Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

POISONINGS & INGESTIONS
757
cramping and vomiting. Emesis can be treated with
antiemetics and a slowed administration rate of the solution.
Hyperchloremia has been reported and requires repeated
serum chloride determinations during the procedure. It is
also important to note that activated charcoal, if indicated,
should be given before the initiation of whole bowel irriga-
tion. Repeat-dose activated charcoal is not effective when
given during whole bowel irrigation.
5. Ion trapping—Once a drug has been absorbed from the
GI tract, gut decontamination measures become relatively
ineffective. Ion trapping is a method to enhance elimination
of an already absorbed drug by “trapping” it in the urine.
Drugs that acidify urine (eg, salicylates) ionize in alkaline
urine and then cannot be reabsorbed by the kidney and are
therefore excreted. This treatment is most helpful in salicy-
late and phenobarbital ingestions.
The simplest method for ion trapping uses 1 L of 0.45%
saline solution to which 2 ampules of sodium bicarbonate
have been added. The solution is infused intravenously at a
rate of 150–250 mL/h. Urine pH is monitored, with the goal
being a pH of 7.0–8.0. Potassium deficits need to be replaced
because alkalinization of the urine is difficult to achieve in
the hypokalemic patient. Complications of urinary alkalin-
ization are volume overload and hypokalemia.
6. Hemodialysis and hemoperfusion—In some situa-
tions, hemodialysis or hemoperfusion may be required to
eliminate the toxin. Indications include patients refractory to
supportive care alone, those who have a potentially toxic
drug level or highly toxic dose of the ingestant, and those in
whom other routes of elimination are impaired (eg, by renal
failure). Few toxins are amenable to this type of therapy;
cases in which hemodialysis or hemoperfusion may be useful
are listed in Table 36–8.
Current Controversies & Unresolved Issues
Administration of activated charcoal has become the pri-
mary means for decontamination of the gut in most cases of
toxic ingestion. Gastric lavage was once a mainstay for
decontamination of the gut and removal of the ingested
agent. Recent studies, however, have shown little change in
outcome for most patients who undergo gastric lavage. In
addition, this method has the potential for causing serious
side effects such as aspiration. Gastric lavage should be lim-
ited to patients who ingest a potentially lethal amount of an
agent poorly adsorbed to charcoal or those who present less
than 1 hour after ingesting a potentially significant amount
of a toxic agent—and it should be done with care.
Ipecac, a central- and peripheral-acting agent used to
induce vomiting in patients with toxic ingestions, was once a
common method of gastric decontamination. However, this
agent is no more effective than gastric lavage, and vomiting
after ipecac can persist for several hours, precluding the use
of oral activated charcoal. Its use is contraindicated in caus-
tic and hydrocarbon ingestions and in infants under 6
months of age. At this point, syrup of ipecac has little, if any,
role in the management of toxic ingestions.
In the past, forced diuresis was recommended in the treat-
ment of several drug ingestions. Studies have shown that forced
diuresis does not enhance elimination significantly and that the
relatively large volumes of intravenous crystalloid needed can
lead to pulmonary edema, particularly in patients with cardiac
dysfunction. Forced diuresis is therefore no longer recom-
mended as a modality in treating drug ingestions.
Bateman DN: Gastric decontamination: A view for the millen-
nium. J Accid Emerg Med 1999;16:84–6. [PMID: 10191436]
Bond GR: The role of activated charcoal and gastric emptying in
gastrointestinal decontamination: A state-of-the-art review.
Ann Emerg Med. 2002;39:273–86. [PMID: 11867980]
Krenzelok EP, McGuigan M, Lheur P: Position statement: Ipecac
syrup. American Academy of Clinical Toxicology, European
Association of Poisons Centre and Clinical Toxicologists. J Toxicol
Clin Toxicol 1997;35:699–709. [PMID: 9482425]
Mokhlesi B et al: Adult toxicology in critical care: I. General
approach to the intoxicated patient. Chest 2003;123:577–92.
[PMID: 12576382]
Watson WA et al: 2004 Annual Report of the American Association
of Poison Control Centers Toxic Exposure Surveillance System.
Am J Emerg Med 2005;23:589–666. [PMID: 16140178]
Zimmerman JL: Poisonings and overdoses in the intensive care
unit: General and specific management issues. Crit Care Med
2003;31:2794-801. [PMID: 14668617]
MANAGEMENT OF SPECIFIC POISONINGS
Sedative-Hypnotic Overdose
ESSENTIALS OF DIAGNOSIS
Dysarthria.
Ataxia.
Emotional lability.
Altered sensorium.
Horizontal and vertical nystagmus.
Respiratory, cardiovascular, and renal failure.
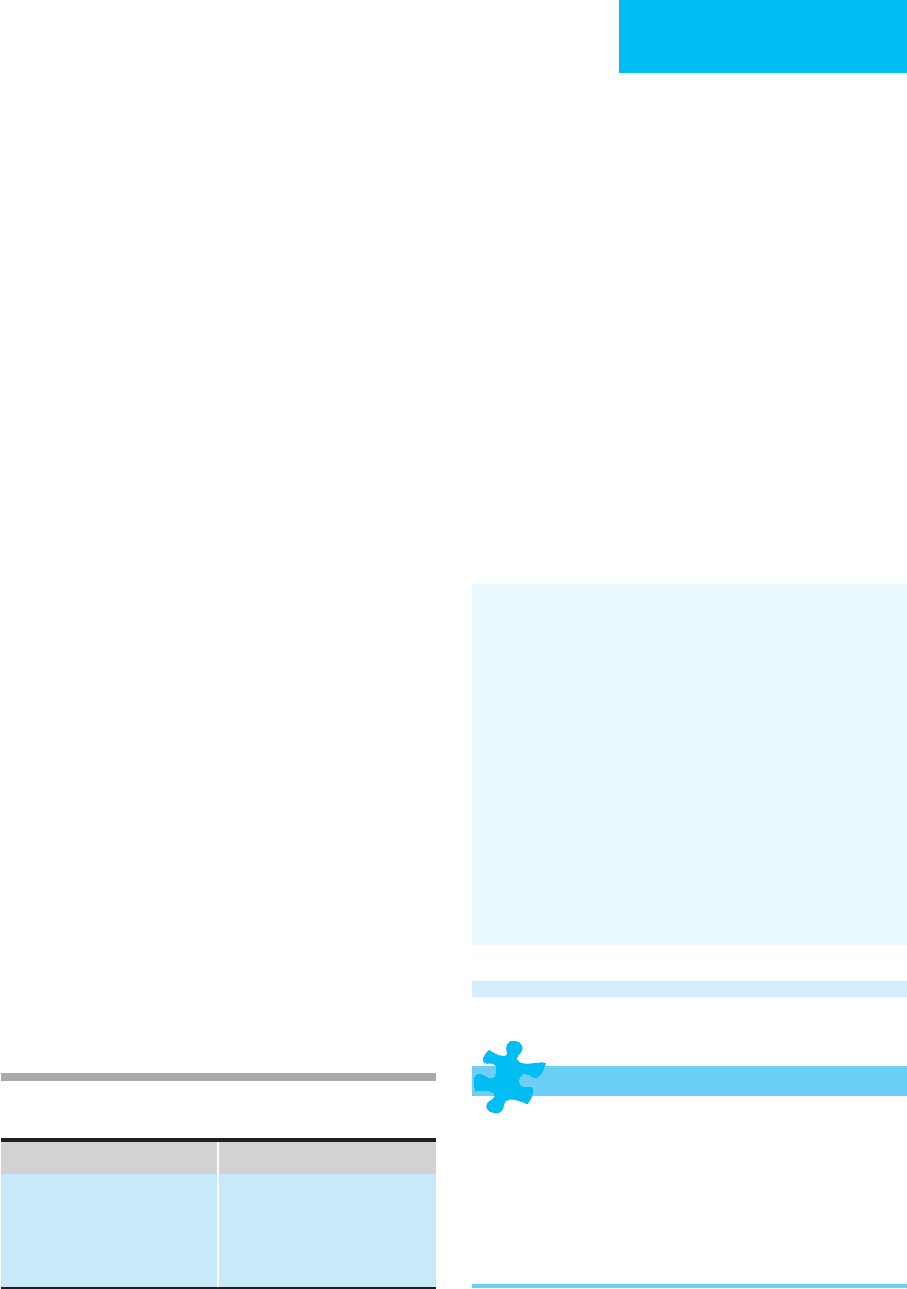
Table 36–8. Poisons amenable to hemoperfusion or
hemodialysis.
Hemoperfusion Hemodialysis
Digitalis
Carbamazepine
Paraquat
Phenobarbital
Theophylline
Ethylene glycol
Methanol
Lithium
Salicylate
Theophylline

CHAPTER 36
758
General Considerations
Sedative-hypnotic abuse is common, particularly among
patients who began using the drugs therapeutically for
sleep or as anxiolytics. Other patients may use these drugs
orally or intravenously because of the disinhibition and
euphoria they produce. In the past, short-acting barbitu-
rates such as amobarbital, pentobarbital, and secobarbital
were used commonly; these agents are used much less fre-
quently because benzodiazepines are now prescribed more
commonly. Their use is frequently combined with other
drugs or with alcohol.
Continued abuse of sedative-hypnotics is more likely to
cause mental and physical impairment when compared
with narcotics. When administered intravenously, the alka-
line barbiturate solutions cause sclerosis of the veins and
may result in profound ischemia if intraarterial injection
occurs.
Withdrawal from sedative-hypnotics produces a charac-
teristic syndrome that may be fatal. Although a period of ini-
tial improvement may occur after 8–16 hours of abstinence,
rapid deterioration with agitation, altered mental status, and
seizures frequently follows. ICU admission is mandatory for
any patient suspected of having barbiturate withdrawal
symptoms.
Clinical Features
A. Symptoms and Signs—An overdose of these drugs results
in findings similar to those of intoxication with alcohol: ataxia,
altered sensorium, and dysarthria. Both horizontal and vertical
nystagmus may be present. When intoxication is severe, respira-
tory and cardiovascular compromise may occur. Ventilation is
usually slow and shallow, and pulmonary edema or pneumoni-
tis may develop. Centrally mediated vasomotor depression
results in a decrease in blood pressure. If perfusion is not main-
tained, renal failure may follow. Tissue hypoxia may develop as
a result of decreased respiratory function, and pupillary dilation
may be seen. Deep tendon reflexes also may be depressed.
B. Laboratory Findings—Routine laboratory studies should
include electrolytes and an arterial blood gas determination.
A sample of blood should be obtained and sent for barbitu-
rate concentration determination. Lethal levels vary widely
depending on patient factors and the presence of coinges-
tants. An acetaminophen level should be determined in case
this agent was coingested.
C. Imaging Studies—A chest x-ray is advisable to evaluate
the extent of atelectasis and pneumonitis present at the time
of admission.
Differential Diagnosis
Ingestions of nonbarbiturate sedatives such as chloral
hydrate, ethchlorvynol, glutethimide, methyprylon, and
methaqualone are the considerations when treating a barbi-
turate overdose. Coingestion of alcohol, benzodiazepines, or
opioids also must be considered.
Treatment
A. General Measures—When cardiovascular and respira-
tory parameters are normal and stable, supportive care gener-
ally is all that is required. However, when intoxication is
severe, hypoventilation and depressed cough and gag reflexes
are indications for intubation to protect the airway, prevent
aspiration, and allow for mechanical ventilation as needed.
B. Decontamination—Lavage generally should be consid-
ered if ingestion has been within the preceding 45 minutes.
Food in the stomach decreases absorption and may prolong
the time during which lavage is useful; however, if obtunda-
tion is a concern, the risks of lavage may not outweigh any
potential benefits of this procedure.
C. Diuresis—Although believed to be useful in the past,
forced diuresis is no longer felt to be useful. Sodium bicar-
bonate to alkalinize the urine prevents tubular reabsorption
of phenobarbital and supplemental potassium chloride
should be given to ensure alkalinization of the urine. Careful
serum electrolyte monitoring is mandatory.
D. Cardiovascular Support—Hypotension usually responds
to the administration of balanced salt solutions such as nor-
mal saline or lactated Ringer’s solution, although vasopres-
sors may be required. If large amounts of fluid are necessary
for resuscitation, fluid administration should be guided by
central venous or pulmonary artery catheter monitoring to
prevent pulmonary edema.
E. Hemodialysis—When renal failure occurs, hemodialysis
may be necessary. Most of the barbiturates are dialyzable,
although the short-acting forms have the lowest percentage
of removal.
Withdrawal
Withdrawal from sedative-hypnotics may be fatal. Symptoms
of withdrawal typically occur after 8–16 hours of abstinence
and include anxiety, tremulousness, weakness, and insomnia.
GI symptoms include abdominal cramping, anorexia, nau-
sea, and vomiting. As withdrawal progresses, neurologic
findings become predominant and are characterized by
twitching, coarse tremors, increased startle response, and
hyperactive deep tendon reflexes. After 2–3 days, grand mal
seizures may occur. As the seizures subside, improvement usu-
ally is noted, although some patients develop organic brain
syndrome with disorientation, visual and auditory hallucina-
tions, and delusions. Hyperthermia may lead to cardiovascular
collapse and death.
When withdrawal is suspected, the patient should be given
an intravenous dose of pentobarbital or phenobarbital based on
an estimate of the most recent consumption. This dose then can
be reduced by about 10% per day until the patient is drug-free.
POISONINGS & INGESTIONS
759
Mohammed Ebid AH, Abdel-Rahman HM: Pharmacokinetics of
phenobarbital during certain enhanced elimination modalities
to evaluate their clinical efficacy in management of drug over-
dose. Ther Drug Monit 2001; 23:209–16. [PMID: 11360027]
Palmer BF: Effectiveness of hemodialysis in the extracorporeal
therapy of phenobarbital overdose. Am J Kidney Dis
2000;36:640–3. [PMID: 10977799]
Opioids
ESSENTIALS OF DIAGNOSIS
Decreased level of consciousness.
Depressed respiration.
Miosis.
Pulmonary edema.
General Considerations
Narcotic abuse is a major problem worldwide. Although the
drugs of choice traditionally have been morphine and
heroin, the shorter-acting agents such as fentanyl have come
into vogue, especially among health care workers. Most nar-
cotics are administered intravenously because of the rapid
euphoria they produce. Methadone, a long-acting oral agent,
is used commonly in narcotic addiction treatment/mainte-
nance programs. Pentazocine is a synthetic analgesic with
both agonist and antagonist properties. When given to a
narcotic-dependent patient, pentazocine may cause with-
drawal symptoms. In high doses, it can cause visual halluci-
nations and dysphoria.
Immediate care of the narcotic overdose or withdrawal
patient focuses on resuscitation, stabilization, and use of
antidotes. Critical care of patients suffering from narcotic
overdose and withdrawal may include the treatment of con-
ditions caused by narcotic use and the sharing of injection
needles. These include pulmonary hypertension (presum-
ably from cotton fiber emboli), endocarditis (from bacterial
contamination), necrotizing fasciitis, and tetanus. Other
reported complications include hepatitis, AIDS, cutaneous
abscesses, and Guillain-Barré syndrome. Many patients will
use other intoxicants concurrently, such as alcohol or
cocaine, which complicates their care.
Clinical Features
A. Symptoms and Signs—Patients with opioid overdoses
present most commonly with decreased level of conscious-
ness, depressed respiration, and miotic pupils. In severe
cases, such as cases of attempted suicide, respiratory depres-
sion may be pronounced. Pulmonary edema may be seen,
particularly in heroin overdose. Other common findings
include hypo- or hyperthermia, emesis, hypoxia, hypoten-
sion, and depression of deep tendon reflexes.
B. Laboratory Findings—A blood sample should be sent for
toxicology screen and alcohol level and to check for other
CNS depressants. Routine electrolytes, a complete blood
count, and liver function tests should be obtained. In cases of
pulmonary edema, pulse oximetry and/or an arterial blood
gas analysis will help to assess severity. In patients with oral
opioid ingestions, an acetaminophen level should be deter-
mined. If the patient is febrile and uses opioids by injection
blood cultures should be sent.
C. Imaging Studies—A chest x-ray should be obtained in
patients suspected to have pulmonary edema or other indi-
cations of pulmonary compromise. A head CT scan may be
useful in patients with depressed level of consciousness who
do not respond appropriately to naloxone to exclude the
presence of a mass lesion or intracranial bleed.
Treatment
A. General Measures—Most patients transferred to the
ICU will already have been stabilized and intravenous access
established. Patients should be reassessed on arrival to the
ICU because those with significant narcotic overdose are at
high risk for respiratory depression and airway compromise.
If indicated by either a low blood glucose determination or
in the obtunded patient in whom this measurement cannot
be made, 50 mL of 50% dextrose should be given intra-
venously along with 100 mg thiamine.
Mechanical ventilation may be required both for
decreased respiratory drive and for management of pul-
monary edema. Hypotension usually responds to volume
infusion and correction of hypoxia. Pulmonary edema
caused by narcotic overdose usually does not respond to the
customary regimen of diuretics and preload and afterload
reduction, and intubation is often required.
B. Decontamination—If the use of coingestants is sus-
pected, administration of activated charcoal is advisable; this
can be done either orally or via an nasogastric (NG) tube. If
there is a risk of aspiration, however, charcoal should be used
only if it has a high likelihood of improving the patient’s
outcome.
C. Narcotic Antagonists—Several narcotic antagonists have
been used—naloxone, naltrexone, nalmefine, nalorphine, and
levallorphan; the latter two also have agonist properties.
Although naltrexone is longer-acting than naloxone, its use in
the acute setting has been disappointing, and naloxone is the
drug of choice in this situation. An initial dose of 0.2–0.8 mg
should be administered intravenously for heroin and mor-
phine overdoses, titrating to response. When the abused drug
is codeine, pentazocine, or propoxyphene, an initial dose of
up to 2 mg naloxone may be required. When effective, an
improvement in respiration and mental status typically
occurs in less than 2 minutes, often in seconds. If no response
to a total dose of 2 mg is seen, the diagnosis of narcotic

CHAPTER 36
760
overdose should be questioned. Because the half-life of nalox-
one is substantially shorter than that of most narcotic agents,
repeat dosing may be required to prevent recurrence of respi-
ratory and mental status depression. Continuous administra-
tion of naloxone intravenously may be required in some cases
to prevent relapse of respiratory depression.
D. Other Modalities—Because of the complications associ-
ated with narcotic abuse, additional therapy in the ICU may
be required for pulmonary edema, pneumonitis, cardiac
valvular compromise, or infectious complications. Overdosage
with meperidine may cause hyperactive reflexes and convul-
sions. Rhabdomyolysis may occur, particularly in patients
who have been obtunded for a significant amount of time; if
not treated, patients may develop renal failure from the myo-
globinuria seen in this condition.
Withdrawal
Withdrawal from narcotics produces autonomic distur-
bances, hyperexcitability, and personality changes character-
ized by drug-seeking behavior. Within the first 8 hours of
withdrawal, lacrimation, rhinorrhea, diaphoresis, and sneez-
ing are common. This is followed by nausea and vomiting,
diarrhea, and abdominal cramping. Patients may exhibit
tremors and twitching in association with myalgias.
Pilomotor erection produces the “cold turkey” appearance of
the skin. All the symptoms are relieved by the administration
of narcotic.
Clark NC, Lintzeris N, Muhleisen PJ: Severe opiate withdrawal in a
heroin user precipitated by a massive buprenorphine dose. Med
J Aust 2002;176:166–7. [PMID: 11913917]
Compton WM, Volkow ND: Major increases in opioid analgesic
abuse in the United States: Concerns and strategies. Drug
Alcohol Depend 2006;81:103–7. [PMID: 16023304]
Joranson DE, Ryan KM, Gilson AM, Dahl JL: Trends in medical use
and abuse of opioid analgesics. JAMA 2000;283:1710–4. [PMID:
10755497]
Paulozzi LJ: Opioid analgesic involvement in drug abuse deaths in
American metropolitan areas. Am J Public Health
2006;96:1755–7. [PMID: 17008568]
Sachdeva DK, Jolly BT: Tramadol overdose requiring prolonged
opioid antagonism. Am J Emerg Med 1997;15:217–8. [PMID:
9115538]
Sympathomimetics
ESSENTIALS OF DIAGNOSIS
Agitation, anxiety, hallucinations, psychosis.
Seizures.
Coma, stroke, encephalopathy.
Hypertension, tachycardia.
General Considerations
Sympathomimetics are a category of drugs that induce a
physiologic state similar to that caused by catecholamine
release. Many different prescription, over-the-counter, and
recreational or abuse drugs fall into this category.
Examples include amphetamine and its derivatives, over-
the-counter products for appetite control, cold remedies, and
stimulants (eg, phenylpropanolamine, caffeine, ephedrine, and
pseudoephedrine).
Overuse of sympathomimetics causes toxicity by induc-
ing excessive release of neurotransmitters, including epi-
nephrine and norepinephrine, and the subsequent α- and
β-adrenergic effects they produce. α-Adrenergic effects are
primarily vasoconstriction, diaphoresis, and dilated pupils;
β
1
-adrenergic effects lead to tachycardia, and β
2
-adrenergic
effects cause bronchodilation and vasodilation. The clini-
cal effects that result from any specific sympathomimetic
drug depend on the relative α- or β-adrenergic actions of
that drug (eg, phenylpropanolamine is an α-selective drug
that causes hypertension, diaphoresis, and mydriasis).
Duration of toxicity is usually limited; however, patients
may demonstrate prolonged toxicity if they ingest bags con-
taining the drug for illicit transport or if they use “Ice,” a
long-acting, smokable form of methamphetamine.
Clinical Features
A. Symptoms and Signs—Sympathomimetic toxicity
causes a toxic syndrome that includes primarily CNS and
cardiovascular effects (see Table 36–2). Both illicit drug users
and those who use excessive amounts of over-the-counter
medications (eg, diet aids, stimulants, and cold medications)
may present with sympathomimetic poisoning.
CNS toxicity is manifested as agitation, anxiety, delusions,
hallucinations, paranoia, and seizures. Sympathomimetics
may cause a psychotic state indistinguishable from that seen
in schizophrenia; although almost always temporary, this
psychosis may take weeks to months to resolve. Less common
but more severe effects include coma, strokes (ischemic and
hemorrhagic), hypertensive encephalopathy, and focal neu-
rologic deficits.
Cardiovascular effects include hypertension and sinus
tachycardia. Hypertension may be of rapid onset and severe.
Because these patients often do not have underlying hyper-
tension, they have no CNS autoregulation at these exces-
sively high blood pressures. As a result, they are much more
likely to suffer serious CNS sequelae such as hemorrhagic
strokes or encephalopathy from acute hypertension. Sinus
bradycardia or atrioventricular block occurs mainly after
ingestion of drugs with primarily α-agonist properties.
Patients may suffer tachydysrhythmias, cardiac ischemia,
and rarely, infarction.
Other findings include rhabdomyolysis with or without
renal failure, diarrhea, intestinal cramping, and hyperther-
mia. Pupils typically are dilated if the patient ingests an agent

POISONINGS & INGESTIONS
761
with α-adrenergic properties; by the same mechanism, these
patients also may be diaphoretic.
B. Laboratory Findings—Laboratory abnormalities are
variable and not diagnostic. Toxicology screening may be
positive for sympathomimetic drugs, but it is by no means
comprehensive of the wide array of available agents; there-
fore, a negative screen does not exclude sympathomimetic
toxicity. Leukocytosis is common as a result of demargina-
tion caused by catecholamine stimulation. Patients should
have a creatine kinase (CK) determination to evaluate for
rhabdomyolysis. Serum electrolytes (especially potassium)
and blood pH should be tested.
C. Imaging Studies—CT scanning is indicated in patients
with altered mental status or seizures.
Differential Diagnosis
Thyrotoxicosis may present in a manner identical to sympa-
thomimetic overdose. A history of thyroid disease is sugges-
tive of the diagnosis, as is the presence of goiter or physical
findings suggestive of hyperthyroidism. CNS infections may
cause similar clinical findings. Drug withdrawal (eg, ethanol
and benzodiazepines) also presents with agitation and car-
diovascular abnormalities. Similar clinical findings result
from toxic effects of theophylline, tricyclic and SSRI antide-
pressants, anticholinergics, isoniazid, phencyclidine, and
salicylates, and from interaction between monoamine oxi-
dase inhibitors and other drugs. The agitation and paranoia
seen in these patients may mimic psychiatric disorders such
as schizophrenia.
Treatment
A. General Measures—After initial assessment and stabi-
lization, treatment should be individualized to the drug
involved and the toxic clinical effects manifest. If the drug
was ingested, gastric lavage should be considered if presenta-
tion is within 1 hour of ingestion or if the patient is trans-
porting the drugs as a body packer. Care must be taken to
protect the airway because these patients may seize as a result
of their ingestion. Activated charcoal should be administered
to all patients with an oral ingestion. Repeat-dose activated
charcoal is helpful in enhancing caffeine elimination. Forced
diuresis, hemodialysis, and hemoperfusion are not helpful in
these poisonings.
B. Hypertension—Hypertension is a medical emergency in
these patients because of the risk of hemorrhage or
encephalopathy. Patients with evidence of end-organ dys-
function from hypertension (eg, headache, renal compro-
mise, cardiac ischemia, and heart failure) should be treated
with antihypertensive agents. Nitroprusside is a good choice
because it is easily titratable and doses can be adjusted rap-
idly. Phentolamine may be used in patients who overdose on
pure α-agonists such as phenylpropanolamine. Although
nifedipine is a potent antihypertensive agent, it is not easily
titrated, and cases of prolonged hypotension from its use
have been reported. Labetalol may be a good choice in
patients with significant tachycardia.
C. Arrhythmias—Sinus tachycardia rarely requires interven-
tion. Supraventricular tachycardia is usually benign; how-
ever, when the patient suffers compromise from the rapid
ventricular response, verapamil or adenosine may be used to
control the rhythm. Esmolol may be used to treat both
supraventricular tachycardia and ventricular dysrhythmias.
Esmolol and other β-adrenergic blockers may worsen hyper-
tension because of unopposed α-adrenergic activity.
D. Seizures—Seizures and agitation should be treated with
benzodiazepines. Status epilepticus may develop and may
require treatment with phenobarbital and phenytoin. If these
medications are ineffective, paralysis may be required to pre-
vent rhabdomyolysis, acidosis, and hyperthermia.
Continuous electroencephalographic monitoring is required
in these patients because they may continue to have electri-
cal seizure activity despite chemical paralysis.
E. Psychosis—Benzodiazepines may be used to treat psy-
chosis associated with sympathomimetic overdoses.
Although neuroleptics have been used in the past, they can
lower the seizure threshold and alter thermoregulation; their
use probably should be avoided in this situation.
F. Myocardial Ischemia—Although actual myocardial
infarction is rare, patients with angina pectoris should be
managed with aspirin, nitrates, and heart rate control.
Patients usually respond to this treatment and should be
monitored for elevation of cardiac enzymes or changes in the
ECG consistent with myocardial infarction.
G. Hyperthermia—Hyperthermia can be severe and life-
threatening. When present, aggressive treatment is war-
ranted. Patients with agitation or seizures should receive
benzodiazepines. Antipyretics are rarely helpful. All clothing
should be removed and patients sprayed with a mist of water
or covered with damp sheets to increase evaporation, and a
fan is helpful. Those with excessive agitation or seizures who
do not respond to benzodiazepines may need paralysis to
control heat production.
Derlet RW, Horowitz BZ: Cardiotoxic drugs. Emerg Med Clin
North Am 1995;13:771–91. [PMID: 7588189]
Guharoy R et al: Methamphetamine overdose: Experience with six
cases. Vet Hum Toxicol 1999;41:28–30. [PMID: 9949482]
Holstege CP, Eldridge DL, Rowden AK: ECG manifestations: the
poisoned patient. Emerg Med Clin North Am 2006;24:159–77.
[PMID: 16308118]
Swalwell CI, Davis GG: Methamphetamine as a risk factor for
acute aortic dissection. J Forensic Sci 1999;44:23–6. [PMID:
9987866]

CHAPTER 36
762
Phencyclidine
ESSENTIALS OF DIAGNOSIS
Nystagmus.
Hypertension.
Tachycardia.
Agitation, psychosis, violent behavior.
Seizures.
General Considerations
Phencyclidine (PCP), pharmacologically related to ketamine,
is an illicit hallucinogen used as a recreational drug. The
usual method of consumption is by smoking cigarettes that
have been soaked in a solution of PCP. PCP also can be used
via the intranasal route or by ingestion. Some patients have
become intoxicated from percutaneous exposure by han-
dling the drug. Absorption is rapid by any route; effects are
seen within a few minutes to half an hour. The drug is highly
lipid-soluble, and inconstant release from adipose tissue may
lead to waxing and waning findings that are predominantly
due to CNS effects. Metabolism is primarily in the liver. The
half-life varies from 7 hours to over 3 days.
Clinical Features
The clinical presentation of PCP intoxication is extremely
variable, ranging from confusion to agitation. Alterations in
mental status are erratic, and violent behavior often occa-
sions transport to a hospital. Concurrent use of other drugs
of abuse is common, and the treating physician must be
aware of this possibility when evaluating these patients. In
addition, phencyclidine is an analgesic agent. These patients
may suffer significant traumatic injuries with minimal find-
ings on examination.
A. Symptoms and Signs—The most common findings
(>50% of patients) are nystagmus (horizontal, vertical, or
rotatory) and hypertension. Although hypertension is com-
mon, medical complications are rare. Tachycardia is also
common, but rates over 130 beats/min are unusual. The level
of consciousness may vary from comatose to agitated to fully
alert. Mental status may wax and wane, and unpredictable
and precipitous violent outbursts may occur. These patients
may require physical and chemical restraints to prevent them
from hurting themselves or the medical personnel caring for
them. Hallucinations, frank psychosis, and seizures are com-
mon. Most symptoms resolve spontaneously within hours;
however, some patients may remain symptomatic for several
days or even a week. The psychosis may last months, and in
these cases, recovery may be gradual. Rhabdomyolysis is a
relatively common complication of PCP intoxication and
may lead to renal failure in up to 2.5% of cases.
B. Laboratory Findings—Urine for PCP level may be sent to
confirm the diagnosis. Quantitative levels are not necessary
and do not correlate with clinical effects. If patients who
appear to be PCP-intoxicated have negative urine results,
they need to be evaluated for other causes of their symptoms
(see “Differential Diagnosis” below).
Elevated creatine kinase levels are found in up to 70% of
cases and can occur even in the absence of excessive muscle
activity. Although usually positive for blood, initial urine
dipstick may be negative despite a significant elevation in
CK, so all patients with PCP intoxication should have a
serum sample sent for CK measurement.
C. Concealed Injuries—Because PCP has anesthetic proper-
ties, patients may suffer significant trauma in the prehospital
setting that may not be manifested in the usual fashion. All
patients should undergo a thorough physical evaluation for
trauma and be reevaluated several times during the hospital
stay, particularly as their mental status improves.
Differential Diagnosis
Lethargic patients may have consumed other intoxicants,
including sedative-hypnotic drugs or barbiturates. Patients
who are agitated or violent must be evaluated for possible
sympathomimetic use or a withdrawal syndrome. Other
causes include head trauma, infection (eg, meningitis or
encephalitis), metabolic derangements, and psychiatric
disorders.
Treatment
A. Decontamination—Gastric lavage is rarely indicated
because PCP is typically inhaled. If patients ingest the agent,
activated charcoal should be used.
B. Supportive Measures—Most patients respond to mini-
mal measures such as being placed in a quiet, darkened room
with minimal stimulation. Benzodiazepines may be useful to
decrease agitation. In some cases, however, specific treatment
measures may be necessary.
Patients with hypertension or tachycardia rarely need
intervention for these problems; end-organ dysfunction
should be managed in the usual manner. Hyperthermia
requires treatment with antipyretics and cooling measures as
necessary. Seizures should be treated with benzodiazepines.
If the patient develops refractory seizures, phenytoin may be
used, but neuromuscular blockade may be required to pre-
vent acidosis, hyperkalemia, and rhabdomyolysis.
Continuous electroencephalographic monitoring is required
in this situation.
In the past, urinary acidification was advocated to cause
urinary ion trapping of the drug and enhance elimination.
Because only a small amount of the drug is excreted
unchanged in the urine, and because induction of aciduria is
difficult to achieve and may lead to renal dysfunction owing
to rhabdomyolysis, this treatment is no longer recommended.
POISONINGS & INGESTIONS
763
C. Hydration—If serum CK is elevated, vigorous hydration is
required, and intravenous crystalloid is the mainstay of ther-
apy. Normal saline should be used until the patient is
volume-repleted and has a good urine outflow; the goal is a
urine output of 150 mL/h. Adequate urine output is the
mainstay of therapy, but additional therapy with intravenous
mannitol and bicarbonate also may be used. Follow serial CK
levels to ensure that levels decrease. BUN and creatinine lev-
els should be measured to monitor renal function, and potas-
sium levels and blood gases should be followed to evaluate
hyperkalemia and acidosis.
D. Restraints and Sedation—Patients who are agitated or
violent may require physical or chemical restraints. The use
of physical restraints alone may exacerbate rhabdomyolysis
as the patient fights against the restraints. Restrained patients
should be placed in a quiet room to avoid stimulation.
Benzodiazepines or haloperidol may be used for sedation.
Brust JC: Acute neurologic complications of drug and alcohol
abuse. Neurol Clin 1998;16:503–19. [PMID: 9537972]
Greydanus DE, Patel DR: The adolescent and substance abuse:
Current concepts. Dis Mon 2005;51:392–431. [PMID: 16316792]
Haroz R, Greenberg MI: Emerging drugs of abuse. Med Clin North
Am 2005;89:1259–76. [PMID: 16227062]
Leshner AI: Hallucinogens and dissociative drugs including LSD,
PCP, ketamine, dextromethorphan. National Institute on Drug
Abuse Research Report Series. NIH Pub. No. 01-4209.
Washington: NIH, 2001.
Mokhlesi B, Garimella PS, Joffe A et al: Street drug abuse leading
to critical illness. Intensive Care Med 2004;30:1526–36. [PMID:
14999443]
Wills B, Erickson T: Drug- and toxin-associated seizures. Med Clin
North Am 2005;89:1297–321. [PMID: 16227064]
Cocaine
ESSENTIALS OF DIAGNOSIS
Hypertension.
Tachycardia and other dysrhythmias.
Headache.
Myocardial infarction.
Transient ischemic attacks, stroke.
Seizures.
General Considerations
Cocaine is available as cocaine hydrochloride, a water-soluble
crystalline salt that can be used intranasally or dissolved and
injected intravenously. Cocaine is also available in an alkaloid
form that is not water-soluble and can be smoked in a free-
base form or mixed with baking soda and water and smoked
as the “crack” form. Absorption from all sites is rapid. The
half-life varies with the route of administration; intravenous
use or smoking leads to a half-life of 60–90 minutes, whereas
intranasal or oral use has a half-life of several hours.
Cocaine has several effects. It causes CNS release of neu-
rotransmitters, including dopamine; acts as a local anes-
thetic; blocks neuronal catecholamine reuptake; and inhibits
serotonin reuptake. The end result of these mechanisms is a
spectrum of clinical findings primarily involving the central
nervous and cardiovascular systems. Respiratory and meta-
bolic effects also may be noted.
Clinical Features
A. Symptoms and Signs—Hypertension occurs frequently
and can be severe. It can lead to intracranial bleeding, aortic
dissection, and cardiac ischemia. Tachycardia is also com-
mon, as are dysrhythmias, including atrial fibrillation, atrial
tachycardia, ventricular tachycardia, and rarely, asystole.
Cocaine is a potent vasoconstrictor that may result in
organ ischemia. Myocardial infarction, bowel ischemia, renal
infarction, and limb ischemia all have been reported. A com-
bination of vasospasm, enhanced platelet aggregation, and
enhanced workload caused by an excessive demand for oxy-
gen produces end-organ dysfunction. In addition to organ
ischemia, cocaine can cause a myocarditis manifested by ele-
vated CK-MB enzymes and diffuse ST-segment elevations or
T-wave inversions on ECG.
There are many CNS manifestations of cocaine toxicity.
Headache is common in chronic abusers. In patients who
develop CNS complications owing to cocaine, cerebral
infarction occurs in about one-fourth, subarachnoid hemor-
rhage in another one-fourth, and intraparenchymal hemor-
rhage in the remainder.
Patients who abuse cocaine also may present with
depressed mental status or frank coma, a condition known as
cocaine abstinence syndrome. This phenomenon is likely due
to CNS depletion of neurotransmitters. These patients char-
acteristically have been using large amounts of cocaine for
over a week and present either after a seizure or when they
are found obtunded. They may be frankly comatose or
extremely difficult to arouse, often prompting extensive
medical evaluation of their altered mental status. Typically,
they awaken completely within 24 hours.
Seizures occur in up to 2% of cocaine abusers, and
although they usually occur soon after cocaine use, they may
not present until several hours later. Transient ischemic
attacks have been described and may lead to stroke; cocaine
use should be considered in the differential diagnosis of a
young patient with a stroke. Strokes are independent of the
route of administration and may occur as late as 24 hours
after use. They can present in first-time users but are more
common in chronic abusers.
Pulmonary complications include pneumothorax and
pneumomediastinum in patients who smoke or snort
cocaine. Pulmonary edema is rare in most cases of cocaine
CHAPTER 36
764
toxicity but is a common finding in patients who die of
cocaine intoxication.
Rhabdomyolysis may occur with excess muscle activity
and hyperthermia. Hyperthermia, when present, is often
severe.
B. Laboratory Findings—Laboratory evaluation of patients
with serious intoxication should include an ECG and meas-
urements of serum electrolytes, total CK levels, and a urine
test for myoglobin. Blood for cardiac markers may be indi-
cated by the patient’s clinical presentation. Toxicology
screens for cocaine may focus the diagnosis.
C. Imaging Studies—CT head scanning should be per-
formed in any patient with a concerning headache or in
those with neurologic findings or altered mental status. Plain
films of the abdomen may reveal packets in the intestines of
patients who swallow containers of the drug for the purpose
of transport (“body packers”).
Differential Diagnosis
Other stimulants, including sympathomimetics, SSRIs, theo-
phylline, phencyclidine, and anticholinergic drugs, can cause
a similar clinical picture. Withdrawal from ethanol or benzo-
diazepines may present similarly, as can thyrotoxicosis and
CNS infection. Psychiatric disorders are also in the differen-
tial diagnosis.
Treatment
A. Supportive Measures—Basic supportive measures such
as intravenous access, fluid administration, and supplemen-
tal oxygen should be initiated as indicated by the clinical sit-
uation. Gastric decontamination is not indicated in most
cases; however, patients who have ingested packets of the
drug are candidates for whole bowel irrigation.
B. Hyperthermia—When hyperthermia is present, the
patient should be undressed completely and sprayed with a
cool mist or draped with a wet sheet. A fan can be used to
facilitate evaporation. Ice packs should be placed at the neck,
axillae, and groin. Care should be taken not to overcool the
patient. Antipyretic agents are not effective.
C. Seizures—Initial treatment of agitation and seizures
should be with benzodiazepines. Neuroleptics may be effec-
tive, but since they lower the seizure threshold, their use is
discouraged. Seizures refractory to benzodiazepines can be
treated with phenobarbital or phenytoin. Status epilepticus
unresponsive to this therapy should be treated with pharma-
cologic paralysis and mechanical ventilation; continuous
EEG monitoring is necessary in these cases to ensure that the
paralyzed patient is not seizing.
D. Hypertension—Mild hypertension usually does not require
intervention. Severe hypertension or labile hypertension
should be treated with intravenous nitroprusside. Labetalol is
another alternative, especially in the tachycardiac patient.
Tachydysrhythmias that require treatment may respond to β-
blockers such as esmolol or metoprolol, but the patient must
be observed carefully for the development of worsening hyper-
tension from the unopposed α-adrenergic stimulation and β-
adrenergic blockade. Concurrent use of nitroprusside with
β-blockers is often necessary. Patients suspected of having a
myocardial infarction should receive standard therapy, but may
or may not have classic arteriosclerotic coronary artery disease.
E. Rhabdomyolysis—Rhabdomyolysis should be treated
with isotonic fluids to ensure a urine output of over 150 mL/h.
The addition of mannitol or alkalinization also may be
useful.
Camus P et al: Drug-induced and iatrogenic infiltrative lung dis-
ease. Clin Chest Med 2004;25:479–519. [PMID: 15331188]
Feldman JA et al: Acute cardiac ischemia in patients with cocaine-
associated complaints: Results of a multicenter trial. Ann Emerg
Med 2000;36:469–76. [PMID: 11054201]
Hollander JE, Henry TD: Evaluation and management of the
patient who has cocaine-associated chest pain. Cardiol Clin
2006;24:103–14. [PMID: 16326260]
Kleerup EC et al: Chronic and acute effects of “crack” cocaine on
diffusing capacity, membrane diffusion, and pulmonary capil-
lary blood volume in the lung. Chest 2002;122:629–38. [PMID:
12171843]
Miller MB: Arrhythmias associated with drug toxicity. Emerg Med
Clin North Am 1998;16:405–17. [PMID: 9621850]
Shanti CM, Lucas CE: Cocaine and the critical care challenge. Crit
Care Med 2003;31:1851–9. [PMID: 12794430]
Tricyclic Antidepressants
ESSENTIALS OF DIAGNOSIS
Tachycardia, arrhythmias.
Seizures.
Sensorium may range from awake and alert to comatose.
Mydriasis.
Dry skin.
Ileus.
Urinary retention.
General Considerations
Tricyclic antidepressants (TCAs) such as amitriptyline, doxepin,
and trimipramine work therapeutically by blocking reuptake
of norepinephrine into adrenergic nerves, but they also have
significant toxic effects related to their anticholinergic
and α-adrenergic blocking properties. When ingested, they
are absorbed rapidly; in overdose situations, owing to the slowed
intestinal motility from the anticholinergic effects, absorption
may be prolonged, increasing the half-life to as much as 3–4 days.

POISONINGS & INGESTIONS
765
Clinical Features
A. Signs and Symptoms—Patients with TCA overdose may
deteriorate rapidly, progressing from awake with normal
vital signs to having seizures or cardiac arrest within less than
an hour of significant ingestion. Mental status may range
from awake and alert to having seizures to frankly comatose.
Patients with suspected TCA ingestion need immediate
medical evaluation and close observation. Evaluation often
reveals both central and peripheral anticholinergic effects:
tachycardia, mydriasis, dry skin, urinary retention, ileus, ele-
vated temperature (usually mild), altered mental status (eg, agi-
tation, anxiety, delirium, and coma), seizures, and occasionally,
respiratory depression. Cardiovascular effects are usually the
cause of death and can include sinus tachycardia, dysrhyth-
mias, atrioventricular blockade, and hypotension (decreased
contractility and α-adrenergic blockade). This ingestion
should be suspected in any patient who presents with seizures,
anticholinergic signs (including coma), and cardiovascular
abnormalities, particularly if the ECG is abnormal.
B. Electrocardiography—The single most valuable initial test
in patients suspected of having a TCA overdose is the ECG.
Common findings include sinus tachycardia, PR-interval and
QT-segment prolongation, and nonspecific ST-segment
changes. QRS complex prolongation suggests a serious over-
dose. Rightward and superior terminal QRS forces (a wide,
prominent S wave in leads I, aVF, and V
6
, with a prominent R
wave in aVR) are very suggestive of TCA overdose.
C. Laboratory Findings—General laboratory evaluation is
rarely helpful. Drug levels correlate poorly with toxic effects
and can vary widely in an individual patient.
D. Imaging Studies—Since some TCAs are radiopaque, a
plain film of the abdomen may show tablets in the stomach
or intestines.
Differential Diagnosis
The combination of altered mental status, seizures, and car-
diovascular abnormalities suggests several diagnoses.
Toxicologic causes include phenothiazines, anticholinergics,
and theophylline; less commonly, β-blockers, calcium chan-
nel blockers, and local anesthetic drug overdose (eg, lido-
caine) can cause these findings. Nontoxicologic causes
include meningitis, sepsis, hypoglycemia (severe), anaphy-
laxis, and head trauma.
Treatment
A. Initial Management—General measures aimed at stabi-
lization, monitoring, and intravenous access should be insti-
tuted rapidly. A urinary catheter should be placed to monitor
urine output and provide easy determination of urine pH.
Syrup of ipecac should be avoided because these patients may
deteriorate rapidly and become obtunded before vomiting
begins, placing them at risk for aspiration. Gastric lavage should
be considered in patients presenting within 1 hour of ingestion
of a large amount of TCAs. If gastric lavage is performed,
suction and airway management equipment must be readily
available in the event the patient develops seizures. Activated
charcoal, 100 g, should be placed down the lavage tube (if
used) or given to the patient via NG tube. There is some evi-
dence that a repeated-dose activated charcoal regimen (every
2–4 hours) may be helpful in significant ingestions.
TCA overdose patients need to be admitted to the ICU if
they have any of the following: persistent tachycardia (>120
beats/min); dysrhythmias, including premature ventricular
contractions; QRS >100 ms; hypotension; or evidence of
CNS toxicity. Patients admitted should be monitored until
they are free of toxicity for 24 hours. Patients who present
with none of the preceding and do not develop any of the
listed admission criteria after 6 hours of observation may be
discharged; a psychiatric evaluation before discharge is pru-
dent and is mandatory in cases of attempted suicide.
B. Bicarbonate Therapy—Alkalinization of the blood is a
mainstay in the therapy of TCA ingestion. It effectively treats
most of the major adverse effects of the drug, including
hypotension, cardiac conduction abnormalities, and dys-
rhythmias. Alkalinization has varying efficacy in the treat-
ment of seizures and coma. Optimal blood pH is 7.50, and
the urine pH should be over 7.0. Alkalinization is achieved by
intravenous sodium bicarbonate therapy; in intubated
patients, transient hyperventilation will alkalinize the blood
until intravenous therapy can be initiated.
Supportive care and alkalinization therapy usually are ade-
quate to manage patients with TCA overdose. In some cases,
additional measures will be needed to stabilize the patient.
Those with severe agitation, delirium, or seizures may require
benzodiazepines or barbiturates for control. Dysrhythmias
refractory to alkalinization can be treated with lidocaine or
cardioversion. Class Ia antiarrhythmic agents should be
avoided in this patient population because they can exacerbate
dysrhythmias. Hypotension that does not respond to alkalin-
ization can be managed with fluid boluses or with vasopres-
sors; since the hypotension is often due to α-adrenergic
blockade, α-adrenergic agonists (eg, phenylephrine or
methoxamine) are a good choice. Dopamine may be ineffec-
tive or may exacerbate hypotension owing to its β-agonist
effects (peripheral β
2
-adrenergic stimulation produces vasodi-
lation). Hemodialysis and hemoperfusion are relatively inef-
fective in these patients because the TCAs are highly
protein-bound and not easily removed by these measures.
Current Controversies and Unresolved Issues
In the past, physostigmine was recommended for treatment
of TCA overdose. As an acetylcholinesterase inhibitor,
physostigmine increases acetylcholine availability at receptor
sites and reverses central and peripheral anticholinergic
effects. It has not been proven to be effective in treating
hypotension, ventricular dysrhythmias, and conduction dis-
turbances, which are the major causes of fatal toxicity in TCA
overdoses. Significant adverse effects such as atrioventricular
CHAPTER 36
766
blockade, bradycardia, and asystole may occur with
physostigmine. Therefore, use of physostigmine is not rec-
ommended in the treatment of TCA overdose.
Kerr GW, McGuffie AC, Wilkie S: Tricyclic antidepressant over-
dose: A review. Emerg Med J 2001;18:236–41. [PMID:
11435353]
Liebelt EL et al: Serial electrocardiogram changes in acute tricyclic
antidepressant overdoses. Crit Care Med 1997;25:1721–6.
[PMID: 9377889]
Liebelt EL, Francis PD, Woolf AD: ECG lead aVR versus QRS inter-
val in predicting seizures and arrhythmias in acute tricyclic
antidepressant toxicity. Ann Emerg Med 1995;26:195–201.
[PMID: 7618783]
O’Connor N et al: Prolonged clinical effects in modified-release
amitriptyline poisoning. Clin Toxicol (Phila) 2006;44:77–80.
[PMID: 16496498]
Seger DL et al: Variability of recommendations for serum alkalin-
ization in tricyclic antidepressant overdose: A survey of U.S.
poison center medical directors. J Toxicol Clin Toxicol
2003;41:331–8. [PMID: 12870873]
Thanacoody HK, Thomas SH: Tricyclic antidepressant poisoning:
Cardiovascular toxicity. Toxicol Rev 2005;24:205–14. [PMID:
16390222]
Woolf AD et al: Tricyclic antidepressant poisoning: An evidence-
based consensus guideline for out-of-hospital management.
Clin Toxicol (Phila) 2007;45:203–33. [PMID: 17453872]
Serotonin Syndrome
ESSENTIALS OF DIAGNOSIS
Coma, somnolence, confusion, agitation, or seizures.
Autonomic instability, including fever, diaphoresis,
tachycardia, hyper- or hypotension, mydriasis.
Clonus (may be spontaneous), especially ocular clonus,
rigidity, hyperreflexia.
History of use of serotonin-based antidepressants or
other drugs associated with serotonin release.
General Considerations
The serotonin syndrome historically has been associated with
cocaine, amphetamines, and other drugs that cause increased
release of serotonin, such as a drug of abuse, 3,4–methylene-
dioxymethamphetamine (MDMA or “ecstasy”), or dex-
tromethorphan, bromocriptine, and linezolid. With the
increased use of selective serotonin reuptake inhibitors
(SSRIs) as antidepressants, overdose of these agents is respon-
sible for a number of cases of serotonin syndrome.
Clinical Features
A. Symptoms and Signs—The serotonin syndrome shares
many symptoms and signs with overdose of sympath-
omimetics (eg, tachycardia and mydriasis) and with the
neuroleptic malignant syndrome (eg, rigidity, hyperthermia,
and alterations of mental status). In fact, distinguishing sero-
tonin syndrome from these may be difficult. Most cases of
serotonin syndrome are mild and self-limited, but severe
complications can include diaphroresis with severe fluid loss,
rhabodomyolysis, marked hyperthermia, and death.
Diagnostic criteria have been proposed, but these are some-
what nonspecific.
B. Laboratory Findings—Laboratory evaluation in patients
with serious intoxication should include an ECG and meas-
urements of serum electrolytes, total CK levels, and urinary
myoglobin. There are no specific tests for this syndrome,
although toxicology studies may demonstrate the presence of
concomitant cocaine, amphetamines, or other drugs.
Differential Diagnosis
The differential diagnosis includes sympathomimetic over-
dose, including amphetamines and cocaine, both of which
also can trigger the serotonin syndrome. A more confusing
clinical picture is the neuroleptic malignant syndrome, in
which muscular rigidity, altered mental status, and hyper-
thermia are key features. Some authors have suggested that
dilated pupils with clonus and hyperreflexia rather than
severe muscle rigidity make it more likely to be the serotonin
syndrome. A key differential feature is evidence of an over-
dose of an SSRI or other drug. While neuroleptic malignant
syndrome may occur at any time after a neuroleptic is pre-
scribed, it is not more likely after an overdose. Other possible
syndromes include thyroid storm and withdrawal from ben-
zodiazepines or ethanol.
Treatment
A. Supportive Measures—Basic supportive measures such
as intravenous fluid administration and supplemental oxy-
gen should be initiated as indicated by the clinical situation.
When hyperthermia is present, the patient should be
undressed completely and sprayed with a cool mist or draped
with a wet sheet. A fan can be used to facilitate evaporation.
Ice packs should be placed at the neck, axillae, and groin.
Care should be taken not to overcool the patient. Antipyretic
agents are not effective.
B. Specific Treatment—Potential drugs precipitating the
serotonin syndrome should be discontinued. Benzodiazepines
generally are considered useful for the serotonin syndrome.
They are anticonvulsants, are not associated with serotonin
release, and are anxiolytic and sedating. Dantrolene uncou-
ples excitation-contract in skeletal muscles and has been
used in malignant hyperthermia, neuroleptic malignant
syndrome, and serotonin syndrome. There are case reports
of benefit from dantrolene in serotonin syndrome but no
controlled trials.
C. Current Controversies—A number of authors have com-
mented on the approach when it is not clear whether a
