Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

NEUROSURGICAL CRITICAL CARE
687
and vomiting, photophobia, nuchal rigidity, depressed level
of consciousness (eg, somnolence, obtundation, or coma),
cranial nerve palsies, and motor abnormalities can occur.
The severity of symptoms is related to the site and extent of
the bleeding. Following aneurysmal subarachnoid hemor-
rhage, the patient is categorized by grade using the Hunt and
Hess classification system (Table 31–3). This system has been
widely accepted and is the equivalent of the Glasgow Coma
Score in trauma patients.
B. Imaging Studies—
1. CT scanning—Ninety percent of patients with subarach-
noid hemorrhage have evidence of subarachnoid blood on
initial CT scans obtained within the first 48 hours after rup-
ture. Scanning also detects intraparenchymal and intraven-
tricular bleeding. The extent and location of subarachnoid
hemorrhage can help to determine the location of the
aneurysm and identify patients at highest risk for developing
cerebral vasospasm. Rebleeding, hydrocephalus, and cerebral
infarction also can be verified using this technique.
2. Angiography—Once the diagnosis of subarachnoid hem-
orrhage has been established, a form of cerebral angiography
should be performed unless a surgical lesion such as a signif-
icant intraparenchymal hematoma is present and requires
emergent lifesaving evacuation. Angiography is required
prior to aneurysm surgery to localize the aneurysm, define its
anatomy, and identify areas of cerebral vasospasm that may
require postponement of surgery. All cerebral vessels should
be imaged because of the occurrence of multiple aneurysms
in 15–20% of patients.
3. Transcranial Doppler ultrasonography—Transcranial
Doppler ultrasonography has become a useful technique for
monitoring patients at risk for developing vasospasm. With
progressive arterial narrowing, blood flow velocity increases
through the constricted segment and can be detected by this
procedure. Since this technique is noninvasive and portable,
it can be performed at the bedside in the ICU. It can detect
arterial narrowing prior to the development of ischemic
symptoms so that therapy aimed at improving cerebral blood
flow can be instituted.
C. Lumbar Puncture—In patients in whom no subarachnoid
hemorrhage is present on CT and the history is suggestive of
rupture of an intracranial aneurysm, lumbar puncture should
be performed. Bloody or xanthochromic fluid is the most
sensitive indicator of subarachnoid hemorrhage. CSF cultures
must be sent to rule out meningitis. However, lumbar punc-
ture never should be performed prior to CT scanning because
patients with elevated ICP are at risk for herniation following
removal of fluid from the spinal subarachnoid space.
D. Laboratory Findings—Coagulation parameters, includ-
ing a platelet count, bleeding time, and prothrombin and
partial thromboplastin times, should be obtained. If abnor-
mal clotting parameters are present, they should be corrected
rapidly because of the increased risk of rebleeding.
E. Electrocardiography—The ECG is abnormal in many
cases of subarachnoid hemorrhage and may identify cardiac
arrhythmias or ischemia that may require treatment.
Treatment
A. Surgery or Embolization—Most centers advocate early
intervention (within 24 hours of rupture) with either surgery
or embolization. Early treatment of the aneurysm has the
advantage of preventing rebleeding and allowing aggressive
therapy for vasospasm should it develop. Because of the risk
of exacerbating ischemia by brain retraction, surgery may be
delayed in patients who are medically unstable or who have
severe vasospasm.
B. Preoperative ICU Therapy—Prior to surgery, treatment
is aimed at reducing the risk of rebleeding and preventing
ischemic complications related to vasospasm. Patients
should remain at bed rest in a quiet setting. Mild analgesics
(not aspirin because of its antiplatelet properties) are used if
headache or neck pain is severe. Stool softeners are useful to
prevent straining, which can increase ICP and promote
rerupture.
C. Blood Pressure Control—Systolic blood pressure should
be maintained below 150 mm Hg; however, hypotension
must be avoided so that cerebral perfusion pressure is not
reduced to ischemic levels. Intravenous administration of
sodium nitroprusside has the advantage of being rapidly
reversible. Mild intravascular fluid augmentation using intra-
venous colloid infusion (5% albumin, 250 mL every 6–8
hours) helps to maintain adequate cerebral perfusion.
D. Reduction of Ischemic Deficits Owing to Vasospasm—
Vasospasm is the most frequent cause of morbidity and mor-
tality in patients admitted after subarachnoid hemorrhage
and occurs in 22–44% of patients. Arterial narrowing may
lead to diminished perfusion and cause infarction.
Vasospasm is induced by products of erythrocyte break-
down, and the risk of developing this complication is related
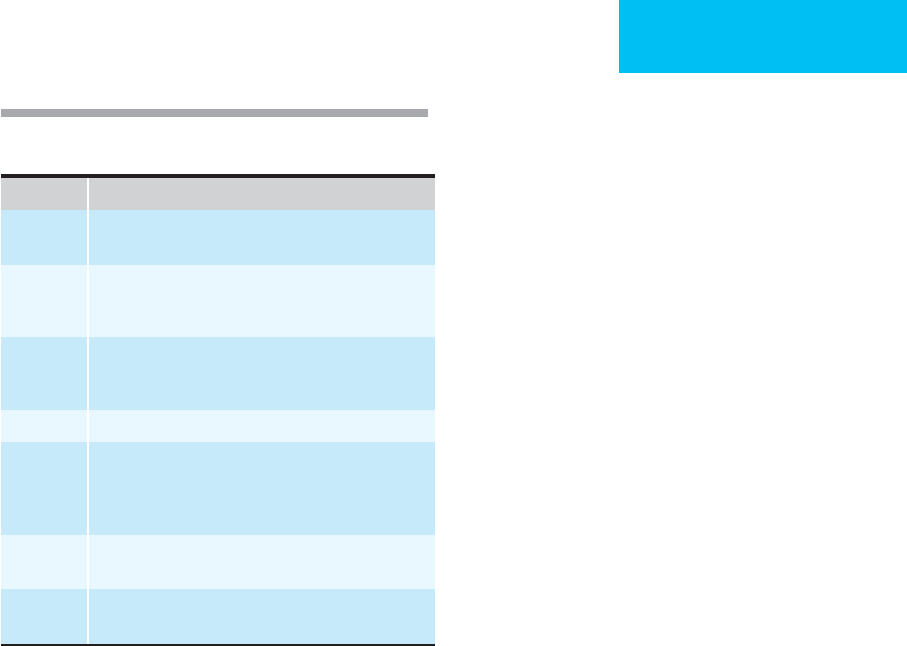
Grade 1 Asymptomatic, or minimal headache and slight nuchal
rigidity.
Grade 2 Moderate to severe headache, nuchal rigidity, no
neurologic deficit other than a cranial nerve palsy.
Grade 3 Drowsiness, confusion, or mild focal deficit.
Grade 4 Stupor, moderate to severe hemiparesis, early decere-
brate rigidity, and vegetative disturbances.
Grade 5 Deep coma, decerebrate rigidity, moribund rigidity.
Table 31–3. Hunt and Hess grades for the assessment
of patients with subarachnoid hemorrhage.
CHAPTER 31
688
to the quantity of blood in the subarachnoid space. There is
a peak incidence 4–12 days after subarachnoid hemorrhage,
and vasospasm then resolves gradually. Prophylactic therapy
using calcium channel blockers and mild volume expansion
are only partially effective. Once vasospasm has been diag-
nosed by transcranial Doppler ultrasonography or angiogra-
phy, more intense therapy is warranted. If ischemic
neurologic symptoms are evident, aggressive treatment
should be instituted immediately.
Induced hypervolemia, hemodilution, and hypertension
(triple-H therapy) may augment cerebral blood flow and
prevent ischemic cellular damage. Because cerebral autoreg-
ulation can be impaired after subarachnoid hemorrhage,
hypertension and hypervolemia may increase cerebral blood
flow directly. Decreased blood viscosity by induced hemodi-
lution can improve cerebral blood flow in regions of hypop-
erfusion. The optimal hematocrit is between 31% and 33%.
Oxygen-carrying capacity of the blood is not significantly
reduced in this range. Since aggressive therapy is often
required, placement of an indwelling pulmonary artery
catheter is recommended to monitor hemodynamics.
Therapy should be titrated to ameliorate ischemic symp-
toms. In addition, cerebral blood flow measurements may
aid in documenting adequate perfusion following treatment.
A poor outcome may occur despite triple-H therapy in most
patients with a low Glasgow Coma Score and evidence of
hydrocephalus at the onset of vasospasm.
Oral administration of the calcium channel antagonist
nimodipine (60 mg orally every 4 hours for 21 days) has been
shown to reduce ischemic neurologic deficits attributable to
vasospasm following aneurysmal subarachnoid hemorrhage.
E. Prevention of Seizures—Patients who have sustained
aneurysmal subarachnoid hemorrhage are at risk for seizures
and should receive anticonvulsants (eg, phenytoin, 18 mg/kg
intravenously initially, followed by 300–400 mg daily)
because of the risk of seizure-induced arterial hypertension,
ICP alterations, and local increased cerebral blood flow
requirements.
F. Respiratory Management—Intubation and mechanical
ventilation are required in comatose patients and those with
respiratory compromise. Mild hyperventilation can be useful
to control elevations of ICP.
G. Correction of Electrolyte Disturbances—Hyponatremia
is common following subarachnoid hemorrhage and can
lead to harmful cellular volume changes in the CNS. (Please
refer to the preceding discussion of cerebral salt wasting.)
Correction of hyponatremia should be accomplished care-
fully so that abrupt sodium changes do not occur.
Administration of hypertonic saline (3%) is often necessary
to improve the sodium level and volume depletion.
H. Intracranial Pressure Monitoring—Placement of a ven-
tricular catheter is necessary to monitor ICP in comatose
patients and to treat hydrocephalus if present. This also helps
clear erythrocyte breakdown products, which are associated
with the development of hydrocephalus. Care should be taken
to avoid rapid overdrainage of CSF because abrupt reduction
in ICP may induce aneurysm rebleeding. Many patients even-
tually will require a permanent ventriculoperitoneal shunt.
I. Antifibrinolytic Therapy—Agents such as aminocaproic
acid that inhibit dissolution of the fibrin clot have been shown
to reduce the incidence of rebleeding. However, this positive
effect is offset by an increased risk of permanent ischemic
sequelae and systemic venous thrombosis. Treatment with
antifibrinolytic agents does not improve clinical outcome fol-
lowing aneurysmal hemorrhage and should not be used.
J. Angioplasty—Even though treatment using hypervolemic
hemodilution and induced arterial hypertension is effective,
a significant number of patients do not respond to these
techniques. Balloon dilation angioplasty can mechanically
increase vessel diameter and has been shown to improve
cerebral blood flow and relieve symptoms dramatically.
Cerebral angioplasty is a new technique and is indicated,
where available, in subjects who do not respond to medical
therapy. Intraoperative vasodilating agents such as papaver-
ine also can be infused during catheter angiography.
Adams HP et al: Predicting cerebral ischemia after aneurysmal
subarachnoid hemorrhage: Influences of clinical condition, CT
results, and antifibrinolytic therapy. A report of the Cooperative
Aneurysm Study. Neurology 1987;37:1586–90.
Barker FG, Heros RC: Clinical aspects of vasospasm. Neurosurg
Clin North Am 1990;1:277–88.
Kassell NF et al: Treatment of ischemic deficits from vasospasm
with intravascular volume expansion and induced arterial
hypertension. Neurosurgery 1982;11:337–43.
Newell DW et al: Angioplasty for the treatment of symptomatic
vasospasm following subarachnoid hemorrhage. Neurosurgery
1989;71:654–60.
Ojemann RG, Heros RC, Crowell RM: Surgical Management of
Cerebrovascular Disease. Baltimore: Williams & Wilkins, 1988.
Qureshi AI et al: Early predictors of outcome in patients receiving
hypervolemic and hypertensive therapy for symptomatic
vasospasm after subarachnoid hemorrhage. Crit Care Med
2000;28:824–34. [PMID: 10752836]
Tumors of the Central Nervous System
ESSENTIALS OF DIAGNOSIS
Generalized signs of mass effect.
Aphasia.
Memory disturbance.
Hemiparesis.
Sensory impairment.
Seizure may be the presenting sign.

NEUROSURGICAL CRITICAL CARE
689
General Considerations
The critical care of patients harboring brain tumors requires
an understanding of intracranial mass effect, cerebral edema
and the blood-brain barrier, progression of neurologic
symptoms, seizures, and serum electrolyte abnormalities.
Careful serial neurologic examination and physiologic mon-
itoring can result in optimal care for the patient with a brain
tumor.
The signs of either a primary or metastatic brain tumor
are the result of the tumor’s location, mass effect, and rate of
growth and of metabolic disturbances. The Monro-Kellie
doctrine describes the relationship between intracranial vol-
ume (composed of brain, CSF, and blood) and ICP. The brain
can accommodate enlarging mass lesions until a critical vol-
ume is reached. The actual volume tolerated is increased if
growth is gradual. At this point, the ICP increases dramati-
cally (Figure 31–2). Normally, the endothelial tight junctions
of cerebral vessels (blood-brain barrier) prevent the leakage
of large solutes and water into the brain. Vessels in cerebral
tumors tend to have less constant tight junctions and may
lack certain enzymes that degrade vasoactive substances in
the brain such as leukotrienes. Reactive edema fluid thus
accumulates in the extracellular space adjacent to the tumor.
Edema can cause neurologic deterioration by increasing ICP
and causing a midline shift of brain structures. Hyponatremia
can occur in patients with CNS neoplasms and may cause
cytotoxic edema and seizures. This can occur secondary to
cerebral salt wasting, as described earlier. Conversely, hyper-
natremia can result from hypothalamic dysfunction and lack
of antidiuretic hormone response and is referred to as dia-
betes insipidus. These patients lose excessive amounts of free
water. Any serum sodium abnormality can result in altered
mental status and eventually coma and neuronal cell death.
Clinical Features
A. Symptoms and Signs—In contrast to the generalized
symptoms of mass effect, edema, and sodium imbalance,
which include headache, nausea and vomiting, and mental
status changes, the precise location of a tumor can cause spe-
cific neurologic deficits. These deficits include aphasia, mem-
ory or personality disturbances, hemiparesis, and visual or
sensory impairment. In many patients, no neurologic deficit
is present on initial presentation, and a seizure is the first
indication of a CNS neoplasm. In the awake patient, the his-
tory should be taken carefully to determine the exact initial
symptoms and the rate at which the problems have
advanced. This information can indicate the approximate
location in the nervous system and serves as a clue to the rate
of tumor growth. Neurologic examination in the ICU should
include ophthalmoscopy for papilledema, detailed mental
status and language assessment, cranial nerve tests, motor,
sensory, and reflex tests, and testing of cerebellar function.
B. Imaging Studies—A chest x-ray should be performed to
evaluate whether a metastatic source of CNS disease is likely.
The study of choice for a suspected CNS mass lesion is CT
scan or MRI. The latter technique gives finer detail and sub-
tracts the image of cortical bone. It is particularly helpful in
evaluating the posterior fossa and skull base. SPECT-
thallium scans are useful in differentiating high-grade versus
low-grade gliomas.
C. Electroencephalography—Electroencephalography can
localize dysfunctional cortex and epileptogenic foci related to
neoplastic growths.
Differential Diagnosis
Several disease processes should be considered when evaluat-
ing a patient who presents with confusion, headache, dys-
phasia, motor or sensory deficits, seizures, hyponatremia, or
any combination of these findings. Stroke usually presents
with a sudden onset of fixed neurologic signs and differs
from the progressive course of a CNS neoplasm. The gradual
progression of a neurodegenerative disease can result in
symptoms similar to those caused by a mass lesion, but pre-
liminary CT scanning or MRI can rule out this lesion.
Infections such as meningitis, encephalitis, and especially
cerebral abscess can result in global or focal neurologic dys-
function and seizures but frequently are accompanied by
fever, leukocytosis, and (in the case of cerebral abscess) char-
acteristic findings on CT scan or MRI. An important distinc-
tion to be made is whether the mass represents a primary or
metastatic lesion. In the latter, a general physical examination
with radiologic studies and metastatic evaluation is required.
Treatment
A. Immediate ICU Intervention—Treatment of the patient
with altered mental status and findings of papilledema
should begin with protection of the airway and elevation of
the head. The neck should not be flexed nor the head turned
so that optimal venous drainage of the brain via the jugular
veins can be ensured. Hyperventilation, systemic arterial
hypertension, and bradycardia are signs of Cushing’s
response (to raised ICP) and identify a patient in great dan-
ger. Mannitol, 1 g/kg, should be infused rapidly via an intra-
venous catheter. This can be followed by 0.25–0.5 g/kg
every 4 hours accompanied by frequent testing of serum
osmolarity. If seizure activity has been observed or is sus-
pected, a loading dose of phenytoin (18 mg/kg) should be
infused intravenously at a rate not to exceed 50 mg/min. A
daily dose of 300–400 mg can be started the next day. An
immediate CT scan or MRI scan should be obtained. If a
tumor is diagnosed and significant mass effect is present,
placement of a ventricular catheter can be considered in
patients at risk of critical elevation in ICP. Ventricular
catheters allow continuous ICP monitoring and drainage of
CSF. If a neurologic deficit or significant cerebral edema is
present, dexamethasone should be administered. The initial
dose can be as high as 20–24 mg intravenously, followed by
10 mg every 6 hours. This steroid can stabilize endothelial
CHAPTER 31
690
cell membranes and reduce the accumulation of cerebral
edema. For the severely ill or deteriorating patient, endotra-
cheal intubation should be performed with hyperventilation
to achieve a Pa
CO
2
of 30–35 mm Hg. Lowering the Pa
CO
2
con-
stricts cerebral arterioles and reduces the volume of blood in
the brain, thereby alleviating one component of intracranial
volume and increased ICP.
B. Nonoperative Therapy—For patients in poor medical
condition, with multiple metastatic lesions, or with a solitary
tumor in an inaccessible location, stereotactic or CT-guided
biopsy followed by radiation or chemotherapy (or both)
should be instituted. Patients should be weaned from venti-
lator support and ventricular drainage whenever possible.
This may be difficult in a deteriorating patient because of
ethical and family considerations.
C. Surgery—The goals of surgery are to obtain a tissue diag-
nosis and decrease the mass effect by safely removing as
much of the lesion as possible. Craniotomy (removal of a
replaceable bone flap) or craniectomy (removal of sections of
the base of the skull that are not replaced) with microscope-
assisted removal of the tumor can be accomplished with very
satisfactory morbidity and mortality results. Bipolar coagu-
lation forceps, suction and irrigation, ultrasonic aspirators,
and (less frequently) lasers can be used to precisely remove
tumor while limiting damage to surrounding brain. For
tumors in the sellar region, a transnasal, transsphenoidal
approach is most useful. The risks of operation include
increased neurologic deficit, bleeding, deep vein thrombosis,
pulmonary embolism, and death. Mortality rates in most
large centers for patients undergoing removal of intracranial
tumors are under 5%.
Current Controversies and Unresolved Issues
Several aspects of the care of critically ill patients harboring
brain tumors remain controversial. It is still unclear what the
roles of surgery and radiation are in the patient with a low-
grade primary brain tumor. The risk of slow progression of
tumor growth over many years may not outweigh the ill
effects of operation or postirradiation angiopathy and neu-
ronal death (ie, radiation necrosis). Another debatable aspect
of care is the role of chemotherapy for high-grade primary
tumors. Prolongation of survival of 3–6 months with
chemotherapy (beyond the 6–12-month survival of surgery
and radiation alone) may not outweigh the short-term mor-
bidity associated with intravenous antineoplastic therapy.
Deep vein thrombosis and pulmonary embolism repre-
sent a considerable risk to the patient with a brain tumor
who is less mobile or bedridden, yet the role of perioperative
anticoagulation remains an unresolved issue. The duration
of prophylactic anticonvulsant therapy following craniotomy
remains debatable. The range in practice is between 1 month
and 12 months.
Future issues that are likely to make a major impact on the
therapy for critically ill patients with brain tumors include
advances in stereotactic radiation, manipulation of the
blood-brain barrier for selective delivery of antineoplastic
agents to the tumor, and molecular engineering to selectively
transfect tumor cells with gene fragments capable of inducing
differentiation and stopping cellular proliferation. At the pres-
ent time, however, surgical reduction of the total malignant
cell mass and radiation remain standard therapy for malignant
brain tumors. Frameless image-guided neurosurgery has
improved intraoperative visualization of these tumors and
provides hope for improved outcomes in the future.
Brennan RW: Differential diagnosis of altered states of conscious-
ness. In Youmans JR (ed), Neurological Surgery: A
Comprehensive Reference Guide to the Diagnosis and
Management of Neurosurgical Problems, Vol. 1. Philadelphia:
Saunders, 1990.
Plum F, Posner JB: The Diagnosis of Stupor and Coma, 3d ed. San
Francisco: Davis, 1985.
Wilkinson HK: Intracranial pressure. In Youmans JR (ed),
Neurological Surgery: A Comprehensive Reference Guide to the
Diagnosis and Management of Neurosurgical Problems, Vol. 2.
Philadelphia: Saunders, 1990.
Cervical Spinal Cord Injuries
ESSENTIALS OF DIAGNOSIS
Neck pain.
Motor or sensory deficits.
Hypoventilation.
Neurogenic shock.
Priapism.
General Considerations
Approximately 10,000 new cervical and thoracic spinal cord
injuries occur each year in the United States. Most result
from motor vehicle accidents, falls, gunshot wounds, and
sporting accidents. Improved acute management has permit-
ted many patients to survive the initial injury and to have a
near-normal life expectancy. Adolescents and young adults
suffer the highest incidence of spinal cord injuries, with the
majority occurring in young males. Although the loss of
motor and sensory function imposes a catastrophic physical
and emotional handicap, many spinal cord injury patients
are able to return to a nondependent functional state.
Most spinal cord injuries occur in the mobile cervical
region. The cervical cord contains lower motor neurons as
well as long tracts conveying motor and sensory fibers that, if
damaged, can result in variable neurologic dysfunction. In
addition, the cervical cord also conducts vital respiratory and
sympathetic functions that can be damaged following
trauma, leading to devastating respiratory or circulatory
collapse. Secondary events such as hypotension, hypoxia, and
reinjury of the cord can cause further neurologic deterioration.

NEUROSURGICAL CRITICAL CARE
691
Because of these unique features, all patients with cervical
cord injuries should be admitted to an ICU staffed by per-
sonnel experienced with the complex care of spinal cord
injuries.
Pathophysiology
There are a number of anatomic, chemical, and vascular
changes that occur in response to blunt injury of the spinal
cord. From immediately following and up to 3–5 hours after
injury, there is focal swelling of the cord owing to disruption
of blood vessels and their endothelial tight junctions. This
leads to localized bleeding and leakage of albumin, neuro-
transmitters, extracellular calcium, lactate, and prostaglandins.
There is a decrease in local blood flow beginning in the cen-
tral regions of the cord and spreading to the surrounding
white matter (centripetal decrease in blood flow). This leads
to worsening edema over the first 2–3 days and central cavi-
tary necrosis over the ensuing week. The level of injury may
rise as much as two vertebral levels in response to these sec-
ondary events. Diminished swelling followed by cord atro-
phy becomes evident after the first week after injury.
Experimental and clinical treatment strategies are aimed at
blocking this cascade of secondary events following spinal
cord contusion. Calcium channel blockers, diuretics, corti-
costeroids, and other free-radical scavengers may be helpful,
although their true efficacy is debated.
Clinical Features
A. History—The key to the initial diagnosis of cervical spine
injury is maintaining a high level of suspicion for an under-
lying bony or ligamentous injury. This is especially true in
patients involved in motor vehicle accidents or significant
falls, particularly if they have other associated injuries such as
head trauma or extremity fractures.
Many trauma patients are conscious and may complain
of neck pain, numbness, or weakness suggestive of spinal
cord injury. In trauma patients with altered mental status, it
is best to assume that an unstable cervical spine injury is
present until proved otherwise by radiography.
B. Symptoms and Signs—Several complications of cervical
cord injury may require immediate attention and therefore
must be diagnosed promptly. Hypoventilation and respira-
tory compromise secondary to injury of cord segments sup-
plying the phrenic nerve (C3–5) usually can be diagnosed
easily and require immediate assisted ventilation. Although
respiratory dysfunction may not be apparent immediately
after a high cervical injury, respiratory status may deteriorate
during the first few days in the ICU. This can be secondary to
primary muscle fatigue or “ascending” cord involvement
from edema or ischemia. Neurogenic shock may be encoun-
tered following cervical cord injury. This results from inter-
ruption of sympathetic fibers that are descending to the
T1–L2 spinal cord segments and can lead to hypotension,
bradycardia, and hypothermia. Priapism also may occur in
males owing to unopposed parasympathetic impulses.
Although neurogenic shock patients do not appear to be
hypovolemic (eg, the skin is warm and the pulse is slow),
their hypotension responds to rapid administration of
intravascular colloid and crystalloid solutions, and use of
vasopressors such as dopamine or dobutamine is often indi-
cated to maintain arterial pressure and perfusion. Central
venous pressure and cardiac monitoring may be required
along with the frequent assessment of temperature.
After initial resuscitation, meticulous neurologic assess-
ment should be performed to determine the level and sever-
ity of spinal cord damage. Evaluation should include
assessment of motor strength; sensory testing; assessment of
reflexes, including abdominal cutaneous, cremasteric, and
bulbocavernosus reflexes; rectal and perirectal examination;
and palpation of the entire spine while the patient is carefully
log-rolled to maintain spinal alignment.
A complete spinal cord lesion is defined as total loss of
motor and sensory function below the level of injury. One
must not be confused by spinal mass reflexes such as reflex
withdrawal of an extremity in response to pain, which is not
representative of true motor function and may mistakenly
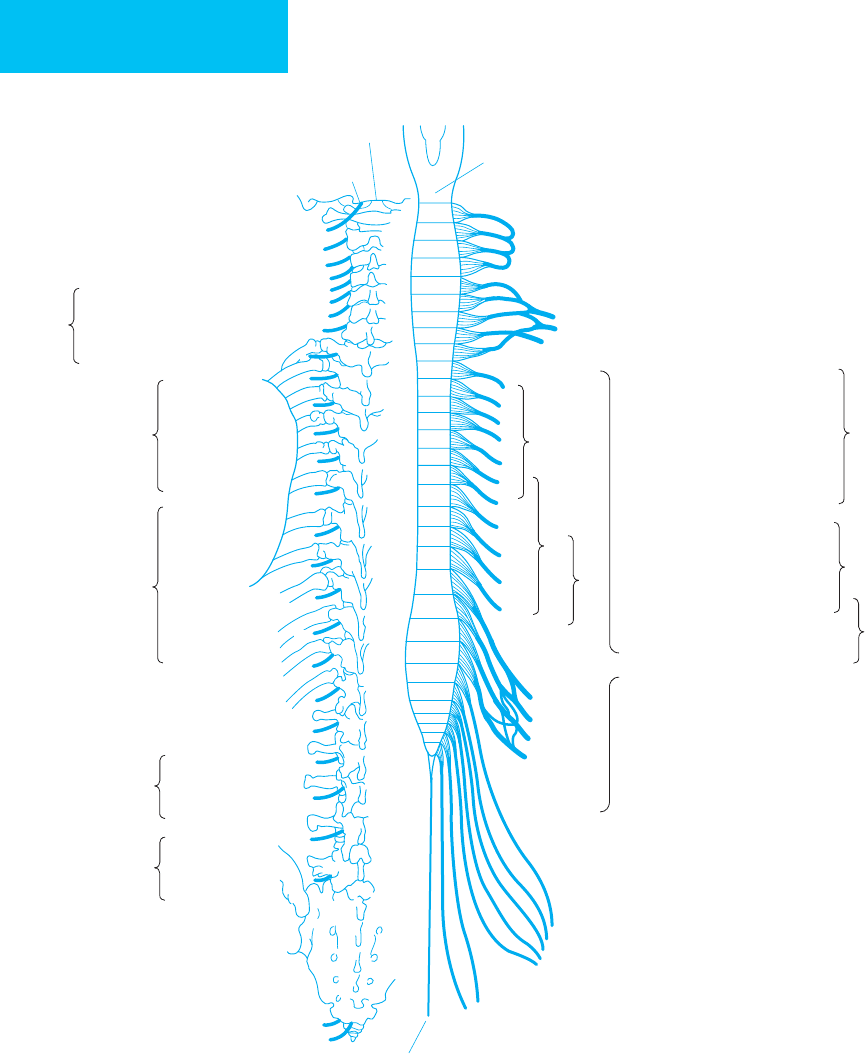
lead to classification of the injury as incomplete. Figure 31–4
portrays the motor and sensory levels of the spinal cord, and
Table 31–4 lists the important motor findings associated with
injuries at different cervical levels.
Patients with complete cervical cord lesions present ini-
tially in a state known as spinal shock, defined as a total loss of
motor and sensory function associated with an areflexic, flac-
cid trunk and extremities below the level of the lesion. In a
complete lesion, spinal shock occurs immediately after the
injury and may persist for 1–2 weeks, after which time upper
motor neuron findings develop with increased deep tendon
reflexes and increased muscular tone associated with spastic-
ity. However, abdominal cutaneous reflexes remain absent.
The mass reflex may occur and is characterized by exagger-
ated involuntary extremity movement owing to loss of
descending cortical inhibition. Interruption of autonomic
fibers results in bladder paralysis, urinary retention, poor gas-
tric emptying, and intestinal ileus with abdominal distention.
An incomplete lesion is characterized by evidence of any
motor or sensory function below the level of the lesion. In
severe incomplete injuries, spinal shock may be present ini-
tially but begins to wear off within 24 hours. Patients with
incomplete cervical cord injuries generally show some degree
of neurologic recovery (up to 40% may make a functional
recovery), whereas patients with true complete injuries
demonstrate no significant neurologic recovery. Rectal
examination is an essential part of the complete neurologic
assessment because any evidence of sacral sparing, such as
voluntary sphincter contraction or sensation in the perianal
region, classifies the injury as incomplete and implies the
possibility of some functional recovery. Important incom-
plete spinal cord injury syndromes include the following:
1. Anterior cord syndrome—This syndrome is associated
most often with cervical flexion injuries and results in loss of
CHAPTER 31
692
Spinal
nerves
Spinous processes
Medulla
oblongata
Cervical
plexus
Brachial
plexus
F
i
r
s
t
r
i
b
1
1
2
3
4
5
6
7
8
1
2
2
3
3
4
4
5
5
6
7
8
9
9
10
10
11
12
1
2
3
4
4
5
1
1
2
2
3
3
4
4
5
1
1
5
3
2
1
12
11
8
7
6
1
2
3
4
5
6
7
8
1
2
23
3
4
4
5
5
6
6
7
7
8
8
9
9
10
10
11
11
12
1
2
2
3
3
4
4
5
1
2
1
3
5
4
1
12
1
1
2
6
3
4
5
7
2
3
4
5
6
7
8
1
5
5
Sacro-
coccygeal
plexus
Filum terminale
Hearing, equilibrium
Taste
Pharynx, esophagus
Larynx, trachea
Occipital region (C1, 2)
Neck region (C2, 3, 4)
Shoulder (C4, 5)
Axillary (C5, 6)
Radial (C6, 7, 8)
Median (C6, 7, 8)
Ulnar (C8, T1)
Arm
Thorax
Femoral
region
(L1, 2, 3)
Abdomen
Epigastrium
Spine pf
scapula (T3)
Inferior
angle of
scapula (T7)
Umbilicus
(T10)
Anterior
Median
Lateral
Posterior
Crural
region
(L4, 5)
Median
Lateral
SENSORY LEVELS
Intercostal
and thoracic
muscles
Lumbar muscles
Lumber plexusSacral plexus
Arm
Forearm
Hand
Abdominal muscles
Scrotum, penis
Labia
Perineum (S1, 2)
Bladder (S3, 4)
Rectum (S4, 5)
Anus (S5, C1)
Gluteal region (T12, L1)
Inguinal region (L1, 2)
MOTOR LEVELS
Facial muscles VII
Pharyngeal, palatine muscles X
Laryngeal muscles XI
Tongue muscles XII
Esophagus X
Sternocleidomastoid XI (C1, 2, 3)
Neck muscles (C1, 2, 3)
Trapezius (C3, 4)
Rhomboids (C4, 5)
Diaphragm (C3, 4, 5)
Supra-, infraspinatus (C4, 5, 6)
Deltoid, brachioradialis, and
biceps (C5, 6)
Serratus anterior (C5, 6, 7)
Pectoralis major (C5, 6, 7, 8)
Teres minor (C4, 5)
Pronators (C6, 7, 8, T1)
Triceps (C6, 7, 8)
Long extensors of carpi and
digits (C6, 7, 8)
Latissimus dorsi, teres major
(C5, 6, 7, 8)
Long flexors (C7, 8, T1)
Thumb extensors (C7, 8)
Interossei, lumbricales, thenar,
hypothenar (C8, T1)
Iliopsoas (L1, 2, 3)
Sartorius (L2, 3)
Quadriceps femoris (L2, 3, 4)
Gluteal muscles (L4, 5, S1)
Tensor fasciae latae (L4, 5)
Adductors of femur (L2, 3, 4)
Abductors of femur (L4, 5, S1)
Tibialis anterior (L5)
Gastrocnemius, soleus (L5, S1, 2)
Biceps, semitendinosus,
semimembranosus (L4, 5, S1)
Obturator, piriformis, quadratus
femoris (L4, 5, S1)
Flexors of the foot, extensors
of toes (L5, S1)
Peronei (L5, S1)
Flexors of toes (L5, S1, 2)
Interossei (S1, 2)
Perineal muscles (S3, 4)
Vesicular muscles (S4, 5)
Rectal muscles (S4, 5, C1)
Figure 31–4. Motor and sensory levels of the spinal cord. (Reproduced, with permission, from Waxman SG: Correlative
Neuroanatomy, 20th ed. New York: McGraw-Hill, 2000.)
NEUROSURGICAL CRITICAL CARE
693
motor function and pain and temperature perception (ie,
corticospinal and spinothalamic tracts), with preservation of
proprioception and perception of vibration and light touch
(dorsal columns) below the level of the lesion. This is
thought to result either from direct anterior trauma or from
injury to the anterior spinal artery, which supplies the ante-
rior two-thirds of the spinal cord. The paired posterior spinal
arteries supply the dorsal columns and the posterior one-
third of the cord.
2. Central cord syndrome—This is most commonly due
to a hyperextension injury in an older patient with preexist-
ing cervical spondylosis or stenosis. The motor and sensory
deficits are greater in the upper extremities (more pro-
nounced distally) than in the lower extremities. Hemorrhagic
necrosis in the central portions (eg, gray matter) of the cer-
vical cord results in upper extremity weakness. Since the
lumbar leg and sacral tracts are peripheral in the cervical
cord, they are relatively spared.
3. Brown-Séquard’s syndrome—This syndrome occurs
with hemisection of the spinal cord, usually from penetrat-
ing injuries such as stab or gunshot wounds. The result is
ipsilateral loss of motor and dorsal column function (ie,
vibration, proprioception, and discriminatory touch)
immediately below the level of injury associated with con-
tralateral loss of pain and temperature sensation one or two
levels below the injury (spinothalamic tracts decussate
within one to two levels of their entry).
4. Posterior spinal cord syndrome—This rare syndrome
results from disruption of the posterior columns, causing
loss of vibration, proprioception, and discriminatory sense
below the level of the lesion.
C. Imaging Studies—Radiographs are essential for the eval-
uation and diagnosis of cervical spine injuries. These should
include a cervical spine series with lateral, anteroposterior,
and odontoid (open mouth) views. Radiographs are
inspected for the presence of prevertebral soft tissue swelling,
alignment of the anterior and posterior aspects of the verte-
bral bodies, angulation of the bony spinal canal, and the pres-
ence of fractures. The odontoid view is essential to diagnose
axis (C2) fractures or Jefferson fractures of the ring of the
atlas (displacement of the lateral masses of C1). Ligamentous
damage should be suspected in patients with minimal sublux-
ation or persistent neck pain without evidence of a fracture.
Dynamic flexion and extension cervical radiographs, which
should only be considered in awake and cooperative patients,
are useful to detect instability secondary to ligamentous
injury. These x-rays may be performed several days after the
initial injury so that muscle spasms, which can mask instabil-
ity by limiting subluxation, may subside.
CT scanning is excellent for visualizing the bony struc-
tures of the spinal canal and is the next step in evaluating a
fracture or subluxation. In patients with neurologic symp-
toms or signs and no radiographic evidence of bony abnor-
malities, MRI should be obtained. MRI demonstrates the
cord and soft tissue structures with outstanding clarity and
can identify intraaxial contusions and cord compression
from a herniated disk or hematoma. However, MRI does not
demonstrate bony structures very well.
The role of myelography in spinal cord injury is contro-
versial. Myelography should be performed if there is a signif-
icant incomplete neurologic deficit that cannot be explained
by bony abnormalities and if an MRI cannot be obtained.
D. Other Studies—Somatosensory evoked potentials are
occasionally useful to confirm or dispute the diagnosis of
complete spinal cord injury. This is especially true in patients
who are difficult to examine, such as those with altered men-
tal status.
Treatment
Optimal treatment of spinal cord injuries must be initiated at
the scene of the accident. The spinal cord is susceptible to
reinjury after the primary insult, making prevention of sec-
ondary injury one of the most important aims of therapy.
This includes immediate spinal immobilization with sand-
bags or a hard collar and rapid correction of hypoxia,
hypotension, shock, or hypothermia, if present. Early place-
ment of a nasogastric tube and an indwelling urinary
catheter are necessary because an atonic bladder and GI tract
commonly accompany cervical cord injuries.
Segment Important Characteristics
C1 to C3 No arm motor function. Absent respiratory muscle
contractions. If C3 is spared, patient can support neck.
C4 If the C4 segment is functional, patients may only
require initial ventilatory support and then, after
strengthening, may self-ventilate.
C5 Useful movements of the deltoid, biceps, and usually
the brachialis muscles are present, permitting shoulder
shrug, elbow flexion, and forearm pronation.
C6 Allows wrist extension.
C7 Functional upper extremity movements with maintained
innervation of the triceps (elbow extension), extensor
digitorum (finger extension), and flexor carpi ulnaris
(wrist extension). Weak finger flexors with poor grasp.
C8 Improved hand function due to innervation of most
hand intrinsic muscles.
T1 Complete hand strength maintained because of innerva-
tion of all hand intrinsic muscles.
Table 31–4. Important motor characteristics associated
with injuries at different cervical levels and T1.

CHAPTER 31
694
Serial neurologic examinations are important to detect
signs of deterioration so that corrective measures can be
taken expeditiously. The patient must be maintained in opti-
mal physiologic condition to maximize the chances of neu-
rologic repair and recovery.
A. Respiratory Care—Patients with cervical cord injuries
frequently develop worsening of their respiratory status in
the ICU. This may be secondary to diaphragm fatigue or
ascending neurologic damage from edema or ischemia and
may require prompt respiratory support. Intubation in
patients with unstable cervical injuries should be performed
using fiberoptic nasotracheal intubation (see below for selec-
tion of neuromuscular blocking agents). Hypoventilation,
particularly during sleep, is not uncommon in the early stages
following high cervical cord injury and may require nighttime
ventilation. This is probably due to an impaired respiratory
drive to CO
2
or diaphragm fatigue. A high index of suspicion
for this disorder, which usually resolves in 1–2 weeks, must be
maintained in the early phases of ICU care.
Aggressive pulmonary toilet and aerosol bronchodilators
should be used to avoid atelectasis, mucus plugs, and pneu-
monia. Prophylactic antibiotics should not be used to pre-
vent pulmonary infections.
B. Hemodynamic Support—During spinal shock, decreased
sympathetic outflow may be manifested by bradycardia or
hypotension. However, one must not overlook a source of
hemorrhage (eg, liver laceration or pelvic fracture) because
such patients will not complain of pain. Hypotension from
spinal shock usually responds well to intravenous infusions
of crystalloid and colloid solutions. Vasopressors such as
dopamine may be required. Atropine, although short-acting,
may rapidly reverse hypotension associated with bradycardia.
Placement of a temporary cardiac pacemaker may be required
for severe bradycardia. Following recovery from spinal shock,
reflex hypertension, sweating, pilomotor erection, and rarely,
bradycardia or cardiac arrest (autonomic dysreflexia) may
occur. This is usually precipitated by painful stimuli such as
bladder catheterization, respiratory suctioning, or colorectal
manipulation. Hypertensive crises, which can be life-
threatening, should be treated by elimination of the precipi-
tating stimulus and administration of rapid-acting
intravenous antihypertensive agents. In recurrent severe
attacks, prophylaxis with phenoxybenzamine may be useful.
C. Cervical Immobilization—Unstable malaligned cervical
spine subluxations or fractures should be managed initially
with external immobilization. This can be achieved by
attaching tongs or a halo ring to the patient’s skull and apply-
ing distraction force through a pulley system attached to
weights. One must exclude the presence of atlanto-occipital
dislocation because traction in this condition can result in
overdistraction and serious injury. Gentle application of
5–10 lb is used initially, gradually increasing by up to 5 lb per
cervical level (eg, 20 lb for C4 and 30 lb for C6). More weight
may be required for reduction, but no more than 10 lb per
level should be administered. After each weight increase, the
lateral x-ray should be repeated to determine if realignment
has been achieved. It is often necessary to administer muscle
relaxants such as diazepam (5–10 mg intravenously every
8 hours) during skeletal traction to reduce muscle contrac-
tions or spasms that can hinder spinal realignment.
Application of a halo vest orthosis may be the proper choice
for certain bony injuries of the cervical spine.
D. Surgery—The principal goal in the management of cervi-
cal spine injuries is prevention of secondary neurologic
injury and provision of an optimal environment for recov-
ery. Securing a stable cervical spine (ie, bones, muscles, and
ligaments) will prevent further neurologic injury and reduce
the chance for persistent cervical pain resulting from insta-
bility. In general, bony lesions heal well if immobilized prop-
erly, whereas ligamentous injuries typically do not heal. The
indications for operation are decompression of incompletely
injured neural tissue and reduction and stabilization of
malaligned or unstable cervical segments. Some of the basic
features and treatment modalities for several common cervi-
cal injuries are outlined below.
1. Atlanto-occipital dislocation—These injuries, which
are seen most commonly in children owing to immature
craniovertebral articulations, are often fatal. They involve
extensive ligamentous disruption and can cause injury to the
brain stem, cervical cord, nerve roots, or vertebral artery.
Traction should not be used because it can increase the
distraction and cause further CNS damage. These injuries
are highly unstable and require operative bony fusion.
2. Jefferson fracture of the atlas—This is a burst frac-
ture of the ring of the atlas resulting from an axial force and
is usually asymptomatic. If combined displacement of the
left and right lateral masses on open mouth x-ray is more
than 6.9 mm, immobilization with a halo vest is suggested;
otherwise, a hard cervical collar is sufficient.
3. Axis fractures—A type 1 odontoid fracture involves
only the tip of the odontoid and can be treated with hard cer-
vical collar immobilization. Fractures through the odontoid
base are classified as type 2 and have a high incidence of
nonunion. Current treatment recommendations are for sur-
gical fusion if the fracture is displaced more than 6 mm or
halo vest immobilization for fractures displaced less than
6 mm. Anterior odontoid screw fixation or posterior
atlantoaxial fixation may be performed. Type 3 odontoid
fractures involve the base of the odontoid with extension into
the vertebral body and require only halo vest immobilization
for fusion. Hangman fractures are bilateral fractures of the
C2 pedicles with anterior displacement of C2 onto C3. They
are usually due to hyperextension injuries such as automo-
bile accidents in which the head hits the windshield.
Hangman fractures may be unstable and require traction ini-
tially if malalignment is present, followed by immobilization
in a halo vest. Isolated laminar or spinous process fractures

NEUROSURGICAL CRITICAL CARE
695
of the axis usually can be treated with a hard cervical collar.
Treatment for combined atlas and axis fractures is usually
based on the type of axis fracture present.
4. Wedge compression fracture—This results from a
hyperflexion force causing compression of one vertebra
against an adjacent vertebra. The optimal management of
these injuries is controversial. Simple wedge fractures with-
out associated ligamentous injury or significant subluxation
heal well in a hard cervical collar. If the kyphotic angulation
is significant, or if instability is present, early surgical fusion
or closed realignment with skeletal traction followed by halo
vest application may be warranted. Persistent instability may
be present in 15% of patients treated by immobilization only
and requires subsequent operative surgical fusion. Care must
be taken in patients with neurologic deficits to exclude a
compressive lesion such as an extruded cervical disk that may
require early operation.
5. Flexion teardrop fracture—This is secondary to severe
hyperflexion with disruption of the intervertebral disk associ-
ated with ligamentous damage and a fracture through the
anteroinferior vertebral body. This is a highly unstable injury
often associated with devastating neurologic damage and
requires early realignment by traction. Management after initial
stabilization is controversial and may include halo vest immobi-
lization or surgical fusion. Care must be taken to exclude any
compressive lesions, such as bone or disk material, that may
contribute to neurologic dysfunction and require removal.
6. Facet dislocation—Bilateral facet dislocation occurs
when the inferior articular facet of the upper vertebra slides
forward over the superior articular facet of the lower verte-
bra. This is due to severe hyperflexion injury and is unstable.
Lateral cervical x-rays show anterior subluxation of the
superior vertebra by over 50% of the length of the vertebral
body. Anteroposterior views demonstrate alignment of the
spinous processes. Immediate closed reduction using skele-
tal traction should be attempted; if this fails, open surgical
reduction may be necessary. Surgical fusion is required in
either case. Unilateral facet dislocation results from simulta-
neous flexion and rotation injuries. The lateral cervical
spine x-ray shows anterior subluxation of the superior ver-
tebra, but this is only 30% or less of the length of the verte-
bral body. The spinous processes on anteroposterior views
are rotated and do not align. Although the unilateral locked
facet is a stable injury, it is commonly associated with nerve
root injury and chronic pain. In these patients, closed or
open reduction may be beneficial.
E. Corticosteroids—Although previous versions of this chap-
ter have advocated use of intravenous methylprednisolone
acutely after spinal cord injury, this therapy is now consid-
ered an option rather than a recommendation. Critical
analysis of the original data as well as the clinical experiences
over the past several years have not come out with significant
efficacy of this medication regime. Some clinicians may wish
to use the steroid in the hope that local nerve root improve-
ment may be hastened, but the decision needs to be weighed
against potential complications.
F. Pulmonary Embolism Prophylaxis—Pulmonary embolism
is a constant threat to patients with weak limbs and should
be combated using subcutaneous heparin (5000 units twice
daily), pneumatic compression stockings, or both.
Intravascular insertion of a vena cava filter is highly recom-
mended for patients with lower limb paralysis.
G. Gastrointestinal Considerations—Atony and paralytic ileus
may occur for days to weeks following spinal cord injury.
Early nasogastric decompression is required to reduce
abdominal distention. Serum electrolytes should be evalu-
ated regularly. Because these patients are in a catabolic state
after injury, they often require early nutritional support.
Reflex evacuation of the rectum occurs following the acute
phase of spinal cord injury and can be aided by a regular reg-
imen of laxative agents.
H. Urinary Care—Bladder atonia and sphincter paralysis result
in urinary retention after spinal cord injury. Initial placement
of an indwelling bladder catheter is required, but the catheter
should not be left in place for longer than 2–3 weeks. After this
time, reflex emptying of the neurogenic bladder can occur
spontaneously or in response to stimuli such as suprapubic
compression. Many patients require intermittent bladder
catheterization, and this can be self-administered using metic-
ulous technique. Urologic consultation is frequently helpful to
determine individual bladder care programs.
I. Skin Care—Prevention of decubitus ulcers is a primary con-
cern in spinal injury patients. Patients should be turned at
least every 2 hours, pressure points should be padded, and
kinetic therapy beds should be used if available.
J. Avoidance of Depolarizing Neuromuscular Blocking
Agents—Denervated muscles are hypersensitive to depolar-
ization, and administration of a depolarizing agent (eg, suc-
cinylcholine) can result in rapid hyperkalemia that may be
complicated by ventricular fibrillation.
Janssen L, Hansebout RR: Pathogenesis of spinal cord injury and
newer treatments: A review. Spine 1989;14:23–31.
McBride D: Spinal cord injury syndromes. In Greenberg J (ed),
Handbook of Central Nervous System Trauma. New York: Marcel
Dekker, 1993.
Ogilvy CS, Heros RC: Spinal cord compression. In Ropper AH,
Kennedy SF (eds), Neurological and Neurosurgical Intensive
Care, 2d ed. San Diego: Aspen, 1988.
Sonntag VKH, Hadley MN: Management of upper cervical insta-
bility. In Wilkins RH, Rengachary SS (eds), Neurosurgery Update
II. New York: McGraw-Hill, 1991.
Sypert GW: Management of lower cervical instability. In Wilkins
RH, Rengachary SS (eds), Neurosurgery Update II. New York:
McGraw-Hill, 1991.
696
00
The term acute abdomen denotes an abdominal pathologic
condition that, if left undiscovered and untreated, would
have a deleterious effect on the patient’s health status.
Numerous factors make the diagnosis and treatment of
abdominal conditions more difficult in ICU patients.
Physiologic Considerations
The peritoneum is a complex mesothelium-lined organ that
invests the intraabdominal viscera (visceral peritoneum) and
the abdominal cavity (parietal peritoneum). The peritoneum
functions to maintain the integrity of the intraabdominal
organs and provides lubrication by peritoneal fluid (nor-
mally <50 mL). For free movement of the viscera, the nondi-
aphragmatic peritoneal surface behaves as a passive
semipermeable membrane that allows bidirectional
exchange of water and electrolytes. The diaphragmatic sur-
face is highly specialized, with numerous gaps in the peri-
toneal lining that serve as entrances to a plexus of lymphatic
channels that drain via substernal lymph nodes into the tho-
racic duct. This diaphragmatic absorptive pathway is
enhanced by respiratory excursion and normally accounts
for at least 30% of the total lymphatic drainage of the
abdomen, helping to maintain the balance between visceral
parietal transudation and parietal peritoneal fluid uptake.
The omentum participates in absorption of peritoneal
fluid and particulate material up to 10 μm in diameter. The
omentum is highly mobile and can act to seal off a perforated
viscus or contain a bacterial inoculum.
Pain from intraabdominal disease is transmitted via
somatic sensory and visceral autonomic pathways. Visceral
pain, primarily elicited by distention, is referred in a logical
fashion in the same order as embryologic development; the
nerves accompany the major splanchnic vessels. Foregut
sources (eg, esophagus, stomach, liver, pancreas, biliary tract,
duodenum, and spleen) elicit upper epigastric pain, midgut
lesions (eg, jejunum, ileum, appendix, and right colon) elicit
periumbilical pain, and hindgut lesions (eg left colon and rec-
tum) radiate to the hypogastrium. This visceral pain is typically
colicky in nature and somewhat vague in location—in con-
trast to somatic pain, which is usually constant and well local-
ized to the site of direct parietal peritoneal irritation.
Intraabdominal disease also can cause pain to be referred
to other areas through neural pathways or other anatomic
constraints. Examples of referred pain include shoulder pain
from splenic or hepatic hemorrhage, causing phrenic nerve
irritation, and hip or thigh pain from a psoas abscess.
Pathophysiology
Critical care patients are susceptible to common causes of
abdominal disease such as appendicitis, diverticulitis, and
calculous cholecystitis with approximately the same fre-
quency as the general population. More important, they are
prone to develop more complex and unusual abdominal
processes resulting from a variety of predisposing condi-
tions. For example, recent surgery, especially involving
enteric anastomoses, may lead to intraabdominal abscess or
small bowel obstruction.
Shock with associated low flow states leads to an
increased risk of mesenteric ischemia, acalculous cholecysti-
tis, and possibly gut translocation of bacteria. Present or pre-
vious antimicrobial therapy also may contribute to illness
with overgrowth of resistant organisms, including Clostridium
difficile (pseudomembranous) colitis. The fasting state of
many critically ill patients may contribute to the develop-
ment of acalculous cholecystitis or, along with opioid use,
lead to a colonic pseudo-obstruction (Ogilvie’s syndrome;
see below).
Iatrogenic complications are common in patients under-
going multiple procedures and receiving several medications.
Inadvertent visceral injury may occur during paracentesis or
thoracentesis. Missed intraabdominal disease in traumatized
patients should be strongly considered in any patient not
recovering as expected. The problem of stress gastritis and
stress ulcers has been diminished with aggressive pH moni-
toring and pharmacologic prophylaxis but still presents a
formidable challenge.
32
Acute Abdomen
Allen P. Kong, MD
Michael J. Stamos, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
