Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


DERMATOLOGIC PROBLEMS IN THE INTENSIVE CARE UNIT
617
multiple medications. In general, the interval between initial
dose of the drug and onset of the disease is 1–3 weeks, except
for phenytoin-induced cases, which may occur as late as 8
weeks following the start of therapy. If the patient has a his-
tory of SJS or TEN from previous exposure to a drug, the
time period may be reduced to 24–48 hours. Patients with
AIDS appear to have an increased risk for TEN.
Clinical Features
A. Symptoms and Signs—Fever, nausea, vomiting, diar-
rhea, malaise, headache, upper respiratory symptoms, chest
pain, myalgia and arthralgia, and conjunctivitis usually pre-
cede the skin and mucous membrane lesions by 1–14 days.
Cutaneous involvement appears acutely as tender, discrete,
symmetric erythematous or purpuric macules and urticarial
plaques with atypical target lesions with dusky centers on the
face and upper trunk. Coalescence and extension to the
entire body rapidly ensue. Subsequently, large flaccid bullae
develop within the areas of erythema, and the necrotic epi-
dermis sloughs in sheets. Pressure applied directly over an
intact blister produces lateral spread of the lesion. Gentle
rubbing of erythematous areas induces separation of the epi-
dermis (Nikolsky’s sign). In SJS, the extent of epidermal
detachment is less than 10% of the body surface area. In
TEN, coalescence and extension to the entire body ensue rap-
idly, with detachment of the epidermis exceeding 30% of the
body surface area. The palms and soles may be involved, but
the hairy part of the scalp characteristically is spared.
Mucous membrane involvement is extensive, with erosions
or ulcers of the conjunctiva, lips, oropharynx, trachea,
esophagus, and anogenital area.
The extent of epidermal separation is a major prognostic
factor. Sepsis is the most frequent cause of death and may be
heralded by a sudden drop in temperature. Pulmonary
embolism, pulmonary edema, and GI bleeding are other
important causes of death. Pneumonia superimposed on
sloughing of the tracheobronchial mucosa may require ven-
tilatory assistance. Fluid loss, thermoregulatory impairment,
and increased energy expenditure result from extensive skin
loss, as in burn victims. The mortality rate ranges from
25–75% and is higher in elderly patients. Disabling ocular
sequelae affect up to 50% of survivors. Cutaneous reepithe-
lialization requires 2–3 weeks, whereas the mucous mem-
brane lesions persist longer.
B. Laboratory Findings—Routine laboratory studies
reflect the extent and severity of the disease but are not
specific. There may be evidence of electrolyte depletion
and dehydration. Serum creatinine may be elevated owing
to prerenal azotemia or acute tubular necrosis. Serum
aminotransferase levels often are slightly increased. In vir-
tually all patients, anemia is present; lymphopenia, neu-
tropenia, and thrombocytopenia sometimes are seen and
may indicate a poor prognosis. Biopsy of involved skin
may be very helpful, revealing full-thickness epithelial
necrosis.
Differential Diagnosis
Clinically, TEN and staphylococcal scalded skin syndrome
are quite similar. The latter disorder is caused by an epider-
molytic toxin produced by Staphylococcus aureus. The toxin
produces superficial (subcorneal) skin separation. Nikolsky’s
sign is present, but skin tenderness and mucous membrane
lesions usually are absent. Staphylococcal scalded skin syn-
drome more frequently affects neonates and toddlers, is rare
in adults, and has a much better prognosis than TEN.
Historically, SJS and EM major were considered part of
the same disease group. EM major can be differentiated from
SJS by the presence typical target lesions localized in a sym-
metric acral distribution, low or no fever, and frequent asso-
ciation with HSV infection.
Other differential diagnostic considerations include pem-
phigus vulgaris and other blistering diseases, toxic shock syn-
drome, chemical or thermal burns, and Kawasaki’s disease.
TEN shares many features with—and is considered by some
to be a severe form of—SJS.
Treatment
The principles of therapy are similar to those for major
second-degree burn victims. Ideally, patients should be man-
aged in a burn unit.
A. General Measures—Discontinue the most likely offend-
ing medication, provide pain control as necessary, and attend
to fluids, electrolytes, and nutrition. Aggressive nutritional
support should be started early; nasogastric feeding is pre-
ferred to parenteral nutrition.
B. Infection Control—Prophylactic antibiotics may pro-
mote the emergence of resistant strains of bacteria or
Candida and should be avoided. Obtain blood, urine, and
skin cultures frequently, and start empirical broad-spectrum
antibiotics at the earliest sign of infection. Consider acyclovir
in HIV-infected patients because secondary HSV infection
may be clinically undetectable.
C. Skin and Mucous Membrane Care—Ophthalmologic
consultation is essential to prevent blindness and other ocu-
lar sequelae. Oral hygiene and antisepsis are important.
Intact bullae should be left in place because they provide a
natural dressing. Nonviable, necrotic, and loosely attached
areas of epidermis should be débrided. Apply biologic dress-
ings, such as porcine xenografts and cryopreserved cadaveric
allografts, or synthetic coverings, such as hydrogel dressing
or paraffin gauze, to denuded areas. Silver sulfadiazine must
be avoided in patients suspected of sulfonamide sensitivity.
Current Controversies and Unresolved Issues
Toxic epidermal necrolysis has been considered by some to
be at the most severe end of the spectrum of EM and SJS, but
the two disorders instead may be distinct reactional states
with clinicopathologic similarities. Supporting the latter
view is the observation that the three do not have the same
etiologic spectrum.
CHAPTER 28
618
Although corticosteroids have been used for decades,
recent studies suggest that systemic steroid therapy is more
detrimental than useful in TEN. Claims for a reduction of
morbidity and mortality in response to a large dose of sys-
temic steroids in the first 24–48 hours have not been substan-
tiated, and most authors now suggest that corticosteroids
should not be used. Plasmapheresis, cyclophosphamide,
intravenous immunoglobulin, cyclosporine, and infliximab
likewise have been claimed to be beneficial on the basis of case
reports and uncontrolled studies, but again, there is no proof.
Auquier-Dunant A et al: Correlations between clinical patterns
and causes of erythema multiforme majus, Stevens-Johnson
syndrome, and toxic epidermal necrolysis: Results of an
International Prospective Study. Arch Dermatol
2002;138:1019–24. [PMID: 12164739]
Heymann WR: Toxic epidermal necrolysis 2006. J Am Acad
Dermatol 2006;55:867–9. [PMID: 17052494]
Mittmann N et al: Intravenous immunoglobulin use in patients
with toxic epidermal necrolysis and Stevens-Johnson syndrome.
Am J Clin Dermatol 2006;7:359–68. [PMID: 17173470]
Pereira FA, Mudgil AV, Rosmarin DM: Toxic epidermal necrolysis.
J Am Acad Dermatol 2007;56:181–200. [PMID: 17224365]
Prins C et al: Treatment of toxic epidermal necrolysis with high-
dose intravenous immunoglobulins: Multicenter retrospective
analysis of 48 consecutive cases. Arch Dermatol 2003;139:
26–32. [PMID: 12533160]
Trent J et al: Use of SCORTEN to accurately predict mortality in
patients with toxic epidermal necrolysis in the United States.
Arch Dermatol 2004;140:890–2. [PMID: 15262712]
Phenytoin Hypersensitivity Syndrome
ESSENTIALS OF DIAGNOSIS
High spiking fever, malaise, and rash 2–3 weeks after
starting phenytoin therapy—or sooner if prior exposure
to drug.
Patchy erythematous rash evolving into extensive pru-
ritic maculopapular rash, occasionally with follicular
papules and pustules.
Exfoliative erythroderma, EM, SJS, or TEN may develop,
especially in those with prior adverse reactions to
phenytoin; edema of palms, soles, and face.
Tender localized or generalized lymphadenopathy; mild
to severe hepatic injury; sometimes conjunctivitis,
pharyngitis, diarrhea, myositis, reversible acute renal
failure, and eosinophilia.
General Considerations
A number of adverse skin reactions, ranging from morbilli-
form eruptions to vasculitis, exfoliative erythroderma, EM,
SJS, and TEN, occur in up to 3–15% of patients receiving
phenytoin. In a small percentage of these patients, a distinc-
tive syndrome occurs, characterized by an extensive rash,
fever, eosinophilia, and hepatic injury. The disorder is
believed to be immune-mediated. All age groups are affected.
The incidence is highest in blacks.
Clinical Features
A. Symptoms and Signs—Onset is usually 2–3 weeks after
initiation of therapy—or within days if prior exposure has
occurred—heralded by high spiking fevers, malaise, and a
rash. The cutaneous eruption is variable. It often begins as
patchy erythema that evolves into an extensive pruritic mac-
ulopapular rash. Some patients have follicular papules and
pustules. The rash may generalize into an exfoliative erythro-
derma. EM, SJS, and TEN may occur, especially in patients
with previous adverse reactions to the drug and in those who
continue to receive the drug after developing signs of hyper-
sensitivity. Erythema and edema of the palms and soles and
prominent facial edema are common. The eruption usually
resolves with desquamation.
Tender localized or generalized lymphadenopathy is a
consistent finding. Virtually all patients with this syndrome
have hepatic injury, which varies from mild and transient to
severe and fulminant, resulting in massive hepatic necrosis.
Hepatosplenomegaly is found in most patients. Other fea-
tures of the syndrome, not uniformly present, are conjunc-
tivitis, pharyngitis, diarrhea, myositis, and reversible acute
renal failure. In general, the signs and symptoms resolve rap-
idly once the medication is discontinued; however, multior-
gan abnormalities may progress even after the phenytoin has
been stopped. Some patients endure a prolonged and com-
plicated course of exacerbations and remissions. The mortal-
ity rate approaches 20% in patients with severe liver damage.
B. Laboratory Findings—Laboratory studies are important
for monitoring the severity and progression of the reaction.
Leukocytosis with eosinophilia (5–50%) is common.
Coombs-negative hemolytic anemia and atypical circulating
lymphocytes may be seen. The degree of elevation in serum
aminotransferases and alkaline phosphatase levels reflects
the severity of liver injury, and renal function may be abnor-
mal. It is of note that the erythrocyte sedimentation rate and
serum complement levels are normal in this disorder.
Differential Diagnosis
Other anticonvulsant medications, particularly phenobarbi-
tal, may cause reactions indistinguishable from phenytoin
hypersensitivity disorder. Infectious mononucleosis may
resemble this syndrome.
Treatment
The medication must be discontinued. Data regarding cross-
reactivity among the anticonvulsants is scanty, but if anti-
convulsant therapy is still necessary, valproic acid or
carbamazepine may be safer alternatives.
DERMATOLOGIC PROBLEMS IN THE INTENSIVE CARE UNIT
619
General supportive care is vital because of the multisys-
tem involvement. Systemic corticosteroids are sometimes
used, but their effectiveness has not been documented.
Arif H et al: Comparison and predictors of rash associated with 15
antiepileptic drugs. Neurology 2007;68:1701–9. [PMID:
17502552]
Gogtay NJ, Bavdekar SB, Kshirsagar NA: Anticonvulsant hypersen-
sitivity syndrome: A review. Expert Opin Drug Saf 2005;4:
571–81. [PMID: 15934861]
Kaminsky A et al. Anticonvulsant hypersensitivity syndrome. Int J
Dermatol 2005;44:594–8. [PMID: 15985033]
Seitz CS et al: Anticonvulsant hypersensitivity syndrome: Cross-
reactivity with tricyclic antidepressant agents. Ann Allergy
Asthma Immunol 2006;97:698–702. [PMID: 17165282]
PURPURA
Purpura results from hemorrhage into the skin or mucous
membranes. Incomplete blanching on pressure is characteris-
tic. Purpuric lesions may be a clue to acutely life-threatening
diseases but are seen in benign conditions as well. An impor-
tant step in evaluating the patient with purpura is to determine
whether the lesions are macular (flat) or palpable.
Nonpalpable purpura, the result of bleeding into the skin
without inflammation, is due to disorders of hemostasis and
vessel wall integrity. In these cases, small petechial hemor-
rhages (<3 mm) occur. Common causative factors are throm-
bocytopenia and disorders of platelet function. Petechiae also
may be a clue to diseases that affect the integrity of blood ves-
sels, for example, scurvy or amyloidosis. In contrast, disorders
of coagulation cause bleeding from larger vessels, producing
ecchymoses (ie, hemorrhagic macules >3 mm). Palpable pur-
pura, the expression of inflammatory damage to the vascula-
ture and consequent extravasation of blood, is the hallmark of
small vessel vasculitis but also may be seen with septic emboli.
Purpura develops occasionally as a secondary manifesta-
tion in an inflammatory dermatosis. For example, macular
drug eruptions or exanthematous infectious diseases such as
measles and scarlet fever can become purpuric as a result of
increased permeability of the blood vessels and extravasation
of red cells into the surrounding tissue. Causes of purpura
are classified arbitrarily in Table 28–4. In this section, leuko-
cytoclastic vasculitis, disseminated intravascular coagulation,
and purpura fulminans are discussed.
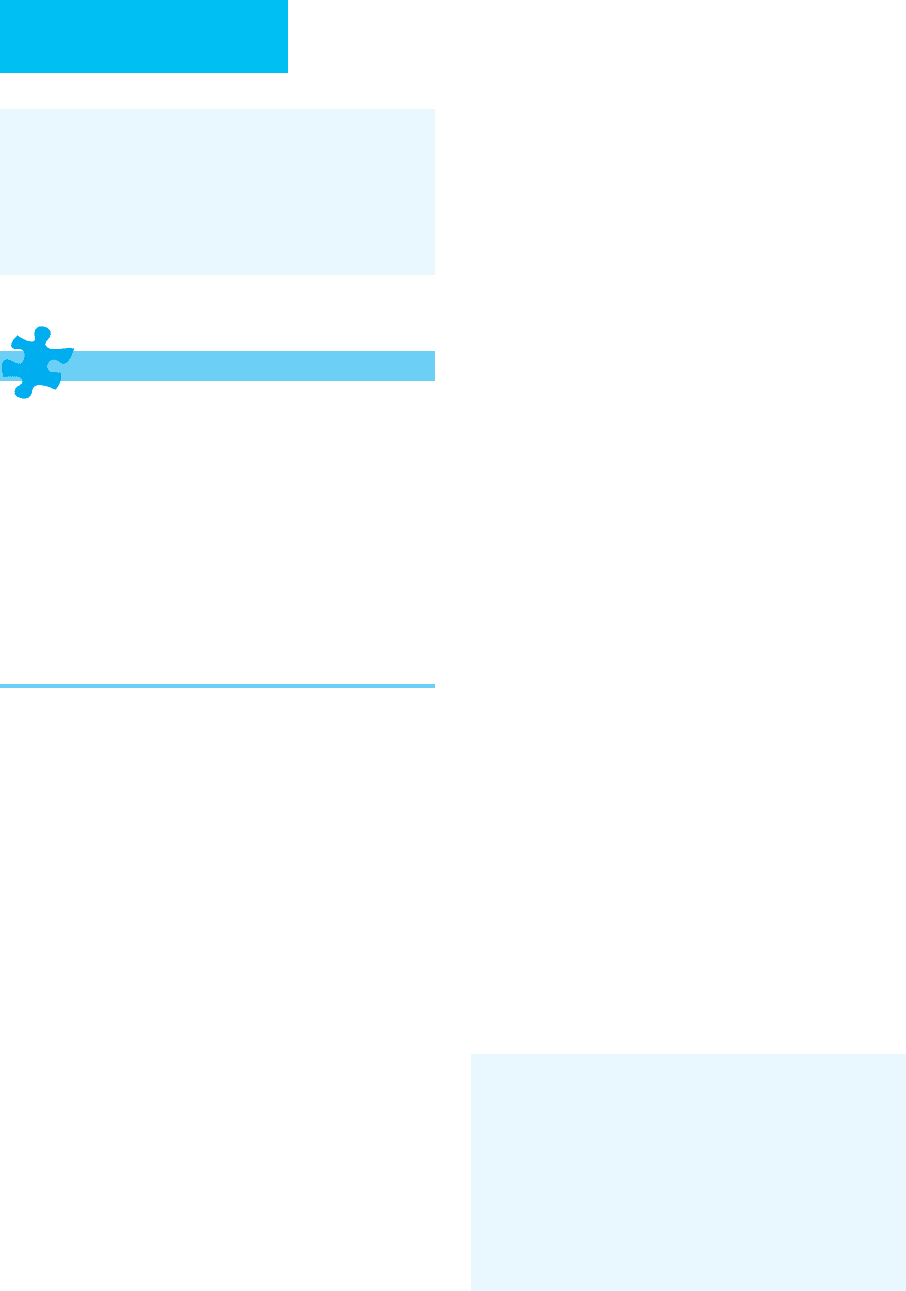
Table 28–4. Causes of purpura.
Vascular Disorders Abnormal distribution
Inflammatory disorders
Diseases associated with splenomegaly
Palpable purpura Kasabach-Merritt syndrome
Vasculitis
Purpura with normal platelet counts
Septic emboli Platelet function defects
Nonpalpable purpura Drugs (eg, salicylates, NSAIDs)
Viral infections Uremia
Rickettsial infections Coagulopathies
Drugs and chemicals
Purpura with high platelet counts
Pigmented purpuric dermatoses Myeloproliferative syndromes
Noninflammatory disorders
Postsplenectomy
Trauma Various neoplasms and inflammatory diseases
Amyloidosis Disorders of Coagulation
Scurvy
Acquired
Dysproteinemic states Vitamin K deficiency
Solar purpura Disseminated intravascular coagulation
Abnormalities of Platelet Number and Function Parenchymal liver disease
Thrombocytopenic purpuras
Cardiopulmonary bypass surgery
Increased platelet destruction Lupus anticoagulant syndrome
Microangiopathic diseases
Inherited
Infections Classic hemophilia
Immunologic disorders von Willebrand’s disease
Idiopathic thrombocytopenic purpura (ITP)
Thrombotic disorders
Drug-induced thrombocytopenia Protein C and S deficiency
Autoimmune diseases (eg, SLE) Antithrombin III deficiency
Decreased platelet production Drugs (eg, aminocaproic acid, estrogen compounds)
Neoplastic replacement of bone marrow Nephrotic syndrome
Myelosuppressive disorders Anticoagulant necrosis
Radiation
Chemotherapy
Infections
CHAPTER 28
620
Leukocytoclastic Vasculitis
ESSENTIALS OF DIAGNOSIS
Palpable purpura; hemorrhagic bullae, purpuric
plaques, vesicles, pustules on a purpuric base, and
urticaria-like papules may be present.
Systemic symptoms occur in 40–50%, including fever,
myalgias, and arthralgias; abdominal pain, GI bleeding,
and pulmonary disease (eg, pneumonitis, pleuritis, or
hemoptysis) occur less frequently.
Biopsy of involved skin shows necrotizing vasculitis
with prominent neutrophilic infiltrates in and around
the vessel walls, extravasated red blood cells, and dep-
osition of fibrin.
General Considerations
Vasculitis is defined as inflammation and subsequent necro-
sis of the vessel wall. Various clinical syndromes share vas-
culitis as a feature and may be classified according to the size
and type of involved vessels (eg, postcapillary venule, arteri-
ole, vein, or artery), the type of inflammatory infiltrate (eg,
necrotizing or granulomatous), and the organs affected
(Table 28–5). Some forms of vasculitis are confined to the
skin, whereas others involve internal organs and may cause
severe and potentially fatal disease. When the small vessels of
the skin are involved, the most common finding is palpable
purpura. Involvement of larger vessels produces subcuta-
neous nodules, stellate-shaped purpura, or necrosis.
Pathophysiology
Most of the vasculitic diseases are immunologically mediated
and probably are due to immune complex deposition. The evi-
dence for immune complex–mediated damage is most com-
pelling for small-vessel, or “leukocytoclastic,” vasculitis. The
pathologic process involves the following sequence of events:
deposition of circulating soluble antigen-antibody complexes
in postcapillary venule walls, activation of the complement
cascade, chemotaxis of neutrophils to the sites of immune
complex deposition, and release of lysosomal enzymes and
other products from neutrophils, resulting in necrosis of the
vessel wall. Hemorrhage, thrombosis, and surrounding tissue
necrosis follow. The inflammatory cell infiltrate and edema in
and around the vessels cause the lesions to become palpable. In
some situations, vasculitis may result from direct invasion of
vessels by infectious agents. Cell-mediated immune damage
may be involved in granulomatous vasculitis.
Clinical Features
A. Symptoms and Signs—As noted earlier, the classic cuta-
neous finding in leukocytoclastic vasculitis is palpable pur-
pura (although the palpability may be subtle). However,
hemorrhagic bullae, purpuric plaques, vesicles, pustules on a
purpuric base, and urticaria-like papules may be present.
Affected patients also may have ulcerative, infarcted, or retic-
ulated lesions. The lesions arise in crops, predominantly on
the lower extremities and in dependent areas. Edema of the
lower legs is common. About 40–50% of patients with leuko-
cytoclastic vasculitis have systemic symptoms. Fever, myal-
gias, and arthralgias may accompany the cutaneous
manifestations. Kidney involvement may be transient, with
hematuria or proteinuria, or may lead to glomerulonephritis
or renal failure. Abdominal pain, GI bleeding, and pul-
monary disease (eg, pneumonitis, pleuritis, or hemoptysis)
occur less often. Peripheral neuropathies occur infrequently
and portend a poor prognosis.
B. Laboratory Findings—The definitive diagnosis of cuta-
neous vasculitis depends on compatible cutaneous lesions
plus histopathologic confirmation of blood vessel damage.
Necrotizing vasculitis is characterized by a prominent neu-
trophilic infiltrate in and around the vessel wall associated
with nuclear fragments (“nuclear dust”), extravasated red
blood cells, and deposition of fibrin. Furthermore, granulo-
matous vasculitis shows fibrinoid necrosis of the blood vessels
associated with intravascular and extravascular granulomas.
Evaluation of lesions by direct immunofluorescence for
the presence of immunoglobulins and complement may help
to confirm the diagnosis. However, negative results are com-
mon, and this test is often of little clinical value.
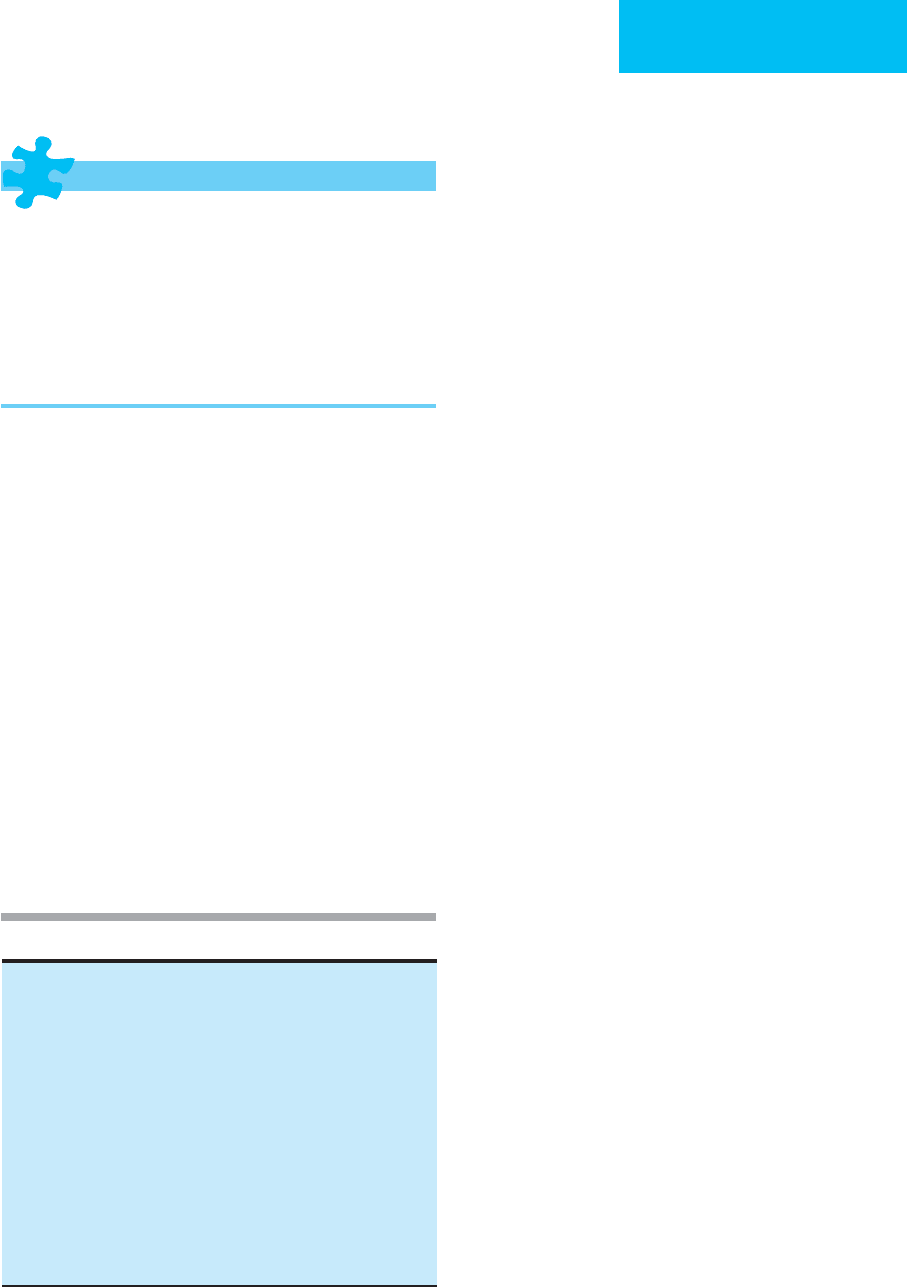
Leukocytoclastic (hypersensitivity) vasculitis
Systemic-cutaneous vasculitis
Variants of leukocytoclastic vasculitis
Urticarial (hypocomplementemic) vasculitis
Serum sickness
Henoch-Schönlein purpura
Rheumatic vasculitis
Systemic lupus erythematosus
Rheumatoid vasculitis
Sjögren’s syndrome
Scleroderma and dermatomyositis
Polyarteritis nodosa
Cutaneous type
Systemic type
Granulomatous vasculitis
Churg-Strauss syndrome (allergic granulomatosis)
Wegener’s granulomatosis
Giant cell arteritis
Temporal arteritis
Takayasu’s arteritis
Miscellaneous
Degos’ disease (malignant atrophic papulosis)
Kawasaki’s disease
Lucio phenomenon
Table 28–5. Classification of vasculitis.

DERMATOLOGIC PROBLEMS IN THE INTENSIVE CARE UNIT
621
Once the diagnosis of cutaneous vasculitis is established, a
comprehensive evaluation is necessary to determine the pres-
ence and extent of internal involvement and to identify poten-
tial underlying causes (Table 28–6). Some recommended
screening studies include the following: complete blood count
and erythrocyte sedimentation rate; chemistry profile; serum
protein electrophoresis and cryoglobulin titer; hepatitis B and
C screens; antinuclear antibody titer, anti-Ro and anti-La titers,
C3, C4, total hemolytic complement, and VDRL; urinalysis and
stool occult blood; throat culture and antistreptolysin O titer;
and chest x-ray. Depending on the clinical situation, other tests
may include antineutrophilic cytoplasmic antibody titers, anti-
cardiolipin antibodies, direct immunofluorescence, biopsy of
affected organs, radiographic studies (including angiograms)
of affected organs, malignancy screening tests, echocardiogra-
phy, visceral angiography, and nerve conduction studies.
Differential Diagnosis
Palpable purpura occurs in both vasculitis and septicemia.
Certain clinical patterns favor the diagnosis of sepsis and
sometimes can provide clues to the causative organism. The
skin lesions associated with staphylococcal sepsis are acrally
located, asymmetric, and fewer in number than those associ-
ated with vasculitis. The characteristic lesions of gonococcal
bacteremia are discrete, tender pustules on a hemorrhagic
base, often accompanied by polyarthralgias, tenosynovitis, or
septic arthritis. The well-known skin findings in infective
endocarditis are painful nodules on the volar surfaces of the
fingers and toes (Osler’s nodes), nontender hemorrhagic mac-
ules on the palms and soles (Janeway’s lesions), and subungual
splinter hemorrhages. Petechiae, ecchymoses, hemorrhagic
vesicles and pustules, and ulcerated nodules all may be seen
with sepsis. The diagnosis is confirmed by a positive blood cul-
ture or a positive culture or Gram stain from the skin lesions.
Palpable purpura also can occur in nonseptic embolic disor-
ders such as atheromatous emboli or left atrial myxoma.
Treatment
The therapy of vasculitis is based on the extent and severity of
the disease. Any associated disease, infection, chemical, or drug
should be treated or removed. For vasculitis limited to the skin,
conservative therapy is appropriate because most cases are acute
and self-limited. Bed rest, antihistamines, and nonsteroidal anti-
inflammatory drugs may suppress or control cutaneous lesions
effectively. For necrotic or highly symptomatic eruptions,
colchicine, dapsone, or prednisone may be useful.
For systemic vasculitis, therapy with immunosuppressive
and/or cytotoxic agents such as corticosteroids, azathioprine,
cyclosporine, methotrexate, and mycophenolate mofetil is
usually necessary. Plasmapheresis may be tried in patients
refractory to other therapeutic modalities. Monoclonal anti-
body therapy with infliximab may be of value.
Cutaneous ulcers or bullae are treated with debridement,
tap water soaks, topical antibiotics, and vapor-permeable
membranes.
Carlson JA, Cavaliere LF, Grant-Kels JM: Cutaneous vasculitis:
Diagnosis and management. Clin Dermatol 2006;24:414–29.
[PMID: 16966021]
Gedalia A: Henoch-Schonlein purpura. Curr Rheumatol Rep
2004;6:195–202. [PMID: 15134598]
Gonzalez-Gay MA, Garcia-Porrua C, Pujol RM: Clinical approach
to cutaneous vasculitis. Curr Opin Rheumatol 2005;17:56–61.
[PMID: 15604905]
Hayat S, Berney SM: Cutaneous vasculitis. Curr Rheumatol Rep
2005;7:276–80. [PMID: 16045830]
Langford CA: Vasculitis in the geriatric population. Rheum Dis
Clin North Am 2007;33:177–95. [PMID: 17367699]
Mang R, Ruzicka T, Stege H: Therapy for severe necrotizing vas-
culitis with infliximab. J Am Acad Dermatol 2004;51:331–2.
[PMID: 15280860]
Marder W, McCune WJ: Advances in immunosuppressive drug
therapy for use in autoimmune disease and systemic vasculitis.
Semin Respir Crit Care Med 2004;25:581–94. [PMID:
16088501]
Russell JP, Gibson LE: Primary cutaneous small vessel vasculitis:
Approach to diagnosis and treatment. Int J Dermatol
2006;45:3–13. [PMID: 16426368]
Suresh E: Diagnostic approach to patients with suspected vasculi-
tis. Postgrad Med J 2006;82:483–8. [PMID: 16891436]
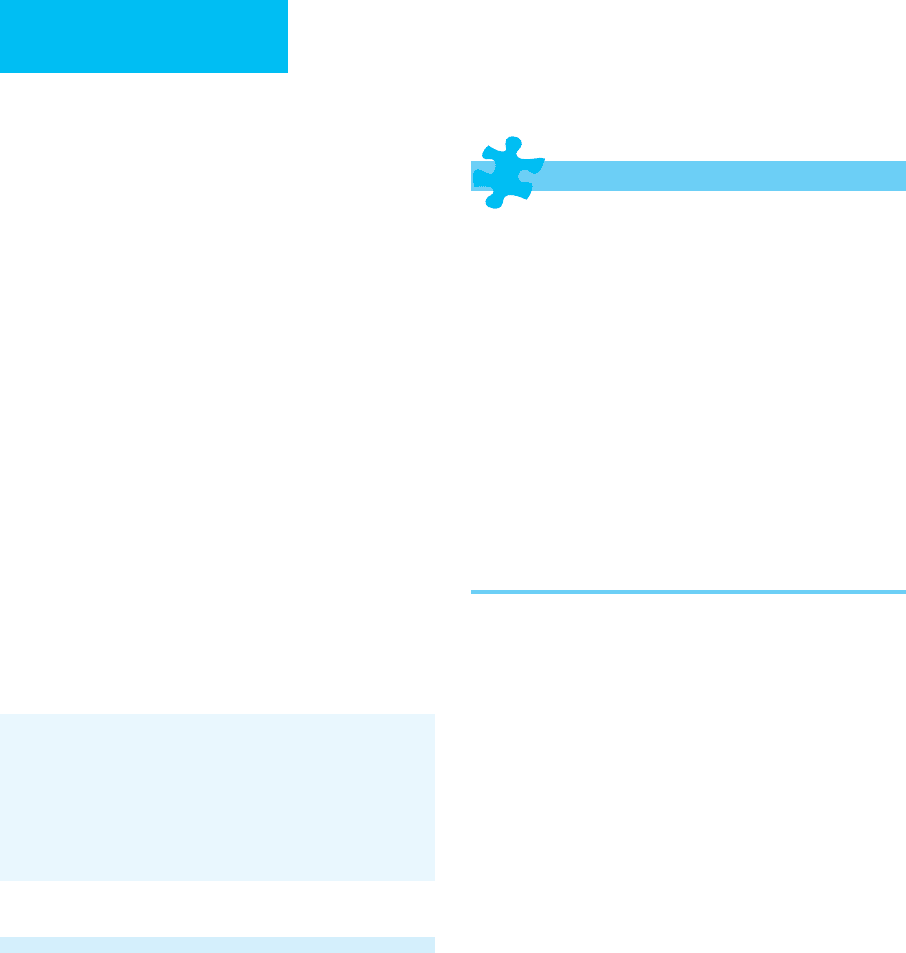
Drugs: See Table 28–2.
Chemical
Insecticides
Petroleum products
Weed killers
Foreign proteins
Heterologous serum
Snake antivenin
Hyposensitization antigens
Infections
Group A beta-hemolytic streptococci
Hepatitis B
Mycobacterial diseases
Influenza
Abnormal immunoglobulins
Multiple myeloma
Cryoglobulinemia
Macroglobulinemia
Rheumatic diseases
Rheumatoid arthritis
Systemic lupus erythematosus
Dermatomyositis
Sjögren’s syndrome
Miscellaneous diseases
Ulcerative colitis
Lymphomas and leukemias
Malignant tumors
Idiopathic
Table 28–6. Causes of vasculitis.
CHAPTER 28
622
Disseminated Intravascular Coagulation
& Purpura Fulminans
ESSENTIALS OF DIAGNOSIS
Extensive skin necrosis, fever, and hypotension associ-
ated with evidence of disseminated intravascular coag-
ulation.
Sudden appearance of large, irregular areas of purpura,
especially over the extremities.
Skin lesions are tender, enlarge rapidly, and may evolve
into hemorrhagic bullae with subsequent necrosis and
black eschar formation; necrosis of an entire extremity
may develop.
May be associated with pulmonary, hepatic, or renal
failure; GI bleeding; and hemorrhagic adrenal infarction.
General Considerations
Disseminated intravascular coagulation (DIC) is a dynamic
process associated with a variety of underlying diseases and
is the result of uncontrolled activation of coagulation and
fibrinolysis. Purpura fulminans is an acute, severe, often rap-
idly fatal syndrome characterized by extensive necrosis of the
skin associated with fever and hypotension. Purpura fulmi-
nans represents the extreme end of the spectrum of DIC.
Pathophysiology
The central pathogenic events in DIC are excessive generation
of thrombin and formation of intravascular fibrin clots, sec-
ondary activation of the fibrinolytic system, and consump-
tion of platelets and coagulation factors. Abnormalities of the
endogenous anticoagulants protein C and protein S may be
directly related to the pathogenesis of purpura fulminans by
contributing to the thrombotic tendency in patients with
DIC. Neonates with homozygous protein C deficiency present
with massive thrombosis of skin capillaries and veins, result-
ing in cutaneous necrosis, secondary sepsis, and death (pur-
pura fulminans neonatalis). Acquired deficiencies of proteins
C and S have been reported in liver disease and sepsis.
Purpura fulminans occurs most commonly in children and
often follows an infectious process such as scarlet fever or
streptococcal pharyngitis, meningococcemia, varicella, rube-
ola, or Rocky Mountain spotted fever. Purpura fulminans also
has been associated directly with S. aureus strains that pro-
duce high levels of toxic shock syndrome toxin 1 or staphylo-
coccal enterotoxins. Adults also may be affected, and the
syndrome may occur without a preceding illness.
Clinical Features
A. Symptoms and Signs—Cutaneous findings of DIC may
range from insignificant bruising and oozing from venipuncture
sites to massive hemorrhage and necrosis of skin and vital
organs. Purpura fulminans is characterized by the sudden
appearance of large, irregular areas of purpura, especially
over the extremities. The lesions are tender, enlarge rapidly,
and may evolve into hemorrhagic bullae with subsequent
necrosis and black eschar formation. The trunk, ears, and
nose may be involved. Necrosis of an entire extremity may
develop. Fever, chills, and hypotension almost always accom-
pany the disorder. Complications may include pulmonary,
hepatic, and renal failure, as well as GI bleeding and hemor-
rhagic adrenal infarction (Waterhouse-Friderichsen syn-
drome). Mortality rates range from 20–40%. The differential
diagnosis of purpura fulminans encompasses the entire spec-
trum of purpuric conditions.
B. Laboratory Findings—Because of the dynamic balance
between intravascular clot deposition and dissolution, serial
laboratory studies may be required to diagnose and monitor
DIC. The blood count usually shows thrombocytopenia, and
anemia may result from bleeding or microangiopathic
hemolysis. Consumption of coagulation factors and fibrino-
gen causes prolongation of the prothrombin time and partial
thromboplastin time. There is hypofibrinogenemia, and
increased fibrin degradation products (fibrin split products)
are present. More specific tests, such as measurement of the
D-dimer fragment, a breakdown product of cross-linked fib-
rin, may be helpful.
Treatment
Immediate attention must be directed toward stabilizing the
patient and treating the underlying cause. Heparin may pre-
vent further clot formation but should be avoided in patients
with suspected or documented intracranial bleeding. Plasma
or platelet replacement therapy may be indicated in patients
with active bleeding, but efficacy has not been proved in ran-
domized, controlled trials. Recombinant human activated
protein C should be considered in sepsis-related DIC.
Surgical debridement of necrotic eschars, grafting, and even
amputation are sometimes necessary.
Betrosian AP, Berlet T, Agarwal B: Purpura fulminans in sepsis. Am
J Med Sci 2006;332:339–45. [PMID: 17170624]
Fourrier F: Recombinant human activated protein C in the treat-
ment of severe sepsis: An evidence-based review. Crit Care Med
2004;32:S534–41. [PMID: 15542961]
Franchini M, Manzato F: Update on the treatment of disseminated
intravascular coagulation. Hematology 2004;9:81–5. [PMID:
15203862]
Kravitz GR et al: Purpura fulminans due to Staphylococcus aureus.
Clin Infect Dis 2005;40:941–7. [PMID: 15824983]
Levi M, de Jonge E, van der Poll T: Plasma and plasma components
in the management of disseminated intravascular coagulation.
Best Pract Res Clin Haematol 2006;19:127–42. [PMID:
16377546]
Zeerleder S, Hack CE, Wuillemin WA: Disseminated intravascular
coagulation in sepsis. Chest 2005;128:2864–75. [PMID:
16236964]
DERMATOLOGIC PROBLEMS IN THE INTENSIVE CARE UNIT
623
LIFE-THREATENING DERMATOSES
Pemphigus Vulgaris
ESSENTIALS OF DIAGNOSIS
Flaccid, easily ruptured blisters on noninflamed skin;
after rupture, nonhealing crusted erosions remain.
Superficial detachment of the skin after pressure or
trauma variably present (Nikolsky’s sign).
Skin biopsy shows characteristic intraepidermal cleft
just above the basal cell layer, with separation of ker-
atinocytes from one another (acantholysis).
Direct immunofluorescence of normal-appearing skin
shows intercellular IgG and complement deposition
throughout the epithelium.
General Considerations
Pemphigus vulgaris is a rare life-threatening autoimmune dis-
ease characterized by intraepithelial vesicles and bullae.
Stratified squamous epithelium of both skin and mucosal sur-
faces is involved. The pathogenic process involves circulating
IgG autoantibodies directed against the intercellular substance
of the epidermis. The mean age at onset is the sixth decade.
Clinical Features
A. Symptoms and Signs—Nonhealing oropharyngeal ero-
sions are common and often precede the skin findings by
weeks or months. The primary cutaneous lesion is a flaccid
blister on noninflamed skin. These blisters rupture easily,
leaving nonhealing erosions that ultimately develop crusts. A
positive Nikolsky sign (tractional pressure adjacent to a
lesion causes skin separation) is characteristic but not
pathognomonic. With treatment, the lesions generally heal
without scarring. The sites of predilection are the scalp, face,
axillae, and oral cavity. The conjunctival, vaginal, and
esophageal mucosa and the vermilion border of the lips also
may be involved. The process may become generalized.
Oropharyngeal involvement causes difficulty in swallowing,
and laryngeal involvement produces hoarseness. Prior to the
availability of corticosteroids, the mortality rate of pemphi-
gus approached 60–90% owing primarily to protein, fluid,
and electrolyte losses or to sepsis. More recently, the mortal-
ity rate has dropped to the range of 5–15%; the most com-
mon causes of death today are infection and complications
of treatment.
B. Laboratory Findings—The diagnosis is based on patho-
logic findings, including skin biopsy showing a characteristic
intraepidermal cleft just above the basal cell layer, with sepa-
ration of keratinocytes from one another (acantholysis). The
acantholytic cells line the vesicle and also lie free within the
cavity. A Tzanck smear from the base of a bulla may show
acantholytic epidermal cells. Direct immunofluorescence of
normal-appearing skin near a lesion shows intercellular IgG
and complement deposition throughout the epithelium.
Indirect immunofluorescence of the patient’s serum demon-
strates circulating intercellular autoantibodies in about
80–90% of patients specific for desmoglein-3 alone when
lesions are limited to the mouth and for both desmoglein-3
and -1 when skin lesions are present in addition to oral lesions.
However, titers of the circulating autoantibodies do not corre-
late with disease severity but often parallel disease activity.
Fluid, electrolyte, and nutritional disturbances may occur
but are less pronounced than in disorders involving loss of
the entire thickness of the epidermis (eg, TEN).
Differential Diagnosis
Histopathologic examination, immunofluorescent microscopy,
and bacterial cultures permit differentiation from EM, SJS,
TEN, bullous drug eruptions, and bullous impetigo, as well
as from other primary blistering diseases such as bullous
pemphigoid and dermatitis herpetiformis.
Treatment
Discontinue drugs known to cause pemphigus (eg, penicil-
lamine and captopril).
A. Specific Treatment—Prednisone, 60–120 mg/day, in com-
bination with azathioprine, 100–150 mg/day, is usually effective.
Prior to initiation of therapy, the patient should be evaluated for
contraindications to systemic steroids. Patients with a history of
tuberculosis or a positive skin test for tuberculosis need con-
comitant isoniazid while receiving immunosuppressive therapy.
When control of the blistering is achieved, prednisone is
reduced gradually as tolerated. Methotrexate, cyclophos-
phamide, mycophenolate mofetil, cyclosporine, intravenous
high-dose immunoglobulins, gold, chlorambucil, and plasma-
pheresis are alternative modalities, as is pulse corticosteroid
therapy. Monoclonal antibodies may be of value in the future.
B. Topical Therapy—Silver sulfadiazine or mupirocin oint-
ment may reduce secondary infection. Whirlpool treatments
are helpful in removing crusts from lesions. Oral mucosal
erosions may benefit from topical steroids, antiseptics, vis-
cous lidocaine, and attention to oral hygiene.
Akerman L, Mimouni D, David M: Intravenous immunoglobulin
for treatment of pemphigus. Clin Rev Allergy Immunol
2005;29:289–94. [PMID: 16391404]
Berookhim B et al: Treatment of recalcitrant pemphigus vulgaris
with the tumor necrosis factor alpha antagonist etanercept.
Cutis 2004;74:245–7. [PMID: 15551718]
Bystryn JC, Rudolph JL: Pemphigus. Lancet 2005;366:61–73.
[PMID: 15993235]
El Tal AK et al: Rituximab: A monoclonal antibody to CD20 used
in the treatment of pemphigus vulgaris. J Am Acad Dermatol
2006;55:449–59. [PMID: 16908351]
CHAPTER 28
624
Mutasim D: Management of autoimmune bullous diseases:
Pharmacology and therapeutics. J Am Acad Dermatol
2004;51:859–77. [PMID: 15583576]
Ruocco E et al: Life-threatening bullous dermatoses: Pemphigus
vulgaris. Clin Dermatol 2005;23:223–6. [PMID: 15896536]
Stanley JR, Amagai M: Pemphigus, bullous impetigo, and the
staphylococcal scalded-skin syndrome. N Engl J Med 2006;355:
1800–10. [PMID: 17065642]
Generalized Pustular Psoriasis
ESSENTIALS OF DIAGNOSIS
Acute onset of widespread sterile pustules arising on ten-
der, warm, erythematous skin that coalesce into lakes of
pus; the tongue and mouth are commonly involved.
Recurrent waves of pustulation and remissions occur;
fever and leukocytosis are often present; bacterial
infections and sepsis may be complications.
Arthritis and pericholangitis are sometimes present;
rarely, there is associated hypotension, high-output
heart failure, and renal failure; a history of psoriasis
may or may not be present.
Characteristic subcorneal pustules are seen on histologic
examination.
General Considerations
In addition to the exfoliative erythrodermic form of psoriasis,
another serious and sometimes fatal type is generalized pus-
tular psoriasis. It is characterized by the acute onset of wide-
spread erythematous areas studded with many sterile pustules
and associated with fever, chills, and leukocytosis. The disease
may develop either de novo or in individuals with a history of
psoriasis. The exact pathogenesis is unclear; however, precip-
itating events include topical and systemic corticosteroid
therapy and its subsequent withdrawal, other medications
(eg, sulfonamide drugs, penicillin, lithium, and pyrazolones),
infections, pregnancy, and hypocalcemia. Pustular psoriasis
tends to occur in patients over 40 years of age.
Clinical Features
A. Symptoms and Signs—The primary lesions are sterile
pustules that arise on tender, warm, erythematous skin and
coalesce into lakes of pus. Lesions typical of psoriasis vulgaris
may coexist. The tongue and mouth are commonly involved,
with geographic tongue and superficial erosions. These
patients appear ill and complain of itching and burning. The
course is punctuated by recurrent waves of pustulation and
remissions. Arthritis and pericholangitis sometimes occur.
Circulatory shunting through the skin may lead to significant
edema and, rarely, hypotension, high-output heart failure,
and renal failure. Superimposed bacterial infections or sepsis
can complicate the clinical picture.
B. Laboratory Findings—Laboratory data are nonspecific
but may be helpful. Leukocytosis, hypoalbuminemia, and
hypocalcemia are seen often during flares of this disorder,
although Gram stains and bacterial cultures of lesions are
negative. HIV serology should be checked because severe
exacerbations of psoriasis can be seen in HIV-infected indi-
viduals. Histologic examination of a lesion shows a charac-
teristic subcorneal pustule.
Differential Diagnosis
The diagnosis of pustular psoriasis is generally clear-cut on
clinical and histologic grounds. Other diagnostic consider-
ations include miliaria rubra, acneiform secondary syphilis,
pustular drug eruptions, and folliculitis. Cellulitis may be
suggested by the marked edema and erythema of the legs.
Treatment
A. Specific Treatment—The drugs of choice in this severe
form of psoriasis are the retinoids acitretin and isotretinoin.
These drugs should not be used in patients with lipid abnor-
malities or active hepatitis, and effective contraception must
be ensured during and for at least 3 years after treatment in
women of childbearing potential. Most patients show signif-
icant improvement in 5–7 days. Precipitating causes, includ-
ing lithium, antimalarials, diltiazem, propranolol, and
irritating topical medications, must be identified and
removed. Withdrawal from systemic corticosteroids is the
most common trigger. Oral acitretin works rapidly; but in
women of childbearing age, isotretinoin may be a better
choice because it has a shorter period of teratogenicity.
Methotrexate and cyclosporine are alternatives in carefully
selected patients; methotrexate is absolutely contraindicated
in HIV-infected patients. Hydroxyurea, mycophenolate
mofetil, and azathioprine have been used in some patients.
Recent case reports suggest that monoclonal antibodies to
tumor necrosis factor-α may be very helpful in patients with
pustular psoriasis. Systemic steroids should be avoided.
B. General Measures—A medium-potency topical steroid
applied twice daily to affected areas, emollient creams, cool
compresses, and baths alleviate discomfort. Attention must
be paid to fluid and electrolyte imbalances. The patient
should be monitored for secondary infection and sepsis.
Aaronson D, Lebwohl M: Review of therapy of psoriasis: The pre-
biologic armamentarium. Dermatol Clin 2004;22:379–88.
[PMID: 15450334]
Benoit S et al: Treatment of recalcitrant pustular psoriasis with
infliximab: Effective reduction of chemokine expression. Br J
Dermatol 2004:150:1009–12. [PMID: 15149518]
de Gannes GC et al: Psoriasis and pustular dermatitis triggered by
TNF-α inhibitors in patients with rheumatologic conditions.
Arch Dermatol 2007;143:223–31. [PMID: 17310002]
Mengesha YM, Bennett ML: Pustular skin disorders: Diagnosis and
treatment. Am J Clin Dermatol 2002;3:389–400. [PMID:
12113648]
DERMATOLOGIC PROBLEMS IN THE INTENSIVE CARE UNIT
625
Exfoliative Erythroderma
ESSENTIALS OF DIAGNOSIS
Generalized or nearly generalized diffuse erythema
with desquamation.
Pruritus, malaise, fever, chills, and weight loss may be
present.
There may be a history of primary dermatologic dis-
ease, or the erythroderma may be a sign of malignancy
(T-cell lymphoma); the cause in many cases remains
undetermined.
General Considerations
Exfoliative erythroderma is a clinical syndrome characterized
by generalized or nearly total diffuse erythema of the skin
accompanied by variable degrees of desquamation.
Exfoliative erythroderma is a nonspecific endpoint of skin
reactivity; multiple conditions can lead to it (Table 28–7).
Approximately half of all cases are due to exacerbation of a
primary dermatologic condition. Underlying skin diseases
such as psoriasis and various forms of eczema may become
generalized through neglect, the abrupt discontinuation of
therapy, or intercurrent cutaneous or systemic infection (eg,
HIV-infected individuals are at risk of development of ery-
throdermic psoriasis). Less commonly, exfoliative erythro-
derma is the initial manifestation of a dermatosis. The
remaining cases are nearly equally divided among undeter-
mined causes, drug reactions, and underlying malignancies,
most commonly cutaneous T-cell lymphoma.
Clinical Features
A. History—A careful history with attention to preexisting der-
matoses, family history of skin conditions, medication history,
and clues to occult malignancy may suggest a specific cause.
B. Symptoms and Signs—Most patients complain of pru-
ritus. The entire skin surface is red, scaly, and indurated.
Excoriations, peripheral edema, and moderate symmetric
lymph node enlargement are common; massive or asym-
metric lymphadenopathy and splenomegaly are suggestive
of an underlying lymphoma. The mucous membranes usu-
ally are spared. There may be symptoms of orthostatic
hypotension owing to increased insensible water loss.
Congestive heart failure owing to marked circulatory
shunting through the skin may develop in patients with
preexisting cardiac disease.
Thermoregulatory dysfunction can result in relative
hypothermia and chills, thereby concealing the fever of sep-
sis. Nevertheless, patients with erythroderma owing to
drugs or lymphoma—or patients with secondary infections—
often present with fever. Secondary bacterial infection
manifests as purulent exudate or crusting. Sepsis, pneumo-
nia, and complications of malignancy are the leading causes
of death.
C. Laboratory Findings—Laboratory studies are usually of
limited value in establishing the underlying cause but are
necessary for assessing response to the skin disease.
Leukocytosis and anemia are common, whereas eosinophilia
suggests a drug offender. Atypical circulating lymphocytes
(Sézary cells), if present in sufficiently high numbers, sug-
gest Sézary’s syndrome, the leukemic phase of cutaneous T-
cell lymphoma. Hypoalbuminemia and negative nitrogen
balance result from protein loss by desquamation and an
elevated metabolic rate. Serologic testing for HIV is recom-
mended for patients with erythrodermic psoriasis.
Other tests should include urinalysis and stool occult
blood, chest x-ray, and ECG. Skin biopsy results usually are
nonspecific but may be diagnostic in leukemia, cutaneous T-
cell lymphoma, or Norwegian crusted scabies. Routine
biopsy of superficial lymph nodes is even less helpful because
the pathologic findings are usually reactive (dermatopathic
lymphadenopathy). However, biopsy of unusually promi-
nent or asymmetric lymph nodes may yield a diagnosis of
lymphoreticular malignancy.
Differential Diagnosis
Exfoliative erythroderma should be differentiated from other
conditions associated with diffuse erythema, such as com-
mon morbilliform drug eruptions, various viral and bacter-
ial exanthems, early phases of TEN, toxic shock syndrome,
and graft-versus-host disease.
Treatment
Irrespective of the underlying cause, all exfoliative erythro-
dermas may be treated initially in a similar manner. The
Underlying dermatosis
Eczematous conditions
Contact dermatitis
Atopic dermatitis
Seborrheic dermatitis
Psoriasis
Pityriasis rubra pilaris
Pemphigus foliaceus
Norwegian scabies
Others
Drugs: See Table 28–2.
Malignancies
Cutaneous T cell lymphoma
Hodgkin’s disease
Miscellaneous lymphomas and leukemias
Idiopathic
Table 28–7. Causes of exfoliative erythroderma.
CHAPTER 28
626
goals of therapy are relief of symptoms and reduction of
cutaneous inflammation.
A. Specific Treatment—Once the cause is established, spe-
cific treatment may be initiated. Systemic steroids should be
avoided unless indicated as specific therapy for the underly-
ing disease.
B. General Measures—Patients must be monitored closely
for complications of erythroderma, including anemia, elec-
trolyte imbalances, high-output heart failure, hypothermia,
pneumonia, and sepsis. Administer systemic antibiotics to
patients with cutaneous or systemic infection. Adequate
nutrition is essential. One should stop any potentially
offending medications and keep the patient warm. Daily
whirlpool treatments aid in removing scale and decreasing
bacterial colonization. Baths and wet compresses also may be
used. After each whirlpool treatment, apply a medium-
potency topical steroid such as fluocinolone acetonide
0.025% and bland emollient such as petrolatum to the entire
body; frequent applications of the emollient each day help to
partially restore skin barrier function. Topical medium-
potency steroids such as fluoninolone acetonide 0.025%
ointment may be used 2–3 times daily. Antihistamines are
helpful in controlling pruritus.
Inspect the skin regularly for morphologic changes that
may be diagnostic of an underlying dermatitis as the ery-
throderma subsides.
Akhyani M et al: Erythroderma: A clinical study of 97 cases. BMC
Dermatol 2005;5:5. [PMID: 15882451]
Rothe MJ, Bernstein ML, Grant-Kels JM: Life-threatening erythro-
derma: Diagnosing and treating the “red man.” Clin Dermatol
2005;23:206–17. [PMID: 15802214]
Sigurdsson V et al: Erythroderma: A clinical and follow-up study
of 102 patients, with special emphasis on survival. J Am Acad
Dermatol 1996;35:53–7. [PMID: 8682964]
CUTANEOUS MANIFESTATIONS OF INFECTION
The febrile patient with a rash often presents a clinical
dilemma in that both noninfectious and infectious causes
must be considered. Among the noninfectious causes already
discussed are drug eruptions, vasculitis, and exfoliative ery-
throderma. In addition, systemic lupus erythematosus, juve-
nile rheumatoid arthritis, and Kawasaki’s disease may be
manifested as eruptions associated with fever.
Systemic viral, bacterial, rickettsial, and fungal diseases
may involve the skin, producing a multiplicity of cuta-
neous reactions that, in general, are not pathognomonic
either for infection or for a specific organism. The follow-
ing discussion focuses on life-threatening infections with
sufficiently distinctive skin findings to facilitate early diag-
nosis. Cutaneous manifestations of sepsis were addressed
earlier.
Varicella-Zoster
ESSENTIALS OF DIAGNOSIS
Primary infection—varicella
After a prodromal period of 1–3 days, small erythema-
tous macules appear and evolve into clear vesicles; pru-
ritus is intense; new crops appear at 3–5-day intervals.
Vesicles form crusted erosions; oropharyngeal vesicles
rupture quickly to form superficial mucosal ulcers.
In normal adults as well as immunosuppressed indi-
viduals, varicella may be complicated by life-
threatening pneumonia, hepatitis, myocarditis,
encephalitis, and DIC.
Reactivation infection—herpes zoster
Acute, usually painful unilateral eruption in dermatomal
distribution, with clusters of vesicles occurring on a
background of erythema; in persons with compromised
immune systems, the lesions may become severe and
necrotic.
General Considerations
Varicella-zoster virus (VZV) is a herpesvirus that typically
causes a self-limited infection but is capable of producing
life-threatening illness. Primary infection produces varicella;
reactivation of latent virus in sensory ganglia results in her-
pes zoster (shingles). Varicella is spread by direct person-to-
person contact or inhalation of infected droplets. Contact
with the lesions of herpes zoster may produce varicella in a
person not previously infected with VZV.
Clinical Features
A. Symptoms and Signs—After primary exposure to VZV,
the incubation period ranges from 11–21 days but may be
shorter in immunocompromised persons. The prodromal
symptoms in children are minimal and consist of low-grade
fever and malaise. In adults, the symptoms are more severe
and include prolonged fever, malaise, and arthralgias. One to
a few days after onset of illness, small erythematous macules
appear on the trunk, face, and proximal extremities. The pri-
mary lesion evolves rapidly into a clear vesicle that, if left
undisturbed, becomes cloudy. The vesicles eventually rup-
ture to form crusted erosions. New crops appear at irregular
intervals over the next 3–5 days, giving the characteristic
finding of lesions in various stages of development. Pruritus
is often intense. Healing with scarring is not uncommon,
particularly in excoriated or secondarily infected lesions.
Oropharyngeal vesicles rupture quickly to form superficial
mucosal ulcers. In normal adults as well as immunosup-
pressed individuals, varicella may be especially severe and
complicated by life-threatening pneumonia. Hepatitis,
