Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

ACUTE ABDOMEN
697
Clinical Features
A. Symptoms—While many patients in the ICU are unable
to give a history because of intubation or altered mental sta-
tus, a detailed review of recent symptomatology should be
obtained whenever possible. Family members and friends
should be interviewed. Patients may have been transferred
from a hospital ward or may have had recent contact with
the hospital or emergency room. However obtained, the his-
tory should describe any preexisting medical conditions,
previous surgery, present medications, prior abdominal
complaints, changes in eating or bowel habits, and recent
weight loss. Exposure to toxic substances (including alco-
hol) and recent trauma should be noted. The obstetric and
gynecologic history should include data about menses and
sexual contacts.
Events leading to hospitalization need to be reviewed,
and if pain is part of the symptomatology, a history of its
presentation and progression is helpful. Despite efforts to
elicit a detailed history, this is often not possible in critically
ill patients.
1. Location of the pain—The location of pain can give
valuable information about its cause. Even more important is
an account of its progression and changes in location
(Table 32–1). Knowing where the pain began occasionally
means more than determining where it is at presentation. A
perforated ulcer may cause lower abdominal pain from intes-
tinal contents collecting in the pelvis owing to gravitational
effects or even owing to a pelvic abscess, whereas a detailed
history may reveal days or weeks of epigastric or right upper
quadrant pain. Pain radiating to some other area of the body
also may give valuable information. For example, epigastric
pain that radiates through to the back is more likely to be due
to pancreatitis than to reflux esophagitis.
2. Nature of the pain—Episodic or crampy pain is usually
due to blockage or obstruction of a hollow viscus during
contraction or attempted peristalsis such as in bowel
obstruction or during an attack of acute cholecystitis.
Questioning and observation often will determine what fac-
tors increase or relieve the pain. Patients with direct peri-
toneal inflammation will resist movement, whereas patients
with renal colic will writhe about with no apparent exacerba-
tion from the movement itself.
3. Progression of the pain—Since virtually all patients
subjected to abdominal operations have postoperative pain,
progression of the pain gives important information about
its source. Incisional pain usually begins to subside after the
first 72 hours, whereas pain owing to other causes such as an
intraabdominal abscess or bowel obstruction often will begin
after 72 hours and become progressively worse.
B. Physical Examination—A comprehensive physical
examination of the ICU patient can be difficult and frustrat-
ing, especially just after an operation. Nevertheless, a com-
plete examination is essential on admission to the unit,
starting with measurement of routine vital signs. Body
temperatures should be obtained from a reliable site—rectal,
bladder, or core measurements from a Swan-Ganz catheter
probe will suffice. Oral and axillary temperatures are often
unreliable. Fever with or without hypotension arouses sus-
picion of abdominal disease, and the presence of both often
will suggest an acute abdomen. Examination to exclude an
extraabdominal source of sepsis should include inspection
of old and existing intravenous sites, chest auscultation
and percussion, inspection of all wounds (traumatic and
surgical), and gross evaluation of urine, especially in
catheterized patients.
1. Observation—Abdominal examination should begin
with careful observation of not only the abdomen but also
the patient’s body position and general demeanor. Is the
patient resting comfortably or in significant distress, with
guarding of the abdominal area? Any distention, ecchymoses,
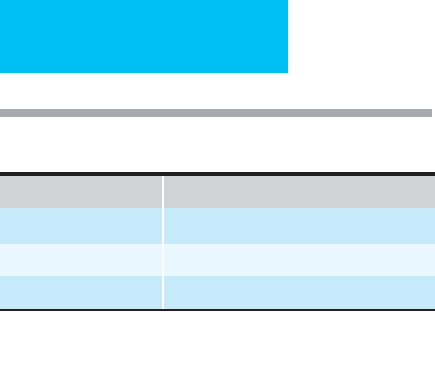
Table 32–1. Locations of common etiologies of acute
abdomen.
Epigastrium Suprapubic and Pelvic
Esophageal disease Cystitis
Peptic ulcer disease Diverticulitis
Pancreatitis (including Proctitis
pseudocyst) Pelvic abscess
Cardiac disease Renal colic
Hiatal hernia (including Left Upper Quadrant
paraesophageal) Pancreatitis (including pseudocyst)
Right Upper Quadrant Splenic disease
Cholecystitis Hiatal hernia (including
Cholangitis paraesophageal)
Pancreatitis (including Renal colic
pseudocyst) Left lower lobe pneumonia
Peptic ulcer disease Colitis (especially ischemic)
Renal colic Subphrenic abscess
Hepatitis Periumbilical
Appendicitis Umbilical hernia
Cecal volvulus Early appendicitis
Hepatic abscess Small bowel obstruction
Subphrenic abscess Mesenteric ischemia
Right lower lobe pneumonia Aortic aneurysm
Right Lower Quadrant Left Lower Quadrant
Appendicitis Diverticulitis
Diverticulitis Sigmoid volvulus
Crohn’s disease Colitis (especially ischemic)
Colonic obstruction Renal colic
Psoas abscess Inguinal hernia
Pelvic inflammatory disease Pelvic inflammatory disease
Ovarian cyst or torsion Ovarian cyst or torsion
Ectopic pregnancy Ectopic pregnancy
Inguinal hernia Epididymitis
Epididymitis Pelvic abscess
Pelvic abscess Psoas abscess

CHAPTER 32
698
and old surgical scars should be noted. Some abdominal dis-
tention is normal in the postoperative abdominal surgical
patient, but any increase in distention postoperatively may
signify problems such as a nonfunctioning nasogastric tube,
prolonged ileus, small bowel obstruction, or development of
ascites. Recent incisions should be inspected, and any ery-
thema, edema, or fluid discharge should alert the examiner
to a potential wound or intraabdominal infection.
2. Auscultation—Auscultation is difficult in a noisy ICU
environment and therefore frequently neglected. Absent
bowel sounds may be normal in recent postoperative patients
but in others may be viewed appropriately with suspicion.
Hyperactive, high-pitched rushes may signify bowel obstruc-
tion. Abdominal bruits indicate the presence of aneurysms,
arteriovenous fistulas, or severe atherosclerotic disease.
3. Percussion—Gentle percussion with close attention to
grimacing or other movement by the patient can give sub-
tle information about localized peritoneal irritation. The
presence of a tympanic area in the right upper quadrant
overlying the liver suggests pneumoperitoneum. Percussion
also can help to detect bowel obstruction (calling for naso-
gastric intubation) or ascites or may disclose a distended
bladder owing to a nonfunctioning or nonexistent Foley
catheter.
4. Palpation—Palpation may reveal hepatomegaly or
splenomegaly, an abdominal wall hernia, a distended gall-
bladder, an intraabdominal tumor or abscess, or an aortic
aneurysm. Rebound tenderness is intended to elicit peri-
toneal irritation. Gentle percussion is a good test for local-
ized peritonitis. Gently bumping the patient or the bed or
having the patient cough will cause enough peritoneal move-
ment to exacerbate pain from peritoneal inflammation.
Careful observation of the patient’s facial expression and
body position will be revealing. Deep palpation of the
abdominal wall and sudden release to elicit rebound tender-
ness is often misleading and in the presence of peritonitis
often will increase guarding and make subsequent examina-
tions more difficult.
When cholecystitis is in the differential diagnosis, right
upper quadrant palpation may reveal tenderness or even a
positive Murphy sign (ie, arrested inspiration during palpa-
tion of the right upper quadrant). Although the retroperi-
toneum and pelvis are less accessible to direct palpation,
indirect evidence of inflammation can be elicited. Pain on
hyperextension of the hip, on stretching the iliopsoas muscle
(psoas sign), and on flexion and internal rotation of the hip,
stretching the obturator muscle (obturator sign), can indi-
cate an adjacent inflammatory process. Gentle palpation or
percussion of the posterior costovertebral angles should
diagnose or exclude pyelonephritis.
5. Rectal and pelvic examination—Genitourinary and
rectal examinations are essential to evaluate for incarcerated
hernias, pelvic or rectal masses, cervical motion tenderness,
prostatic or scrotal disease, and bloody stools. Stool may be
guaiac-tested to confirm a clinical suspicion, but—at least in
the ICU patient population—this test is too insensitive and
nonspecific to be useful in making clinical decisions.
C. Laboratory Findings—A white blood cell count is non-
specific and relatively insensitive—its absolute level is less
useful than its trend. A differential count indicating a left
shift increases the sensitivity of this test. The hematocrit is
helpful or even essential in diagnosing intraabdominal or GI
bleeding.
Urinalysis should be performed with attention to the
presence of white blood cells or white blood cell casts indica-
tive of urinary tract infection. Urine specific gravity can give
information useful in fluid resuscitation efforts, and the
presence of glucose or ketones is of diagnostic and therapeu-
tic importance.
Elevated liver enzymes (eg, AST, ALT, and alkaline phos-
phatase) direct attention to the liver (eg, hepatitis) and bil-
iary system (eg, cholangitis or cholecystitis). Bilirubin
elevation is seen in hepatobiliary disease but also can be asso-
ciated with sepsis, hemolysis, and cholestasis owing to par-
enteral nutrition.
Serum amylase is neither sensitive nor specific, although
markedly elevated values usually indicate pancreatitis.
Elevated serum amylase is also seen with perforated ulcer,
mesenteric ischemia, facial trauma, parotitis, and ruptured
ectopic pregnancy. Lipase or Pankrin values may improve
specificity in the diagnosis of pancreatitis. Arterial blood gas
measurements may demonstrate acidosis or hypoxia. Acidosis
may reflect severe sepsis or ischemia, whereas hypoxia may
reflect acute respiratory distress syndrome (ARDS) owing to
uncontrolled sepsis. Additionally, arterial lactate levels may be
more specific in identifying worsening acidosis, especially in
the setting of preexisting acidosis such as renal failure.
D. Imaging Studies—Although bedside studies are rela-
tively risk free, CT scans, MRI, arteriography, and nuclear
medicine scans usually require patient transport. In this
select group of critically ill patients, transfer to other areas of
the hospital carries significant risks.
1. Bedside films—Radiographs of the chest can evaluate for
pulmonary infections as well as free air when performed
with the patient in a sitting position. Pleural effusions, espe-
cially when asymmetric, may signify an intraabdominal
process. Abdominal radiographs may show a colonic volvu-
lus or obstructed bowel gas pattern, biliary or renal calculi, or
(rarely) pneumobilia. Ultrasound can be useful as a diagnos-
tic and therapeutic tool—intraabdominal abscesses can be
identified with this procedure and percutaneous drainage
facilitated. Cholecystitis (calculous or acalculous) can be
diagnosed and even treated (percutaneous cholecystostomy).
In questionable cases, percutaneous aspiration with analysis
of gallbladder contents (ie, Gram stain and culture) can be
invaluable.
2. Radiology department studies—CT scans have
assumed a primary position in the diagnosis of acute

ACUTE ABDOMEN
699
abdomen. They should not be used indiscriminately, how-
ever, and are of little value in the first week after abdominal
surgery, when normal postoperative findings (ie, blood, air,
and seromas) make identification of an abscess difficult. In
the critically ill patient with multiple-organ-system failure,
transport to the radiology department may carry a greater
risk than the potential benefit. These patients perhaps
should be considered for early laparotomy. CT scanning for
intraabdominal abscesses has an accuracy rate greater than
95%. Studies that have looked specifically at critically ill sur-
gical patients, however, are not so promising, with sensitiv-
ity rates as low as 50% and with only 25% of the scans
actually providing beneficial information that perhaps
altered the outcome of therapy. CT scans should be per-
formed only when the information obtained is expected to
have that result.
GI contrast studies can be useful occasionally in patients
with recent anastomoses or in those with possible missed
injuries (especially esophageal injuries). In general, water-
soluble agents (eg, Gastrografin) should be used.
Angiography is useful in patients with suspected mesenteric
ischemia and should be performed early after initial resusci-
tation. In addition to securing the diagnosis, intraarterial
vasodilators (eg, papaverine) can be used as primary therapy
or to demarcate and salvage marginally viable intestine.
Angiography also plays a diagnostic role in selected patients
with GI bleeding, aiding in localization of the bleeding site,
and it has therapeutic applications in the delivery of intraar-
terial vasopressin or embolization. Blood loss of at least
0.5 mL/min is required before it can be detected by angiog-
raphy.
99m
Tc-tagged red blood cell scans have a reported sen-
sitivity of 0.05–0.1 mL/min and may play a role in screening
patients for the more invasive angiographic approach.
Gallium- or indium-tagged white blood cell scans are
useful occasionally in relatively stable patients. The poor
specificity of the tests, especially in the postoperative patient,
and the 24–48-hour time period for completion limit their
usefulness.
E. Peritoneal Lavage—Extensively used in abdominal
trauma, diagnostic peritoneal lavage also may be quite useful
in selected ICU patients. The same factors that make assess-
ment of critically ill patients difficult (eg, altered mental sta-
tus, intubation, etc.) make lavage an attractive alternative.
Numerous studies have shown its utility in selected patients
with white blood cell counts greater than 500/μL or red
blood cell counts greater than 50,000–100,000/μL. Lavage
has limited if any usefulness in the recent postoperative
patient. In this setting, CT- or ultrasound-guided percuta-
neous aspiration is safer and more reliable.
F. Endoscopy—In the presence of active upper GI bleeding,
esophagogastroduodenoscopy is of proved diagnostic and
therapeutic benefit. Flexible sigmoidoscopy and colonoscopy
also may be of diagnostic value in the patient with possible
ischemic colitis or pseudomembranous colitis. Up to a third
of patients with pseudomembranous colitis have negative
C. difficile toxin assays; visualization and biopsy will increase
the diagnostic accuracy to over 95%. Ischemic colitis can
occur as a result of embolic disease, shock (low-flow state),
or—not uncommonly in the ICU setting—after aortic sur-
gery. Endoscopy can confirm the diagnosis and can allow
observation of the progression of disease in selected patients.
Endoscopic retrograde cholangiopancreatography has a
proven therapeutic role in septic patients with cholangitis,
allowing stone extraction or stenting.
Evaluation of the Postoperative Abdomen
Postoperatively, a number of potential intraabdominal com-
plications can occur in the ICU patient. These include such
diverse problems as intraperitoneal bleeding, anastomotic
dehiscence, early small bowel obstruction, and fascial dehis-
cence. Early recognition and aggressive corrective action are
required.
To identify a failure to recover on schedule after laparo-
tomy, one must understand the normal course following
major abdominal surgery. Third-space fluid sequestration
occurs in approximate proportion to the magnitude of the
surgery. Mild to moderate abdominal distention and olig-
uria—frequently seen in the first 24–72 hours after sur-
gery—can make identification of postoperative hemorrhage
difficult. Not infrequently, a declining hematocrit is attrib-
uted to dilutional effects or to equilibration. The accompany-
ing tachycardia may be falsely attributed to pain. Alert
watchfulness for possible postoperative bleeding can avert a
disastrous outcome.
Fever is the most commonly observed postoperative
physiologic abnormality. The presence of fever suggests
infection, but the approach to evaluation must be methodi-
cal. A single febrile episode in most patients should call for
nothing more than a review of the history and a physical
examination. Intermittent spikes of recurrent fever may war-
rant a more thorough investigation—again directed by a
thorough physical examination. The goal should be to iden-
tify a complication early while intervention still may improve
the outcome.
Other than missed injuries to hollow viscera (traumatic
or iatrogenic), intraabdominal sepsis—including abscess and
anastomotic leaks or dehiscences—typically is manifested
between 5 and 10 days after surgery. Early recognition and
treatment are critical. Subtle signs may aid in early diagnosis.
Third spacing should resolve within 48–96 hours, and obser-
vation of a vigorous postoperative diuresis during this period
is a reliable sign of improvement. Leukocytosis following
major surgery is frequently regarded as a normal finding
(largely owing to demargination), whereas failure of the
white blood cell count to return to normal or an increase
from a declining value should suggest the possibility of
intraabdominal sepsis. Other findings include glucose intol-
erance, continued tachycardia, worsening acidosis, pro-
longed ileus, or persistent diarrhea on return of bowel
function (owing to adjacent pelvic abscess).

CHAPTER 32
700
Treatment
Following the initial evaluation of an ICU patient for consid-
eration of an acute abdomen, the primary decision is
whether urgent surgery is required. Resuscitation with intra-
venous fluids is usually necessary to correct third-space
losses or bleeding. A bladder catheter should be inserted to
monitor urine output and, unless contraindicated, a naso-
gastric tube to decompress the stomach. Both H
2
blockers
and antacids are effective, with greatest efficacy achieved by
maintaining the gastric pH higher than 5.0. An arterial and a
pulmonary artery flotation catheter may be necessary in some
patients to monitor hemodynamic function and intravascular
volume. Antibiotics should be given as indicated. Caution
should be exercised in giving antibiotics to patients with
undiagnosed but suspected sepsis because of concerns about
obfuscating the clinical picture and frustrating further evalu-
ation. Antibiotic therapy is largely adjunctive, although small
abscesses or phlegmonous processes owing to contained
enteric leaks often will resolve with their use.
SPECIFIC PATHOLOGIC ENTITIES
Bowel Obstruction
The diagnosis of early postoperative small bowel obstruc-
tion frequently is delayed primarily because of the differen-
tial consideration of persistent adynamic ileus. The
characteristic symptoms of obstruction include abdominal
distention, obstipation, and vomiting. These symptoms also
characterize adynamic ileus, and the first step in differentia-
tion is consideration of the diagnosis. Further confusing the
clinical picture is the side effect of opioid analgesics on
decreasing GI motility.
The clinical history and physical examination are often
nondiagnostic, although the patient who has brief return of
GI function followed by its cessation probably has an adhe-
sive obstruction. Plain radiographs likewise are frequently
nondiagnostic in this setting.
A nasogastric tube should be inserted. Hypovolemia
should be corrected and electrolytes checked, with special
attention to hypokalemia and hypocalcemia. If there is a pos-
sibility of intraabdominal abscess or sepsis, CT scan or ultra-
sonography is indicated. If the diagnosis is still in doubt, a
water-soluble contrast study (eg, Gastrografin) can be diag-
nostic as well as therapeutic because of the cathartic effect of
the hyperosmolar solution. Drainage of an abscess may
relieve the localized ileus or obstruction. Patients who are
receiving adrenal corticosteroids may develop adynamic ileus
if the drug is withdrawn too quickly. High doses (300 mg
hydrocortisone daily or equivalent) intravenously will give
prompt resolution.
Complete obstruction warrants reoperation as soon as
resuscitation is complete. Partial obstruction often will resolve
with conservative management.
Enteric Fistula
Risk factors for enteric fistula include previous radiation,
inflammatory bowel disease, and chronic corticosteroid
administration. After initial resuscitation, the first maneuver
is to determine the need for early operation. A controlled fis-
tula is present when enteric contents are captured by a drain
or when rapid egress from a wound results in little or no
peritoneal contamination or irritation—such cases can be
expected to resolve with nonoperative therapy. Percutaneous
drainage of an associated abscess found by ultrasound or CT
scan may allow closure of the fistula and improve the
patient’s physiologic status prior to definitive management.
Complicating conditions include radiation damage, malig-
nancy, inflammatory bowel disease, the presence of a foreign
body, and distal intestinal obstruction. Water-soluble con-
trast studies are occasionally helpful to visualize the site of
fistula, evaluate the adequacy of drainage, and rule out distal
obstruction. Once a decision to attempt conservative man-
agement is made, useful therapeutic maneuvers may include
restriction of oral intake, parenteral nutrition, octreotide
acetate (50–200 μg subcutaneously twice to three times
daily), and nasogastric suction. Elemental diets may be sub-
stituted for parenteral nutrition in selected patients—especially
those with distal fistulas or with fistulas not in continuity
(eg, duodenal stump and pancreatic).
Conversely, an anastomotic leak or dehiscence that results
in free peritoneal spillage requires emergent operation for
patient survival. The clinical setting and physical examina-
tion usually will allow an accurate assessment. Oliguria and
hypovolemia often portend extensive peritoneal contamina-
tion and third spacing, whereas diffuse peritoneal irritation
manifested by a rigid abdomen on examination offers no real
dilemma. The patient with localized peritoneal signs, mild to
moderate leukocytosis, and perhaps minimal additional fluid
requirements presents a more difficult decision.
Intraabdominal Abscess
Intraabdominal abscess is usually the result of contamination at
the time of surgery or leakage of enteric contents. The process
has been contained by the patient’s immune system and
defense mechanisms, including the omentum. Antibiotics—
especially with smaller collections—may resolve the process.
Larger abscesses—especially those with continued enteric
communication—may require percutaneous or open drainage
or even intestinal resection to control the process. The exact
role and limitations of percutaneous drainage seem to depend
more on the availability of an experienced interventional radi-
ologist than on any absolute criteria, although multiloculated
and interloop abscesses may be less amenable to this tech-
nique. Success rates range from 25–100%. Infected pancreatic
necrosis and other phlegmonous processes are not amenable
to the percutaneous approach. Of particular importance is
appropriate attention to ensure continued success, including
catheter irrigations, frequent rescanning, and contrast studies.
ACUTE ABDOMEN
701
Cholecystitis
Patients in the ICU may develop calculous or acalculous
cholecystitis as well as cholangitis or biliary pancreatitis. The
diagnosis may already be known or suspected, as in the
patient admitted for observation of acute pancreatitis, or
may be a confounding factor, as in the recent cardiac surgical
patient developing acalculous cholecystitis.
The typical findings of right upper quadrant pain, fever,
and Murphy’s sign may not be present even in an awake,
responsive patient. Elevated liver enzymes or unexplained
fever often prompt consideration of biliary disease. Well-
recognized risk factors for cholecystitis (ie, NPO, parenteral
nutrition, recent surgery, and shock) should arouse suspi-
cion. Perhaps the main difficulty is the lack of a reliable diag-
nostic examination in a critically ill patient, especially one
with acalculous disease. The findings of sludge in the gall-
bladder by ultrasound and nonvisualization on
99m
Tc-HIDA
scan are nonspecific and even expected in patients being
maintained on long-term parenteral nutrition. The tech-
nique of percutaneous cholecystostomy (transhepatic) or
aspiration of gallbladder contents with analysis (eg, Gram
stain and culture) can be useful and deserves consideration
in the most unstable patients. The diagnosis remains largely
a clinical one, and exploration is often required for confirma-
tion and treatment. Surgical exploration frequently is based
on clinical suspicion and nonexclusionary test results.
Colonic Pseudo-Obstruction (Ogilvie’s
Syndrome)
Typical findings include abdominal distention, abdominal
pain, and obstruction. Plain abdominal radiographs are usu-
ally diagnostic, although contrast studies or endoscopy may
be necessary to exclude volvulus and distal colonic obstruc-
tion. Predisposing factors include bed rest, spinal fractures
and cord injuries, and prolonged opioid use. Treatment is
required when the cecal diameter exceeds 10 cm on a plain
film of the abdomen. Therapy should include correction of
electrolyte disturbances (especially hypokalemia), cessation
of narcotics, and nasogastric decompression to prevent fur-
ther gaseous distention. Neostigmine has emerged as the
treatment of choice. If the cecal diameter exceeds 12 cm, and
if there is no improvement with the preceding measures,
colonoscopic decompression is usually effective, with
15–20% of patients requiring repeated procedures. Operative
treatment (eg, tube cecostomy or right colectomy) is reserved
for patients with signs of present or impending perforation
or a situation in which a skilled endoscopist is not available.
Abdominal Compartment Syndrome
The concept of elevated intraabdominal pressure having
detrimental clinical sequelae was enunciated over two
decades ago. Initially, renal “toxicity” was focused on, and
oliguria remains one of the earlier clinical signs. Other
sequelae include pulmonary compromise and mesenteric
ischemia. The important factors to keep in mind are to have
a high index of suspicion (especially in patients with signifi-
cant abdominopelvic trauma), to use bladder pressure meas-
urements as a reflection of intraabdominal pressure, and to
consider or perform decompressive laparotomy early if indi-
cated. Control of the open abdomen may be accomplished by
superficially securing an opened 3-L intravenous fluid bag.
Also, the application of an external vacuum-assisted closure
(VAC) device can be applied in this setting.
CURRENT CONTROVERSIES & UNRESOLVED
ISSUES
Bacterial Translocation and Enteral Feedings
The clinical picture of a critically ill patient succumbing to
sepsis and multiple-organ-system failure without any appar-
ent septic focus is a not infrequent clinical problem. A large
volume of data—largely experimental or anecdotal—points
to bacterial translocation across a dysfunctional GI barrier as
the cause. Attempts at correction or prevention have
included selective gut decontamination, maintenance of
intravascular volume, and enteral feedings. Adequate enteral
feedings initiated early appear to maintain adequate GI bar-
rier function. Crucial to this effect seems to be the amino
acid glutamine, a specific nutrient that supports intestinal
mucosal cell growth and replication. Glutamine-containing
enteral nutrition may prevent or at least lessen the severity of
multisystem organ failure induced by bacterial translocation
and bypass the difficulties inherent in enteral feedings in this
group of patients. Additionally, the concept of “immune
enhancing” diets rich in arginine, nucleotides, and fish oil is
being investigated.
Activated Protein C and Corticosteroids in Sepsis
Despite recent advances in critical care, patients continue to
succumb to septic states. This may occur as a result of
delayed recognition or presentation, diminished immune
responses, or overwhelming insults.
Sepsis is associated with widespread inflammation and
intravascular coagulation. Activated protein C is an anticoag-
ulant currently being evaluated in the setting of sepsis, dif-
fuse systemic inflammation, and multiple-organ-system
dysfunction. A recent study has shown a statistically signifi-
cant decrease in 28-day mortality associated with use of acti-
vated protein C. Downsides to use of this drug include its
cost and the associated risk of coagulopathy.
The use of corticosteroids in septic patients is widely con-
troversial. One recent study revealed that small-dose hydro-
cortisone and fludrocortisone in very select patients
conferred a slight decrease in mortality. However, the routine
use of corticosteroids in all patients with sepsis is not justi-
fied. Further research is needed on this topic.

CHAPTER 32
702
Monoclonal Antibodies
Numerous monoclonal antibodies have been tested and
show promise. These agents are targeted against mediators of
sepsis and in no way obviate standard identification and
treatment of the septic source. They include antibodies
against gram-negative endotoxin as well as tumor necrosis
factor and interleukin-1. Of these, monoclonal antibodies
against tumor necrosis factor are the only ones with proven
efficacy in human trials, albeit with a modest benefit
(3.5–4% increase in survival). Appropriate selection of
patients and timing of therapy are among the ongoing clini-
cal issues. Additionally, their widespread use may be limited
by the expected prohibitive costs.
Laparoscopy
The laparoscope has become a common tool of the general
surgeon in the last 20 years, and it is only natural that its role
in critical care patients has been explored. The laparoscope is
likely to be mainly a diagnostic instrument for the near
future because of the untoward cardiovascular and respira-
tory side effects of prolonged abdominal insufflation, espe-
cially in this group of high-risk patients. If anecdotal results
are supported by further prospective investigations,
laparoscopy may supplant peritoneal lavage for the bedside
diagnosis of peritonitis or visceral perforation.
REFERENCES
Annane D et al: Effect of treatment with low doses of hydrocortisone
and fludrocortisone on mortality in patients with septic shock.
JAMA 2002;288:862–71. [PMID: 12186604]
Bernard GR et al: The Recombinant Human Activated Protein C
Worldwide Evaluation in Severe Sepsis (PROWESS) Study Group:
Efficacy and safety of recombinant human activated protein C for
severe sepsis. N Engl J Med 2001;344:699–709. [PMID: 11236773]
Bower RH et al: Early enteral administration of a formula (Impact)
supplemented with arginine, nucleotides, and fish oil in intensive
care unit patients: Results of a multicenter, prospective, random-
ized, clinical trial. Crit Care Med 1995;23:436–49. [PMID:
7874893]
Chambers A et al: Therapeutic impact of abdominopelvic computed
tomography in patients with acute abdominal symptoms. Acta
Radiol 2004;45:248–53. [PMID: 15239417]
Dhillon S et al: The therapeutic impact of abdominal ultrasound in
patients with acute abdominal symptoms. Clin Radiol
2002;57:268–71. [PMID: 12014871]
Fusco MA et al: Estimation of intra-abdominal pressure by bladder
pressure measurement: validity and methodology. J Trauma
2001;50:297–302. [PMID: 11242295]
Gagne DJ et al: Bedside diagnostic minilaparoscopy in the intensive
care patient. Surgery 2002;131:491–6. [PMID: 12019400]
Gajic O et al: Acute abdomen in the medical intensive care unit. Crit
Care Med 2002;30:1187–90. [PMID: 12072666]
Galban C et al: An immune-enhancing enteral diet reduces mortal-
ity rate and episodes of bacteremia in septic intensive care unit
patients. Crit Care Med 2000;28:643–8. [PMID: 10752808]
Gracias VH et al: Abdominal compartment syndrome in the open
abdomen. Arch Surg 2002;137:1298–1300. [PMID: 12413323]
Grassi R et al: Serial plain abdominal film findings in the assessment
of acute abdomen: spastic ileus, hypotonic ileus, mechanical ileus
and paralytic ileus. Radiol Med (Torino) 2004;108:56–70.
Kapadia F: Role of ICU in the management of the acute abdomen.
Indian J Surg 2004;66:203–8.
Keim V et al: Evaluation of Pankrin, a new serum test for diagnosis
of acute pancreatitis. Clin Chim Acta 2003;332:45–50. [PMID:
12763279]
Naidu VV et al: Diagnostic peritoneal lavage (DPL): Is it useful deci-
sion making process for management of the equivocal acute
abdomen? Trop Gastroenterol 2003;24:140–3. [PMID: 14978990]
Newton E et al: Surgical complications of selected gastrointestinal
emergencies: pitfalls in management of the acute abdomen.
Emerg Med Clin North Am 2003;21:873–907. [PMID: 14708812]
Pecoraro et al: The routine use of diagnostic laparoscopy in the inten-
sive care unit. Surg Endosc 2001;15:638–41. [PMID: 11591958]
Tjiu CS et al: Severe acute respiratory syndrome mimicking acute
abdomen. Aust NZ J Surg 2004;74:179–80.
703
33
Sofiya Reicher, MD
Viktor Eysselein, MD
Overt gastrointestinal (GI) bleeding is a quintessential gas-
troenterologic emergency. Appropriate and timely patient
resuscitation and treatment are crucial. GI bleeding carries
considerable morbidity, and 7–10% mortality rates have
been reported. Mortality is up to 30% in patients with in-
hospital onset of GI bleeding. GI bleeding is common, with
incidence of 20–100 per 100,000 adults.
Management of GI bleeding presents unique challenges
owing to the wide spectrum of etiologies, clinical presenta-
tions, and diagnostic and treatment modalities. Furthermore,
treatment approaches to GI bleeding have changed signifi-
cantly over the past decade.
This chapter discusses major causes of severe GI bleeding,
focusing on management aspects pertinent to critical care
medicine. We consider bleeding as severe when hemoglobin
falls acutely by more than 2 g/dL, requiring patient hospital-
ization and consideration of blood transfusion. Occult GI
bleeding is not discussed in this chapter.
Upper Gastrointestinal Bleeding
ESSENTIALS OF DIAGNOSIS
Hematemesis and melena: hematochezia is almost
always lower GI bleeding but may be seen with severe
upper GI bleeding.
Ulcers/erosions and varices are responsible for the
majority of upper GI bleeding.
Lifelong risk of variceal bleeding is about 50% in cir-
rhotic patients.
Hemodynamic status and comorbid illnesses are key in
the initial assessment of a bleeding patient. Age, syn-
cope or orthostatic change in blood pressure, fresh blood
in the emesis or nasogastric aspirate, or presence of car-
diopulmonary or liver disease portend poor prognosis
and need for urgent endoscopy.
General Considerations
Upper gastrointestinal (UGI) bleeding is defined by the loca-
tion of bleeding lesion proximal to the ligament of Treitz.
UGI bleeding is five to six times more common than lower
GI bleeding. It is found twice as frequently in men than in
women. Despite recent advances in management and treat-
ment, UGI bleeding mortality and medical costs remain
high. In the United States, UGI bleeding accounts for more
than 300,000 hospital admissions annually with an estimated
cost of $750 million.
Clinical Presentation
Hematemesis (vomiting of blood) is the hallmark of UGI
bleeding. Bright red blood in the emesis or in nasogastric
(NG) aspirate is indicative of recent active bleeding, whereas
“coffee grounds” indicate older blood that has had time to be
reduced by acid in the stomach. Melena, another frequent
complaint, is black tarry stools with a foul odor caused by
degradation of blood in the small intestine and colon.
The distinction between upper and lower GI bleeding
based on stool color is not always reliable. Hematochezia
(bright red blood or maroon color stools with clots), typical
of lower GI bleeding, also can occur in severe UGI bleeding.
Hematochezia in UGI bleeding is a sign of massive hemor-
rhage, and patients are usually orthostatic. In a recent series
of 80 patients with hematochezia, UGI bleeding was found in
11% of patients.
Initial Evaluation
Initial evaluation of a patient with overt GI bleeding starts
with hemodynamic status assessment, critical for proper
Gastrointestinal Bleeding
∗
∗
Tracey D. Arnell, MD, was the author of this chapter in the second
edition.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 33
704
patient triage and timely resuscitation. Syncope or lighthead-
edness, when associated with GI bleeding, are classic signs of
hemodynamic compromise. Unstable vital signs or postural
hypotension indicates significant blood volume loss (>10%),
pointing to possibly massive bleeding (Table 33-1).
Following hemodynamic assessment, a focused history
and physical examination should be performed. Timing,
amount, and color of the blood; potential risk factors for GI
bleeding; and confounding comorbidities are the main
points to be elicited.
Repeated bleeding episodes or passage of bright red blood
or large blood clots indicates clinically significant bleeding.
In trying to identify potential risk factors, a detailed medica-
tion history is particularly important. Aspirin and non-
steroidal anti-inflammatory drugs (NSAIDs) are the most
common causes of UGI bleeding. The risk appears to be
dose-related, but even patients taking low-dose (75 mg)
aspirin are at increased risk for bleeding. The risk is further
amplified when NSAIDs are taken along with corticosteroids
or bisphosphonates. Although data are limited, bleeding risk
also appears to be increased with clopidogrel. Chronic anti-
coagulation itself does not increase the risk for GI bleeding
but is thought to unmask preexisting causes of bleeding.
Particular attention should be paid to associated comor-
bidities. Confounding medical problems, in particular coro-
nary artery disease (CAD), chronic obstructive pulmonary
disease (COPD), and liver disease, affect subsequent resusci-
tative and treatment decisions. Moreover, with recent
advances in GI bleeding management, mortality mostly
results from decompensation of associated illnesses caused
by bleeding rather than from the bleeding itself.
Physical examination of a patient with GI bleeding should
focus on signs of hemodynamic instability and volume loss.
Rectal examination should be performed with attention to
stool color and presence of frank blood or melena. Stool
occult blood testing is not helpful in the acute setting.
Another important goal of the examination is to assess
the severity of comorbid medical conditions. For example,
ascites, spider angiomas, and abdominal wall collateral veins
indicate significant liver disease. Respiratory status should be
checked in all patients, particularly those with in COPD, to
determine sedation risk and the need for endotracheal intu-
bation prior to therapeutic interventions.
After initial resuscitation, physical examination usually is
followed by NG aspiration. Presence of blood in NG aspi-
rates confirms an upper GI source of bleeding, but a 10–15%
false-negative rate of NG aspiration has been reported, mostly
in patients with postpyloric bleeding lesions. Some experts
consider NG aspiration redundant if endoscopy is planned
within a few hours. However, finding of bright red blood in the
aspirate has been shown to correlate strongly with GI bleeding
mortality and is an independent predictor of rebleeding. NG
lavage also helps to clear blood and blood clots from the stom-
ach prior to endoscopy, improving diagnostic yield. To clear
the stomach prior to endoscopy, some experts also recom-
mend administration of a promotility agent such as erythro-
mycin (3 mg/kg intravenously). Cold water or saline lavage is
no longer recommended because it does not facilitate hemo-
stasis. Testing of NG aspirate for occult blood is notoriously
unreliable and should be discouraged.
The initial evaluation concludes with focused laboratory
tests, including hemoglobin, prothrombin time (PT) or inter-
national normalization ratio (INR), platelet count, and assess-
ment of renal and liver function. In patients with CAD (or high
risk for CAD), an ECG should be obtained. If chest pain or sig-
nificant ECG changes are present, cardiac biomarkers need to
be checked. Initial hemoglobin values often underestimate the
extent of blood loss because hemodilution can take up to
72 hours to occur. Thus initial hemoglobin can be misleading
in risk stratification decisions. A blood urea nitrogen
(BUN):creatinine (Cr) ratio of more than 36 may be seen in
UGI bleeding. Blood proteins are degraded by bacteria in the
upper intestinal tract and are absorbed as urea, thus increasing
BUN. The sensitivity of a BUN:Cr ratio of more than 36 for
UGI bleeding is about 90%, but specificity is quite low (~30%).
The results of the initial evaluation should provide answers
to two main questions: (1) Is bleeding moderate or massive,
based on the degree of hemodynamic compromise, and (2) is
there exacerbation of a comorbid illnesses by the bleeding?
Resuscitation
Resuscitation has a dual goal: (1) aggressively restore intravas-
cular volume and (2) optimize comorbid conditions in order
to decrease bleeding and minimize treatment-related compli-
cations. The degree of hemodynamic instability and associated
illnesses determines the extent of resuscitative measures and
monitoring. Older patients and patients with significant car-
diopulmonary disease or hemodynamic compromise should
be monitored in the ICU. For these patients, endoscopy should
be performed at the bedside in the ICU to optimize monitor-
ing. Patients with altered mental status or massive bleeding
should be electively intubated for airway protection. All
patients need two large (at least 18 gauge) intravenous
catheters placed or central venous access obtained.
Initial volume resuscitation should be done with normal
saline or lactated Ringer’s. Colloids can be given. In patients
Finding % Blood Loss
Shock 20–25%
Postural hypotension 10–20%
Normal <10%
Modified from Feldman M et al: Sleisenger and Fordtran’s
Gastrointestinal and Liver Disease. Philadelphia: Saunders, 2003,
p. 212.
Table 33–1. Gastrointestinal bleeding: vital signs and
blood loss.
GASTROINTESTINAL BLEEDING
705
with cardiopulmonary, renal, or liver disease, central venous
monitoring can be helpful to monitor volume status closely.
Concurrently with intravascular volume resuscitation,
any hemostatic abnormalities need to be corrected. A target
level for INR of less than 1.5 and platelet count greater than
50,000/μL should be sought when active GI bleeding is
occurring. Appropriate clotting factors, usually in the form
of fresh-frozen plasma, are given to achieve rapid reversal of
coagulopathy. Even if deficient, vitamin K typically does not
correct a coagulopathy fast enough and should be used only
as an adjunct to clotting factors.
Transfusion of packed red blood cells is usually consid-
ered when hemoglobin is less 10 g/dL, especially in patients
with cardiopulmonary disease. Clinical data supporting this
threshold value are limited. However, maintaining the hemo-
globin level above 10 g/dL showed a trend toward improved
survival in critically ill patients with CAD. Aiming at a hemo-
globin level of greater than 8 g/dL appears to be safe for
young, healthy patients without comorbidities.
Risk Stratification
Initial evaluation and the patient’s response to resuscitation
determine patient risk, and patients can be stratified into high-
or low-risk categories for rebleeding and mortality. Indeed,
80% of patients with UGI bleeding stop bleeding without
treatment. It is crucial to identify the remaining 20% who are
at increased risk for continued bleeding and mortality.
Multiple scoring systems have been proposed based on both
clinical and endoscopic criteria. Because physicians typically
determine risk prior to endoscopy, risk stratification schemes
based on clinical parameters alone are most practical.
Predictors of rebleeding and mortality are age greater
than 65 years, shock, comorbid illnesses, bright red blood per
rectum or in the emesis, low initial hemoglobin, and high
transfusion requirements. For example, a scoring system that
has been prospectively validated recently includes initial vital
signs, presence of syncope or melena, hemoglobin, BUN, and
presence of hepatic or cardiac disease. This system correctly
identified up to 99% of patients with serious bleeding and
more than 20% of low-risk patients who were further man-
aged as outpatients. However, because such risk stratification
schemes mostly come from cohort studies, concerns remain
about their prospective validity.
We use a simple risk stratification system based on
patient age, orthostatic changes in blood pressure or heart
rate or syncope, history of cardiopulmonary or liver disease,
and fresh blood in emesis or NG aspirate. Patients with these
clinical predictors are considered to be at high risk for con-
tinued bleeding and mortality. Such patients require ICU
monitoring and endoscopy in the ICU immediately after
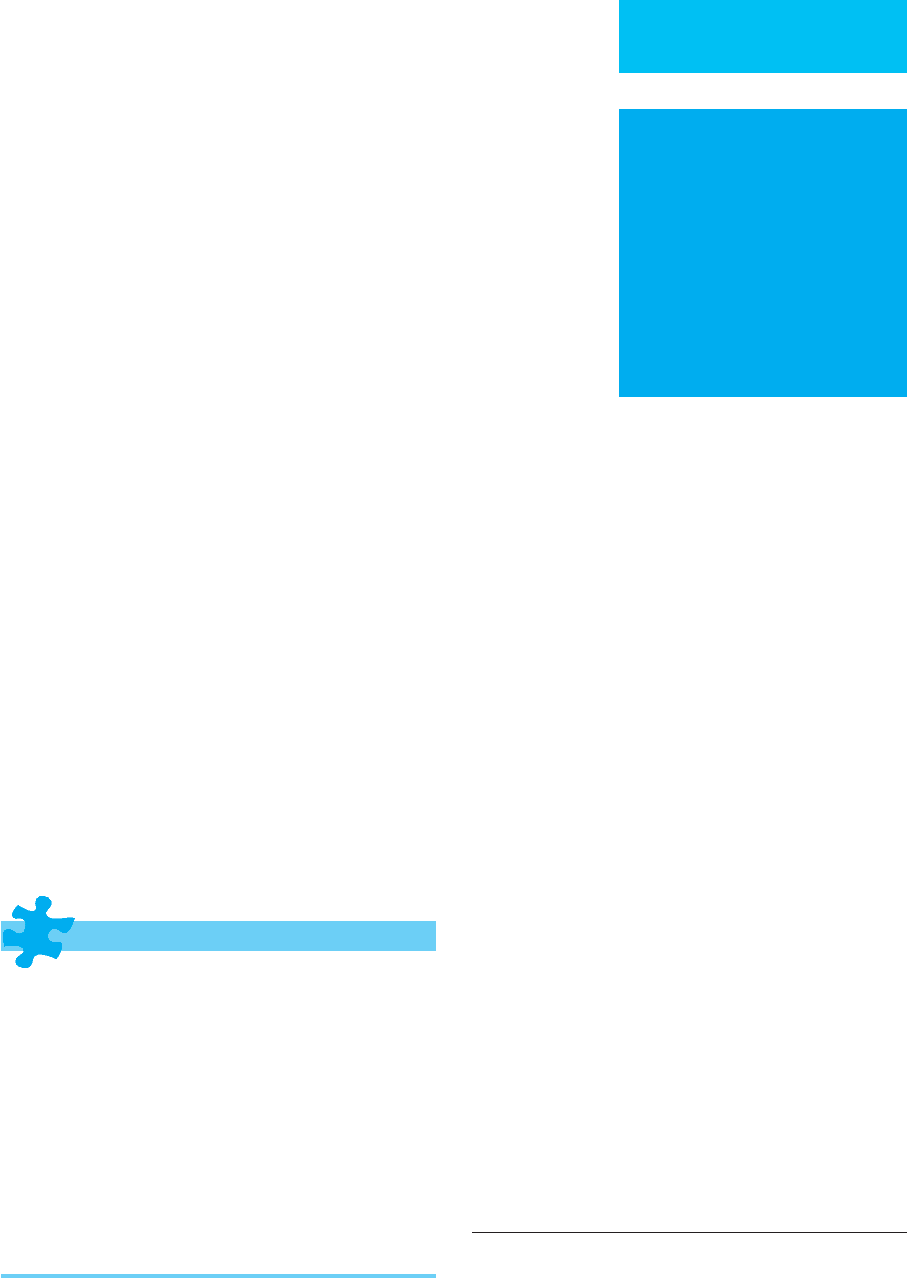
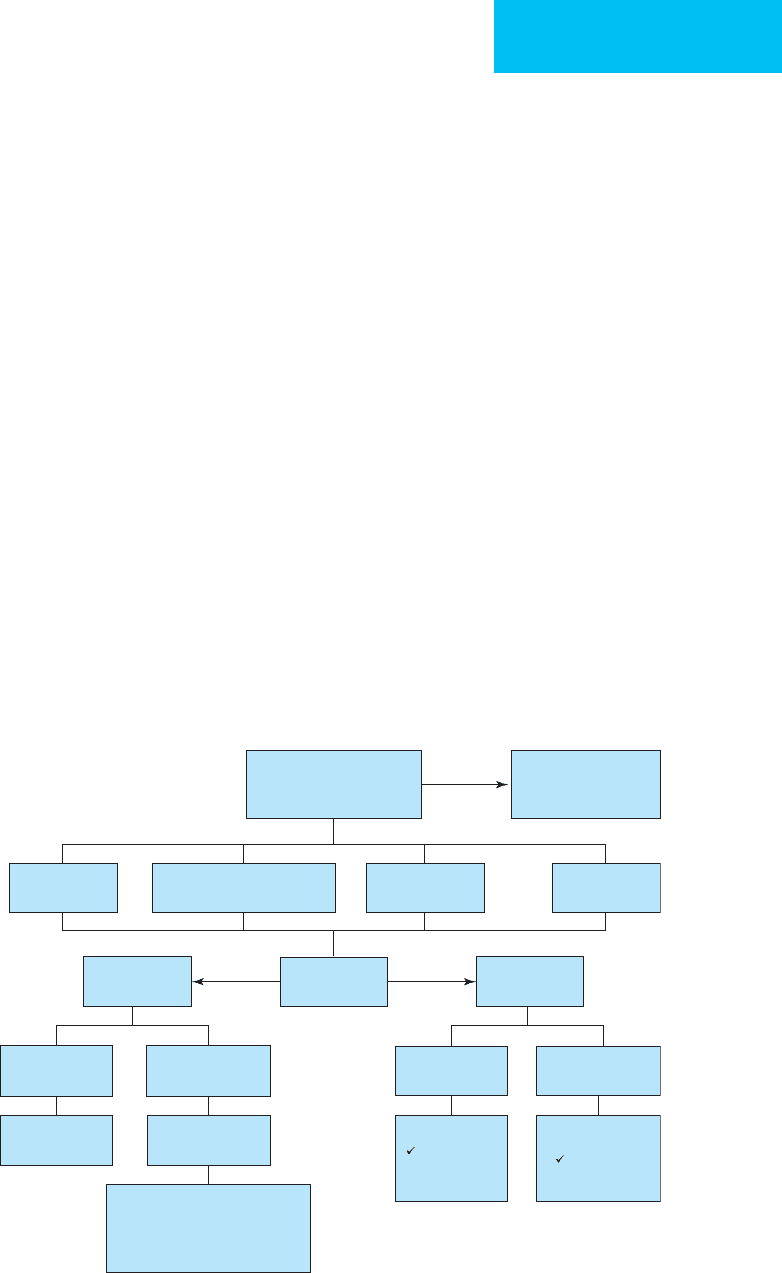
resuscitation is completed (Figure 33–1). In life-threatening
hemorrhage, when patients fail initial resuscitation, we per-
form endoscopy in the operating room with surgical service
backup rather than delaying endoscopy with repeated resus-
citation attempts.
Non-variceal
bleeding
Endoscopic
therapy
Endoscopic
therapy
Gastric
PPI IV
H. pylori
Inpatient
48–72 h
PPI PO
H. pylori
Early discharge
Hematemesis
Melena
Coffee-ground emesis
Older age
Syncope
Orthostatic hypotension
Fresh blood in
NG aspirate
Liver disease
CAD
No endoscopic
therapy
TIPS
IV octreotide, 3–5 days
antibiotics
IV PPI
Repeat EGD in 2–3 weeks
Variceal
bleeding
IV fluids, blood
IV PPI
± Octreotide/FFP
Urgent
endoscopy
Esophageal
Figure 33–1. Management of upper gastrointestinal bleeding.
CHAPTER 33
706
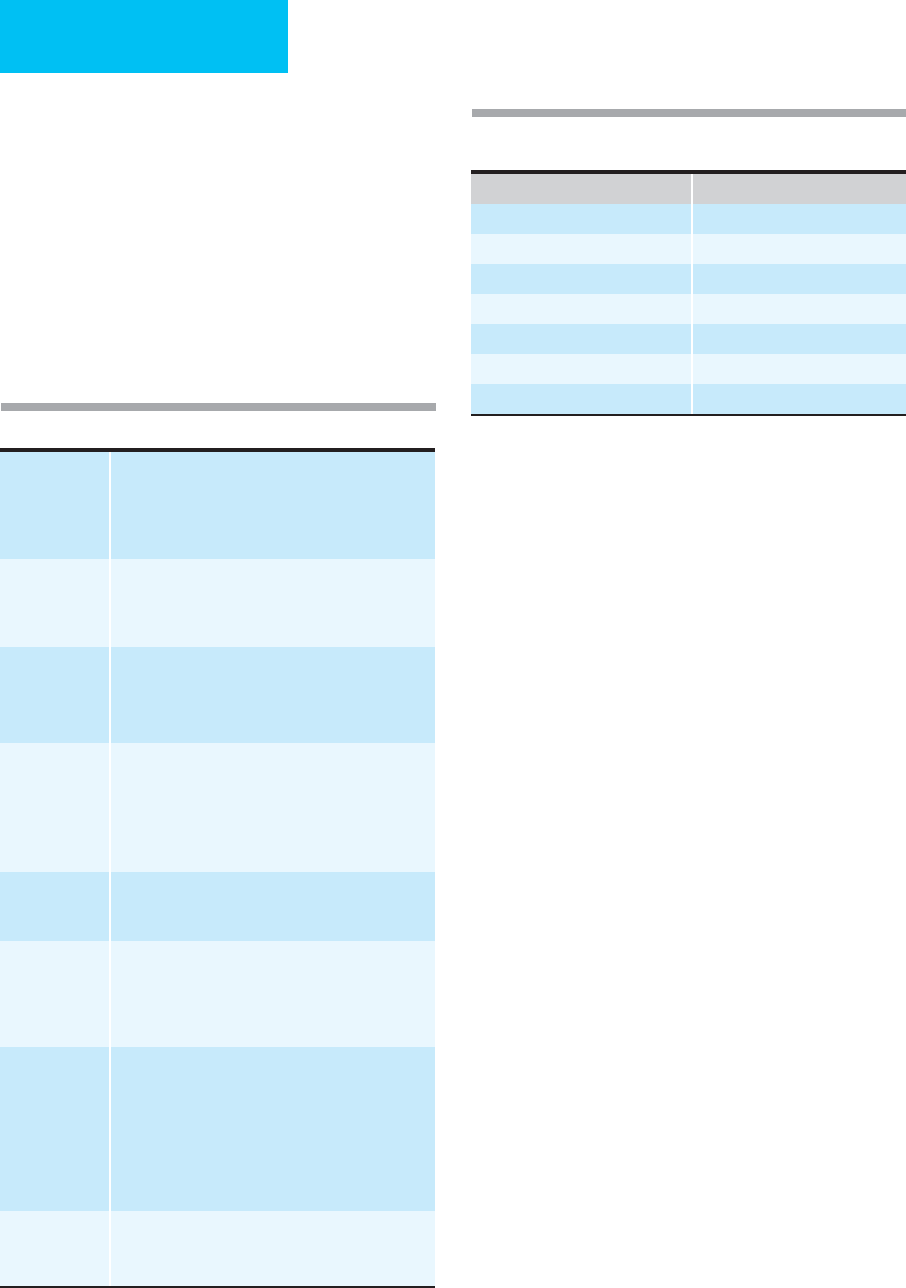
Causes of UGI Bleeding
Causes of acute UGI bleeding can be grouped into six main
categories based on anatomic and pathophysiologic parame-
ters: ulcers or erosions, portal hypertension, vascular lesions,
trauma, tumors, and miscellaneous (Table 33–2). For
decades, peptic ulcer disease has been the most common
cause of UGI bleeding, followed by esophageal varices.
Recently, the trends have changed (Table 33–3). The latest
review of the Clinical Outcomes Research Initiative (CORI)
database showed that peptic ulcer disease accounts for fewer
than 21% of UGI bleeding episodes. Nowadays, the most
common cause is nonspecific mucosal abnormalities (such
as erosions), responsible for 42% of UGI bleedings. This
changing dynamic is most likely brought about by wide-
spread use of NSAIDs and by increased recognition and treat-
ment of Helicobacter pylori infection.
A. Peptic Ulcer Disease—Peptic ulcer disease can be a
result of H. pylori infection, NSAID use, stress, or excess gas-
tric acid exposure. H. pylori is a spiral gram-negative bac-
terium found in 90% of duodenal ulcers and 70% of gastric
ulcers. It is thought to be transmitted via the fecal-oral route
and is commonly acquired in early childhood. H. pylori does
not typically invade mucosa but makes mucosa more suscep-
tible to gastric acid damage. It also stimulates host immune
response, resulting in chronic inflammation (gastritis) and
further mucosal damage. Most infected individuals are
asymptomatic, but in some, chronic inflammation and
increased gastric acid secretion lead to ulcer formation.
NSAIDs are another common cause of gastroduodenal
ulceration. Aspirin and NSAIDs are prescribed very often,
and their use is particularly widespread in the elderly because
of aspirin’s cardioprotective effects and the role of NSAIDs in
osteoarthritis management. Until recently, NSAID-related
injury was thought to be limited primarily to the stomach
and duodenum. Later reports showed that NSAIDs are also a
common cause of distal small bowel and even colonic ulcer-
ation. NSAID-induced mucosal injury results from both
direct topical and systemic effects of prostaglandin inhibi-
tion. NSAIDs also can be a contributing factor to nonhealing
ulcers from other causes. Although erosions and small ulcer-
ations are found frequently in NSAID users, most patients
are asymptomatic. The risk of clinically significant ulceration
and bleeding with chronic NSAID treatment is about 1%.
Peptic ulceration also commonly occurs with severe
stress, including major trauma, burns, sepsis, and multiorgan
system failure. The injury is likely the result of impaired
mucosal defense mechanisms secondary to decreased
mucosal blood flow. Over the past decade, the incidence of
stress-induced ulcer bleeding has been declining, with the
recently reported rate in critically ill patients only 1.5%. The
Cause Relative Frequency
Mucosal abnormalities 37%
Peptic ulcer disease 21%
Esophagitis 15%
Varices 12%
AVM 6%
Mallory-Weiss tear 5%
Tumors 4%
Table 33–3. Common causes of upper gastrointestinal
bleeding.
Table 33–2. Causes of upper gastrointestinal bleeding.
Ulcerative
erosive
Peptic ulcer disease
Infectious (
H. pylori
, CMV)
NSAIDs, ASA
Stress-induced
Zollinger-Ellison syndrome
Esophagitis
Peptic
Infectious (
Candida
, HSV, CMV)
Pill-induced (alendronate, ASA, NSAIDs, tetracycline)
Portal
hypertension
Varices
Esophageal
Gastric
Portal hypertensive gastropathy
Vascular
malformation
Arteriovenous malformations
Idiopathic angiomas
Osler-Weber-Rendu syndrome
Dieulafoy’s lesion
Radiation-induced telangiectasia
Gastric antral vascular ectasia
Traumatic,
postoperative
Mallory-Weiss tear
Foreign body
Aortoenteric fistula
Tumors Benign
Leiomyoma
Gastrointestinal stromal tumors
Lipoma
Polyps (adematous, inflammatory)
Malignant
Adenocarcinoma
GI stromal tumor
Sarcomas
Lymphoma
Carcinoid
Melanoma
Kaposi’s sarcoma
Miscellaneous Hemobilia
Hemosuccus pancreaticus
Meckel’s diverticulum
