Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

POISONINGS & INGESTIONS
777
theophylline toxicity. Of the two procedures, hemoperfusion
is the method of choice. It is important to initiate these pro-
cedures early because if hemodynamic instability develops,
hemodialysis may not be possible.
Cantrell FL: Treatment of theophylline overdose. Am J Emerg Med
1997;15:547. [PMID: 9270403]
Charytan D, Jansen K: Severe metabolic complications from theo-
phylline intoxication. Nephrology (Carlton) 2003;8:239–42.
[PMID: 15012710]
Chyka PA et al: Prophylaxis of seizures after theophylline overdose.
Pharmacotherapy 1997;17:1044–5. [PMID: 9324199]
Shannon M: Life-threatening events after theophylline overdose: A
10-year prospective analysis. Arch Intern Med 1999;159:989–94.
[PMID: 10326941]
Shannon MW: Comparative efficacy of hemodialysis and hemop-
erfusion in severe theophylline intoxication. Acad Emerg Med
1997;4:674–8. [PMID: 9223689]
Methanol & Ethylene Glycol
ESSENTIALS OF DIAGNOSIS
Methanol:
Visual disturbances.
Nausea, vomiting, abdominal pain.
Lethargy and confusion.
Seizures and coma.
Abdominal tenderness.
Ethylene glycol:
Stage I: intoxication, slurred speech, ataxia, stupor, hal-
lucinations, seizures, coma.
Stage II: hypertension, tachycardia, high-output renal
failure, myositis.
Stage III: costovertebral angle tenderness; oliguria or
anuria.
General Considerations
Methanol and ethylene glycol are CNS depressants that are
found most commonly in antifreeze and deicing products.
Ingestions of these compounds occur sporadically in alco-
holic patients seeking an ethanol substitute, as an accidental
ingestion, or epidemically in groups of patients seeking CNS
effects. Both methanol and ethylene glycol are absorbed rap-
idly from the GI tract. Methanol blood levels peak 30–90
minutes after ingestion, whereas ethylene glycol levels peak
1–4 hours after ingestion. Although the parent compounds
are relatively benign, both are metabolized in the liver by
alcohol dehydrogenase to toxic metabolites. Formic acid is
the major toxic metabolite of methanol; glycolic acid and
oxalic acid are the predominant metabolites of ethylene gly-
col. The half-lives of methanol and ethylene glycol are 14–18
and 3–8 hours, respectively. When ethanol is ingested at the
same time as either compound, the half-life can more than
double because alcohol dehydrogenase preferentially metab-
olizes ethanol. Ingestions as small as 30–60 mL of these com-
pounds have been fatal in adults. Even very small amounts
may cause significant morbidity.
Clinical Features
A. Symptoms and Signs—If presentation is soon after
ingestion, apparent intoxication may be the only finding.
Because toxicity is from metabolites rather than from the
parent compound, specific toxic clinical effects may not be
noted for many hours after ingestion. The delay is increased
when ethanol is ingested at the same time.
1. Methanol—The latent period from ingestion of
methanol to manifestations of toxicity is 12–24 hours. At that
time, about half of patients will complain of visual distur-
bances, which include cloudy, blurred, or misty vision.
Scotomas are common. The patient typically appears intoxi-
cated and often complains of a headache. Nausea, vomiting,
and abdominal pain are common. Ophthalmologic examina-
tion may reveal multiple eye abnormalities, including dilated
and fixed pupils, constricted visual fields, retinal edema, and
hyperemia of the optic disk. However, some patients may
have a completely normal eye examination despite having
subjective visual complaints. Patients may be lethargic or
confused. Seizures and coma may occur. Abdominal tender-
ness is common. Death may follow abrupt respiratory arrest
without warning, so careful monitoring is mandatory.
2. Ethylene glycol—Ethylene glycol ingestion presents in
three stages. Stage I, known as the CNS stage, occurs 30 minutes
to 12 hours after ingestion. It is characterized by intoxication,
slurred speech, ataxia, stupor, hallucinations, seizures, and
coma. The patient may complain of nausea and vomiting and
may be mildly hypertensive and tachycardic. Stage II, the
cardiopulmonary stage, manifests 12–24 hours after inges-
tion. Patients become significantly hypertensive and tachy-
cardic and may develop high-output cardiac failure. Some
patients also develop diffuse myositis with muscle tenderness.
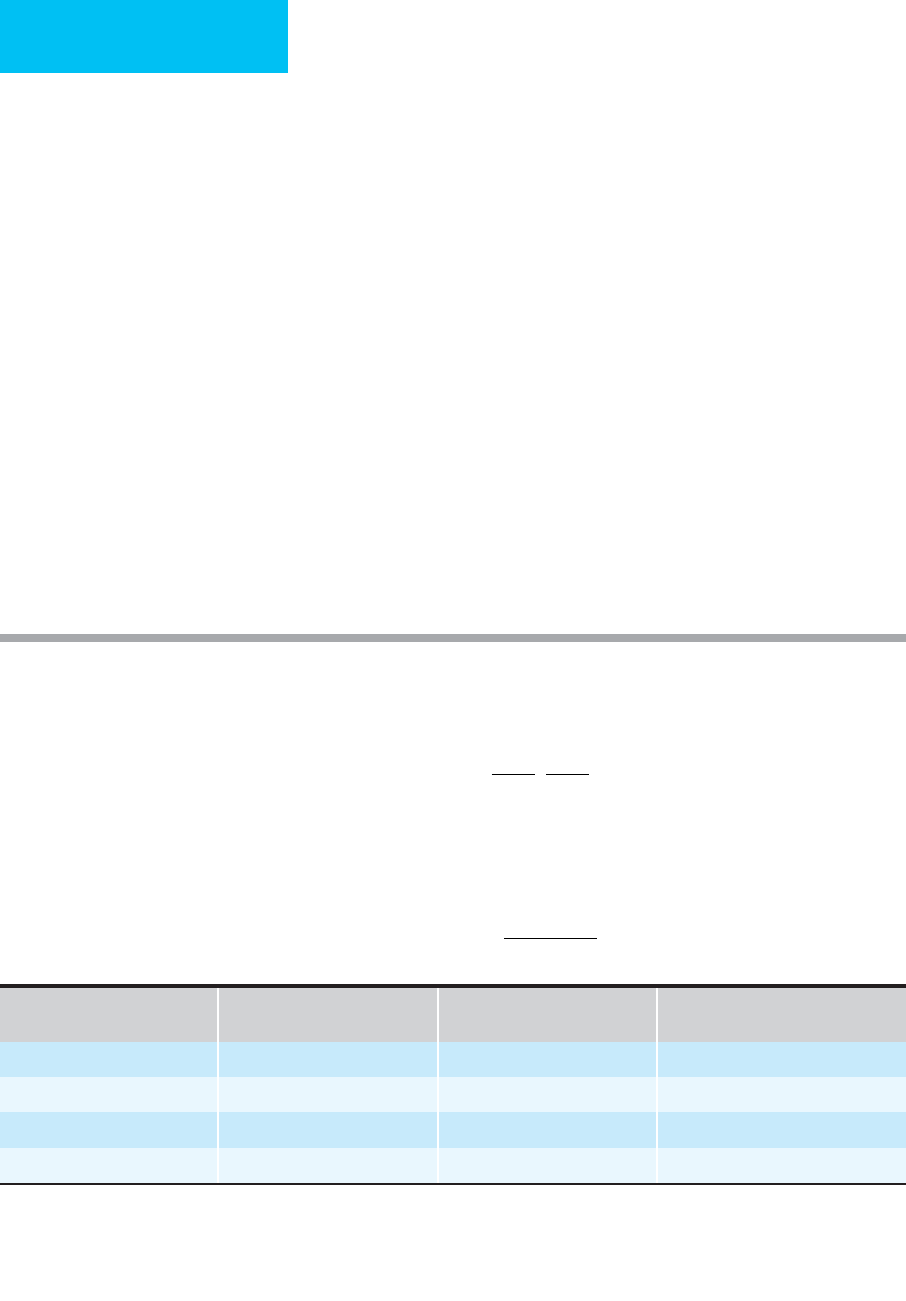
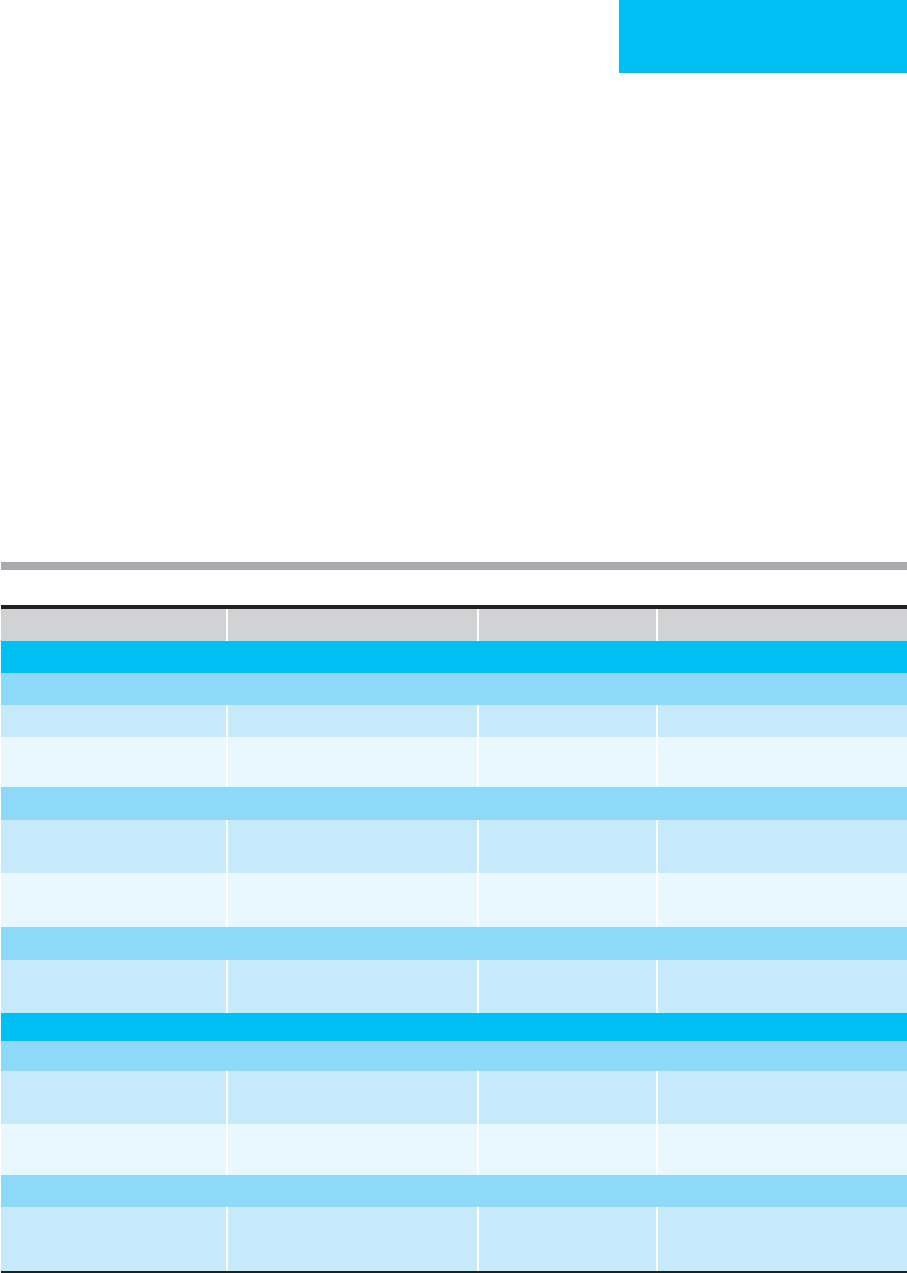
Refractory dysrhythmias, hypotension, or seizures
Acute ingestion with level >90–100 mg/L
Chronic ingestion with—
Level 60–90 mg/L
Level 40–60 mg/L and—
Age <6 months or >60 years
Congestive heart failure
Liver disease
Unable to tolerate oral charcoal
Patient not tolerating current level
Table 36–12. Indications for hemoperfusion or
hemodialysis in theophylline toxicity.
CHAPTER 36
778
Stage III, the renal stage, occurs 24–72 hours after ingestion.
Patients complain of flank pain and costovertebral angle ten-
derness. Oliguria, frank renal failure, and anuria develop.
B. Laboratory Findings—Laboratory evaluation of these
patients is notable for an elevated osmolal gap (Table 36–13).
Most patients with ethylene glycol ingestion have crystalluria at
presentation. The crystals can be either envelope-shaped cal-
cium oxalate crystals or needle-shaped calcium oxalate mono-
hydrate crystals. Leukocytosis and hypocalcemia occur in up to
85% of patients who ingest ethylene glycol. Metabolic acidosis
with an increased anion gap is sometimes the first clue to
ingestion of these toxic alcohols.
Treatment
A. General Measures—Supportive care should be initiated
as described rapidly. Gastric lavage is rarely effective after
ingestion of these compounds.
B. Specific Treatment—Specific treatment of these intoxi-
cations is the mainstay of therapy and is similar for both
methanol and ethylene glycol.
Any patient with a history, clinical presentation, or labo-
ratory findings suggestive of methanol or ethylene glycol
ingestion should be treated. There are three major goals:
(1) to correct the metabolic acidosis, (2) to block the produc-
tion of metabolites, and (3) to remove the parent compound
and toxic metabolites.
1. Acidosis—Acidosis is treated with intravenous sodium
bicarbonate. Bicarbonate therapy should be initiated when
the pH drops below 7.2, with therapy directed at maintaining
the pH above that level. Massive doses of bicarbonate may be
required because the toxic metabolites are inorganic acids
that are being produced continuously. Blood pH should be
measured frequently. Iatrogenic hypernatremia may develop
if large doses of bicarbonate are needed.
2. Metabolites—Production of toxic metabolites can be
blocked by administering either ethanol or fomepizole, both
of which alter metabolism of the parent compounds to toxic
metabolites by alcohol dehydrogenase. Ethanol can be
administered either orally or intravenously. The loading dose
of ethanol for an average adult is 0.6 g/kg (1.2 mL/kg of 50%
ethanol orally or 6 mL/kg of 10% ethanol intravenously over
30 minutes). Intravenous solutions should be at concentra-
tions of 10% or less to decrease toxicity. Infusion should
provide blood ethanol levels of 100–150 mg/dL to ensure
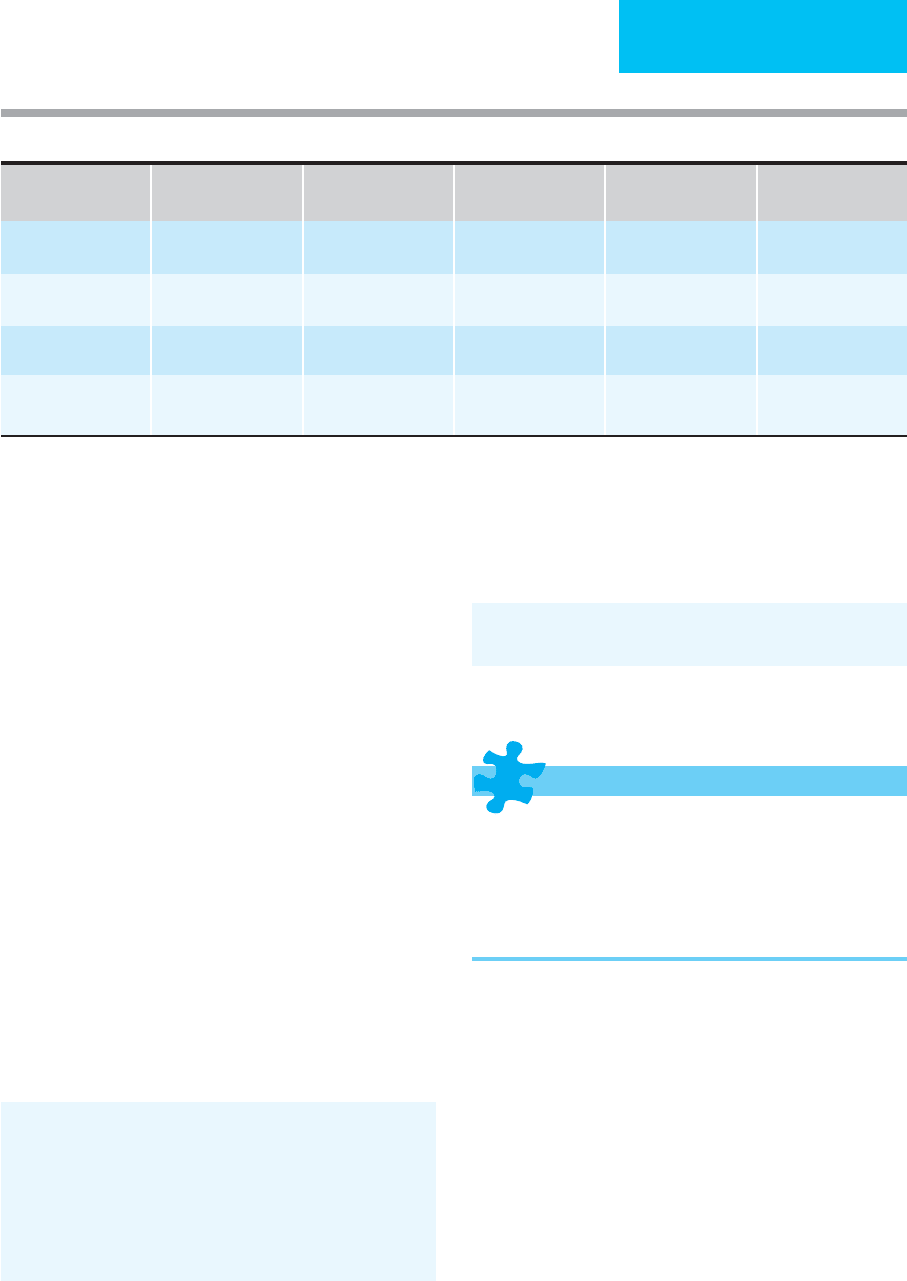
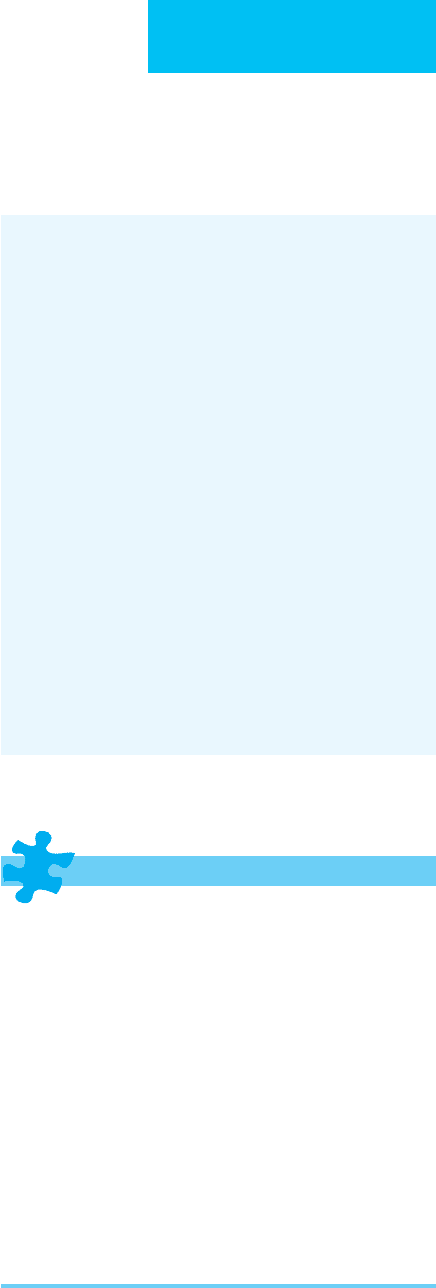
Molecular Weight Toxic Concentration
Approximate
Corresponding ΔGosm (mosm/kg)
Ethanol 46 300 65
Methanol 32 50 16
Ethylene glycol 62 100 16
Isopropanol 60 150 25
Note: Most laboratories use the freezing point method for calculating osmolality. If the vaporization point method is used, alcohols are
driven off and their contribution to osmolality is lost.
Note: A normal osmolar gap may be present in the face of a potentially lethal methanol or ethylene glycol ingestion.
Modified from Saunders CE, Ho MT (editors): Current Emergency Diagnosis & Treatment, 4th ed. Originally published by Appleton & Lange.
Copyright © 1992 by The McGraw-Hill Companies, Inc.
Table 36–13. Use of the osmolal gap in toxicology.
The osmolal gap (Δosm) is determined by subtracting the calculated serum osmolality from the measured serum osmolality.
Δosm = Measured osmolality – Calculated osmolality
Serum osmolality may be increased by contributions of circulating alcohols and other low-molecular-weight substances. Since these substances are not
included in the calculated osmolality, there will be a gap proportionate to their serum concentration and inversely proportionate to their molecular weight:
Serum concentration
(mg/dL)
osm
Molecul
=×Δ
aar weight
10
Calculated
osmolality
(mosm/kg)
Na meq/L=
+
2[ ( )] ++
Glucose
(mg/dL)
18
+
BUN
(mg/dL)
2.8
POISONINGS & INGESTIONS
779
preferential metabolism of ethanol over the toxic alcohol.
Since alcohol dehydrogenase has a higher affinity for ethanol
and will preferentially metabolize ethanol rather than the
toxic alcohols, the goal is to maintain a blood ethanol level of
100–150 mg/dL, which saturates the enzyme (Table 36–14).
Fomepizole (4-methylprazole) may be preferred over
ethanol for the treatment of methanol and ethylene glycol
ingestions. This agent blocks the metabolism of the toxic
alcohols by alcohol dehydrogenase. It offers the benefit of not
needing to maintain a blood level as with ethanol treatment,
but it is expensive. Fomepizole is extremely effective, but
dialysis remains necessary to definitively remove the alcohols
and their metabolites.
3. Decontamination—Once bicarbonate and ethanol or
fomepizole therapy have been instituted, hemodialysis is begun
to remove the parent compound and toxic metabolites. This
has the additional benefit of correcting severe acidosis refrac-
tory to intravenous bicarbonate therapy. However, hemodialy-
sis also removes ethanol. Patients with methanol ingestion also
should receive folic acid, 50 mg intravenously every 4 hours.
Those with ethylene glycol ingestion should be given thiamine,
100 mg intramuscularly, and pyridoxine, 100 mg orally.
Barceloux DG et al: American Academy of Clinical Toxicology
practice guidelines on the treatment of ethylene glycol poison-
ing. J Toxicol Clin Toxicol 1999;37:537–60. [PMID: 10497633]
Green R. The management of severe toxic alcohol ingestions at a
tertiary care center after the introduction of fomepizole. Am J
Emerg Med 2007;25:799–803. [PMID: 17870485]
Hovda KE et al: Fomepizole may change indication for hemodial-
ysis in methanol poisoning: Prospective study in seven cases.
Clin Nephrol 2005;64:190–7. [PMID: 16175943]
Megarbane B, Borron SW, Baud FJ: Current recommendations for
treatment of severe toxic alcohol poisonings. Intensive Care
Med. 2005;31:189–95. [PMID: 15627163]
Isopropyl Alcohol
ESSENTIALS OF DIAGNOSIS
Headache, dizziness, confusion.
Intoxication with poor coordination.
Abdominal pain, nausea, vomiting.
Tachycardia.
Miosis and nystagmus.
General Considerations
Isopropyl alcohol is a clear and colorless liquid found in rub-
bing alcohol, skin and hair products, and antifreeze. It is
ingested occasionally as a substitute for ethanol. Up to 80%
of the volume ingested is absorbed from the GI tract within
30 minutes. Half the isopropyl alcohol is excreted
unchanged by the kidney, with the remainder metabolized
in the liver to acetone. Both isopropyl alcohol and acetone
are CNS depressants. Isopropyl alcohol ingestion is usually
relatively benign, with patients surviving after ingestions of
up to 1 L. Some patients develop serious toxicity with doses
as low as 2–4 mL/kg. Although uncommon, dermal exposure
can cause toxicity.
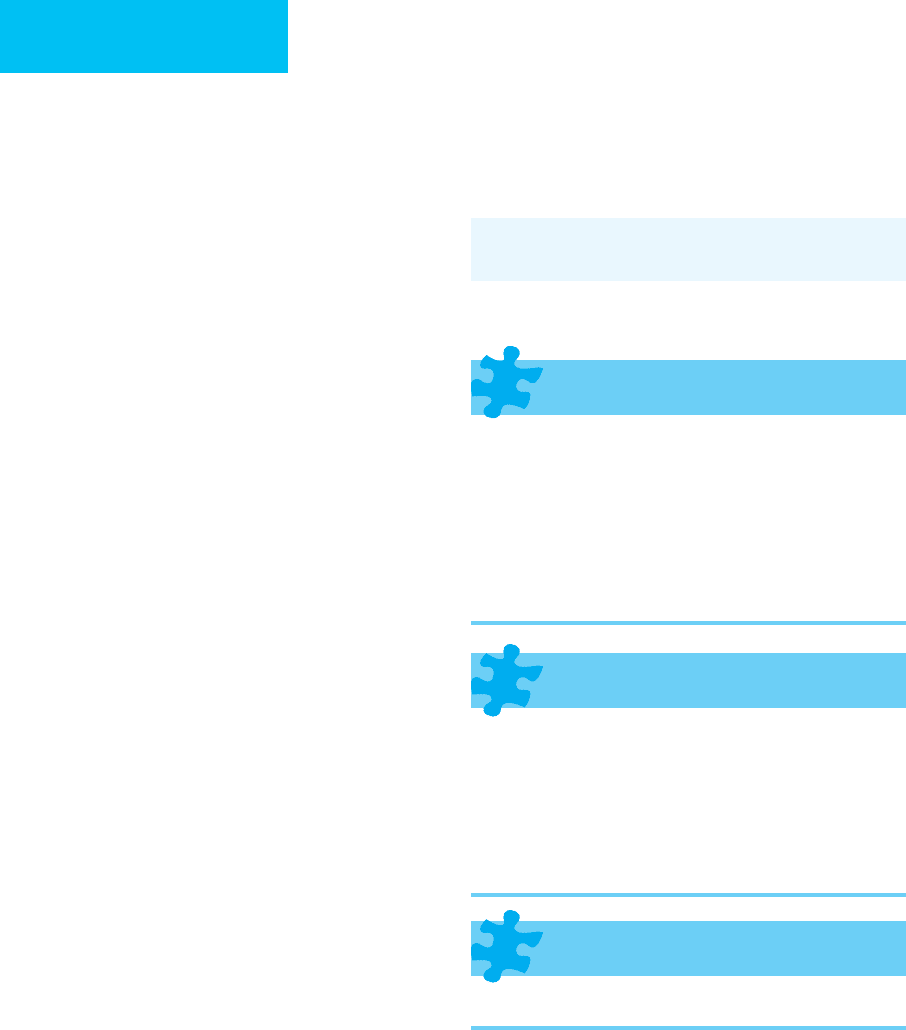
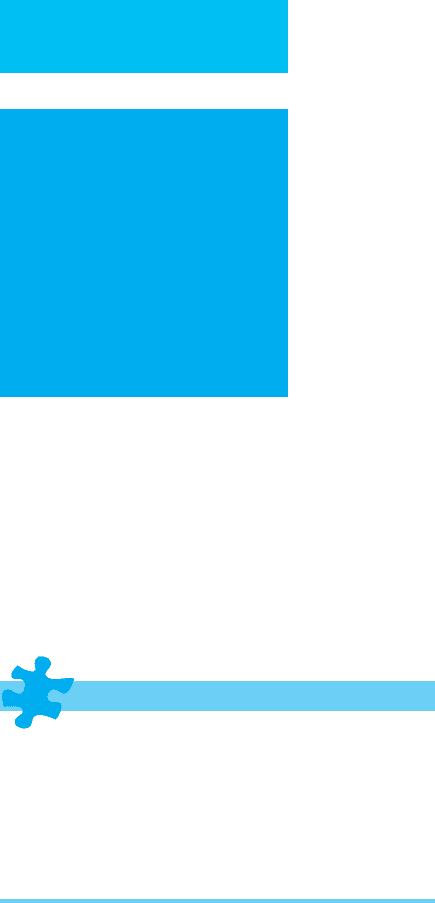
Loading Dose
Infusion Rate During
Dialysis
Infusion Rate After
Dialysis
Total Over 36 Hours
Amount of ethanol Chronic drinker
Nondrinker
42 g
42 g
18.0 g/h
11.8 g/h
10.8 g/h
4.6 g/h
474 g
251 g
Volume of IV 10%
ethanol
Chronic drinker
Nondrinker
530 mL
530 mL
228 mL/h
149 mL/h
137 mL/h
58 mL/h
6010 mL
3010 mL
Volume of oral 43%
ethanol
Chronic drinker
Nondrinker
125 mL
125 mL
54 mL/h
35 mL/h
32 mL/h
14 mL/h
1410 mL
749 mL
Volume of oral 90%
ethanol
Chronic drinker
Nondrinker
60 mL
60 mL
26 mL/h
17 mL/h
15 mL/h
7 mL/h
666 mL
359 mL
∗
Calculated to achieve and maintain blood ethanol concentration of 100 mg/dL, assuming ethanol dialysance of 120 mL/min and a 6-hour
dialysis period.
From McCoy HG et al: Severe methanol poisoning: An application of a pharmacokinetic model for ethanol therapy and hemodialysis. Am J Med
1979;67:806.
Table 36–14. Ethanol doses
∗
for treatment of methanol poisoning in a 70-kg adult.
CHAPTER 36
780
Clinical Features
A. Symptoms and Signs—GI and CNS effects predomi-
nate. Patients often complain of headache, dizziness, confu-
sion, intoxication, and poor coordination. Abdominal pain,
nausea, and vomiting are also common. Because isopropyl
alcohol is a gastric irritant, it may cause gastritis, which can
result in hematemesis. Massive upper GI bleeding from hem-
orrhagic gastritis is a rare but potentially fatal complication
of this ingestion.
Examination of these patients is usually normal except
for evidence of intoxication. Mild sinus tachycardia may be
seen. Hypotension can occur following severe ingestions.
Patients may have miosis, nystagmus, and decreased deep
tendon reflexes.
B. Laboratory Findings—Serum ketosis without acidosis is
the hallmark of isopropyl alcohol ingestion. The metabolism
of isopropyl alcohol produces acetone, which is a ketone
without acidic properties. Since isopropyl alcohol increases
serum osmolality, an osmolal gap also may be present. For
every 1 mg/dL of isopropyl alcohol in the blood, there is a
rise in serum osmolality of 0.18 mOsm/kg. Hypoglycemia is
frequently present.
Differential Diagnosis
Patients who appear intoxicated may have ingested ethanol,
methanol, ethylene glycol, or isopropanol. All these alcohols
can cause an elevated osmolal gap, but ethylene glycol and
methanol also cause a metabolic acidosis not observed with
isopropyl alcohol ingestions. Other causes of metabolic
abnormalities such as hyperglycemia, hyperosmolar states,
infections (eg, sepsis and meningitis), and head trauma also
should be considered.
Treatment
A. General Measures—Intravenous fluid resuscitation, oxy-
gen administration, and hemodynamic monitoring should be
initiated. If the patient presents more than 30 minutes after
ingestion, gastric decontamination is not effective. Activated
charcoal does not bind alcohols well and should only be given
if coingestion of another substance is suspected.
Patients with hematemesis should have blood sent for
typing in case bleeding becomes clinically significant and the
patient requires transfusion. Hypotension should be man-
aged with crystalloid infusion; if necessary, vasopressors may
be added.
B. Glucose Supplementation—Since hypoglycemia is
common with significant isopropyl alcohol ingestion, fre-
quent evaluation of the blood glucose with administration of
supplemental intravenous glucose as needed is mandatory.
Hourly rapid glucose determinations should be followed
with more frequent monitoring if patients have symptoms
typical of hypoglycemia.
C. Dialysis—Dialysis is rarely necessary following isopropyl
alcohol ingestion. The only indication for hemodialysis is in
the patient who remains hypotensive despite crystalloid and
vasopressor administration.
Zaman F, Pervez A, Abreo K: Isopropyl alcohol intoxication: A
diagnostic challenge. Am J Kidney Dis 2002;40:E12. [PMID:
12200829]
Mushroom Poisoning
ESSENTIALS OF DIAGNOSIS:
CYCLOPEPTIDES
Early:
Colicky abdominal pain.
Watery diarrhea, nausea, vomiting.
Late:
Right upper quadrant pain.
Hepatomegaly, asterixis, jaundice, encephalopathy,
liver failure.
ESSENTIALS OF DIAGNOSIS:
GYROMITRIN
Early:
Dizziness, bloating, nausea, vomiting.
Headache.
Late:
Hepatic failure.
Seizures and coma.
ESSENTIALS OF DIAGNOSIS:
OTHERS
Findings related to specific ingestion.
General Considerations
Severe mushroom poisoning is rare in the United States, with
only 200–350 cases and 50 deaths reported each year.
Children account for half of these ingestions, which occur
most commonly in the spring, summer, and fall. Of the 500
species of mushrooms in the United States, 100 are toxic, and
only 10 are potentially fatal when ingested. The toxicity of
any particular mushroom is variable and depends on the cli-
mate, the amount of rainfall, and the maturity of the plant.
POISONINGS & INGESTIONS
781
Toxic mushrooms are divided into eight categories
grouped by the effects of the toxin and the time to manifes-
tation of effects. Table 36–15 summarizes these categories.
Half the reported mushroom ingestions and 95% of the fatal
cases result from the cyclopeptide group. Mushrooms har-
boring this toxin are found chiefly along the northwest
Pacific Coast region of North America, including California.
Ingestions occur most commonly in the summer and fall.
Toxicity is due to GI irritation and hepatic failure. Mortality
rates are as high as 50%, with death often owing to hepatore-
nal syndrome, which occurs 6–16 days after ingestion.
The remainder of the fatal ingestions result from con-
sumption of mushrooms in the gyromitrin group, also known
as false morels. Found in California woodlands, these poison-
ings occur most commonly in the early spring. Gyromitrins
are hydrolyzed in the liver to monomethylhydrazine, which
causes toxicity by inactivating pyridoxal phosphate.
Both cyclopeptide and gyromitrin toxins have delayed
symptom onset from time of ingestion; this characteristic
serves as an important clue that the patient may have
ingested a potentially lethal mushroom.
Mushrooms that contain toxins that affect the autonomic
nervous system are found virtually everywhere, often growing
alongside other nontoxic mushrooms. Two types of auto-
nomic syndromes occur in this category. Ingestion of mush-
rooms that contain significant amounts of muscarine
produces stimulation of postganglionic parasympathetic mus-
carinic effectors, causing a cholinergic toxidrome. Ingestion of
the coprine group of mushrooms (“inky caps”) is usually non-
toxic, and these mushrooms often are considered a delicacy.
Coingestion of ethanol with these mushrooms, however, leads
to a disulfiram-like reaction probably owing to blocking of
aldehyde dehydrogenase in the liver. If the ethanol is ingested
before or concurrently with the mushrooms, this toxicity does
not occur. Instead, sensitivity to ethanol begins 2 hours after
ingestion of the mushrooms and lasts up to 5 days.
Ingestion of mushrooms that affect the CNS often consti-
tutes a form of recreational drug use. Inadvertent consumption
Poison Symptoms Onset Examples
Rapid-Onset Toxicity
Poisons affecting the autonomic nervous system
Muscarine Cholinergic toxidrome 1–2 hours
Clitocybe
species
Coprine “Nature’s disulfiram”: flushing, nausea,
vomiting, diaphoresis
30 minutes after ethanol
Coprinus
species
Poisons affecting the central nervous system
Ibotenic acid, muscimol Dizziness, incoordination, myotonic
jerks, spasms, hallucinations
30 minutes to 2 hours
Amanita muscaria
Psilocybin, psilocin Euphoria or dysphoria, lethargy, deep
sleep, hallucinations (visual)
30 minutes to 1 hour
Psilocybe
species
Poisons affecting the gastrointestinal system
Multiple Nausea, vomiting, diarrhea, abdominal
pain
30 minutes to 2 hours ”Little brown mushrooms,”
widespread
Delayed-Onset Toxicity
Poisons causing cellular destruction
Cyclopeptides Abdominal pain, nausea, vomiting, diar-
rhea, delayed jaundice, coma
6–24 hours
Amanita phalloides, Galerina marginata
Gyromitrin, monomethylhydrazine Nausea, vomiting, diarrhea, incoordina-
tion, seizures, coma
6–12 hours
Gyromitra
species
Poisons affecting the renal system
Orelline, orellanine Gastritis, delayed renal failure 3–14 days
Cortinarius
species (especially Japan,
Europe)
Table 36–15. Classification of mushroom toxicity.

CHAPTER 36
782
of mushrooms in this category also occurs because they are
often found along the Pacific Coast in the spring, summer,
and fall. Although these mushrooms rarely produce serious
toxicity in adults, children may develop lethal complications.
Clinical Features
A. History—Mushroom toxicity presents with a wide array
of symptoms depending on the type of mushroom ingested.
Patients who present with mushroom toxicity may or may
not relate a history of ingestion. They may not connect their
consumption of the mushrooms with their illness, or if they
are using mushrooms for recreational purposes, they may be
hesitant to give medical personnel this information. In clini-
cal settings suggestive of mushroom ingestion, clinicians
should ask specifically about this possibility.
One of the most important historical pieces of information
that should be sought from the patient is the time from inges-
tion to the onset of symptoms; mushrooms that are potentially
lethal (those containing cyclopeptides and gyromitrins) have a
time delay of at least 4–6 hours from ingestion to symptoms, a
very important clinical clue in determining the potential for
serious toxicity. Any patient who presents with symptoms that
occur more than 6 hours after ingesting a potentially toxic
mushroom should be considered to have a possibly fatal inges-
tion. It should be kept in mind, however, that patients may
coingest several different types of toxic mushrooms, and a
rapid onset of symptoms does not exclude concurrent inges-
tion of a potentially lethal one.
B. Symptoms and Signs—Cyclopeptides, the most com-
monly lethal mushroom toxin, cause a three-phase illness.
The GI phase begins abruptly 6–12 hours after ingestion and
is characterized by severe colicky abdominal pain, profuse
watery diarrhea, nausea, and vomiting. These symptoms last
up to 24 hours and then resolve. The patient feels well during
a latent phase of 3–5 days, but hepatic toxicity is occurring. At
the end of this phase, the patient presents with findings typi-
cal of liver failure, including right upper quadrant pain,
hepatomegaly, asterixis, jaundice, or frank encephalopathy.
Gyromitrin-containing mushrooms (false morels) cause
gastritis with an onset 6–12 hours after ingestion. The patient
complains of dizziness, bloating, nausea, vomiting, and
severe headache. Hepatic failure may occur in severe cases,
usually 3–4 days after ingestion. Seizures and coma are also
described.
The Cortinarius species of mushrooms, found most com-
monly in Japan and Europe, contains orelline, which results in
a delayed presentation 24–36 hours after ingestion with a self-
limited gastritis-like illness. Three to fourteen days after inges-
tion, the patient presents with night sweats, anorexia, headache,
chills, and a severe burning thirst. Oliguria and flank pain also
may be present. These patients may develop renal failure.
The remainder of the toxic mushrooms cause symptoms
soon after ingestion. Toxins that affect the autonomic nervous
system include muscarine and coprine. Fifteen minutes to 1 hour
after ingestion of muscarine-containing mushrooms, the
patients will complain of headache, nausea, vomiting, and
abdominal pain and may develop cholinergic symptoms of
salivation, lacrimation, urination, defecation, and diaphoresis.
In severe cases, bronchospasm, bronchorrhea, bradycardia, and
shock may occur. In most cases, however, symptoms are usually
mild and resolve in 2–6 hours. Coprine-containing mush-
rooms alone do not cause toxicity; however, when ethanol is
ingested 2 hours to 5 days after ingestion of these mushrooms,
the patient may develop a disulfiram-like syndrome. Fifteen to
twenty minutes after drinking ethanol, the patient complains of
a severe headache, facial flushing, paresthesias, lightheadedness,
orthostatic hypotension, vomiting, palpitations, and tachycar-
dia. Although the patient feels ill, these symptoms rarely cause
significant compromise and abate after several hours.
Mushrooms that affect the CNS contain one of several
toxins, including ibotenic acid, muscimol, and psilocybin.
Symptoms usually begin 30 minutes to 4 hours after inges-
tion. Patients complain of drowsiness, incoordination, wax-
ing and waning mental status, and formed or unformed
visual hallucinations. Psilocybins are renowned for causing
alterations in perceptions of shapes, sounds, and colors.
Ibotenic acid and muscimol may cause anticholinergic
effects that are rarely severe except in children; these effects
are seizures, coma, tachycardia, and hypertension. Most of
these patients resolve their symptoms within several hours
without sequelae.
The final group of toxic mushrooms are those known as
“little brown mushrooms” and cause primarily a self-limited
GI illness characterized by rapid onset of malaise, nausea,
vomiting, and diarrhea within 1–3 hours of ingestion. These
symptoms usually resolve within 24–48 hours.
C. Laboratory Findings—Laboratory results are related
specifically to the type of ingestion.
1. Cyclopeptides—Laboratory evaluation may reveal hypo-
glycemia, elevated aminotransferases, metabolic acidosis,
and coagulopathy.
2. Gyromitirin—Laboratory evaluation may show elevated
liver function tests and coagulopathy; these patients also may
have methemoglobinemia.
3. Orelline—Laboratory evaluation may reveal red blood
cell casts, elevated BUN, serum creatinine, proteinuria, and
hematuria.
Differential Diagnosis
Owing to the wide range of symptoms caused by toxic mush-
rooms, the differential diagnosis depends on the type of mush-
room ingested. Most of the toxic mushrooms cause a GI
syndrome that may be confused with gastroenteritis, infectious
diarrhea, or other GI diseases. Liver failure (associated with the
cyclopeptides and gyromitrins) can be caused by other toxins,
particularly acetaminophen, as well as entities such shock liver,
severe hepatitis, and alcoholism. CNS effects of mushroom
toxicity also can be observed in patients who ingest anticholin-
ergics, LSD, peyote, and other hallucinogens. The cholinergic
POISONINGS & INGESTIONS
783
syndrome that occurs with muscarine-containing mushrooms
is also found in organophosphate poisoning.
Treatment
Treatment of patients with toxic mushroom ingestions
depends on the type of mushroom ingested and the symp-
toms. If there is any possibility that the patient may have
ingested a potentially lethal mushroom—even if it cannot be
confirmed—the patient should be treated aggressively.
A. Decontamination—In general, all patients who may
have ingested potentially lethal mushrooms should have
gastric emptying if they present as long as 4 hours after
ingestion. Repeated-dose activated charcoal should be given
to these patients and those presenting after this 4-hour time
period.
B. Antidotes—Although several potential antidotes have
been used to treat patients who may have ingested
cyclopeptide-containing mushrooms, none have been
proved to be effective. These patients need supportive care
and ultimately may need liver transplantation if liver failure
becomes severe.
C. Renal Dialysis—Cortinarius mushroom toxicity that
results in renal failure should be managed with dialysis as
needed. These patients may need dialysis for weeks to
months but usually will recover renal function eventually.
D. Other Measures—If significant methemoglobinemia
(metHb >30% or symptomatic hypoxia or ischemia and a
metHb <30%) develops in a patient who ingests gyromitrin-
containing mushrooms, one should give methylene blue,
0.1–0.2 mL/kg of a 1% solution intravenously over 5 minutes.
Such patients who develop intractable seizures refractory to
standard therapy may respond to pyridoxine, 25 mg/kg
intravenously given over 25–30 minutes.
Patients with cholinergic symptoms from muscarine-
containing mushrooms usually need observation only.
However, if they develop bronchospasm, bronchorrhea,
bradycardia, or shock, they should be treated with atropine,
0.5–1 mg intravenously, repeated as needed for recurrence of
symptoms. This dose should be repeated every 10–20 minutes
until the symptoms resolve.
Patients who ingest hallucinogenic mushrooms do not
need specific medical interventions. They should be placed
in a dark, quiet room and observed until the effects subside.
If patients manifest significant anticholinergic signs, they
should be monitored closely and receive specific treatment
for anticholinergic toxicity if indicated.
Current Controversies and Unresolved Issues
Several antidotes have been used to treat cyclopeptide toxic-
ity. Thioctic acid, a coenzyme in the Krebs cycle, has been
used in a dose of 50–150 mg intravenously every 6 hours with
variable results. Its only major side effect is hypoglycemia,
which requires close monitoring. Since this poisoning can be
life-threatening, use of thioctic acid should be considered
with the understanding that its effects have not been validated.
Other treatments, including high-dose penicillin, silibinin,
high-dose steroids, hyperbaric oxygenation, and pyridoxine,
have been used with inconclusive results.
Alves A et al: Mushroom poisoning with Amanita phalloides: A
report of four cases. Eur J Intern Med 2001;12:64–6. [PMID:
11173014]
Bedry R et al: Wild-mushroom intoxication as a cause of rhab-
domyolysis. N Engl J Med 2001;345:798–802. [PMID: 11556299]
Berger KJ, Guss DA: Mycotoxins revisited, part I. J Emerg Med
2005;28:53–62. [PMID: 15657006]
Berger KJ, Guss DA: Mycotoxins revisited, part II. J Emerg Med
2005;28:175–83. [PMID: 15707814]
Broussard CN et al: Mushroom poisoning: From diarrhea to liver
transplantation. Am J Gastroenterol 2001;96:3195–8. [PMID:
11721773]
Danel VC, Saviuc PF, Garon D: Main features of Cortinarius spp
poisoning: A literature review. Toxicon 2001;39:1053–60.
[PMID: 11223095]
Escudie L et al: Amanita phalloides poisoning: Reassessment of
prognostic factors and indications for emergency liver trans-
plantation. J Hepatol 2007;46:466–73. [PMID: 17188393]
Ganzert M, Felgenhauer N, Zilker T: Indication of liver transplan-
tation following amatoxin intoxication. J Hepatol 2005;42:
202–9. [PMID: 15664245]
Kaneko H et al: Amatoxin poisoning from ingestion of Japanese
Galerina mushrooms. J Toxicol Clin Toxicol 2001;39:413–6.
[PMID: 11527238]
Nordt SP, Manoguerra A, Clark RF: 5-Year analysis of mushroom
exposures in California. West J Med 2000;173:314–7. [PMID:
11069864]
Organophosphates
ESSENTIALS OF DIAGNOSIS
Muscarinic effects:
Bronchospasm, bronchorrhea.
Salivation, lacrimation, urination, defecation, gastric
emesis (SLUDGE) syndrome.
Blurred vision.
Nicotinic effects:
Muscle fasciculations, weakness, paralysis.
Ataxia.
CNS effects:
Headache.
Slurred speech.
Confusion.
Seizures, coma.
Depression of the respiratory center.

CHAPTER 36
784
General Considerations
Organophosphates are found most commonly in herbicides
and insecticides and are in the form of organophosphates or
carbamates. They also can be used in chemical warfare or ter-
rorism events. They act by causing irreversible inactivation of
acetylcholinesterase, resulting in an accumulation of acetyl-
choline at cholinergic receptors. The toxicity results from
excessive muscarinic, nicotinic, and CNS effects of the excess
acetylcholine. Toxicity may develop after oral or dermal
exposure.
Patients with organophosphate toxicity may be exposed
accidentally at work, often by dermal exposure. Alternatively,
patients may accidentally or intentionally ingest these com-
pounds. The diagnosis often is made clinically because there
are no laboratory tests immediately available to detect these
compounds.
Clinical Features
A. Symptoms and Signs—Patients present with a myriad of
symptoms. Peripheral muscarinic effects include bron-
chospasm, bronchorrhea, nausea, vomiting, diarrhea, miosis,
blurred vision, urinary incontinence, salivation, diaphoresis,
and lacrimation. The combination of salivation, lacrimation,
urination, defecation, and gastric emesis is known as the
SLUDGE syndrome and is very suggestive of organophos-
phate poisoning. Nicotinic effects consist primarily of skele-
tal muscle symptoms, particularly muscle fasciculations,
weakness, ataxia, and frank paralysis. Blood pressure and
heart rate effects vary depending on whether muscarinic or
nicotinic effects predominate. Patients may be tachycardic or
bradycardic and hypertensive or hypotensive. Elevated CNS
acetylcholine concentrations cause headache, slurred speech,
confusion, seizures, and coma, as well as depression of the
respiratory centers. Respiratory failure is the usual cause of
death, often owing to a combination of central respiratory
depression, respiratory muscle weakness, bronchospasm, and
increased bronchial secretions.
B. Laboratory Findings—There are no laboratory tests
immediately available that characterize this ingestion, and
the diagnosis is often made on the basis of a potential for
exposure to the toxin combined with a suggestive clinical
presentation. Laboratory testing for cholinesterase activity
will show decreased activity of this enzyme and often con-
firms the diagnosis. However, this test is usually not per-
formed on an emergent basis, and several days may pass
before results become available. Definitive diagnosis is made
by appropriate response to treatment (eg, atropine or prali-
doxime) and decreased cholinesterase activity in the blood.
Differential Diagnosis
The combination of salivation, lacrimation, urination, and
defecation strongly suggests organophosphate poisoning.
This diagnosis is of particular importance if the patient is
diaphoretic and has bronchospasm, with excessive pul-
monary secretions and muscle weakness. Patients with myas-
thenia gravis in cholinergic crisis present with a similar
clinical picture.
Treatment
A. Decontamination—Medical personnel should wear
gowns and gloves when treating patients with organophos-
phate poisoning because they may become contaminated
and symptomatic from either the patient’s clothing or secre-
tions and body fluids. Patients with dermal exposure need
copious irrigation in a protected area. Gastric lavage should
be attempted if the ingestion was less than 1 hour before
presentation and the patient is not already vomiting. After
lavage, activated charcoal should be given through the NG
tube before it is removed. Intubation and ventilatory support
should be considered early.
B. Atropine—Atropine antagonizes the peripheral mus-
carinic effects of the excess acetylcholine and may moderate
some of the CNS effects, but it does nothing to alter the
skeletal muscle nicotinic effects, nor does it restore acetyl-
cholinesterase to an active state. Indications for the use of
atropine are suspected organophosphate poisoning in a
patient who has muscarinic symptoms and signs. The drug
can be used both diagnostically and therapeutically.
Diagnostically, a dose of 1 mg (or 0.015 mg/kg) intra-
venously should dilate the pupils and increase the heart rate
within 10 minutes. If there is no response to this dose,
cholinergic toxicity is suggested. At that point, 2–4 mg (or
0.02–0.05 mg/kg) of atropine should be given intravenously
every 10–15 minutes, with the endpoint being a drying of
secretions, particularly bronchial secretions. Pupillary dila-
tion and tachycardia should not be used as endpoints
because these effects may be seen before drying of bronchial
secretions is achieved. Massive doses of atropine may be
needed to achieve full effect.
C. Pralidoxime—Pralidoxime reverses phosphorylation of
acetylcholinesterase and therefore restores its activity. This
drug will reverse the nicotinic effects of muscle weakness and
also reverses some of the CNS effects of the poison. Because
pralidoxime is more effective in reversing the nicotinic than
the muscarinic effects, it should be used in conjunction with
atropine. Indications for pralidoxime include the nicotinic
effects of organophosphate poisoning (eg, fasciculations and
weakness) or CNS effects (eg, altered mental status). Blood
should be drawn and sent for cholinesterase activity before
the drug is administered. The dose is 1–2 g (or 25–50 mg/kg)
intravenously over 5–15 minutes. End-organ effects are seen
in 15–45 minutes and are manifested by increased muscle
strength. Dosing can be repeated in 1–2 hours if weakness
and fasciculations persist. Pralidoxime can be repeated every
4–12 hours as needed. Its side effects (eg, nausea, headache,
and tachycardia) are rare and usually result from too rapid
injection.

POISONINGS & INGESTIONS
785
In moderate to severe poisoning, atropine and prali-
doxime should be continued for at least 24 hours; in severe
poisonings, therapy may need to be continued for days to
weeks. Treatment with antidotes can be discontinued when
clinical response indicates that they are no longer needed—
that is, when there is an absence of clinical improvement
with therapy and a lack of recurrence of signs and symptoms
of toxicity when the antidotes are withheld.
Calvert GM et al: Acute occupational pesticide-related illness in
the US, 1998–1999: Surveillance findings from the SENSOR-
pesticides program. Am J Ind Med 2004;45:14–23. [PMID:
14691965]
Eddleston M, Phillips MR: Self-poisoning with pesticides. Br Med J
2004;328:42–4. [PMID: 14703547]
Hsieh BH et al: Acetylcholinesterase inhibition and the
extrapyramidal syndrome: A review of the neurotoxicity of
organophosphate. Neurotoxicology 2001;22:423–7. [PMID:
11577800]
Lee P, Tai DY: Clinical features of patients with acute organophos-
phate poisoning requiring intensive care. Intensive Care Med
2001;27:694–9. [PMID: 11398695]
Okumura T et al: The Tokyo subway sarin attack: Lessons learned.
Toxicol Appl Pharmacol 2005;207:471–6. [PMID: 15979676]
Peter JV, Moran JL, Graham PL: Advances in the management of
organophosphate poisoning. Expert Opin Pharmacother
2007;8:1451–64. [PMID: 17661728]
Worek F et al: Diagnostic aspects of organophosphate poisoning.
Toxicology 2005;214:182–9. [PMID: 16051411]
786
00
Patients with injuries owing to environmental hazards and
toxic exposure may require admission to an ICU for resuscita-
tion, stabilization, and definitive treatment. This chapter
reviews the essentials of diagnosis and treatment of heat
stroke, hypothermia, frostbite, near-drowning, envenomation,
electric shock (and lightning injury), and radiation injury.
Heat Stroke
ESSENTIALS OF DIAGNOSIS
Core body temperature approaching 41°C.
Confusion, stupor, coma.
Hypotension and tachycardia.
Muscle stiffness.
Hot, dry skin.
Elevated hematocrit and hyperkalemia.
General Considerations
The three major manifestations of heat illness are heat
cramps, heat exhaustion, and heat stroke. The syndromes
usually occur in warm, humid environments after strenu-
ous physical exertion. However, elderly persons with med-
ical problems or infants may be affected under less severe
conditions.
Heat cramps and heat exhaustion result from the deple-
tion of fluid and electrolytes. Complete recovery occurs after
removal of the patient from the stressful environment and
the institution of replacement therapy. Heat stroke results
from the failure of thermoregulatory mechanisms. It is a
medical emergency, and prompt reduction of body tempera-
ture is necessary to prevent morbidity and mortality.
To maintain a constant body temperature, heat loss must
equal heat production. Cutaneous vasodilation allows for heat
loss through the processes of radiation, conduction, and con-
vection. Evaporative heat loss occurs from sweating and to a
lesser extent from the airway. When the environmental tem-
perature exceeds body temperature, the only effective means
of heat loss is through sweating. Although significant amounts
of heat can be dissipated through this mechanism, sweating
becomes less efficient under conditions of high humidity.
Heat stress syndromes develop as a result of processes
that attempt to maintain normal body temperature. Heat
stroke results from failure of thermoregulatory mechanisms.
Heat cramps and heat exhaustion commonly occur after
excessive sweating in a hot environment. Heat cramps are
painful spasms of voluntary muscles that occur as a result of
electrolyte depletion. Depletion of fluid and electrolytes con-
tributes to the weakness and mental status changes associ-
ated with heat exhaustion.
Heat stroke occurs when the core body temperature
exceeds 41°C. Heat stroke may occur in otherwise healthy
people after extreme exertion in a hot climate, particularly in
unacclimatized individuals. In this setting, heat production
exceeds heat loss, resulting in failure of thermoregulatory
mechanisms. Once these mechanisms have failed, body tem-
perature may rise quite rapidly. Signs and symptoms can
develop suddenly. A rise in core body temperature above
42°C is associated with protein denaturation and cellular
lipid membrane dissolution. Hypovolemia owing to dehy-
dration may exacerbate the direct organ injury.
Nonexertional heat stroke is often called classic heat stroke
and commonly affects elderly or debilitated individuals with
impaired thermoregulation owing to disease or medications.
The volume status of a patient with nonexertional heat
stroke is unpredictable. In both exertional and nonexertional
heat stroke, myocardial dysfunction may occur as a result of
direct damage to the myocytes.
The neurologic abnormalities associated with heat
stroke range from confusion and stupor to coma and seizure
disorders. Cerebral and cerebellar neurons may be destroyed
by the increased temperature. Intracerebral hemorrhage and
37
Care of Patients with
Environmental Injuries
James R. Macho, MD
William P. Schecter, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
