Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

CRITICAL CARE OF VASCULAR DISEASE & EMERGENCIES
637
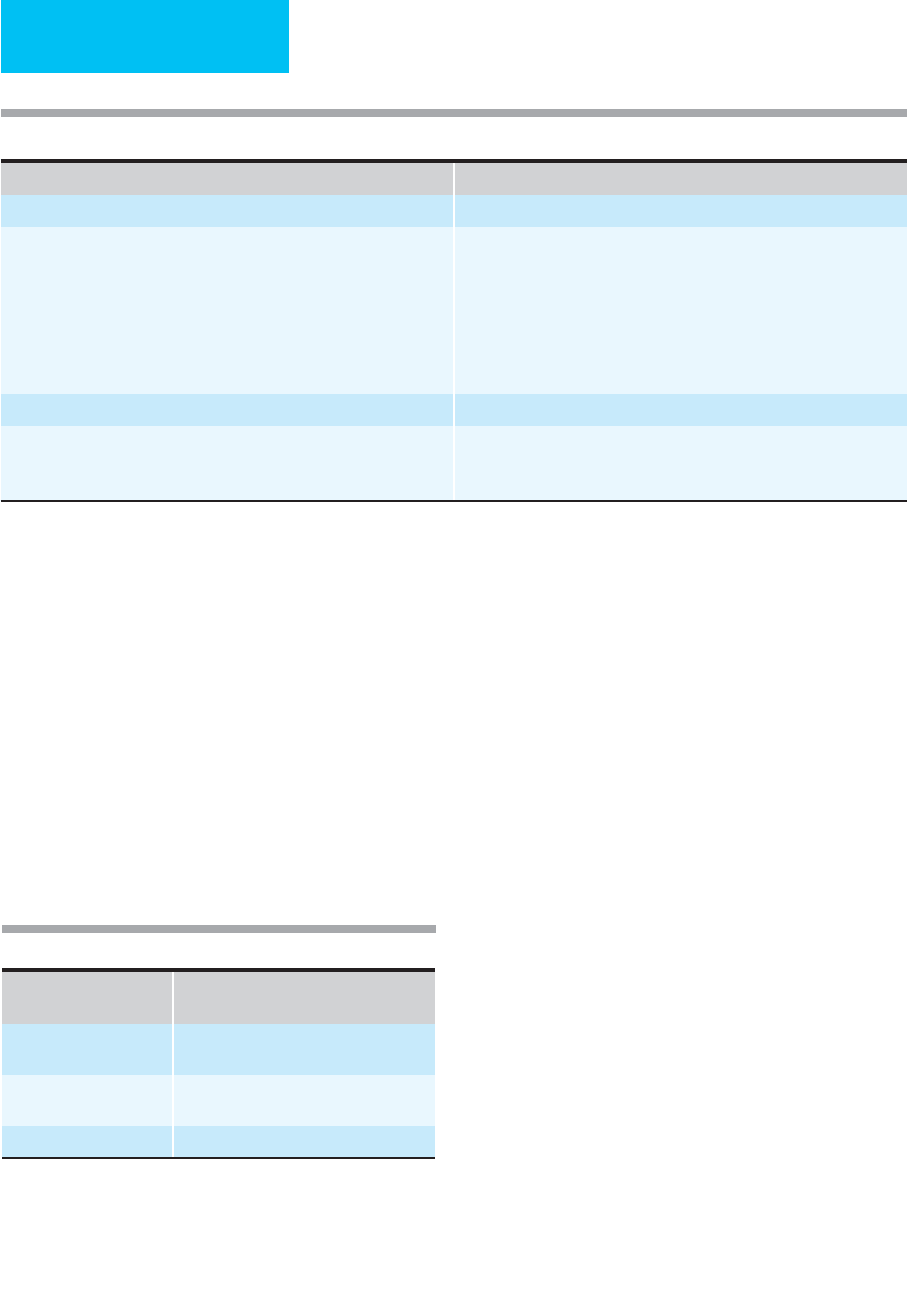
therapeutic window when combined with thrombolytic ther-
apy. Table 29–5 details the currently available thrombin
inhibitors. Lepirudin and argatroban are approved for the
treatment of thrombosis in patients with heparin-induced
thrombocytopenia. There are no currently agents available for
reversing the effects of the direct thrombin inhibitors.
E. Thrombolytic Agents—Thrombolytic agents such as
urokinase, streptokinase, and recombinant tissue plasmino-
gen activator (rt-PA; alteplase) have been evaluated in
numerous clinical trials for safety and efficacy and in com-
parison with operative management. Initially, an intense
thrombolytic state was induced with systemic therapy sus-
tained by constant intravenous infusion. In 10 uncontrolled
studies involving 1800 patients, best results were obtained
within 72 hours of onset of symptoms. Lysis was observed in
40%, with no difference in success rates between embolic or
thrombotic occlusions. Unfortunately, serious hemorrhagic
complications occurred in one-third of patients.
Regional or intraarterial thrombolysis has become an alter-
native to systemic therapy. The rate of successful reperfusion
(50–85%) appears to be higher than what is reported with sys-
temic infusion. Local infusion coupled with arteriography
conferred an additional advantage in delineating the cause of
the arterial occlusion (thrombosis versus embolus). Vessel wall
morphologic characteristics that may lead to early recurrent
thrombosis also were unmasked and further directed appro-
priate management (surgery versus angioplasty). Prolonged
arterial catheterization (hours to days) resulting in major
bleeding (6–20%) remains the main disadvantage of this
approach. Current thrombolytic agents include streptokinase,
urokinase, alteplase, reteplase, and tenecteplase.
Urokinase, a relatively inexpensive trypsin-like protease,
converts plasminogen directly to plasmin. Initially, the main
advantages of urokinase over streptokinase were its direct
action on plasminogen and its nonantigenicity. However,
pyretic reactions have been observed and attributed to inter-
leukins present during the manufacturing process. As a result,
urokinase is currently not available in the United States.
Alteplase is now the only thrombolytic agent available for
peripheral arterial thrombolysis. A naturally occurring acti-
vator of plasminogen, it is produced and released by the
endothelium. Manufactured through recombinant DNA
techniques, it is nonantigenic, has a half-life of 3.5–4 min-
utes, and has a high affinity for fibrin, which enhances lysis at
the thrombus level. Similar to urokinase, the primary route
of metabolism is hepatic.
Reteplase is a new plasminogen activator approved for
treatment of acute myocardial infarction and is used anecdo-
tally in the peripheral vasculature. Designed for use as bolus
therapy through recombinant DNA technology, experience
with reteplase in arterial and venous thromboembolic dis-
ease is limited.
An inert zymogen activated by the presence of fibrin clot,
prourokinase is converted to an active two-chain urokinase
that is highly fibrin-specific. Availability of this agent is also
limited.
Tenecteplase, a genetically engineered variant of alteplase,
has a prolonged half-life, increased fibrin specificity, and
higher resistance to inhibition by circulating plasminogen
activator inhibitor-1. A three-amino-acid substitution
resulted in a 14–19-minute half-life and more specific fibri-
nolysis in comparison with alteplase. Pending approval by
the Food and Drug Administration (FDA) for treatment of
acute myocardial infarction, the role of tenecteplase in the
management of peripheral arterial and venous thrombotic
occlusion has yet to be explored.
Because of the lack of evidence demonstrating the bene-
fits of improved limb salvage, lower mortality, or cost-
effectiveness, thrombolytic therapy cannot be regarded as
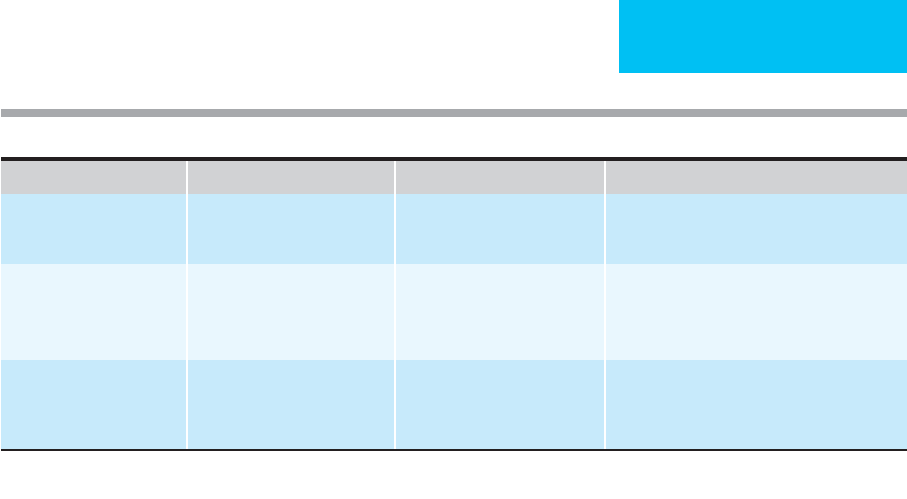
Drug
Dose
∗
Duration Notes
Lepirudin Load: 0.4 mg/kg IV then
0.15 mg/kg/hr
2–10 days Keep aPTT between 1.5 and 2.5 times normal.
Indicated for use in patients with HIT.
Bivalirudin Load: 1.0 mg/kg IV, followed
by 2.5 mg/kg/h for 4 h, then
0.2 mg/kg/h
20 h Has only been studied with concomitant aspirin
treatment.
Argatroban Initial dose 2 μg/kg/min IV Indicated as an anticoagulant in heparin-induced
thrombocytopenias. Monitor aPTT beginning 2 h
after start of infusion—steady state should be
1.5–3 times initial baseline.
∗
Check current prescribing information. Doses may need to be adjusted in the presence of comorbidites such as hepatic and/or renal failure.
Table 29–5. Currently available thrombin inhibitors.
CHAPTER 29
638
first-line treatment in the management of acute limb
ischemia. However, it remains a reasonable alternative in a
select group of patients, especially those with distal throm-
boembolic occlusions in surgically inaccessible small arteries
of the hands and feet and in patients who are at high risk for
surgery (Table 29–6).
F. Surgery—Operation is the best treatment of acute extrem-
ity ischemia, achieving both life and limb salvage. Adequate
preoperative support is essential. In the presence of active
cardiac risk, use of local anesthesia must be considered and
adequate intravenous hydration provided to minimize renal
insufficiency. At the time of surgery, placement of the inci-
sion is guided by the cause of occlusion, the presence of a
palpable pulse, and a history of previous revascularization.
In patients with embolic occlusion, exploration of the
femoral artery is considered in the presence of femoral and
distal pulses. A below-the-knee approach is preferred in
patients presenting with a palpable popliteal pulse and dis-
tal embolization. Patients with acute ischemia and a previ-
ous bypass graft usually are explored through the distal
anastomosis.
A transverse incision is often sufficient for passage of a
Fogarty catheter. Longitudinal arteriotomy is considered if
the cause is not known for certain or if bypass is necessary.
Removal of the entire embolic material is essential, and suc-
cess is confirmed through an intraoperative arteriogram to
ensure patency of the arterial runoff distal to the embolus.
Approximately 35–40% of completion angiograms will iden-
tify residual thrombus.
Although highly successful in embolic occlusion, blind
thromboembolectomy in patients with acute on chronic
thrombosis is highly dangerous and risks further intimal dis-
ruption to an already diseased vessel. Often these patients
require further surgical revascularization (eg, bypass or
endarterectomy) or endovascular management (eg, thrombol-
ysis, angioplasty, or stent placement in debilitated patients).
Intraoperative lytic therapy has been reported in several
series for the following indications: residual thrombus on
angiography, slow flow despite the absence of an angiographic
defect, prolonged ischemia with evidence of thickened blood
on retrograde bleeding, and persistent ischemia despite
restoration of sufficient proximal inflow. In a series of 78
patients, limb salvage was achieved in 73% of the 67%
treated successfully.
A new approach to intraoperative thrombolysis undergo-
ing recent investigation is high-dose isolated limb perfusion.
Surgical cutdowns of the femoral vessels are performed, with
intraarterial insertion of standard infusion pumps. A tourni-
quet is applied proximal to the exposed vessels, and venous
effluent is drained by gravity or through the use of extracor-
poreal pump support with concomitant dialysis.
Fasciotomy should be considered in all patients following
successful revascularization in the setting of prolonged
ischemia. Common clinical indications are pain out of pro-
portion to findings, pain on passive stretch, tense muscular
compartments with elevated pressures, and compartmental
hypesthesia and paralysis.
G. Supportive Care—Perioperative care of the patient fol-
lowing revascularization of an acutely ischemic limb can
vary from simple to extremely complex. Reperfusion of an
ischemic extremity can lead to the release of toxic cellular
products, the generation of oxygen-free radicals, hyper-
kalemia, increased intracellular calcium overload, myoglo-
binuria, and altered arachidonic acid metabolism. Critical
care therefore is directed toward ameliorating the damage
done by cellular breakdown.
Appropriate hemodynamic monitoring is essential.
Correction of electrolyte abnormalities and prompt treat-
ment of hyperkalemia through brisk diuresis and adminis-
tration of insulin and glucose can prevent fatal cardiac
arrhythmias. Adequate fluid volume and the administration
of mannitol—a free-radical scavenger and osmotic
diuretic—is the best strategy to correct acidosis and to pre-
vent acute renal failure caused by myoglobin precipitates.
Local mechanical factors are also important to prevent
skin and soft tissue breakdown. The extremity should be kept
warm but must not be heated in an effort to restore flow
because this will increase the metabolic rate, further the lac-
tic acidosis, and contribute to tissue destruction. Similarly,
cooling is inappropriate. Care must be taken to prevent
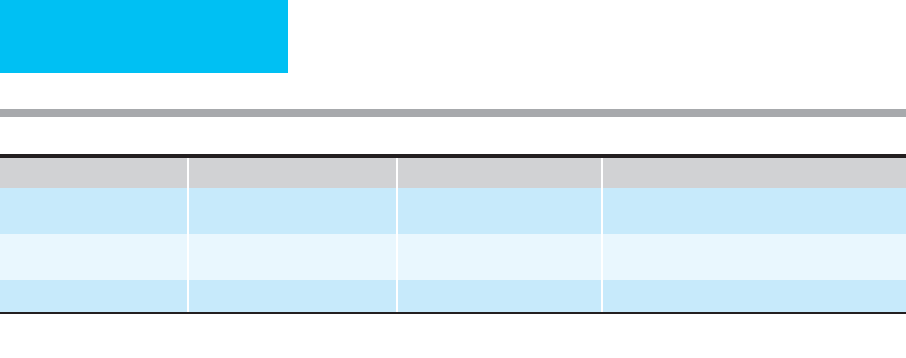
Drug Half-Life Intravenous Dose Intraarterial Dose
Altepase (t-PA) 3.5 min 50 mg over 2 h, followed by 0.05–0.1 unit/kg/h
Reteplase 14 min 10 units over 2 min, then 10 0.25–1 unit/h
Tenectplase 15 min 0.5 mg/kg Unknown
Data from Schmittling ZC, Hodgson KJ: Thrombolysis and mechanical thrombectomy for arterial disease. Surg Clin North Am 2004;84:1237–66.
Table 29–6. Thrombolytic agents.

CRITICAL CARE OF VASCULAR DISEASE & EMERGENCIES
639
pressure on an ischemic extremity. Heel pads and cushions
should be used as needed. Other vascular precautions
include keeping linens suspended with a bed cradle and posi-
tioning the patient in reverse Trendelenburg.
In patients who have not undergone fasciotomy, fre-
quent and careful assessment of the lower extremities is
warranted. In the event that a compartment syndrome is
diagnosed, prompt decompression is required to preserve
tissue viability.
Pain control typically requires high doses of an opioid
such as morphine. Analgesia must not be increased to the
point that symptoms are masked and a reliable neurologic
examination cannot be obtained. Short-acting intravenous
agents such as fentanyl have been used with success, pro-
vided that the dose is regulated so as not to obscure worsen-
ing of symptoms.
Prognosis
Despite recent advances in perioperative critical care, the
mortality rate after acute leg ischemia remains relatively
high. Both the mortality rate and the need for amputation
are directly related to the duration of ischemia. A recent
study found that no amputations were required when sur-
gery was undertaken within 2 hours compared with a 44%
amputation rate when operation was delayed up to 7 days.
The mortality rate was 10% in patients with symptoms pres-
ent for less than 2 hours and 32% in those whose symptoms
were present for up to 8 hours. Coexisting cardiopulmonary
complications were the underlying cause of most fatalities,
especially in patients with acute arterial thrombosis in con-
trast to peripheral embolism.
Current Controversies and Unresolved Issues
The cause of ischemic injury remains unclear. While it is
logical to assume that hypoxia is the culprit, investigations
have shown that most of the tissue damage actually occurs
during the time of reperfusion. Even short periods of
ischemia followed by reperfusion can cause cell damage. A
recent canine study found that 3 hours of partial ischemia
resulted in more tissue damage than the same period of
complete ischemia. Furthermore, the extent of postreperfu-
sion damage can be decreased by graded reflow. These inves-
tigations suggest that scavengers of free radicals may be
useful in the treatment of acute vascular insufficiency.
Although numerous investigations have been under-
taken, little improvement has been made over the last 2
decades in morbidity and mortality associated with surgical
thrombectomy in this fragile patient group. The advantage of
surgery stems from rapid restoration of blood flow. On the
contrary, pharmacologic thrombolysis is much less invasive.
The main disadvantage is the time lag involved for revascu-
larization. What is needed is an ideal therapeutic option that
achieves rapid blood flow and is minimally invasive. The
advent of endovascular surgery has spurred the development
of percutaneous mechanical thrombectomy devices to
answer this need. Current devices in various stages of clinical
trials include rheolytic, clot aspiration, and microfragmenta-
tion catheters.
Andersen JC: Advances in anticoagulation therapy: The role of
selective inhibitors of factor Xa and thrombin in thrombopro-
phylaxis after major orthopedic surgery. Semin Thromb
Hemost 2004;30:609–47. [PMID: 15630666]
Comerota AJ, Schmieder FA: Intraoperative lytic therapy: Agents
and methods of administration. Semin Vasc Surg 2001;14:
132–42. [PMID: 11400089]
Eslami MH, Ricotta JJ: Operation for acute peripheral arterial
occlusion: Is it still the gold standard? Semin Vasc Surg
2001;14:93–9. [PMID: 11400084]
Friedl HP et al: Ischemia-reperfusion in humans: Appearance of
xanthine oxidase activity. Am J Pathol 1990;136:491–5. [PMID:
2316621]
Greenberg RK, Ouriel K: Arterial thromboembolism. In
Rutherford R (ed), Vascular Surgery, 15th ed. Philadelphia:
Saunders, 2000.
Jackson MR, Clagett GP: Antithrombotic therapy in peripheral
arterial occlusive disease. Chest 2001;119:283–9S. [PMID:
11157655]
Kubaska SM, Greenberg RK: Techniques for percutaneous treat-
ment of acute arterial occlusion. Semin Vasc Surg 2001;14:
114–22. [PMID: 11400087]
Kasirajan K, Marek JM, Langsfeld M: Mechanical thrombectomy
as first-line treatment for arterial occlusion. Semin Vasc Surg
2001;14:123–31. [PMID: 11400088]
Lyden SP, Shortell CK, Illig KA: Reperfusion and compartment
syndromes: Strategies for prevention and treatment. Semin Vasc
Surg 2001;14:107–13. [PMID: 11400086]
Ouriel K, Vieth FJ: Acute lower limb ischemia: Determinants of
outcome. Surgery 1998;124:336–41. [PMID: 9706157]
Ouriel K, Veith FJ, Sasahara AA: A comparison of recombinant
urokinase with vascular surgery as initial treatment for acute
arterial occlusion of the legs. Thrombolysis or Peripheral
Arterial Surgery (TOPAS) investigators. N Engl J Med
1998;338:1105–11. [PMID: 9545358]
Patrono C et al: Platelet-active drugs: The relationship among
dose, effectiveness, and side effects. Chest 2001;119:
39–63S.
Schmittling ZC, Hodgson KJ: Thrombolysis and mechanical
thrombectomy for arterial disease. Surg Clin North Am
2004;84:1237–66. [PMID: 15364553]
Singh S et al: Thromboembolectomy and thrombolytic therapy in
acute lower limb ischemia: A five-year experience. Int Angiol
1996;15:6–8.
Working Party on Thrombolysis in the Management of Limb
Ischemia: Thrombolysis in the management of lower limb
peripheral arterial occlusion: A consensus document. Am J
Cardiol 1998;81:207–18. [PMID: 9591906]
Weaver FA et al: Surgical revascularization versus thrombolysis for
nonembolic lower extremity native artery occlusions: Results of
a prospective, randomized trial evaluating surgery versus
thrombolysis for ischemia of the lower extremity. The STILE
Investigators. J Vasc Surg 1996;24:513–21.
Weitz JI, Hirsh J: New anticoagulant drugs. Chest 2001;119:
95–107S. [PMID: 11157644]
CHAPTER 29
640
Deep Venous Thrombosis
ESSENTIALS OF DIAGNOSIS
Multiple risk factors.
Aching pain exaggerated by motion.
Calf and thigh swelling.
Tenderness to palpation and dorsiflexion.
Erythema, cyanosis, or venous distention.
General Considerations
Three factors (Virchow’s triad) contribute to the develop-
ment of venous thrombosis: stasis, increased coagulabil-
ity, and vessel wall damage. Contrary to former belief,
low flow alone is not sufficient to cause thrombosis.
Thrombophlebitis is venous thrombosis that follows inflam-
mation of the vessel wall. Because of underlying intimal
irregularities, the clot adheres firmly and is unlikely to
become dislodged. Phlebothrombosis occurs without vessel
wall injury and results in minimal clot adherence.
Patients at risk for the development of deep venous
thrombosis may be divided into three groups: (1) Low-risk
patients are under 40 years of age and are free of systemic
disease. Surgery lasts less than 60 minutes and is uncompli-
cated. Overall risk for the development of deep venous
thrombosis is less than 2%, and the chance of proximal pro-
gression is less than 1%. (2) Moderate-risk patients are over
age 40 and have undergone general anesthesia for more than
60 minutes. They also may have risk factors such as cancer,
obesity, varicose veins, bed rest, or cardiac failure. If prophy-
laxis is not given, the risk for development of deep venous
thrombosis is between 10% and 40% and that of proximal
propagation is between 2% and 8%. The risk of fatal pul-
monary embolism is almost 1%. (3) High-risk patients have
a history of deep venous thrombosis or of pulmonary
embolism. They undergo extensive abdominal or pelvic pro-
cedures for advanced disease or for some orthopedic indica-
tion. The risk of calf vein thrombosis is between 40% and
80% without prophylaxis. Proximal extension occurs in
10–20%, leading to fatal pulmonary embolism in up to 5%.
Risk factors for the development of venous thrombi and rec-
ommended prophylaxis are listed in Table 29–7. Most deep
venous thrombi are initiated by platelet adhesion either to
endothelial tissue or to exposed collagen of damaged vascular
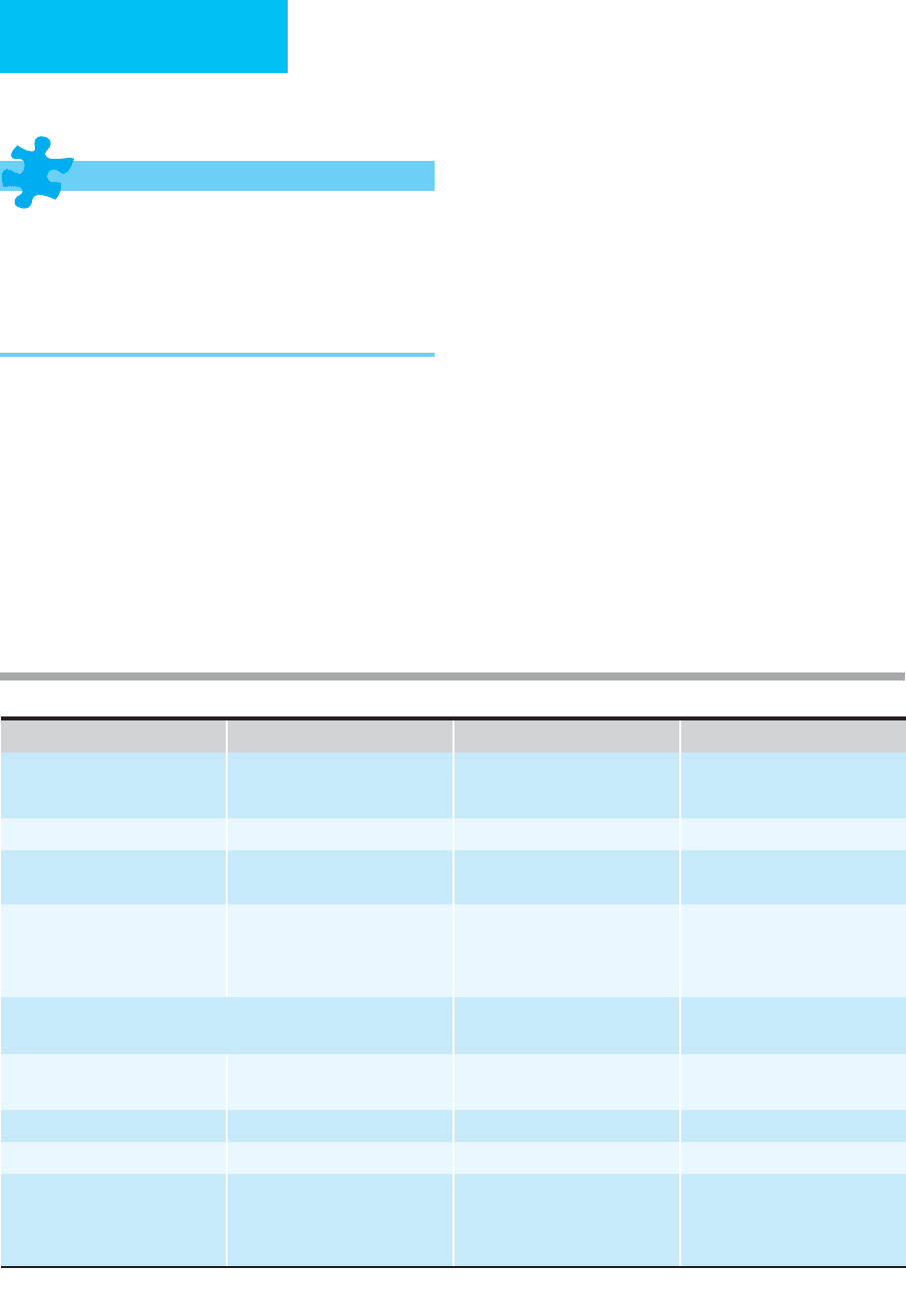
Low Risk Moderate Risk High Risk
Event or condition
General surgery
Age <40 years or time <60 minutes Age >40 years or time >60 minutes Age >40 years or time >60 minutes
plus risk factor
Orthopedic surgery — — Elective hip or knee surgery
Trauma — — Extensive soft tissue injury; major
fractures; multiple trauma
Medical conditions Pregnancy Myocardial infarction postpartum,
especially with previous deep
venous thrombosis; estrogen use;
varicose veins
Stroke, paraplegia, spine fracture,
prolonged bed rest, burns, hyperco-
agulable state, obesity
Incidence of thromboembolism without prophylaxis (%)
Distal calf veins 2
10–40 40–80
Proximal veins (pelvis, thigh,
popliteal veins)
0.4 2–8 10–20
Symptomatic pulmonary embolism 0.2 1–8 5–10
Fatal pulmonary embolism 0.002 0.1–0.4 1–5
Recommended prophylaxis Graduated compression stockings;
early ambulation
Heparin (5000 units SC twice daily),
LMWH, external or pneumatic
compression
Heparin (5000 units SC three times
daily), LMWH, external pneumatic
compression, inferior vena caval
filter, warfarin
Adapted from Colman RW et al (eds): Hemostasis and Thrombosis: Basic Principles and Clinical Practice. Philadelphia: Lippincott, 1994.
Table 29–7. Risk stratification for venous thrombosis and recommended prophylaxis.
CRITICAL CARE OF VASCULAR DISEASE & EMERGENCIES
641
walls. As platelet aggregation continues, the clot becomes
organized and begins to trap circulating white and red blood
cells. Deposition of fibrin organizes the clot and allows it to
build a stable matrix.
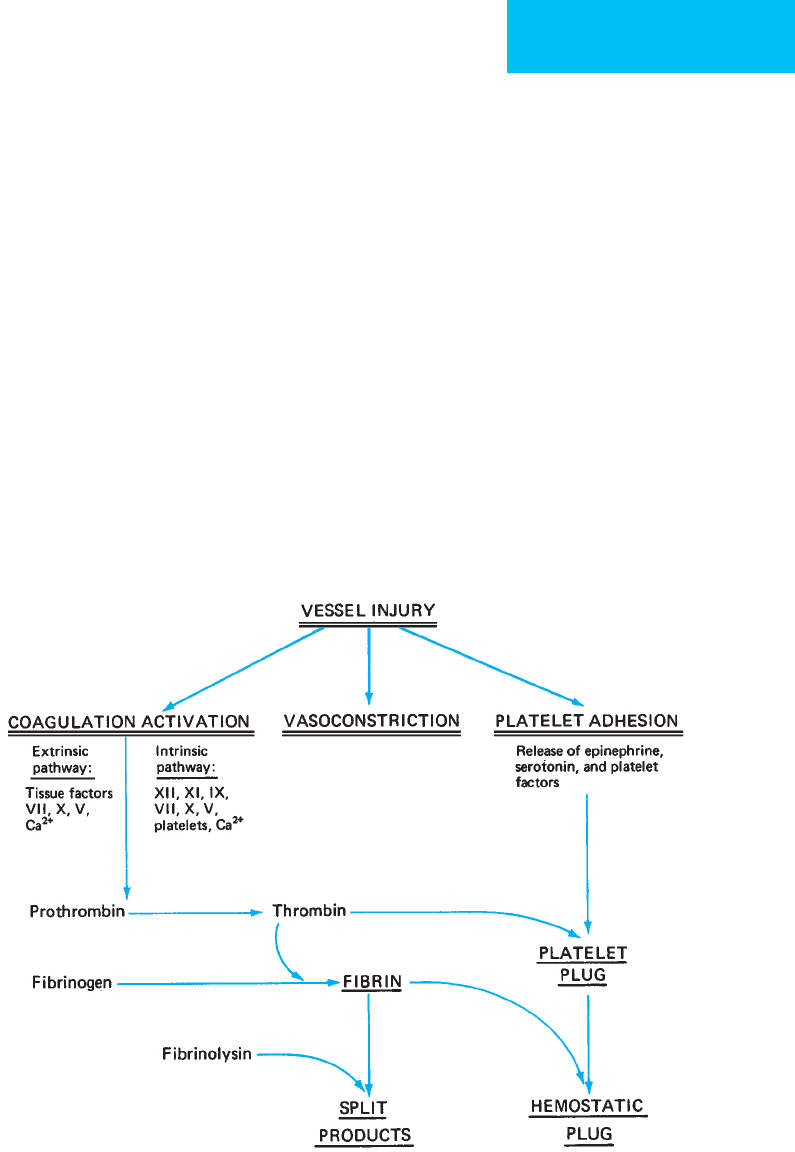
Activation of either the intrinsic or the extrinsic clotting
system contributes to thrombus formation. Adhesion of fac-
tor XII to exposed endothelium results in progressive activa-
tion of factor X. Activated factor X (Xa), along with factor V,
converts prothrombin to thrombin and fibrinogen to fibrin,
producing an insoluble clot. Platelets accumulate within the
matrix and provide a surface for further fibrin deposition.
Thromboxane A
2
, produced and released by platelets, aids
the process by contributing to vasoconstriction and further
platelet aggregation. Prostacyclin, which is produced by vas-
cular intima, limits the process by causing vascular dilation
and by inhibiting platelet aggregation. Antithrombin III
inhibits the action of factors IX, X, XI, and XII. Proteins C
and S, produced by the liver, inhibit coagulation by destroy-
ing factors V and VII and provide negative feedback to con-
trol the generation of thrombin (Figure 29–1).
The velocity of blood flow is inversely proportional to the
propensity for intravascular clotting. However, the threshold
for thrombus formation is decreased in the face of vascular
endothelial injury. Such injury may be caused by catheters,
infection, or external influences. In normal veins, the
endothelium is well supplied with prostacyclin and plas-
minogen, which prevent thrombus formation even at low
flow rates. However, when intimal damage is present—or in
the face of a hypercoagulable state—thrombus accumulates
rapidly. Red clots predominate in the venous system and
consist of platelets, red blood cells, and fibrin. White
thrombi, which contain chiefly platelets, are usually found in
the arterial system.
Hypercoagulable states are common in postoperative
critical care patients. The plasma concentration of clotting
factors rises after surgery. Maximum procoagulant activity
corresponds temporally with the peak incidence of throm-
boembolism. Detection of hypercoagulability remains diffi-
cult except in certain pathologic conditions such as
decreased concentrations of antithrombin III, protein C, and
Figure 29–1. Factors involved in arrest of hemorrhage. Injury to the blood vessel wall initiates a series of reactions
that arrest hemorrhage. The exposed subendothelial collagen initiates formation of the platelet plug (primary hemo-
stasis). The coagulation system is activated, leading to production of fibrin, which interacts with the platelet aggregate
to form a hemostatic seal. These relationships are also involved in spontaneous thrombus formation, although the
inciting event is usually not identifiable. (Reproduced, with permission, from Way LW (ed), Current Surgical Diagnosis &
Treatment, 10th ed. Originally published by Appleton & Lange. Copyright © 1993 by The McGraw-Hill Companies, Inc.)

CHAPTER 29
642
protein S. Use of some medications, such as oral contracep-
tives, is known to increase the risk of thromboembolic dis-
ease. Ill-defined alterations in the clotting mechanism that
predispose to clotting accompany some severe systemic dis-
eases such as cancer and sepsis.
Most deep venous thrombi begin in the veins of the calf.
When limited to this location, they are usually asymptomatic
except for mild calf pain and minimal swelling. Extension
into the deep venous system of the thigh produces more
swelling, pain, and purpura. Proximal propagation involves
the veins of the pelvis (iliofemoral thrombosis). As outflow is
restricted, the lower extremity swells and causes obstruction
of lymphatic channels, producing a blanched “milk leg”
(phlegmasia alba dolens). If patency is not restored, cyanosis
and venous gangrene result. This condition, known as phleg-
masia cerulea dolens (“blue leg”), is more common in the left
lower extremity than in the right from compression of the left
iliac vein as it passes under the right iliac artery. Phlegmasia
cerulea dolens is usually associated with disseminated malig-
nancies or sepsis. It is accompanied by hypotension and
hypovolemia, which result from venous pooling in the leg.
Thrombosis of the deep veins of the thigh and pelvis dra-
matically increases the risk of pulmonary embolism.
Approximately 85% of clinically significant pulmonary
emboli arise from the thighs and pelvis. Eighty percent of
deep venous thrombi remain confined to the calf, whereas
20% extend proximally. In the latter group, 40–50% will
result in pulmonary embolism if not treated appropriately.
Unfortunately, only 30% of those with confirmed pul-
monary embolism have objective signs consistent with deep
venous thrombosis.
Venous thrombosis of the upper extremities is becoming
increasingly prevalent in the ICU as a result of chronic
indwelling central venous catheters. Patients being main-
tained on long-term parenteral nutrition, hemodialysis,
antibiotics, or chemotherapy or those with poor peripheral
access are some of those at risk. Other predisposing factors
include exertion, thoracic outlet syndrome, congenital mal-
formations, and trauma (Table 29–8). Approximately 3–6%
of all pulmonary emboli and 1–2% of fatal pulmonary
emboli have been reported to originate from clots in the deep
veins of the upper extremity.
Superficial venous thrombi typically present as a small
lump or cord. These are usually of no systemic significance
except in the saphenous vein of the thigh, where they can
propagate through the saphenofemoral junction and gain
access to the deep iliofemoral system. When such proximal
extension is noted, ligation of the saphenous vein just distal
to its origin is warranted.
Clinical Features
A. Symptoms and Signs—Patients may complain of a
vague aching sensation or tightness in the calf or thigh. This
is worsened by active motion of the calf or foot. When super-
ficial thrombosis is present, localized tenderness is usually
also present.
Physical examination is notoriously unreliable for deep
venous thrombosis and accurately detects only 50% of cases.
Areas with increased tenderness to palpation include the
sole, the region deep to Achilles’ tendon, the groove between
the tibia and fibula, the regions over the soleus and gastroc-
nemius muscles, in the popliteal fossa, over the adductor
muscles of the thigh, and at the femoral vein near the
inguinal ligament. Tenderness induced by compression of
the calf muscles anteriorly against the interosseous mem-
brane or with passive dorsiflexion of the ankle (Homans’
sign) is present in less than 30% of patients. Inflation of a
sphygmomanometer cuff (40 mm Hg) placed above the knee
may provoke pain at the site of the thrombosis. A difference
of 1.5 cm in diameter between the swollen and the contralat-
eral leg supports the diagnosis.
Deep venous thrombosis of the axillary and subclavian
veins of the upper extremity results in swelling of the entire
arm. Pitting edema is usually absent. Percussion over the
clavicle and the course of the axillary vein often elicits
tenderness.
B. Noninvasive Diagnostic Techniques—Hand-held
continuous-wave Doppler devices test for continuity
between the deep system of the leg and the intrathoracic vena
cava. The probe is placed initially at the popliteal fossa and
subsequently over the femoral vein. The patient is instructed
to inspire, at which time an augmentation of flow should be
heard. The increased flow is due to transmission of the neg-
ative intrathoracic pressure to the deep system. This is a use-
ful screening test that can be performed at the bedside, but it
has a sensitivity of only about 75% when compared with
venography. Duplex scans and color-coded Doppler exami-
nations have accuracy rates between 90% and 100% for
detecting large thrombi of the femoral veins in symptomatic
patients. The sensitivity decreases to 59%, although the sen-
sitivity remains at 98%, in asymptomatic patients. Accuracy
also diminishes when examining the distal veins of the calf
owing to poor visualization. Isolated instances of iliac vein
thrombosis are also not detectable by ultrasound imaging
but may be diagnosed by simple Doppler examination.
Source Incidence (%)
Catheter-associated
Spontaneous (effort-induced)
Miscellaneous
Intravenous drug use
Thoracic tumors
Trauma
Radiation
30–40
20–30
30–40
Table 29–8. Etiology of upper extremity venous
thrombosis.

CRITICAL CARE OF VASCULAR DISEASE & EMERGENCIES
643
Multiple studies have shown that repeat duplex scanning has
an improved negative predictive value in patients suspected
of deep vein thrombosis but who have negative initial scans.
Pressure on the underlying vein by the ultrasound probe
helps to establish the age of the clot because fresh thrombi
are poorly organized and easily compressible. This is the
diagnostic test of choice for most patients, although it
requires an experienced technician to perform and interpret.
Impedance plethysmography relies on changes in electri-
cal resistance associated with alteration in limb volume. Deep
venous thrombosis impedes venous outflow and causes a
slower change in impedance when a proximally occluding
cuff is deflated. This technique is very accurate in ambulatory
patients but should be interpreted cautiously in those with
congestive heart failure or hypervolemia. It is more sensitive
for iliac and femoral vein thrombosis than for calf thrombi
and generally cannot be used in patients with fractures or
bandages that prevent proper electrode positioning. A posi-
tive test correctly indicates the presence of thrombosis in 90%
of patients. Recently, however, the sensitivity for plethysmog-
raphy in symptomatic patients was found to be much less
than earlier studies reported. In asymptomatic patients, the
specificity also falls. Impedance plethysmography can over-
look sizable thrombi that are not totally occlusive and can
interpret any pelvic venous outflow obstruction (eg, enlarged
nodes or pregnancy) as a venous thrombus. It also may be
falsely negative in patients with well-developed collaterals.
CT scanning and MR venography have successfully
diagnosed thrombi in the proximal veins and have proved
to be superior to conventional phlebography in visualizing
the great veins, identifying intraluminal thrombi, distin-
guishing new thrombi, and delineating adjacent abnormal-
ities. Ongoing prospective trials are confirming these initial
findings.
C. Invasive Diagnostic Studies—Contrast venography is
the “gold standard” with which all noninvasive modalities are
compared. It is the most reliable technique for detecting
thrombi in any location. Positive findings on venography
include constant filling defects, abrupt termination of the
dye column, nonfilling of the entire deep venous system or
portions thereof, and diversion of flow through collaterals.
The venogram catheter may be exchanged for one capable of
delivering thrombolytic agents if that therapeutic route is
chosen. Overall accuracy is better than 90%. A negative study
virtually eliminates the possibility of venous thrombosis.
Complications include foot pain at the site of injection and a
2–3% incidence of thrombosis owing to contrast
material–induced endothelial cell injury. Not routinely used
for primary diagnosis, phlebography has been advocated in
the diagnosis of symptomatic recurrent venous thrombosis
and after hip operations in suspected patients in whom non-
invasive means lack sensitivity.
D. Laboratory Findings—Several blood tests are available
that detect activation of the clotting cascade, including meas-
urement of fibrinopeptide A, fibrin monomers, and fibrin
degradation products. Plasma D-dimer, a degradation prod-
uct of plasmin digestion of mature cross-linked fibrin, is ele-
vated in patients with venous thrombosis. The sensitivity
measured by enzyme-linked immunosorbent assay
approaches 97%. Although highly accurate, confirmation of
venous thrombosis with an elevated D-dimer concentration
is necessary with objective imaging tests.
Differential Diagnosis
See Table 29–9.
Prevention
All critically ill patients should be considered for throm-
boembolic prophylaxis. Particular attention should be paid
to those with preexisting risk factors (see Table 29–7).
A. Physical Measures—Early ambulation or exercise of the
lower extremity muscles is probably the best and most cost-
effective prophylactic measure for preventing subsequent
venous thrombosis. Lower extremity elevation and active
flexion-extension exercises of the ankle will prevent stasis.
Prolonged standing in one position should be discouraged
because it promotes venous pooling. Use of thigh-high
antiembolism stockings is encouraged when they are fitted
properly. Casual application of stockings that extend only to
the knee are unlikely to be of value.
Of the compression techniques available, intermittent
compression garments are best. Garments with single com-
partments for the calves or multiple sequential compart-
ments are available. Maximum benefit is realized when they
are applied prior to surgery. Direct sequential compression
promotes blood flow and also stimulates systemic fibri-
nolytic activity. Therefore, benefit still accrues even with only
unilateral application can be achieved because of bandages
or casts. Studies have shown a reduction in the incidence of
thrombosis from 23–7% in patients so treated.
B. Anticoagulation—When used properly, preoperative
anticoagulation decreases the incidence of postoperative deep
venous thrombosis and secondary pulmonary embolism.
Lymphatic obstruction
Cellulitis
Baker’s cyst
Traumatic contusion
Tendon rupture
Congestive heart failure
Nephrosis
Arterial occlusion
Table 29–9. Differential diagnosis of deep venous
thrombosis.

CHAPTER 29
644
1. Warfarin—Coumarin derivatives act by suppressing the
formation of vitamin K–dependent clotting factors (II,VII, IX,
and X). When these agents are initiated before and continued
after operation, they are safe and effective. Coumarins require
several days to reach full effect because of the time interval
required for clearance of normal coagulation factors. These
agents are usually started after the patient has already been sys-
temically anticoagulated with unfractionated heparin.
Initiation of therapy with warfarin alone can have deleterious
effects. Protein C and protein S—natural anticoagulants—are
similarly reduced (especially protein C) with factor VII,
thereby shifting the hemostatic balance toward coagulation. In
patients with underlying protein C and protein S deficiency,
warfarin-induced skin necrosis can occur from thrombotic
occlusion of small vessels in the subcutaneous tissue. This
effect is manifested within 3–8 days of administration of the
initial dose. Patients with protein C and protein S deficiency
should not receive a loading dose of warfarin, and heparin
should be continued until the international normalization
ratio (INR) is therapeutic for 2 consecutive days.
Several drug interactions are known to occur with war-
farin. Of particular importance are those that increase
hepatic degradation (eg, barbiturates) and those that dis-
place warfarin from albumin (eg, aspirin and nonsteroidal
anti-inflammatory agents). Coumarins are also teratogenic
and should not be given to pregnant patients.
2. Heparin—Unfractionated heparin binds with antithrom-
bin III to prevent the conversion of prothrombin to throm-
bin. A “low dose”unfractionated heparin (LDUH) regimen is
used customarily prior to surgery and in the postoperative
period while the patient is still at risk. The postulated mech-
anism of action is enhancement of antithrombin III. The
usual regimen consists of 5000 units given subcutaneously
2 hours before surgery and every 8–12 hours during the
postoperative period. No changes in the usual coagulation
parameters can be detected at this dosing level. Increased
bleeding at the time of surgery generally does not occur.
Heparin prophylaxis is unlikely to be effective when started
in the postoperative period. It is not effective for patients
undergoing hip surgery and should not be used in those with
bleeding disorders or for scheduled intracerebral procedures.
An adjusted-dose heparin regimen has been described for
patients undergoing total hip replacement. Two days prior to
surgery, the patient receives 3500 units of heparin subcuta-
neously every 8 hours, with the dose adjusted to elevate the
aPTT to the high-normal range. This regimen has been
shown to reduce the incidence of deep venous thrombosis in
hip replacement patients from 39–13%.
3. Low-molecular-weight heparin (LMWH)—LMWHs
are produced by depolymerization of unfractionated
heparin. They have a more uniform molecular weight, longer
half-life, and more predictable pharmacokinetics. Significantly,
when compared with unfractionated heparin, they have a
higher ration of anti–factor Xa activity to anti–factor IIa
activity and are less likely to lead to heparin-induced
thrombocytopenia. LMWH has several clinical advantages
over unfractionated heparin. First evaluated in the 1980s in
high-risk surgical patients, one daily dose administered sub-
cutaneously is as effective as two or three doses of unfrac-
tionated heparin for deep vein thrombosis prophylaxis. It has
become the anticoagulant of choice for preventing deep vein
thrombosis in most orthopedic procedures. Its long half-life
precludes the need for laboratory monitoring, and it is more
effective than unfractionated heparin in preventing recur-
rence of venous thrombosis. Inpatient and outpatient uses of
LMWH have equivalent safety and efficacy. LMWH and
LDUH appear to be equally effective in reducing the inci-
dence of deep vein thrombosis in general surgical patients.
Studies have reported contradictory results with regard to
the incidence of wound hematomas and bleeding complica-
tions when comparing LMWH and LDUH likely because of
the doses used. Higher doses of LMWH are associated with
more bleeding, whereas lower doses are equivalent to LDUH
in preventing venous thromboembolism in moderate-risk
patients and have a lower rate of bleeding complications.
Currently, two LMWH preparations are approved in the
United States for the prevention of deep venous thrombosis
(Table 29–11). Enoxaparin is approved for use in patients
undergoing abdominal surgery as well as hip and knee sur-
gery. It is also approved for use in medical patients who are
at risk owing to severely restricted mobility during acute ill-
ness. The usual dose of enoxaparin in abdominal surgical
patients is 40 mg by subcutaneous injection given once daily.
The first dose should be administered 2 hours prior to sur-
gery, and the drug should be continued for 7–12 days after
surgery. The same dosing regimen applies to medical patients
with the exception that the drug should be started at the time
of immobilization. Dalteparin is approved for use in patients
undergoing hip replacement surgery and those undergoing
abdominal surgery who are at risk for thromboembolic com-
plications. The dose for abdominal surgical patients is 2500
IU given by subcutaneous injection starting 1–2 hours prior
to surgery, and then the drug is given once daily for 5–10
days. Neither of the LMWH preparations requires routine
monitoring of coagulation parameters during its use. Careful
monitoring for bleeding complications is mandatory. The
dose of LMWH may need to be reduced in older patients and
in those with renal and/or hepatic impairment.
4. Low-molecular-weight dextran—Dextran 40 acts by
coating platelet surfaces to reduce adhesion. It also increases
plasma volume and decreases the viscosity of blood. An
important mechanism of action may be the prevention of
platelet adhesion to venous valve cusps. The usual dose of
dextran 40 is 100–200 mL as an intravenous bolus (intra-
operatively), followed by 30–40 mL/h for 2–3 days after
surgery. Because dextran 40 is a volume expander, patients
with congestive heart failure or respiratory distress should
be monitored carefully for hypervolemia. Dextran potenti-
ates the effects of heparin, reducing the dosing requirements
of the latter by up to 50%.

CRITICAL CARE OF VASCULAR DISEASE & EMERGENCIES
645
5. Factor Xa Inhibitors—Fondaparinux is a synthetic
molecule that is an indirect inhibitor of factor Xa. It acts by
potentiating the anti–factor Xa activity of antithrombin.
Fondaparinux has no platelet effect, nor does it modulate
primary hemostasis. It is currently approved in the United
States for deep vein thrombosis prophylaxis in patients
undergoing hip fracture or replacement surgery and knee
replacement surgery. Fondaparinux has no effect on routine
coagulation studies, and monitoring is not necessary. The
usual dose is 2.5 mg given subcutaneously starting 6–8 hours
after surgery. Administration either prior to surgery or soon
after surgery is associated with an increased risk of major
bleeding.
Management of Deep Vein Thrombosis
The objectives of treatment are to limit further accumulation
of thrombus, prevent embolization, and minimize injury to
venous valves.
A. Supportive Therapy—Treatment of calf vein thrombi
remains largely controversial, with most centers recommend-
ing supportive care. In several large trials, anticoagulation was
withheld safely in patients with suspected deep vein thrombo-
sis and normal results on serial examinations with compres-
sion ultrasonography. Only supportive therapy is required,
consisting of bed rest, leg elevation, and mild analgesics.
Although some advocate the use of warm soaks, this measure
can macerate the overlying skin and promote infection. Early
ambulation should be encouraged, with elastic stockings as
required. Anticoagulation is indicated in patients with symp-
tomatic deep vein thrombosis identified by duplex scanning
and those with recurrent venous thrombosis.
B. Anticoagulation—Thrombi of the proximal veins (ie,
popliteal vein, femoral vein, and iliac veins) or of the axillary
and subclavian veins requires anticoagulation. Heparin,
either unfractionated or low-molecular weight, is the agent of
choice because it limits further propagation of the thrombus.
A recent consensus conference found that there is no differ-
ence between them regarding their efficacy or safety.
However, because of the advantages of convenient dosing,
facilitation of outpatient therapy, and a potentially lower risk
for recurrent deep vein thrombosis, some prefer the use of
LMWH over unfractionated heparin (UFH). Additionally,
there may be a survival advantage favoring the use of LMWH
in venous thromboembolic disease associated with malig-
nancy. For most patients, an initial bolus dose of 100 units/kg
(UFH) followed by a continuous infusion of 10 units/kg per
hour is adequate. Larger doses (200 units/kg as bolus injec-
tion) may be given if the clot extends into the iliac or femoral
system, if there is profound edema of the leg, or if imaging
studies indicate the presence of a long tail extending proxi-
mally. Anticoagulation should be assessed by monitoring
either the aPTT or the activated clotting time (ACT). The
heparin infusion should be titrated to keep the aPTT
between 1.5 and 2.5 times normal. Failure to achieve a
therapeutic level of anticoagulation within 24 hours carries a
25% risk of recurrent deep venous thrombosis. Bleeding
complications are reduced if dosage is regulated by monitor-
ing of anticoagulation and if the heparin is given by continu-
ous infusion rather than by intermittent bolus administration.
Five days of intravenous heparin therapy followed by oral
warfarin is usually effective and generally is regarded as con-
ventional therapy.
Although warfarin therapy can be started concomitantly
with heparin, most prefer to wait several days before starting
oral anticoagulation. Titration of the dose to achieve an INR
of 2.0–3.0 is adequate. Oral anticoagulation is continued for
3–6 months following discharge from the hospital based on
risk factors (Table 29–10).
Platelet counts should be obtained initially and every
other day to detect the development of heparin-induced
antiplatelet antibodies. Immune heparin-induced thrombo-
cytopenia (HIT) is suspected when the platelet count falls
below 100,000/μL or less than 50% of the baseline value. This
IgG-mediated platelet deficiency is seen in 3% of patients
and occurs 5–15 days after heparin therapy is initiated.
Management of patients with persistent thrombosis and HIT
can be difficult. Two agents, argatroban and lepirudin, have
been approved for patients with HIT needing anticoagulant
therapy. Argatroban is begun with a continuous intravenous
infusion at 2 μg/kg per minute and titrated to keep the
aPTT 1.5–3 times the initial baseline. Lepirudin (recombi-
nant hirudin) achieves rapid anticoagulation with a loading
dose of 0.4 mg/kg followed by an infusion of 0.15 mg/kg per
hour. It is adjusted to maintain an aPTT 1.5–3 times normal.
Oral warfarin then is instituted for the appropriate duration.
Approximately 3% of patients receiving oral anticoagula-
tion will present with recurrent deep venous thrombosis.
These patients should be assessed for a deficiency in
antithrombin III and proteins C and S. Bleeding is the major
complication of anticoagulation and occurs in 5–10% of
patients. This often presents as oozing from wounds, melena,
or a heme-positive gastric aspirate. If bleeding continues
despite discontinuation of heparin, protamine sulfate, a
heparin inhibitor, may be required. Infusion of fresh-frozen
plasma and vitamin K can counteract the effects of warfarin.
When LMWH is employed, the dose used depends on the
preparation (Table 29-11). Meta-analysis has failed to find a
clear advantage of one LMWH over the others with regard to
both safety and efficacy. Once-daily administration appears
as safe and effective as twice-daily use. Although anticoagu-
lation monitoring generally is unnecessary, anti–factor Xa
levels may be followed for 4 hours after injection, with a
desirable therapeutic range of 0.6–1.0 units/mL for twice-
daily administration and 1.0–2.0 units/mL for once-daily
administration. Monitoring is recommended for patients
with renal impairment because of the risk of accumulation
of anti–factor Xa activity.
C. Thrombolytic Therapy—There are currently two throm-
bolytic agents available for use in venous thrombosis.
CHAPTER 29
646
Multiple investigations have determined that streptokinase
and recombinant tissue plasminogen activator (rt-PA;
alteplase) are superior to intravenous heparin in preserving
venous patency and valvular function. Approximately 50% of
patients treated with thrombolytic agents retain valve func-
tion compared with 7% of those treated with heparin alone.
If complete thrombolysis is achieved, the incidence of post-
phlebitic syndrome is reduced. However, owing to the vari-
able nature of this syndrome, further investigation is
warranted to confirm these early findings.
Thrombolytic agents followed by heparin result in more
rapid resolution of lower extremity and pulmonary emboli,
restoring hemodynamic homeostasis. The main disadvantage
is the additional 1–2% risk of intracranial hemorrhage.
Because the incidence and mortality of pulmonary embolism
are the same in the two treatment modalities, systemic throm-
bolysis is reserved for acute massive pulmonary embolus in an
unstable patient with no bleeding dyscrasias. Young patients
with massive ileofemoral venous thrombosis (eg, phlegmasia
cerulea dolens) also may benefit from thrombolysis.
Neither streptokinase nor alteplase directly dissolves the
clot but rather requires activation of the fibrinolytic system.
Absolute contraindications to the use of lytic therapy include
active bleeding, recent (<2 months) cerebrovascular acci-
dent, or intracranial disease. Major contraindications include
recent surgery and evidence of GI hemorrhage. Prior to insti-
tution of therapy, the fibrinogen level, thrombin time, PT
and aPTT, platelet count, and hematocrit should be deter-
mined. Heparin administration should be discontinued.
Dosing regimens vary widely, but common doses are as fol-
lows: (1) streptokinase, 250,000 units over 30 minutes, fol-
lowed by an infusion of 100,000 units/h up to 72 hours, or
(2) alteplase, 100 mg infused over 2 hours. Within 4 hours of
commencing therapy, thrombin time, fibrinogen level, and
fibrin degradation products should be assessed. A lytic state
is documented by an elevated thrombin time and the pres-
ence of fibrin degradation products. Hematocrit should be
assessed every 6 hours. Elevation of fibrin degradation
products is anticipated. Infusion for more than 24 hours sel-
dom produces additional results. Lytic therapy should be
Patient Characteristic Recommendation
Calf vein thrombosis Up to 3 months of anticoagulant therapy
Proximal venous thrombosis or pulmonary embolus without previous
episode
a. Transient clinical risk factor—major orthopedic surgery or trauma
b. Metastatic cancer
c. Hypercoagulable risk factors
∗
or
Idiopathic thromboembolism
Anticoagulant therapy for 4–6 weeks or until risk factor is resolved and
patient is mobile, whichever is later.
Long-term anticoagulation (indefinite)
Either 3–6 months of therapy
or
Lifelong anticoagulation
Recurrent venous thromboembolism 1 year or lifelong anticoagulation
Any venous thromboembolism during pregnancy Unfractionated intravenous heparin for 5 days, followed by adjusted-dose
subcutaneous heparin every 12 hours
†
or low-molecular-weight heparin
until delivery followed by oral warfarin for 4–6 weeks.
∗
Hypercoagulable risk factors include protein C and S, antithrombin III, plasminogen deficiencies; resistance to activated protein C; hyper-
homocystinemia, and antiphospholipid antibodies.
†
aPTT should be checked 6 hours after initial subcutaneous dosing.
Adapted from Ginsberg JS: Management of venous thromboembolism. N Engl J Med 1996;335:1816.
Table 29–10. Recommendations for long-term management of venous thromboembolism.
Drug Name
Subcutaneous Dose for Treatment of
Venous Thromboembolism
Enoxaparin
100 anti-Xa units/kg every 12 h*,
†
or 150
anti-Xa units/kg every 24 h
‡
Dalteparin
100 anti-Xa units/kg twice daily
‡
or 200
anti-Xa units/kg once daily
‡
Tinzaparin
175 anti-Xa U/kg once daily
†
∗
For enoxaparin, 100 anti-Xa units/kg corresponds to a dose of
100 mg/kg.
†
FDA approved for this indication.
‡
FDA approved for this indication.
Data from McRae SJ, Ginsberg JS: Initial treatment of venous throm-
boembolism. Circulation 2004;110;I3–I9.
Table 29–11. Low-molecular weight heparins.
