Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CRITICAL CARE OF THE ONCOLOGY PATIENT
457
METABOLIC DISORDERS
Hypercalcemia of Malignancy
ESSENTIALS OF DIAGNOSIS
Mental status changes, lethargy, confusion, weakness.
Altered deep tendon reflexes without localized neuro-
logic signs.
History of malignancy, usually far-advanced.
Elevated serum calcium, chloride:phosphate ratio, and
(often) parathyroid hormone–related polypeptide
(PTHrP).
General Considerations
Hypercalcemia is the most serious metabolic disorder associ-
ated with cancer. Between 10% and 20% of patients with can-
cer will develop hypercalcemia at some point, and life
expectancy is poor in these patients, even when they are
actively treated. Treatment of hypercalcemia of malignancy is
usually palliative because most of these patients have
advanced disease. However, symptoms are usually improved
with treatment, and many patients may be made well enough
to go home from the hospital. While treatment of hypercal-
cemia may not prolong survival, it clearly improves quality
of life.
Pathogenesis
Serum calcium is regulated by hormones and locally acting
cytokines at three main sites: the gut, the skeletal system, and
the kidneys. Parathyroid hormone (PTH) increases the num-
ber and function of osteoclasts, inhibits osteoblasts, and
increases renal tubular reabsorption of calcium, all of which
increase extracellular calcium levels. The hormone also
increases production of active vitamin D, which increases the
absorption of calcium from the gut.
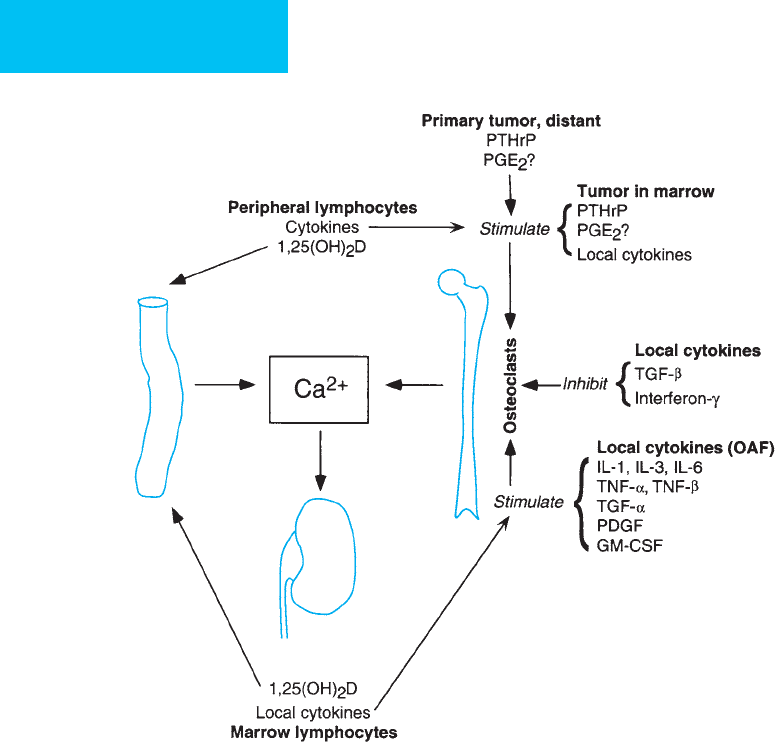
In all cases of cancer-related hypercalcemia, there is
increased calcium resorption from bones relative to bone
formation (Figure 20–1). Increased bone resorption is
maintained through the destructive action of tumor cells by
increased osteoclast activation mediated through the action
of PTH-related polypeptide (PTHrP) and by locally acting
cytokines. Squamous cell carcinomas originating in the
lung, head and neck, esophagus, uterine cervix, vagina, and
penis—as well as cancers of the breast, lung, and kidney—
produce PTHrP. This hormone shares homology with the
amino-terminal portion of parathyroid-produced PTH
only in 8 of the first 13 amino acids. It has predicted iso-
forms of 139, 141, and 173 amino acids compared with 84
amino acids in PTH. PTHrP, like PTH, can mediate bone
resorption of calcium and renal tubular absorption of
calcium, but unlike PTH, serum calcium levels do not regu-
late its secretion. Recently, an aberrant extracellular calcium-
sensing receptor (CaR) has been associated with a
counterproductive increased release of PTHrP by tumor
cells, as well as potentially stimulating cell growth and
inhibiting apoptosis.
PTH and PTHrP are distinguishable by radioassay, and
for this reason, it is possible to distinguish humoral hypercal-
cemia of malignancy from coexisting primary hyperparathy-
roidism. Despite a high frequency of bony metastases,
prostate, small cell lung cancer, and colorectal carcinoma are
rarely associated with hypercalcemia.
In addition to PTHrP, a number of locally active
cytokines augment resorption of calcium from bone, includ-
ing interleukin 1 (IL-1), IL-3, IL-6, IL-8, and IL-11 and
tumor necrosis factors (TNF-α and TNF-β)—all of which
are components of what was formerly called osteoclast-
activating factor. Furthermore, transforming growth factor
(TGF-α), platelet-derived growth factor, and certain
hematopoietic colony-stimulating factors such as granulocyte-
macrophage colony-stimulating factor (GM-CSF) also can
augment bone resorption. In patients with myeloma,
increased bone resorption from cytokines is the primary
mechanism of hypercalcemia. Prostaglandin E
2
also can
increase bone resorption. Two locally acting cytokines also
decrease the amount of calcium from bone: interferon-γ
and transforming growth factor β (TGF-β). Both inhibit
osteoclasts and bone resorption, and TGF-β promotes
osteoblast activity.
Some Hodgkin’s and non-Hodgkin’s lymphomas can 1-
hydroxylate sufficient amount of vitamin D to its more
highly active form. This increases gut absorption of calcium
and, together with the calcium resorption from cytokines
acting locally in bone, may produce hypercalcemia.
Hypercalcemia is a prominent feature of adult T-cell lym-
phomas (45% of cases) and of lymphomas and leukemias
associated with HTLV-1 (90%).
Clinical Features
When hypercalcemia results from malignancy, the cancer is
rarely occult. Patients with severe hypercalcemia (serum cal-
cium >14 mg/dL) are usually symptomatic. These symptoms
are often related to the rapidity of onset of hypercalcemia.
The clinical features of hypercalcemia and, in particular,
its neuromuscular manifestations tend to be much more
prominent in the elderly. Other factors such as the patient’s
performance status, recent chemotherapy, sites of metastasis,
and the presence of hepatic or renal dysfunction may
increase the severity of symptoms. Since calcium is a critical
regulator of cellular function, patients with hypercalcemia
may have a wide range of symptoms affecting different organ
systems. Conversely, the most common symptoms of hyper-
calcemia may be nonspecific and are similar to those seen in
patients with chronic or terminal illnesses, such as nausea,
anorexia, weakness, fatigue, lethargy, and confusion. In late
CHAPTER 20
458
stages, patients may be stuporous or comatose, and their
symptoms may mimic a neurologic emergency.
A. Neurologic—The major neurologic manifestations
include weakness, altered mental status, and altered deep
tendon reflexes. Initial manifestations may include subtle
personality changes, impaired concentration, apathy, mild
confusion and irritability, lethargy, hallucinations, and psy-
chosis, with progression to stupor and coma. Focal neuro-
logic signs are usually absent.
B. Gastrointestinal—Because of the depressive action of
hypercalcemia on autonomic nervous tissue, nonspecific
symptoms such as anorexia, nausea, and vomiting may
occur. These often progress to include abdominal pain, con-
stipation, frank obstipation, increased gastric acid secretion,
and acute pancreatitis.
C. Renal—Hypercalcemia causes a reversible tubular defect
in the kidney that limits urinary concentrating ability and
promotes dehydration or hypovolemia. If able, patients will
admit to polyuria, nocturia, and polydipsia. Metabolic alka-
losis is common, and acidosis occurs only when azotemia
supervenes. This contrasts with the effects of PTH, in which
a mild hyperchloremic acidosis is seen. Hypercalcemia also
can lead to precipitation of calcium phosphate crystals in the
Figure 20–1. Mechanisms of hypercalcemia of malignancy. Osteoclast activity can be stimulated by hormones,
cytokines, and other substances from certain primary tumors distant from bone or by tumor in the bone marrow. In
other patients, local production of cytokines known as osteoclast-activating factors are the primary mediators of
increased calcium mobilization. Both peripheral blood and marrow lymphocytes produce cytokines that affect osteo-
clasts. 1,25(OH)
2
vitamin D increases calcium absorption from the small intestine. Other local cytokines have an
inhibitory effect on osteoclast activity. [1,25(OH)
2
D = vitamin D; PTHrP = parathyroid hormone–related polypeptide;
IL = interleukin; TGF-α and TGF-β = transforming growth factors α and β; TNF-α and TNF-β = tumor necrosis factors α
and β; PDGF = platelet-derived growth factor; GM-CSF = granulocyte-macrophage colony-stimulating factor.]
CRITICAL CARE OF THE ONCOLOGY PATIENT
459
kidneys and ureters and the formation of renal calculi. Such
complications, however, are not commonly associated with
hypercalcemia of malignancy, and when they occur, the pos-
sibility of coexisting primary hyperparathyroidism should be
considered.
D. Cardiovascular—Hypercalcemia may cause electrocar-
diographic disturbances such as prolongation of the PR and
QRS intervals and shortening of the QT interval. With severe
hypercalcemia (>16 mg/dL), the T wave widens, increasing
the QT interval. At higher serum calcium concentra-
tions, bradyarrhythmias and bundle branch block may
develop, followed by complete heart block and cardiac arrest
in systole.
E. Bone and Extraskeletal Tissues—Hypercalcemia can
result either from humorally mediated bone resorption or
from osteolytic metastasis. Pain, fractures, and skeletal defor-
mities can occur. Metastatic calcification occurs in long-
standing and very severe hypercalcemia. Extraskeletal
deposition of calcium has been observed with hypercalcemia
in several organs, including the heart, lungs, kidneys, skin,
joints, and conjunctivae.
F. Laboratory Findings—Serum calcium, phosphate, and
albumin levels should be determined in all patients. Ionized
calcium is responsible for clinical manifestations and is
almost half the total serum calcium in normal subjects (the
rest is protein-bound). Measured ionized calcium is the
most accurate predictor of clinical features. A clinical esti-
mate of the “effect” of ionized calcium is the corrected
serum calcium equal to the measured calcium + 0.8 ×
(4 – measured albumin). This calculation is especially
helpful when hypoalbuminemia coexists with hypercal-
cemia. Hypophosphatemia in the presence of hypercal-
cemia strongly suggests the presence of PTHrP or primary
hyperparathyroidism. Elevated alkaline phosphatase is usu-
ally not helpful because it is seen in both primary hyper-
parathyroidism and hypercalcemia of malignancy. Direct
measurement of PTH and PTHrP may be necessary in some
patients.
G. Radiographs—Nephrocalcinosis and nephrolithiasis may
be present in long-standing hypercalcemia and suggest
hyperparathyroidism.
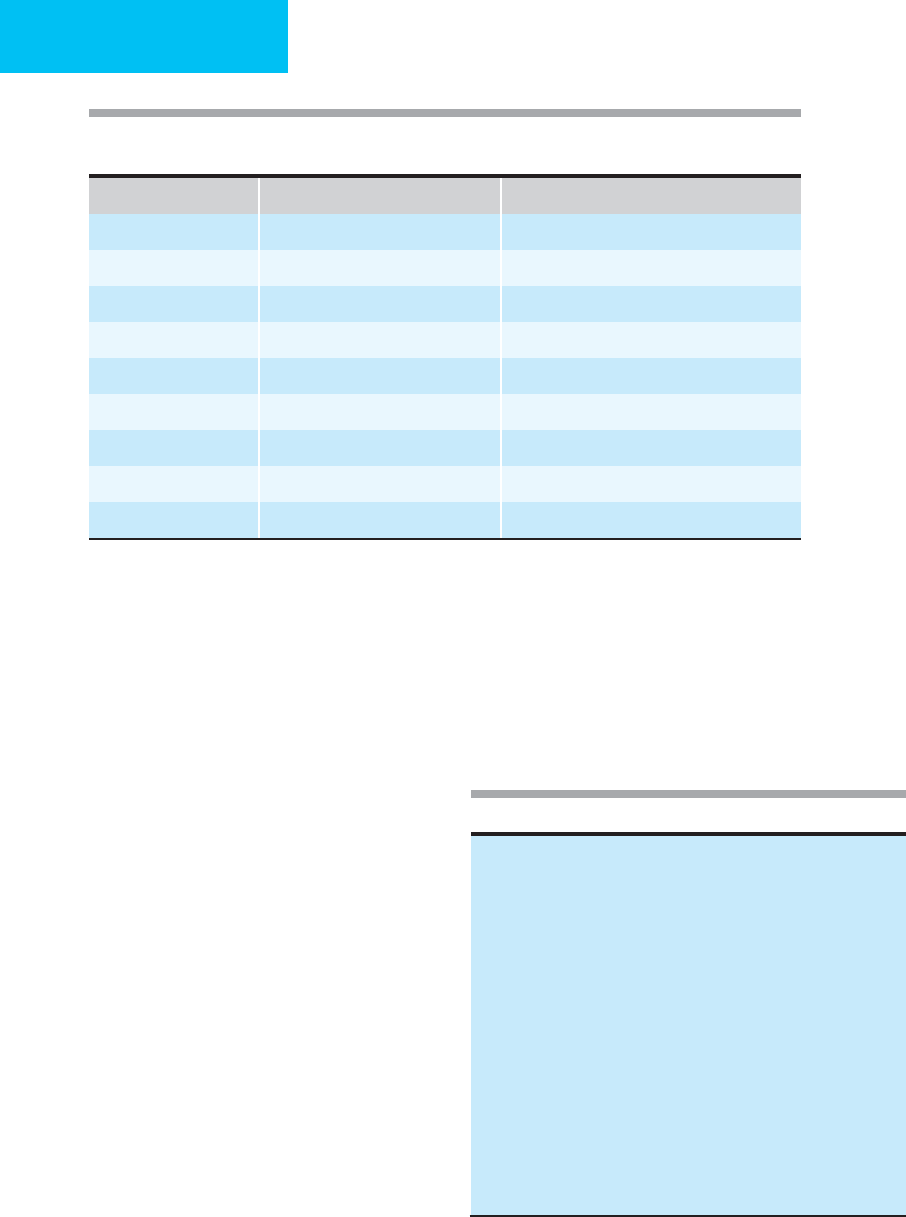
Differential Diagnosis
The differential diagnosis of hypercalcemia of malignancy
includes a wide variety of conditions (Table 20–2). Among
all patients, the two most common causes of hypercalcemia
are malignancy (35%) and primary hyperparathyroidism
(54%). Among hospitalized patients with hypercal-
cemia, 77% have malignancies, 4% have coexistent hyper-
parathyroidism, 2% have vitamin D intoxication, 2%
have tamoxifen-induced hypercalcemia, and 16% are due to
other causes. Table 20–3 lists features that may be used to
differentiate primary hyperparathyroidism from hypercal-
cemia of malignancy.
Treatment
There is no one regimen that should be applied to the acute
management of all cases of hypercalcemia. Moderate hyper-
calcemia with minimal symptoms may be managed with
administration of intravenous 0.9% NaCl. If the hypercal-
cemia is more severe and is symptomatic, furosemide and
calcitonin may be added. Since the effects of calcitonin are
not long-lasting, the use of bisphosphonates early in treat-
ment is indicated. In patients with lymphoma or myeloma
and hypercalcemia, corticosteroids are useful because of the
significant role of cytokines in the hypercalcemia.
Intravenous administration of sodium phosphate can lower
the serum calcium level rapidly, but its use is dangerous
because calcium phosphate complexes will deposit in blood
vessels, lungs, and kidneys with resulting severe organ dam-
age and even fatal hypotension. Therefore, intravenous phos-
phates are not recommended. Oral phosphates are of limited
value because diarrhea often develops with an intake of more
than 2 g/day. Azotemia and hyperphosphatemia are con-
traindications to phosphate therapy.
Table 20–2. Causes of hypercalcemia.
I. Primary hyperparathyroidism (54%)
II. Cancer (35%)
A. Caused by hormones (HHM) (80%)
1. Most common: Lung cancer (especially epidermoid) and renal
cell carcinoma.
2. Less common: Head and neck cancer, ovarian cancer,
hepatoma, pancreatic cancer, bladder cancer, endometrial
cancer, lymphomas, leukemia, multiple myeloma.
3. Isolated case reports: Esophageal cancer, colon cancer, rectal
cancer, cervical cancer, uterine leiomyosarcoma, vulvar cancer,
cancer of the penis, prostate cancer, adrenal cancer, melanoma,
hemangiopericytoma, branchial rest cancer, parotid cancer,
breast cancer, mammary dysplasia.
B. Caused by metastatic destruction of bone (20%). Breast cancer
(most common), multiple myeloma, lymphoma, and leukemia.
III. Others (11%)
A. Nonparathyroid endocrine disorders: Thyrotoxicosis, pheochromo-
cytoma, adrenal insufficiency, vasoactive intestinal polypeptide
hormone-producing tumor.
B. Granulomatous diseases: 1,25-(OH)
2
vitamin D excess, sarcoidosis,
tuberculosis, histoplasmosis, coccidioidomycosis, leprosy.
C. Medications: Thiazide diuretics, lithium, estrogens, and antiestrogens.
D. Milk-alkali syndrome.
E. Vitamin A or vitamin D intoxication.
F. Familial hypocalciuric hypercalcemia.
G. Immobilization.
H. Parenteral nutrition.
HHM = humoral hyperglycemia of malignancy.
CHAPTER 20
460
Therapy for hypercalcemia in cancer patients centers on
four main mechanisms: (1) correction of volume depletion,
(2) inhibition of bone resorption of calcium, (3) enhance-
ment of renal calcium excretion, and (4) treatment of the
underlying malignancy. Table 20–4 summarizes the available
drugs and their dosages.
A. Fluid and Electrolytes—Volume and electrolyte reple-
tion are the first priorities. Normal saline (0.9% NaCl), usu-
ally containing potassium chloride (10–20 meq/L), is given at
a rate of 2–3 L/day. Loop diuretics such as furosemide (40–80 mg
intravenously) are used to induce calciuresis and preclude
volume overload once fluid deficits are corrected. Judicious
fluid administration or central venous pressure monitoring
may be appropriate in patients with poor urine output or
congestive heart failure. As a result of calcium-related renal
tubular impairment and the resulting polyuria, urine out-
put may not be a reliable measure of intravascular volume
repletion.
B. Calcitonin—Calcitonin is a useful adjunct in the initial
phase of therapy. It is nontoxic and acts within 4–24 hours.
Calcitonin promotes renal excretion of calcium, inhibits
bone resorption, and inhibits gut absorption of calcium. The
effects of calcitonin, however, are minor and of short dura-
tion. Calcitonin is usually administered over 24 hours as an
intravenous infusion in a dose of 3 units/kg or 100–400 units
subcutaneously every 8–12 hours.
C. Corticosteroids—Corticosteroids decrease intestinal cal-
cium absorption and inhibit bone resorption and in that way
act as vitamin D antagonists. They also inhibit the action of
some of the locally acting cytokines that mediate calcium
mobilization from bone. They are effective primarily in
hematologic malignancies and breast cancer, essentially to
control chronic hypercalcemia.
Primary Hyperparathroidism Hypercalcemia of Malignancy
Symptoms Mild or absent Symptomatic
Serum calcium Mildly increased (<14 mg/dL) Significantly increased (>14 mg/dL)
Serum phosphorus Decreased Variable
Serum potassium Normal Usually decreased
Serum chloride Increased
∗
Low or normal
Serum bicarbonate Decreased (hyperchloremic acidosis) Normal or increased
Urinary calcium Increased Markedly increased
Urinary cAMP Increased Variable
1,25-(OH)
2
vitamin D Increased Usually decreased
∗
Serum chloride:phosphate ratio is increased.
Table 20–3. Features used to differentiate primary hyperparathyroidism from malignancy-
related hypercalcemia.
Table 20–4. Treatment of hypercalcemia of malignancy.
1. IV fluid replacement with 3–6 L of 0.9% NaCl with 40–80 mg of
potassium chloride per liter over 24 hours.
2. Furosemide, 40–160 mg IV over 24 hours.
3. Bisphosphonates:
Pamidronate, 60–90 mg in 1 L 0.9% NaCl over 4–24 hours.
Etidronate, 7.5 mg/kg in 300 mL 0.9% NaCl over 3 hours for
3–5 days.
4. Calcitonin: Extremely useful in patients with life-threatening
hypercalcemia. It has the most rapid action: 2–4 hours.
600 IU in 1 L 0.9% NaCl over 6 hours.
6–8 IU/kg IM every 6–8 hours for 2–3 days.
5. Corticosteroids: 200–300 mg of hydrocortisone per day or equivalent.
6. Gallium nitrate: 200 mg/m
2
in 1 L 5% dextrose over 24 hours for
5 days.
7. Plicamycin: 25 μg/kg for total dose of 1.5–2 mg IV administered
in brief infusion or over 12 hours. No benefit from prolonged
infusion.
8. Phosphates: Oral phosphates, 0.5–3 g/d diluted in water.
IV phosphates should not be given.
Formula to correct serum calcium for changes in serum albumin
concentration: Corrected serum calcium = measured total calcium
value (mg/dL) − serum albumin valve (g/dL) + 4.
CRITICAL CARE OF THE ONCOLOGY PATIENT
461
D. Bisphosphonates—Bisphosphonates are used routinely
because of their efficacy and low toxicity. They are potent
inhibitors of osteoclasts and bind to hydroxyapatite in bone
to inhibit dissolution. A single dose of pamidronate (60–90 mg
in 1 L of normal saline over 4–24 hours) by intravenous infu-
sion is safe and effective. Significant reductions in serum cal-
cium usually occur in 1–2 days and persist for several weeks.
Zoledronic acid is a more potent bisphosphonate that has
been associated with a higher proportion of correction of
hypercalcemia and more rapid normalization than
pamidronate. It is given intravenously as 4 mg over not less
than 15 minutes. The dose must be adjusted for renal insuffi-
ciency. Rare complications of bisphosphonates include acute
systemic inflammatory reaction, eye inflammation, renal fail-
ure, nephrotic syndrome, and hypocalcemia. Jaw osteonecro-
sis is seen primarily with long term use of bisphosphonates.
E. Dialysis—Hemodialysis is very effective in the treatment
of hypercalcemia but is usually reserved for management in
the setting of renal failure or life-threatening manifestations.
F. Other Therapies—Plicamycin and gallium nitrate decrease
bone resorption. Prostaglandin synthetase inhibitors and
other investigational drugs such as amifostine (WR-2721)
have been used. Amifostine inhibits PTH secretion and bone
resorption and facilitates urinary excretion of calcium.
All patients should be encouraged to avoid immobilization
and ambulate. In addition, liberal fluid intake and avoidance
of large amounts of foods rich in calcium are also suggested.
Halfdanarson TR, Hogan WJ, Moynihan TJ: Oncologic emergen-
cies: Diagnosis and treatment. Mayo Clin Proc 2006;81:835–48.
[PMID: 16770986]
Horwitz MJ, Stewart AF: Humoral hypercalcemia of malignancy.
In Favus MJ (ed), Primer on the Metabolic Bone Diseases and
Disorders of Mineral Metabolism, 5th ed. Philadelphia:
Lippincott Williams & Wilkins, 2003, pp. 246–50.
Spinazze S, Schrijvers D: Metabolic emergencies. Crit Rev Oncol
Hematol 2006;58:79–89. [PMID: 16337807]
Hypocalcemia in Malignant Disease
ESSENTIALS OF DIAGNOSIS
Tetany; paresthesias of the face, hands, and feet.
Positive Chvostek and Trousseau signs.
Muscle cramps, laryngeal spasm, headache, lethargy.
Low serum calcium (corrected) or low ionized calcium.
Osteoblastic metastases (breast or prostate cancer) or
tumor lysis syndrome with elevated serum phosphorus.
General Considerations
Hypocalcemia is a rare complication of cancer resulting from
osteoblastic metastasis secondary either to rapid bone healing
in patients with prostate or breast cancer receiving hormonal
therapy or to hyperphosphatemia in patients with tumor
lysis syndrome. The most common neoplasm associated with
hypocalcemia is prostate cancer, and 31% of patients with
prostate cancer and extensive osteoblastic bone metastasis
develop hypocalcemia. The skeleton in these patients has
been described as a “calcium sink.” Hypocalcemia secondary
to tumor lysis syndrome may be severe and appears to
result from a rise in the serum calcium × phosphorus prod-
uct, leading to precipitation of calcium in soft tissues,
including the kidneys, and the development of secondary
hyperparathyroidism.
Hypocalcemia also may occur secondarily in patients with
low circulating 1,25(OH)
2
vitamin D and calcifying chon-
drosarcoma. Magnesium deficiency results in hypocalcemia
in patients with prolonged nasogastric drainage, parenteral
hyperalimentation without magnesium supplementation,
cisplatin therapy, long-term diuretic therapy, chronic diar-
rhea, and chronic alcoholism and does not respond to cal-
cium replacement alone. Treatment of hypercalcemia with
plicamycin, bisphosphonates, or intravenous phosphate also
may cause hypocalcemia.
Clinical Features
The diagnosis of hypocalcemia is made with ease in patients
who develop tetany. Paresthesias of the face, hands, and feet
associated with muscle cramps, laryngeal spasm, diarrhea,
headache, lethargy, irritability, or seizures are the common
clinical manifestations. Chvostek’s and Trousseau’s signs are
usually present. The ECG usually shows a prolonged QT
interval. In long-standing cases, dry skin, papilledema, and
cataracts may develop.
Differential Diagnosis
The differential diagnosis of hypocalcemia should include
severe alkalosis secondary to vomiting, nasogastric suction,
or hyperventilation and severe muscle cramps resulting from
vincristine or procarbazine therapy.
Treatment
Treatment of acute severe hypocalcemia (serum calcium < 6
mg/dL) consists of intravenous administration of calcium
gluconate or calcium chloride, 1 g every 15–20 minutes until
tetany disappears, and magnesium sulfate, 1 g intravenously
or intramuscularly every 8–12 hours if the serum magne-
sium level is less than 1.5 mg/dL or is unknown. In patients
with moderate hypocalcemia (serum calcium >7 mg/dL),
calcium and magnesium may be replaced more slowly.
Carmeliet G et al: Disorders of calcium homeostasis. Best Pract Res
Clin Endocrinol Metab 2003;17:529–46. [PMID: 14687587]
Maalouf NM et al: Bisphosphonate-induced hypocalcemia: Report
of 3 cases and review of literature. Endocr Pract 2006;12:48–53.
[PMID: 16524863]
CHAPTER 20
462
Tumor Lysis Syndrome
ESSENTIALS OF DIAGNOSIS
Lethargy, tetany, muscle cramps, convulsions.
Administration of chemotherapy to patient with rapidly
proliferating malignancy.
Elevated serum uric acid, potassium, phosphate, and
urea nitrogen.
General Considerations
When given to a patient with a highly responsive (usually
rapidly growing) malignancy, chemotherapy may trigger
release of massive amounts of potassium, phosphate, uric
acid, and other breakdown products of dying tumor cells
into the bloodstream. Hypocalcemia owing to hyperphos-
phatemia may occur. This syndrome of tumor lysis occurs
most commonly in patients with rapidly proliferating and
chemotherapy-sensitive malignancies, such as acute
leukemia and Burkitt’s lymphoma and, on rare occasions,
following treatment of solid tumors and chronic lympho-
cytic leukemia (CLL). Tumor lysis syndrome has been
reported after chemotherapy, radiotherapy, monoclonal
antibody treatment, corticosteroids, and rarely sponta-
neously. Life-threatening complications may occur, including
renal failure from hyperuricemia and cardiac arrhythmias
induced by hyperkalemia or hypocalcemia.
Diagnosis
Diagnosis of tumor lysis syndrome is made most often from
laboratory studies. However, lethargy, tetany, muscle cramps,
and convulsions occurring in a patient with an appropriate
tumor who has just received chemotherapy should prompt
evaluation. Hyperkalemia, hyperphosphatemia, azotemia,
and oliguria usually are present.
Treatment
Early recognition of risk is the key to prevention and treat-
ment of this complication of cancer therapy. Despite appro-
priate treatment, renal insufficiency still may occur.
However, prognosis is good, and recovery to baseline renal
function is expected.
A. Hyperkalemia—Immediate treatment of hyperkalemia
consists of administration of 50–100 mL of 50% dextrose in
water and 10 units of regular insulin. Removal of potassium
can be achieved with oral sodium polystyrene sulfonate,
20–30 g every 6 hours. Hemodialysis may be necessary for
the management of refractory hyperkalemia.
B. Hyperphosphatemia—Hyperphosphatemia is typically
severe, with serum levels ranging from 6 up to as much as
35 mg/dL resulting from tumor cell lysis and subsequent
renal failure. Patients should be given 20% dextrose in water
and insulin until the serum phosphate level falls below 7
mg/dL. Aluminum hydroxide, 30–60 mL orally every 2–6
hours, is used to bind phosphate in the intestines. Oral fluids
are given at the rate of 2–4 L every 24 hours. Dialysis may be
necessary for patients with renal failure. Hyperphosphatemia
may be accompanied by hypocalcemia as well.
C. Hyperuricemia and Hyperuricosuria—Increased uri-
nary uric acid excretion may occur in untreated patients with
rapidly growing malignancies or during their treatment with
chemotherapy or radiation therapy. Uric acid nephropathy
secondary to the precipitation of uric acid crystals in the kid-
neys may result. Nephrolithiasis with urate stones or urate
interstitial nephritis also may occur. When massive doses of
allopurinol are used to prevent uric acid production, renal
oxypurinol stones may form occasionally.
Prevention of anticipated hyperuricemia is the corner-
stone of management. Allopurinol should be given to
patients with myeloproliferative disorders and hematologic
malignancies at least 12 hours before starting chemotherapy.
Rasburicase, a recombinant urate oxidase, does not cause
xanthine and hypoxanthine to accumulate but rather con-
verts urate to allantoin, a much more soluble product.
Rasburicase is much more effective and rapid in lowering
plasma uric acid levels. However, rasburicase is highly
immunogenic, with development of antirasburicase anti-
bodies occurring in the majority of patients exposed. This
limits the use of this agent to those with severe and poorly
responsive hyperuricemia.
D. Hydration—Vigorous hydration and alkalinization of the
urine decrease the risks of urinary tract precipitation of uric
acid and may decrease hyperkalemia. Urine flow should be
maintained at a rate of more than 100 mL/h, and urine pH
should be between 7.0 and 7.5. Sodium bicarbonate or aceta-
zolamide is given to alkalinize the urine. The ideal choice of
intravenous fluid is not clear, but usually dextrose 5% in
0.45% NaCl is given with 50–100 meq of NaHCO
3
added per
liter starting 24–48 hours before treatment, if possible. A rare
complication of urinary alkalinization is precipitation of
calcium phosphate stones.
Coiffier B, Riouffol C: Management of tumor lysis syndrome in
adults. Exp Rev Anticancer Ther 2007;7:233–9. [PMID:
17288532]
Del Toro G, Morris E, Cairo MS: Tumor lysis syndrome:
Pathophysiology, definition, and alternative treatment
approaches. Clin Adv Hematol Oncol 2005;3:54–61. [PMID:
16166968]
Rampello E, Fricia T, Malaguarnera M: The management of tumor
lysis syndrome. Nat Clin Pract Oncol 2006;3:438–47. [PMID:
16894389]
Tiu RV et al: Tumor lysis syndrome. Semin Thromb Hemost
2007;33:397–407. [PMID: 17525897]
CRITICAL CARE OF THE ONCOLOGY PATIENT
463
Hyponatremia in Malignancy
ESSENTIALS OF DIAGNOSIS
Nausea, anorexia, lethargy, confusion, weakness, con-
vulsions, coma.
Low plasma sodium with persistent excretion of con-
centrated urine.
Normal renal function with low serum urea nitrogen,
absence of fluid retention, and absence of intravascular
volume contraction.
History of malignancy, most frequently associated with
small cell carcinoma of the lung.
General Considerations
Hyponatremia in malignant disease is most often associated
with the syndrome of inappropriate antidiuretic hormone
secretion (SIADH), resulting from secretion of ADH by the
tumor. SIADH causes an increase in total body water with
moderate expansion of plasma volume, hyponatremia,
plasma hypo-osmolality, and inability to excrete maximally
diluted urine. It may occur with any malignancy but is most
frequently associated with small cell carcinoma of the lung
and mesothelioma. Other causes of SIADH are the admin-
istration of thiazide diuretics, vincristine, cyclophos-
phamide, chlorpropamide, tolbutamide, carbamazepine,
intravenous opioids, and psychotropic drugs (eg, amitripty-
line and thioridazine) in the setting of treatment of the can-
cer patient.
Clinical Features
A. Symptoms and Signs—Lethargy, nausea, anorexia, and
generalized weakness are the most common symptoms. Such
symptoms, however, are nonspecific and may be caused by
the primary cancer rather than hyponatremia. Confusion,
convulsions, coma, and death may occur if hyponatremia is
severe or of rapid onset.
B. Laboratory Findings—Plasma sodium concentration is
less than 135 meq/L, and there is persistent excretion of
urinary sodium. Renal function tests are normal, and
edema and intravascular volume contraction do not occur.
Blood urea nitrogen (BUN) concentration is characteristi-
cally low.
Diagnostic criteria for SIADH include hyponatremia
with low serum urea nitrogen (<10 mg/dL), absence of
intravascular volume contraction, persistent urinary excre-
tion of sodium (>30 meq/L), absence of fluid retention such
as peripheral edema or ascites, normal renal function, and
plasma hypotonicity in the presence of urine that is not
maximally dilute (urine osmolarity >100–150 mOsm/L with
plasma osmolarity <260 mOsm/L).
Differential Diagnosis
The differential diagnosis of low plasma sodium consists of
a long list that includes edematous states (eg, heart failure,
nephrotic syndrome, and cirrhosis), myxedema, salt-wasting
states (eg, mineralocorticoid deficiency, glucocorticoid
deficiency, and chronic renal failure), GI electrolyte losses
with hypotonic fluid replacement, compulsive water drink-
ing, and hypothalamic disorders. Pseudohyponatremia
secondary to hyperglycemia, mannitol administration,
and paraproteinemia should be excluded.
Treatment
Treatment of hyponatremia is discussed in Chapter 2. The
management of severe hyponatremia (plasma sodium < 110
meq/L) should be aggressive in a patient who is comatose or
convulsing, with the goal of raising plasma sodium above
120 meq/L but no higher than 130 meq/L. In other patients,
a maximum increase in plasma sodium of 8 meq/L in 24 hours
should be the target because of the complication of osmotic
demyelination syndrome.
Patients with plasma sodium levels of 125 meq/L or less
should be restricted to 500–700 mL of fluid a day. Patients
with higher plasma sodium concentrations are restricted to
1000 mL/day. Severe hyponatremia or symptomatic hypona-
tremia of any severity may require other treatment.
Administration of 0.9% NaCl will not correct hyponatremia
in patients with SIADH who have a urine osmolality of more
than 308 mOsm/L. In these patients, hypertonic saline (3%
NaCl, 1000 mL over 6–8 hours) and furosemide (40–80 mg
every 6–8 hours as needed) may be necessary. Central venous
pressure monitoring can reduce the risk of the precipitous
development of pulmonary edema. Plasma sodium and potas-
sium concentrations should be monitored hourly. Furosemide
and hypertonic saline are discontinued when plasma sodium
exceeds 110 meq/L and fluid restriction is started.
Direct antagonism of inappropriately secreted arginine
vasopressin should facilitate water elimination. Conivaptan,
a new vasopressin antagonist approved for euvolemic
hyponatremia, is given with an intravenous loading dose of
20 mg, followed by 20 mg administered as a continuous
intravenous infusion over 24 hours.
For chronic hyponatremia, demeclocycline, 150–300 mg
orally four times daily, may be given to patients who cannot
tolerate chronic fluid restriction or do not improve with fluid
restriction. Demeclocycline induces nephrotoxic diabetes
insipidus and may cause azotemia.
Adler SM, Verbalis JG: Disorders of body water homeostasis in
critical illness. Endocrinol Metab Clin North Am
2006;35:873–94. [PMID: 17127152]
CHAPTER 20
464
Ellison DH, Berl T: Clinical practice: The syndrome of inappropri-
ate antidiuresis. N Engl J Med 2007;356:2064–72. [PMID:
17507705]
Oh MS: Management of hyponatremia and clinical use of vaso-
pressin antagonists. Am J Med Sci 2007;333:101–5. [PMID:
17301588]
Hypokalemia & Ectopic ACTH Secretion
A number of tumors secrete ACTH, stimulate adrenal pro-
duction of corticosteroids, and result in Cushing’s syndrome.
These tumors include small cell lung cancer; carcinoid
tumors of the bronchi, pancreas, thymus, and ovary; islet cell
tumors; and cancers of the ovary, thyroid, and prostate, as
well as pheochromocytoma, hematologic malignancies,
and sarcomas. Unfortunately, most malignant causes of
ectopic ACTH production are rapidly fatal. Patients typically
present with weakness, cachexia, and hypertension. Typical
features of nonmalignant chronic Cushing’s syndrome are
often absent.
The differential diagnosis of hypokalemia includes GI
losses associated with alkalosis, vomiting, prolonged nasogas-
tric suction, villous adenoma of the colon, Zollinger-Ellison
syndrome, and chronic laxative abuse. Hyperaldosteronism,
hypercortisolism, hypercalcemia, and licorice ingestion also
may cause hypokalemia.
The most effective treatment of hypokalemia is control of
the underlying tumor. Carcinoid, thyroid tumors, pheochro-
mocytoma, and islet cell tumors are treated surgically if they
are resectable. If the tumors are nonresectable, chemotherapy
may be used (eg, mitotane, metyrapone, ketoconazole, and
aminoglutethimide). Potassium replacement should be
accomplished as early as possible. Spironolactone, 100–400 mg
daily, is helpful.
Hypophosphatemia in Malignancy
Hypophosphatemia (serum phosphorus <3 mg/dL) is occa-
sionally associated with rapidly growing tumors (eg, acute
leukemia) and marked nutritional deprivation and cachexia.
Symptoms may include generalized weakness, respiratory
muscle weakness causing respiratory failure, decreased
myocardial function, platelet dysfunction, and leukocyte dys-
function. Hemolysis and rhabdomyolysis may occur with
serum phosphorus levels of less than 1 mg/dL. The manage-
ment of severe hypophosphatemia (serum phosphorus <1
mg/dL) consists of intravenous administration of a solution
of 30–40 mmol/L of neutral sodium phosphate or potassium
phosphate at the rate of 50–100 mL/h. Intravenous adminis-
tration of phosphates should be monitored very carefully.
Patients with mild hypophosphatemia (serum phosphorus
1–2 mg/dL) can be given inorganic phosphate supplements
orally unless severely symptomatic.
Hyperglycemia in Malignancy
Hyperglycemia not due to insulin deficiency is present in
many patients with cancer. It occurs in patients with
glucagonoma, somatostatinoma, pheochromocytoma, and
ACTH-secreting tumors. Nonketotic hyperglycemia with
hyperosmolar coma may occur as a complication of treat-
ment with cyclophosphamide, vincristine, or prednisone in
patients with mild diabetes mellitus and in patients who are
receiving hyperalimentation.
Hyperglycemia caused by a tumor may respond to treat-
ment of the primary tumor with surgical resection, radiation
therapy, or chemotherapy. Hyperosmolar coma is treated
with replacement of fluid losses (intravenous NaCl solu-
tions) and insulin administration.
Hypoglycemia in Malignancy
Hypoglycemia may be secondary to inappropriate secretion
of insulin (insulinoma) or to nonsuppressible insulin-like
substances that are produced by some tumors. Large
retroperitoneal fibrosarcomas, mesotheliomas, and renal,
adrenal, and primary hepatocellular carcinomas are the most
common tumors associated with hypoglycemia. Patients
with extensive hepatic metastases may develop severe hypo-
glycemia secondary to depletion of glycogen and impaired
gluconeogenesis. Other causes of hypoglycemia include
administration of drugs such as insulin, oral hypoglycemic
agents, alcohol, and salicylates. Starvation, chronic liver dis-
ease, hypoadrenalism, hypopituitarism, and myxedema also
may cause hypoglycemia. Pseudohypoglycemia may occur in
patients with marked granulocytosis, especially in the setting
of myeloproliferative disorders.
Tumor-associated hypoglycemia produces changes that
are characteristic of hypoglycemia in the fasting state, such as
fatigue, convulsions, or coma. On the other hand, tremors,
sweating, tachycardia, and hunger are symptoms more char-
acteristic of reactive hypoglycemia in the postprandial state.
Intravenous glucose is the treatment of choice and should
be given to all patients with blood glucose levels below 40
mg/dL and symptomatic patients with glucose levels below
60 mg/dL. Continuous infusion of 10–20% dextrose in
water should be given at a rate to maintain a blood glu-
cose level above 60 mg/dL. If blood glucose levels cannot
be increased to a safe level, prednisone, diazoxide, or
glucagon may be considered.
Lactic Acidosis
Lactic acidosis is seen in the ICU most often because of
severe hypoperfusion from septic or cardiogenic shock.
Rarely, patients with leukemia or lymphoma without obvi-
ous shock appear to have tumor overproduction of lactic
acid, possibly related to increased anaerobic metabolism
from lack of perfusion to tumor. There may be associated
CRITICAL CARE OF THE ONCOLOGY PATIENT
465
hypoglycemia. Treatment of the underlying tumor may help,
but lactic acidosis in cancer patients has a poor prognosis.
Spinazze S, Schrijvers D: Metabolic emergencies. Crit Rev Oncol
Hematol 2006;58:79–89. [PMID: 16337807]
SUPERIOR VENA CAVA SYNDROME
ESSENTIALS OF DIAGNOSIS
Distention of neck and anterior chest wall veins.
Edema of the face; cyanosis and edema of upper
extremities.
Clinical evidence of intrathoracic malignancy.
General Considerations
There are no clinical or experimental data to support the
concept that superior vena cava obstruction is an oncologic
emergency, except perhaps on very rare occasions when the
patient presents with symptoms caused by tracheal obstruc-
tion or severe cerebral edema.
Superior vena cava syndrome was first described in 1751.
Malignant tumors are the most common cause (60%), but
recently, benign causes have increased in proportion to the
number of intravascular devices placed in the large systemic
veins in the thorax. Bronchogenic carcinoma is the leading
cause of superior vena cava syndrome and is responsible for
nearly 80% of all malignant causes. Approximately 5% of all
patients with bronchogenic carcinoma develop superior vena
cava syndrome during their lifetime, but the frequency of
this syndrome in small cell cancer is much higher. Malignant
lymphomas are responsible for approximately 15% of malig-
nant cases. Other causes (<5%) include metastatic disease to
the mediastinal lymph nodes (from primary breast and tes-
ticular cancer and, rarely, sarcomas). Benign causes are now
most commonly from complications of intravascular devices
(eg, catheters and pacemakers), with mediastinal fibrosis sec-
ondary to histoplasmosis, tuberculosis, pyogenic infection,
and radiation therapy to the mediastinum much less com-
mon. Very rarely, superior vena cava syndrome may be
caused by benign mediastinal tumors such as dermoids, ter-
atomas, thymomas, retrosternal goiters, sarcoidosis, and
aneurysms of the ascending thoracic aorta.
Malignant obstruction of the superior vena cava may be
caused by the tumor compressing its thin wall or invading it.
Thrombosis with clot formation is usually present. Collateral
circulation develops gradually. The collateral circulation
involves the internal mammary, intercostal, azygos, hemiazy-
gos, superior epigastric, and inferior epigastric veins. It
should be noted that in rapidly growing tumors, engorge-
ment of the venous collateral circulation may be absent.
Incompetence of the valves of internal jugular veins may
result only rarely in severe cerebral edema. Obstruction of
the trachea by mediastinal tumors is a serious associated
complication.
Clinical Features
The most common physical findings in superior vena cava
syndrome are neck and anterior chest wall vein distention
(60%), tachypnea (50%), edema of the face (50%), and
cyanosis and edema of the upper extremities (15%). The
diagnosis of superior vena cava syndrome is made on clinical
grounds in almost all patients. Superior vena cavography
may be used to verify the diagnosis and localize the site of
obstruction. Chest radiographs, CT scans, and MRI demon-
strate, evaluate, and define the extent of the mediastinal
lesion. Chest radiographs readily demonstrate a mass in
more than 90% of patients. MRI has no specific advantage
over CT scan in this disorder.
Although the symptoms of superior vena cava syndrome
are quite distressing to the patient, attempts to obtain a defi-
nite histopathologic diagnosis should be pursued vigorously
at the earliest opportunity. More than 60% of these patients
have small cell lung cancer or lymphomas that are appropri-
ately treated with chemotherapy, and early treatment with
radiation therapy or corticosteroids before making a definite
histopathologic diagnosis may make subsequent diagnosis
difficult or impossible. The diagnosis may be established by
sputum cytology, bone marrow biopsy, bronchoscopy, lymph
node biopsy, mediastinotomy, and anterior thoracotomy.
Mediastinoscopy with biopsy is not recommended owing to
the high incidence of severe hemorrhage, increasing neck
edema, and failure of wound healing. Adequate tissue biopsy
and a touch-preparation for pathologic examination should
be done when the diagnosis of lymphoma is suspected.
Ample data support the safety of invasive diagnostic proce-
dures in patients with superior vena cava syndrome except
those with tracheal obstruction or laryngeal edema.
Treatment
Supportive therapy should be instituted as soon as the
patient is admitted to the hospital. Upper airway obstruction
from tracheal compression with resulting hypoxia must be
addressed promptly. Corticosteroids may reduce associated
brain and possibly tracheal edema and lessen secondary
inflammatory reaction. Endotracheal intubation should be
avoided if possible in patients with tracheal obstruction to
prevent further edema. Frequently, the tracheal obstruction
is present in the more distal part of the trachea and cannot
be bypassed with endotracheal intubation. Tracheostomy is
rarely indicated for the same reasons. Placement of a self-
expanding metal endoprosthesis stent provides rapid relief
and is successful in over 90% of patients.
Chemotherapy is the treatment of choice for patients
with small cell lung cancer, lymphomas, and germ cell
tumors—more than 60% of patients with superior vena cava

CHAPTER 20
466
syndrome. Radiation therapy is the only treatment available
for other cancers. Spiral saphenous vein bypass grafting also
may be useful in selected patients. Anticoagulants and
antifibrinolytic agents are of no value and may be harmful.
Diuretics are of little help.
Overall, it has been observed that improvement in symp-
toms occurs in 50–70% of patients over a period of 1–2
weeks of treatment rather than within the first few days. It is
suggested that such improvement may be due to the develop-
ment of collateral circulation rather than to relief of the vena
caval obstruction. Studies have shown that in patients with
complete clinical symptomatic relief, the superior vena cava
lumen remained completely obstructed in 46% on venogra-
phy and in 76% at autopsy. Individual mortality is related to
the underlying malignancy rather than to the presence of
superior vena caval obstruction.
Rice TW, Rodriguez RM, Light RW: The superior vena cava syn-
drome: Clinical characteristics and evolving etiology. Medicine
(Baltimore) 2006;85:37–42. [PMID: 16523051]
