Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


ANTITHROMBOTIC THERAPY
837
administered within 3 hours of onset of symptoms.
Thrombolytic agents are also used to reestablish patency of
clotted indwelling venous catheters and vascular grafts.
Indications, timing of administration, use of adjunctive
antithrombotic agents, and choice of specific agent for throm-
bolytic therapy are evolving. Thrombolysis reduces mortality
from acute myocardial infarction by about 20–50%. In
patients not undergoing percutaneous transthoracic coronary
angioplasty for acute myocardial infarction, alteplase may be
more effective than streptokinase. Bolus fibrinolytic agents,
reteplase and tenecteplase, are potentially advantageous
because they can be given quickly and could be available in the
prehospital setting. Reteplase appears to be equivalent in safety
and efficacy to alteplase, whereas tenecteplase has a somewhat
lower rate of major bleeding. Any available fibrinolytic agent
may be used with acute myocardial infarction. Although the
newer agents are much more expensive than streptokinase, the
contribution of drug costs to the overall cost of care—particu-
larly for acute myocardial infarction—has not been shown to
be significant. When cost-effective analyses have been done,
streptokinase appears to be marginally more cost-effective than
the other agents but should not be given to patients previously
treated with streptokinase owing to its antigenicity. Urokinase
is used primarily for dissolution of catheter thromboses.
The principal goal of fibrinolytic therapy is to reestablish
patency of an occluded blood vessel (or indwelling catheter).
Fibrinolytic therapy for myocardial infarction results in
angiographically confirmed patency about 50% of the time.
Additional antithrombotic therapy may be required to
improve reperfusion. The role of heparin combined with fib-
rinolytics for patients with acute myocardial infarction is
controversial, and the combination appears to be associated
with a high rate of major bleeding. Ongoing studies are
required to define the optimal use of heparin (UFH or
LMWH) or other anticoagulants such as the hirudin deriva-
tives and heparinoids in combination with fibrinolytic ther-
apy. Antiplatelet agents have been shown to be very
important as an adjunct to fibrinolytic therapy. Platelets play
a key role in the development of coronary thrombosis.
Aspirin and platelet GP IIb/IIIa inhibitors potentiate fibri-
nolysis and improve coronary artery patency rates, although
bleeding complications also may be increased when streptok-
inase is combined with GP IIb/IIIa inhibitors. Large trials
recently completed will provide additional information
about the safety and efficacy of various combinations of
antiplatelet agents and fibrinolytics in the treatment of acute
myocardial infarction. In addition, the combination of
reduced-dose fibrinolytic therapy with invasive coronary
interventions (eg, angioplasty) may improve outcomes.
Further study in this area is needed to define optimal dosing
to enhance coronary artery patency while maintaining an
acceptable rate of hemorrhage.
Alteplase is approved for use in acute nonhemorrhagic
stroke and is effective when administered intravenously
within 3 hours of the onset of symptoms. The risk of intra-
cerebral hemorrhage is 3%, but because it can lead to improved
neurologic function, this may be an acceptable risk. Only an
estimated 2% of all stroke patients are able to receive
alteplase within the 3-hour time frame, limiting its potential
impact on outcomes from stroke. Streptokinase increases
early mortality and intracerebral hemorrhage when used in
the treatment of acute stroke and is not recommended.
Recently, MRI to locate arterial occlusions, followed by
superselective intraarterial thrombolysis, has been suggested
as a potentially beneficial approach for patients with acute
stroke who are more than 3 hours from the onset of symp-
toms. This approach has an even higher risk of hemorrhage
(10% overall), but in centers equipped with a stroke unit and
all necessary personnel and technologic support quickly
available, it may prove to increase the number of patients
who could benefit from thrombolysis for acute stroke.
Fibrinolytic therapy is of limited value in the treatment of
massive PE. Hemodynamic instability and radiographic
changes improve more rapidly than with anticoagulation
only, but there does not appear to be any significant
improvement in overall outcome compared with anticoagu-
lation alone. Fibrinolytic therapy of PE should be considered
for patients with hemodynamic instability, severe gas-
exchange abnormalities, or significant impairment in right
ventricular function. Echocardiography to assess right ven-
tricular function plays a key role in determining the potential
benefit of fibrinolytic therapy or other means of reducing
clot burden (eg, thromboembolectomy). Fibrinolytic therapy
for DVT has not improved outcome over anticoagulation in
most patients, with the possible exception of patients with
severe venous occlusion and threatened gangrene of the
limb. Despite a high rate of clot lysis, there is no good evi-
dence that thrombolytic therapy reduces the rate of post-
phlebitic syndrome following DVT. Furthermore,
hemorrhagic complications are much higher than with stan-
dard anticoagulation in the treatment of VTE.
Fibrinolytic therapy is effective in the treatment of acute
arterial thrombus in medium and large peripheral arteries. A
fibrinolytic agent administered through a catheter proximal
to the clot dissolves it completely about 75% of the time.
Catheter-directed intraarterial administration appears to be
superior to intravenous administration. Thrombolysis
should be considered prior to revascularization surgery as
long as the affected limb is still salvageable. Surgery can be
avoided in 35% of these patients, and overall mortality
appears to be somewhat better than with immediate surgery.
Urokinase, 5000 units, may be instilled into an occluded
venous catheter without excessive pressure, which could dis-
lodge the clot or rupture the catheter. Because venous
catheters may be occluded by substances other than clots (eg,
drug precipitate), urokinase is not always effective.
The most common complication of thrombolytic therapy
is hemorrhage (3–40%). Hemorrhagic complications can be
minimized if patients are selected properly and monitored
carefully. The use of other antithrombotic agents—particularly
heparin—increases the risk of bleeding. Contraindications to
thrombolytic therapy include major ischemic changes or

CHAPTER 39
838
signs of intracranial hypertension on CT scan, seizure at the
onset of a stroke, previous stroke or serious head injury
within the preceding 3 months, active or recent visceral
bleeding, aortic dissection, major surgery, trauma, arterial or
lumbar puncture in the preceeding 2 weeks, severe uncon-
trolled hypertension (>180/110 mm Hg), significant throm-
bocytopenia (platelet count <100,000/μL), signs of
pericarditis, pregnancy, recent retinal laser surgery, cardio-
genic shock (except when owing to massive PE), and the use
of heparin with a prolonged aPTT or oral anticoagulants
resulting in an INR greater than 1.5. Thrombolytic therapy
results in decreased plasma fibrinogen concentration and
increased fibrin degradation products, but these tests are not
predictive of efficacy or clinical bleeding. The bleeding time,
if prolonged, may correlate with minor bleeding but is not
usually monitored.
The thrombin time is the best laboratory test for moni-
toring the status of the fibrinolytic system. When the throm-
bin time is prolonged more than five to seven times normal,
the incidence of bleeding complications increases signifi-
cantly. Intracerebral hemorrhage is more common in patients
who are elderly or underweight, who have prior neurologic
disease, or who are receiving antithrombotic drugs. Women
appear to have a higher risk of intracerebral hemorrhage. If
major bleeding occurs with thrombolytic therapy, the drug
should be stopped immediately. Hypofibrinogenemia can
be reversed with cryoprecipitate, and aminocaproic acid
can be given to inhibit plasmin activity. If the patient is
receiving heparin, protamine sulfate can be used to reverse
its effect.
Other potential adverse reactions to certain thrombolytic
agents (eg, streptokinase and anistreplase) include allergic
reactions and the development of neutralizing antibodies
that preclude repeated usage for 6–24 months and perhaps
longer. Cholesterol emboli rarely may complicate throm-
bolytic therapy, resulting in the “purple toe syndrome” and
multiorgan failure. Arrhythmias may accompany reperfusion
of an ischemic myocardium.
Antithrombotic Therapy in Pregnancy
Pregnancy and the postpartum period pose special chal-
lenges in the management of thromboembolic disorders. In
addition to the apparent increased risk of venous thrombo-
embolic events, certain pregnancy complications (eg, fetal
loss, preeclampsia, abruption, fetal growth retardation, and
intrauterine death) are associated with maternal throm-
bophilias (eg, antiphospholipid antibodies, factor V Leiden,
prothrombin gene mutation, antithrombin deficiency, and
hyperhomocysteinemia). In addition, women who are taking
warfarin for preexisting conditions (eg, venous thromboem-
bolism or mechanical heart valves) require continued
antithrombotic therapy during this higher-risk period.
Warfarin is contraindicated between 6 and 12 weeks of preg-
nancy because of its teratogenicity and because it may
increase the risk of fetal bleeding. UFH does not cross the
placenta and appears to be safe and effective during preg-
nancy. LMWH and danaparoid have a lower risk of osteo-
porosis and thrombocytopenia than UFH. Dosing may be
adjusted for increasing weight, or anti–factor Xa levels
(drawn 4 hours after morning dose) can be monitored (tar-
get range 0.5–1.2 units/mL). Because these agents do not
cross the placenta, fetal bleeding is not a complication; how-
ever, there have been recent reports of congenital anomalies
with some of the LMWH preparations (eg, enoxaparin and
tinzaparin), and there has been insufficient clinical experi-
ence with danaparoid during pregnancy to determine its ter-
atogenicity. Maternal bleeding occurs with the same
frequency as in other situations requiring anticoagulation
(major bleeding, about 2%). Bleeding can complicate deliv-
ery. The aPTT may not adequately reflect the anticoagula-
tion effect of UFH because of increased factor VIII and
fibrinogen that occurs during pregnancy. When possible,
UFH or LMWH should be discontinued 24 hours before
labor (eg, when electively induced). UFH and LMWH are
not secreted in breast milk, and warfarin does not appear to
cause an anticoagulant effect in babies who are breastfed by
mothers taking warfarin. Guidelines for the management of
antithrombotic agents during pregnancy are outlined in
Table 39-11.
The use of heparin (UFH and LMWH) during pregnancy
appears to be effective for prophylaxis and treatment of VTE.
In women with mechanical heart valves, heparin is not be as
effective as warfarin for prevention of thromboembolic com-
plications, particularly if the aPTT is only moderately ele-
vated. Choices for anticoagulation in these women include
using warfarin (target INR 3.0), except for weeks 6–12 and
near delivery, when UFH can be substituted, to prevent fetal
embryopathy or bleeding, or to use UFH throughout preg-
nancy. If UFH is used, it is imperative that high doses be used
and that the aPTT (6 hours after subcutaneous injection) is
monitored closely. The addition of low-dose aspirin (81–162
mg/day) may reduce the risk of thrombosis but also increases
the risk of bleeding. Maternal and fetal deaths from throm-
botic complications have been reported when enoxaparin
was used for thromboprophylaxis in pregnant women with
prosthetic heart valves; however, the incidence of this com-
plication is not known. The optimal approach for manage-
ment of anticoagulation for women with mechanical valves
during pregnancy is not clear owing to a lack of sufficient
clinical trials.
Low-dose aspirin appears to be safe when administered in
the second and third trimesters to modestly reduce the risk
of preeclampsia and intrauterine growth retardation in high-
risk women and appears to be safe for both mother and fetus.
Additional studies are required to determine the optimal
selection of patients, timing, and dose of aspirin therapy.
Low-dose aspirin combined with heparin reduces the risk of
miscarriage in women with the antiphospholipid antibody
syndrome and recurrent miscarriage, but it is uncertain
whether this strategy is effective in women with other throm-
bophilic conditions.
ANTITHROMBOTIC THERAPY
839
Women at high risk for thromboses during pregnancy,
such as those with prior VTE, inherited thrombophilic disor-
ders, and antiphospholipid antibody syndrome (without
prior thrombosis or miscarriage), should be considered for
prophylactic anticoagulation with UFH or LMWH during
pregnancy and the postpartum period. Determining the
optimal management strategy for these patients is difficult
because there are inadequate data available to support spe-
cific recommendations. A discussion of the potential risks
and benefits, known and uncertain, with each patient must
be undertaken at the onset of pregnancy.
Antiphospholipid Antibody Syndrome
Significant thrombotic events in the presence of the
antiphospholipid antibody syndrome (APLA) pose special
therapeutic challenges. Acute management with heparin may
be complicated by baseline elevation in the aPTT. If baseline
aPTT is prolonged, monitoring should be performed using a
specific heparin assay that depends on factor Xa inhibition
(therapeutic range 0.3–0.7). LMWH can be used without the
need for laboratory monitoring. The optimal intensity and
duration of warfarin therapy (following initial therapy with
UFH or LMWH) for these patients is unclear, but higher-
intensity warfarin (INR at least 3) is probably superior to
lower-intensity warfarin, and longer-duration therapy (2–4
years) offers a lower rate of recurrence than 6 months of
anticoagulation. Low-dose aspirin (81 mg daily) should be
added to oral anticoagulation for arterial thrombosis or for
recurrent VTE despite adequate oral anticoagulation.
Heparin therapy (UFH or LMWH) has been advocated by
some for patients with APLA syndrome, but there is no direct
evidence that it is superior if INR is monitored and adjusted
carefully. Some patients also have hypoprothrombinemia,
with baseline prolongation of the PT, which makes monitor-
ing with INR unreliable. Coagulation tests that are insensi-
tive to the lupus anticoagulant may be required in these
patients (eg, prothrombin-proconvertin test or chromogenic
factor X level). Corticosteroids and immunosuppressive
agents may improve coagulation abnormalities, but the ben-
efits are usually short-lived. If patients have multisystem
involvement, corticosteroids, immunosuppressives, and
plasmapheresis may be beneficial; however, ongoing treat-
ment of the thrombotic diathesis with anticoagulation is
advisable. Management of APLA syndrome during preg-
nancy was discussed earlier.
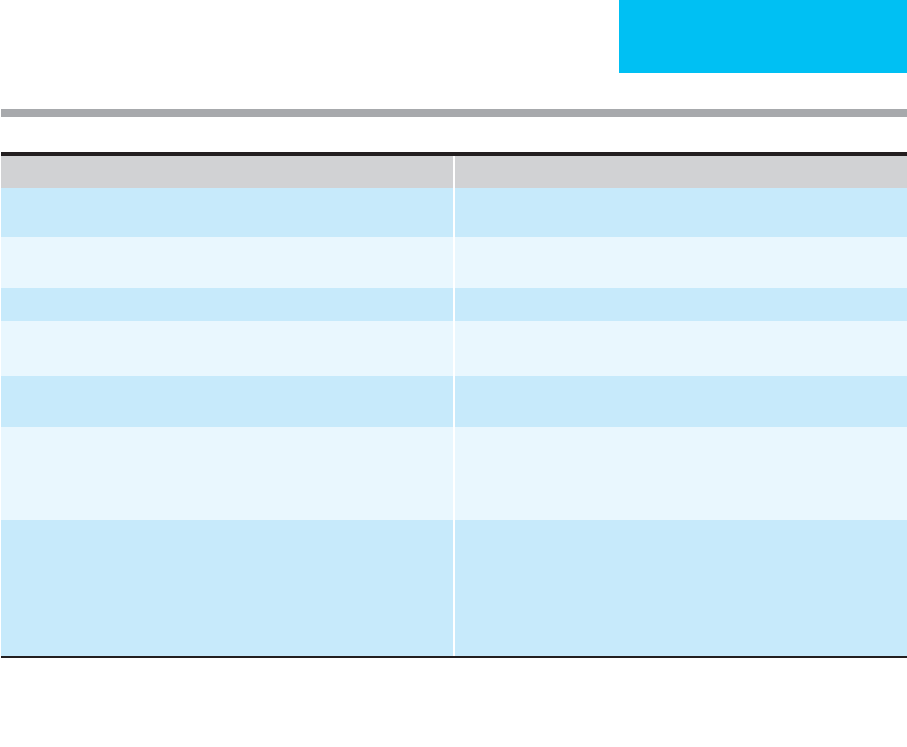
Table 39–11. Antithrombotic therapy during pregnancy.
Clinical Situation Recommendation
Women on long-term anticoagulation who wish to become pregnant Frequent pregnancy tests; convert to LMWH or adjusted-dose UFH once
pregnant
VTE during pregnancy LMWH or adjusted-dose UFH throughout pregnancy and for at least
6 weeks postpartum
Prior VTE with transient risk factors
∗
Close surveillance during pregnancy; postpartum anticoagulation
†
Prior VTE with thrombophilia or family history
∗
Low- to moderate-dose UFH or LMWH throughout pregnancy; postpartum
anticoagulation
Multiple prior VTE
∗
LMWH or adjusted-dose UFH throughout pregnancy; resume long-term
anticoagulation postpartum
Thrombophilia without history of VTE No clinical data to support specific recommendation; consider prophylaxis
for patients with AT deficiency, factor V Leiden or prothrombin G20210A
heterozygotes, homozygous factor V Leiden or prothrombin G20210A
mutation
Mechanical heart valve Options:
1. LMWH, monitor anti-Xa activity
2. Adjusted-dose UFH
3. LMWH or adjusted-dose UFH until week 13; warfarin until mid-third
trimester, resume LMWH or UFH until term
4. Consider adding aspirin, 75–162 mg/day for high-risk women
∗
Recommendations should be individualized; very low recurrence of VTE in small study of these patients.
†
All pregnant women with history of VTE should consider use of graduated compression stockings throughout pregnancy and postpartum.
CHAPTER 39
840
Immunologically mediated thrombocytopenia is com-
mon in APLA syndrome but generally is mild and does not
require treatment. When severe thrombocytopenia
(<20,000/μL) is present, increased bleeding during anticoag-
ulation may occur. Treatment as for other immune thrombo-
cytopenias should be given to achieve a reasonable platelet
count (ie, >50,000/μL) to decrease the risk of serious hemor-
rhage with concomitant anticoagulation. Catastrophic APLA
syndrome (eg, multiorgan and bowel thrombosis, gangrene,
livedo reticularis, and stroke) requires aggressive therapy
with anticoagulation, plasmapheresis, and immunosuppres-
sive agents but is associated with a high rate of mortality
despite these measures.
Thrombosis in Cancer Patients
The risk of thrombosis in patients with cancer is significant
and is due to several factors, many of which may be present
simultaneously: activation of coagulation by tumors, throm-
bocytosis, tumor angiogenesis, trapping of cancer cells in the
microcirculation of organs, treatment (ie, chemotherapy and
hormonal therapy), indwelling vascular catheters, obstruc-
tion of venous and lymphatic channels, surgical procedures,
and limited mobility. Postoperative VTE is much higher in
patients undergoing cancer surgery, and recurrence of VTE
after completion of anticoagulation is more common in
patients with cancer. Patients undergoing major cancer sur-
gery, especially when associated with prolonged immobility,
should be considered for thromboprophylaxis with LMWH
postoperatively. Extending the duration of prophylaxis from
8–10 days to 4 weeks reduces the risk of VTE from 12–4.8%.
LMWH may be superior to warfarin for the treatment of
established VTE in cancer patients, reducing the rate of treat-
ment failure and improving survival. Studies have shown
conflicting results with LMWH therapy for patients with
advanced malignancy without established VTE. There may
be a small survival advantage for selected patients with bet-
ter initial prognosis, but the risks of bleeding, cost, and
inconvenience to the patient must be considered before initi-
ating therapy. Prevention of catheter-associated thrombosis
has not been studied adequately, but low-dose warfarin ther-
apy may be considered for patients at high risk of clotting.
Patients receiving therapy associated with an increased rate
of thrombosis should be educated about symptoms of VTE
and monitored closely. Prophylactic dose LMWH may be
useful for the prevention of thrombosis associated with thali-
dodmide therapy for multiple myeloma, whereas low-dose
warfarin, although used frequently, has not yet been shown
to be effective.
Future Directions
There are several exciting active areas of research in the
field of antithrombotic therapy. Many new agents are in
various stages of development. Modifications of existing
antithrombotic agents may serve to increase the predictabil-
ity of anticoagulant effect, improve bioavailability and con-
venience, and decrease complications. Combinations of
various antithrombotic agents are under investigation in an
attempt to improve efficacy while maintaining an acceptable
risk for hemorrhage.
Several classes of anticoagulants are under active inves-
tigation: inhibitors of the factor VIIa–tissue factor pathway,
factor Xa inhibitors, and direct thrombin inhibitors. One of
the most promising agents had been an orally active throm-
bin inhibitor, ximelegatran. The development of an orally
active agent with a more predictable anticoagulant response
would be a major advance over warfarin for the outpatient
management of thromboembolic disease. Ximelegatran is
metabolized to melagatran (the active agent), has a pre-
dictable anticoagulant response at a fixed dose, and does
not require monitoring. It had been shown to be effective
and safe for postoperative thromboprophylaxis and treat-
ment of VTE, atrial fibrillation, and acute coronary syn-
dromes (combined with aspirin). Unfortunately, liver
toxicity led to this drug being withdrawn from the market
worldwide in 2006.
In addition to new anticoagulants, attempts to augment
the naturally occurring anticoagulant pathway of protein C
and the fibrinolytic system may prove useful. Recombinant
activated protein C has been tested in patients with sepsis
and has been shown to decrease mortality; however, it may
increase the risk of bleeding. New antiplatelet agents, includ-
ing additional platelet GP IIb/IIIa receptor inhibitors, are
also being studied.
While endeavoring to improve the benefit-risk ratio of
antithrombotic therapy, cost-effectiveness holds major
importance in the future of antithrombotic therapy. The
indications for antithrombotic therapy are continuously
expanding, and the cost of many new agents is very high.
It is important that any new antithrombotic drug be com-
pared with older, established therapies, with demonstra-
tion of definite advantage, before changing the standard
of care for patients with or at risk for thromboembolic
disease.
REFERENCES
Di Nisio M, Middeldorp S, Buller HR: Direct thrombin inhibitors.
N Engl J Med 2005;353:1028–40. [PMID: 16148288]
Ginsberg JS et al: Anticoagulation of pregnant women with mechan-
ical heart valves. Arch Intern Med 2003;163:694–8. [PMID:
12639202]
Gurewich V: Ximelagatran: Promises and concerns. JAMA
2005;293:736–9. [PMID: 15701916]
Hirsh J et al: The Seventh ACCP Conference on Antithrombotic and
Thrombolytic Therapy: Evidence-based guidelines. Chest
2004;126:163–703S.
Hirsh J, O’Donnell M, Weitz JI: New anticoagulants. Blood
2005;105:453–464. [PMID: 15191946]

ANTITHROMBOTIC THERAPY
841
Kearon C et al: Comparison of low-intensity warfarin therapy with
conventional-intensity warfarin therapy for long-term prevention
of recurrent venous thromboembolism. N Engl J Med
2003;349:631–9. [PMID: 12917299]
Lee AY et al: Low-molecular-weight heparin versus a coumarin for
the prevention of recurrent venous thromboembolism in
patients with cancer. N Engl J Med 2003;349:146–53. [PMID:
12853587]
Lee AY et al: Randomized comparison of low molecular weight
heparin and coumarin derivatives on the survival of patients with
cancer and venous thromboembolism. J Clin Oncol
2005;23:2123–9. [PMID: 15699480]
Lemoine NR: Antithrombotic therapy in cancer. J Clin Oncol 2005;23:
2119–20. [PMID: 15699474]
McIntosh BA: Developing an algorithm for treating heparin-induced
thrombocytopenia. Clin Adv Hematol Oncol 2004;2:216–22.
[PMID: 16163184]
Otzurk MA et al: Current debates in antiphospholipid syndrome:
The acquired antibody-mediated thrombophilia. Clin Appl
Thromb Hemost 2004;10:89–126. [PMID: 15094931]
Selleng K, Warkentin TE, Greinacher A: Heparin-induced thrombo-
cytopenia in intensive care patients. Crit Care Med
2007;35:1165–76.[PMID: 17334253]
Seshadri N et al: The clinical challenge of bridging anticoagulation
with low-molecular-weight heparin in patients with mechanical
prosthetic heart valves: An evidence-based comparative review
focusing on anticoagulation options in pregnant and nonpreg-
nant patients. Am Heart J 2005;150:27–34. [PMID: 16084147]
This page intentionally left blank
Index
A
Abacavir, 315t
Abciximab, 825
Abdominal trauma, 132–133
Abortion, septic, 813
Abruptio placentae, 820
Abscess
brain, 678
hepatic, 372t
intraabdominal, 177–179, 178f, 372t, 405
lung, 147–148, 148f
pancreatic, 179, 180, 350, 372t
periannular, 368
perinephric, 366
renal, 366, 368
soft tissue, 407, 408t
splenic, 368
Absence seizures, 663, 663t. See also Seizures
ACE (angiotensin-converting enzyme) inhibitors
adverse effects, 497
after acute myocardial infarction, 509
for heart failure, 468, 471, 472, 510
nephrotoxicity, 316t
Acetaminophen poisoning/overdose, 771–773, 772f
Acetate, 123t
Acetazolamide, 66, 295
Acetylcysteine
for acetaminophen overdose, 772–773
for acute respiratory failure, 264
for inhalation injury, 746
Acetylprocainamide, 92t
Acid-base homeostasis
in acute renal failure, 331
buffering systems, 56–57
disorders, 58–59, 58t, 59f, 59t. See also Metabolic acidosis; Metabolic
alkalosis; Respiratory acidosis; Respiratory alkalosis
renal functions in, 57–58
respiratory function in, 58
Acinetobacter baumanii, 376t, 391
Acitretin, 624
Acquired immunodeficiency syndrome (AIDS). See Human
immunodeficiency virus (HIV) disease
Acticoat, 736
Activated charcoal, for poisonings, 756, 756t
Activated partial thromboplastin time (aPTT), 409, 411t
Activated protein C. See Drotrecogin alfa
Acute abdomen
clinical features, 697–698, 697t
controversies and unresolved issues
activated protein C and corticosteroids in sepsis, 701
bacterial translocation and enteral feedings, 701
laparoscopy, 702
monoclonal antibodies, 702
endoscopy, 699
imaging studies, 698–699
pathophysiology, 696
peritoneal lavage, 699
physiologic considerations, 696
postoperative, 699
specific pathologic entities
abdominal compartment syndrome, 701
cholecystitis. See Cholecystitis
colonic pseudo-obstruction (Ogilvie’s syndrome), 172,
355–356, 701
enteric fistula. See Gastrointestinal tract, fistulas
intraabdominal abscess. See Intraabdominal infections/abscess
small bowel obstruction. See Small bowel obstruction
treatment, 700
Acute arterial insufficiency
clinical features, 634–635, 634t, 635t
controversies and unresolved issues, 639
differential diagnosis, 636
general considerations, 632
imaging studies, 635
pathophysiology, 632–634, 633t
prognosis, 639
treatment
anticoagulation, 636
platelet-active agents, 636
rheologic agents, 636
supportive care, 638–639
surgery, 638
thrombin inhibitors, 636–637, 637t
thrombolytic agents, 637–638, 638t
Acute fatty liver of pregnancy, 809–810
Acute limb ischemia. See Acute arterial insufficiency
Acute lung injury (ALI), 296–297. See also Acute respiratory
dist
r
ess syndrome
Acute mesenteric ischemia
clinical features, 174, 649
differential diagnosis, 650
essentials of diagnosis, 648
general considerations, 648
imaging studies, 174–175, 175f, 649–650
pathophysiology, 174, 648–649
postoperative, 655
prognosis, 650–651
treatment, 650
Acute myocardial infarction
hypomagnesemia and, 49
non-ST-segment-elevation (non-STEMI)
clinical features, 503
essentials of diagnosis, 502
evaluation of stabilized patient, 503
general considerations, 502–503
treatment, 503–504, 505t
ST-segment elevation (STEMI)
clinical features, 506
complications, 509–512. See also Cardiogenic shock
differential diagnosis, 507
Page numbers followed by f or t indicate figures or tables, respectively.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.

INDEX
844
Acute myocardial infarction, ST-segment elevation (STEMI) (Cont.):
essentials of diagnosis, 505
general considerations, 506
imaging studies, 506–507
treatment, 507–509
thyroid function in, 577–578
Acute radiation syndrome, 800–801
Acute respiratory distress syndrome (ARDS)
in acute pancreatitis, 348
acute renal failure in, 327t
barotrauma in, 163f, 166–167
clinical features, 299–301, 299t
controversies and unresolved issues
fluid management, 308
periodic lung recruitment, 309
prone positioning, 309
routine use of PV curves, 309
definition, 296, 296t
in diabetic ketoacidosis, 592–593
differential diagnosis, 301, 301t
essentials of diagnosis, 295
general considerations, 5t, 295–296
imaging studies, 160–161, 161f, 162f, 163f, 164f, 301
multiple organ system failure in, 299–300
pathophysiology, 296–298
physiologic manifestations
altered lung mechanics, 298–299, 299f
increased airway resistance, 299
refractory hypoxemia, 298, 298f
prognosis, 307–308
treatment
infection treatment and prevention, 307
mechanical ventilation
extracorporeal membrane oxygenation, 306–307
inverse-ratio ventilation, 306
lower tidal volume strategy, 304–306, 304t, 305f
partial liquid ventilation, 307
pressure-controlled ventilation, 306
ventilator strategies and tactics, 274t
volume-present ventilation, 306
oxygen therapy, 302
pharmacologic therapy, 307
positive end-expiratory pressure, 302–304, 303f
reminders, 5t
supportive care, 307
Acute respiratory failure
in acute pancreatitis, 348
in ARDS. See Acute respiratory distress syndrome
in asthma. See Status asthmaticus
in COPD. See Chronic obstructive pulmonary disease
hypercapnic
clinical features, 249, 249t
pathophysiology, 248–249, 249f
treatment considerations, 253–254
hypoxemic
clinical features, 249t, 252
pathophysiology, 250–252, 250t
treatment considerations, 254
in neuromuscular disorders. See Neuromuscular disorders
in obesity-hypoventilation syndrome, 311, 313
in obstructive sleep apnea. See Obstructive sleep apnea
oxygen delivery and tissue hypoxia in, 252–253
temperature and blood gases in, 253
in thoracic wall disorders. See Thoracic wall disorders
treatment. See also specific disorders
airway management
endotracheal intubation. See Endotracheal intubation
natural vs. artificial, 254
obstruction, 254
bronchodilators
anticholinergics, 261–262
beta-adrenergic agonists, 260–261
magnesium sulfate, 262–263
mechanisms of action, 260
theophylline, 262
chest physiotherapy, 264–265
corticosteroids, 263
expectorants, 264
leukotriene antagonists and inhibitors, 264
mechanical ventilation. See Mechanical ventilation
oxygen therapy
complications, 259–260
delivery devices, 258–259, 259t
inspired oxygen concentration, 257–258, 258f
oxygen saturation and oxygen content, 257, 257f
Pa
O
2
and P(
A
-a)
O
2
, 257
respiratory stimulants, 264
sedatives and muscle relaxants, 264
Acute tubular necrosis. See also Renal failure, acute
causes, 94t, 322t, 325
clinical features, 325
treatment, 325–326
Acyclovir, 315t, 627
Adenosine, 486
ADH (antidiuretic hormone), 23, 24–25
Adhesions, abdominal, 352
Adrenal insufficiency, acute
clinical features, 573–574
controversies and unresolved issues, 576
essentials of diagnosis, 572
general considerations, 572
pathophysiology, 572–573
treatment, 574–576, 575t
Adrenocorticotropic hormone (ACTH),
464, 574
Advance health care directive, 217
Adynamic ileus. See Ileus
AICD (automatic implantable cardioverter defibrillator)
imaging studies, 143
presence in ICU patients, 491
for ventricular arrhythmias, 491
AIDS. See Human immunodeficiency virus (HIV) disease
Air embolism, 141, 195, 199
Air plethysmography, 635
Aircraft, for critical care transport, 210
Airway management
artificial airways for, 101
endotracheal intubation for. See Endotracheal intubation
during interfacility transport, 211–212
intermediate airways for, 102
laryngeal mask airway for, 102
mechanical maneuvers, 101

INDEX
845
in prolonged mechanical ventilation, 103
surgical, 103
Airway resistance
anesthesia and, 99
in ARDS, 299
in mechanical ventilation, 268
Albendazole, for cysticercosis, 677
Albumin. See also Serum albumin
for hypovolemic shock, 229
for nephrotic syndrome, 76t
for nutrition support, 135
synthesis, 119
Albuterol
for acute respiratory failure, 260, 261
for hyperkalemia in renal failure, 42
for status asthmaticus, 537
Alcohol intoxication, 226
Alcoholic hepatitis, 131
Alcoholic ketoacidosis, 61t, 62
Aldosterone, in hypovolemic shock, 224
Aldosterone deficiency, 40
Alfentanil, 111t, 113
ALI (acute lung injury), 296–297. See also Acute respiratory
distress syndrome
Allergic reactions, transfusion-related, 83t
Alloimmunization, red blood cells, 80
Allopurinol, 316t
Alpha-adrenergic agents, 237, 241
Alpha
1
-antitrypsin concentrate, 76t
Alpha
2
-antiplasmin, 410t
Alteplase, 836t. See also Thrombolytic therapy
for acute arterial insufficiency, 637, 638t
for deep venous thrombosis, 646
for pulmonary embolism, 558
for stroke, 676, 676t
Altered mental status, in diabetic ketoacidosis, 584, 584f
Alveolar hypoventilation, 248
Ambulance transport, 209–210, 209t
Amebic meningoencephalitis, 677
American Burn Association, burn center referral guidelines, 724t
American Hospital Association, patient’s bill of rights, 215, 216t
Amikacin, 92t
Aminocaproic acid, 76t, 417, 524, 688
Aminoglycosides
nephrotoxicity, 315t
nutrient deficiencies caused by, 124t
once-daily dosing, 399
resistance to, 376t
Amiodarone
in acute myocardial infarction, 508
adverse effects, 496
for atrial fibrillation, 488
therapeutic ranges, 92t
for ventricular tachycardia, 491
Amlodipine, 501
Ammonium chloride, 124t
Amniotic fluid embolism, 811
Amphotericin B
for cryptococcal pneumonia, 604
electrolyte abnormalities and, 95
for hematogenously disseminated candidiasis, 389
hypokalemia and, 36
lipid formulations, 377–378
nephrotoxicity, 315t
protein binding, 89t
Ampicillin, 339t, 376t
Amplitude ratio, 191f, 192f
Amrinone, 244
Amyotrophic lateral sclerosis, 283
Anabolic steroids, 135
Anaerobic threshold, 223
Anaphylactic shock, 238–240, 239t
Anaphylactoid reactions, 239, 239t
Anaphylaxis, 562–564
Ancrod, 832
Anemia
chronic, 71–72
hemolytic, 73
sickle cell, 73
Anesthesia
airway effects, 97
cardiovascular effects, 97–98
hypothermia and, 100–101
inhaled, 97–100
intravenous agents, 114
regional, 98, 100
respiratory effects, 98–100
Aneurysms
great vessels
clinical features, 516
differential diagnosis, 516–517
essentials of diagnosis, 514
general considerations, 514–515, 515f
imaging studies, 516
treatment, 517
intracranial, rupture of. See Subarachnoid
hemorrhage
mycotic, 368
Angina pectoris
stable. See Myocardial ischemia
unstable. See Unstable angina pectoris
Angiodysplasia, 711
Angioedema, 564–565
Angiography
in acute arterial insufficiency, 635
in acute mesenteric ischemia, 175, 649
in aortic dissection, 516
cerebral, 684–685, 687
in lower gastrointestinal bleeding, 712
pulmonary. See Pulmonary angiography
Angiotensin receptor blockers, 316t
Anidulafungin, 378
Anion gap, 60. See also Metabolic acidosis
Anisindione, 835–836
Ankle-brachial index (ABI), 635
Ankylosing spondylitis, 286
Antacids, 124t
Anterior cord syndrome, 691, 693
Anti-D immune globulin, 76t
Antibiotics
for A. baumanii, 391
for burn wound infection, 737

INDEX
846
Antibiotics (Cont.):
for community-acquired pneumonia, 364–365, 365t
for COPD exacerbations, 292–293
for dialysis-related peritonitis, 339t
duration of treatment, 399
for extended-spectrum β-lactamases, 390–391
for group 1 β-lactamases, 391
guidelines for use, 376–378, 391–392
for infections in neutropenic patients, 374
for infective endocarditis, 368–369
for intraabdominal infections, 372t, 373
for methicillin-resistant S. aureus, 390
for necrotizing fasciitis, 371
nephrotoxicity, 315t
for nosocomial pneumonia, 381
prophylactic
for surgical infections, 397
in upper gastrointestinal bleeding, 709
resistance to, 376, 376t, 389–391
routes of administration, 399, 402
for sepsis, 362
for urinary catheter–associated infections, 383
for urinary tract infection, 367
for vancomycin-insensitive S. aureus, 390
for vancomycin-resistant enterococci, 389
for vancomycin-resistant S. aureus, 390
Anticholinergics
for acute respiratory failure, 261–262, 291–292
poisoning/overdose, 753t
for status asthmaticus, 537
Anticholinesterases, 110
Anticoagulants, in hemostasis, 410t
Anticoagulation therapy. See Antithrombotic therapy
Anticonvulsants, 665–666, 665t
Antidiuretic hormone (ADH), 23, 24–25
Antifibrinolytic agents, 76t, 417, 524, 688
Antihistamines, 563, 565
Antihypertensives
after acute myocardial infarction, 509
after vascular surgery, 653–654
for hypertensive crisis, 481–482
nephrotoxicity, 316t
poisoning/overdose, 767–768
Antiphospholipid antibody syndrome, 839–840
Antiplatelet agents, 821–822
aspirin. See Aspirin
clopidogrel. See Clopidogrel
cyclooxygenase inhibitors, 822
glycoprotein IIb/IIIa receptor inhibitors. See Glycoprotein
IIb/IIIa receptor inhibitors
nephrotoxicity, 316t
for stroke, 674
ticlopidine, 316t, 823–824, 824t
Antipsychotics
atypical, for delirium, 435
Antithrombin, 410t
Antithrombin II concentrate, 76t
Antithrombotic therapy
for acute arterial insufficiency, 636
anisindione, 835–836
anticoagulants
defibrinating agents, 832
direct thrombin inhibitors, 831
indirect thrombin inhibitors, 831–832
low-molecular-weight heparin. See Low-molecular-weight
heparin
unfractionated heparin. See Unfractionated heparin
warfarin. See Warfarin
in antiphospholipid antibody syndrome, 839–840
antiplatelet agents, 821–822
aspirin. See Aspirin
clopidogrel. See Clopidogrel
cyclooxygenase inhibitors, 822
glycoprotein IIb/IIIa receptor inhibitors. See Glycoprotein
IIb/IIIa receptor inhibitors
nephrotoxicity, 316t
ticlopidine, 316t, 823–824, 824t
in canc
er patients,
840
in continuous renal replacement therapy, 341–342
for deep venous thrombosis/pulmonary embolism
prophylaxis, 644–645
treatment, 554–557, 645, 646t
defibrinating agents, 832
dextrans. See Dextrans
future directions, 840
in hemodialysis, 337
phosphodiesterase III inhibitors, 532, 825
physical measures, 558, 561, 647, 821
in pregnancy, 827t, 838–839, 839t
in stroke, 674
for unstable angina or non-STEMI, 504, 505t
Antithyroid drugs, 568, 568t
Antituberculosis drugs, 603
Antivenin, 796
Anxiety and fear, 433, 438–440, 439t
Aortic dissection
classification, 515–516
clinical features, 483–484, 516
DeBakcy classification, 515
differential diagnosis, 516–517
essentials of diagnosis, 483
etiology, 515
general considerations, 483
imaging studies, 484–485, 484f, 485f, 516
Stanford classification, 515
treatment, 485, 517
Aortic regurgitation, 198, 475
Aortic stenosis, 475
Aortic surgery, 655, 656
Aortic transection, 515
APACHE (Acute Physiology, Age, Chronic Health Evaluation)
score, 12
Apnea threshold, 99
Aprotinin, 424
aPTT (activated partial thromboplastin time), 409, 411t
Arachidonic acid, 231, 231f, 232t
ARDS. See Acute respiratory distress syndrome
Argatroban
for acute arterial insufficiency, 636–637, 637t
for heparin-induced thrombocytopenia, 645, 829t
mechanisms of action, 831
Arginine vasopressin (AVP). See Antidiuretic hormone
