Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

467
0021
Cardiac Problems
in Critical Care
Shelley Shapiro, MD, PhD
Malcolm M. Bersohn, MD, PhD
Critically ill patients can present challenging cardiac prob-
lems for both diagnosis and management. Many critically ill
patients develop cardiac problems secondary to the metabolic
and hemodynamic consequences of their underlying illness.
Others have preexisting cardiac conditions that are either well
compensated or asymptomatic prior to presentation to the
ICU and become clinically relevant during their ICU course.
A final group of patients is treated in the ICU for known car-
diac conditions or has their heart condition diagnosed during
their ICU admission. In all of these patients, the interplay of
the cardiac illness with other medical problems critically
influences the patient’s outcome. Therefore, defining the type
and severity of the underlying cardiac problem, considering
their relationship to other medical problems, and treating the
heart disease are important considerations. As always, the key
factor in the management of cardiac problems is a high
degree of suspicion and early diagnosis. Methods for identify-
ing and diagnosing cardiac disease in critically ill ICU
patients will be emphasized throughout this chapter.
Congestive Heart Failure
ESSENTIALS OF DIAGNOSIS
Cardiomegaly, decreased ventricular ejection fraction or
abnormal ventricular wall motion, elevated pulmonary
artery wedge pressure, low cardiac output.
May have a previously known cause such as valvular heart
disease or cardiomyopathy but also may present as a result
of ischemia or secondary to severe systemic hypertension.
Acute pulmonary edema: dyspnea, orthopnea, rales,
and wheezing; abnormal chest x-ray with perihilar con-
gestion; hypoxemia.
Cardiogenic shock: hypotension; abnormal renal,
hepatic, and CNS function due to decreased perfusion;
lactic acidosis.
General Considerations
Congestive heart failure is a major therapeutic and diagnos-
tic challenge because of the number of its possible causes, the
number of patients who have heart failure, and the associ-
ated disability. Congestive heart failure is the most frequent
diagnostic category coded in Medicare patients. Determining
the cause and severity of congestive heart failure is extremely
important for effective treatment. Although coronary artery
disease is a frequent cause of congestive heart failure, partic-
ularly in the elderly, there are many other causes. For exam-
ple, congestive heart failure with pulmonary edema
secondary to mitral stenosis is managed quite differently
from that due to dilated cardiomyopathy. Therapy effective
in treating congestive heart failure in a patient with severe
mitral regurgitation could be lethal in a patient with critical
aortic stenosis. With the ability to perform valve replace-
ment and repair, coronary bypass grafting and angioplasty,
and the possibility of cardiac transplantation, a specific car-
diac diagnosis has implications for interventional manage-
ment as well as drug therapy.
The causes of chronic congestive heart failure may be very
different from the causes of acute failure. Acute congestive
heart failure in critically ill patients is due to myocardial
ischemia or infarction, acute valvular insufficiency (eg, mitral
or aortic regurgitation), worsening aortic stenosis or mitral
stenosis, acute myocarditis (rare), cardiotoxic drugs, alcohol,
and sepsis. Often, volume overload (owing to fluid volume
administered in the ICU for treatment of hypotension or as
part of administration of therapy for other disease processes)
precipitates heart failure in the ICU setting. This may be com-
pounded by anemia and/or by reduced renal function result-
ing in additional fluid retention and volume expansion. The
role of excessive fluid resuscitation and accumulating vol-
ume overload in ICU patients cannot be too highly empha-
sized. Hypoalbuminemia also can add to the picture by
allowing fluid to transudate at lower oncotic pressures.
Recently, a new acute form of heart failure has been
described in patients suffering acute severe stress resulting in
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.

CHAPTER 21
acute severe myocardial dysfunction (mimicking myocardial
infarction or acute cardiomyopathy). This syndrome, more
common in females, appears to be reversible but presents as
life-threatening heart failure. Chronic congestive heart fail-
ure is often idiopathic, although in many cases it is associated
with ischemic heart disease, chronic valvular heart disease,
and hypertension. The additional stress of the ICU and asso-
ciated critical illness may worsen preexisting myocardial dys-
function and heart failure in a previously stable patient.
A high degree of suspicion of congestive heart failure is
required to identify subtle cases or patients with coexisting
heart failure. Patients in the ICU with dyspnea and hypox-
emia often have combined heart and lung disease, and
patients with known pulmonary disease can develop cardiac
disease as a result of the increased stress of sepsis, hypoxia, or
deterioration of pulmonary function. Any patient with unex-
plained hypoxemia, hypotension, or a worsening clinical
state requires assessment of cardiac function.
A. Cardiac Function in the Normal Heart—Cardiac out-
put is the product of stroke volume and heart rate. Stroke
volume is determined by three factors: preload, afterload,
and contractility. In the intact heart, preload is the end-
diastolic tension or wall stress and is ultimately determined
by the resting length of the muscle or the degree of stretch of
the muscle fibers. Preload is directly related to the compli-
ance of the ventricle and the end-diastolic pressure.
Although preload is a measure of force, in conceptual terms
it can be thought of as being most closely related to the end-
diastolic volume of the ventricle. As the ventricular volume
and pressure increase, so does the preload. Pulmonary capil-
lary wedge pressure is often used when clinically describing a
patient’s preload.
Afterload is the resistance against which the ventricle
ejects blood. Afterload or tension on the left ventricle can be
described by the formula ΔP × r/h, where ΔP is the trans-
mural pressure during ejection, r is the radius of the left ven-
tricular chamber, and h is the thickness of the ventricular
wall. Stroke volume is inversely proportional to afterload.
Contractility is the inherent ability of the muscle to con-
tract and is independent of the loading conditions on the heart
(ie, preload and afterload). Circulating catecholamines and
increased sympathetic efferent activity increase contractility.
Cardiac performance can be improved for a given level of
myocardial contractility by changing the loading conditions.
B. Cardiac Function in Congestive Heart Failure—
Congestive heart failure develops when cardiac function is
inadequate to maintain sufficient cardiac output to supply
the metabolic needs of the body at normal filling pressures
and heart rate. In mild heart failure, cardiac function may
be adequate at rest. However, exercise or illness can
increase metabolic demands that may not be met when
cardiac reserve is inadequate. Thus congestive heart failure
may be precipitated by critical illness with attendant fever,
anemia, and vasodilation. In heart failure owing to
decreased left ventricular function with reduced stroke vol-
ume, cardiac output may be transiently maintained by
increased heart rate or by increased preload with ventricu-
lar dilation and increased volume. The increasing use of
beta-blockers in the treatment of chronic congestive heart
failure, ischemia, and chronic coronary artery disease may
blunt the sympathetic response and tachycardia necessary
to maintain cardiac output. Acutely, however, cardiac out-
put may be insufficient, and signs and symptoms of hypop-
erfusion including hypotension, cyanosis, and peripheral
vasoconstriction, may be present (forward failure).
Inadequate ventricular emptying (low forward flow) results
in elevated left atrial and left ventricular end-diastolic vol-
ume and pressure that are transmitted back into the lungs
and the pulmonary venous system with transudation of
fluid. Clinically, this is manifested by rales, hypoxemia, and
dyspnea (backward failure).
A number of neurally and hormonally mediated
responses develop in an attempt to compensate for inade-
quate cardiac performance. These compensatory responses
include renal-mediated fluid retention and peripheral vaso-
constriction, tachycardia, and ventricular dilation which
attempt to maintain systemic blood pressure and cardiac out-
put. However, these compensations frequently are counter-
productive and worsen hemodynamic status. For example,
vasoconstriction, while maintaining systemic blood pressure,
increases ventricular afterload, ultimately decreasing stroke
volume and cardiac output; fluid retention increases preload
(improving stroke volume), but it also raises pulmonary
venous pressure and is detrimental to oxygenation and gas
exchange. Tachycardia increases cardiac output but also
increases myocardial oxygen demand which is particularly
devastating in the setting of myocardial ischemia and
decreases diastolic time needed for optimal ventricular fill-
ing, which is particularly problematic in patients with dias-
tolic dysfunction (problems with ventricular stiffness).
It is now well recognized that vasoconstriction and tachy-
cardia, previously considered compensatory and useful to
the patient, play important roles in the progression of con-
gestive heart failure. This is why afterload-reduction therapy
with angiotensin-converting enzyme (ACE) inhibitors or
other vasodilating agents and aggressive diuretic therapy have
greatly improved survival in this disorder. Beta-adrenergic
blockade in stable patients with compensated heart failure is
useful and prolongs life by decreasing the disadvantageous
effects of adrenergic stimulation. The benefit of beta-blockers
must be weighed against worseing heart failure and should
be withheld until heart failure is well controlled.
Clinical Features
A. Symptoms and Signs—Patients with congestive heart
failure may develop symptoms slowly or acutely. They may
complain of peripheral edema or of congestive symptoms
such as dyspnea, orthopnea, or paroxysmal nocturnal dysp-
nea. Symptoms consistent with decreased cardiac output
468

CARDIAC PROBLEMS IN CRITICAL CARE
469
include fatigue and exercise intolerance. Chest pain may be a
feature of acute-onset congestive heart failure associated
with myocardial ischemia, infarction, or severe hypertension.
Because of sedation and decreased activity in the critical care
setting, ICU patients may not complain of any symptoms at
all. An increasing heart rate, decreasing oxygen saturation, or
increasing oxygen requirement may be the only clues.
Patients who present with acute pulmonary edema may
have pink frothy sputum, rales, expiratory wheezes, and cen-
tral along with peripheral cyanosis. Tachycardia and
hypotension are manifestations of decreased cardiac output;
in these patients, low output may be accompanied by periph-
eral vasoconstriction, with peripheral cyanosis, cold extrem-
ities, and diaphoresis. In patients in whom severe systemic
hypertension is causally related to congestive heart failure,
blood pressure may be high despite low cardiac output. In
patients with cardiogenic shock, hypotension is accompa-
nied by evidence of very poor peripheral perfusion. On
examination, patients with dilated cardiomyopathy may have
an S
3
gallop, a murmur consistent with mitral regurgitation,
and elevated jugular venous pressure. Other findings depend
on the specific cause and may include murmurs consistent
with valvular heart disease and an S
4
gallop. However, in an
ICU setting, many of the findings may be blunted or difficult
to appreciate. Patients with long-standing chronic heart fail-
ure may have high filling pressures and severe heart failure
without the development of rales or an S
3
owing to the devel-
opment of chronic pulmonary hypertension and other com-
pensatory mechanisms. They are in heart failure nevertheless
and respond to appropriate therapy once the diagnosis is
established.
B. Laboratory Findings—Patients may present with hypox-
emia, metabolic acidosis from lactic acidosis, and hypona-
tremia. In patients with hypotension or shock, renal and
hepatic function tests may be abnormal.
C. Electrocardiography—The ECG should be examined for
evidence of myocardial ischemia or infarction, atrial hyper-
trophy, and ventricular hypertrophy. Rhythm disturbances
(eg, atrial fibrillation or flutter) may be a cause or an effect
of congestive heart failure. Patients with dilated cardiomy-
opathy or severe left ventricular hypertrophy owing to
hypertension or hypertrophic processes may have conduc-
tion or voltage abnormalities consistent with left ventricular
hypertrophy. Tachycardia may indicate poor hemodynamic
performance.
D. Imaging Studies—
1. Chest x-ray—Chest x-ray may show cardiomegaly in
patients with dilated or hypertrophic cardiomyopathy.
However, patients with valvular heart disease may have only
a mild increase in heart size or isolated chamber enlarge-
ment. Ventricular dilatation may not be present in acutely
developing heart failure and therefore not seen on x-ray.
Cardiogenic pulmonary edema is usually marked by central
or perihilar infiltrates, increased size of vessels serving the
upper portions of the lungs in the upright position, and
increased prominence of interlobular septa—usually bilat-
eral and symmetric. Pleural effusions are common. Chest
x-rays are very important to exclude pulmonary disease that
may mimic heart failure, in particular acute respiratory
distress syndrome (ARDS) and severe pneumonia.
2. Echocardiography—Noninvasive testing, particularly
in a critically ill patient, may be difficult but gratifying if suc-
cessful in identifying a treatable cause of congestive heart
failure. Echocardiography, because of its portability, repro-
ducibility, and ability to evaluate myocardial and valvular
function, is a valuable tool in the assessment of ICU
patients. Hemodynamic data, including an estimate of right
ventricular pressure, left atrial pressure, valve areas, left ven-
tricular ejection fraction, and ventricular volumes, can be
obtained at the bedside if image quality is adequate. Cardiac
output can be estimated with echo Doppler using the conti-
nuity equation. Myocardial ischemia can be inferred by
identification of segmental wall motion abnormalities at
rest or during special interventions designed to bring out
abnormalities in ischemic regions. Dobutamine or adeno-
sine infusion can be performed with echocardiography and
ECG monitoring to obtain a bedside stress test. Pericardial
effusions can be diagnosed and measured and their hemo-
dynamic impact evaluated. Echocardiography is a sensitive
technique for diagnosing cardiac tamponade. Assessment of
valvular regurgitation and monitoring the response to ther-
apy are other uses for echocardiography.
Echocardiography is technically difficult in about 10% of
patients overall. Although echo-enhancing contrast agents can
improve image quality, ICU patients, because they are often
mechanically ventilated and have multiple intravenous or cen-
tral lines in place, are difficult to position ideally and often are
more difficult to image properly with echocardiography.
Transesophageal technology has increased the value of echocar-
diography by providing images of good quality in patients who
have had inadequate transthoracic studies. With trans-
esophageal echocardiography, the heart is imaged via a trans-
ducer inserted into the esophagus through the mouth. The close
proximity of the esophagus to the left atrium provides an excel-
lent acoustic window resulting in better images. Views unob-
tainable with conventional transthoracic echocardiography are
possible with this technique. The pulmonary veins, both atrial
appendages, and the ascending and descending aorta can be well
imaged in addition to the ventricles and valves.
3. Radionuclide angiography—Radionuclide angiogra-
phy can measure right and left ventricular ejection fractions
and evaluate wall motion. Myocardial uptake of technetium
pyrophosphate at times can be useful to identify myocardial
infarction or cardiac contusions. A number of radionuclide
techniques are used to assess coronary artery disease. These
studies are not performed at bedside and are of no utility in
ICU patients.

CHAPTER 21
470
4. CT scan—In patients who can be moved to the scanner,
CT scanning provides high-resolution tomographic imaging
of the heart and great vessels and can assess right and left
ventricular size. CT scans also can assess lung parenchyma to
rule out a primary pulmonary process and differentiate con-
gestive heart failure from other lung diseases. With the use of
contrast material, pulmonary thromboembolism or proxi-
mal pulmonary artery thrombosis can be seen with spiral CT
scanning (CT angiogram).
5. Cardiac catheterization/pulmonary artery
catheterization—When noninvasive studies cannot
fully answer questions about cardiac function, bedside
balloon-tipped flow-directed (Swan-Ganz catheter) pul-
monary artery catheterization is performed. The catheter is
used to measure a variety of hemodynamic parameters,
including left ventricular end-diastolic pressure (pul-
monary artery wedge pressure) and thermodilution cardiac
output. Newer modified catheters can continuously meas-
ure cardiac output and oxygen saturation. The catheter is
placed transvenously into the pulmonary artery by way of
the right atrium and right ventricle, usually without fluoro-
scopic guidance. The catheter is often of critical importance
in defining cardiac function and differentiating cardiac
from pulmonary disease in patients with pulmonary infil-
trates and dyspnea. The pulmonary artery catheter is par-
ticularly useful for monitoring the effect of intravenous
drugs on hemodynamics when cardiac output is low. In
patients with acute severe congestive heart failure, the goal
is to maximize cardiac output while lowering wedge pres-
sure in order to relieve pulmonary edema.
In selected patients, left-sided heart catheterization allows
direct measurement of left ventricular pressures and func-
tion, imaging of the coronary arteries to rule out critical
obstruction, and angiographic measurement of cardiac out-
put and left ventricular ejection fraction. Left-sided heart
catheterization requires fluoroscopy and cannot be done in
most ICUs.
Differential Diagnosis
Patients with clinical features of congestive heart failure pre-
senting with dyspnea, orthopnea, rales, and wheezing instead
may have pneumonia, ARDS, fluid overload, or exacerbation
of chronic obstructive pulmonary disease (COPD) or
asthma. Cardiomegaly may be due to ventricular hypertro-
phy, right ventricular dilatation, or pericardial effusion
rather than an enlarged left ventricle itself. In patients who
present with symptoms and signs of primarily right-sided
heart failure—such as elevated jugular venous pressure,
ascites, edema, and evidence of right ventricular hypertrophy—
lung disease resulting in cor pulmonale, or pulmonary arte-
rial hypertension (eg, pulmonary arteriopathy, idiopathic or
secondary pulmonary arterial hypertension, or pulmonary
emboli) should be considered. Patients with hypotension
from cardiac failure should be distinguished from those with
volume depletion, sepsis, and pulmonary embolism.
Treatment
A. General Measures—After determining the underlying
cause of congestive heart failure, treatment in the ICU con-
sists of quickly reversing the hemodynamic problem without
adding further ones. In very ill patients, initial management
of congestive heart failure should use intravenous medica-
tions. In this form, medications can be titrated rapidly and
stopped quickly if necessary. Intravenous administration of
drugs guarantees absorption, particularly in patients with
bowel edema and decreased bowel motility. Although some
intravenous agents have long half-lives and slow onsets of
action, nitroprusside, nitroglycerin, nesiritide, dopamine,
dobutamine, and milrinone act quickly and are easily reversed.
Cardiogenic shock may require the initial or concomitant
use of vasopressor drugs such as dopamine and inotropic
drugs such as dobutamine or milrinone to allow the institu-
tion of afterload-reduction therapy. Nitroprusside is a potent
reducer of left ventricular afterload and is particularly valu-
able in treating severe congestive heart failure. Disadvantages
include toxicity in patients with renal insufficiency who are
given nitroprusside over a prolonged period of time.
Intravenous preparations of ACE inhibitors are effective and
have longer durations of action. Digoxin and diuretics are still
important despite development of newer classes of drugs.
Because of negative inotropic effects, calcium channel block-
ers and beta-blockers are used with extreme caution, if at all,
in patients with acute congestive heart failure. Occasionally,
however, congestive heart failure may be secondary to tach-
yarrhythmias, left ventricular diastolic dysfunction, or severe
transient ischemia, and these drugs then play an important
role. Close hemodynamic monitoring, usually with a pul-
monary artery catheter, allows the physician to titrate multi-
ple drugs optimally. In cases of severe cardiogenic shock with
low cardiac output, use of mechanical devices including
intraaortic balloon pump or left ventricular assist devices is a
consideration. The use of these devices involves decisions
regarding long-term treatment options, prognosis, and
underlying disease etiologies. The decision to intervene at this
level requires consultation with a cardiac catheterization team
and the heart transplant team or heart failure specialists.
General treatment of congestive heart failure in critically
ill patients includes oxygen, bed rest, and reduction of meta-
bolic derangements that increase myocardial oxygen demand
(eg, fever and anemia). Endotracheal intubation and
mechanical ventilation usually are not necessary, except in
severe cardiogenic pulmonary edema.
B. Specific Treatment of Congestive Heart Failure—
Patients with congestive heart failure can be subdivided into
several groups for which specific treatments can be described
as follows:
1. Systolic dysfunction without hypotension—These
patients have low stroke volumes and ejection fractions and
usually have tachycardia. Pulmonary edema may accompany
systolic dysfunction. Digoxin, diuretics, and ACE inhibitors are
the mainstays of therapy. Several studies have shown that ACE
CARDIAC PROBLEMS IN CRITICAL CARE
471
inhibitors prolong life in patients with chronic congestive heart
failure owing to left ventricular dysfunction and in patients
with myocardial infarction associated with reduced left ventric-
ular function. If the patient is felt to be stable enough to toler-
ate oral therapy, small doses of an ACE inhibitor and digoxin
can be initiated. Hypotension may accompany ACE inhibitor
therapy if cardiac output fails to increase after vasodilation, and
inotropic drug support of blood pressure may be required.
Withholding or reducing the dosage of diuretics when ACE
inhibitors are added often can prevent the development of
hypotension. Serum creatinine and potassium levels must be
observed carefully because of the effect of ACE inhibitors on
renal function (particularly in patients with renal artery steno-
sis) and on the renin-aldosterone system.
Diuretics are useful in reducing volume overload, partic-
ularly when signs of right-sided failure such as peripheral
edema, elevated jugular venous pressure, and liver engorge-
ment are present. Intravenous furosemide can be given in a
dose of 10–80 mg (more in patients with poor response) and
repeated as needed. Continuous infusion of furosemide at a
rate of 5–10 mg/h is also effective. Metolazone or
hydrochlorothiazide can augment the effectiveness of
furosemide by further inhibiting reabsorption of sodium.
Sustained diuresis with any of these agents is associated with
significant loss of potassium and magnesium. Nesiritide is a
recombinant human B-type natriuretic peptide that is indi-
cated for intravenous treatment of acutely decompensated
congestive heart failure. It is given as an initial bolus of 2 μg/kg,
followed by continuous infusion of 0.01 μg/kg per minute
for less than 48 hours. Hypotension is a known side effect.
Spironolactone has been shown to decrease mortality in
chronic congestive heart failure and can be added to help
spare potassium loss in the acute situation. Finally, patients
in severe congestive heart failure with renal dysfunction may
be unable to excrete large amounts of sodium and water, so
ultrafiltration may be needed to correct volume overload.
Newer devices allow removal of fluid at rates up to 400 mL/h
using specially designed 18-gauge peripheral lines and there-
fore eliminate the need for a large-bore vascular catheters.
However, if electrolyte abnormalities and renal dysfunction
compound the volume overload, dialysis may be required.
Noninvasive positive-pressure ventilation using tight-fitting
masks can be useful in acute pulmonary edema. A significant
reduction in the need for mechanical ventilatory support has
been demonstrated in patients present with acutely decompen-
sated congestive heart failure with the use of this noninvasive
form of ventilation compared to standard therapy. It appears
that the positive-pressure breathing lowers preload and left
ventricular afterload, improves oxygenation, and provides time
for pharmacologic therapy to work.
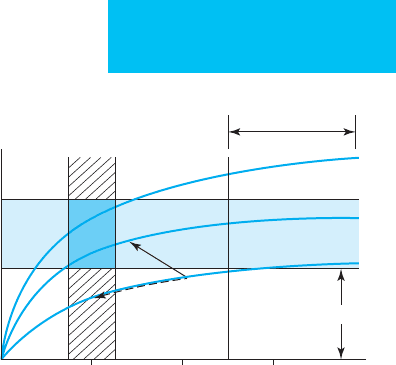
The effect of various drugs on filling pressures and cardiac
output can be demonstrated on the Frank-Starling curve
(Figure 21–1). Both digoxin and afterload-reducing agents
improve the patient’s cardiac output or stroke volume for a
given filling pressure (move the patient to a more effective
curve). In contrast, diuretics lower the left ventricular filling
pressure, relieving symptoms of dyspnea, but they also may
reduce cardiac output. The patient moves down along the
same function curve. Optimal treatment, therefore, should use
agents that move the patient to a better function curve, and
diuretics are employed to help lower filling pressures—if
they remain elevated—and to expedite symptomatic improve-
ment. In some patients with mild to moderate congestive heart
failure, bed rest alone will result in significant diuresis. In addi-
tion, improvement of cardiac output with afterload-reducing
agents and digoxin ultimately will result in diuresis. On the
other hand, both preload- and afterload-reducing agents can
result in venodilation and thus fluid retention, so diuretics
may be needed to counteract this unwanted side effect.
Although major emphasis has been placed on ACE
inhibitors in the treatment of chronic congestive heart fail-
ure, other drugs are effective, including preload-lowering
agents such as nitrates and afterload-reducing agents such as
hydralazine. For example, the combination of hydralazine
and nitrates has been shown to prolong life in patients with
chronic congestive heart failure.
2. Severe congestive heart failure with hypotension
(cardiogenic shock)—Patients with severe congestive
heart failure associated with hypotension, pulmonary
edema, and metabolic acidosis require aggressive and immediate
10 20 30
End-diastolic pressure (mm Hg)
Low output
1
2
3
Pulmonary edema
Normal
Stroke volume
Normal
Figure 21–1. Curves demonstrating the relationship
between stroke volume and left ventricular end-diastolic
pressure (preload) and showing the normal range for each
variable. End-diastolic pressures greater than 25 mm Hg
are associated with pulmonary edema. Curve 1 represents
severely depressed left ventricular function, with normal
stroke volume being achieved only at substantially ele-
vated preload (high left ventricular end-diastolic pressure).
Curve 2 demonstrates a normal relationship between
stroke volume and preload. Curve 3 represents a condition
of increased inotropy. Treatment with afterload-reducing
agents or inotropic drugs can improve stroke volume by
moving an individual from curve 1 to curve 2 (solid
arrow). Diuretics can lower filling pressure by moving a
patient along his or her own curve (dashed arrow).

CHAPTER 21
472
intervention. These patients often have some reason for acute
deterioration such as ischemia, myocardial infarction, new or
worsening valvular insufficiency, poor adherence to medical
therapy, volume overload, or concomitant medical problems.
Even before invasive hemodynamic monitoring is instituted,
hemodynamic support can be started using intravenous
agents. With severe hypotension, blood pressure support is
required—intravenous dopamine should be administered in
dosages titrated to achieve a systolic blood pressure of approx-
imately 90 mm Hg or greater. An exception to this precept
would be a patient with cardiomyopathy whose known systolic
blood pressure is chronically 80 mm Hg. In such cases, clinical
markers of hypoperfusion such as decreased mental status or
acidosis should help to determine the appropriate blood pres-
sure goal. The inotropic drugs dobutamine and milrinone can
be used in conjunction with or as an alternative to dopamine to
increase cardiac output. Dobutamine has the further advantage
of peripheral vasodilation with reduction in left ventricular
afterload.
In patients with either adequate blood pressure (systolic
blood pressure >100 mm Hg) or even marginal pressure (sys-
tolic pressure 90–100 mm Hg), nitroprusside can be started at
small dosages (0.01–0.1 μg/kg per minute) and titrated upward
every 3–5 minutes while blood pressure is observed closely.
Although these are low starting doses, they may avoid the signif-
icant and rapid hypotension that sometimes occurs with larger
doses, and rapid dose adjustments make it possible to reach the
effective dose in a relatively short period. The goal of reducing
left ventricular afterload with nitroprusside is to increase cardiac
output. However, if peripheral resistance drops in response to
nitroprusside without an increase in cardiac output, hypoten-
sion will occur. The drop in blood pressure following nitroprus-
side administration can be dealt with by immediately
discontinuing the drug and providing inotropic support if
needed. The extremely short half-life of intravenous nitroprus-
side makes this a safe and valuable agent to try even before inva-
sive hemodynamic monitoring can be started.
Loop diuretics are also extremely valuable in this setting if
marked volume overload (pulmonary edema) is evident, as
furosemide causes a lowering of preload even before diuresis
occurs. Intravenous furosemide can be given in a dose of 10
to 40 mg (more in patients with poor response) and can be
repeated as needed. Continuous infusion of furosemide at a
rate of 5–10 mg/h is also very effective. Intravenous nitroglyc-
erin has preload-reducing as well as some afterload-reducing
properties and can be used alone or in conjunction with
intravenous nitroprusside to improve cardiac output and
reduce left-sided pressures. Nesiritide must be used with cau-
tion in cardiogenic shock to avoid worsening of hypotension.
Intraaortic balloon pumps and left ventricular assist
devices have been used to treat patients with extreme cardio-
genic shock. They are used acutely to allow time to explore
opportunities for additional interventions including angio-
plasty, cardiac surgery, or heart transplantation. This level of
tertiary management is undertaken in referral centers with
appropriate equipment, resources, and surgical staff and in
selected patients with potential for good outcomes.
Echocardiography assists in the management of patients
with cardiogenic shock in several ways: (1) by identifying surgi-
cally correctable valvular abnormalities such as severe aortic or
mitral valvular disease that may be contributing to failure, (2) by
identifying segmental wall motion abnormalities suggestive of
ischemia, and (3) by establishing baseline left ventricular func-
tion in patients with new onset congestive heart failure.
A pulmonary artery catheter will enable the physician to
adjust medications more carefully, with the goal of maximizing
cardiac output at acceptably high end-diastolic filling pressures.
The pulmonary artery catheter is strongly recommended to
help guide the management of congestive heart failure patients
who have hypotension and congestive symptoms. Using a pul-
monary artery catheter, a cardiac index (cardiac output divided
by body surface area) of less than 2 L/min/m
2
is considered car-
diogenic shock and is incompatible with prolonged survival.
Heart rate and cardiac output need to be considered in optimiz-
ing hemodynamics, particularly in patients with congestive
heart failure and myocardial ischemia. If an adequate cardiac
index is maintained by an increased heart rate rather than
improved stroke volume, ultimate outcome will be poor.
Conversely, patients with bradycardia in the setting of conges-
tive heart failure may have dramatically improved cardiac out-
put with a pacemaker or the use of pharmacologic agents that
increase the heart rate.
Calculation of stroke volume to assess therapy is very use-
ful. The mixed venous oxygen (O
2
) saturation (S
–
v
O
2
) is another
way of assessing severity of disease and response to therapy. It
reflects delivery and utilization of O
2
and the effectiveness of
cardiac output. Some pulmonary artery catheters have an
oximeter probe at their tips to continuously monitor S
–
v
O
2
in
addition to pulmonary artery pressures. A decrease in S
–
v
O
2
can
be an early marker of decreased cardiac output and function. A
desirable goal of therapy in treating cardiogenic shock is to
attain a mixed venous O
2
saturation of greater than 70%.
After optimizing hemodynamic variables with intravenous
medications and attaining a period of stability, a gradual change
to oral medication is appropriate. Oral afterload-reducing agents
(eg, ACE inhibitors, angiotensin-receptor blockers, or hydralazine)
should be added while reducing the dosages of intravenous
agents. An intravenous ACE inhibitor such as enalaprilat given
every 6 hours is an alternative to oral ACE inhibitors.
3. Congestive heart failure with severe systemic
hypertension—Treatment is directed at the pathophysio-
logic mechanisms of congestive heart failure in severe hyper-
tension, including reduction of systemic blood pressure and
intravascular volume. In these patients, left ventricular sys-
tolic function may be normal, whereas left ventricular dias-
tolic dysfunction is a major problem resulting in congestion
and pulmonary edema. Systolic dysfunction, if present, may
improve significantly following afterload reduction.
Control of blood pressure with reduction of left ventric-
ular afterload is the major focus of initial therapy. If systolic
function is unknown, an intravenous agent such as nitro-
prusside or nitroglycerin is recommended to lower systemic
pressures and to improve filling pressures acutely. Intravenous

CARDIAC PROBLEMS IN CRITICAL CARE
473
enalaprilat also can be considered (see the section “Hypertensive
Crisis”). For continued treatment of hypertension, β-adrenergic
blockers or calcium channel blockers can be added after conges-
tive heart failure has improved and acceptable left ventricular
systolic function has been documented. However, these agents
should be used with caution in patients with high filling pres-
sures and severe hypertension because they may depress
myocardial function without adequately reducing the afterload.
The net result may be worsening congestive heart failure or
hemodynamic collapse. Pulmonary artery catheterization may
be helpful when considering the use of β-adrenergic blockers or
calcium channel blockers in these patients, but catheterization is
not needed to initiate therapy with nitroprusside unless
hypotension develops early in treatment, raising the possibility
of complicating cardiac or pulmonary problems.
4. High-output or volume-overload congestive heart
failure—These patients present with congestive symptoms
and signs (eg, pulmonary edema and peripheral edema), but
systolic cardiac function is normal, and cardiac output may be
elevated. Treatment should be directed at the cause of the high
cardiac output (eg, anemia, thiamine deficiency, sepsis, and
hyperthyroidism) or volume overload state (eg, renal failure,
iatrogenic volume overload, and excessive sodium intake).
Rapid lowering of intravascular volume by ultrafiltration may
improve blood pressure, hypoxemia, and edema, especially in
patients who do not respond well to diuretic therapy. In the
ICU patient, volume overload may be due to obligate fluid
intake from hyperalimentation, blood product replacement, or
antibiotic therapy.
5. Congestive heart failure with diastolic dysfunc-
tion—Diastolic dysfunction means that ventricular filling is
impaired, and left ventricular end-diastolic pressures may be
elevated. Diastolic dysfunction is the most difficult form of
heart failure to treat. Systolic function is preserved, but ven-
tricular relaxation and filling are inadequate. Diastolic dys-
function is seen commonly in patients who have
hypertension with left ventricular hypertrophy and/or
ischemia. Patients with hypertrophic cardiomyopathy also
can have significant diastolic heart failure with preserved sys-
tolic function. Elderly patients can have undiagnosed diastolic
heart failure with or without systemic hypertension. Patients
with amyloidosis also have low ventricular compliance
resulting in diastolic dysfunction, but systolic dysfunction
often accompanies this clinical picture. Patients with dias-
tolic dysfunction have congestive symptoms (eg, shortness
of breath and pulmonary edema) despite normal ejection
fraction and normal systolic wall motion. Diuretics usually
are required to reduce preload and symptoms related to
elevated left atrial pressure. Beta-adrenergic blockade to
slow the heart rate, allowing more time for diastolic filling,
can be helpful. On occasion, too aggressive diuretic therapy
becomes counterproductive in patients with diastolic dys-
function by reducing stroke volume, systemic blood pres-
sure, and cardiac output. Because cardiac output is the
product of heart rate and stroke volume, excessive bradycardia
from beta-blockers or calcium channel blockers also can
worsen the clinical situation by causing an inadequate cardiac
output.
6. Isolated right-sided heart failure with pulmonary
hypertension—Patients may have isolated right-sided heart
failure secondary to pulmonary arterial hypertension (PAH).
Pulmonary hypertension may be related to congenital heart
disease, lung disease , medications, liver disease (eg, portopul-
monary hypertension), HIV infection, and collagen vascular
diseases (eg, scleroderma and mixed connective tissue disease)
or may be idiopathic. PAH owing to pulmonary emboli or
proximal pulmonary arterial thrombus need to be considered
and excluded with appropriate diagnostic tests before conclud-
ing that pulmonary hypertension is due to a pulmonary arteri-
opathy. Pulmonary venous hypertension also must be excluded
(ie, left-sided heart disease). In PAH, the pathophysiologic
mechanism of the dyspnea and orthopnea is not entirely clear,
although gas exchange in the lungs is inefficient because of
maldistribution of perfusion. Compression of the left ventricle
with abnormal septal motion and relative left ventricular filling
difficulties because of right ventricular encroachment into the
pericardial space is another possible mechanism.
Diuretics are used to reduce right atrial pressure and
right ventricular and right atrial volume. Oxygen may
reduce pulmonary hypertension in patients with PAH or
lung diseases. As oxygenation improves, liver engorgement,
abdominal distention, and lung mechanics improve. One
goal is to reduce right atrial pressure to less than 10 mm Hg.
Finally, digoxin may be helpful by increasing right ventricu-
lar function. Reduction of pulmonary artery pressures and
right ventricular afterload with nitric oxide or intravenous
prostacyclin should be considered when a clear diagnosis of
PAH is made (in the absence of left-sided heart failure). In
the last 3 to 4 years, there have been dramatic advances in the
treatment of PAH in terms of chronic management, includ-
ing the use of endothelin-receptor blockers (eg, bosentan),
phosphodiesterase-5 inhibitors (PDE-5) including sildenafil,
and prostacyclins (eg, epoprostenol, treprostinol, and ilo-
prost). Acute treatment with inhaled nitric oxide can restore
oxygenation and stabilize a patient until long-term treat-
ment issues can be addressed. This is in the realm of tertiary
care at institutions able to administer such therapy.
Abraham WT et al: In-hospital mortality in patients with acute
decompensated heart failure requiring intravenous vasoactive
medications: An analysis from the Acute Decompensated Heart
Failure National Registry (ADHERE). J Am Coll Cardiol
2005;46:57–64. [PMID: 15992636]
Bradley TD et al: Continuous positive airway pressure for central
sleep apnea and heart failure. N Engl J Med 2005;353:2025–33.
[PMID: 16282177]
Fonarow GC et al: Characteristics, treatments, and outcomes of
patients with preserved systolic function hospitalized for heart
failure: A report from the OPTIMIZE-HF Registry. J Am Coll
Cardiol 2007;50:768–77. [PMID: 17707182]
Hunt SA et al: ACC/AHA 2005 guideline update for the diagnosis
and management of chronic heart failure in the adult.
Circulation 2005;112:e154–235. [PMID: 16160202]
CHAPTER 21
474
Jessup M et al: Heart failure. N Engl J Med 2003;348:2007–18.
[PMID: 12748317]
Mehra MR: Optimizing outcomes in the patient with acute decompen-
sated heart failure. Am Heart J 2006;151:571–9. [PMID: 16504617]
Onwuanyi C, Taylor M: Acute decompensated heart failure:
Pathophysiology and treatment. Am J Cardiol 2007;99:25–30D.
[PMID: 17378992]
Peter JV et al: Effect of non-invasive positive pressure ventilation
(NIPPV) on mortality in patients with acute cardiogenic pul-
monary edema: A meta-analysis. Lancet 2006;367:1155–63.
[PMID: 16616558]
Publication Committee for the Vasodilatation in the Management
of Acute CHF (VMAC) Investigators: Intravenous nesiritide vs
nitroglycerin for treatment of decompensated congestive heart
failure: A randomized, controlled trial. JAMA 2002;287:
1531–40. [PMID: 11911755]
Yancy CW et al: Clinical presentation, management, and in-hospital
outcomes of patients admitted with acute decompensated heart
failure with preserved systolic function: A report from the Acute
Decompensated Heart Failure National Registry (ADHERE)
Database. J Am Coll Cardiol 2006;47:76–84. [PMID: 16386668]
Zile MR, Baicu CF, Gaasch WH: Diastolic heart failure:
Abnormalities in active relaxation and passive stiffness of the left
ventricle. N Engl J Med 2004;350:1953–9. [PMID: 15128895]
Valvular Heart Disease
ESSENTIALS OF DIAGNOSIS
Valvular insufficiency:
Dyspnea, pulmonary edema, new murmur.
Echocardiogram with Doppler demonstrating regurgitation.
Valvular stenosis:
Dyspnea, pulmonary edema, murmur, syncope,
hypotension; decreased carotid pulses (aortic stenosis).
Atrial fibrillation (mitral stenosis), left ventricular
hypertrophy (aortic stenosis).
Echocardiogram documenting decreased valve area.
Prosthetic valve dysfunction:
New onset of symptoms of congestive heart failure,
syncope; change in examination (new murmur,
change in intensity of valve sounds).
Echocardiographic evidence of increased valve pres-
sure gradient, thrombosis, or other dysfunction.
Infective endocarditis:
May or may not have history of valvular heart dis-
ease or prosthetic valve.
New onset of heart failure with valvular insufficiency
or unexplained fever and pathologic heart murmur.
Echocardiographic evidence of valvular disease, pos-
itive blood cultures.
General Considerations
As with congestive heart failure, treating valvular heart dis-
ease in the ICU setting involves considering the possibility
and proceeding to assess its severity. Few ICUs can afford the
luxury of a quiet place to auscultate the heart, but with
patience and perseverance, the experienced clinician can
detect important murmurs. The acoustic qualities of the
murmurs are affected by cardiac output. Patients in shock
with low-output states and febrile or anemic patients with
high-output states may present with misleading physical
findings that under- or overestimate the severity of their
valvular heart disease. At the bedside, echocardiography
affords the physician a convenient window on the heart and
a way to quantitate valve dysfunction and clarify the relation-
ship between valve function and myocardial function.
Acute valvular insufficiency with regurgitation may be
due to endocarditis, trauma, papillary muscle dysfunction
(mitral valve), or ischemia. Patients may present with wors-
ening of chronic valvular disease from myxomatous degener-
ation or prolapse with and without connective tissue
disorders or rheumatic heart disease. Isolated aortic valve
insufficiency may be due to aortic diseases such as aortic dis-
section, cystic medial necrosis, and syphilitic aortitis. Most
commonly, however, chronic aortic regurgitation results
from a congenital bicuspid aortic valve. Mitral stenosis is
almost always due to rheumatic heart disease. Aortic stenosis
is occasionally due to rheumatic heart disease but more often
is due to progressive valvular calcification in the elderly,
either of a normal valve or of a congenital bicuspid valve.
Patients with previous valve surgery with prosthetic or
bioprosthetic valves represent a special circumstance. These
valves are subject to a variety of chronic and acute complica-
tions, including infective endocarditis, calcification with
simultaneous stenosis and incompetence, thrombosis with
valve dysfunction, and peripheral embolic events such as
strokes, valve dehiscence, and paravalvular leaks. Valve
repairs also can be subject to some of the same problems,
including endocarditis, recurrent valve dysfunction, and rel-
ative valve stenosis, after repair of valvular regurgitation.
Clinical Features
A. Symptoms and Signs—Specific findings depend on
which valve is abnormal. Patients with aortic or mitral valvu-
lar stenosis or insufficiency may present with congestive heart
failure, including pulmonary edema and evidence of
decreased cardiac output. Physical findings include rales, S
3
gallop, wheezing, peripheral vasoconstriction, tachycardia,
and murmurs. Other important findings to be sought include
the character of arterial pulses, intensity of the heart sounds,
and changes in the quality of murmurs with different maneu-
vers such as the Valsalva maneuver. Chest pain is a frequent
accompanying symptom in patients with significant aortic
stenosis or aortic regurgitation. Atrial arrhythmias frequently
accompany mitral valve disease with left atrial enlargement.

CARDIAC PROBLEMS IN CRITICAL CARE
475
B. Electrocardiography—The ECG may suggest features of
specific valvular as heart diseases—for example, left ventric-
ular hypertrophy as seen in aortic stenosis and regurgitation,
and left atrial enlargement and right ventricular hypertrophy
as seen in mitral stenosis.
C. Imaging Studies—The chest x-ray may show cardiomegaly
with specific chamber enlargement. Echocardiography is
extremely useful in assessing valvular heart disease. It can
provide evidence of leaflet abnormalities, including vegeta-
tions and decreased motion of valve leaflets, as well as esti-
mates of valve cross-sectional area in valvular stenosis. The
size of the atria and ventricles can be determined and wall
motion and ejection fraction estimated. With Doppler tech-
niques, one can quantitatively estimate regurgitant blood
flow across an abnormal valve, measure valve pressure gradi-
ents and calculate valve areas.
D. Additional Studies—Pulmonary artery catheters directly
measure pulmonary artery pressures and cardiac output and
provide an estimate of left atrial pressure (pulmonary artery
wedge pressure). Cardiac catheterization is usually required
to assess valve function prior to surgery and to identify coex-
istent coronary artery disease.
Treatment: Native Valves
A. Valvular Regurgitation—The management of left-sided
valvular regurgitation is determined by the severity of the
regurgitation, the specific cause, and the degree of left ven-
tricular dysfunction. The severity of regurgitation can be
estimated echocardiographically using color-flow and
continuous-wave Doppler and calculating left ventricular
and left atrial pressures noninvasively. Echocardiography
also will help to define operability and determine the cause
of the valve dysfunction. Mild to moderate aortic or mitral
regurgitation without symptoms requires no treatment. In
patients with more severe left-sided valvular regurgitation,
associated congestive heart failure (pulmonary edema) can
be treated with diuretics and digoxin. However, the most
important therapy is the use of unloading agents such as
ACE inhibitors, hydralazine, and, if needed, nitroglycerin
and nitroprusside. These drugs work by decreasing down-
stream resistance and increasing downstream compliance.
Forward blood flow increases while regurgitant flow
decreases, so ventricular filling pressures decline while car-
diac output improves. The management of congestive heart
failure owing to aortic or mitral regurgitation is quite similar
to the management of congestive heart failure owing to sys-
tolic ventricular dysfunction.
In patients with such severe valvular regurgitation that
cardiac output is very low and there is hypotension (cardio-
genic shock), emergent valve surgery may be necessary.
Invasive hemodynamic monitoring with a pulmonary artery
catheter is essential, and maximal unloading of the left ventri-
cle with intravenous nitroprusside should be started immedi-
ately. Inotropic drugs such as dopamine may be required to
maintain adequate systemic blood pressure even though—by
increasing afterload—valvular regurgitation may be tran-
siently worsened. Mitral regurgitation associated with car-
diogenic shock may benefit from an intraaortic balloon
pump, but this therapy is contraindicated in those with aor-
tic valve regurgitation.
B. Valvular Stenosis—Aortic stenosis is treated with sur-
gery when it results in congestive heart failure. Choices for
medical management are limited, but possible pharmaco-
logic interventions include mild diuresis and the use of
digoxin. Systemic vasodilators, useful in other forms of heart
failure, may cause severe hypotension in patients with aortic
stenosis. In selected patients with combined stenosis and
ventricular dysfunction, judiciously used intravenous
unloading therapy has been employed with hemodynamic
monitoring. This type of hemodynamic manipulation is per-
formed in the catheterization laboratory or under the guid-
ance of a cardiologist and is not the standard of care.
Dopamine can be tried if shock develops, but by this time,
surgery is essential. A rapid and limited search for confound-
ing problems can be undertaken to try to find ways to
improve the patient acutely. Atrial fibrillation, for example,
because it results in a decrease in left ventricular filling in the
patient with severe aortic stenosis, should be treated aggres-
sively with the goal of returning the patient to sinus rhythm.
Successful cardioversion of atrial fibrillation may result in
acute improvement in cardiac output.
Severe mitral stenosis is also a surgical problem, although
it is somewhat more amenable to pharmacologic therapy. The
most important goal is to decrease the heart rate, thereby pro-
longing diastolic filling time and allowing the left atrium to
empty. Left atrial pressure and, therefore, pulmonary venous
pressure are determined by the degree of left atrial emptying.
In patients with mitral stenosis, left atrial emptying is limited
by decreased mitral orifice size, and the smaller the valve area,
the longer it takes for the atrium to empty. Inadequate time
for emptying leads to increased left atrial pressure and vol-
ume and worsening pulmonary congestion. Thus, by slowing
the heart rate and lengthening diastole, the left atrium has
more time in which to empty. Therefore, if left ventricular
function is preserved and there is only mild to moderate
mitral regurgitation, heart rate control using beta-blockers or
calcium channel blockers (or digoxin, if the patient has atrial
fibrillation) often will greatly improve symptoms.
Treatment: Prosthetic Valves
A. Transvalvular Dysfunction of Prosthetic Valves—This
entity can be a true medical emergency resulting in rapid
deterioration of a stable patient and can lead to death if not
recognized and treated promptly. Bioprosthetic valves tend
to calcify and become both stenotic and incompetent over
time. Once the valve becomes dysfunctional, further progres-
sion can be rapid, with a rigid leaflet suddenly becoming
severely incompetent and producing fulminant congestive

CHAPTER 21
476
heart failure. Mechanical prosthetic valves are more durable,
with, for example, Starr-Edwards valves (ball-cage valves)
functioning for more than 30 years. However, ingrowth of
tissue (pannus formation) or thrombosis secondary to inad-
equate anticoagulation can result in the development of valve
dysfunction with either obstruction, regurgitation, or both
depending on where the tissue ingrowth or clot develops.
Progressive thrombosis, particularly on a single-leaflet
mechanical valve, can result in death because the valve may
stick in the closed position. The St. Jude valve, because it is a
bileaflet device, usually develops both insufficiency and
stenosis. Other less frequent problems have resulted from
mechanical damage to the valve, such as strut fracture with
Björk-Shiley-type valves and loss of poppets owing to ball
variance and fractures in the older Starr-Edwards valves. In
evaluating patients with suspected prosthetic valve dysfunc-
tion, physical examination may show evidence of congestive
heart failure. The murmurs that accompany the prosthetic
valve may be fainter than usual because of low cardiac out-
put or high filling pressures. The key to the diagnosis of pros-
thetic valve dysfunction is a high degree of clinical suspicion
and noninvasive assessment of valvular function. Patients
with prosthetic valves who present with worsening heart fail-
ure should undergo Doppler evaluation of the valves to
assess gradients across the valves and to estimate valve area.
Transesophageal echocardiography is extremely useful in this
setting and can confirm valve obstruction by demonstrating
the presence of a clot and reduced prosthetic leaflet motion.
A large pressure gradient across the valve or the presence of
substantial transvalvular regurgitation is suggestive of valve
thrombosis. Cinefluoroscopy can be used to assess opening
angles of the mechanical prosthetic valves by measuring the
angle on still frames. The angle of opening for specific valve
models is known. If the valve does not open to the expected
amount, valve dysfunction and thrombosis can be suspected.
Treatment includes immediate heparinization if throm-
bosis is suspected, hemodynamic monitoring, and surgical
evaluation for urgent valve replacement. Valve replacement is
critical and can be lifesaving. Patients who present with
severe heart failure in this setting sometimes can be helped
dramatically by use of thrombolytic agents, including
alteplase or streptokinase. Risks of thrombolytic therapy
include embolization of lysed clots and CNS hemorrhage,
but the risks may have to be accepted when cardiogenic
shock occurs secondary to valve thrombosis and surgery is
considered too hazardous. Results with alteplase can be seen
within 90 minutes. Heparinization must be continued after
thrombolytic therapy to prevent immediate thrombosis.
B. Emboli—Thrombi forming on prosthetic valves are a
source of thromboemboli, which can cause complications
based on where the emboli lodge, including strokes, renal
infarction, ischemic limbs, pulmonary emboli, and coronary
artery occlusion. Emboli occur uncommonly in anticoagu-
lated patients; however, inadequate anticoagulation or discon-
tinuation of anticoagulation—particularly with mechanical
valves—can result in embolic events. Treatment is supportive
with use of intravenous anticoagulation for treatment of
peripheral embolization and prevention of further emboli.
Surgical removal of emboli can be performed if they are in
accessible locations, such as in limb vessels. In patients who are
already adequately anticoagulated with warfarin, the addition
of aspirin or dipyridamole has been shown to decrease the fre-
quency of recurrent embolization.
In patients with cerebral emboli, the decision to anticoag-
ulate may be difficult because of the risk of conversion of a
bland embolic stroke to a hemorrhagic one. Most neurolo-
gists recommend waiting 48–72 hours before anticoagulating
such patients unless the concern for recurrent emboli is felt
to outweigh these risks. Finally, surgical replacement of a
partially thrombosed valve in a patient with stroke is associ-
ated with a very high risk of perioperative intracerebral hem-
orrhage owing the combination of low cerebral perfusion
and the need for heparin during the procedure.
C. Paravalvular Leaks and Valve Dehiscence—Valve dehis-
cence is another form of valve dysfunction seen with both bio-
prosthetic and mechanical valves. The artificial valve is attached
to the myocardium or to the annulus where the native valve
previously resided. Paravalvular leaks can be a result of techni-
cal problems occurring at the time of surgery or may develop
years later as a result of prosthesis infection (endocarditis).
Paravalvular leaks are a result of space developing between the
sewing ring of the valve and the annulus or cardiac tissue.
Small, hemodynamically insignificant leaks are often seen as a
result of minor surgical imperfections and can remain stable
for years. Paravalvular leaks secondary to infective endocarditis
often are associated with valve dehiscence, and these paravalvu-
lar leaks tend to progress—often rapidly. This results in severe
hemodynamic dysfunction, further dehiscence of the valve,
instability of the valve, and frequently, hemolysis owing to
mechanical destruction of red blood cells as they pass through
the disordered valve. However, paravalvular leaks can develop
over time even in the absence of infection.
Development of a paravalvular leak in the setting of
endocarditis is a surgical emergency. Complications include
progressive uncontrollable congestive heart failure, sepsis,
and complete dehiscence of the valve resulting in death.
Echocardiography—particularly transesophageal—or car-
diac catheterization is required to define the severity of the
valve lesions, assess overall cardiac function, and guide valve
replacement. In the absence of infection, the decision with
regard to valve replacement is determined by the degree of
regurgitation and associated heart failure. Paravalvular leaks
that increase over time suggest instability of the valve and
necessitate valve replacement.
Treatment: Infective Endocarditis (Prosthetic
or Native Valve)
Infective endocarditis is a pleomorphic disease that can be
rapidly progressive when caused by invasive organisms or
can be slowly progressive and debilitating resulting in
