Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CRITICAL CARE ISSUES IN PREGNANCY
817
Investigations have shown, however, that the average blood
loss after vaginal delivery is near 500 mL, whereas that fol-
lowing cesarean section is in excess of 1 L. The working
definition of postpartum hemorrhage therefore is relative.
Most would acknowledge the presence of postpartum hem-
orrhage when blood loss exceeds 1 L, when there is a 10%
change in the hematocrit between admission and postpar-
tum determinations, or when transfusion is necessary.
The most common causes of early postpartum hemorrhage
(<24 hours after delivery) are uterine atony, lower genital tract
lacerations, and retained products of conception. Less common
causes include placenta accreta, uterine rupture, inversion of
the uterus, and coagulopathies. Uterine atony is by far the most
common and may be associated with the antepartum use of
oxytocin or with uterine overdistention from multiple gesta-
tion or polyhydramnios. Other factors thought to be associated
with uterine atony include high parity, prolonged labor,
cesarean section, precipitous labor, chorioamnionitis, and the
use of tocolytic agents (especially magnesium sulfate).
Lower genital tract lacerations occur frequently and usu-
ally present with vaginal bleeding immediately after delivery.
Uterine lacerations can bleed into the peritoneal cavity or
retroperitoneal space and therefore do not always present
with vaginal hemorrhage. Factors associated with lower gen-
ital tract lacerations are forceps or vacuum delivery, fetal
macrosomia or malpresentation, and precipitate delivery.
Failure of the placenta to completely separate is a risk fac-
tor for the development of both uterine atony and postpar-
tum hemorrhage presumably owing to the placental
fragments interfering with the normal contraction of the
uterus that is necessary for hemostasis. Retention of a suc-
centuriate lobe (accessory lobe of the placenta) may present
with postpartum hemorrhage in the early postpartum
period. Placenta accreta also may cause life-threatening hem-
orrhage owing to the inability of the placenta to completely
separate from the uterine wall. Risk factors for placenta acc-
reta include previous puerperal curettage or previous uterine
surgery, including cesarean section, and placenta previa.
Uterine rupture is an uncommon but catastrophic cause
of postpartum hemorrhage. Because uterine artery blood
flow is between 500 and 600 mL/min, hemorrhage from this
cause can result in rapid maternal exsanguination. Conditions
thought to predispose to uterine rupture include previous
uterine surgery, breech extraction, obstructed labor, abnor-
mal fetal position, and high parity.
Uterine inversion is also a rare complication of delivery,
although it may recur in a patient’s subsequent pregnancies.
Uterine inversion is most remarkable for the development of
shock out of proportion to the amount of blood lost.
Coagulopathies frequently are associated with postpar-
tum hemorrhage. They often occur in association with other
complications of pregnancy such as abruptio placentae,
retained dead fetus, and amniotic fluid embolism. In addi-
tion, preexisting chronic coagulation disorders are signifi-
cant contributors to postpartum hemorrhage.
Delayed postpartum hemorrhage occurring between
24 hours and 6 weeks after delivery may require admission to
the ICU for resuscitation, observation, and perioperative
care. Common causes include infection, placental site subin-
volution, and retained products of conception, as well as
underlying coagulopathy.
Clinical Features
Although the initial management of postpartum hemorrhage
will be accomplished in the delivery room, the ICU physician
should be familiar with the basic principles of diagnosis and
early management. The first priority is to establish the cause.
The relationship between the onset of hemorrhage and the
time of delivery is critical in establishing the diagnosis.
Bleeding prior to delivery of the placenta often indicates a
genital tract laceration, a coagulopathy, or a partial separation
of the placenta. When bleeding begins after the placenta is
delivered, uterine atony, uterine inversion, retained fragments
of the placenta, or placenta accreta may be responsible. The
placenta should be inspected to ensure that torn vessels are
not present, which might indicate the presence of an acces-
sory lobe; that appropriate contour is observed; and that por-
tions are not missing (suggesting placenta accreta).
Uterine atony requires fundal massage and the adminis-
tration of ecbolic drugs (see next). Lacerations should be
sutured in a manner that allows closure of the wound and
compression of the underlying vessels. Hematomas may
form as the result of lacerations. Hematomas below the
pelvic diaphragm usually are accompanied by severe pain
and a palpable mass. Sudden onset of shock without signifi-
cant apparent blood loss suggests that the bleeding point is
above the pelvic diaphragm.
A coagulopathy is suggested by the presence of bleeding
from remote locations such as intravenous insertion sites.
The diagnosis of coagulopathy may be made rapidly by
observing a tube of the patient’s blood for clot formation. If
a firm clot forms within 5 minutes, it is unlikely that clini-
cally significant hypofibrinogenemia is present.
Treatment
A. General Measures—Postpartum hemorrhage represents
a special cause of hemorrhagic (hypovolemic) shock. A sta-
ble airway and adequate intravenous access must be ensured.
Initial resuscitation should be with balanced salt solutions,
although blood replacement will be required early if hemor-
rhage cannot be arrested. Packed red blood cells are usually
used. In the event of severe hemorrhage, replacement of clot-
ting factors also may be needed via the use of fresh-frozen
plasma. Fresh-frozen plasma should be given only if labora-
tory testing shows that the patient has developed a coagu-
lopathy. Blood should be warmed to prevent hypothermia.
Arterial blood gas and hemoglobin determinations should
be performed regularly during resuscitation and after control
of bleeding. Measurements of blood pressure, pulse rate, and

CHAPTER 38
818
urine output will help to assess volume status. Pulmonary
artery catheters are seldom required, although a central
venous catheter may be helpful in actively bleeding patients
who require ongoing resuscitation and transfusion.
B. Ecbolic Agents—Hemorrhage from uterine atony should
be managed with fundal massage plus an intravenous infusion
of oxytocin (10–40 units/L of normal saline). If oxytocin does
not arrest the hemorrhage, treatment with either methyler-
gonovine (0.2 mg intramuscularly) or carboprost
tromethamine (15-methylprostaglandin F
2α
), 0.25 mg intra-
muscularly, may be used. Misoprostol (800 mg per vagina or
rectum) also may be effective. Methylergonovine may be asso-
ciated with an increase in maternal blood pressure and should
not be used in the patient with hypertension. Prostaglandin
agents may provoke bronchospasm and should be not be
used in patients with significant asthma.
C. Surgery—When postpartum hemorrhage cannot be con-
trolled by massage and ecbolic agents, emergent surgery usu-
ally is required. In many cases, these procedures will have
been performed before the patient is transferred to the ICU.
Occasionally, however, a previously stable patient will require
exploration for hemorrhage after it has been controlled.
Common surgical procedures include evacuation of
hematomas caused by lacerations (combined with suturing
of the injury and control of the bleeding vessel), ligation of
pelvic arterial vessels, packing, and hysterectomy. Recent
reviews of cesarean hysterectomy reveal that the average
blood loss for this procedure when done emergently was
3000 mL, and the most common antecedent complications
were uterine rupture, placenta accreta and uterine atony.
D. Angiographic Embolization—When bleeding continues
from an identifiable localized area, embolization via a radi-
ographically placed catheter may be extremely helpful. Some
authors have described the placement of embolization
catheters prophylactically in patients at highest risk of post-
partum hemorrhage.
E. Delayed Postpartum Hemorrhage—Fewer than 1% of
patients with postpartum hemorrhage present more than 24
hours after delivery. Infection and retained products of concep-
tion are the most common causes, with subinvolution of the
placental site also being a consideration. Uterine curettage
should be performed only when retained products of concep-
tion are suspected because of the risk of intrauterine adhesions.
Pelvic and uterine ultrasonography may be helpful in determin-
ing whether retained products are present, although all postpar-
tum uteri contain some clot and debris. Even when there is not
retained placental tissue, evacuation of intrauterine clots allows
more efficient uterine contraction and often results in hemosta-
sis. Estrogens may be used to improve endometrial regrowth
after curettage and to avoid intrauterine adhesions. Ecbolic
agents and antibiotics may be given if retained products of con-
ception are not present. If hemorrhage persists more than 12–24
hours, the patient should undergo curettage for presumed
retained products, even in the absence of a definite diagnosis.
Jansen AJ et al: Postpartum hemorrhage and transfusion of blood
and blood components. Obstet Gynecol Surv 2005;60:663–71.
[PMID: 16186783]
Oyelese Y, Smulian JC: Placenta previa, placenta accreta, and vasa
previa. Obstet Gynecol 2006;107:927–41. [PMID: 16582134]
Tamizian O, Arulkumaran S: The surgical management of post-
partum haemorrhage. Best Pract Res Clin Obstet Gynaecol
2002;16:81–98. [PMID: 11866499]
Trauma During Pregnancy
Accidental injury occurs in approximately 1 in 12 pregnancies.
While many of these incidents are minor, one should bear in
mind that two patients are at risk. Serious injuries during preg-
nancy do not result in a higher maternal mortality rate than do
similar injuries in a nongravid patient. Fetal death, however, is
common, with fetal loss rates of up to 61% reported in studies
of severe trauma. Eighty-five percent of all maternal deaths
from trauma are due to closed head injuries and hemorrhagic
shock, whereas fetal deaths result from abruptio placentae as
well as maternal death and fetal hypoxia. Because of this com-
bined risk, and because of the risk of preterm labor, pregnant
patients often require inpatient observation.
The physiologic changes of pregnancy make the patient
both more and less susceptible to the effects of trauma. The
increased plasma volume and decreased hematocrit further
the potential for diminished oxygen delivery following
blood loss. Fluid resuscitation requirements after hemor-
rhage are greater because of the 50% increase in maternal
intravascular volume. Conversely, the increased blood vol-
ume makes the mother more tolerant of blood loss without
change in her vital signs. The increase in maternal heart rate
(15–20 beats/min) and the decrease in both systolic and
diastolic blood pressures (10–15 mm Hg) may confound
attempts to evaluate volume replacement. Furthermore, an
elevation of coagulation factors during pregnancy increases
the risk for thrombogenesis with surgery or prolonged
immobilization.
As pregnancy progresses into the second trimester, fetal
growth distends the uterus upward into the abdomen, where
it becomes more susceptible to direct injury. The bladder also
becomes more prone to injury, especially after the twelfth
week of gestation. Because blood flow to the uterus is abun-
dant (as much as 600 mL/min), direct injury to the uterus
may cause rapid exsanguination. Uterine blood vessels lack
autoregulation, so maternal shock causes a substantial
decrease in fetal oxygen delivery. Uterine blood flow may fall
before maternal shock becomes manifest and may result in
fetal hypoxia in the face of normal maternal vital signs. Fetal
responses to decreased perfusion and hypoxia include alter-
ations in heart rate (bradycardia or tachycardia), loss of heart
rate variability, and repetitive late decelerations.
Motor vehicle accidents are the principal cause of acci-
dental injuries during pregnancy and account for about 50%
of all cases of blunt abdominal trauma, but 82% of injuries

CRITICAL CARE ISSUES IN PREGNANCY
819
resulting in fetal death. Three-point-restraint seat belts are
preferable for pregnant passengers because the incidence of
body flexion and uterine compression is less than that
induced by lap belts alone. Placental abruption is the most
common cause of fetal demise after blunt abdominal trauma.
Abruption is caused by deformation of the elastic uterus
around the inelastic placenta. The shearing force thus pro-
duced tears the decidua basalis. Current evidence indicates
that the position of the placenta does not influence the devel-
opment of abruption. Uterine rupture is uncommon and
probably occurs in less than 0.6% of all traumatic injuries
during pregnancy. It carries a maternal death rate of less than
10%, but a fetal death rate of nearly 100%. Maternal pelvic
fractures occur frequently but do not necessarily preclude
subsequent vaginal delivery. Such fractures are of concern
when they are comminuted and badly displaced because they
carry the potential to injure the uterus and fetus. Placental
abruption and pelvic fractures are highly correlated.
Gunshot wounds are the most common type of penetrat-
ing injury sustained by pregnant patients. Regrettably, inci-
dents occur in which there was clear intent to harm the fetus.
When compared with nonpregnant victims, pregnant
patients actually have a lower mortality rate after abdominal
gunshot wounds, perhaps because the enlarged uterus and its
contents protect the patient by absorbing and dissipating the
missile’s kinetic energy. Upper abdominal gunshot and stab
wounds, however, cause a higher incidence of intestinal
injury because of cephalad displacement of the viscera by the
uterus. Direct injury of the fetus by a bullet occurs in 70% of
cases, with a 65% intrauterine fetal death rate. Maternal
death is much less common.
Burns, electrocution, and suicide attempts are less com-
mon causes of injury. Unless a burn covers more than 30% of
the patient’s body surface area, it generally will not affect the
pregnancy. Fetal outcome is probably related to gestational age
at the time of the burn. The highest mortality rate is recorded
during the first trimester. Topical iodine solutions should be
avoided because large amounts may be absorbed through
the burn wound. House current electrical injuries occur
uncommonly but may be associated with a high fetal mor-
tality rate because of the path of the current through the
patient’s body. Pregnant victims of electrocution may report
a reduction in fetal movements immediately after the incident.
Fetal demise or intrauterine growth retardation may follow.
Oligohydramnios has been reported at the time of delivery.
Management
A. General Principles—Pregnant patients who require ICU
admission following injury commonly will be resuscitated
and stabilized in the emergency department. Initial treat-
ment in the ICU may be advisable, however, because of the
availability of invasive monitoring.
On arrival, initial concern must be directed toward the
mother, with attention paid to establishment of an adequate
airway, breathing, and circulation. The patient should lie in
the left lateral position, if possible, to prevent compression of
the vena cava by the gravid uterus. Both maternal hypoten-
sion and fetal hypoxia may result from caval compression. If
concern about the cervical spine precludes the decubitus
position, an assistant should displace the uterus by hand to
the left in an attempt to decompress the vena cava.
Alternatively, the entire bed or support board can be tilted.
Supplemental oxygen should be given to increase oxygen
delivery to the fetus. Upper extremity intravenous catheters
should be placed to ensure adequate intravenous access. A
nasogastric tube should be inserted during the early stages of
resuscitation to allow gastric decompression and prevent
aspiration. In the presence of a viable fetus, continuous fetal
heart rate monitoring should be instituted as soon as possible.
Blood is preferred as the initial fluid for resuscitation of
hypotensive trauma patients. Particular attention must be
paid to Rh compatibility. If Rh-incompatible blood is inad-
vertently given to an Rh-negative woman, anti-D antibody
should be given in a dose of 300 mg for every 30 mL of whole
blood or 15 mL of packed red blood cells transfused.
Pregnant patients require more volume replacement than do
nonpregnant patients because of their physiologically
expanded intravascular space.
A bladder catheter should be placed as soon as possible
both to measure the urine output and to help establish the
integrity of the urethra and bladder. Urine so obtained
should be inspected for gross blood and tested for micro-
scopic hematuria.
Normal physical signs of abdominal injury such as pain
and loss of bowel sounds may be masked by the pregnant
uterus. Conversely, all these findings may be produced by the
pregnancy itself. Vaginal bleeding generally is considered an
ominous sign because it may signal placental abruption or
severe pelvic injury.
B. Laboratory Studies—Studies should include hemoglo-
bin serum electrolytes, coagulation profile, amylase, and
blood crossmatch. Routine arterial blood gases are advisable.
When placental separation is suspected because of a pelvic
fracture, fetal distress, uterine tetany, or vaginal bleeding,
measurements of blood fibrinogen concentration, fibrin
degradation products, and platelet count are of particular
importance. Additionally, a tube of blood should be obtained
and observed for clot formation. Noncoagulable blood indi-
cates probable placental abruption and mandates immediate
replacement of fibrinogen with fresh-frozen plasma or cryo-
precipitate, followed by evacuation of the uterus. The possi-
bility of fetomaternal hemorrhage should be evaluated with
a Kleihauer-Betke study. Fetomaternal hemorrhage is most
common when the placenta is located anteriorly, when pelvic
tenderness is present, and following motor vehicle accidents.
If severe, it can result in fetal anemia or fetal death.
C. Imaging Studies—Critical radiographic studies should
not be withheld in an attempt to avoid fetal x-ray exposure.
The fetal risks from various doses of x-ray and the expected
CHAPTER 38
820
doses from various procedures were discussed previously.
The need for chest and abdominal x-rays should be guided
by the nature and severity of the injury. Free air under the
diaphragm on an upright chest x-ray is an indication for
immediate laparotomy. Traumatic separation of the pubic
symphysis in or after the second trimester is difficult to
detect on x-ray because of the normal ligamentous laxity that
accompanies pregnancy. Maternal and fetal complications
are more common after pelvic fractures, and their presence
must be identified.
Obstetric ultrasound should be performed in all cases of
trauma during pregnancy. It is helpful in diagnosing a retro-
placental clot, although absence of a visible clot on ultra-
sound cannot rule out placental abruption. Additionally,
ultrasound can aid in estimating gestational age when a his-
tory cannot be obtained.
D. Peritoneal Lavage—Open peritoneal lavage through a
supraumbilical incision is an excellent technique for diag-
nosing abdominal injuries. Approximately 1 L of lavage fluid
is instilled through the small incision and allowed to return
passively to the container. Criteria that constitute a positive
lavage include (1) a red blood cell count of more than
100,000/μL, (2) a white blood cell count of more than
500/μL, (3) the presence of GI contents, bile, or bacteria, and
(4) increased amylase.
E. Fetal Monitoring—Immediately on patient arrival in the
ICU, fetal heart monitoring should be instituted. Such mon-
itoring provides information about both the fetus and the
mother. The fetus may be compromised by hypoxia before
the mother becomes hypotensive. Bradycardia, tachycardia,
and loss of beat-to-beat variability are ominous signs.
Monitoring in gestations beyond 18–20 weeks may be able to
predict abruptio placentae. Although intermittent ausculta-
tion is possible, it should not substitute for electronic surveil-
lance. The gestational age at which monitoring is mandatory
is controversial, but all authorities would monitor potentially
viable fetuses (>22–23 weeks). Monitoring necessitates the
presence in the ICU of personnel experienced in the inter-
pretation of fetal heart rate patterns.
F. Tocodynamometry (Uterine Contraction Monitoring)—
Tocodynamometry is of significant importance in predicting
early placental abruption. The incidence of abruption
increases with frequent uterine activity (more than eight
uterine contractions per hour), and about 25% of trauma
patients with at least three uterine contractions in a 20-
minute period suffered either abruptio placentae or preterm
labor. Another study found that these complications did not
occur in patients who were without contractions for the first
4 hours. Monitoring during the first 4–6 hours after admis-
sion therefore has been proposed, with additional monitor-
ing only in patients with contractions on initial monitoring
or with a change in maternal condition.
G. Surgery
1. Trauma—Certain kinds of trauma must be managed
operatively. Bowel injuries must be repaired, fractures
reduced, and wounds closed. Pregnancy should not delay or
contraindicate surgical exploration.
2. Abruptio placentae—Evacuation of the uterus is indi-
cated for placental abruption. If gestation has continued for
more than 30 weeks, immediate cesarean section may save
both the fetus and the mother. In cases of intrauterine fetal
demise, labor and spontaneous vaginal delivery may occur.
Caution must be exercised to detect DIC, which is more
common after extensive abruption. If both the platelet count
and the fibrinogen concentration decline, fresh-frozen
plasma or cryoprecipitate should be given and a hysterotomy
performed if delivery is not imminent. The coagulopathy
usually ceases when the placenta is removed.
3. Uterine rupture—Shock, severe abdominal pain, and
lack of fetal heart tones suggest uterine rupture. It may be
difficult to localize the fundus of the uterus, and fetal parts
may be easily palpable through the abdominal wall. An
abdominal x-ray usually shows that the fetal skeleton is in an
unusually high location in the abdomen. Peritoneal lavage is
always positive for blood and returns more fluid than was
instilled (amniotic fluid). At surgery, massive bleeding may
have to be controlled with bilateral internal iliac artery liga-
tion. Supracervical hysterectomy may be required.
4. Cesarean section—Adequate exposure of abdominal
injuries usually can be achieved with careful mobilization of
the uterus. Cesarean section may be required, however, when
the gravid uterus prevents access to deep pelvic injuries.
Patients with undisplaced pelvic fractures usually do not
require cesarean section.
Premature separation of the placenta and fetal head
injuries both may be consequences of maternal trauma dur-
ing pregnancy. Placental separation coexisting with a living
fetus often mandates an emergent cesarean section. In the
case of a live fetus undergoing labor after maternal trauma,
consideration should be given to fetal ultrasound for evi-
dence of fetal head injury. If such evidence exists, this fetus
also may benefit from cesarean delivery.
Cusick SS, Tibbles CD. Trauma in pregnancy. Emerg Med Clin
North Am 2007;25:861–72, xi. [PMID: 17826221]
El-Kady D et al: Trauma during pregnancy: An analysis of mater-
nal and fetal outcomes in a large population. Am J Obstet
Gynecol 2004;190:1661–8. [PMID: 15284764]
Mattox KL, Goetzl L: Trauma in pregnancy. Crit Care Med
2005;33:S385–9. [PMID: 16215362]
Muench MV, Canterino JC. Trauma in pregnancy. Obstet Gynecol
Clin North Am 2007;34:555–83, xiii. [PMID: 17921015]
Weiss HB, Songer TJ, Fabio A: Fetal deaths related to maternal
injury. JAMA 2001;286:1863–8. [PMID: 11597288]
821
0039
Antithrombotic Therapy
Elizabeth D. Simmons, MD
Pathologic blood clot formation within blood vessels
(thrombosis) and embolization of clots to distant sites result
from complex interactions among platelets and coagulation
proteins, the fibrinolytic system, and the blood vessel itself.
Thrombi are composed of red blood cells, platelets, and fib-
rin in varying proportions depending on the conditions
present at the site of thrombus formation. Very diverse clini-
cal conditions are associated with increased risks of such
pathologic thrombosis and embolization (Table 39–1).
Thromboembolic disease is a major cause of morbidity and
mortality; 30–40% of all deaths in the United States are
attributed to thrombotic events, and nonfatal events occur in
hundreds of thousands of people each year.
Antithrombotic therapy consists of strategies (both phar-
macologic and physical) to prevent pathologic blood clot
formation or to treat established thromboses in order to
limit the clinical consequences of such clots. The decision to
use antithrombotic therapy in clinical practice is often com-
plicated because of the diversity of the clinical conditions
affecting patients, difficulties in establishing accurate diag-
noses of thromboembolism, and our still incomplete under-
standing of the risks and benefits of antithrombotic therapy
in the prevention and treatment of thromboembolic disease.
Numerous new pharmacologic agents have been developed
or are under development, and various combinations of
antithrombotic agents are being used in diverse settings.
Physical Measures
Venous stasis and damage to blood vessels are the two most
important risk factors for the development of venous throm-
boembolism (VTE). Physical measures to decrease venous
stasis are quite important in preventing venous clots, particu-
larly in hospitalized patients. Limiting bed rest as much as
possible for most medical patients and early mobilization
after surgery can decrease the period of risk for venous throm-
bosis. Intermittent pneumatic compression devices (IPCs) and
the venous foot pump (VFP) reduce venous stasis, increase
venous flow, and reduce the risk of deep vein thrombosis
(DVT) in lower-risk patients but have not been demonstrated
to reduce the risk of pulmonary embolism (PE). These devices
are used primarily in patients with high bleeding risk or in
combination with pharmacologic agents for prevention of
VTE. IPCs should not be used in the presence of established
thrombosis, severe peripheral vascular disease, skin ulcers, or
after leg trauma if there is compromised tissue viability.
Graduated compression stockings may help to control leg
edema but are not highly effective for the prevention of VTE.
They are not recommended as an isolated measure for preven-
tion of VTE in patients at moderate to high risk.
Interruption of the inferior vena cava using a fluoroscop-
ically placed filter is indicated for treatment of patients with
lower extremity venous thrombosis who have a major con-
traindication to anticoagulant therapy or for patients with
recurrent thromboembolism despite adequate anticoagula-
tion. Inferior vena cava filter placement reduces the risk of PE
but does not prevent recurrence or extension of lower
extremity thromboses. Therefore, unless contraindicated, ini-
tiation of anticoagulation as soon as possible after filter place-
ment is advised.
Surgical or transvenous embolectomy is performed occa-
sionally in selected patients with life-threatening thromboem-
bolic disease, particularly in patients with contraindications to
anticoagulation or thrombolysis.
Antiplatelet Agents
Antiplatelet therapy (alone or in combination with anticoag-
ulants) is most beneficial in prevention or treatment of arte-
rial thrombosis. Arterial thrombi usually develop in
abnormal blood vessels and are associated with activation of
both blood coagulation and platelets; however, arterial
thrombi are composed primarily of platelets held together by
fibrin strands. Antiplatelet agents inhibit platelet function
through several biochemical pathways or by exerting effects
on the platelet membrane.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 39
822
Antiplatelet agents are useful in the management of
patients with unstable angina; suspected acute myocardial
infarction; a history of myocardial infarction, nonfatal stroke,
transient ischemic attacks, or peripheral vascular disease; and
those undergoing vascular procedures. Antiplatelet agents are
not as useful as other measures for prevention of VTE, such as
anticoagulation, particularly in high-risk surgical patients or
for stroke prevention in patients with atrial fibrillation.
Inhibitors of Cyclooxygenase (Aspirin,
Nonsteroidal Anti-inflammatory Agents)
Cyclooxygenase (COX) is a key enzyme in the prostaglandin
pathway within platelets and endothelial cells. The final prod-
uct of this pathway differs in platelets and endothelial cells.
Thromboxane A
2
(TXA 2), a potent inducer of platelet aggre-
gation, is produced in platelets, whereas prostacyclin, an
inhibitor of platelet aggregation, is produced in endothelial
cells. Aspirin irreversibly inhibits COX (COX-1 more so than
COX-2), which cannot be resynthesized by platelets because
they have no nucleus. Vascular prostacyclin production is
affected to a much lesser extent by aspirin because endothelial
cells can resynthesize cyclooxygenase, and because prostacy-
clin is also COX-2–derived, which is much less sensitive to
inhibition by aspirin. Thus aspirin is an ideal pharmacologic
agent for the treatment and prevention of thromboembolic
disease. Several of the nonsteroidal anti-inflammatory drugs
(NSAIDs) also inhibit platelet COX, but inhibition is
reversible. NSAIDs may cause clinical bleeding in patients
with underlying hemostatic defects or after invasive proce-
dures, but they are generally not used therapeutically for treat-
ment or prevention of thromboembolic disorders. COX-2
inhibitors do not inhibit production of platelet TXA 2 and do
not have antithrombotic properties; these agents actually may
increase the risk of thromboembolism.
Three reversible COX inhibitors (ie, indobufen, flur-
biprofen, and triflusal) that may have beneficial effects simi-
lar to those of aspirin have been investigated as alternatives
to aspirin; none are currently approved for use in the United
States, and it is unclear whether they will prove to have any
advantage over currently available treatments.
Aspirin is rapidly and completely absorbed from the GI
tract, metabolized to salicylate, and circulates as salicylate
bound primarily to albumin. Salicylate is metabolized in the
liver and excreted in the urine. The serum half-life of salicy-
late is 15–20 minutes. The effect of aspirin on platelet func-
tion begins within 1 hour of ingestion (3–4 hours for
enteric-coated preparations) and lasts the life of the platelet
(8–10 days). Enteric-coated tablets should be chewed if rapid
antiplatelet effect is necessary. Gastric irritation may be
reduced with enteric-coated and timed-release forms of
aspirin, but absorption may be reduced or delayed.
Ingestion of aspirin in doses commonly used in clinical
practice prolongs the bleeding time in normal subjects some-
what variably, typically by 1–3 minutes, and out of the normal
range only in about half of subjects. Aspirin inhibits platelet
aggregation in vitro, but these laboratory effects do not corre-
late well with in vivo hemostasis. In patients with underlying
hemostatic defects (eg, hemophilia, von Willebrand disease,
uremia, mild preexisting disorders of platelet function, and
thrombocytopenia), aspirin may markedly prolong the bleed-
ing time and cause serious bleeding.
Stasis Immobilization
Congestive heart failure
Surgery
Advanced age
Obesity
Atrial fibrillation
Blood vessel abnormalities Trauma, coronary artery disease, peripheral
vascular disease, varicosities, vasculitis,
artificial surfaces (vascular grafts, heart
valves, indwelling catheters), diabetes
mellitus
Homozygous homocystinuria
Previous thrombosis
Abnormalities of
physiologic
antithrombotic
mechanisms
Antithrombin deficiency
Protein C or S deficiency
Hereditary resistance to activated protein C
(factor V Leiden and prothrombin gene
mutation G20210A)
Methylenetetrahydrofolate reductase
(MTHFR) gene mutation C677T
Defective or deficient plasminogen
Plasminogen activator deficiency
Abnormalities of
coagulation and
fibrinolysis
Malignancy
Pregnancy
Oral contraceptives
Hormone replacement therapy
Tamoxifen
Nephrotic syndrome
Lupus anticoagulant/antiphospholipid
antibody syndrome
Prothrombin complex concentrate solution
Dysfibrinogenemia
Factor VIII >150%
Abnormalities of platelets Myeloproliferative disorders
Paroxysmal nocturnal hemoglobinuria
Hyperlipidemia
Diabetes mellitus
Heparin-associated thrombocytopenia
Thrombotic thrombocytopenic purpura
Hyperviscosity Polycythemia
Leukemia
Sickle cell disease
Leukoagglutinin
Hypergammaglobulinemia
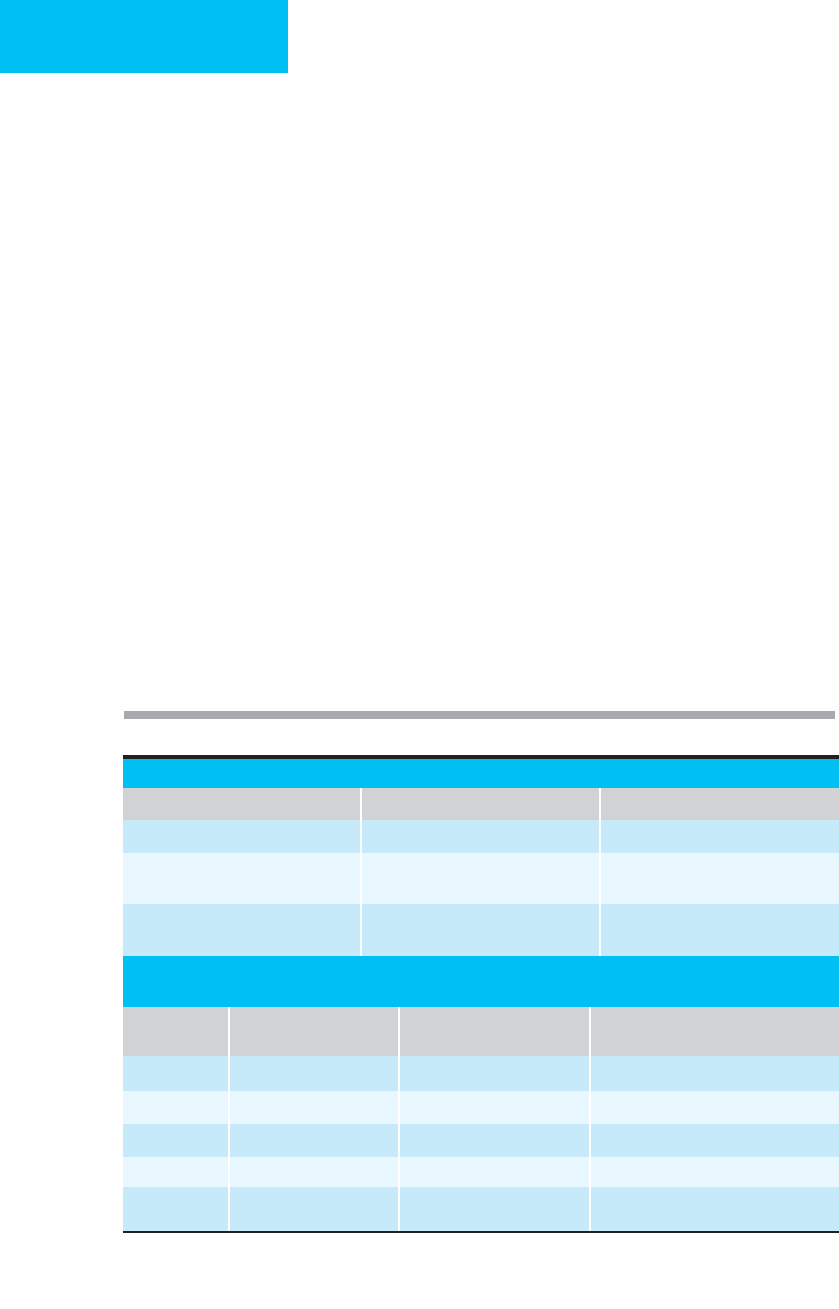
Table 39–1. Conditions associated with pathologic
thromboembolism.

ANTITHROMBOTIC THERAPY
823
The clinical benefits of aspirin have been established by
large trials of patients with various thromboembolic phenom-
ena, with endpoints including development of thrombosis,
death from thrombosis, and bleeding complications.
Laboratory tests of platelet function are not useful for monitor-
ing such patients in clinical practice. The measurable
antiplatelet effects of aspirin are equivalent over a wide range of
daily aspirin dosage (300–3600 mg/day), and the therapeutic
benefits have been demonstrated with as little as 75 mg/day (or,
in one study, 30 mg/day). The minimum effective dose varies for
different disorders, but for most situations, a daily dose between
50 and 100 mg is effective and minimizes toxicity with long-
term use. In acute myocardial infarction and acute ischemic
stroke, a dose of 160 mg/day reduces early mortality and recur-
rent events. Higher-dose aspirin (eg, 650–1500 mg/day) does
not improve outcome and actually may be detrimental.
Currently available data support the use of aspirin in car-
diovascular disease prevention, stable and unstable angina,
acute myocardial infarction, transient ischemic attacks and
incomplete stroke, severe carotid stenosis, stroke following
carotid artery surgery, and in patients with prosthetic heart
valves (in combination with oral anticoagulation). The ben-
efits of aspirin following vascular or valve surgery, arterial
procedures, or creation of fistulas or shunts are less certain
but appear to include a reduction in risk of arterial occlusion
compared with no therapy. Aspirin, although more effective
than placebo, is less effective than anticoagulation in pre-
venting recurrent stroke associated with nonvalvular atrial
fibrillation. Aspirin has not been shown to be effective for
treatment of established VTE and is inferior to other meas-
ures for prevention of VTE, especially in high-risk patients.
Although one large trial showed a benefit of aspirin—alone
or in combination with anticoagulation—for patients under-
going hip surgery, it is less effective than anticoagulation.
The safety and efficacy of aspirin in combination with
anticoagulants have not been clearly established.
Aspirin resistance resulting in treatment failure has been
observed in some patients receiving aspirin for the treatment of
ischemic vascular disease. The mechanisms underlying resist-
ance are not known, and there is currently no reliable platelet
function test to predict which patients are unlikely to benefit
from aspirin. Concomitant therapy with other NSAIDs can
reduce the antiplatelet effect of aspirin because of competition
for binding sites in the platelet and may be one important
mechanism of aspirin treatment failure because of widespread
use of these over-the-counter medications. Patients who
develop recurrent ischemic events despite aspirin are candi-
dates for alternative antiplatelet therapy or anticoagulation.
Adverse effects of aspirin include dose-dependent GI irrita-
tion (eg, dyspepsia, nausea and vomiting, occult blood loss, and
gastric ulceration), hypersensitivity reactions, abnormal liver
function tests (rare), nephrotoxicity (rare), and at high doses,
tinnitus and hearing loss. Enteric-coated aspirin does not
reduce the risk of GI bleeding compared with regular aspirin.
Concomitant use of NSAIDs may increase the risk of GI bleed-
ing. Omeprazole is effective at treating and preventing GI ulceration
and bleeding associated with NSAIDs and may permit chronic
use of aspirin in patients at high risk for cardiovascular events
who have had this complication. Overdosage of aspirin (salicy-
late intoxication) may be life-threatening and is manifest by
metabolic acidosis and respiratory alkalosis, dehydration, fevers,
sweating, vomiting, and severe neurologic symptoms. Reye’s
syndrome in infants and children appears to be associated with
aspirin usage. In patients at risk for major bleeding, the
antithrombotic effects of aspirin may result in serious bleeding.
High doses of aspirin may result in interference with prothrom-
bin synthesis, prolongation of the prothrombin time, and signif-
icant hemorrhagic sequelae. Subarachnoid hemorrhage may
occur with the use of more than 15 aspirin per week, particu-
larly in older or hypertensive women.
Inhibitors of ADP-Mediated Platelet Aggregation
(Ticlopidine, Clopidogrel)
Ticlopidine and clopidogrel are structurally related
thienopyridines that inhibit platelet function. Repeated daily
dosing results in cumulative inhibition of ADP-induced
platelet aggregation and slow recovery of platelet function
after stopping the drug. The major properties of ticlopidine
and clopidogrel are compared in Table 39–2.
Ticlopidine is well absorbed (80–90%) from the GI tract.
It is rapidly metabolized with one active metabolite. Steady
state levels are achieved with 250 mg twice daily after 14 days.
The onset of antiplatelet effect is delayed (up to 2 weeks), so
ticlopidine should not be used when a rapid antiplatelet
effect is needed. Ticlopidine was introduced as a potential
alternative to aspirin, but its high cost, toxicity, and only
marginally better efficacy have limited its use in current
practice. Ticlopidine is approved for stroke prevention when
aspirin has failed or in patients who cannot tolerate aspirin.
Ticlopidine may cause neutropenia (2.4%), thrombocy-
topenia, or pancytopenia (0.04–0.08%), particularly in the
first 3 months of therapy, so monitoring of blood counts
must be done during that time. Thrombotic thrombocy-
topenic purpura (TTP) has been reported with ticlopidine
therapy (0.02–0.04%), but ticlopidine also has been used
successfully in management of TTP. Other adverse effects
include diarrhea (20%), skin rash (2–15%), increase in total
cholesterol levels (mean increase of 9%), and reversible liver
function test abnormalities (rare).
Clopidogrel is rapidly absorbed and metabolized to active
metabolites (the main one being SR 26334, a carboxylic acid
derivative). The onset of inhibition of platelet aggregation is
dose-dependent, occurring 2 hours after a single dose
(400 mg) but after 2–7 days with lower daily dosing (50–100
mg daily). Platelet function returns to normal 7 days after
stopping the drug, consistent with irreversible inhibition of
platelet function. A loading dose of 300 mg followed by 75 mg
daily will result in a rapid and sustained antiplatelet effect; a
loading dose of 600 mg is used in patients undergoing percu-
taneous coronary intervention, but the optimal loading dose
has not been determined. Clopidogrel appears to have
CHAPTER 39
824
approximately the same antiplatelet effects as ticlopidine, but
because of its better safety profile, it has replaced ticlopidine
for most clinical situations. Its therapeutic efficacy appears to
be equivalent to aspirin in most settings except for sympto-
matic peripheral artery disease, in which it may be superior.
It is currently approved for use in patients with recent stroke
or myocardial infarction and in those who have peripheral
arterial vascular disease. Clopidogrel combined with aspirin
decreases the rate of cardiovascular events following acute
coronary syndromes compared with aspirin monotherapy
and is the standard regimen following placement of coronary
stents (for at least 1 month; longer duration may be better).
Combination therapy is associated with more bleeding than
with aspirin alone, but only with higher doses of aspirin
(>100 mg/day). The most common side effects of clopido-
grel are rash and diarrhea. GI bleeding occurs less often than
with aspirin (2%); however, in one study in patients who had
bleeding ulcers while taking aspirin, clopidogrel was associ-
ated with a higher rate of recurrent bleeding than aspirin
when each was combined with a proton-pump inhibitor.
Neutropenia has been reported less often than with ticlopi-
dine (0.8%), as has TTP (reported occurrence 1:250,000 per-
sons, about the same as the general population), usually
occurs within the first 2 weeks of treatment.
Integrin αIIbβ3 (Platelet Glycoprotein IIb/IIIa)
Receptor Inhibitors
Platelet glycoprotein IIb/IIIa (GP IIb/IIIa) inhibitors block
the binding of fibrinogen to its receptor on the platelet
membrane, preventing platelet aggregation. There are three
GP IIb/IIIa inhibitors currently approved for use in the
United States: abciximab (recombinant humanized mono-
clonal antibody), eptifibatide (synthetic heptapeptide similar
to that found in snake venom from Sistrurus m barbouri), and
tirofiban (a nonpeptide mimetic), all of which are given intra-
venously. Prolongation of bleeding time and decreased
platelet aggregation in vitro are seen with all these agents, but
in contrast to aspirin, ticlopidine, and clopidogrel, these
effects are rapidly reversible after discontinuation of the drug.
Results of six large studies have shown that these agents, in
combination with aspirin and heparin, are effective for pre-
venting ischemic complications associated with percutaneous
coronary artery interventions. The benefits of these agents are
less certain for management of patients with acute coronary
syndromes who are not undergoing percutaneous interven-
tion; studies have yielded conflicting results in terms of bene-
fits, whereas in all studies there is a higher risk of bleeding
compared with standard therapy. Only diabetes have consis-
tently benefited from addition of one of these agents to stan-
dard therapy. Although coronary flow and reinfarction rates
are improved by adding GP IIb/IIIa blockade to throm-
bolytic therapy in acute myocardial infarction, there does not
appear to be any mortality benefit for combined therapy, and
bleeding is increased by the combination. Four orally active
agents have been tested and are not more effective when
combined with aspirin or when given in place of aspirin for
patients with acute coronary syndromes and may increase
mortality. The observed increase in mortality may be due to
increased bleeding and a possible paradoxical prothrombotic
Ticlopidine Clopidogrel
Absorption (oral) 90% Rapid
Half-life 24–36 hours (single dose); 96 hours (after 14 days
or therapy)
Active metabolite SR 26334: 8 hours
Active metabolities Yes Requires metabolism to active inhibitor: SR 26334
Onset of antithrombotic action Delayed up to 2 weeks 2 hours (single 400 mg dose); 1 day (50–100 daily dose)
Recovery of platelet function after
discontinuing drug
7 days 7 days
Recommended dose 250 mg orally twice daily 300 mg loading dose; 75 mg orally daily
Clinical use Cerebral ischemia with aspirin failure or intolerance Peripheral vascular disease, prevention of recurrent
stroke, myocardial infarction. Combined with aspirin
after coronary artery stent placement.
Side effects Neutropenia (2.4%), thrombocytopenia, TTP
(0.2%–0.04%), aplastic anemia, rash, diarrhea
Rash, diarrhea, TTP (1/1,000,000), neutropenia
(0.8%), gastrointestinal bleeding (2%)
Expense About $2–3/pill About $3/pill
TTP = thrombotic thrombocytopenic purpura.
Table 39–2. Comparison of ticlopidine and clopidogrel.

ANTITHROMBOTIC THERAPY
825
effect owing to activation of platelets. GP IIb/IIIa inhibitors
can cause bleeding similar to that seen with fibrinolytic ther-
apy. They are contraindicated in patients with platelet counts
of less than 100,000/μL.
Abciximab binds rapidly to the platelet receptors, fol-
lowed by dose-dependent inhibition of platelet aggregation,
accompanied by prolongation of the bleeding time. Bleeding
time returns gradually to normal by 12 hours after a bolus
injection, and platelet aggregation normalizes within 48 hours.
A bolus dose of 0.25 mg/kg followed by a 10 μg/min contin-
uous infusion results in sustaining of the antiplatelet effect.
This regimen has been used to prevent ischemic events in
patients undergoing percutaneous transthoracic coronary
angioplasty (PTCA). Major bleeding, especially in combi-
nation with full-dose heparin, can occur with abciximab.
Reversible thrombocytopenia may occur (1–2%) as soon as
2 hours after starting therapy. Antibodies develop in about
6%. The antiplatelet effects of abciximab may be responsi-
ble for its therapeutic benefits, but it also inhibits throm-
bin formation, which may contribute to its antithrombotic
properties.
Eptifibatide may cause less bleeding time prolongation
than other GP IIb/IIIa inhibitors while causing equivalent
inhibition of platelet aggregation, although this effect may
have been related to methods of measurement. Like abcix-
imab, eptifibatide can inhibit thrombin generation. Several
dosing regimens have been used for eptifibatide, ranging
from a 90–180 μg/kg bolus followed by continuous infusion
rates between 0.5 and 2 μg/kg per minute for 18–24 hours.
Bleeding time returns to normal 1 hour after stopping the
infusion, whereas inhibition of platelet aggregation may last
4 hours or more. Eptifibatide does not appear to increase the
overall rate of thrombocytopenia, but it may cause severe
thrombocytopenia in a small number of patients.
Tirofiban is a nonpeptide inhibitor of the GP IIb/IIIa
receptor that increases bleeding time and inhibits platelet
aggregation. Its effects are augmented by simultaneous
administration of aspirin. Onset of platelet inhibition is
rapid (5 minutes) and returns to normal within 1.5–4 hours
after discontinuation. Reported studies use bolus doses of
5–15 μg/kg followed by infusions of 0.05–0.15 μg/kg per
minute. Severe reversible thrombocytopenia may complicate
treatment with tirofiban.
Dextran
Dextran (available in high- and low-molecular-weight formu-
lations) interferes with platelet function and fibrin polymer-
ization and enhances plasmin-mediated fibrinolysis. Although
dextran is a volume expander, hemodilution induced by dex-
tran does not appear to influence its antithrombotic effects.
Dextran is less effective than other agents for prevention of
VTE. Dextran has been used primarily during carotid
endarterectomy and microvascular procedures, but because
there are few data from controlled clinical trials, firm recom-
mendations about its role cannot be made. Dextran is not
effective in the treatment of active thromboembolic disease.
Because of its volume-expanding properties, dextran should
be avoided in patients at risk for volume overload. Dextran
occasionally may cause hypersensitivity reactions.
Phosphodiesterase Inhibitors
Dipyridamole is the only phosphodiesterase inhibitor cur-
rently in use in the United States. Dipyridamole does not affect
platelet aggregation but prolongs platelet survival time in
patients with arterial thrombosis or prosthetic heart valves.
Dipyridamole does not appear to be a particularly effective
antithrombotic agent on its own, in part, owing to limited
bioavailability. A new preparation with improved bioavailabil-
ity combined with aspirin is available (200 mg dipyri-
damole/25 mg aspirin) and has demonstrated a significant
reduction in recurrent stroke or death in patients with prior
strokes or transient ischemic attacks (TIAs). The most com-
mon side effect of dipyridamole is headache; it does not
appear to increase the risk of bleeding compared with placebo.
Anticoagulants
The commonly used anticoagulants interfere with blood clot
formation and extension by inhibiting coagulation factors
(eg, unfractionated and low-molecular-weight heparin) or
blocking the synthesis of biologically active coagulation fac-
tors (eg, vitamin K antagonists). These anticoagulants have
demonstrated efficacy in a wide range of thromboembolic
conditions, both venous and arterial. Indications for use of
anticoagulants are expanding. The development of several
new anticoagulants, including several direct thrombin
inhibitors (DTIs), with different mechanisms of action and
more favorable therapeutic indices has expanded the use of
anticoagulant therapy and increased the therapeutic options
for patients with complicated medical conditions.
Unfractionated Heparin (UFH)
UFH is derived from porcine intestine or bovine lung and is
a mixture of molecules of heterogeneous size (MW
3000–33,000). Heparin binds to antithrombin (AT; also
known as antithrombin III) and accelerates antithrombin’s
inhibition of activated thrombin and other coagulation fac-
tors (particularly activated factor X). Only about a third of
administered UFH contains the specific pentasaccharide
sequence that is necessary for binding to AT, and only those
molecules have anticoagulant activity. An additional
sequence of 13 saccharides is required for the AT-heparin
complex to bind with thrombin; however, only the pentasac-
charide sequence is required for inactivation of activated fac-
tor X. This heparin-AT interaction is the major mechanism
for heparin’s anticoagulant effect. At high concentrations,
heparin also can bind directly to heparin cofactor II and
inactivate thrombin. Heparin, particularly the high-
molecular-weight fractions, also inhibits platelet function. In
addition to its anticoagulant properties, heparin can increase
CHAPTER 39
826
vascular permeability, inhibit vascular smooth muscle cell
proliferation, and interfere with normal bone homeostasis.
Heparin is not well absorbed from the GI tract, so it must
be administered parenterally (subcutaneously or intra-
venously). Subcutaneous UFH has lower bioavailability and
should be accompanied by an intravenous bolus injection if
immediate anticoagulation is required and a higher initial
dose (about 10% greater than for IV administration).
The pharmacology of heparin is complex. It circulates
bound to plasma proteins, binds to endothelial cells, where it
is neutralized by platelet factor 4, and is taken up by
macrophages and desulfated. There is a nonlinear dose-
response relation and a dose-dependent biologic half-life.
The route of elimination of heparin is not certain; plasma
clearance is accelerated by the presence of acute thromboem-
bolism. The rate of clearance of heparin depends on the size
of the molecules; larger molecules are cleared more rapidly
than low-molecular-weight molecules.
Although there is a relationship between the dose of
UFH and its efficacy (as well as safety), the variability of
response to UFH requires monitoring and adjustment of
dose. Monitoring of UFH activity is based on its biologic
effect on in vitro coagulation. UFH prolongs three impor-
tant in vitro coagulation parameters: the thrombin time
(TT), the prothrombin time (PT), and the activated partial
thromboplastin time (aPTT). The TT is the most sensitive
indicator of heparin’s effect and may be used to detect even
small amounts of heparin. The TT is useful to differentiate
heparin’s effect from that of circulating inhibitors of coag-
ulation, which are phospholipid-dependent and therefore
will result in a prolonged aPTT but normal TT. The PT is
the least sensitive measure of heparin’s effect and is usu-
ally normal unless the patient is also receiving oral antico-
agulant treatment or is overanticoagulated. The aPTT is
intermediate in sensitivity and is the most commonly used
test for monitoring UFH. However, recent clinical studies
have found that the aPTT does not always reliably predict
response to therapy. In addition, commercial reagents
used in the aPTT assay have variable sensitivity to
heparin, which makes monitoring UFH therapy of uncer-
tain accuracy. Nevertheless, the aPTT is still the most
commonly used method for monitoring response to UFH.
In most clinical situations, the desired aPTT while receiv-
ing UFH is one and one-half to two times the control
time. Suggested adjustment of UFH dose based on aPTT
results is outlined in Table 39–3 and ideally should be
based on calibration of the aPTT reagent to correspond to
therapeutic heparin levels (0.3–0.7 IU/mL). Dose modifi-
cations should be made when UFH is used in combination
with thrombolytic therapy or platelet GP IIb/IIIa antago-
nists. When UFH is given subcutaneously, peak plasma
levels are reached after 3 hours.
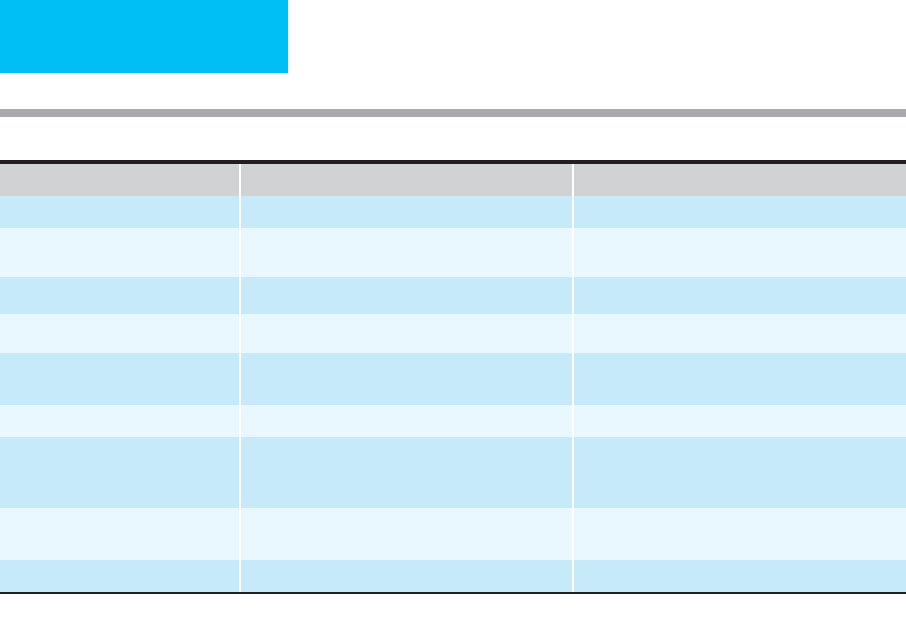
A. Initial Dose
Indication Loading Dose by IV Bolus Initial Maintenance Infusion
∗
Venous thromboembolism 80 units/kg 18 units/kg/h
Unstable angina or acute myocardial
infarction
60–70 units/kg to maximum of
5000 units
12–15 units/kg/h (maximum
1000 units/h)
Concomitant alteplase for acute STEMI 60 units/kg to maximum of
4000 units
12 units/kg/h (maximum
1000 units/h)
Table 39–3. Unfractionated heparin, dosing and adjustment.
B. Subsequent Dose Adjustments Based on aPTT (First aPTT Obtained 6 hours after Starting
Unfractionated Heparin)
aPTT (s)
Rate Change
(units/kg/h)
Additional Action Obtain Next aPTT
<35 +4 Rebolus 80 units/kg 6 h
35–45 +2 Rebolus 40 units/kg 6 h
46–70
†
0 None Following morning
71–90 –2 None 6 h
>90 –3 Hold infusion 60 min 6 h
∗
Unfractionated heparin, 25,000 units in 250 mL D
5
W (100 units/mL).
†
The therapeutic range for aPTT should be standardize to correspond to therapeutic anti–factor Xa levels
(0.3–0.7 IU/mL).
