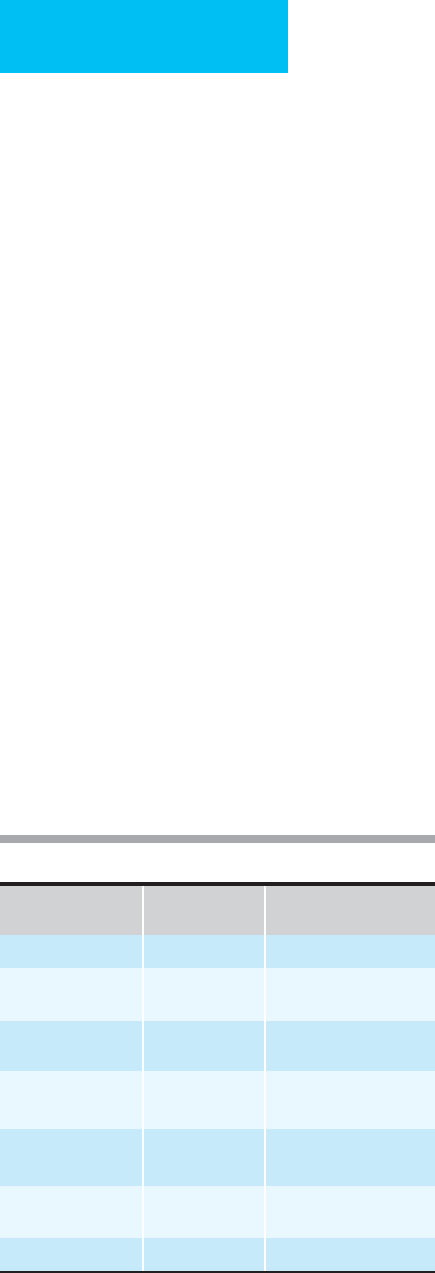
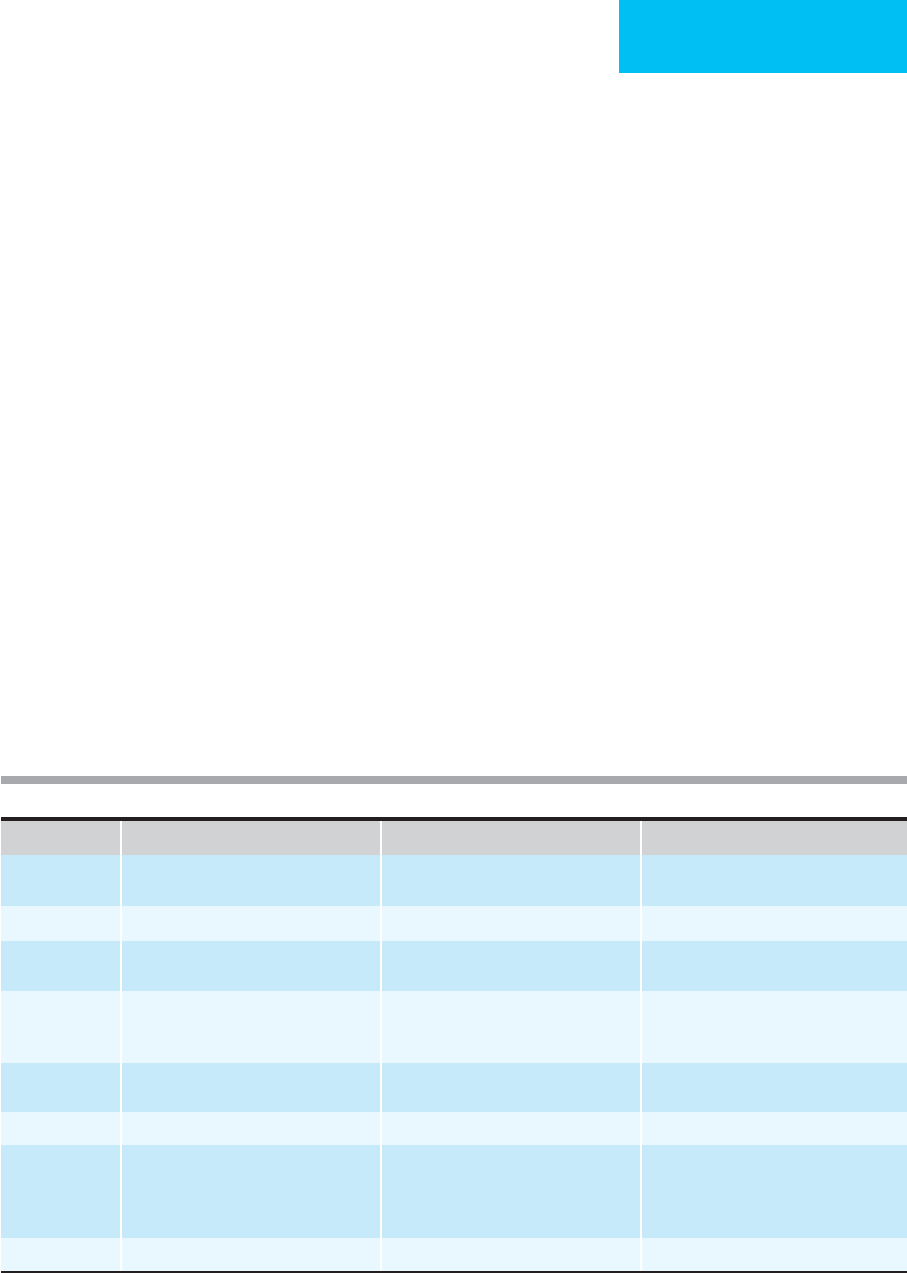
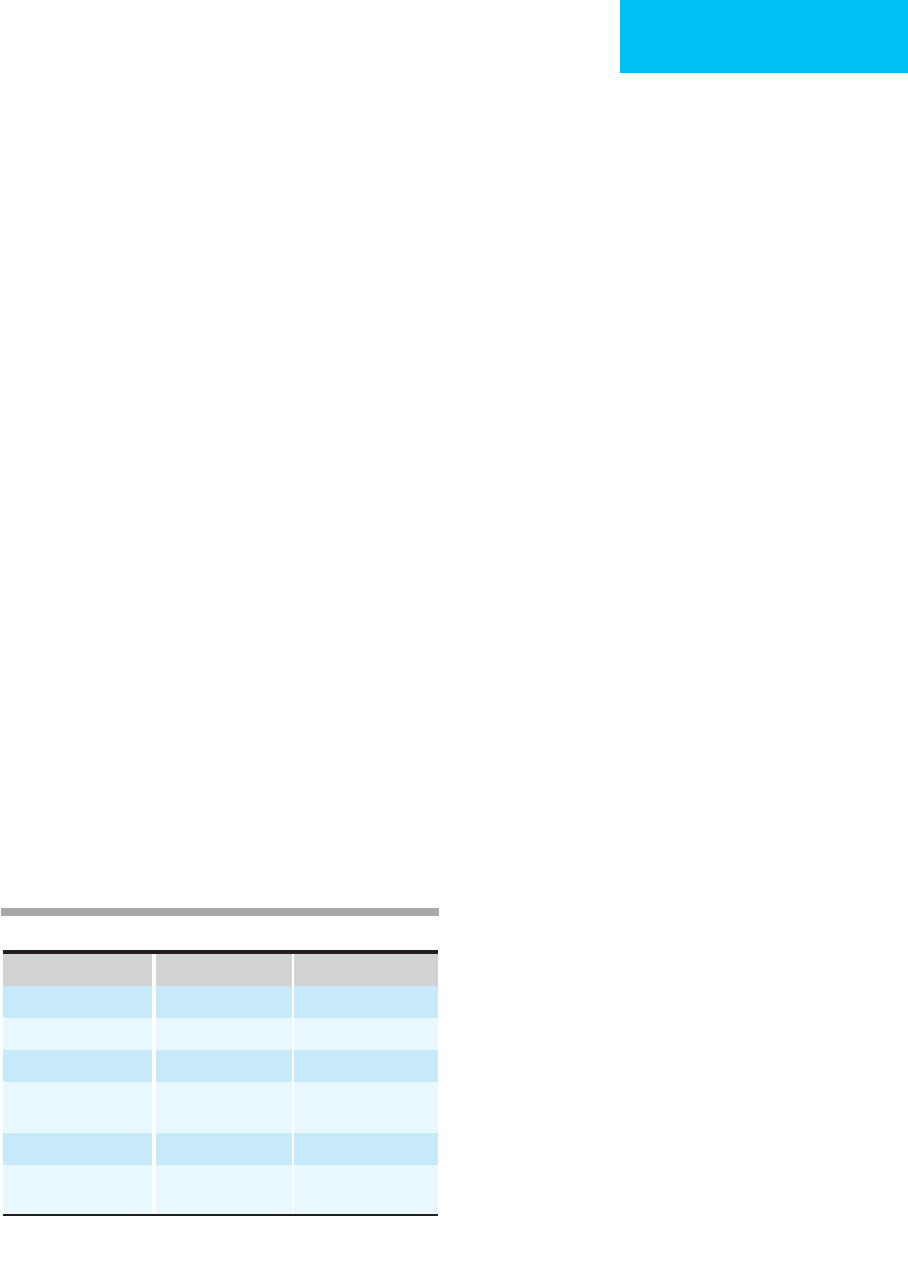
Anatomic Level Mental Status Pupillary Size and Position Eye Movement Motor Responses
Respiration and
Circulation
Diencephalon Drowsy Small (1–2 mm) Normal Abnormalities of flexion Cheyne-Stokes
Midbrain Coma Fixed in mid position Dysconjugate Abnormalities of
extension
Hyperventilation
Pons Coma 1 mm in primary pontine
injury; fixed and 4–5 mm
with prior midbrain injury
Complete paralysis Abnormalities of
extension
Hyperventilation
Medulla Variable Variable Variable Flaccid Apnea, circulatory
collapse
Table 30–1. Localization of brain lesions in a comatose patient.
CHAPTER 30
660
With acute injury to the midbrain, the pupils become fixed
in midposition as a result of simultaneous injury of sympa-
thetic and parasympathetic fibers. In contrast, injury to the
pons often is associated with pinpoint, minimally reactive
pupils. Lateral tentorial herniation of the temporal lobe may
result in compression of the third cranial nerve and the
parasympathetic fibers traveling with it, causing dilation of
the pupil on the side of the herniation. In some lateral herni-
ations there will be compression of the contralateral third
nerve against the edge of the tentorium.
A major characteristic of coma owing to metabolic dis-
eases is sparing of the pupillary response. This occurs
because metabolic coma causes selective dysfunction of the
cortex, whereas the centers in the brain stem that control the
pupils are spared. Many comas owing to drugs spare the
pupils, although some commonly used drugs do influence
the pupillary response (Table 30–2).
The ophthalmoscopic examination can provide valuable
information. Papilledema usually implies increased intracra-
nial pressure, whereas subhyaloid hemorrhage, which
appears as a fresh, red flame-shaped hemorrhage between
the retina and vitreous, is virtually pathognomonic of sub-
arachnoid hemorrhage.
Despite the importance of the ophthalmoscopic evalua-
tion, under no circumstances should the pupil be dilated in a
comatose patient because changes in the pupils are often the
most reliable clinical indication of deterioration following
brain injury.
C. Oculomotor System—As with pupillary responses,
changes in the oculomotor system often occur with primary
neurologic injury. The system responsible for moving the
eyes is located between the sixth nerve in the pons and the
third nerve in the midbrain. Closely adjacent to the sixth
nerve is a gaze center known as the pontine paramedian retic-
ular formation (PPRF). Just prior to moving one of the eyes
laterally, which is accomplished with the sixth nerve, there is
rapid firing in the PPRF. The contralateral eye will deviate
medially via fibers that travel from the PPRF, cross in the
pons, and travel medially to the contralateral third nerve
nucleus in the medial longitudinal fasciculus.
The simplest way to test the viability of this system is the
oculocephalic (“doll’s eye”) reflex. For this test, the patient is
positioned with 30-degree neck extension, and the head is
moved from side to side. If the brain stem PPRF and the
vestibular system are intact, the eyes should move smoothly
in the direction opposite to that in which the head is moved.
A more precise test is the caloric oculovestibular response.
For this test, the comatose patient is elevated to a 30-degree
angle, and one tympanic membrane is irrigated with ice-cold
water. Ten milliliters usually is sufficient to produce a
response. Within 1–2 minutes, both eyes should deviate lat-
erally toward the side where the cold water was instilled. In
metabolic or toxic coma this system is spared, whereas in
many structural comas the oculovestibular system is
impaired; in brain death, it is absent. In the normal, awake
patient, slow deviation toward the side of the stimulus is lost,
and nystagmus in the contralateral direction is observed.
D. Motor Systems—Primary brain lesions often are associ-
ated with focal motor deficits, but in metabolic or toxic
states, focal motor findings are normally absent. With lateral
cortical or internal capsular injury, the examination shows
contralateral motor deficit. Posturing in flexion (decorticate
posturing) supervenes when diffuse dysfunction of the dien-
cephalon occurs. Injury of the brain stem motor systems
between the red nucleus in the midbrain and the vestibu-
lospinal nuclei in the medulla leads to an abnormal extensor
response in the arms with flaccid or extensor response in the
legs (decerebrate posturing). Injury to motor systems at or
below the level of the vestibulospinal nuclei results in flaccid-
ity. With progressive neurologic injury, moving from higher
to lower centers, one sees a progression from paralysis to
flexor posturing to extensor posturing to flaccidity.
E. Respiratory and Circulatory Changes—With injury at
the level of the pons, abnormal respirations may occur. Once
the medulla is injured, there is loss of respiratory function,
and apnea ensues. Similarly, in the beginning stages of
medullary compression, abnormalities in blood pressure—
usually hypertension—can present. As the medullary injury
progresses, hypotension intervenes.
The first manifestation of a compressive lesion of the
medulla often is respiratory or circulatory collapse. Severe
hypertension is sometimes the first or main manifestation
of posterior fossa lesions. For these reasons, posterior fossa
lesions are difficult to diagnose and can be catastrophic
when missed.
Drug Type
Pupillary
Response
Other Changes
Opioids Pinpoint None
Barbiturates and
benzodiazepines
Reactive None
Anticholinergics
(scopolamine, etc.)
Pupils dilated Tachycardia, seizures
Anticholinesterases
(organophosphates)
Pupils constricted Bradycardia, sweating,
salivation
Cocaine and
amphetamine
Pupils dilated Tachycardia, hypertension,
hypotension, arrhythmia
Neuroleptics Pupils variable Motor rigidity,
hypotension, hyperthermia
Antidepressants Pupils dilated Rarely seizure
Table 30–2. Physical findings in drug-induced comas.
CRITICAL CARE OF NEUROLOGIC DISEASE
661
Differential Diagnosis
The major group of diseases that cause coma include meta-
bolic, toxic, and primary neurologic injury. The cause usually
can be determined by neurologic examination.
A. Metabolic Coma—In any patient with unexplained coma
suggesting metabolic dysfunction, it is important to measure
serum sodium, glucose, urea nitrogen, and creatinine; to
determine Pa
O
2
and Pa
CO
2
; and to perform liver and thyroid
function tests. A toxicology screen also is mandatory. Sepsis
can lead to coma, and evidence for infection should be sought
in any delirious or comatose patient. The physician should
have a low threshold for obtaining lumbar puncture for cere-
brospinal fluid (CSF) analysis in a patient with unexplained
coma. Comas owing to various metabolic factors have more
similarities than differences. Table 30–3 lists the major meta-
bolic causes of coma and comments on subtle differences in
coma owing to these various metabolic abnormalities.
Elderly people are particularly vulnerable to the effects of
metabolic insults and poorly tolerant of mild fluctuations in
metabolic status. Therefore, it is common to observe an eld-
erly patient in coma owing to relatively mild metabolic
abnormalities, whereas this same combination of metabolic
changes might not lead to coma in a young, otherwise
healthy individual. One typical example is the elderly patient
who develops delirium or even coma associated with a
pulmonary or urinary tract infection. In fact, elderly
patients’ changes in mental status sometimes are the first
manifestation of sepsis. Many patients with primary brain
injury, however, demonstrate mild metabolic abnormalities,
and one should not automatically assume that subtle meta-
bolic changes explain why a patient is in coma.
B. Toxic Coma—Coma secondary to drugs often resembles
coma from other metabolic processes. However, respiratory
suppression may be more common in patients with drug-
induced coma. Similarly, some groups of drugs have specific
effects on the pupils. The drugs that can cause coma are too
numerous to list in this chapter. Table 30–2 lists some com-
monly abused drugs and emphasizes the characteristics of
coma associated with drug overdose.
C. Primary Brain Injury—CNS infection, trauma, and
stroke can lead to coma. Massive rises in intracranial pressure
such as those seen with severe head injury, subarachnoid
hemorrhage, or blockage of CSF flow by a ventricular mass
cause sudden coma. Coma also occurs with acute injury to
the reticular activating system in the brain stem owing to
basilar artery thrombosis or pontine hemorrhage. In any
patient with altered consciousness and focal motor findings,
it should be assumed that a focal brain lesion is present.
Once it has been determined that a primary neurologic
event is a possible cause of the coma, emergency scan of the
brain is required. CT generally can be done quickly, is very
sensitive for acute hemorrhage, and demonstrates most focal
injuries. However, many patients with coma secondary to
ischemic brain injury, isodense subdural hematomas,
encephalitis, and meningitis will not show changes on CT
unless contrast material is used. If readily available, MRI is a
Disease Coma Mechanisms and Features Treatment
Hyponatremia Acutely: <120 meq/L
Chronically: <110 meq/L
Leads to true cytotoxic edema.
Skin can be doughy.
Hypertonic saline. Overly rapid correction
may lead to central pontine myelinolysis.
Hypernatremia >155 meq/L Loss in brain water. Seizures common. Slow rehydration.
Hypoglycemia <30 meq/dL Deprivation of brain glucose for energy
metabolism. Seizures are common.
Needs urgent glucose replacement.
Hyperglycemia Ketotic or nonketotic Changes in brain water and pH contribute
to both. Nonketotic coma often has
focal findings.
Slow correction.
Hypoxia Pa
O
2
usually <40 mm Hg Loss of brain O
2
for aerobic
metabolism.
Needs urgent correction.
Renal failure Variable Brain acidosis is a factor. Renal dialysis.
Hepatic failure Variable. Often precipitated by medications
or gastrointestinal bleeding
Brain ammonia and changes in glutamine
or dopamine hypothesized as causes.
Hyperventilation and decerebrate
posturing.
Treat precipitating factor.
Lactulose administration.
Hypothyroidism Chronic low levels Clinical findings of myxedema. Slow thyroid hormone replacement.
Table 30–3. Metabolic comas: mechanisms and treatment.
CHAPTER 30
662
good choice, although the imaging process takes longer than
CT scanning and is more expensive. Cerebral blood flow
imaging, single-photon-emission computed tomography
(SPECT), and diffusion MRI also may be helpful in the eval-
uation and management of patients with acute brain injury.
D. Brain Death—The diagnosis of brain death is an
unavoidable issue in the practice of critical care medicine
and must be approached with sensitivity to the patients’ close
associates and an awareness of the possibility of organ dona-
tion. When brain death appears likely, a frank discussion
with family members usually is indicated. It should be recog-
nized that spinal reflexes and even myoclonus may persist in
the brain-dead patient and can be misunderstood both by
medical personnel and by family members. Declaration of
brain death requires the demonstration of irreversible loss of
both brain stem and cerebral function and should be done in
consultation with a neurologist. Permanent loss of cerebral
function with preservation of brain stem function is termed
the chronic vegetative state, and current practice requires that
such patients be given appropriate supportive care.
Treatment
The first step in the management of a patient in coma is to
secure the airway and ensure adequate oxygenation. This
may require intubation. Furthermore, intubation should be
considered when control of Pa
CO
2
is necessary. Hypercapnia
causes cerebral vasodilation, and hypocapnia causes vaso-
constriction; the former can increase intracranial pressure,
and the latter can reduce it. In addition, aspiration is a com-
mon problem in the patient with altered consciousness and
another reason to consider intubation.
Just as important in the management of coma is the quick
assessment and control of the circulatory system. Even in
patients with initially normal blood pressures, sudden loss of
systemic perfusion can occur and can lead to irreversible brain
injury. Therefore, a large-bore intravenous catheter should be
placed in all comatose patients so that circulatory access is
assured. Following this and when dealing with an unknown
cause, 100 mg thiamine and then a bolus of dextrose should be
administered as treatment for potential cases of Wernicke’s
encephalopathy or hypoglycemia. In many patients with brain
lesions and increased intracranial pressure, reflex systemic
hypertension occurs. In the case of cerebellar or ventricular
mass lesions, focal findings may be subtle or even absent and
can lead to the incorrect assumption that the coma is due to
hypertension and the primary problem ignored. Unexpected
herniation can occur in such patients. Irrespective of the cause
of increased intracranial pressure, lowering of systemic blood
pressure could result in loss of cerebral perfusion.
Once respiration and circulation are maintained, the
focus is on treatment appropriate to the diagnosis. The next
chapter outlines the management of coma owing to
increased intracranial pressure. Many metabolic causes of
coma such as hypernatremia, hyponatremia, hyperglycemia,
and hepatic encephalopathy have protocols that demand
meticulously organized treatments that often require days.
Similarly, drug-induced comas may require specific treat-
ment. In coma owing to barbiturate or benzodiazepine tox-
icity, simply maintaining respiratory and circulatory
support until the drug is cleared will be sufficient, whereas
other poisons may require administration of specific anti-
dotes (see Chapter 37).
SEIZURES
All physicians in critical care medicine on occasion will have
to manage seizures, which may be seen as the patient’s pri-
mary problem or as a problem complicating other illnesses.
Prompt recognition and treatment of seizures are important
because prolonged or frequently repeated generalized
seizures may lead to permanent brain injury.
The basic functional property of neurons is electrochem-
ical, and the basic disturbance of this property that underlies
all seizures is termed the paroxysmal depolarization shift. The
various lesions that produce seizures result in a paroxysmal
production of synaptic potentials, which brings neurons
above their threshold and causes repetitive action potentials.
Thus the electrochemical disturbance is propagated, and
clinical seizures result.
Seizures may occur as a result of substrate deprivation,
synaptic dysfunction, or brain injury or as a manifestation of
primary generalized epilepsy. The brain depends on two
major substrates—oxygen and glucose—and deprivation of
either may result in seizures. Similarly, sodium is required to
maintain the electrochemical property of neurons, and
extreme changes in sodium concentration also can lead to
seizures. In general, the magnitude of hypoglycemia,
hypoxia, and hyponatremia must be great enough to result in
alteration of consciousness, following which seizures occur.
Similarly, various toxic insults can result in seizures by alter-
ing synaptic function.
Direct brain injury may cause seizures, both acutely and in
delayed fashion. In acute head injury, mechanical factors
probably disturb membrane function, and the resulting
seizures are seen within minutes to hours following the
trauma. These seizures may be limited and do not typically
recur. Brain injury from laceration in open head wounds or
direct tissue damage in closed head injury may result in post-
traumatic seizures. Pathologically, this occurs after healing
and gliosis have taken place at the injured site. Typically, these
seizures begin a few months to a year following trauma. The
precise nature of this “ripening” process is unclear, but den-
dritic abnormalities have been observed on surviving neurons
in the areas of gliosis. Direct electric shock also can cause
seizures and is a classic method for testing the effectiveness of
proposed anticonvulsant medications in animal models.
Finally, a common cause of seizures is primary generalized
epilepsy. The precise pathophysiologic mechanisms are
unknown, but most investigators believe the disturbance
probably is related to ion channel, neurotransmitter, and
CRITICAL CARE OF NEUROLOGIC DISEASE
663
synaptic dysfunction. Potential insights into the pathophysiol-
ogy of primary generalized epilepsy are provided by the pro-
posed mechanism of action of anticonvulsant medications.
For example, phenytoin and carbamazepine are thought to act
at sodium channels, whereas valproic acid is thought to act at
sodium and calcium channels. In addition, a great deal of
investigation with valproic acid concerns its action on γ-
aminobutyric acid (GABA) receptors. Phenobarbital has been
found to block posttetanic potentiation produced by elec-
troshock and also may act at calcium and chloride channels.
Classification of Seizures
Recognition and understanding of the seizure type is the first
step in the evaluation process and serves as a guide for
workup and management. The types of seizures are summa-
rized in Table 30–4.
A. Partial Seizures—Partial seizures are those that arise
from a focal area of the cortex. The clinical nature of the
seizure is dictated by the functional specialization of the cor-
tical area from which it arises. Focal motor seizures are a
good example. Note that a seizure is an activation of function
and not a loss of function, as occurs in a transient ischemic
attack. Partial seizures that are limited and not associated
with alteration of consciousness are termed simple partial
seizures. Impairment of consciousness coupled with a partial
seizure is called a complex partial seizure.
Complex partial seizures generally arise from the tempo-
ral lobe or other limbic structures. At the onset of this type
of seizure, the patient commonly experiences some auto-
nomic or emotional symptoms, such as a feeling of fear, asso-
ciated with a rising or breathless sensation within the chest
or a sense of being startled. Abdominal sensations are
reported commonly. The patient may experience other phe-
nomena such as déjà vu or may experience visual or olfactory
hallucinations. These altered perceptions tend to be stereo-
typed from seizure to seizure in any given patient and are
usually brief in duration. Following this type of onset, the
patient has an alteration of consciousness and usually has lit-
tle memory of what occurs until the seizure is completed.
To an observer, the onset of a complex partial seizure may
appear only as a motionless stare. After the onset, the patient
may develop some type of automatic and repetitive move-
ments. Examples are lip smacking or movements of one or
both extremities or repetitive picking at some part of the
body or a piece of clothing. During this time, the patient is
poorly responsive to the environment but still may have
some limited interaction. The patient then seems to recover
but remains confused for variable periods, usually only a few
minutes. Most seizures last from a few minutes to about
15 minutes. In repetitive, frequent complex partial seizures,
the patient seems to be in a twilight state, awake yet poorly
responsive to the examiner and the environment.
B. Generalized Tonic-Clonic Seizures—These were at one
time called grand mal seizures. Such seizures are sometimes
preceded by a cry. They are always accompanied by loss of
consciousness, but the tonic and clonic phases are variable.
The tonic phase usually precedes the clonic phase, and all the
extremities are involved in both phases. During the tonic
phase, there is expression of extensor motor dysfunction,
whereas throughout the rhythmic clonic phase, there is flexor
motor predominance. The duration of a single generalized
seizure is measured in minutes, and there always will be a
period of postictal confusion that is likewise usually brief.
Generalized tonic-clonic seizures may develop as a conse-
quence of spread from a partial seizure; in this instance, it
would be designated as secondarily generalized. Tonic-clonic
seizures, generalized at onset, may be caused by metabolic
abnormalities, drug withdrawals, poisons, or other patho-
logic states that affect overall brain function. Primary gener-
alized epilepsy is a major cause of generalized tonic-clonic
seizures. However, the essential pathogenesis of primary gen-
eralized epilepsy is poorly understood. In general, the pri-
mary generalized epilepsies (both generalized and absence)
have their onset in childhood.
C. Absence Seizures—Typical absence seizures were for-
merly called petit mal seizures. They are due to another type
of primary generalized epilepsy and always begin abruptly
with the patient losing cognitive contact. There may be some
fluttering of the eyelids, but body tone is maintained, and the
patient does not fall. Typically, after a few moments (occa-
sionally up to 1 minute or longer), the patient abruptly
regains awareness and will continue the interrupted activity.
Some patients recognize that the period of absence has
occurred, but others do not. This type of seizure is not asso-
ciated with a postictal state. The EEG shows generalized three
per second spike-and-wave discharges during the seizure.
Characteristically, the discharges are provoked by hyperven-
tilation. Absence seizures can be very frequent and pro-
longed—a condition referred to as absence status.
D. Status Epilepticus—Status epilepticus exists whenever
seizures are persistent or there is incomplete recovery
between seizures. Generalized tonic-clonic status epilepticus
is a medical emergency. The consequences of status can
Simple partial (focal seizure with preservation of consciousness)
Complex partial (focal seizure with alteration of consciousness)
Secondarily generalized tonic-clonic
Primarily generalized tonic-clonic (grand mal)
Absence (petit mal)
Status epilepticus
Convulsive tonic-clonic
Nonconvulsive
Absence
Partial (epilepsia partialis continua)
Table 30–4. Classification of seizures.

CHAPTER 30
664
include aspiration pneumonia, hypoxia, hypotension, hyper-
thermia, autonomic instability with cardiac arrhythmias,
hyperkalemia, lactic acidosis, myoglobinuria, decreased
cerebral perfusion, and death. Furthermore, prolonged gen-
eralized tonic-clonic seizures can result in permanent neu-
ronal injury, particularly in the hippocampus, cerebellum,
and neocortex.
In nonconvulsive status, the patient has impairment or
loss of consciousness without generalized motor seizures.
Nonconvulsive status can be quite subtle and difficult to rec-
ognize in the critical care setting. The patient may show an
occasional twitch of an extremity or a facial twitch.
Sometimes the only evidence for seizure activity involves eye
movements, which can be observed only by lifting the eye-
lids. Nonconvulsive status of this type often is associated
with significant metabolic encephalopathy and sometimes
with underlying structural brain disease. Electroence-
phalography is required for diagnosis.
Another type of generalized nonconvulsive status is
absence status, also called spike-wave status. Absence status
most often occurs in children who have generalized epilepsy.
In adults it is rare, but it may occur suddenly in elderly
patients and present as a confusional state with minor
automatisms such as eye blinking or facial twitching.
Status epilepticus also can occur with partial seizures.
This has been called epilepsia partialis continua, and focal
motor seizures are the type most apt to be seen by the criti-
cal care physician. Complex partial status presents with a
patient in a confusional state, often with various automa-
tisms as described previously.
Clinical Features
A. History and Examination—The history is critical in the
diagnosis of seizures, and a comprehensive review of the his-
tory and the hospital course is required. Patients may
describe their symptoms, particularly in the case of complex
partial seizures; however, many patients are unaware of activ-
ity during the episode because consciousness has been
impaired. In fact, patients are sometimes even unaware that
they have had a lapse of consciousness. Thus it is important
to obtain a history from the patient and from witnesses such
as nurses, other patients in the room, family members, or
other attending physicians. Neurologic examination should
be directed toward signs of metabolic encephalopathy,
increased intracranial pressure, and lateralized findings
indicative of focal brain disease. An EEG may help to clarify
the nature of the seizure, particularly if it is obtained during
or soon after the seizure activity. Unless an obvious cause for
a seizure is known (eg, medication noncompliance in a
patient who has a known and previously evaluated seizure
disorder), brain imaging is necessary to see if structural brain
disease is present. If an infectious cause is suspected and there
is no contraindication owing to intracranial mass effect, lum-
bar puncture should be performed to obtain CSF for exami-
nation. If mass effect is present, neurosurgical consultation
should be obtained.
With new-onset seizures in the critical care setting, a use-
ful approach is to consider reversible causes first. In most
instances, these seizures will be generalized, tonic-clonic in
nature. Hypoxic-ischemic events are a common cause of
such seizures. The magnitude and duration of brain oxygen
deprivation will determine the severity of the seizure, as well
as the ultimate outcome. A brief seizure or several brief
seizures with rapid resolution may require no anticonvulsant
therapy. If the hypoxia-ischemia is severe, the seizures may be
prolonged and difficult to treat, and hypoxia-ischemia also
may be a cause of nonconvulsive status epilepticus.
The most common causes of drug-withdrawal seizures are
ethanol, barbiturates, and opioids. Ethanol-withdrawal seizures
usually occur after 24–72 hours of abstinence and rarely lead to
status epilepticus unless there are other underlying diseases.
Theophylline is probably the most common pharmacologic
cause of seizures in the ICU. Lithium toxicity may cause an
encephalopathy that may include seizures. Penicillin toxicity
causes seizures but is a rare occurrence usually associated with
kidney failure. A more common metabolic cause of seizures is
hyponatremia, which often is associated with inappropriate
antiduretic hormone secretion, and/or fluid overload.
Seizures occurring with acute neurologic disease often are
partial, or partial with secondary generalization, and the par-
tial onset may not be clinically apparent. Herpes simplex
encephalitis tends to be focal, whereas encephalitis from
other causes is more generalized. Electroencephalography
and imaging studies are helpful in the differential diagnosis.
Seizures usually do not occur with uncomplicated meningi-
tis. If they occur in bacterial meningitis, one should suspect
a complicating cortical venous thrombosis. Brain abscesses
commonly cause seizures.
The EEG is very useful in critical care neurology. To obtain
the maximum information from the EEG, the clinician
should provide the electroencephalographer with a brief his-
tory that includes the patient’s age, a description of the level
of consciousness, and a list of the medications being admin-
istered. One syndrome that can be defined with the EEG is
called periodic lateralized epileptiform discharges (PLEDs).
Affected patients are stuporous or comatose, may have occa-
sional epileptiform twitching movements of one side of the
face, and show the characteristic lateralized epileptiform dis-
charges. PLEDs usually are associated with some underlying
structural brain disease, such as an old infarct, and a superim-
posed metabolic encephalopathy. In general, the prognosis is
hopeful with correction of the metabolic disturbance and,
usually, administration of anticonvulsant medication.
In the case of seizures, the EEG can be diagnostic if
obtained during the seizure, but also it may show interictal
discharges and abnormalities supportive of the diagnosis and
indicate any focal aspect. Sometimes it is helpful to employ
closed-circuit TV, together with an electroencephalographic
monitoring system, to fully evaluate the seizure as well as the
progress of therapy. The EEG also is helpful in establishing
the diagnosis of a generalized toxic-metabolic encephalopathy
whether or not seizures are present.
CRITICAL CARE OF NEUROLOGIC DISEASE
665
Differential Diagnosis
Seizures may be associated with many different pathologic
states, including structural disease owing to neoplasms, vas-
cular anomalies, old strokes, and past trauma, or metabolic
encephalopathies. Other common problems leading to
seizures include poisoning, drug withdrawal, infections such
as viral encephalitis, and primary generalized epilepsies. Poor
compliance with the anticonvulsant regimen is a common
reason for a patient with epilepsy to develop status epilepti-
cus as well as to have poor seizure control. Drug level moni-
toring in these patients is essential.
Partial seizures of any type imply an underlying struc-
tural brain disease. Likewise, a postictal paresis (Todd’s pare-
sis) implies underlying focal disease.
Treatment
The management of seizures in critical care practice requires
first the removal or correction of precipitating causes and sec-
ond the administration of anticonvulsant medication. Often
it will seem prudent to administer anticonvulsant medication
on a temporary basis while causative conditions are resolving.
Whether anticonvulsants are administered orally or intra-
venously, it is critical to monitor serum concentrations to
ensure a therapeutic range. Phenytoin (fosphenytoin IV
preparation fully converted to phenytoin after injection),
phenobarbital, and valproate can be administered either
intravenously or orally. Lorazepam and diazepam are useful
anticonvulsants only when given intravenously.
Table 30–5 lists the doses and average half-lives of these
anticonvulsant medicines administered intravenously. Since
these half-lives are variable, the information provides an
approximation of the duration of action.
The major limiting factor for diazepam is that it peaks
into the therapeutic range for only a brief time; seizures may
recur 15–20 minutes after it is given. On the other hand, it is
rapidly effective. There may be some risk of apnea when
diazepam and phenobarbital are given together. Lorazepam
also is rapidly effective and has a longer duration of action.
The dose of lorazepam is usually 2–10 mg, or 0.1 mg/kg. It
can be administered in 2-mg increments at intervals of a few
minutes until the seizures are controlled or the maximum
dose is reached.
Both fosphenytoin or phenytoin and phenobarbital are
effective anticonvulsants, although their onset of action may
be slower than that of the benzodiazepines. Phenytoin, phe-
nobarbital, and valproate can be continued orally. Phenytoin
must be administered at a rate no faster than 50 mg/min
because of the risk of cardiac arrhythmia. Electrocardiographic
monitoring is advised while phenytoin is given. Phenytoin
should not be mixed in a dextrose solution because it will pre-
cipitate. The initial intravenous dose is 18–20 mg/kg of body
weight; the maximum dose is 30 mg/kg. Fosphenytoin is
dosed in phenytoin equivalents (PEs); it can be mixed in nor-
mal saline or a 5% dextrose solution and infused at a rate up
to 150 mg PE per minute. Extravasated phenytoin solution
often is harmful to surrounding tissues, whereas extravasated
fosphenytoin usually results in no tissue damage.
The intravenous dose of phenobarbital is 300–1000 mg
(or 15–20 mg/kg) for seizure control. Usually it is supplied
in 60-mg units, so an initial dose of 300 mg is convenient and
can be repeated every 10–20 minutes until seizure control
occurs or the maximum dose is reached.
Valproate sodium injection is a broad-spectrum anticon-
vulsant; it has complete bioequivalence with oral valproate and
may be mixed in normal saline or 5% dextrose solution. The
recommended infusion rate is up to 20 mg/min. Valproate is
the drug of choice for absence seizures. Intravenous valproate,
lorazepam, and diazepam are effective in absence status.
Levetiracetam also is available as an intravenous solution
as well as an oral preparation. It is approved as adjunctive ther-
apy in the treatment of partial-onset seizures in adults when
oral administration is not feasible. The intravenous dose is
equivalent to the oral dose (1000–3000 mg/day given twice daily)
and is supplied in 500-mg/5-mL vials. It should be diluted in
100 mL normal saline and infused over 15 minutes.
Levetiracetam is 66% excreted unchanged in the urine and has
no metabolism involving hepatic cytochrome P450 isoenzymes.
Seizures from metabolic encephalopathies, nonconvul-
sive status, and PLEDs often do not respond fully and quickly
to anticonvulsive medications. In this circumstance, it is best
to maintain therapeutic anticonvulsant blood concentrations
while pursuing therapy of underlying diseases. Partial
seizures or partial status likewise may be resistant to treat-
ment. In such cases, two anticonvulsant drugs can be tried,
but it is best to maintain them in the usual therapeutic range
and determine if with time there is greater benefit.
Generalized tonic-clonic status epilepticus does consti-
tute an emergency and must be controlled. Ventilation and
cardiac function must be supported. If hypoglycemia is a
consideration, 50 mL of a 50% dextrose solution should be
Drug Average Half-Life Dose
∗
Diazepam 1 hour 10–30 mg
Lorazepam 3 hours 2–10 mg
Phenytoin 12 hours 18–20 mg/kg
Fosphenytoin
12 hours
†
20 mg phenytoin
equivalents (PE)/kg
Phenobarbital 99 hours 15–20 mg/kg
Valproate sodium
injection
‡
10 hours 250–500 mg
∗
Status epilepticus or loading.
†
Converted to phenytoin in 10–15 minutes.
‡
T
MAX
= 1 hour.
Table 30–5. Intravenous anticonvulsants.
CHAPTER 30
666
administered promptly. If there is any possibility that the
patient is an alcoholic, dextrose should be preceded by
100 mg thiamine to prevent Wernicke’s encephalopathy.
Anticonvulsant medication for status epilepticus always
must be administered intravenously and be given in full
loading doses. A common mistake is to give inadequate
amounts of several different drugs.
If generalized tonic-clonic seizures persist despite the
patient’s being given intravenous anticonvulsants, pentobar-
bital anesthesia is recommended. This should be accomplished
with neurologic consultation and under electroencephalo-
graphic control. Pentobarbital is given in a dosage of 5 mg/kg
for induction of anesthesia and 0.5–2 mg/kg per hour for
maintenance. The drug is administered so as to titrate the EEG
to a burst-suppression pattern. When it is judged that an
appropriate interval of time has lapsed (about 24–48 hours),
the pentobarbital dose may be reduced to test for seizure
recurrence. If the seizures are controlled, the pentobarbital
may be withdrawn, but therapeutic levels of an anticonvulsant
such as phenytoin must be present and maintained.
Current Controversies and Unresolved Issues
Resistant partial or lateralized seizures and nonconvulsive
generalized status epilepticus remain problems in manage-
ment, and there is some uncertainty about how vigorous the
physician should be in the administration of medications.
No absolute indication exists for the choice of first med-
ication to treat generalized tonic-clonic status; rather, it is a
matter of common practice and personal choice.
In the past few years, the number of oral antiepileptic drugs
available has increased dramatically, and experience with them
in daily practice is accumulating but is not yet great. Use of
these drugs, as well as other treatments, including surgical and
vagus nerve stimulation, and the management of chronic
seizure disorders are mostly beyond the scope of critical care
practice. Neurology consultation is recommended when newly
prescribing or switching oral antiepileptic medicine.
NEUROMUSCULAR DISORDERS
Respiratory failure and cardiac failure are the most serious
potential complications of neuromuscular diseases and can
lead to death if not treated appropriately. Diseases directly
affecting respiration include Guillain-Barré syndrome,
myasthenia gravis, amyotrophic lateral sclerosis, and
Duchenne’s muscular dystrophy. Less commonly, botulism,
tetanus, porphyria, and diphtheritic polyneuropathy cause
neuromuscular failure. Similarly, a number of neuronal poi-
sons can lead to severe weakness and even respiratory fail-
ure. Chronic neuromuscular diseases can lead to secondary
pulmonary problems, including phrenic nerve injury,
kyphoscoliosis, pulmonary emboli, atelectasis, and most fre-
quently, aspiration pneumonia. Another potential problem
associated with neuromuscular diseases involves cardiac
complications such as arrhythmias, as seen in Guillain-Barré
syndrome, or conduction blocks with sudden death, as seen
in myotonic dystrophy. Advances in the ICU treatment of
these patients have decreased morbidity and mortality rates,
avoiding sudden death in some instances.
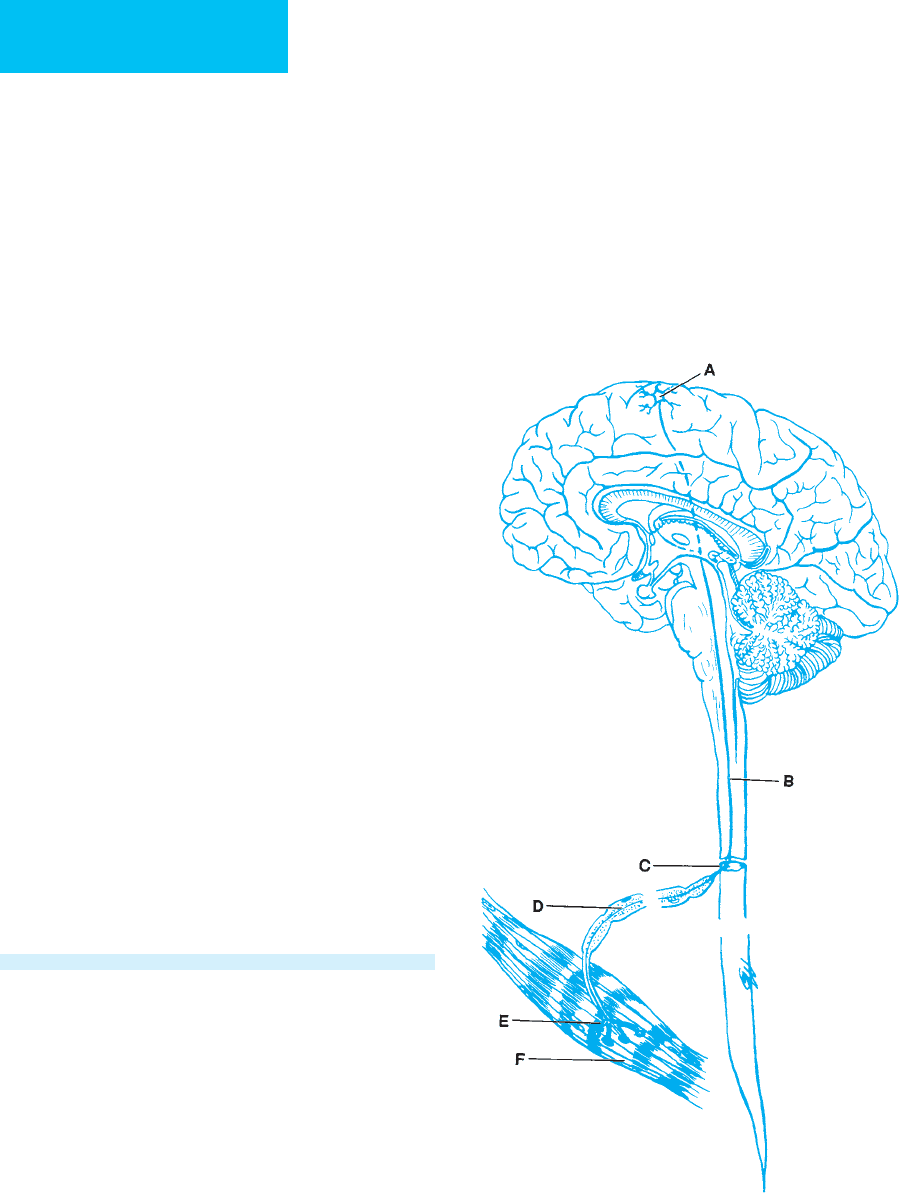
Pathophysiology
Progressive weakness may result from disorders anywhere
along the motor tract (Figure 30–1). Lesions in the brain,
particularly the upper motor neuron pathways (site A) or
Figure 30–1. Localization of lesions causing neuro-
muscular diseases. A. Cortex (upper motor neuron).
B. Spinal cord. C. Anterior horn cell. D. Peripheral nerve
(axon or myelin). E. Neuromuscular junction. F. Muscle.
