Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

ANTITHROMBOTIC THERAPY
827
UFH is effective for prevention and treatment of VTE
(DVT and PE; Table 39-4), mural thrombus after myocardial
infarction, unstable angina, and acute myocardial infarction.
UFH is usually combined with antiplatelet agents (eg,
aspirin, clopidogrel, and more recently, GP IIb/IIIa receptor
inhibitors) in the treatment of acute ischemic heart disease.
UFH has been used in conjunction with thrombolysis for
coronary artery occlusion; however, recent studies have sug-
gested that UFH may increase the risk of bleeding with little
added benefit over thrombolysis, particularly in patients
receiving aspirin. UFH is used alone or in combination with
GP IIb/IIIa inhibitors during percutaneous coronary inter-
vention (PCI). UFH is not effective for prevention of
restenosis after coronary angioplasty, and prolonged infusion
of UFH after completion of PCI increases bleeding without
reducing ischemic events. Guidelines for use of UFH in coro-
nary artery disease have been proposed (see Table 39–4);
however, ongoing trials probably will result in modification
of these guidelines as results of studies using newer agents
and combinations of agents are reported. UFH is also used
during extracorporeal circulation of blood (in cardiovascular
surgery and hemodialysis), prior to cardioversion in atrial
fibrillation (if no mural thrombus is detected by trans-
esophageal echocardiography), in some cases of dissemi-
nated intravascular coagulation, and to treat fetal growth
retardation in pregnant women. Heparin (UFH or low-
molecular-weight heparin) is generally the anticoagulant of
choice during pregnancy because it does not cross the pla-
centa and is not teratogenic. Heparin is also used when
chronic oral anticoagulation (eg, in patients with heart
valves, atrial fibrillation, and recurrent thromboembolic dis-
ease) is interrupted for invasive procedures or when recur-
rent thromboembolism occurs despite adequate oral
anticoagulation.
Multiple factors modify the anticoagulant effects of UFH
(Table 39–5), so the precise dose of UFH in a given patient
cannot be predicted in advance. When immediate anticoag-
ulation is required, an intravenous bolus is given followed by
continuous intravenous infusion or intermittent subcuta-
neous UFH (see Table 39–3). Continuous infusion is used
more often because of its lower risk of hemorrhage, but inter-
mittent subcutaneous UFH may be used in selected situations
(eg, thromboprophylaxis). Long-term use of subcutaneous
UFH during pregnancy or other conditions requiring long-
term outpatient heparin therapy has been replaced with sub-
cutaneous low-molecular-weight heparin. Careful monitoring
of the aPTT is essential for patients maintained on UFH to
ensure adequate anticoagulant effect without undue risk of
hemorrhage (see Table 39–3). Larger doses of UFH are
required to treat established thromboembolic disease than for
prevention of VTE possibly because thrombin bound to fibrin is
much less sensitive to inhibition by UFH than circulating throm-
bin and because of increased plasma reactive proteins, which
bind and neutralize UFH. Heparin resistance (requirement of
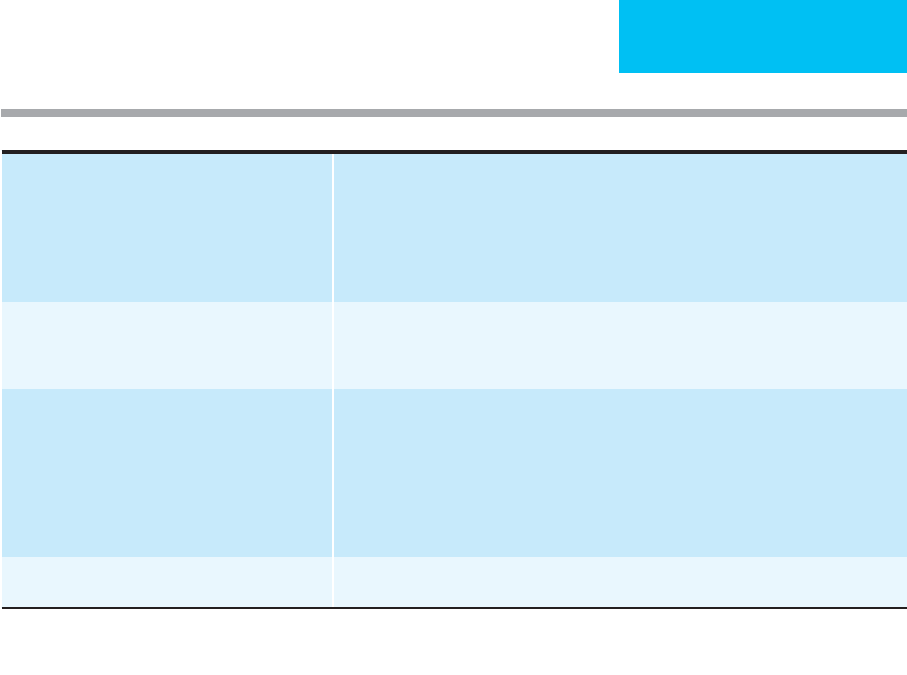
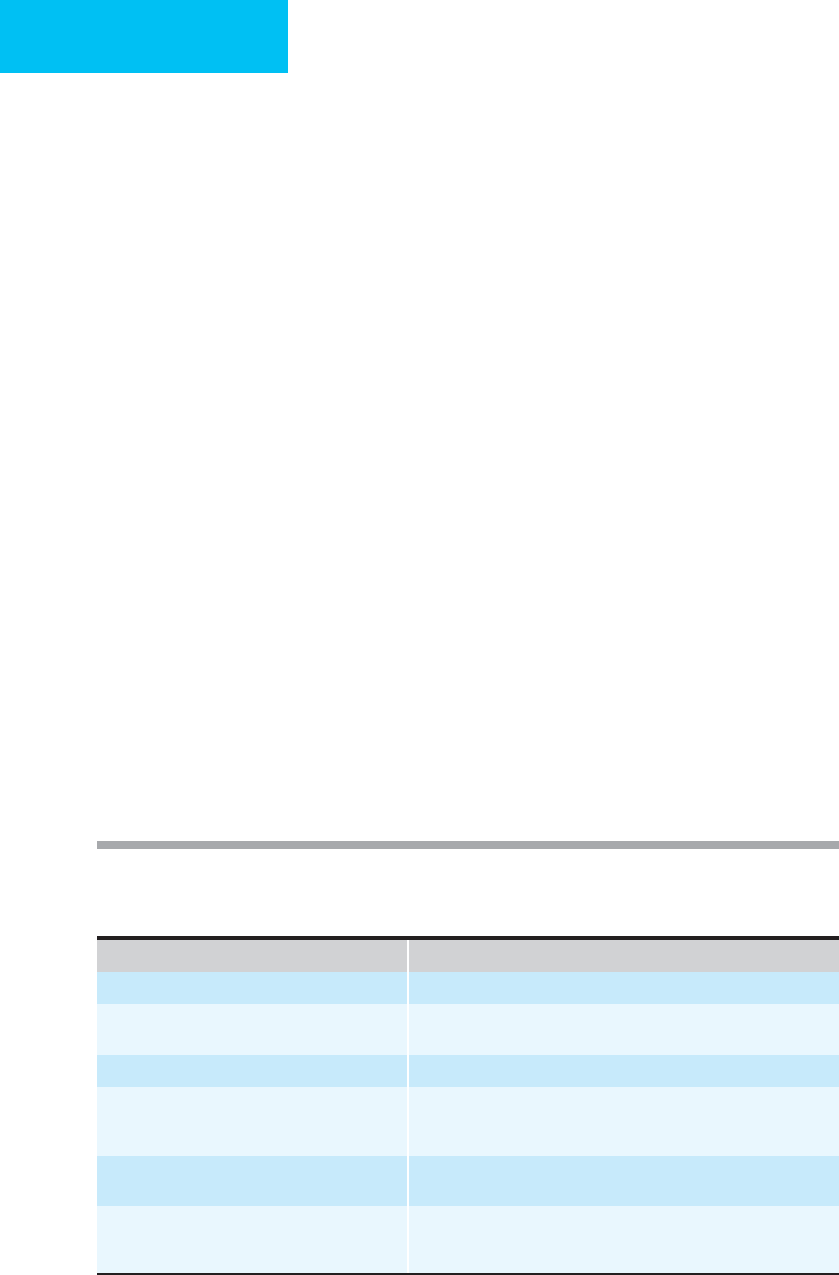
Table 39–4. Indications and administration of anticoagulants in selected settings.
∗
Prevention of venous thromboembolism Low risk (patients <40 with no risk factors undergoing minor surgery): early mobilization.
Moderate risk (<40 with risk factors for VTE or patients age 40–60): UFH every 12 hours, LMWH
(<3400 units/day), IPC.
High risk (patient >60, 40–60 with risk factors): UFH every 8 hours, LMWH (>3400 units/day), or IPC.
Highest risk (multiple risk factors, hip or knee arthroplasty, hip fracture surgery, major trauma,
spinal cord injury): LMWH (>3400 units/day), fondaparinux, oral anticoagulant (INR 2–3), or
IPC combined with UFH every 12 hours or LMWH daily.
Treatment of acute venous thromboembolism Adjusted-dose UFH. Monitor and adjust according to Table 39–3; OR full-dose LMWH (dose varies
by preparation). Begin oral anticoagulation on day 1. Continue UFH or LMWH until fully
anticoagulated with oral agent (overlap with oral anticoagulant in therapeutic range at least
2 days, usually 4–5 days total heparin).
Coronary artery disease (if no contraindication to
anticoagulation)
Non-ST-segment acute coronary syndrome (NSTEMI). Use UFH in combination with antiplatelet
therapy. Dose as in Table 39-3, target aPTT between 50 and 75 seconds
†
or LMWH (dose varies
with preparation.
Acute MI with ST-segment elevation (STEMI) or new left bundle branch. Use UFH in combination with
fibrinolytic: Dose as in Table 39–3, target aPTT between 50 and 75 seconds, administer for 48
hours (longer in patients at high risk for systemic or venous thromboembolism—anterior MI,
pump failure, atrial fibrillation, left ventricular thrombus, previous thromboembolism) or LMWH
(dose varies with preparation).
Chronic outpatient use (pregnancy,
warfarin failure)
∗
UFH at 12,000 units SC twice daily. Monitor aPTT 6 hours after injection and adjust subsequent
dose to maintain aPTT 50–85 seconds if LMWH is unavailable.
∗
Choice of specific regimen should take into account individual patient characteristics, including risk of thrombosis, risk of bleeding with
anticoagulation and renal function.
†
7th ACCP Conference Guidelines
CHAPTER 39
828
very large doses of heparin to prolong the aPTT) may occur
owing to the presence of elevated factor VIII or fibrinogen
levels, increased heparin-binding proteins, increased
heparin clearance, or AT deficiency. Measuring anti–factor
Xa levels may be a better alternative for monitoring heparin
therapy in these patients. It is not necessary to cause prolon-
gation of the aPTT for prevention of VTE in moderate-risk
patients, although in very high-risk patients—for example,
those undergoing orthopedic surgery—prolongation of the
aPTT to the upper end of normal is required to prevent
thrombosis.
Hemorrhage is the most common complication of
heparin therapy. Hemorrhage occurs more frequently with
high-dose heparin therapy and when the aPTT is prolonged
beyond the therapeutic range. Intermittent bolus UFH
results in a higher rate of hemorrhage than continuous-
infusion UFH, which may be due to the higher total daily
dose required to maintain a therapeutic aPTT with intermit-
tent administration. Concomitant use of aspirin or other
antiplatelet drugs increases the risk of hemorrhage, but in
patients with coronary thrombosis, the risk is felt to be
acceptable. The presence of other hemostatic defects, chronic
alcoholism, and the overall general condition of the patient
also influence the risk of hemorrhage with heparin therapy.
Management of hemorrhage associated with UFH varies
depending on the severity of the bleeding and the degree of
the anticoagulant effect, as measured by the aPTT. If the indi-
cation for anticoagulation is strong, continuation of UFH
with close monitoring of the aPTT and blood counts may be
acceptable for patients with trivial bleeding. If minor bleed-
ing is associated with an aPTT that is markedly prolonged
above the therapeutic range, withholding UFH until the
aPTT falls into the desired range (usually within a few hours)
is recommended if the patient is stable, with clinical evalua-
tion of the patient before resuming UFH for evidence of con-
tinued hemorrhage. Serious bleeding requires cessation of
UFH therapy, whereas truly life-threatening bleeding (eg,
intracranial hemorrhage or hemorrhage associated with
hemodynamic instability) may require immediate reversal of
UFH with protamine sulfate. One milligram of protamine
sulfate per 100 units of UFH (50 mg protamine sulfate for a
5000-unit dose of UFH), given intravenously over 10 minutes
(to avoid hypotension), will neutralize UFH given 30 minutes
earlier. The dose of protamine sulfate should be reduced
depending on the time interval from UFH administration
(eg, give 50% of the dose if 60 minutes have elapsed and 25%
if 2 hours have elapsed), and for reversal of continuous-
infusion UFH, the dose of protamine sulfate should be esti-
mated based on the UFH infused in the preceding 2–3 hours.
Since protamine sulfate has a shorter half-life than UFH,
the dose may need to be repeated. Side effects of prota-
mine sulfate include hypotension with rapid administra-
tion and prolongation of the aPTT (with possible bleeding)
if excess protamine is given. Recombinant platelet factor
4 (2.5–5 mg/kg) has been reported to be effective for reversal
of UFH as well but is not available everywhere.
Heparin-induced thrombocytopenia (HIT) occurs com-
monly (5–15%) with therapeutic UFH administration, less
commonly with prophylactic UFH, and appears to be more
common with UFH derived from bovine lung than that from
porcine intestine. The onset of thrombocytopenia is usually
between 3 and 15 days after initiation of treatment with UFH
(median 10 days) but may be as short as a few hours in a pre-
viously sensitized individual, particularly if the prior treat-
ment with UFH was within 3 months of reexposure.
Resolution of thrombocytopenia occurs within 4–5 days of
discontinuation of UFH.
Thrombocytopenia in this disorder is immunologically
mediated. Heparin molecules greater than MW 4000 bind to
platelet factor 4 and form complexes to which heparin-
induced antibodies bind. Platelets are activated, resulting in
increased thrombin generation. Thrombosis, usually associ-
ated with very severe thrombocytopenia, occurs in about
0.4% of patients.
Diagnosis is usually made on clinical grounds, but sero-
logic tests are available to confirm the presence of HIT anti-
bodies. Although these tests are sensitive for the presence of
HIT antibodies, they are less specific and therefore must be
interpreted with caution. Prevention of this disorder by
shortening the duration of UFH administration is impor-
tant. Initiation of oral anticoagulants simultaneously with
UFH in patients who will require long-term anticoagulation
will permit a shorter course of UFH and is highly recom-
mended for patients requiring long-term anticoagulation.
Frequent (every 1–2 days) monitoring of the platelet count is
important for identification of patients before thrombosis
occurs. The use of low-molecular-weight heparin (or hepari-
noids) appears to be associated with a lower risk of heparin-
induced thrombocytopenia as well.
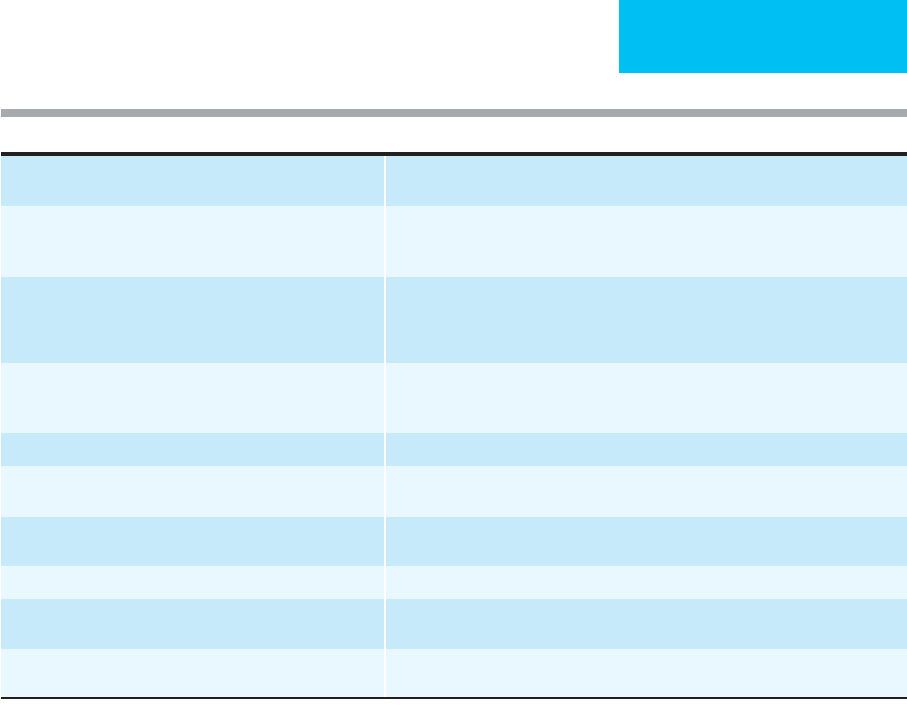
Management of HIT is outlined in Table 39–6. Stopping
UFH is the most common intervention, but there appears to
be a marked risk in clinically significant thrombosis in the
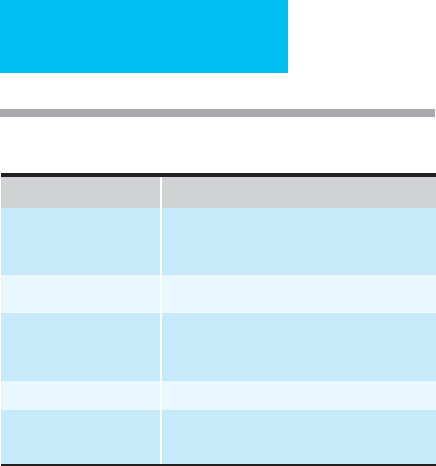
Table 39–5. Endogenous factors modifying the
anticoagulant effect of heparin.
Factor Mechanism
Platelets Bind and protect factor Xa from heparin.
Produce platelet factor 4 and neutralizes
heparin.
Fibrin Binds thrombin and protects if from heparin.
Endothelial surfaces Bind thrombin and protects it from heparin.
Bind and neutralize heparin via displaced
platelet factor 4.
Plasma proteins Bind and neutralize heparin.
Antithrombin
(antithrombin III)
Hereditary or acquired deficiency state results
in heparin resistance.
ANTITHROMBOTIC THERAPY
829
week after cessation of UFH. Warfarin may aggravate throm-
bosis and should be delayed until the platelet count is over
100,000/μL. There are two anticoagulants currently approved
in the United States for use in HIT—lepirudin (a recombi-
nant hirudin) and argatroban (a selective direct thrombin
inhibitor)—that should be considered even without overt
thrombosis. Bivalirudin (another hirudin analogue), which
is approved in the United States as an alternative to heparin
in patients undergoing percutaneous coronary interventions,
appears to be promising, and because it has only minor renal
excretion, it may be preferable to lepirudin in patients with
significant renal impairment. Anticoagulation with the alter-
native agent should be continued until the platelet count has
returned to normal. Ancrod also has been used for treatment
of HIT but is not available in the United States.
If anticoagulant therapy is necessary in a patient with a
suspected history of HIT (without complicating thrombo-
sis), heparin-dependent antibodies (platelet activation assay
or antigen assay) may help to determine the risk of reexpo-
sure to heparin. If negative, short-term treatment with UFH
with careful monitoring may be acceptable. Patients with a
history of HIT-associated thrombosis should be considered
for treatment with anticoagulants other than heparin.
Other adverse effects of UFH include transient elevation of
liver function tests (particularly ALT and AST), hyperkalemia,
osteoporosis (owing to heparin binding to osteoblasts that
release factors that stimulate osteoclasts; clinically significant
with long-term UFH administration), skin necrosis, alopecia,
hypersensitivity reactions, and hypoaldosteronism.
Low-Molecular-Weight Heparins (LMWHs)
LMWHs are prepared by depolymerization of UFH by
chemical or enzymatic means. Like UFH, LMWH accelerates
antithrombin-mediated inactivation of factor Xa, but unlike
UFH, LMWH does not inactivate thrombin because it lacks
the additional 13 saccharides required for heparin to form a
complex with AT. Because it binds less strongly to plasma
proteins, cells, and thrombin, LMWH has greater bioavail-
ability at low doses, a longer half-life, and a more predictable
anticoagulant response than UFH. LMWH can be adminis-
tered subcutaneously at a fixed dose (adjusted for weight)
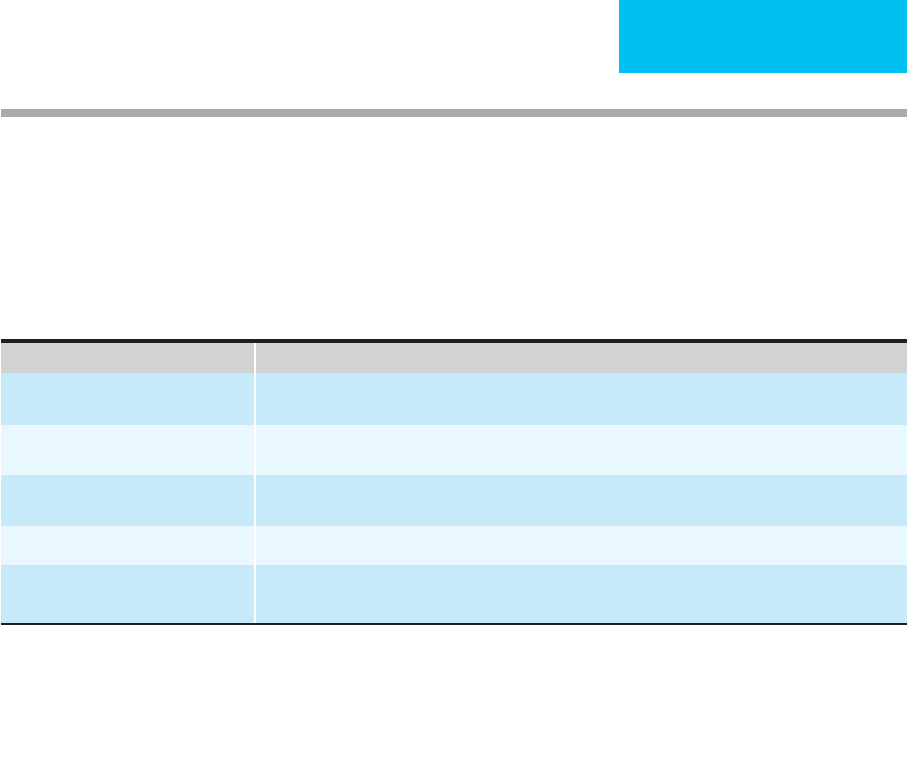
1. Monitor platelet counts during heparin therapy every 1–2 days.
2. Exclude other causes of acute thrombocytopenia (other drugs, sepsis, DIC, pseudothrombocytopenia).
3. Evaluate for thrombotic complications (iliofemoral artery occlusion, cerebral infarction, and myocardial infarctions are the most common; other
arterial thromboses and venous thromboses occur less commonly).
4. Do not administer platelet tranfusions (increased risk of thrombosis).
5. Discontinue heparin (including heparin flushes) for platelet count below 100,000/uL.
6. Administered alternative anticoagulant until the platelet count has recovered and oral anticoagulation has taken effect, if long-term anticoagulation
is required. Overlap alternative anticoagulant with warfarin for a minimum of 5 days.
∗
7. Consider lower extremity ultrasound to assess for subclinical thrombosis.
Anticoagulant Dose/Monitoring
Lepirudin (a recombinant hirudin
derivative)
0.4 mg/kg (up to 44 mg) IV bolus followed by 0.15 mg/kg/h. Adjust dose to maintain aPTT 1.5–2.5 times
normal range. May omit bolus in patients with renal failure.
Danaparoid (a heparinoid, available
outside the United States)
2250 units IV bolus followed by 400 units/h for 4 hours, then 300 units/h for 4 hours, then 150–250
units/h. Monitor anti-factor Xa activity (if available), maintain at 0.5–0.8 anti-factor Xa units/mL
Argatroban (a selective direct thrombin
inhibitor)
2 μg/kg/min. Adjust dose to maintain aPTT 1.5–3 times control (but <100 seconds)
Bivalirudin
†
(an analog of hirudin)
0.2 mg/kg/h. Adjust dose to maintain aPTT 1.5–2.5 times baseline.
Fondaparinux (a synthetic
pentasaccharide)
Not approved for HIT but may be useful as an alternative to heparin in patients with preexisting thrombocy-
topenia to avoid the development of HIT.
∗
Do not administer warfarin in patients with heparin-induced thrombocytopenia and deep venous thrombosis until platelet count is
>100,000 (potential risk for venous-limb gangrene). If anticoagulant therapy is necessary in a patient with a suspected history of heparin-
induced thrombocytopenia without complicating thrombosis, laboratory assessment for heparin-dependent antibodies (platelet activation
assay or antigen assay) may help determine risk of reexposure. If negative, short-term treatment with heparin along with careful monitoring
may be acceptable. Patients with a history of hepain-induced thrombocytopenia-associated thrombosis should be considered for alternative
anticoagulants.
†
FDA-approved for other indications (angioplasty).
Table 39–6. Management of heparin-induced thrombocytopenia.
CHAPTER 39
830
once or twice daily (dosing depends on specific preparation)
and does not require laboratory monitoring using the aPTT.
These two factors make outpatient use of LMWH possible in
selected situations. LMWH preparations are excreted
renally, and the biologic half-life is prolonged in patients
with renal failure. The incidence of HIT appears to be less
with LMWH than with UFH. LMWH has been used in some
patients with HIT, but thrombocytopenia may persist.
Several LMWH preparations are now approved for use in
the United States: enoxaparin, dalteparin, and tinzaparin.
Selection of one preparation over another is difficult at pres-
ent because few studies comparing different preparations and
dosing regimens have been performed. Cost ultimately may
be as important as any other factor for choosing which
LMWH to use. The major advantage of LMWHs compared
with UFH relates to their convenience of administration, pre-
dictable anticoagulant response at a weight-adjusted fixed
dose, and lack of need for laboratory monitoring. Exceptions
include renal failure and obesity, in which cases monitoring
may be useful. In patients with creatinine clearances of less
than 30 mL/min, anti–factor Xa activity accumulates with
repeated dosing, although this varies among the different
LMWHs. Use of UFH may be preferable in these patients, but
when LMWH is needed, decreasing the dose and monitoring
anti–factor Xa activity should be performed to prevent over-
anticoagulation. Few studies have addressed dosing in very
obese patients. There does not appear to be an increased risk
of bleeding during therapeutic anticoagulation with LMWH
in obese patients, but most studies have included very few
markedly obese patients. Measuring anti–factor Xa activity 4
hours after subcutaneous administration may provide useful
information for dose reduction. Conversely, since obesity is
an independent risk factor for thromboembolism, weight-
based dosing or a 25% increase in fixed-dose LMWH may be
preferable for thromboprophylaxis in very obese patients. A
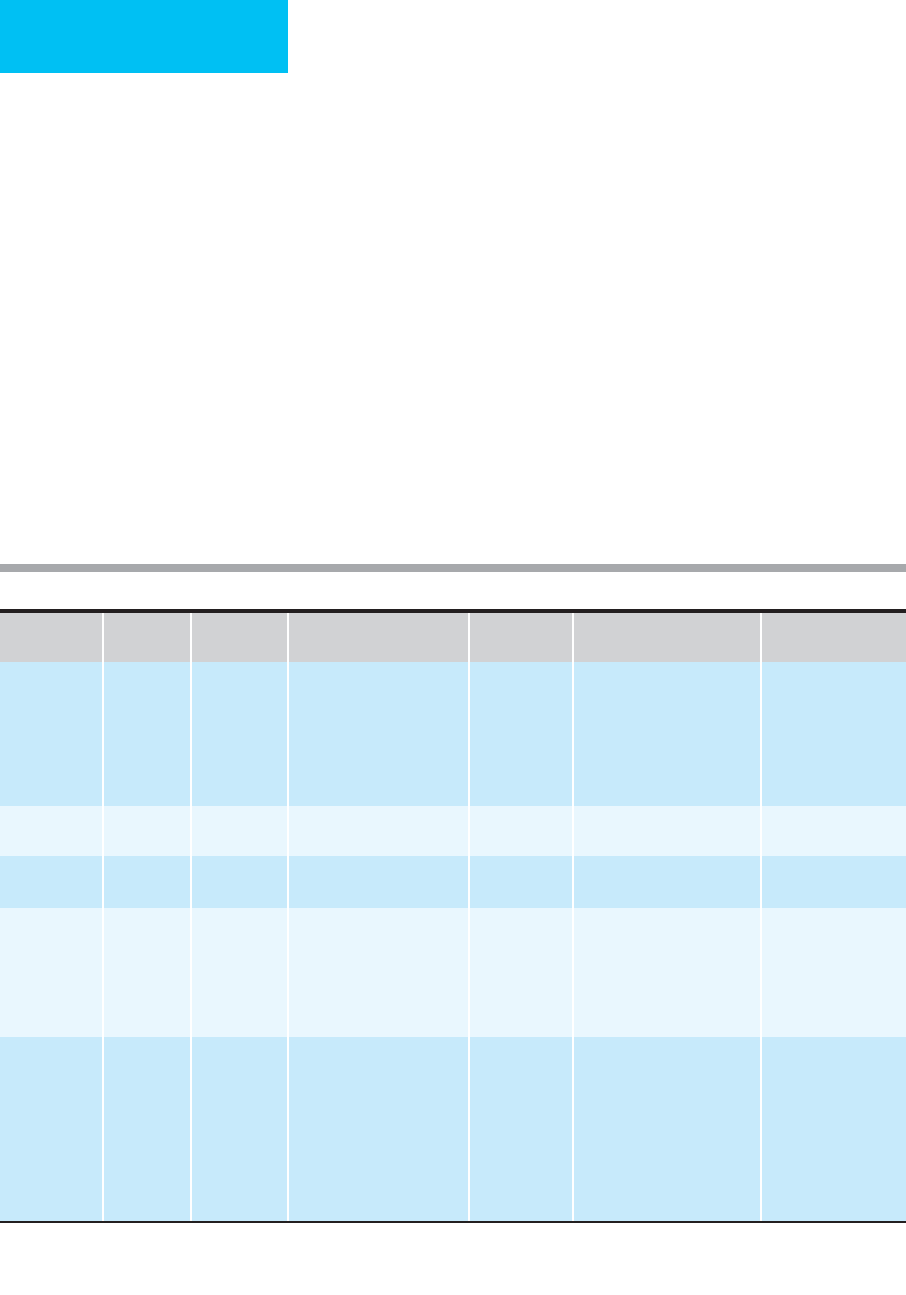
comparison of UFH and LMWH is presented in Table 39–7.
LMWH is effective for prevention of VTE in patients
undergoing major orthopedic procedures (eg, hip fracture or
replacement or knee replacement) or neurosurgery, after
major trauma (in patients eligible for anticoagulation), and
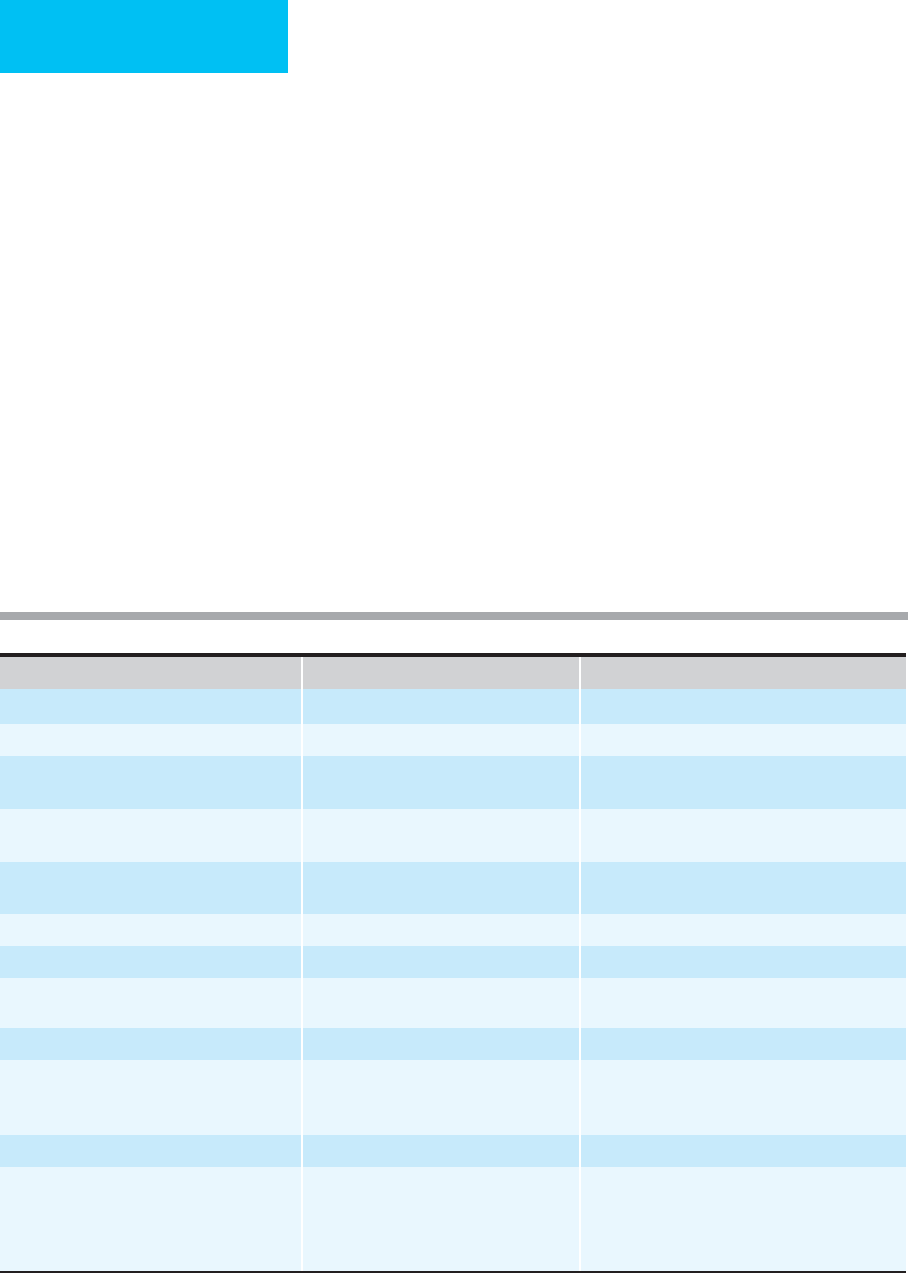
Unfractionated Heparin (UFH) Low-Molecular-Weight Heparin (LMWH)
Plasma half-life Dose-dependent; range 1–2.5 hours Increased; range 2–6 hours; prolonged in renal failure
Bioavailability Lower Better
Molecular weight: range
(Mean)
3000–30,000
(15,000)
100–10,000
(4500–5000)
Binding properties: proteins, cells (macrophages,
endothelium, osteoblasts)
High Low
Relative inactivation: Xa/IIa Lower Higher (five to six times compared with
unfractionated heparin)
aPTT Prolonged Not prolonged
Efficacy Equivalent Equivalent (most situations)
Major bleeding Approximately equivalent: 0–7% higher
(fatal, 0–2%), higher in acute stroke
Approximately equivalent: 0–3% (fatal, 0–0.8%),
higher in acute stroke
Heparin-induced thrombocytopenia 2.5–6% Decreased
Osteoporosis 30%: decreased bone density;
15%: vertebral fractures
2–3%: vertebral fractures in pregnancy
Decreased
2.5%: vertebral fractures
Cost $15/d, full dose >$100/d, full dose
Reversibility with protamine sulfate (PS) Good: 1 mg PS/100 units UFH (bolus dose);
estimate for infusion based on total amount
in preceeding 2–3 hours.
Fair, not reliable: <8 hours since LMWH at 1 mg/100
anti-factor Xa units (1 mg enoxaparin = 100 units)
>8 hours: smaller dose.
Repeat with 50% of original dose if persistent
bleeding.
Table 39–7. Comparison of unfractionated heparin and low-molecular-weight heparin.

ANTITHROMBOTIC THERAPY
831
in high-risk medical patients (see Table 39-4). LMWH is as
effective as UFH in the treatment of DVT and PE. It can be
administered to outpatients with acute DVT, but treatment
of PE may require hospitalization. LMWH is equivalent in
efficacy to warfarin for prevention of recurrent DVT follow-
ing acute DVT, with a lower incidence of minor bleeding, but
it is much more expensive. There also may be a higher rate of
rebound thromboembolism after discontinuation of the
drug than with warfarin.
The role of LMWH in coronary artery disease continues
to evolve as studies in various clinical syndromes are com-
pleted. LMWH is more effective than UFH in combination
with aspirin in the acute treatment of unstable angina and
non-ST-segment-elevation myocardial infarction. LMWH in
combination with thrombolytic therapy for acute myocardial
infarction has not been studied as extensively as UFH and
cannot be recommended until adequate studies demonstrate
efficacy and safety. LMWH may be used as an alternative to
UFH in patients undergoing PCI but is more difficult to
monitor and adjust than UFH. LMWH is not effective for
prevention of restenosis after coronary angioplasty and does
not reduce post-PCI ischemic events when administered fol-
lowing PCI. The use of LMWH is not recommended for
thromboprophylaxis in patients with prosthetic heart valves
but may be used as bridging therapy for these patients when
oral anticoagulation is temporarily interrupted.
Complications of therapy with LMWH are similar to
those seen with UFH heparin, with the exceptions of throm-
bocytopenia and osteoporosis, which occur less often with
LMWH. There may be less major bleeding in patients treated
for DVT with LMWH, but in most other situations the risk
is approximately equivalent to that seen with UFH. The use
of LMWH and heparinoids in the setting of spinal or
epidural anesthesia—or with spinal puncture—may cause
bleeding in the spinal column with subsequent prolonged or
permanent paralysis. If excessive bleeding does occur, labora-
tory assessment with a anti–factor Xa heparin assay can be
performed. The usual therapeutic range is between 0.5 and
1.0 unit/mL. When heparin anti–factor Xa is greater than
1.0 unit/mL, the aPTT also may be prolonged. Protamine
sulfate is much less effective for reversing the effect of
LMWH than UFH, but if serious bleeding occurs, protamine
sulfate, 1 mg per 100 anti–factor Xa units of LMWH (1 mg
of enoxaparin = 100 anti–factor Xa units), may be given, and
a smaller (50% of the original dose) dose may be given if
bleeding continues. Activated factor VII therapy recently has
been reported to reverse bleeding owing to LMWH, but has
not been adequately evaluated.
New Anticoagulants
Direct Thrombin Inhibitors
Lepirudin (a recombinant hirudin derivative), bivalirudin
(an analogue of hirudin), and argatroban are direct throm-
bin inhibitors that do not depend on antithrombin to exert
their anticoagulant effects. Unlike heparin, these agents bind
to free and clot-bound thrombin, do not bind to plasma pro-
teins, and are not neutralized by platelet factor 4. Hirudin
and argatroban are approved for use in HIT; bivalirudin is
approved for use as an alternative to heparin in patients
undergoing PCI (see Table 39–6). Studies of these agents in
other clinical settings have not shown clear advantages over
heparin, and there are no antidotes available to reverse the
anticoagulant effects of these drugs should bleeding occur.
Therefore, use of these agents has been restricted to the spe-
cific indications listed earlier. Lepirudin is cleared extensively
by the kidneys, requiring significant dose reduction and care-
ful monitoring in patients with renal impairment.
Bivalirudin has minor renal excretion and may be useful for
patients with impaired renal function as an alternative to lep-
irudin. Argatroban is a carboxylic acid derivative that inter-
feres with thrombin by binding to its active site. Several other
agents in this class are under investigation, some of them well
absorbed from the GI tract (eg, ximelagatran) with a pre-
dictable anticoagulant response, making laboratory moni-
toring unnecessary.
Indirect Thrombin Inhibitors
A. Pentasaccharide Analogues—These are synthetic ana-
logues of the pentasaccharide sequence responsible for bind-
ing heparin to antithrombin. They form a complex with
antithrombin that binds to and inhibits factor Xa; the pen-
tasaccharide is then released and can be reused. Fondaparinux
is the only agent in this class approved for use in the United
States for thromboprophylaxis following major orthopedic
surgery. It is administered subcutaneously once a day, is
excreted renally, and cannot be given to patients with creati-
nine clearances of less than 30 mL/min. Because it does not
bind to platelet factor 4, it should not cause thrombocytope-
nia. Fondaparinux is more effective than enoxaparin for pre-
vention of thromboembolism following major orthopedic
surgery. The rate of major bleeding may be higher than with
enoxaparin but appears to be similar if the first dose is given
6–8 hours after surgery. Fondaparinux is as effective as UFH or
LMWH in the initial treatment of VTE and is under investiga-
tion for patients with acute coronary syndromes. There is no
antidote for fondiparinux, but severe, uncontrolled bleeding is
potentially treatable with recombinant factor VIIa. However,
this extremely expensive agent is not available everywhere.
B. Heparinoids—Heparinoids are low-molecular-weight
glycosaminoglycuronans derived from porcine intestinal
mucosa. Danaparoid is available only outside the United
States for treatment of HIT and is a mixture of heparan sul-
fate, dermatan sulfate, and chondroitin sulfate. The small
heparan sulfate portion of this drug (4% of the total) has a
high affinity for antithrombin and is responsible for the major
anticoagulant effect of danaparoid. Dermatan sulfate also
mediates development of heparin cofactor II–thrombin com-
plexes and contributes to the anticoagulant effect. Danaparoid
has a higher ratio of anti–factor Xa activity compared with

CHAPTER 39
832
anti–factor IIa activity (20:1) than UFH (1:1) and LMWH
(2–4:1) and has fewer effects on platelet function than UFH.
It is similar to LMWH in its anticoagulant effects and has
minimal effect on coagulation parameters (ie, aPTT, PT, and
thrombin time), but it has certain structural differences (eg,
contains galactosamine, absent in LMWH) that distinguish it
from LMWH. A functional anti–factor Xa assay using dana-
paroid as the standard can be used to monitor the anticoag-
ulant effect of danaparoid when the agent is given for more
than 3 days. Danaparoid is as effective as lepirudin in the
treatment of HIT with less major bleeding. Danaparoid does
not cross the placenta, so it should be safe for treatment of
HIT during pregnancy.
Defibrinating Agents
Ancrod, an enzyme derived from the Malayan pit viper, is an
anticoagulant that cleaves fibrinogen and causes hypofib-
rinogenemia. Ancrod is licensed for use in Canada. Ancrod is
an effective anticoagulant that apparently causes minimal
excess bleeding. It is not associated with the development of
thrombocytopenia, is an excellent alternative anticoagulant
for patients with HIT, and has shown some promise in the
treatment of acute ischemic stroke. An initial dose of 1 unit/kg
is infused intravenously over 8–12 hours, followed by daily
maintenance doses adjusted for the level of fibrinogen
(see Table 39–7). Neutralizing antibodies develop with
long-term use, thus limiting its usefulness to situations in
which only short-term anticoagulation is required. An
antivenom is available to reverse its effect, and cryoprecipi-
tate also may be required for fibrinogen replacement if
excessive bleeding occurs.
Oral Anticoagulants
Warfarin
Warfarin (a 4-hydroxycoumarin compound) is the most
commonly used oral anticoagulant in North America.
Warfarin interferes with the metabolism of vitamin K,
inhibiting reduction of vitamin K to its active form, vitamin
KH
2
, in a two-step process in the liver. Vitamin KH
2
is essen-
tial for posttranslational modification (γ-carboxylation) of
the vitamin K–dependent coagulation factors and natural
anticoagulants (eg, factors II, VII, IX, and X and proteins C
and S). Decreased carboxylation of these important proteins
impairs their biologic function by impeding calcium-
binding capability and induces an anticoagulant effect.
Reduced protein C and S levels have the potential for causing
thrombosis, but in most situations, the anticoagulant effect
predominates.
Warfarin is absorbed rapidly from the GI tract, reaching
peak plasma levels in 90 minutes, circulates bound to plasma
proteins (97% albumin-bound), is metabolized in the liver,
and is excreted in urine and bile. The anticoagulant effect of
warfarin is not immediate. Until carboxylated coagulation
factors are adequately depleted, blood coagulation is normal.
The vitamin K–dependent proteins have plasma half-lives
ranging from 6 hours (factor VII) to 72 hours (prothrombin
and factor II). Proteins C and S have relatively short half-lives
(~8 hours). Because levels of factor VII, protein C, and pro-
tein S fall at about the same time—and 1–3 days before
depletion of the other coagulation factors—a relative hyper-
coagulable state may exist in the first 1–2 days after initiation
of warfarin. Although an observable anticoagulant effect
usually occurs after 2 days, the full antithromboic effect is
delayed for 4–5 days. The delayed effect may be of impor-
tance for patients with HIT and those with inherited or
acquired deficiency of protein C or protein S, who may be
particularly susceptible to warfarin-induced skin necrosis.
Whenever rapid anticoagulation is needed or in patients
with known thrombophilic states (eg, protein C or S defi-
ciency), heparin (UFH or LMWH) should be given for at
least 4 days at the start of warfarin therapy until the interna-
tional normalization ration (INR) is in the therapeutic
range. A loading dose of warfarin should not be given. The
initial dose should be between 5 and 10 mg for most patients
(lower for patients at high risk of bleeding or elderly
patients), with subsequent dosing based on results of the
INR. The average dose required to achieve a therapeutic level
by 4–5 days is 5 mg daily.
The anticoagulant effect of warfarin is assessed by in vitro
coagulation tests, the PT and aPTT. The therapeutic range
for warfarin depends on the indication for which it is used,
but at usual doses, the aPTT is normal or minimally pro-
longed, whereas the PT is maintained at 1.3 (low intensity) to
2.5 (high intensity) times control (PT ratio). Because of
marked interlaboratory variability in the sensitivity of the
thromboplastin reagents used in the PT assay, a standardized
approach has been adopted. This approach requires calibra-
tion of the thromboplastin to a reference preparation using
the international sensitivity index (ISI). Results then are
reported as the INR based on a formula comparing the PT
ratio obtained with the laboratory thromboplastin with that
with the reference thromboplastin. The therapeutic range of
warfarin for most indications ranges from an INR of 2–3
(low intensity) to an INR of 2.5–3.5 (high intensity). If the
thromboplastin reagent used by a clinical laboratory remains
constant, the PT and INR will be predictably related to each
other. Substitution of a reagent with either more or less sen-
sitivity, however, may dramatically alter the relationship of
the PT and INR. The INR is more reliable than the PT and is
the preferred method of reporting for warfarin monitoring.
It is important to fill the collection tube adequately when
measuring the INR because the concentration of the citrate
anticoagulant in the test sample affects the INR. Underfilling
the tube may lead to erroneously high INR results.
Although there is a direct dose-response relation, there is
marked variation in anticoagulant response to warfarin
among patients. There is also significant variability of antico-
agulant response during long-term therapy in individual
patients. This variability results from many factors, including

ANTITHROMBOTIC THERAPY
833
endogenous stores of vitamin K, changes in dietary intake or
recent therapeutic administration of vitamin K, genetically
determined differences in warfarin sensitivity, use of antibi-
otics (which may impair synthesis of vitamin K by intestinal
flora) or other drugs (which may increase or decrease war-
farin effect), the presence of liver disease, fat malabsorption
(including obstructive jaundice), hypermetabolic states,
pregnancy, poor patient compliance, and laboratory inaccu-
racy. In addition, elderly patients appear to be more sensitive
to warfarin, possibly owing to decreased clearance of war-
farin with age. Because of this marked variability, continued
monitoring is required, and most patients require dosage
adjustments periodically. Initial monitoring should be per-
formed daily until therapeutic and then two or three times
weekly until the INR is stable. When the PT or INR is stable,
monitoring every 4 weeks is usually adequate, although more
frequent monitoring may increase the amount of time the
PT or INR is in the therapeutic range (time in therapeutic
range [TTR]). Intensity of therapy and TTR are important
determinants of therapeutic efficacy of warfarin. More fre-
quent monitoring is advisable for elderly patients, those who
take multiple medications, or those who are at higher risk for
bleeding.
Although patients taking warfarin are commonly
instructed to limit their intake of vitamin K–rich vegetables,
it is preferable to suggest that the intake of these vegetables
remain relatively constant in the diet because the nutritional
benefits of these foods unrelated to vitamin K may be impor-
tant. Numerous drugs influence the anticoagulant effect of
warfarin through multiple mechanisms, and bleeding unre-
lated to the anticoagulant effect of warfarin may result from
effects on other hemostatic pathways (eg, aspirin and other
antiplatelet drugs and heparin), as well as effects on intestinal
mucosa (eg, aspirin). Before beginning warfarin therapy—or
before adding new medications when a patient is taking
warfarin—a review of potential interactions should be
undertaken (readily available in pharmaceutical handbooks
such as the Physicians’ Desk Reference or other drug com-
pendiums). The frequency of monitoring should be
increased in patients taking warfarin whenever new medica-
tions are started to allow proper dose adjustments.
The decision to use long-term oral anticoagulation is
based on an assessment of the risk to the patient of bleeding
compared with the potential benefits related to its anticoag-
ulant effect. Warfarin is effective for management of multiple
thromboembolic conditions and is used when long-term
anticoagulation is required. Candidates for long-term anti-
coagulation include those with artificial heart valves, chronic
atrial fibrillation, left ventricular mural thrombus, recurrent
cerebrovascular ischemia, and antiphospholipid antibody
syndrome.
The role of warfarin is well established and accepted in
the prevention and treatment of VTE. Long-term use is effec-
tive for prevention of recurrent VTE. Treatment for 3–6
months reduces the risk of recurrent VTE compared with
shorter durations of treatment. Patients with temporary or
reversible risk factors for VTE, such as surgery or trauma,
have a lower risk of recurrence and can be managed with
3 months of warfarin. For patients with idiopathic VTE,
extended treatment duration beyond 6 months reduces the
risk of recurrence but carries an increased risk of serious
bleeding, and when discontinued, the risk of recurrence
increases. Therefore, treatment duration for patients with
idiopathic VTE must take into consideration individual
patient characteristics and preferences. Two years of warfarin
therapy has been shown to reduce the risk of recurrent VTE
significantly (from 8.6–2.2%) in the subset of patients with
factor V Leiden or prothrombin 20210A mutation compared
with 6 months. Patients with antiphospholipid antibodies
have an increased risk of recurrent VTE and mortality (29%
and 15%, respectively) and should be considered for
extended duration of treatment with warfarin. Patients with
cancer have a higher risk of recurrent VTE and also should be
considered for longer term treatment with warfarin. Following
a second VTE, indefinite anticoagulation with warfarin
reduces the risk of recurrence compared with 6 months of
therapy from 20.7–2.6% but is associated with a threefold
increase in the risk of major bleeding. Careful patient
selection and monitoring are needed to balance the benefits
of longer-duration anticoagulation with its risks.
Warfarin is effective for prevention of systemic or cere-
bral emboli in patients with atrial fibrillation, artificial heart
valves, left ventricular mural thrombus, or very low left ven-
tricular ejection fractions. It is also effective for long-term
treatment of patients with peripheral arterial embolism and
may prevent thrombosis of peripheral arterial bypass grafts
in high-risk patients. Antiplatelet agents are preferred over
warfarin for the prevention of acute myocardial infarction in
patients with peripheral arterial disease; for prevention of
stroke, recurrent infarction, or death in patients with acute
myocardial infarction; and for prevention of myocardial
infarction in men at high risk, but cardiac mortality is
reduced in the highest-risk patients by combining low-
intensity warfarin with aspirin. This combination carries a
risk of cerebral hemorrhage if blood pressure is not moni-
tored and controlled. Warfarin is not better than aspirin for
prevention of recurrent stroke, even in patients taking
aspirin at the time of the stroke, but is still recommended by
some neurologists for patients with recent noncardiac
embolic strokes or TIAs. Low-dose warfarin (0.5–1 mg/day)
is often used to prevent thrombosis of vascular access
catheters in cancer patients and to prevent thrombosis asso-
ciated with thalidomide therapy, but efficacy has not been
established for these situations.
The target INR for most indications is 2–3. A higher INR
(2.5–3.5) is recommended for patients with certain pros-
thetic heart valves (eg, tilting-disk and bileaflet mitral valves
and caged-ball or disk valves). Higher-intensity warfarin
may be considered for patients with recurrent VTE occur-
ring on therapeutic doses of warfarin or thrombosis associ-
ated with antiphospholipid antibodies (although this
remains controversial). Lower-intensity warfarin treatment
CHAPTER 39
834
(INR 1.5) is recommended when it is combined with aspirin
for prevention of fatal coronary events in patients at very
high risk.
Bleeding is the most common complication of warfarin
and is related to the intensity of the anticoagulation (espe-
cially in patients over 75 years of age), concomitant use of
aspirin, coexisting hemostatic defects (including renal fail-
ure), age over 75 years, history of GI bleeding, cancer, pres-
ence of anemia, and history of stroke or atrial fibrillation. If
GI bleeding or hematuria occurs when the INR is less than
3.0, an underlying GI or renal lesion should be suspected,
although spontaneous bleeding may occur when the INR is
in the high-intensity range or above. Prolonged use (lifelong)
also may increase the cumulative risk of bleeding. Patients
who consume excess alcohol or those who suffer from fre-
quent falls have a much higher risk of serious bleeding. There
are rare patients who have been identified to have mutations
in factor IX that cause an unusual susceptibility to bleeding
without prolongation of the INR.
Overdosage of warfarin (accidental or intentional) may
lead to serious bleeding. Management of hemorrhage associ-
ated with warfarin is similar to that encountered with
heparin in terms of using clinical criteria to determine the
urgency of the situation. Mild excess prolongation of the INR
(<5.0) without hemorrhage should be managed expectantly
by withholding warfarin until the INR returns to the desired
range and then resuming at a lower dose. Serious bleeding
may require immediate reversal with fresh-frozen plasma
(2–3 units) to provide functional vitamin K–dependent fac-
tors. Because vitamin K is a fat-soluble vitamin that is stored
in the liver, reversal of warfarin effects with vitamin K may
result in resistance to subsequent warfarin therapy. Low-dose
oral vitamin K
1
(phytonadione, 1–2.5 mg) will lower the INR
to less than 5 in patients with INR values between 5 and 9,
and 5 mg will correct INR values of greater than 9 in the
majority of patients within 24 hours without inducing war-
farin resistance. Intravenous vitamin K
1
should be reserved
for patients with an urgent need to reverse anticoagulation—
particularly patients with life-threatening hemorrhage not
controlled by fresh frozen plasma who will not require sub-
sequent warfarin therapy.
Patients receiving chronic warfarin therapy undergoing
invasive procedures likely to cause bleeding may require
interruption of warfarin. Depending on the patient’s risk for
perioperative thromboembolism, coverage with UFH or
LMWH may be necessary until the patient resumes warfarin.
Dental procedures may not require interruption of warfarin;
local hemostasis can be achieved with the use of topical
agents, such as tranexamic acid or aminocaproic acid
mouthwashes. Tables 39–8 and 39–9 summarize guidelines
proposed by the American College of Chest Physicians for
warfarin therapy (ie, dose, monitoring, adjustment, and peri-
operative management). Included in Table 39-9 are sug-
gested strategies for reversal of warfarin when time does not
permit withholding warfarin for several days (eg, for urgent
or emergent surgery).
Warfarin skin necrosis is a rare but serious complication
of warfarin, usually occurring 2–7 days after initiation of
warfarin therapy. Extensive thrombosis of venules and cap-
illaries of subcutaneous fat, particularly in the lower extrem-
ities, buttocks, or breast, appears to be most common in
patients who have an inherited or acquired deficiency of
Initial dose: 5 mg/d (lower in patients who are elderly, on multiple medications, malnourished, or have liver disease).
Check INR daily until therapeutic, then two or three times per week until stable, then every 4 weeks.
INR Intervention
Subtherapeutic Increase dose. Continue frequent monitoring until therapeutic.
Therapeutic (range based on underlying condition
requiring anticoagulation)
Continue current dose.
Between therapeutic range and 5 Omit dose. Resume at a lower dose when INR is therapeutic.
5.0–9.0, no bleeding Omit 1 or 2 doses. Resume at a lower dose when INR is therapeutic
OR give vitamin K
1
, 1–2.5 mg orally. Resume warfarin at reduced dose
when therapeutic.
>9.0, no bleeding Hold warfarin, give vitamin K
1
, 3–5 mg orally. Resume warfarin at
reduced dose when therapeutic.
>20.0
or
serious bleeding Hold warfarin. Give vitamin K
1
, 10 mg by slow intravenous infusion.
Supplement with fresh frozen plasma or prothrombin complex concen-
trate if needed.
Table 39–8. Administration and monitoring of warfarin.
ANTITHROMBOTIC THERAPY
835
protein C or protein S. Patients who are known to be defi-
cient in protein C or protein S should receive warfarin only
with simultaneous administration of heparin for at least
5 days to allow for depletion of all the vitamin K–dependent
coagulation proteins to prevent skin necrosis.
Warfarin is teratogenic, resulting in a fetal embryopathy
associated with multiple anomalies when is administered
during the first trimester of pregnancy (estimated incidence
7–28%). Warfarin crosses the placenta and may result in fetal
bleeding. Because of these negative fetal effects, warfarin is
contraindicated between weeks 6 and 12 of pregnancy, and
because it may cause fetal bleeding, it should be avoided near
term. Women of reproductive age who are taking warfarin
should be advised of the teratogenic effects of the drug, and
if pregnancy is contemplated, UFH or LMWH should be
substituted prior to pregnancy (except for women with
mechanical heart valves; see “Antithrombotic Therapy in
Pregnancy”). Warfarin does not cause anticoagulation in
infants who are breastfed by mothers taking warfarin.
Other infrequent side effects of warfarin include alopecia,
GI discomfort, rash, and liver dysfunction. In patients with
underlying arterial vascular disease, warfarin therapy has
been associated rarely with the development of atheroem-
bolic complications, including ischemic toes, livedo reticularis,
gangrene, abdominal pain, and renal and other visceral
infarctions owing to cholesterol emboli. Early reports sug-
gested that chronic warfarin therapy may increase the risk of
bone fractures and osteoporosis, but a meta-analysis of avail-
able studies failed to show a definite association.
Anisindione
Patients who cannot tolerate warfarin may be treated with
anisindione, an oral anticoagulant that is structurally unre-
lated to warfarin but works by a similar mechanism, namely,
inhibition of γ-carboxylation of the vitamin K–dependent
coagulation factors. The drug is well absorbed from the GI
tract, is highly protein-bound, and is metabolized to inactive
metabolites that are excreted in the urine. These metabolites
may cause a red-orange discoloration of the urine. The anti-
coagulant response of anisindione occurs within 20–72
hours, and it is cleared slowly from circulation with a half-life
of 3–5 days. Like warfarin, its anticoagulant effect can be
reversed by vitamin K and fresh-frozen plasma. Anisindione
crosses the placenta and causes fetal malformations and fetal
bleeding, so it should be avoided during pregnancy.
Anisindione is FDA approved for use in myocardial
infarction and venous thrombosis, but there is a lack of good
Low risk for thromboembolism (VTE >3 months ago or atrial
fibrillation without stroke risk factors)
Stop warfarin 4 days before surgery. Give heparin (UFH or LMWH) briefly at prophylactic
doses and resume warfarin simultaneously in the postoperative period.
Intermediate risk for thromboembolism Stop warfarin 4 days before surgery. Use low-dose UFH or prophylactic dose of LMWH
starting 2 days before surgery. After surgery, resume warfarin and continue heparin
until INR therapeutic.
High risk for thromboembolism (VTE <3 months ago; multiple
VTE; mechanical mitral valve; ball-and-cage prosthetic heart
valve)
Stop warfarin 4 days before surgery. Start full-dose intravenous or subcutaneous
heparin or LMWH when INR falls (usually about 2 days before surgery). Stop heparin before
surgery (5 hours for intravenous or 12 hours for subcutaneous UFH or LMWH). Resume
warfarin and continue heparin postoperatively until INR therapeutic.
Low risk of bleeding Continue warfarin at lowered dose (INR 1.3–1.5) for 4–5 days before surgery.
Resume full dose postoperatively. Use prophylactic dose of heparin until INR
therapeutic.
Dental procedures with low risk of bleeding Continue warfarin at usual dose and INR.
Dental procedures with higher risk of bleeding Continue warfarin at usual dose and INR. Use tranexamic acid or aminocaproic acid
mouthwash to control bleeding.
Urgent/emergent surgery (1–8 hours) Vitamin K 10 mg IV over 30 minutes and fresh frozen plasma (2–4 units depending
on INR < or >2.5).
Urgent/emergent surgery (8–12 hours) Vitamin K 10 mg IV over 30 minutes and fresh frozen plasma (2 units if INR >2).
Urgent/emergent surgery (12–24 hours) Vitamin K 10 mg IV or SC; UFH if high risk for thromboembolism until 6 hours before
surgery.
Urgent/emergent surgery (24+ hours) Vitamin K 10 mg SC if INR >2; UFH if high risk for thromboembolism until 6 hours
before surgery.
VTE = venous thromboembolism.
Table 39–9. Management of warfarin during invasive procedures.
CHAPTER 39
836
clinical studies to support its use as a substitute for warfarin
except for patients who are truly intolerant of warfarin. In
those patients, a loading dose of 300 mg on day one, 200 mg
on day two, and 100 mg on day three is followed by daily
maintenance of 50–250 mg, adjusted according to the INR.
Anisindione may cause myelosuppression, dermatitis, jaun-
dice, and renal insufficiency, which have limited its use.
Thrombolytic Therapy
Thrombolytic (fibrinolytic) agents differ from other
antithrombotic agents in that they actually dissolve estab-
lished clots rather than interfering with initiation and prop-
agation of thrombosis. The mechanism of action of these
agents is complex and involves many components of the nat-
urally occurring fibrinolytic system. Activation of plasmino-
gen to plasmin (the major fibrinolytic enzyme) is enhanced
by these drugs, accompanied by increased consumption of its
inhibitor (α
2
-antiplasmin). The net effect is an increase in
free plasmin, which results in degradation of fibrin and other
coagulation factors.
All the available agents cause varying degrees of systemic
activation of the fibrinolytic mechanism and therefore induce
generalized fibrinolysis and fibrinogenolysis and some degree
of platelet dysfunction owing to proteolysis of key membrane
receptors by plasmin, although some are more specific for
plasmin bound to clot (fibrin-specific). These drugs work best
when given soon after onset of symptoms (eg, within 3–4
hours in acute arterial thrombosis, 48 hours for pulmonary
thromboembolism, and 7 days for DVT), before thrombi are
highly cross linked and more resistant to thrombolysis.
Five thrombolytic agents are approved for use in the
United States. Selected features of these agents are outlined in
Table 39–10. Thrombolytic therapy may be used in the treat-
ment of acute arterial thrombosis, including myocardial
infarction and peripheral arterial occlusion, and in the treat-
ment of severe VTE (eg, massive pulmonary thromboem-
bolism with hemodynamic compromise, massive DVT, or
phlegmasia cerulea dolens). Thrombolysis can improve neu-
rologic function in patients with acute nonhemorrhagic stroke
if patients at high risk for bleeding are excluded and if
Drug
t
1⁄2
(min)
Fibrin-
Specific
Indications
(FDA-Approved)
Neutralizing
Antibodies
∗
Typical Dose
†
Estimated Cost
Alteplase 5 Yes
(2+)
Myocardial infarction, acute
cardiovascular accident, pul-
monary thromboembolism
No Myocardial infarction: 100 mg
infusion over 90 minutes to
3 hours; cerebrovascular
accident: 0.9 mg/kg (maxi-
mum 90 mg) infused over
60 minutes with 10% of total
dose given as an initial bolus
$2200
Tenecteplase 18–20 Yes
(3+)
Myocardial infarction. No Single bolus, 30–50 mg
depending on weight in kg
$2200
Reteplase 13–16 Yes
(1+)
Myocardial infarction No Two bolus injections, 10 units
each given 30 minutes apart
$2200
Streptokinase 20 No Myocardial infarction (intra-
venous or intracoronary),
deep vein thrombosis, pul-
monary thromboembolism,
catheter thrombosis, periph-
eral arterial occlusion
Yes 1.5 million units infused over
30–60 minutes intravenously
OR
20,000 units by intracoronary
bolus followed by 2000 to 4000
units/min for 30 to 90 minutes
$300
Urokinase 20 No Myocardial infarction (intra-
coronary), pulmonary
thromboembolism, catheter
thrombosis
No 6000 units/min infused intra-
coronary for up to 2 hours
OR
4400 units/kg infused over
10 minutes followed by 4400
units/kg/hr for 12 hours
OR
5000 units for catheter
thrombosis
$4000–$6000 (myocar-
dial infarction, pul-
monary embolus) $60
(catheter thrombosis)
∗
Presence of neutralizing antibodies precludes repeat use within 6–24 months, possibly longer, because of allergic reactions and decreased
effectiveness of the agent.
†
Doses may vary depending upon clinical situation.
Table 39–10. Comparison of selected fibrinolytic agents.
