Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CARE OF PATIENTS WITH ENVIRONMENTAL INJURIES
797
General Considerations
Spider and scorpion bites are particularly common in the
western United States. Only the female black widow spider
(Latrodectus mactans) is dangerous. Its venom contains a
potent neurotoxin that induces neurotransmitter release fol-
lowing interaction with a specific cell surface receptor. This
action affects mainly the neuromuscular junction and results
in unrestrained muscle contraction and severe cramping.
The local reaction at the site of envenomation is usually mild.
Venom from the brown recluse spider (Loxosceles reclusa)
contains sphingomyelinase D. It is primarily cytotoxic and
causes local tissue destruction. Hemolysis is the principal
systemic effect, and it is usually minor.
Most scorpion stings are harmless and produce only local
reactions. However, venom from Centruroides exilicauda con-
tains a neurotoxin that may cause severe systemic reactions.
Clinical Features
A. Symptoms and Signs—Initially, a black widow spider
bite is painless. Symptoms begin within 10–60 minutes and
include severe pain and muscle spasms of the abdomen and
trunk. Headache, nausea, vomiting, and hyperactive deep
tendon reflexes may be present. Spasms give way to agoniz-
ing pain. Rigidity of the abdominal wall may be confused
with an intraabdominal catastrophe. Hypertension with or
without seizures develops uncommonly. Symptoms are
maximum at 2–3 hours after the bite and may persist for up
to 24 hours.
Brown recluse spider bites produce pain after 1–4 hours.
Initially, an erythematous area with a central pustule or hem-
orrhagic area appears. A bull’s-eye appearance of the lesion
may be noted because of an ischemic halo surrounded by
extravasated blood. Over several days, an ulcer may form,
which, if extensive, requires excision and skin grafting.
Systemic reactions are infrequent but may occur 1–2 days
after the bite and include massive hemolysis, hemoglobin-
uria, jaundice, renal failure, pulmonary edema, and dissemi-
nated intravascular coagulation.
Scorpion stings are extremely painful but often exhibit no
erythema or swelling. Light palpation of the area causes
extreme pain. Generalized reactions are not common but
may develop within 60 minutes: restlessness, jerking, nystag-
mus, hypertension, diplopia, confusion, and rarely seizures.
Death is uncommon.
Differential Diagnosis
The signs and symptoms of black widow spider envenomation
can be easily confused with other common conditions, partic-
ularly those cases with minimal bite-related symptoms. In
some cases, the abdominal pain may mimic an acute
abdomen. Black widow spider envenomation should be con-
sidered in patients presenting with the acute onset of severe
pain and muscle cramps, particularly if the history is consis-
tent with spider bite.
Brown recluse spider bites are occasionally confused with
those of other insects. It should be remembered that spiders
usually bite only once, whereas other insects produce multi-
ple bites.
Treatment
A. Black Widow Spider Bites—The most effective treat-
ment options include specific antivenin alone or with a com-
bination of intravenous opioids and muscle relaxants.
Although calcium gluconate administration has been recom-
mended, it has not been shown to be effective. Intravenous
morphine and benzodiazepines are helpful in achieving relief
of symptoms. Antivenin should be considered in moderate to
severe cases but should be used with caution because it has
been associated with fatal reactions. Advanced life support
measures may be required for patients who develop cardio-
vascular collapse or respiratory failure.
B. Brown Recluse Spider Bites—Most patients can be
treated with supportive measures. Ice may be beneficial.
Exercise of the limb or application of heat will potentiate the
actions of the venom. Patients requiring admission to the
ICU are usually older, with systemic symptoms. Dapsone,
50–100 mg orally twice daily for 10 days, has been used in
patients who do not have glucose-6-phosphate dehydroge-
nase deficiency. Some authorities use oral erythromycin,
250 mg four times daily for 10 days, to control skin infection.
C. Scorpion Stings—Children and older adults must be
admitted to the ICU for observation. The affected part
should be immobilized and ice applied. A tourniquet must
not be used. Respiratory depression may result from the use
of tranquilizers. Opioid analgesics are particularly dangerous
because they seem to potentiate the toxicity of the venom.
Seizures, when present, usually can be controlled with intra-
venous diazepam or phenobarbital. Hypertension may
require the use of sympatholytic agents.
3. Marine Life Envenomations
ESSENTIALS OF DIAGNOSIS
Pain at the site of envenomation.
Systemic symptoms subsequently.
Multiple wounds may be present.
General Considerations
Marine life envenomations are caused most commonly by
stingrays, jellyfish (Portuguese man-of-wars), scorpion
fish, and sea urchins. Although many victims can be
treated in the emergency department and released, critical
care may be required for hemodynamic and respiratory
complications.
CHAPTER 37
798
Clinical Features
A. Stingray—Multiple sites may be present, with pain and
swelling occurring immediately. Local hemorrhage also may
be present. Systemic symptoms, when present, include nau-
sea, vomiting, weakness, vertigo, tachycardia, and muscle
cramps. Syncope, paralysis, hypotension, and tachycardia
may occur with extensive envenomations.
B. Scorpion Fish—Central radiation of pain from the
wound may cause extreme discomfort requiring ICU admis-
sion for control. Systemic symptoms are manifest within the
first few hours after envenomation and include vomiting,
weakness, diarrhea, paresthesias, seizures, fever, hyperten-
sion, cardiac arrhythmias, and respiratory failure.
C. Sea Urchins—Sea urchin venoms contain several toxins,
including cholinergic compounds and neurotoxins. Multiple
spines usually are present in the skin and indicate the nature
of the contact. Systemic reactions include nausea and vomit-
ing, intense pain, paralysis, aphonia, and respiratory distress.
Treatment
A. Stingray—Wounds can be treated with local measures,
including warm soaks and lidocaine. Ice should not be applied.
Operative debridement may be required. Supportive therapy is
usually all that is required. Infection prophylaxis should be
instituted with trimethoprim-sulfamethoxazole or tetracycline.
B. Scorpion Fish—Care is similar to that outlined for
stingray contact. Infection prophylaxis should be instituted
in a similar fashion. Seizures can be treated with phenobar-
bital, phenytoin, or diazepam.
C. Sea Urchins—Although pain can subside within a few
hours, paralysis may last for 6–8 hours and require intuba-
tion and mechanical ventilation until the patient has
regained sufficient strength.
Bogdan GM et al: Recurrent coagulopathy after antivenom treat-
ment of crotalid snakebite. South Med J 2000;93:562–6. [PMID:
10881769]
Dart RC et al: A randomized multicenter trial of crotalinae polyva-
lent immune Fab (ovine) antivenom for the treatment for cro-
taline snakebite in the United States. Arch Intern Med
2001;161:2030–6. [PMID: 11525706]
Dart RC et al: Efficacy, safety, and use of snake antivenoms in the
United States. Ann Emerg Med 2001;37:181–8. [PMID:
11174237]
Forks TP: Brown recluse spider bites. J Am Board Fam Pract
2000;13:415–23. [PMID: 11117338]
Frundle TC: Management of spider bites. Air Med J 2004;23:224–6.
[PMID: 15224078]
Gold BS et al. North American snake envenomation: Diagnosis,
treatment and management. Emerg Med Clin North Am
2004;22:423–33. [PMID: 15163575]
Hall EL: Role of surgical intervention in the management of cro-
taline snake envenomation. Ann Emerg Med 2001;37:175–80.
[PMID: 11174236]
Jasper EH et al: Venomous snakebites in an urban area: what are
the possibilities? Wilderness Environ Med 2000;11:168–71.
[PMID: 11055562]
Majeski J: Necrotizing fasciitis developing from a brown recluse
spider bite. Am Surg 2001;67:188–90. [PMID: 11243548]
Moss ST et al: Association of rattlesnake bite location with severity
of clinical manifestations. Ann Emerg Med 1997;30:58–61.
[PMID: 9209227]
Offerman SR et al: Does the aggressive use of polyvalent antivenin
for rattlesnake bites result in serious acute side effects? West J
Med 2001;175:88–91. [PMID: 11483547]
Perkins RA et al. Poisoning, envenomation and trauma from
marine creatures. Am Fam Physician 2004;69:885–90. [PMID:
14989575]
Scharman EJ et al: Copperhead snakebites: Clinical severity of local
effects. Ann Emerg Med 2001;38:55–61. [PMID: 11423813]
Walter FG et al: Envenomations. Crit Care Clin 1999;15:353–86.
[PMID: 10331133]
Wendell RP: Brown recluse spiders: A review to help guide physi-
cians in non-endemic areas. South Med J 2003;96:486–90.
[PMID: 12911188]
Electric Shock & Lightning Injury
ESSENTIALS OF DIAGNOSIS
Momentary or prolonged unconsciousness.
Cardiac arrhythmias.
Muscular pain, fatigue, headache.
Rhabdomyolysis and renal failure.
General Considerations
Electrical injuries account for more than 500 fatalities each
year in the United States. One-fifth of these deaths are due to
lightning. The number of nonfatal injuries may be three or
four times this number. Patients who have sustained electri-
cal injury or a lightning strike exhibit a number of signs
depending on the energy of the current conducted. Most
household electrical injuries are produced by alternating
current (50–60 Hz) in the 110–220-volt range. Direct current
usually produces less severe injuries for the same amount of
voltage. Electricity can cause partial- or full-thickness burns
with injury to the deeper tissues of the body. In some cases,
the burn injury at the entry and exit points may correlate
directly with the extent of underlying muscle injury, but
extensive deep injuries may be present with only minimal
superficial findings. Myonecrosis and rhabdomyolysis are
frequently present with higher-energy exposures.
Rhabdomyolysis may lead to renal failure if not recognized
and treated promptly. Compartment syndrome can occur in
extremities with resulting circulatory compromise.
Ventricular fibrillation may be present if the current pathway
has included the heart.
CARE OF PATIENTS WITH ENVIRONMENTAL INJURIES
799
A potential difference of more than 440 V is considered
high voltage. At greater than 1000 V, severe tissue destruction
occurs as a result of electrical energy being converted to heat.
Electrocution may be accompanied by arc and flash burns
(see Chapter 35). Associated injuries are a result of falls
owing to tetany of the major muscles.
Lightning strikes impart huge amounts of energy to their
victims. Cardiac and respiratory failure are responsible for
immediate deaths. Those surviving the immediate period are at
risk for delayed neurologic, visual, and otologic as well as mus-
culoskeletal complications. Although neurologic sequelae pre-
viously were thought to be transient, recent investigations have
demonstrated permanent injury in one-half of the victims.
Clinical Features
A. Electric Shock—Shock from household current commonly
produces transient loss of consciousness, although this may be
prolonged. Patients frequently have regained normal function
by the time they arrive in the emergency room, at which time
they complain of headache, muscle cramps, and fatigue.
Nervous irritability and a sensation of anxiety are other com-
mon findings. Patients with prolonged unconsciousness
should undergo CT scanning to rule out an associated cerebral
injury from a fall or direct injury. Cardiac arrhythmias typi-
cally are tachyarrhythmias, with atrial and ventricular fibrilla-
tion being the most common. Difficulty in breathing with
varying degrees of respiratory paresis or complete paralysis
requires immediate attention. Damage to skeletal muscles may
produce a spurious rise in the CK-MB fraction, leading to the
erroneous diagnosis of myocardial infarction.
Burn wounds often accompany electrocution victims.
These injuries are of three types: (1) direct burn, (2) arc
injury, or (3) flame burn from an associated ignition source.
Burn wounds are more common with higher-voltage injuries.
All patients with burn wounds should receive tetanus prophy-
laxis. Patients with more severe burns should be considered
for transfer after stabilization to a specialized burn center.
Additional management is discussed in Chapter 35.
B. Lightning Strike—Patients who require critical care after a
lightning strike usually are admitted for complications or sim-
ply for cardiac monitoring. Lightning victims may present with
paraplegia or quadriplegia that resolves over several hours. This
may be accompanied by autonomic instability. In cases of pro-
longed paresis, imaging studies should be obtained to rule out
a spinal injury. Electrocardiographic changes include nonspe-
cific ST-T-segment changes that may be accompanied by eleva-
tion of cardiac enzymes. Initial hypertension usually resolves
spontaneously and does not require treatment.
Lightning victims may have a number of associated find-
ings related to blunt trauma sustained at the time of impact.
Rib and long bone fractures in the extremities are particu-
larly common. Burns may be present but are superficial in
most patients and often require only superficial wound care.
Unlike those who have sustained electrical injuries, patients
with lightning injuries rarely develop myoglobinuria.
Treatment: Electric Shock
Patients suffering from electrical injuries should be admitted
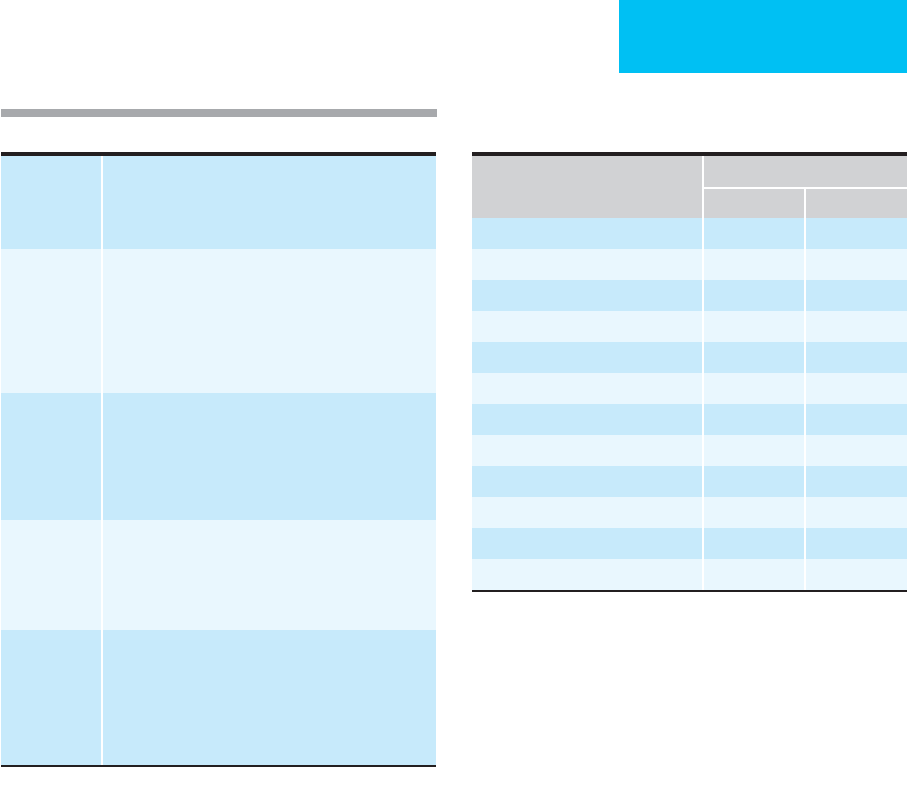
to the ICU when the conditions outlined in Table 37–1 are
present.
A. General Measures—Most electrocution patients admit-
ted to the ICU already will have had the airway secured (if
necessary) and large-bore intravenous catheters inserted for
resuscitation and fluid management. Adequate urine output
must be ensured to prevent renal failure from myoglobin-
uria. The goal is to maintain a urine output of 75–100 mL/h.
Mannitol may be give as a bolus (1 g/kg) and then as an infu-
sion to maintain an osmotic diuresis as long as the urine con-
tains myoglobin (positive hemoglobin nitrotoluidine test).
Sodium bicarbonate may be added to alkalinize the urine
and prevent the precipitation of acid hematin. The calculated
fluid requirement is approximately 1.7 times the standard
fluid calculation based on the total body surface area burned.
Electrolytes should be monitored frequently during the
resuscitation period.
B. Arrhythmias—After initial stabilization, the most imme-
diate risk is from cardiac arrhythmia, particularly when the
electric current has passed through the thorax.
Antiarrhythmics and inotropic support should be instituted
when appropriate. However, most arrhythmias are self-
limited and infrequently cause hemodynamic abnormalities.
Atrial fibrillation occurs occasionally and usually will con-
vert without treatment. Electrocardiographic changes are
present in 10–30% of patients. The most common abnor-
mality is nonspecific ST-T-wave changes. Myocardial infarc-
tion is unusual, but patients with high-voltage injuries may
sustain direct myocardial damage. In these patients, close
monitoring of fluid therapy may be necessary to prevent pul-
monary edema.
C. Neurologic Sequelae—More than half of patients with
severe electrical injury develop loss of consciousness, but full
recovery usually ensues. Neurologic sequelae sometimes are
delayed and may develop days to years after the injury.
Deterioration of neurologic status may be of three types:
(1) ascending paralysis, (2) amyotrophic lateral sclerosis, or
High-voltage electrocution
Burns >20% of BSA
Evidence of entrance and exit burns
Cardiac arrhythmias
Unconsciousness
Respiratory or motor paralysis
Multiple associated injuries
Prior medical compromise
Table 37–1. Criteria for ICU admission following electrical
injury.

CHAPTER 37
800
(3) transverse myelitis. Peripheral nerve injuries and motor
neuropathies result from demyelinization, vacuolization,
gliosis, and perivascular hemorrhage. The prognosis for
recovery of useful function is poor.
D. Burns—Most critical care required by victims of electri-
cal injury relates to burns. This subject is discussed in
Chapter 35.
Treatment: Lightning Strikes
The most severe complication of lightning injury is respira-
tory arrest caused by depression of the respiratory control
center. This can result in secondary cardiac arrest in an oth-
erwise salvageable patient. Surviving victims of lightning
strikes tend to have fewer complications than patients with
electrical injury. Early emergency resuscitation usually stabi-
lizes these patients to the point that only observation is nec-
essary. The need for cardiac monitoring for more than 24
hours is debatable. Most patients will be confused and have
anterograde amnesia covering a period of several days after
the incident. If neurologic deterioration is noted, CT scan-
ning or MRI should be obtained to exclude the possibility of
intracranial hemorrhage or other injury. In most cases, long-
term sequelae from lightning injuries are rare.
Fish RM: Electric injury: II. Specific injuries. J Emerg Med
2000;18:27–34. [PMID: 10645833]
Lee RC: Injury by electrical forces: Pathophysiology, manifesta-
tions, and therapy. Curr Probl Surg 1997;34:677–764. [PMID:
9365421]
Muehlberger T et al: The long-term consequences of lightning
injuries. Burns 2001;27:829–33. [PMID: 11718985]
O’Keefe-Gatewood M et al: Lightning injuries. Emerg Med Clin
North Am 2004;22:369–403. [PMID: 15163573]
Radiation Injury
ESSENTIALS OF DIAGNOSIS
Nausea and vomiting, diarrhea.
Weakness, dehydration.
Bone marrow depression.
Sepsis.
Severe neurologic changes.
Cardiovascular collapse.
General Considerations
Acute radiation syndrome consists of characteristic clinical
manifestations following accidental or therapeutic exposure
to ionizing radiation. In cases of unknown level of exposure,
knowledge of the manifestations enables the clinician to
estimate the exposure dose and determine appropriate
treatment.
Ionizing radiation can be either electromagnetic (eg, x-
rays and gamma rays) or particulate (eg, electrons, protons,
and neutrons). The power of penetration of these particles
is determined by the energy they carry. High-energy parti-
cles can travel deep into the body and cause severe damage
to tissues.
The principal lethal effect of radiation appears to be the
production of chemically active free radicals within cells that
damage essential macromolecules such as DNA. Very high
radiation doses will disrupt cell metabolism and result in
rapid cell death. Moderate radiation doses produce breaks in
double-stranded DNA. No visible effects occur until the cell
attempts mitosis. At that time, cell division may be arrested,
or the daughter cells may lack essential genetic material and
become nonfunctional. Small doses of radiation can produce
gene mutations. This may result in no observable effect or in
subsequent malignant transformation.
Individual tissues vary greatly in their sensitivity to radi-
ation damage. The most sensitive tissues are those that
require continued cellular proliferation for proper function,
such as the GI and hematopoietic systems. Acute radiation
syndrome is most pronounced in these systems. With very
high levels of exposure, dysfunction of the cardiovascular
and central nervous systems is also observed, most likely
resulting from direct organ injury.
Radiation Dosimetry
The rad is the unit of absorbed radiation dose. It is defined
as that quantity of radiation that deposits 100 ergs of energy
per gram of tissue. Clinically, a dose of radiation is often pre-
scribed in grays (Gy) (1 Gy = 100 rads; 1 rad = 1 cGy).
Clinical Features
Radiation injury is characterized by an acute phase, referred
to as the prodromal phase, and a subacute phase, character-
ized by bone marrow and GI dysfunction. The phases are
separated by a latent period of 1–3 weeks, during which time
the patient may be completely asymptomatic. The severity of
acute radiation injury is determined by the dose and the time
over which the exposure occurs. After exposure to less than
150 cGy, most patients have minimal or no prodromal symp-
toms. Slight depression of platelets and granulocytes may be
observed after a latent period of 30 days. Lymphocytes are
most sensitive to radiation and may be decreased.
Patients exposed to 150–400 cGy develop transient nau-
sea and vomiting 1–4 hours following exposure. After a latent
period of 1–3 weeks, GI symptoms occur: nausea, vomiting,
and bloody diarrhea. Bone marrow depression is manifest by
anemia, coagulopathy, and depressed immune function.
Susceptibility to infection is increased significantly.
An acute whole body exposure of 600–1000 cGy results in
an accelerated version of the acute radiation syndrome. GI
complications predominate in the early phase of the illness

CARE OF PATIENTS WITH ENVIRONMENTAL INJURIES
801
and may be life-threatening. Severe hematologic complica-
tions can be expected to develop in survivors.
A fulminating course is seen in patients sustaining acute
whole body exposure to higher doses. Vomiting occurs
shortly after exposure and is rapidly followed by diarrhea,
tenesmus, dehydration, and circulatory collapse. CNS mani-
festations may include ataxia, incoordination, weakness, con-
fusion, seizures, and coma. Death occurs within 48 hours.
Pericarditis with effusions and constriction are delayed
manifestations that develop several months after exposure.
Myocarditis can occur but is less common. If injury is mild,
full recovery is the rule.
Treatment
In cases of moderate radiation exposure, initial treatment is
supportive and uncomplicated. Immediate aggressive ther-
apy is not indicated because the prodromal symptoms usu-
ally are not severe and are self-limited. It is after the latent
period of 1–3 weeks that the more severe clinical manifesta-
tions of the syndrome develop. In cases in which severe
symptoms develop without a latent period, death is
inevitable, and only symptomatic care should be provided.
Patients with moderate to severe radiation exposure
should be admitted to the hospital and isolated. Care should
be exercised to limit patient and personnel movement
through the hospital in order to contain the radiation. Many
radioactive materials are in particulate form and will not
pass through the skin and are removed by washing. To this
end, clothes should be removed and stored in specially
labeled plastic bags. Showering or washing skin surfaces
removes most of the contamination. A Geiger counter
should be used to assess the adequacy of decontamination.
The process can be aided by hair removal. Undiluted house-
hold bleach (5% sodium hypochlorite) can be used after
soap and water. A dilute solution (1 part bleach to 5 parts
water) should be used around the face and wounds. Wounds
should be thoroughly debrided and irrigated to remove
radioactive material.
Fluid loss should be corrected with intensive intravenous
replacement. The blood count should be monitored care-
fully. Reverse isolation is required when the white blood cell
count falls below 1000/μL. Whole blood and platelet transfu-
sions are nearly always required because of anemia and bleed-
ing. When immunosuppression is apparent, blood products
should be irradiated with 5000 cGy before transfusion to
decrease the possibility of a graft-versus-host reaction.
Intestinal microorganisms are a major source of infection,
and prophylactic antibiotics directed against gram-negative
organisms should be administered. The appearance of clinical
signs of infection should prompt a thorough evaluation.
Broad-spectrum antibiotics should be administered until
culture results are obtained.
The use of chlorpromazine or promethazine in an
attempt to control radiation-induced vomiting should be
avoided. These medications depress gastric emptying and
may increase the risk of aspiration and subsequent pul-
monary infection.
Current Controversies and Unresolved Issues
Antidopaminergic agents appear to prevent radiation-
induced vomiting without causing gastroplegia. Clinical tri-
als suggest that domperidone may be effective, but more
controlled studies need to be completed.
In most cases of moderate to severe acute radiation
injury, exposure of the bone marrow is not uniform, and a
return of function can be anticipated. In cases of lethal expo-
sures, the use of bone marrow transplantation as a form of
therapy has been suggested. However, based on current expe-
rience, the likelihood of success cannot be adequately
ensured. Numerous problems exist in the potential applica-
tion of this type of therapy. It could not be used in a mass-
casualty situation because of the extensive resources required
for the treatment of individual patients. Additional problems
can be anticipated in securing suitable HLA-compatible
donors and in controlling graft-versus-host disease. This
treatment was attempted in 13 victims of the Chernobyl acci-
dent. Eleven of these patients died. It is not clear whether the
other two patients would have survived with conventional
supportive therapy.
A newer mode of treatment of pancytopenia is the stim-
ulation of hematopoietic tissue through the use of cytokines
and colony-stimulating factors. This has been demonstrated
to decrease the period of leukocyte count depression and to
elevate the nadir. Additional studies are required to establish
efficacy and optimal dosing regimens.
GI pathogen suppression may be accomplished by the
deliberate inoculation of the gut with nonpathogenic bacte-
ria such as lactobacilli. The theory is that this will result in
normalization of the intestinal flora that had been altered by
antibiotic therapy. Prolonged survival has been demon-
strated in animal models, but studies in humans are lacking.
Bice-Stephens WM: Radiation injuries from military and acciden-
tal explosions: A brief historical review. Mil Med
2000;165:275–7. [PMID: 10802999]
Leikin JB et al: A primer for nuclear terrorism. Dis Mon
2003;8:485–516. [PMID: 12891217]
Meineke V et al: Medical management principles for radiation
accidents. Mil Med 2003;168:219–22. [PMID: 12685687]
Turai I et al: Medical response to radiation incidents and nuclear
threats. Br Med J 2004;328:568–72.

802
00
PHYSIOLOGIC ADAPTATION TO PREGNANCY
The average duration of gestation is 40 weeks from the first
day of the last menses, with term defined as being between
37 and 42 weeks. The mother’s basic physiology is altered in
a number of ways during normal pregnancy. Some of these
may alter her baseline state and response to critical illness,
but others may predispose to injuries and conditions that
require critical care.
Cardiovascular System
Pregnancy causes changes in the appearance and function of
the heart and great vessels. Elevation of the hemidiaphragms,
which accompanies advancing pregnancy, causes the heart to
assume a more horizontal position in the chest, and this
results in lateral deviation of the cardiac apex, with a larger
cardiac silhouette on chest x-ray and a shift in the electrical
axis. The heart does increase in size in pregnancy, but only by
about 12%. Cardiac output increases by 30–50%, with most
of the increase occurring in the first trimester. Both stroke
volume and heart rate increase. The heart rate increases by
about 17%, with the maximum reached by the middle of the
third trimester (32 weeks). Stroke volume increases by 32%,
with the maximum reached by midgestation. After 20 weeks,
cardiac output may decrease significantly (25–30%) when the
patient lies in the supine position as compared with the left
lateral position. This is apparently due to compression of the
inferior vena cava by the pregnant uterus with resulting
decreased venous return. The distribution of cardiac output is
altered as well. At term, 17% of the cardiac output is directed
to the uterus and its contents, and an additional 2% goes to
the breasts. The skin and kidneys also receive additional blood
flow compared with the nonpregnant state. Blood flow to the
brain and liver may increase. Perfusion of other organs such
as the skeletal muscle and gut is unchanged.
Peripheral vascular resistance decreases during preg-
nancy. A concomitant decrease in systemic blood pressure
reaches its nadir at about 24 weeks of gestation. Blood pressure
then rises gradually until term but should not exceed non-
pregnant levels at any time during pregnancy. Central hemo-
dynamic studies of normal pregnant women demonstrate a
significant decrease in both systemic and pulmonary vascu-
lar resistance. Mean arterial pressure, pulmonary capillary
wedge pressure, central venous pressure, and left ventricular
stroke work index are unchanged. Colloid osmotic pressure
is decreased.
Labor and delivery are associated with cardiac stress
beyond that of late pregnancy. Cardiac output may increase
by as much as 40% in patients not receiving adequate pain
relief, although those with adequate anesthesia experience
much smaller rises. The rise in cardiac output is progressive
over the different stages of labor, and there is a further rise
of approximately 15% during each uterine contraction
resulting from the expression of 300–500 mL of blood from
the uterus back into the mother’s circulation. Delivery of
the fetus is associated with as much as a 59% increase in
cardiac output, presumably as a result of autotransfusion of
blood contained in the uterus. This increase may be blunted
by the blood loss at delivery. In patients with clinically sig-
nificant mitral stenosis, delivery may be associated with an
increase in the pulmonary capillary wedge pressure of up to
16 mm Hg.
Respiratory System
During pregnancy, the subcostal angle increases from about
68 degrees to about 103 degrees, with a concomitant increase
in the transthoracic diameter. The resting level of the
diaphragm is 4 cm higher at term than in the nongravid
state. Many authors state that this elevation is a result of pres-
sure from the expanding uterus. However, diaphragmatic
excursions are increased by 1–2 cm over nonpregnant values,
suggesting that uterine pressure is not the sole cause of the
elevation.
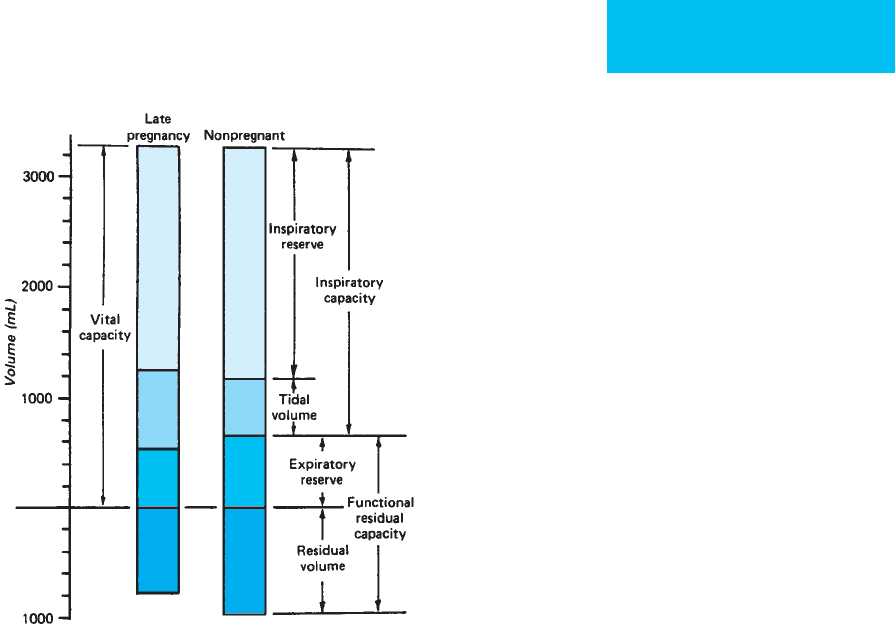
Several aspects of pulmonary function change during
pregnancy (Figure 38–1). Tidal volume increases by about
40%, and residual volume decreases by about 20%. These
38
Critical Care Issues
in Pregnancy
Marie H. Beall, MD
Andrea T. Jelks, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CRITICAL CARE ISSUES IN PREGNANCY
803
changes may make the lung appear denser on x-ray because
it is more collapsed during expiration. Data on vital capacity
in pregnancy are contradictory, with older studies suggesting
that there is no change and some newer ones suggesting that
there is a marked increase. During pregnancy, expiratory
reserve volume decreases by about 200 mL, and inspiratory
reserve volume increases by about 300 mL. Forced expiratory
volume appears to be unchanged.
Total body oxygen uptake at rest increases by about
30–40 mL/min in pregnancy, or about 12–20%. Most of the
oxygen is needed to meet maternal metabolic alterations.
The increased oxygen need is met by increased tidal vol-
ume alone because the pulmonary diffusing capacity
appears to be decreased in pregnancy, and the respiratory
rate does not significantly increase. There is a total increase
in minute ventilation of 48% at term, which exceeds the
need for increased oxygen delivery. This “hyperventilation
of pregnancy” appears to be hormonally mediated and
results in a decrease in Pa
CO
2
to below 30 mm Hg in normal
women. Maternal pH does not change because there is a
reciprocal decline in bicarbonate concentration. The net
result of these acid-base alterations is facilitation of fetal-
maternal CO
2
exchange.
Hematologic System
Both the volume and the composition of the blood change
during pregnancy. Plasma volume increases by 40–60%, the
bulk of the increase occurring before the beginning of the
third trimester. The red blood cell mass also expands, with a
total increase of 25% at term. This percentage can be maxi-
mized (to about 30%) by iron supplementation. An increase
in red blood cell mass occurs throughout pregnancy, but the
early—and in some patients disproportionate—increase in
plasma volume leads to a dilutional anemia. Normal preg-
nant women who are not iron-supplemented have hemoglo-
bin concentrations of approximately 11 g/dL at 24 weeks of
gestation, with little change until term. Those supplemented
with iron have similar hemoglobin concentrations at 24 weeks
but manifest an increase in hemoglobin to near-normal at
term.
The white blood cell count increases to about 10,000/μL at
term. The platelet count may decrease slightly to a mean value
of 260,000/μL at 35 weeks of gestation. Platelet levels above
120,000/μL generally are regarded as normal in pregnancy.
Biochemical characteristics of the blood also change.
Serum osmolarity decreases by about 10 mOsm/L early in
pregnancy and remains constant thereafter. Sodium, potas-
sium, calcium, magnesium, and zinc all demonstrate minor
decreases in their serum levels. Chloride does not change,
although bicarbonate decreases markedly. Serum creatinine
decreases early, with a mean creatinine of 0.66 mg/dL at
12 weeks, and this decrease is maintained at least until 32 weeks
of gestation. The creatinine clearance in pregnancy is
approximately 50% higher than in the nonpregnant state.
The plasma concentrations of albumin and total protein
decrease in proportion to the plasma volume expansion.
Most of the commonly tested serum enzymes do not change
in pregnancy, but alkaline phosphatase does increase as a
result of the production of a placental form of this enzyme.
Creatine kinase decreases in early pregnancy, although the
serum levels return to normal by term. Serum lipids increase
toward term, with the levels of cholesterol and triglycerides
doubling during pregnancy.
The levels of many coagulation factors are altered.
Fibrinogen increases to levels as high as 600 mg/dL at term,
with levels below 400 mg/dL generally being regarded as
unusual. The presence of fibrin degradation products in trace
amounts is also not unusual at term and depends on the sensi-
tivity of the test being used. Coagulation and bleeding times are
not increased. The risk of thromboembolism increases, with a
relative risk of 1.8 in gestation and 5.5 during the puerperium.
The increased risk of thromboembolism also may be due to the
increased incidence of venous stasis and vessel wall injury.
Immune System
Pregnant women appear to be at increased risk of certain
infections, probably owing to the same immune alterations
that allow tolerance of the antigenically foreign placenta. For
Figure 38–1. The components of lung volume in late
pregnancy compared with those in nonpregnant women.
(Reproduced, with permission, from Hytten FE, Leitch I: The
Physiology of Human Pregnancy. Boston: Blackwell, 1964.)
CHAPTER 38
804
this reason, reactivation of viral diseases and tuberculosis are
more common during pregnancy. Severe complications of
common disorders such as varicella and pyelonephritis are
also more frequent. Measurable indices of immune function
such as white blood cell counts and immunoglobulin levels
do not explain the maternal immune dysfunction. Various
theories have been offered to explain these observations, but
none has achieved general acceptance.
Granger JP: Maternal and fetal adaptations during pregnancy: Lessons
in regulatory and integrative physiology. Am J Physiol Regul Integr
Comp Physiol 2002;283:R1289–92. [PMID: 12429557]
Yeomans ER, Gilstrap LC 3
rd
: Physiologic changes in pregnancy
and their impact on critical care. Crit Care Med 2005;33:
S256–8. [PMID: 16215345]
GENERAL CONSIDERATIONS IN THE CARE
OF THE PREGNANT PATIENT IN THE ICU
The care of the pregnant patient is necessarily the care of two
patients. Although care of the mother is the primary concern
in most circumstances, attention also must be paid to fetal
health and well-being.
Position
As discussed earlier, a pregnant woman may experience a
decrease in cardiac output with associated hypotension when
lying in the supine position. For this reason, the pregnant
woman who is beyond the twentieth week of gestation
should avoid lying supine. In the ICU, this means that preg-
nant women who are bedridden and unable to move by
themselves should be positioned with the right hip elevated,
usually with an obstetric wedge, to about 4 in above the plane
of the bed. Alternatively, the patient may be positioned in the
right lateral decubitus position, taking care that she is tilted
adequately to prevent caval compression. This is not neces-
sary in a patient who is in Fowler’s position, that is, with the
head of the bed elevated. Because of the increased risk of
thromboembolism in pregnancy or immediately postpar-
tum, these patients also should receive measures to prevent
deep venous thrombosis. Venous compression stockings may
be of some benefit, but—especially in the recently delivered
patient—heparin in doses adequate to achieve a partial
thromboplastin time (PTT) of 65–85 s or low molecular
weight heparin sufficient to achieve anti–factor Xa levels of
0.05–0.2 units/mL is considered necessary to avoid pelvic or
lower extremity venous thrombosis.
Monitoring
When caring for a critically ill pregnant patient, the question
of how to monitor the fetus arises frequently. Monitoring by
auscultation of fetal heart tones is considered one of the vital
signs in any hospitalized pregnant women. However, contin-
uous fetal heart rate monitoring with an electronic monitor
may be indicated in the viable or near-viable fetus (23 weeks
and beyond), especially if the maternal condition affects pul-
monary or hemodynamic function. Use of the continuous
fetal monitor requires personnel skilled in its interpretation.
Fetal monitoring may be especially helpful during special
procedures or surgery when maternal position, hypotension,
or anesthesia can lead to fetal compromise that could be
reversed with changes in position or fluid resuscitation. Fetal
heart rate monitoring according to a predetermined schedule
(nonstress testing) also may be useful in gauging fetal
response to the mother’s illness and in determining when
fetal compromise may necessitate early delivery. This strategy
(as opposed to continuous fetal heart rate monitoring)
should be reserved for the stable patient whose underlying
condition might result in decreased uteroplacental perfusion
or altered placental function. Additional biophysical testing
might be deemed necessary by the consulting obstetrician,
but that subject is beyond the scope of this chapter.
Teratogenesis and Drugs Used During Pregnancy
Critical care of a pregnant patient necessarily involves the use
of drugs and physical agents that may have an effect on the
developing fetus. The first concern of the physician is properly
with the life and long-term health of the mother. In cases in
which alternative therapies or diagnostic modalities are avail-
able, the physician must consider their possible fetal effects.
Information regarding the potential risk to the fetus of
various agents is available from a number of published
sources and from the manufacturers’ package inserts. In
addition, many areas are served by teratogen “hotline” serv-
ices. The Food and Drug Administration (FDA) requires all
drug manufacturers to rate their drugs for risk in pregnancy
(Table 38–1). Most drugs are not studied in pregnancy dur-
ing the FDA approval period, so most new drugs will be
placed in category C. For this reason, many drugs used rou-
tinely during pregnancy are older ones, with an established
record of safe use.
The overriding principle in choice of a therapeutic agent
is that the anticipated benefit should outweigh any theoretic
risks. Consequently, a potentially teratogenic—but life-
sustaining—pharmacologic intervention for which there is
no good alternative would be acceptable, whereas one with
less proven risk but prescribed as a comfort measure only
might not be.
Imaging Studies
Ionizing radiation is known to be a human teratogen, and the
use of x-ray is appropriately limited in pregnant women.
Persons exposed to high levels of ionizing radiation in utero
may exhibit microcephaly, mental retardation, retarded
growth, and various structural abnormalities. Some reports
also have suggested an increased risk of childhood cancer fol-
lowing prenatal x-ray exposure. Data from atomic bomb sur-
vivors suggest that the most vulnerable period for the fetus is
from 8–15 weeks of gestation. Fetuses in this gestational age
CRITICAL CARE ISSUES IN PREGNANCY
805
range appear to have a linear increase in mental retardation
with increasing x-ray exposure, with an incidence of 0.4% per
rad of exposure, although a definite fetal effect may not be
seen below 5 cGy. Fetuses older than 16 weeks were less sensi-
tive to x-rays. In one study, the risk of childhood leukemia was
estimated to be 1.7 times that of controls in patients exposed
to radiation in utero. The risk for childhood cancers also
appeared to be higher in fetuses exposed to x-rays in the sec-
ond as compared with the third trimester. The fetal exposure
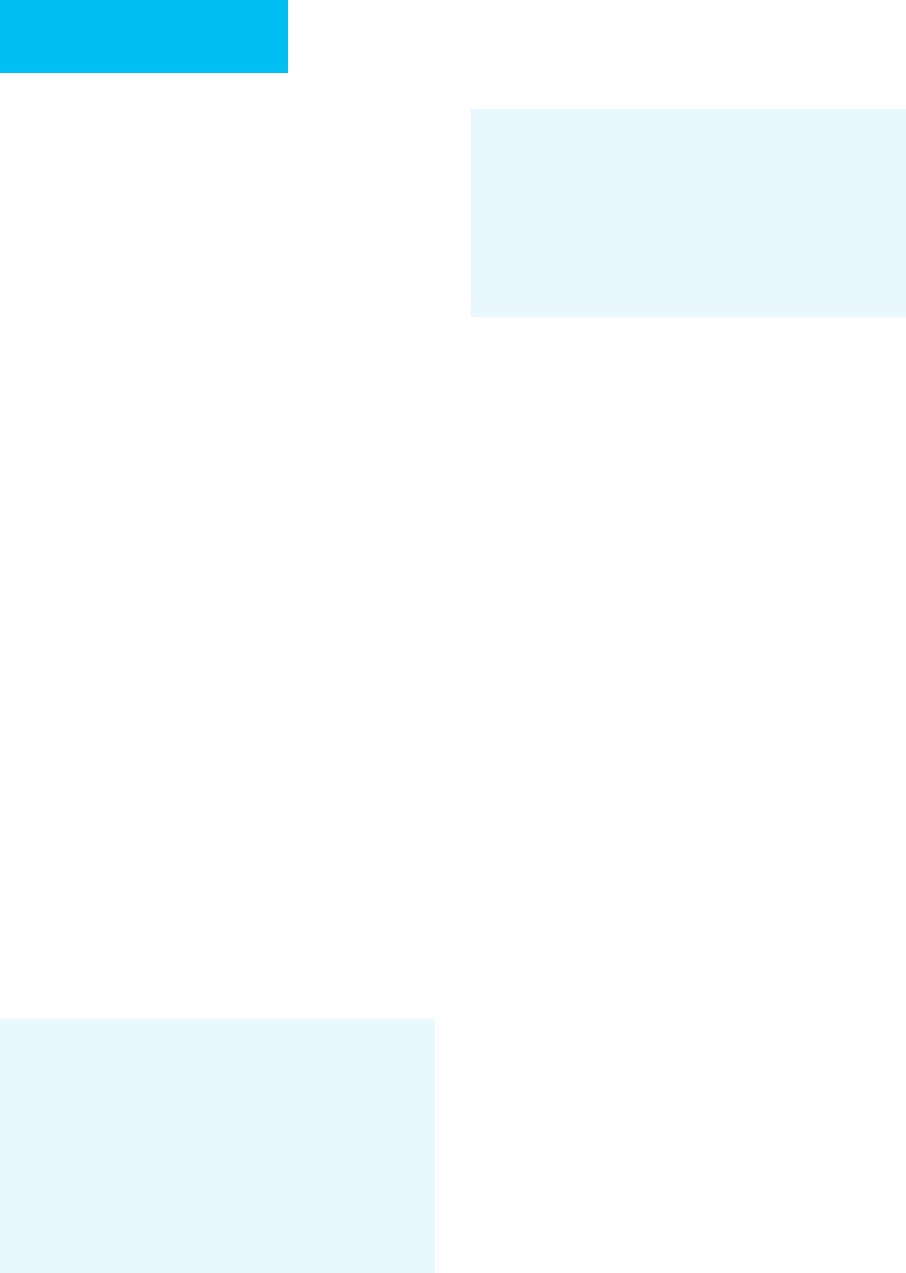
for different radiologic studies has been calculated and is pre-
sented in Table 38–2. As will be apparent, many studies, such
as chest films and head and neck studies, entail only slight
exposure of the fetus, although the fetal exposure owing to
abdominopelvic CT studies is appreciable. Nevertheless, the
uterus and its contents should be shielded whenever possible.
Iodinated contrast media are not contraindicated in preg-
nancy and may be used as in nonpregnant patients. These
media may be rated in category D owing to the risk of fetal
goiter when these agents are injected into the amniotic fluid.
Radionuclide scans should be used with caution in preg-
nancy. Iodine is concentrated in the fetal thyroid after 10 weeks
of gestation, and radioactive iodine may cause harm to the fetal
thyroid. Other radionuclides may be associated with an
increased risk of fetal mutagenesis or teratogenesis if they cross
the placenta in large amounts. Agents bound to large protein
aggregates do not cross the placenta and probably represent a
negligible risk to the fetus. In particular, the performance of
pulmonary ventilation-perfusion scanning for pulmonary
emboli has been calculated to result in a fetal dose of only
50 mrem, and this is largely from fetal exposure to the agent in
the maternal bladder during urinary excretion of the agent.
Ultrasonography is used extensively in obstetrics.
Controlled studies are not available regarding its safety, but
numerous observational studies have lead to the conclusion
that diagnostic ultrasound is safe for use in pregnancy.
However, fetal damage has been demonstrated in animal
models using ultrasound power levels sufficient to cause tis-
sue heating. For this reason, the use of therapeutic ultra-
sound in pregnancy is contraindicated. Few studies are
available concerning the safety of MRI in pregnancy. There is
a theoretical concern that the strong magnetic field may
affect fetal cell migration in the first trimester, and the use of
MRI has been discouraged early in pregnancy, although there
are no reports of adverse human fetal effects.
Total Parenteral Nutrition
As a consequence of depletion of maternal glucose by the
fetoplacental unit, pregnant patients are more sensitive than
Category A Controlled studies in women fail to demonstrate a
risk to the fetus in the first trimester (and there is no
evidence of risk in later trimesters), and the possibil-
ity of fetal harm appears remote.
Category B Either animal-reproduction studies have not demon-
strated a fetal risk but there are no controlled studies
in pregnant women, or animal-reproduction studies
have shown an adverse effect (other than a decrease
in fertility) that was not confirmed in controlled
studies in women in the first trimester (and there is
no evidence of a risk in later trimesters).
Category C Either studies in animals have revealed adverse
effects on the fetus (teratogenic or embryocidal or
other) and there are no controlled studies in women,
or studies in women and animals are not available.
Drugs should be given only if the potential benefit
justifies the potential risk to the fetus.
Category D There is positive evidence of human fetal risk, but the
benefits from use in pregnant women may be accept-
able despite the risk (eg, if the drug is needed in a
life-threatening situation or for a serious disease for
which safer drugs cannot be used or are ineffective).
Category X Studies in animals or human beings have demon-
strated fetal abnormalities, or there is evidence of
fetal risk based on human experience, or both, and
the risk of the drug in pregnant women clearly out-
weighs any possible benefit. The drug is contraindi-
cated in women who are or may become pregnant.
Federal Register 1980;44:31434–67.
Table 38–1. Risk factors for drug use in pregnancy.
Absorbed Dose
Examination Mrad mGy
Upper GI series 100 1
Cholecystography 100 1
Lumbar spine radiography 400 4
Pelvic radiography 200 2
Hip and femur radiography 300 3
Retrograde pyelography 600 6
Barium enema study 1000 10
Abdominal (KUB) radiography 250 2.5
Hysterosalpingography 150 10
CT scan, head ~0 ~0
CT scan, chest 16 0.16
CT scan, abdomen 3000 30
Data from Parry RA, Glaze SA, Archer BR: The AAPM/RSNA Physics
Tutorial for Residents. RadioGraphics 1999;19:1289–1302.
Table 38–2. Estimated doses to the uterus from diagnostic
procedures.
CHAPTER 38
806
nonpregnant ones to starvation. Blood glucose is lower by
15–20 mg/dL in a pregnant woman after a 12-hour fast, and
starvation ketosis is exaggerated. Undernutrition has been
associated with increased infant mortality and decreased
birth weight. These facts suggest that nutrition should be
addressed early in the course of critical care. Total parenteral
nutrition has been used in pregnancy with good fetal out-
comes in patients with intractable nausea and vomiting of
pregnancy as well as in patients with other chronic diseases.
Total parenteral nutrition should be considered in any preg-
nant patient who is expected to be without oral intake for
more than 7 days and in whom enteral (tube) feedings are
contraindicated. In patients in whom shorter durations of
starvation are expected, peripheral nutritional supplementa-
tion is essential. At a minimum, when the patient is denied
oral intake, enough intravenous glucose should be adminis-
tered to avoid ketonemia.
Patient Counseling
The fetal organs are essentially fully formed by the end of the
first trimester. This is important when considering the ter-
atogenic potential of medications given to the mother.
Teratogenic effects are most likely to occur early, when preg-
nancy may not yet be diagnosed. CNS growth and develop-
ment, body growth, and sexual organ development occur in
the second trimester, with CNS development and body
growth continuing during the third trimester. Drugs given
during the last trimester may affect neurologic development
but will not cause significant structural abnormalities other
than impaired fetal growth. A woman in the ICU who is
found to be pregnant should be given complete information
on the timing and dosages of the drugs and diagnostic agents
used in her care. It may be helpful to refer such a patient and
her family to a medical geneticist or prenatal diagnostic cen-
ter for counseling and possible diagnostic procedures. As a
medicolegal issue, it also may be advisable to obtain an
obstetric ultrasound examination as early as possible during
the pregnant patient’s stay in the ICU. Fetal abnormalities
apparent at that time are probably preexisting conditions
and not the result of medications given in the unit.
Furthermore, this will document gestational age and estab-
lish a baseline from which to assess fetal growth.
ACOG Committee on Obstetric Practice: ACOG Committee
Opinion. Number 299, September 2004. Guidelines for diagnos-
tic imaging during pregnancy. Obstet Gynecol 2004;104: 647–51.
[PMID: 15339791]
Briggs GG, Freeman RK, Yaffe SJ: Drugs in Pregnancy and
Lactation: A Reference Guide to Fetal and Neonatal Risk, 7th ed.
Philadelphia: Lippincott Williams & Wilkins, 2005.
De Santis M et al: Ionizing radiations in pregnancy and teratogen-
esis: A review of literature. Reprod Toxicol 2005;20:323–9. [PMID:
15925481]
Fattibene P et al: Prenatal exposure to ionizing radiation: Sources,
effects and regulatory aspects. Acta Pediatr 1999;88:693–702.
[PMID: 10447122]
McNally RJ, Parker L: Environmental factors and childhood acute
leukemias and lymphomas. Leuk Lymphoma 2006;47:583–98.
[PMID: 16690516]
Shepard TH, Lemore RJ: Catalog of Teratogenic Agents, 11th ed.
Baltimore: Johns Hopkins University Press, 2004.
Soubra SH, Guntupalli KK: Critical illness in pregnancy: An
overview. Crit Care Med 2005;33:S248–55. [PMID: 16215344]
Vasquez DN et al: Clinical characteristics and outcomes of obstet-
ric patients requiring ICU admission. Chest 2007;131:718–24.
[PMID: 17356085]
Cardiopulmonary Resuscitation (CPR)
in the Pregnant Woman
The American Heart Association has recommended that
when cardiac arrest occurs in a pregnant woman, standard
resuscitative measures and procedures can and should be
taken without modification. In particular, they endorse the
use of closed-chest compression, defibrillation, and vaso-
pressors as indicated and emphasize the need to displace the
uterus from the abdominal vessels by a right hip wedge or by
manual pressure on the fundus. Finally, they endorse the per-
formance of a perimortem cesarean section promptly if rou-
tine ACLS protocols are ineffective in restoring circulation
(see below).
Labor and Delivery in the ICU
The presence of a pregnant woman in the ICU necessitates a
plan for delivery of the pregnancy, if necessary. On occasion,
spontaneous labor may occur in a patient too unstable to be
transferred to the delivery room. In this case, labor and deliv-
ery must be undertaken in the ICU. Fetal heart rate monitor-
ing may be useful in advising the pediatrician about the fetal
condition even if cesarean section is not an option. Attention
should be paid to achieving adequate maternal analgesia
because of the significant maternal cardiac demands
imposed by unmedicated labor. In the case of any fetus of
22 weeks or more of gestational age or expected to weigh
more than 500 g, a neonatal resuscitation team should be in
attendance at delivery. The delivery should be conducted by
experienced personnel in an atraumatic manner.
Rarely, it may be necessary to perform perimortem
cesarean section in the ICU if the mother has died and an
attempt is being made to salvage the fetus. For this reason, in
any critically ill hospitalized pregnant patient, a determina-
tion should be made as early as possible about the potential
viability of the fetus. If perimortem cesarean section is a pos-
sibility, necessary instruments should be kept at or near the
bedside. In a large series of such procedures, normal infant
survival was associated with delivery within 5 minutes of
maternal death (from cardiac arrest). Fewer than 15% of
infants survived when delivery was performed more than
15 minutes after maternal demise, although fetal survival
after a much longer delay has been reported. Given this infor-
mation and data suggesting that the effectiveness of CPR in
