Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

CRITICAL CARE OF NEUROLOGIC DISEASE
667
brain stem (site B), may lead to progressive weakness.
Likewise, disorders at the level of the spinal cord or the lower
motor neurons (site C), either at the anterior horn cell bod-
ies, motor axons, or myelin (site D) or at the pre- or postsy-
naptic terminals (site E), may lead to weakness. Furthermore,
many of the muscle diseases (site F) can directly impair effec-
tive ventilation. Table 30–6 lists some examples of diseases
that can occur at each site.
One general rule associated with respiratory failure sec-
ondary to neuromuscular disorders is that unlike primary
pulmonary illnesses, where dysfunction in gas exchange
often results predominantly in hypoxemia, respiratory failure
secondary to neuromuscular dysfunction usually leads to
hypoventilation. Arterial blood gases often demonstrate CO
2
retention, or hypercapnia, with relatively mild hypoxemia.
By the time Pa
CO
2
begins to increase, hypoventilation has
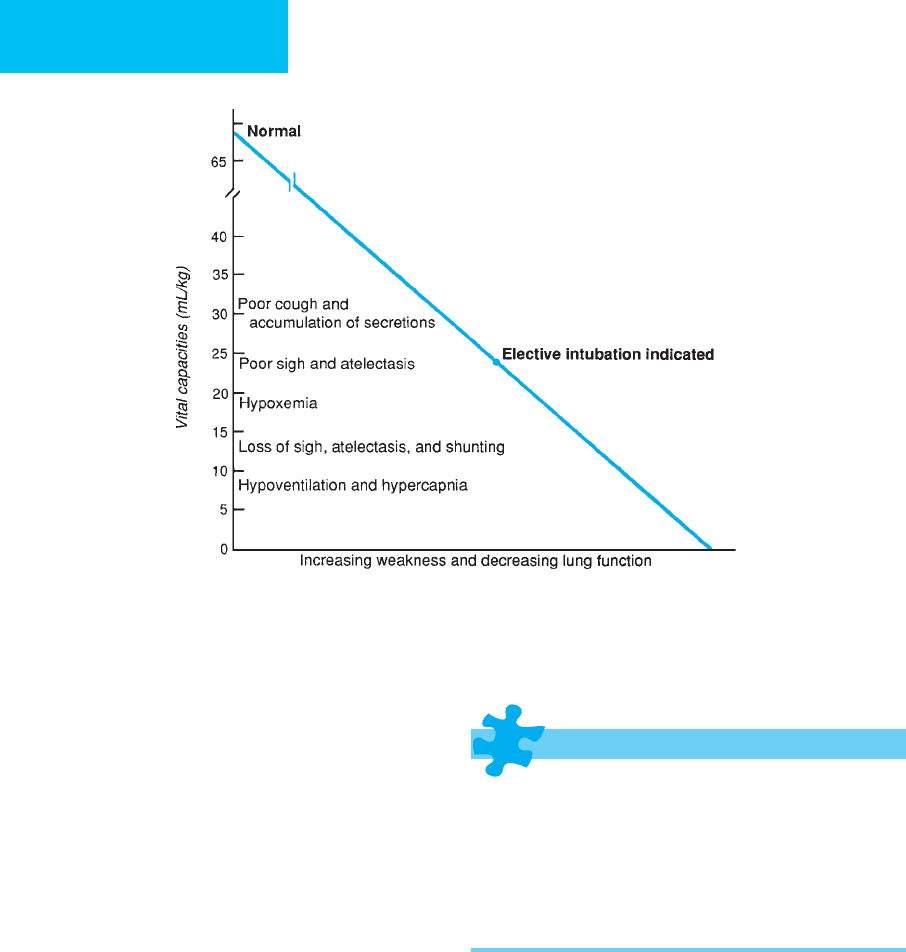
gone beyond the safe limit. Decrease in vital capacity is asso-
ciated with predictable signs of pulmonary dysfunction
(Figure 30–2). Therefore, the single most important param-
eter to measure in patients with neuromuscular diseases is
the vital capacity.
In order to make an etiologic diagnosis of neuromuscu-
lar disease leading to weakness and respiratory failure, spe-
cific clinical symptoms and signs as well as laboratory
diagnostic studies are used to localize the lesions.
Measurements of vital capacity and cardiac monitoring are
essential in patients admitted to the ICU owing to exacer-
bation of neuromuscular diseases because respiratory
compromise and cardiac arrhythmias can develop rapidly.
The clinical presentation of the illness depends on the site
of the lesion.
Spinal Cord Compression
ESSENTIALS OF DIAGNOSIS
Back pain, limb paresis, and spasticity.
Sensory loss below the level of the spinal cord lesion.
Bowel or bladder incontinence.
Neuroimaging studies of the clinically suspected spinal
levels.
Blood cultures and purified protein derivative (PPD) test
if an abscess is suspected.
Biopsies to evaluate tumors and abscesses.
General Considerations
Back pain can be caused by a variety of diseases, such as local
structural disorders, retroperitoneal disease, trauma, infec-
tion, and neoplasms. However, tumors, abscesses, or disk
fragments in the spinal canal may produce an acute syn-
drome of spinal cord compression. This is a neurologic
emergency that may lead to permanent paralysis if not
treated rapidly. Diagnostic signs or symptoms vary depend-
ing on the spinal level of the compression.
Intra- and extramedullary spinal cord malignancies, as
well as various infections with parasitic (eg, cysticercosis),
bacterial (eg, anaerobes, tuberculomas, and gummas), or
viral (eg, varicella-zoster or poliomyelitis) organisms, may
produce direct or compressive lesions to the spinal cord.
Most abscesses are in the thoracic or lumbar areas, and the
agent is usually Staphylococcus aureus. Tuberculosis also may
infect the vertebral column (Pott’s disease), causing kyphosis,
Motor cortex and pyramidal tract
Amyotrophic lateral sclerosis
Brain stem
Progressive bulbar palsy
Spinal cord and lower motor neuron
Spinal muscular atrophies
Amyotrophic lateral sclerosis
Poliomyelitis
Toxins: mercury
Infections: tetanus, spinal cord and epidural abscesses
Peripheral neuropathies
Axonal types (including critical illness polyneuropathy)
Diabetes
Alcohol-related
Uremia
Hypothyroidism
Sarcoidosis
Collagen-vascular diseases
Paraproteinemias
Drugs
Heavy metals
Industrial toxins
Amyloidosis
Carcinoma (remote effect)
Tick paralysis
Demyelinating neuropathies
Guillain-Barré syndrome
Diphtheria
Porphyria
Hereditary: Charcot-Marie-Tooth disease
Neuromuscular junction disorders
Myasthenia gravis
Botulism
Eaton-Lambert syndrome
Pseudocholinesterase deficiency
Organophosphate intoxication
Other drugs and toxins: neomycin, penicillamine
Disease of muscles
Muscular dystrophies
Inflammatory myopathies
Endocrine and metabolic myopathies
Toxic myopathies: alcohol, carbon monoxide
Inherited metabolic myopathies: periodic paralysis; glycogen or lipid
enzymatic defect
Neuroleptic malignant syndrome, malignant hyperthermia
Table 30–6. Neuromuscular diseases affecting respiration.
CHAPTER 30
668
which then may cause cord compression or respiratory
difficulties.
Clinical Features
A. Symptoms and Signs—Diagnosis of a spinal cord
lesion depends on clinical examination and neuroimaging
studies. Limb weakness and the presence of a sensory level
(particularly to pinprick and vibratory senses) are useful in
approximating the level of involvement. Tendon reflexes
below the level of the lesion may be increased, and
Babinski signs may be present. Fever associated with back
pain and myelophthisic signs should arouse suspicion of
epidural abscess.
B. Laboratory Findings—When an infectious cause is sus-
pected, blood cultures and a tuberculin test will help to direct
specific antibiotic therapies. Biopsy examination is indicated
for suspected tumor or abscess.
C. Imaging Studies—MRI or CT scan is necessary to accu-
rately localize the lesion.
Treatment
Early recognition and treatment can prevent irreversible
neurologic damage. Tumors generally respond to surgical
removal or radiotherapy. High-dose corticosteroid therapy
also may be indicated. Selection of antibiotic therapy for
epidural abscess depends on biopsy or culture results.
Guillain-Barré Syndrome
ESSENTIALS OF DIAGNOSIS
Antecedent flulike illness.
Acute or subacute ascending flaccid paralysis.
Early loss of tendon reflexes.
Subjective distal paresthesias and pain.
Occasional cranial nerve deficits.
Elevated protein in CSF with no cells.
General Considerations
Guillain-Barré syndrome is an acute or subacute prima-
rily motor polyneuropathy that is usually idiopathic,
although a number of etiologic factors, including
Mycoplasma pneumoniae and hepatitis B, have been
implicated in rare cases. In more than 50% of patients
with Guillain-Barré syndrome, an antecedent flulike ill-
ness or vaccination occurred within 4 weeks prior to the
neurologic symptoms.
Acute or subacute ascending muscle weakness develops
over 2–4 weeks, followed by gradual recovery over a few
weeks to many months. Eighty-five percent of patients will
have complete functional recovery.
Figure 30–2. Effects of decreasing vital capacities secondary to weakness from neuromuscular diseases.
CRITICAL CARE OF NEUROLOGIC DISEASE
669
Clinical Features
A. Symptoms and Signs—Cranial nerve deficits, especially
of those controlling eye movements and facial muscles, can be
present either alone or associated with limb weakness. Deep
tendon reflexes are absent, whereas pupils and eyelids often
are spared. Miller-Fisher syndrome is a variant of Guillain-
Barré syndrome characterized by absent reflexes, gait ataxia,
and ophthalmoparesis. The prognosis for complete recovery
of this form of Guillain-Barré syndrome is excellent.
B. Laboratory Findings—Lumbar puncture can be diagnostic
by the second week, when CSF shows an elevated protein con-
centration without pleocytosis (albuminocytologic dissociation).
C. Nerve Conduction Studies—Nerve conduction studies
show segmental demyelination and reduction of velocity in
85–90% of patients by the second week. Up to 40% of
patients develop respiratory muscle weakness and/or auto-
nomic instability. Therefore, ICU admission is best for most
patients, and frequent vital capacity measurements and car-
diac monitoring are necessary for timely detection of these
complications.
Treatment
A. Respiratory Care—Respiratory weakness requiring ven-
tilatory support develops in 40% of patients and may be rap-
idly progressive in the early phases. Intubation may be
required. Bulbar muscle weakness can lead to aspiration
pneumonia, which is potentially preventable by placement of
a nasogastric tube, as well as by intubation.
B. Cardiac Care—In up to 40% of patients with Guillain-
Barré syndrome, autonomic dysfunction may occur and
accounts for much of the morbidity and most of the deaths
in this group of patients. The cardiac abnormalities fre-
quently include sinus tachycardia, and asystole can occur.
Therefore, it is essential to maintain cardiac monitoring and
to administer antiarrhythmic drugs as necessary.
C. Other Treatment—When the weakness is progressive and
severe, plasmapheresis or intravenous immune globulin
(IGIV) is recommended. Because most of these patients expe-
rience a significant amount of pain (which may be difficult to
recognize when the patient is intubated), use of opioids as
needed is indicated.
Critical Illness Polyneuropathy
ESSENTIALS OF DIAGNOSIS
Associated with multiorgan failure, often with sepsis.
Difficulty weaning from respirator owing to weakness.
Distal limb weakness with diminished or absent reflexes.
EMG nerve conduction studies characteristic.
General Considerations
Critical illness polyneuropathy has been recognized in asso-
ciation with sepsis and multiorgan failure in the ICU setting.
Sometimes it is first identified because of difficulty weaning
a patient from the ventilator owing to respiratory muscle
weakness. It is an axonal sensorimotor polyneuropathy of
obscure origin; there is no inflammation or demyelination of
the nerves.
Clinical Features
A. Symptoms and Signs—The typical findings on exami-
nation are distal limb weakness with flaccidity and hypore-
flexia or areflexia as well as respiratory muscle weakness or
even quadriplegia in severe cases. Mild facial weakness some-
times occurs, but ophthalmoparesis is uncommon. Distal
sensory loss may be expected, but under the usual circum-
stances of this condition, sensory deficits are difficult or
impossible to assess accurately. Superimposed entrapment or
compression neuropathies, because of positioning problems,
should be considered in the differential diagnosis. Also to be
differentiated is critical illness myopathy, which is a syndrome
of weakness that develops in some critically ill patients after
the use of corticosteroids, often in combination with neuro-
muscular blocking agents. Creatine kinase usually is elevated,
many times to very high levels, and can be associated with
rhabdomyolysis and myoglobinuria. Another condition to be
differentiated is prolonged neuromuscular blockade, which
may occur in critically ill patients after neuromuscular block-
ing agents have been discontinued; the duration can range
from hours to days.
B. Laboratory Findings—Electromyographic and nerve
conduction studies show reduced motor and sensory ampli-
tudes but preserved conduction velocities and distal laten-
cies. This is distinguished from Guillain-Barré syndrome, in
which conduction block and segmental slowing are found.
The CSF protein is normal in critical illness polyneuropathy.
Treatment
Treatment consists of correction and management of under-
lying illnesses. The neuropathy often improves after weeks or
months as sepsis and organ failure resolve. Patients who have
mild or moderate neuropathy may have complete recovery,
whereas those severely affected probably will have residual
and permanent weakness. It is prudent to minimize the use
of neuromuscular blocking agents, especially in patients who
are receiving corticosteroids.
Toxic Neuropathies
There are three anatomic locations where toxins can affect
the peripheral nerve: the cell body, the nerve sheath myelin,
and the axon. Diphtheria toxin, tetanus toxoid, and antibiotic
treatments may lead to acute sensory neuropathy secondary
to myelin loss, whereas the most common toxic neuropathies

CHAPTER 30
670
result in axonal injuries. Many drugs and industrial chemi-
cals can be neurotoxic. Examples of such drugs are isoniazid,
chloramphenicol, metronidazole, disulfiram, amiodarone,
gold, cisplatin, vincristine, lithium, nitrofurantoin, nitrous
oxide, and pyridoxine.
Exposure to industrial chemicals such as arsenic, acry-
lamide, carbon disulfide, mercury, the organophosphate
parathion, and vinyl chloride can cause distal axonal neu-
ropathy. The clinical course depends on the concentration of
the offending agent. Chronic exposure to these agents leads
to an insidious onset of paresthesia in glove-stocking distri-
bution. With more acute exposure, patients develop other
systemic signs along with a more rapid onset of neuropathy.
Two important ubiquitous toxins, lead and arsenic, both
have characteristic clinical presentations.
Lead Poisoning
Lead poisoning can occur via the GI tract, lungs, or skin and
is associated with abdominal cramps and encephalopathy
(particularly in infants). Blood smears show basophilic stip-
pling in the erythrocytes. The elevated lead level can be
measured in serum. Although other nerves may be affected,
lead has a peculiar predilection for radial nerves, resulting in
weakness of wrist and finger extension. Sensory symptoms
are unusual.
Arsenic Poisoning
Arsenic poisoning often results from accidental ingestion of
rat poisons or industrial sprays, although intentional poison-
ings do occur. These patients often develop an acute
polyneuropathy several weeks after exposure. The nail beds
show pale bands called Mees’s lines. After exposure, urine,
hair, and nails all may contain arsenic. With higher exposure,
a painful sensory neuropathy may evolve to a flaccid paraly-
sis beginning in the lower extremity but eventually affecting
the respiratory muscles and upper extremities.
Urine and serum for a heavy metal screen, along with a
careful drug and toxin exposure history, are mandatory in
any patient presenting with an acute neuropathy. Finally,
nerve conduction studies will help to differentiate demyeli-
nating versus axonal types of neuropathy.
Myasthenia Gravis
ESSENTIALS OF DIAGNOSIS
History of fluctuating weakness and fatigability.
Positive edrophonium (Tensilon) test.
Decremental responses on nerve conduction studies.
Positive serologic tests for acetylcholine receptor
antibodies.
Chest CT scan or MRI may show thymoma.
General Considerations
Myasthenia gravis appears to be an autoimmune disease, pri-
marily a disorder of the postsynaptic neuromuscular junction.
Acetylcholine receptor antibodies are found in 85–90% of
patients. Other immunologic diseases such as thyroid disease,
polymyositis, rheumatoid arthritis, and systemic lupus erythe-
matosus all have been associated with myasthenia gravis.
Repetitive stimulation of a motor nerve at 3 Hz shows a
decremental response of electromyographic motor units in
up to 85% of patients with myasthenia gravis, whereas dis-
eases affecting the presynaptic nerve terminal such as
Lambert-Eaton syndrome or botulism demonstrate an incre-
mental response at a higher rate of stimulation.
Clinical Features
A. Symptoms and Signs—Myasthenia gravis is character-
ized by variable weakness and easy fatigability. The motor
weakness worsens with exercise and improves after rest.
Diplopia often is an early symptom, and over 90% of patients
develop ocular muscle involvement. Patients feel strongest in
the morning and weakest at night because their muscles tire
during the day.
B. Laboratory Findings—The edrophonium test demon-
strates that an increase in peripheral acetylcholine improves
motor function. It is performed as follows: (1) Stop other anti-
cholinesterase medications 24 hours prior to the test if possible.
(2) Atropine sulfate, 0.4 mg (1 mL), which blocks muscarinic
“side effects” of edrophonium but not the nicotinic effect at the
neuromuscular junction, and normal saline (1 mL) are used
first as control injections. (3) Edrophonium should elicit a
response in 30–60 seconds that should last for 10–30 minutes.
Draw up 10 mg and give 2 mg for the first dose; if there is no
response, follow with 8 mg. (4) Assess strength of affected mus-
cles 1–2 minutes after each intravenous dose.
The absence of acetylcholine receptor antibodies does not
exclude the diagnosis, but their presence is confirmatory.
Antistriational antibodies are found in 90% of myasthenic
patients with thymoma.
C. Imaging Studies—Approximately 10% of patients
develop thymoma, and 70% will have thymic hyperplasia.
Therefore, chest CT scan or MRI is performed to search for
mass lesions.
Treatment
A. Oral Therapy—Pyridostigmine often is successful first-
line therapy. The usual initial dose is 30 or 60 mg. The inter-
val of dosing can be adjusted in individual patients
depending on observed duration of action but is usually on
the order of 4 hours. Prednisone and other immunosuppres-
sive drugs also are used in difficult cases.
B. Intravenous Therapy—Plasmapheresis, 2–3 L per
exchange three times a week over 2 weeks, has been successful
CRITICAL CARE OF NEUROLOGIC DISEASE
671
in some patients who do not respond to anticholinesterase
medications. Intravenous immune globulin (IGIV) is an
alternative to plasmapheresis, and both are useful in prepar-
ing patients for thymectomy.
C. Thymectomy—Thymectomy improves long-term out-
come in patients with myasthenia gravis, and all patients
undergoing thymectomy should be monitored carefully pre-
and postoperatively in the ICU under the supervision of a
neurologist. Postoperatively, immunosuppression with high-
dose prednisone is helpful in many patients.
D. Exacerbations—When a myasthenic patient presents
with increased weakness, it is important to differentiate
between myasthenic versus cholinergic crisis. A myasthenic
crisis requires treatment with additional anticholinesterase
medications, whereas weakness owing to cholinergic crisis
only improves if the medication is withheld. An edropho-
nium test may be helpful in differentiating the two. In myas-
thenic crisis, look for causes such as infection (especially
aspiration pneumonia), drugs with a potential for blocking
neuromuscular transmission, and excessive use of sedative
drugs. In general, if vital capacity is less than 1 L, it is best to
intubate and stop all myasthenic medication until the cause
of the exacerbation is determined.
Botulism
ESSENTIALS OF DIAGNOSIS
GI symptoms with dry mouth.
Blurred vision, dilated pupils, and diplopia.
Respiratory distress.
Incremental response with repetitive nerve conduction
studies.
Stool examination positive for Clostridium botulinum
and its exotoxin.
General Considerations
Unlike myasthenia gravis, the neuromuscular junction defect
in botulism results primarily from presynaptic cholinergic
conduction blockade. It is an acute poisoning resulting from
ingestion of C. botulinum exotoxin. The organism is found in
inadequately cooked or defectively canned food. Also, it may
be found in clostridial wound infections, which is a source of
the disease in people injecting illicit drugs. In infants
between the ages of 1 and 38 weeks, the toxin may be found
in the GI tract.
Clinical Features
A. Symptoms and Signs—Symptoms begin within 5–50
hours of eating the contaminated food or exposure to the
toxin. Dry mouth and GI symptoms such as cramps, nausea,
vomiting, and diarrhea or constipation, as well as malaise
and headache, are noted initially. Extraocular muscle weak-
ness and dilated, sluggishly reactive pupils cause diplopia and
blurred vision. These patients may rapidly develop dysphagia
and respiratory distress. Respiratory failure and aspiration
pneumonia may be the principal causes of death from botu-
lism. The nervous system is involved in descending fashion,
beginning with muscles innervated by the cranial nerves.
Consciousness and sensation remain intact, however.
B. Laboratory Findings—Botulinus toxin can be isolated
from infected serum, stool, or contaminated food. Since cul-
tures of the organism or evaluation for the toxin may take
several days, repetitive nerve stimulation should be per-
formed as soon as possible in patients suspected of having
botulism. CSF is normal.
C. Nerve Conduction Studies—Diagnostic studies with
high-rate (40 Hz) repetitive nerve stimulation demonstrate
incremental responses of the compound action potentials in
the motor nerves.
Treatment
A. Antitoxin—Type E antitoxin has the greatest clinical effi-
cacy and should be administered as quickly as possible. The
dose may be repeated in 4 hours if the condition worsens.
Skin testing to exclude hypersensitivity should precede
administration of the antitoxin. One vial of antitoxin should
be given orally and one intravenously.
B. Antibiotics—When botulism occurs from a wound infec-
tion, antibiotic therapy with penicillin, 300,000 units/kg per
day intravenously, is preferred. Other useful drugs are clin-
damycin (30 mg/kg per day intravenously) and chloram-
phenicol (50 mg/kg per day intravenously); guanidine
hydrochloride (50 mg/kg per day orally) may improve mus-
cle function.
Inflammatory Myopathies
Most inflammatory myopathies result from autoimmune
processes, although some result from infections. Typical
examples include dermatomyositis, polymyositis, secondary
involvement with lupus erythematosus, and viral myositis. In
20% of older patients (>50 years), polymyositis and der-
matomyositis may be associated with an occult malignancy.
Myalgia and proximal muscle weakness are the most com-
mon complaints in patients with inflammatory myopathies.
Most forms are self-limited, lasting 2–3 weeks. However, ful-
minant myositis may lead to rhabdomyolysis, which can be
fatal. Occasionally, when the swallowing muscles are involved,
the patient requires nasogastric tube feedings.
Laboratory studies often reveal an elevated creatine
kinase and sedimentation rate. Electromyography shows signs
of muscular irritability with fibrillation potentials and small
polyphasic waveforms—all characteristic of inflammatory
CHAPTER 30
672
myopathies. Perivascular infiltrates and perifascicular atro-
phy are seen in muscle biopsy specimens, and this informa-
tion may be necessary for definitive diagnosis.
Neuroleptic Malignant Syndrome
ESSENTIALS OF DIAGNOSIS
Encephalopathy.
Markedly elevated core temperature.
Autonomic dysfunction.
“Lead pipe” muscular rigidity with elevated creatine kinase
General Considerations
Neuroleptic malignant syndrome is a life-threatening idio-
syncratic reaction to neuroleptic agents. The drugs that pro-
duce this syndrome typically include phenothiazines,
butyrophenones, and other postsynaptic dopamine blocking
agents. Failure to recognize the syndrome may lead to a rap-
idly fatal course over hours to several days. Even brief expo-
sure to the drug may produce the syndrome.
Clinical Features
A. Symptoms and Signs—The clinical presentation may
be variable but frequently consists of encephalopathy,
markedly elevated core temperature, and muscular rigidity.
Fever and increased muscle activity are the main features.
Mental status changes may vary from confusion or agitation
to coma. Involuntary movements such as tremor or dyskine-
sia occasionally accompany muscular rigidity—so-called
lead pipe rigidity. When severe rigidity occurs, rhabdomyol-
ysis may result and in turn lead to myoglobinuria and acute
renal failure.
B. Laboratory Findings—There is no unequivocal diagnos-
tic test or criterion for neuroleptic malignant syndrome.
Creatine kinase elevations may range from several hundred
to over 10,000 units per liter.
Differential Diagnosis
Many nonneuroleptic drugs can produce similar disorders.
Examples include cocaine, amphetamines, reserpine, meto-
clopramide, and tricyclic antidepressants in combination
with lithium or monoamine oxidase inhibitors. The differen-
tial diagnosis also includes many causes of encephalopathy
and fever, catatonia, and malignant hyperthermia.
Malignant hyperthermia is a genetically determined
hypermetabolic state with onset shortly after the use of cer-
tain anesthetics. Although it is similar to neuroleptic malig-
nant syndrome in the markedly elevated temperature and
creatine kinase concentrations, it can be distinguished by
the lack of encephalopathy or autonomic dysfunction.
Furthermore, the generation of fever is most likely peripheral
in malignant hyperthermia and central in neuroleptic malig-
nant syndrome. The genetic trait for malignant hyperther-
mia does not appear to impose any risks for development of
neuroleptic malignant syndrome.
Treatment
A. General Measures—Effective treatment requires early
recognition and critical care monitoring of possible
multiple-organ failure. Fever must be controlled, and vigor-
ous intravenous hydration is necessary to lower the body
temperature and minimize the effects of possible rhab-
domyolysis. Blood pressure and urinary output must be
monitored carefully. Most important, dopamine-blocking
agents must be discontinued.
B. Drug Therapy—Centrally acting bromocriptine,
7.5–100 mg/day, has been used to control the high tempera-
ture and rigidity; effects may be seen within hours.
Dantrolene, a peripherally acting muscle relaxant, also is
highly effective. It can be given intravenously at a dosage of
0.25 mg/kg twice daily and increased as needed to control the
rigidity. When the patient is able to take oral medications,
25–600 mg/day may be effective.
Muscular Dystrophies
ESSENTIALS OF DIAGNOSIS
Proximal extremity weakness.
Pseudohypertrophy of the gastrocnemius muscles.
Muscle fiber necrosis and minor regeneration on biopsy.
General Considerations
There are a number of inherited muscular diseases that may
have respiratory or cardiac complications that ultimately
require management in the ICU. Duchenne’s muscular dys-
trophy and myotonic dystrophy are the most common dis-
eases of this type.
Muscular dystrophy patients have an increased rate of
adverse reactions to many anesthetics and frequently have
respiratory complications and prolonged postoperative
courses if they undergo general anesthesia. When possible,
surgery or general anesthesia should be avoided in these
patients. In general, sedatives also are contraindicated
because of their adverse effects on weakened muscles.
Clinical Features
A. Symptoms and Signs—Diagnosis of Duchenne’s mus-
cular dystrophy can be made by the family history (X-linked
recessive, but one-third can be spontaneous mutations),

CRITICAL CARE OF NEUROLOGIC DISEASE
673
clinical examination showing characteristic proximal
extremity weakness, and pseudohypertrophy of the gastroc-
nemius muscles by age 3–4.
B. Laboratory Findings—Muscle biopsies demonstrate pro-
gressive muscle fiber necrosis and minor degrees of regenera-
tion. These patients pursue a steady downhill course and
develop lumbar lordosis and scoliosis. Laboratory studies will
show markedly elevated (10–50 times normal) serum creatine
kinase and characteristic abnormalities on electrocardiography,
electromyography, and muscle biopsies. New findings from
molecular genetic studies show absent dystrophin protein in
muscles of patients with Duchenne’s muscular dystrophy,
whereas patients with the Becker variant (clinically similar but
a later age at onset) have a slightly lower than normal level or
an altered protein. Genetic linkage analysis, although inaccu-
rate, usually provides a carrier status or prenatal diagnosis as a
“percentage risk” rather than a definite yes or no.
Treatment
A. Respiratory Care—Elective intubation is recommended
when vital capacity falls below 15–20 mL/kg. Ventilator set-
tings should be monitored along with arterial blood gases.
Baseline blood gases can be obtained after 20 minutes of F
IO
2
at 100%, after which inspired oxygen concentration can be
decreased to maintain the Pa
O
2
between 75 and 85 mm Hg.
Positive end-expiratory pressure (PEEP) should be set at
3–5 cm H
2
O and tidal volume at 6–8 mL/kg. The intermittent
mandatory ventilation (IMV) rate should be approximately
12/min with 30–40 L/min inspiratory flow. If the patient
requires prolonged intubation—more than 2–3 weeks—a tra-
cheostomy should be performed to maintain a stable airway.
Criteria for weaning a neuromuscular patient from a ven-
tilator include several parameters, the most important of
which is the vital capacity, which should be greater than
15 mL/kg. Inspiratory pressure should be greater than –25 cm
H
2
O and expiratory pressure greater than 40 cm H
2
O. Pa
O
2
should be greater than 80 mm Hg and Pa
CO
2
less than 42 mm
Hg at F
IO
2
of .40. Spontaneous respiration should be less
than 20/min, and there should be no other adverse medical
conditions such as fulminant pneumonia or serious cardiac
problems.
All patients presenting with weakness should be followed
carefully for respiratory status. Good pulmonary toilet is
mandatory. It is helpful to have an accurate diagnosis so that
special precautions can be taken to anticipate or prevent the
progression of symptoms. A superimposed infection may
exacerbate the weakness of many neuromuscular diseases,
and temporary life support will enable the patient to return
to baseline strength. Therefore, it is imperative to exclude the
possibility of a reversible cardiopulmonary complication.
B. Cardiac Care—Between 70% and 90% of patients with
Duchenne’s muscular dystrophy will develop electrocardio-
graphic abnormalities consisting of tall right precordial R
waves and precordial Q waves. Arrhythmias and persistent
tachycardia are noted frequently in Duchenne’s muscular
dystrophy. Patients with myotonic dystrophy also develop
cardiac arrhythmias secondary to conduction abnormalities
and can present with sudden death if not detected early.
Differential Diagnosis
There are many CNS disorders that can mimic neuromuscu-
lar diseases. For example, a brain stem lesion may produce
diplopia that may be mistaken for myasthenia gravis or bul-
bar symptoms that may be mistaken for amyotrophic lateral
sclerosis. Neuroleptic malignant syndrome often is difficult
to differentiate from other causes of fever and encephalopa-
thy. Blood cultures, drug screens, and brain imaging may be
necessary to exclude systemic infections, drug exposures, or
disorders producing changes in autonomic control and tem-
perature such as injury to the hypothalamic region.
A careful history (including family history) and physical
examination generally will distinguish the major groups of
illnesses. However, electrophysiologic studies or laboratory
evaluations sometimes are necessary to differentiate the spe-
cific types of diseases. Nerve conduction studies with repeti-
tive stimulation will help to differentiate presynaptic from
postsynaptic diseases, and serum creatine kinase will help to
distinguish a primary myopathy from neurogenic weakness.
Current Controversies and Unresolved
Issues
A particularly difficult problem is whether to intubate a
patient who has an irreversible advanced neuromuscular dis-
ease. If possible, the issue of code status should be discussed
with the patient and the family prior to clinical deterioration.
Perhaps the patient already has a living will or a family mem-
ber has power of attorney to help with the decision-making
process.
CEREBROVASCULAR DISEASES
ESSENTIALS OF DIAGNOSIS
Stepwise impairment usually produced by occlusive dis-
ease.
Emboli produce sudden deficits.
Intracerebral hemorrhage causes rapid onset of symp-
toms, often with increased intracranial pressure.
General Considerations
Brain stem and cerebral infarctions occur as a result of either
progressive occlusive vascular disease, usually hypertensive
and atherosclerotic, or embolism. In occlusive disease,
infarcts are bland, and in embolic disease, infarcts are hem-
orrhagic if the embolus fragments and the vascular territory

CHAPTER 30
674
is reperfused. A hemorrhagic infarct implies embolism.
Spontaneous intracerebral hemorrhage occurs as a result of
hypertensive vascular disease, but in elderly people it also can
be caused by amyloid angiopathy.
Clinical Features
A. Symptoms and Signs—Stroke owing to occlusive vascu-
lar disease, or thrombosis, tends to have its onset in a stepwise
or progressive fashion. It occurs commonly while the patient
is sleeping. An embolic stroke is sudden in onset and produces
maximum neurologic deficit at the outset. Transient ischemic
attacks can precede either thrombotic or embolic infarction
but probably are more frequent in association with throm-
botic disease. An intracerebral hemorrhage also is sudden in
onset and may cause an acute rise in intracranial pressure
owing to mass effect. The location of a stroke is clinically
helpful; for example, a small lacunar infarct in the internal
capsule is almost certainly due to intracranial, small vessel, or
occlusive disease. The first step in localizing the lesion is a
careful neurologic examination.
B. Imaging Studies—Brain imaging will confirm the loca-
tion of the infarct and determine whether hemorrhage has
occurred. This information is required before anticoagulation
therapy can be started. Typically, a bland infarct will not show
on CT scan in the first few hours up to about 24 hours after
onset. CT imaging, however, is very sensitive for the detection
of fresh bleeding. MRI, especially with diffusion studies, is
sensitive for acute infarction. MR angiography can demon-
strate occluded or stenotic large- and medium-sized arteries.
Differential Diagnosis
A history of hypertension, diabetes mellitus, or tobacco
smoking and a family history of stroke or myocardial infarc-
tion are common in occlusive disease. A history of hyperten-
sion is common in intracerebral hemorrhage. If an embolic
infarction is present, a source should be found; this may be
clots arising in the heart or clots from the periphery reach-
ing the brain as a result of right-to-left cardiac shunting, as
may occur with a patent foramen ovale. Artery-to-artery
embolization, usually from an internal carotid artery, also
may be considered. Strokes secondary to cocaine abuse cur-
rently are a problem not to be overlooked. Also occasionally
encountered are strokes caused by carotid artery or vertebral
artery dissection. These are traumatic in origin, and symp-
tomatic onset usually is 24–72 hours following trauma.
Often a history of neck extension is obtained. An intimal
tear and flap are demonstrated by either endovascular or
MR angiography. A brain CT scan is very sensitive for
demonstrating intracerebral hemorrhage or hemorrhagic
infarction, but an acute bland infarct does not show until
density of the infarcted tissue has decreased and edema
occurs. MRI is sensitive in all cases. Occlusion of large ves-
sels supplying the brain can be demonstrated with Doppler
ultrasound, MR angiography, and CT angiography. Selective
contrast angiography is indicated when the diagnosis is in
doubt and a surgically treatable vascular lesion could be
present. The workup for an embolic source should include
electrocardiography and, if a rhythm disturbance such as
atrial fibrillation is not found, echocardiography. An
embolic source sometimes can be demonstrated only on the
transesophageal echocardiogram.
Rarer causes of stroke include polycythemia, sickle cell
disease, collagen-vascular diseases, lupus anticoagulant, and
hypercoagulable states. Infrequent causes of stroke also are
moyamoya disease, fibromuscular hyperplasia, Takayasu’s
disease, and tuberculous or other arterites. Infarction caused
by arterial spasm associated with ruptured berry aneurysm
and subarachnoid hemorrhage is well known in neurosurgi-
cal practice.
Treatment
In general, the management of an acute stroke consists of
supportive care and control of blood pressure. In this cir-
cumstance, autoregulation of cerebral blood flow is impaired
or lost, and regional brain perfusion is passive and essentially
dependent on systemic blood pressure. Therefore, hypoten-
sion is to be avoided. Edema characteristically develops
24–72 hours following infarction and can lead to complica-
tions owing to mass effect; this is especially critical in the
posterior fossa, where obstruction of CSF flow and second-
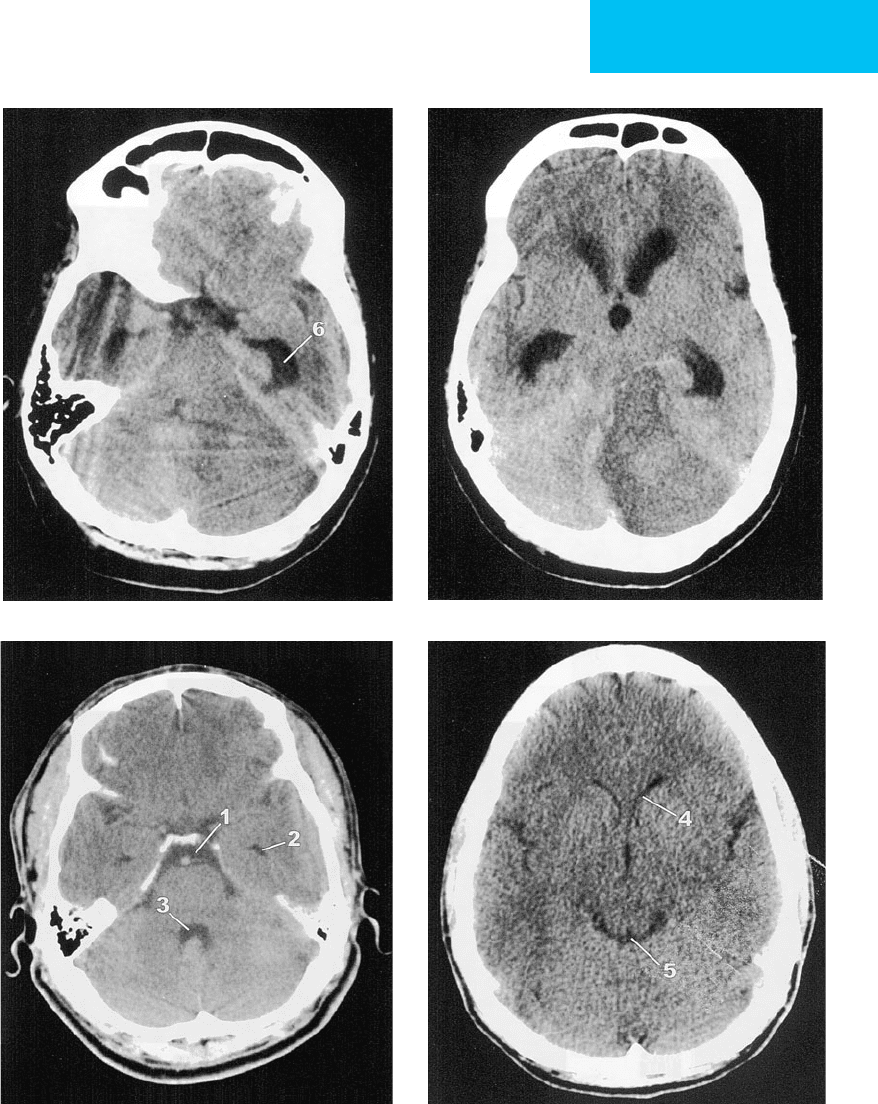
ary hydrocephalus can result (Figure 30–3). Fluid balance in
acute stroke patients therefore should be watched carefully
and kept on the “dry side” to minimize the risk of hypona-
tremia and further brain swelling. Inappropriate antidiuretic
hormone secretion sometimes can complicate this problem.
When progressive mass effect with secondary hydrocephalus
occurs, management is as described in Chapter 29, and will
require consultation with a neurosurgeon. Since many stroke
patients develop dysphagia or have poor mental status, aspi-
ration precautions should be taken, and a nasogastric tube
should be placed. Swallowing evaluations often are necessary
before allowing oral intake.
Anticoagulation is clearly indicated in embolic disease
but usually must be delayed in the presence of a significant
hemorrhagic infarct because of the risk of further bleeding.
However, this factor must be weighed against what one
judges to be the risk for repeated embolization. Common
practice is to delay for about 10–14 days. The efficacy of anti-
coagulation in occlusive vascular disease is less clear, but it is
common practice at this time to anticoagulate patients with
strokes in progression or frequently repeated transient
ischemic attacks. In the critical care situation, initial antico-
agulation for cerebrovascular disease is accomplished with
intravenous heparin.
Antiplatelet therapy has been shown to reduce the inci-
dence of future stroke in patients at risk, including those with
present or prior stroke, and it can be initiated in the acute
phase of a new stroke. The available agents are aspirin or
enteric-coated aspirin, 81–325 mg/day; clopidogrel bisulfate,
CRITICAL CARE OF NEUROLOGIC DISEASE
675
AB
CD
Figure 30–3. A, B. Hypodense lesion in the right cerebellar hemisphere with swelling and mass effect resulting in obliter-
ation of the fourth ventricle and cisterns surrounding the brain stem and secondary enlargement of the third ventricle and the
temporal and lateral ventricles. Approximately 2
1
/
2
hours after this CT scan was obtained, the patient became comatose and
lost brain stem function owing to progressive obstructive hydrocephalus and brain stem compression. Also, intracranial pres-
sure may exceed cerebral perfusion pressure in this circumstance. Timely neurosurgical intervention can prevent this sequence
of events and thus be lifesaving. C, D. Normal studies for comparison. 1 and 5, cistern; 3, fourth ventricle; 2 and 6, temporal
ventricle; 4, lateral ventricle. Third ventricle unlabeled.
CHAPTER 30
676
75 mg/day; or aspirin and extended-release dipyridamole,
one 25/200-mg capsule twice daily. Ticlopidine, 250 mg twice
daily, also is available but is associated with a higher inci-
dence of adverse reactions than the others.
Treatment of acute ischemic stroke with intravenous
recombinant tissue plasminogen activator (rt-PA; alteplase)
has been shown to be beneficial but only if initiated within 3
hours of stroke onset; thus a clear history of time of onset and
prompt transportation to a treatment facility are crucial. The
benefit realized is reduction in long-term disability; improve-
ment taking place in the acute phase is not clearly attributa-
ble to the treatment. Nevertheless, many specialists in this
area believe that within the 3-hour time window, the sooner
the better is the rt-PA treatment. The major adverse event
of this treatment is intracerebral hemorrhage, but even so,
the long-term outcome may be improved if the patient sur-
vives. Overall, the most frequently reported hemorrhage
rate is in the 3–6% or more range. It is essential that the
treating institution establish a system for immediate patient
evaluation and have a protocol in place. Table 30–7 lists the
inclusion and exclusion criteria adopted by the authors’
institution, and Table 30–8 gives the protocol for evaluation
and treatment.
Current Controversies and Unresolved Issues
Carotid endarterectomy generally is recommended to reduce
the risk of future stroke when 70–80% or more of stenosis is
present in a symptomatic artery (it is contraindicated in an
occluded artery). Some data exist indicating that endarterec-
tomy on an asymptomatic, high-grade stenotic carotid artery
is beneficial, but this remains controversial.
Work is in progress to better assess outcome of patients
treated with intravenous rt-PA and to refine selection criteria
for identifying those more or less likely to respond. Also, pro-
tocols are in place to define the role of intraarterial r-tPA and
a device for clot removal in acute cerebrovascular occlusion.
Complications of Central Nervous System
Infections
ESSENTIALS OF DIAGNOSIS
History: neurologic symptoms, exposures.
Examination: level of consciousness, neck stiffness,
focal neurologic findings, seizures.
Brain imaging with and without contrast material.
CSF analysis.
Inclusion criteria
Age 18 or older
Clearly defined time of onset (very important!)
Ability to initiate rt-PA within 180 minutes from time of onset
Exclusion criteria
Minor stroke or rapidly improving symptoms
Hemorrhage or edema on noncontrast head CT
Suspected subarachnoid hemorrhage
Stroke or serious head trauma within 3 months prior to current stroke
Major surgery or trauma within 14 days prior to current stroke
History of intracranial hemorrhage
Systolic blood pressure >185 mm Hg or diastolic blood pressure
>110 mm Hg
Gastrointestinal or urinary tract hemorrhage within 21 days prior to
current stroke
Arterial puncture at a noncompressible site within 7 days prior to
current stroke
Acute myocardial infarction or pericarditis
Patient taking anticoagulants or has received heparin within the
48 hours preceding the onset of stroke and has elevated aPTT
Platelet count <100,000/μL
PT >15 seconds (INR >1.7) or aPTT >34 seconds
Glucose <50 mg/dL or >400 mg/dL
Seizure at onset of stroke
Known or suspected pregnancy or lactating woman
Aggressive treatment required to maintain blood pressure below
indicated parameters
Lumbar puncture within 7 days prior to current stroke
Occult blood in urine or stool
Table 30–7. rt-PA (alteplase) criteria.
1. When notified of a possible rt-PA candidate, call designated medical
personnel immediately.
2. Get the time of onset, a medication list, and complete neurologic
examination. Patient needs a monitored bed in the emergency
room.
3. Obtain stat head CT scan (noncontrast) to rule out hemorrhage;
stat labs: CBC, PT/aPTT/glucose; stat ECG.
4. Go through all exclusion criteria (Table 30–7) and put sheet on chart.
5. Dose: Alteplase (Activase) 0.9 mg/kg (maximum 90 mg total
dose) IV. Give 10% as bolus over 1 minute, remainder by continu-
ous infusion over 60 minutes.
6. If patient recieves rt-PA, needs ICU bed.
7. Order vital signs and neurologic checks (specify what you want
checked):
• Every 15 minutes for 2 hours
• Every 30 minutes for 6 hours
• Every 1 hour for 16 hours
8. Strict blood pressure control (185/95 mm Hg or less). Use IV
labetalol or nitroprusside drip.
9. Urgent: No anticoagulants and no antiplatelet agents whatsoever
for 24 hours after rt-PA given.
10. If there is any worsening on neurologic or mental status examina-
tion,
stop rt-PA
if still being infused and order stat head CT
(noncontrast) to rule out hemorrhage.
Table 30–8. rt-PA (alteplase) protocol.
