Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


PSYCHIATRIC PROBLEMS
437
either. The physician always should ask a depressed patient
about any suicidal ideation. As a practical matter, very few
ICU patients have the means to commit suicide in the unit,
but knowing the patient’s feelings about suicide may help the
physician to gauge the level of depression.
In addition to these cognitive factors, assessing the
patient’s self-esteem often serves as a clue to depression. The
patient who is grieving normally usually feels sad in reaction
to losses sustained or anticipated. The grieving individual
may appear sad but still maintain a proper sense of self-
esteem: “I’m okay, really—I’m still a good person despite my
medical problem.” The depressed individual, on the other
hand, feels worthless and useless: “I’m washed up—a burden
to my family.”
Another way of identifying the depressed individual
engages the physician in using his or her own feelings as an
assessment tool. Depressed patients often generate a feeling
of depression in their physicians; they also may produce a
sense of aversion so that the physician is eager to get away
from the bedside. An appropriately grieving patient, on the
other hand, usually generates a sense of sympathy and sad-
ness in the physician. Thus the physician who is sensitive to
his or her own responses to a patient may be able to confirm
a diagnosis of depression quite readily.
Differential Diagnosis
The key differential diagnosis in a patient who is being con-
sidered for a diagnosis of depression is appropriate grief or
organic mood disturbances. A number of conditions may
produce depressive symptoms. It is completely normal for an
individual to experience sadness and some emotional with-
drawal in response to a loss. Disease often produces a sense
of loss for many individuals, and it may be difficult for the
physician to differentiate appropriate grieving from a clinical
depression. One should consider the degree of dysfunction as
an indicator of depression. Thus, when a patient’s emotional
state is seriously interfering with medical recovery or compli-
ance with medical care, some form of treatment should be
offered. Depression becomes a likely diagnosis when the
patient makes a decision to terminate treatment for a disease
whose prognosis is favorable.
Certain medical conditions frequently produce depressive
symptoms. Examples are Cushing’s disease, hypothyroidism,
and pancreatic carcinoma. Virtually all the organic causes
described in the section on delirium also can produce
depressive states. In fact, a smoldering delirium may be mis-
taken for depression unless cognitive function is assessed.
Some hypoxic individuals, for example, will appear lethargic
and depressed. Medications such as β-blockers, corticos-
teroids, digoxin, cimetidine, levodopa, diazepam, and antihy-
pertensives may produce a depressive picture. Some
dopamine antagonists such as prochlorperazine or metoclo-
pramide produce psychomotor retardation or akathisia that
may mimic depression. A recent study indicated that the
presence of depression at baseline in patients with acute
coronary syndromes predicted failure to return to work and
not feeling better at 1 year. This study provided support for
the assessment of depression in identifying individuals at risk
for poorer outcomes.
Treatment
A key point in the treatment of depression is for the physi-
cian to recognize that depression is a painful and serious
condition that should not be considered “normal.” Just
because a knifing victim might be expected to exsanguinate
and experience a fall in blood pressure, medical treatment is
not withheld; similarly, the identification of depression war-
rants appropriate interventions. In serious cases of depres-
sion, there may be a substantial risk of failing to provide
treatment. A depressed patient is poorly compliant and
poorly motivated to participate in recovery—or may fail to
take adequate nutrition and participate in other aspects of
recovery such as being weaned from a ventilator.
The initial treatment of depression in the ICU should
emphasize psychosocial measures. To the extent possible, the
patient should be permitted to feel some control over what is
happening. Nurses should offer the patient a choice when-
ever possible. For example, the patient can be asked whether
or not pain medication is needed, whether it is time to be
moved, etc. Asking the patient to help plan the day’s bath and
hygiene schedule is very helpful. Encouraging the family to
visit as much as possible also may help to counter depression.
The physician can help to reduce depression by providing
realistic encouragement and support.
If these measures fail to reduce the depression, psychiatric
consultation is indicated followed by pharmacologic treat-
ment. The consultant will inquire about the patient’s psychi-
atric history, particularly to see if some specific antidepressant
medication has been successful in the past. If so, that drug
should be used. If the patient has not had a prior trial of anti-
depressant, a psychostimulant such as dextroamphetamine or
methylphenidate should be considered unless there is a med-
ical contraindication such as tachyarrhythmia. With the usual
starting dextroamphetamine dosage of 2.5 mg at 7 a.m. and
1 p.m., there is little risk of side effects. In an occasional
patient, there may be some increase in blood pressure or
pulse, but these are usually minimal and do not require stop-
ping the trial. If the patient fails to respond to the preceding
dosage, on the next day one can double the dosage to 5 mg
given twice. The maximum dosage is 15 mg twice daily, but
this level is rarely necessary. The medication is given early in
the day so as not to interfere with sleep. Many people have the
misconception that dextroamphetamine may worsen appetite
because it has been used in the past for dieting; in depressed
patients, however, it generally improves appetite.
Dextroamphetamine has the advantage of being essen-
tially free of side effects in most patients; some may have
slight tremor or anxiety. A rare patient may develop persecu-
tory feelings with this drug, but typically only at much higher
doses. The tremendous advantage of dextroamphetamine is
CHAPTER 18
438
the rapidity of response when it is successful. The physician
often can observe a beneficial effect 1–2 hours after the first or
second dose. Many patients report improved mood, energy,
appetite, and will to live. The response rate varies in different
studies from 48 to 80% improvement in depressive symptoms.
A number of other agents are effective and well tolerated
for the treatment of depression. An example is fluoxetine,
which was the first serotonin reuptake inhibitor released in
the United States. Although fluoxetine has essentially no
anticholinergic or blood pressure effects, it elevates many
other drug plasma levels by displacing them from their
plasma protein binding sites. This makes fluoxetine an unde-
sirable medication for most ICU patients. Other newer
agents have been developed that appear well suited for use in
ICU patients. Citalopram, sertraline, and venlafaxine are
effective antidepressants that share fluoxetine’s lack of blood
pressure and anticholinergic effects but are associated with
fewer drug interactions. Bupropion has little blood pressure
or anticholinergic effect, but in its immediate-release form it
has been associated with a higher incidence of seizures than
other antidepressants. All these agents have the limitations of
being available only in oral formulations and taking 1–4
weeks to have an effect.
Tricyclic antidepressants can be considered for ICU
patients, but like the newer agents mentioned briefly earlier,
they take 1–4 weeks to show an effect. Their anticholinergic
and quinidine-like side effects also can cause problems.
Tricyclic antidepressants also have the disadvantage of pro-
ducing marked α-adrenergic blockade, which can have trou-
blesome effects on blood pressure. If treatment with a
tricyclic is elected, nortriptyline is the best choice because it
has the least effect on postural hypotension and only modest
anticholinergic effects. It also has a clear therapeutic window
of maximum effectiveness of 50–150 ng/mL.
Current Controversies and Unresolved Issues
Depression may be hard to differentiate at times from normal
grief and sadness, so it would be useful to have a biologic
marker for the condition. Several years ago there was excite-
ment about using the dexamethasone suppression test as a
marker for major depression. Although this was of important
research significance, it has not been useful clinically because
50% of patients will suppress but still have the disorder.
Therefore, the test is of very little significance in trying to
decide on a diagnosis. It will be important for further research
in depression to develop biologic markers the clinician can use.
Another important area for further research involves the
identification of subtypes of depression so that specific phar-
macotherapy can be tailored appropriately. There have been
attempts to differentiate depression by global measures of
neurotransmitter levels. Cerebrospinal fluid and urinary lev-
els of methoxyhydroxyphenylglycol (MHPG) and serotonin
have been used to predict response to serotonergic and nora-
drenergic antidepressants. These efforts have not yet pro-
duced clinically useful applications.
Anxiety & Fear
ESSENTIALS OF DIAGNOSIS
Overt terror and panic.
Hypervigilance.
Fear of being alone.
Autonomic arousal.
General Considerations
Anxiety is the unpleasant feeling associated with an unknown
internal stimulus and is out of proportion to the threat from
the environment. Fear, on the other hand, is the same feeling
state but derived from a known external stimulus and propor-
tionate to the threat. Obviously, in the ICU these two feelings
are hard to distinguish, and they will be discussed here under
the term fear, which refers to both entities.
Fear is often prominent when the patient first enters the
ICU because of awareness of a substantial threat to his or her
continued existence resulting from the medical or surgical
problem that necessitated the admission. The ICU patient
may be reacting not only to the fear of death but to other
unspoken fears as well. The patient may be anxious about
how the family is responding to the illness and may have con-
cerns about ability to return to work or may harbor unreal-
istic ideas about the nature of the problem and the treatment
required. For example, some patients jump to the conclusion
that they will need open-heart surgery for any type of cardiac
problem. The patient also may associate the illness with a
loved one who had a similar problem. For example, one 59-
year-old man admitted to the coronary care unit feared he
would not survive his heart attack because his father had
died of one at the same age. Asking the patient about whom
he or she knows who had the same medical problem or treat-
ment may reveal a significant factor contributing to the
patient’s fear. A recent study indicated that the risk of devel-
oping posttraumatic stress disorder was linked with anxiety
during the time in the ICU. The study further found that
perceived social support was negatively correlated with
symptoms of posttraumatic stress disorder.
Fear and anxiety may produce significant physiologic
changes. Catecholamine and corticosteroid levels may fluctu-
ate along with anxiety levels. It has been demonstrated that
the perception of physical or emotional stress results in the
activation of several brain regions—serotonergic, cate-
cholaminergic, and perhaps cholinergic nuclei. These path-
ways are apparently then integrated by unknown mechanisms
into the hypothalamus. The end result of this complex
response is the secretion of glucocorticoids. Evidence also has
accumulated for a variety of links between the serotonergic
region and the hypothalamic-pituitary axis that may underlie
the connection between stress and mood. A recent study
found that the risk of cardiocirculatory complications was
PSYCHIATRIC PROBLEMS
439
decreased by a factor of 2 in periods of unrestrictive visiting
policies in an ICU. This also was correlated with a greater
reduction in anxiety score and less of an increase in thyroid-
stimulating hormone during the course of admission. A
restrictive visiting policy was associated with a nonsignifi-
cant increase in mortality rate. The authors concluded the
unrestrictive visiting policy might decrease cardiovascular
complications through lessened anxiety and a more desirable
hormonal profile.
Clinical Features
The physician can observe fear in many guises in the ICU.
Patients with a past history of generalized anxiety, panic, or
“nervous” disorders should be expected to have increased
fearfulness in the ICU. Some patients will demonstrate their
terror and panic overtly. Others may appear hypervigilant,
constantly scanning the environment. Others will talk exces-
sively or seek the presence of the nurse so as not to be left
alone. Some patients will fight going to sleep because of fear
of dying while asleep. Blood pressure and heart rate may be
elevated as the autonomic accompaniments of fear ensue.
Some patients may exhibit their fear by major denial of
illness. These individuals may attempt to demonstrate their
good health by exercising in the coronary care unit. Others
will try to sign out of the hospital against medical advice.
Fear is perhaps recognized most easily in the patient being
weaned from the ventilator “before I’m ready.” These patients
often show stark terror as the ventilator settings are reduced.
In such cases, anxiety may grossly interfere with medical
treatment.
Furthermore, anxiety related to experiences in the ICU
does not dissipate at the door on departure from the unit.
Patients may continue to have nightmares and experience
episodes of hypervigilance and panic even after returning to
home care, thus suggesting the diagnosis of posttraumatic
stress disorder (PTSD). Research is still needed to help pre-
dict which individuals are at the greatest risk for develop-
ment of this syndrome. Some studies have linked its
development to adverse experiences in the ICU. One study
found that the presence of delusional memories of events in
the ICU—as opposed to factual memories—indicated an
increased risk for PTSD-related symptoms and panic follow-
ing discharge from the ICU.
Differential Diagnosis
Anxiety and fear can be confused with the agitation of delir-
ium. The delirious patient, however, will have significant cog-
nitive impairment that is usually not present in the anxious
patient. The physician should continuously assess the anxious
patient for organic factors that could contribute to anxiety.
Medications such as corticosteroids, theophylline, and lido-
caine can produce anxiety and fearfulness. Medical conditions
such as hypoxia, pulmonary emboli, pheochromocytoma,
Cushing’s disease, and early drug or alcohol withdrawal may
have anxiety as a major symptom (Table 18–3).
Treatment
The best treatment of anxiety is prevention. Psychologically
preparing a patient for surgery can have a beneficial effect.
These efforts, as well as those offered by the patient’s primary
physician, can be very effective in preventing anxiety. Similarly,
the physician can intervene postoperatively to minimize
patients’ anxiety. One study suggests that playing a brief tape-
recorded message from the surgeon—explaining that surgery
went well, giving an orientation to the ICU, and reassuring the
patient about early recovery—markedly reduces anxiety.
Nonetheless, for many patients, fear and anxiety will
develop in the ICU. The first step in treating the fearful
patient involves exploring precisely what the patient is most
fearful about. This information may be obtained directly
from the patient who is prepared properly and trusts the
physician. The physician can start by saying, “Most people
have some worries or fears in this situation. What are yours?”
This approach normalizes the presence of fears and makes it
easier to talk about them. Whatever the patient brings up as
a concern should be explored.
Pulmonary disorders
COPD
Pulmonary embolus
Asthma
Hypoxia
Drugs
Drug withdrawal
Drug intoxication (eg, amphetamines, cocaine)
Infections
Tuberculosis
Brucellosis
Cardiac disorders
Mitral valve prolapse
Paroxysmal atrial tachycardia
Subacute infective endocarditis
Angina
Endocrine and metabolic disorders
Insulinomas
Carcinoid tumors
Pheochromocytomas
Hypoglycemia
Thyroid disease
Hypocalcemia
Porphyria
Cushing’s disease
Neurologic disorders
Multiple sclerosis
Akathisia
Temporal lobe epilepsy
Table 18–3. Medical disorders commonly associated
with anxiety.

CHAPTER 18
440
Another valuable technique for helping a patient deal
with fear is reframing the patient’s view of the situation. For
example, one 45-year-old African-American wanted to sign
himself out of the coronary care unit, saying he refused to
believe that he had had a bad heart attack. The doctors
repeatedly tried to warn the patient of the risks of not accept-
ing hospital treatment. The patient responded by doing 10
one-handed push-ups. Finally, psychiatric consultation was
requested. The psychiatrist realized that frightening the
patient only escalated his fear and increased his need to deny
the fear by signing out against advice. The psychiatrist sug-
gested to the patient that it took a strong man to put up with
the bed rest and testing the cardiologists wanted. The con-
sultant suggested that the patient could prove his strength in
this way. In essence, the patient no longer had to equate stay-
ing in the unit as a loss of strength and self-esteem. With this
reframing of his medical care, the patient accepted the
remainder of his treatment without difficulty.
In some ICUs, the psychiatric consultant or liaison nurse
may teach relaxation with the aid of audiotapes. Some
patients may be receptive to learning self-hypnosis. These
techniques may help by restoring the patient’s sense of con-
trol over the environment. These techniques also may be
helpful in the patient being weaned from the ventilator.
If psychosocial interventions do not work or are not
available, medication can be used. Lorazepam is the antianx-
iety drug of choice. Its intermediate half-life (10–20 hours) is
long enough to prevent the withdrawal syndrome that can
occur with shorter-acting agents but not so long that the
drug tends to accumulate. Lorazepam is metabolized in a
one-step conjugation and so can be used in patients with
liver disease. For most patients with mild to moderate anxi-
ety, the dosage of lorazepam is 1–2 mg (depending on age
and weight) every 4–6 hours. For more severe anxiety, one
may double these dosages. Antidepressants such as sertraline
and citalopram also can be useful against anxiety. As with
their use in depression, however, they can take up to 4 weeks
to have a significant effect and must be given orally. When
anxiety is extreme and interfering grossly with the patient’s
care, a shift to antipsychotic medications has been advocated.
Although haloperidol has been advocated for this purpose,
newer agents also should be considered. A recent report
described the use of risperidone for patients with irritability
and hostility. The authors noted that this agent caused fewer
side effects than haloperidol, imposed fewer risks than ben-
zodiazepines, and was effective with a more rapid onset than
antidepressants.
Current Controversies and Unresolved Issues
There is a continuing quest for the anxiolytic agent that gives
relief without clouding the sensorium or producing trouble-
some withdrawal states. For example, triazolam is a popular
sedative benzodiazepine in some regions because it has a
short half-life that makes it unlikely to produce a hangover.
The short half-life, however, has a major disadvantage in
that it may lead to withdrawal syndromes the next day, leav-
ing the patient anxious until the next dose is given. Until the
neurotransmitter systems involving various agents such as
γ-aminobutyric acid are further elucidated, the quest for the
ideal agent will have to continue.
Staff Issues
The ICU staff considered as a group has many psychological
features similar to those found in individual health
providers. Many doctors and nurses, for example, bring cer-
tain psychological motivations to their work. They may feel a
strong need to save and rescue their patients. They also may
demand perfection from themselves. In some sense, whether
it is consciously realized or not, the ICU staff may make the
same demand as a group. This may be manifested in attempts
to save the unsalvageable patient and reluctance to let any
patient die. On the other hand, many patients have unclear
prognoses, and these may be particularly challenging for the
staff. Research suggests that the most difficult patients for
staff to care for are those with multisystem failure and a poor
prognosis.
A useful equation for conceptualizing a staff’s self-esteem
is the following:
In this equation, how staff feel about themselves is equal to
what realistic achievement they can accomplish “divided by”
their expectations. The equation represents a shorthand way of
viewing how the relationship between expectations and
achievements influence self-esteem. In instances where the
expectation is one of omnipotence, unless the achievement is
perceived as a perfect performance, the staff will end up feel-
ing like a failure. In this equation, we should note that the real-
istic achievement is relatively fixed within a narrow range
accomplished by most competent staff. The variable that can
be adjusted most easily is the denominator—expectations. If
staff are successful in reducing this value, the staff can feel
much more satisfied with their accomplishments. This issue is
highlighted when staff have to deal with a dying patient. When
staff are able to shift their expectations away from an unrealis-
tic omnipotent fantasy of saving the patient, they can shift to a
more realistic one such as providing a comfortable, dignified
death. Such a goal is much more easily accomplished.
Identifying Staff Problems
Staff issues often can be identified in staff attitudes toward
patients. For example, following a period in which there had
been an unusually high number of deaths in an ICU, an 80-
year-old patient was admitted to the unit with pneumonia.
She required intubation and ventilation. Although her infec-
tion was controlled rapidly, she had difficulty being weaned
from the ventilator. Staff nurses began to voice concerns such
Self-esteem
realistic achievement
expectatio
=
nns
PSYCHIATRIC PROBLEMS
441
as, “Why are we putting such effort into an 80-year-old
woman? She won’t make it anyhow.” When those concerns
were raised in a staff meeting, other staff members pointed
out that the patient had been living independently until her
pneumonia developed and that her only current problem
was one of pulmonary mechanics that should clear with
time. This discussion helped the staff to perceive that their
view of the patient had been unfairly pessimistic, probably
related to the several recent deaths that had led to a sense of
inadequacy, helplessness, and group depression. They left the
meeting with a clearer understanding of what they could
accomplish with the patient. She eventually was weaned from
the ventilator and returned to her home.
Interventions
There are various approaches to helping the ICU staff deal
with the stress of working with critically ill patients. Units
emphasizing a culture of cooperation and communication
have a reduced length of stay, increased staff longevity, and a
higher perceived quality of care. These observations reinforce
earlier recommendations to schedule regular staff meetings,
including in the invitation a psychiatrist or social worker
familiar with the unit. Ideally, both physicians and nursing
staff should attend this meeting. Staff should raise any feel-
ings they have about patients or ward situations. These feel-
ings can be clarified, shared, and discussed with others.
Identification of exaggerated expectations or other problems
such as group depression can be investigated and resolved.
Junior staff can gain broader perspectives from more experi-
enced staff. These meetings also can facilitate communica-
tion and humor, which are important ways for a staff to cope.
They can help staff deal with the multisystem patient with a
poor prognosis. Staff can become more comfortable realizing
that they are doing the best job possible with this difficult
population and accepting death if it becomes clear that the
patient will have to die despite the best critical care that could
be offered. Recent studies have found that clinicians perceive
conflict in up to 78% of cases requiring decision making for
critically ill patients. The conflict was perceived to occur with
equal frequency between staff and family members and
within the staff. While the presence of conflict was not always
felt to be detrimental, it can be disruptive and lead to morale
problems. Thus meetings in which such issues can be identi-
fied and discussed will benefit the ICU team.
In addition to staff meetings, there are a host of practical
interventions that can help staff deal with the stress of work-
ing in an ICU. Nursing and physician staff can be encouraged
to take adequate time off for restorative recreation and fam-
ily life. Some institutions schedule fewer but longer shifts in
order to provide longer stretches of time off. House staff
might be given the afternoon off on the day following a night
on call—which is probably the single most important vari-
able in reducing house staff distress. Providing strong med-
ical and nursing directors is extremely helpful for staff
dealing with the ambiguities of complex illnesses. Having the
services of an ethicist and a chaplain available on a regular
basis can be an invaluable support strategy. Another measure
to prevent the development of burnout in ICU staff is creat-
ing a system in which staff rotate between the ICU and other
settings to remove staff from the constant stress of the ICU.
Current Controversies and Unresolved Issues
The difficulty of working in an ICU undoubtedly will persist.
As technological advances allow staff to sustain life in the
face of severe, previously untreatable conditions, the ethical
and philosophical tensions these situations give rise to are
likely to increase. Helping the staff to cope with these stres-
sors will remain an ongoing challenge.
REFERENCES
American Psychiatric Association: Diagnostic and Statistical Manual
of Mental Disorders, 4th ed., text revision. Arlington, VA:
American Psychiatric Association, 2000.
American Psychiatric Association: Practice Guideline for the
Treatment of Patients with Delirium. Arlington, VA: American
Psychiatric Association, 1999.
Barie PS, Bacchetta MD, Eachempati SR: The contemporary surgical
intensive care unit: Structure, staffing, and issues. Surg Clin North
Am 2000;80:791–804. [PMID: 10897261]
Breen CM et al: Conflict associated with decisions to limit life-
sustaining treatment in intensive care units. J Gen Intern Med
2001;16:283–89. [PMID: 11359545]
Carter GL, Dawson AH, Lopert R: Drug induced delirium: Incidence,
management and prevention. Drug Saf 1996;15:291–301. [PMID:
8905254]
Di Salvo TG, O’Gara PT: Torsade de pointes caused by high-dose
intravenous haloperidol in cardiac patients. Clin Cardiol
1995;18:285–90. [PMID: 7628136]
Coomber S et al: Stress in UK intensive care unit doctors. Br J
Anaesth 2002;89:873–81. [PMID: 12453932]
Coursin DB, Coursin DB, Maccioli GA: Dexmedetomidine. Curr
Opin Crit Care 2001;7:221–6. [PMID: 11571417]
Deja M et al: Social support during intensive care unit stay might
improve mental impairment and consequently health-related
quality of life in survivors of severe acute respiratory distress syn-
drome. Crit Care 2006;10:R147–58. [PMID: 17042955]
Eisendrath SJ, Dunkel J: Psychological issues in intensive care unit
staff. Heart Lung 1979;8:751–8.
Eisendrath SJ, Link N, Matthay M: Intensive care unit: How stressful
for physicians? Crit Care Med 1986;14:95–8. [PMID: 3943330]
Eisendrath SJ: Reframing techniques in the general hospital. Fam Sys
Med 1986;4:91–5.
Flacker JM, Lipsitz LA: Neural mechanisms of delirium: Current
hypotheses and evolving concepts. J Gerontol 1999;6:B239–46.
Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: A prac-
tical method for grading the cognitive state of patients for the cli-
nician. J Psychiatr Res 1975;12:189–98.
Fumagalli S et al: Reduced cardiocirculatory complications with
unrestrictive visiting policy in an intensive care unit: Results from
a pilot, randomized trial. Circulation 2006;113:946–52.
George J, Bleasdale S, Singleton SJ: Causes and prognosis of delirium
in elderly patients admitted to a district general hospital. Age
Ageing 1997;26:423–27.

CHAPTER 18
442
Han CS, Kim YK: A double-blind trial of risperidone and haloperi-
dol for the treatment of delirium. Psychosomatics 2004;45:
297–301. [PMID: 15232043]
Hart RP et al: Abbreviated cognitive test for delirium. J Psychosom
Res 1997;43:417–23. [PMID: 9330241]
Hassan E, Fontaine DK, Nearman HS: Therapeutic considerations in
the management of agitated or delirious critically ill patients.
Pharmacotherapy 1998;18:113–29. [PMID: 9469686]
Hwang SL et al: Stress-reducing effect of physician’s tape-recorded
support on cardiac surgical patients in the intensive care unit.
J Formos Med Assoc 1998;97:191–96. [PMID: 9549270]
Jones C et al: Memory, delusions, and the development of acute
posttraumatic stress disorder-related symptoms after intensive
care. Crit Care Med 2001;29:573–80. [PMID: 11373423]
Karlsson I: Drugs that induce delirium. Dement Geriatr Cogn
Disord 1999;10:412–15. [PMID: 10473949]
Kerasiotis B, Motta RW: Assessment of PTSD symptoms in emer-
gency room, intensive care unit, and general floor nurses. Int J
Emerg Ment Health 2004;6:121–33. [PMID: 15481474]
Kim KY et al: Treatment of delirium in older adults with quetiapine.
J Geriatr Psychiatry Neurol 2003;16:29–31. [PMID: 12641370]
Lerner DM et al: Low-dose risperidone for the irritable medically ill
patient. Psychosomatics 2000;41:69–71. [PMID: 10665272]
Lopez JF, Akil H, Watson SJ: Role of biological and psychological fac-
tors in early development and their impact on adult life: Neural
circuits mediating stress. Biol Psychiatry 1999;46:1461–71.
Masand PS, Tesar GE: Use of stimulants in the medically ill. Psychiatr
Clin North Am 1996;19:515–47. [PMID: 8856815]
McGee HM et al: Impact of briefly-assessed depression on secondary
prevention outcomes after acute coronary syndrome: A one-year
longitudinal survey. BMC Health Serv Res 2006;6:9–16. [PMID:
16476160]
McGuire BE et al: Intensive care unit syndrome: A dangerous mis-
nomer. Arch Intern Med 2000;160:906–9. [PMID: 10761954]
Mittal D et al: Risperidone in the treatment of delirium: Results
from a prospective open-label trial. J Clin Psychiatry 2004;65:
662–7.
Pirraglia PA et al: Depressive symptomatology in coronary artery
bypass graft surgery patients. Int J Geriatr Psychiatry
1999;14:668–80. [PMID: 10489658]
Raggio B, Malacarne P: Burnout in intensive care unit. Minerva
Anestesiol 2007;73:195–200. [PMID: 17468736]
Sadaki Y et al: A prospective, open-label, flexible-dose study of que-
tiapine in the treatment of delirium. J Clin Psychiatry
2003;64:1316–21. [PMID: 14658945]
Skrobik YK et al: Olanzapine vs haloperidol: treating delirium in a
critical care setting. Intensive Care Med 2004;30:444–9. [PMID:
14685663]
Saravay SM, Lavin M: Psychiatric comorbidity and length of stay in
the general hospital: A critical review of outcome studies.
Psychosomatics 1994;35:233–52. [PMID: 8036253]
Schelling G et al: Health-related quality of life and posttraumatic
stress disorder in survivors of the acute respiratory distress syn-
drome. Crit Care Med 1998;26:651–59. [PMID: 9559601]
Siobal MS et al: Use of dexmedetomidine to facilitate extubation in
surgical intensive-care-unit patients who failed previous weaning
attempts following prolonged mechanical ventilation: A pilot
study. Respir Care 2006;51:492–6. [PMID: 16638158]
Tanimoto S et al: The psychological and physiological effects of
an intensive-care unit environment on healthy individuals.
Clin Perform Qual Health Care 1999;7:77–82. [PMID:
10747570]
Trzepacz P: Update on the neuropathogenesis of delirium. Dement
Geriatr Cogn Disord 1999;10:330–34. [PMID: 10473933]
van der Mast RC: Delirium: The underlying pathophysiological
mechanisms and the need for clinical research. J Psychosom Res
1996;41:109–13. [PMID: 8887824]
443
0019
Care of the Elderly Patient
Shawkat Dhanani, MD, MPH
Dean C. Norman, MD
The elderly are a highly heterogeneous group, and the physi-
cal and medical heterogeneity increases with age. Individuals
over 65 years of age—with or without chronic diseases—vary
widely in their physical, behavioral, and cognitive functions.
Any clinician can relate the “Tale of Two Octogenarians” seen
in practice on the same day: the end-stage patient afflicted
with Alzheimer’s disease seen at the nursing home and the
vigorous retiree seen after his golf game for monitoring of his
historically well-controlled hypertension.
Physiologic rather than chronological age is a better pre-
dictor of the health status of the elderly. An abrupt decline in
physical function or any organ system is almost certainly due to
disease and not due to “normal aging.” Therefore, symptoms in
the geriatric population should not be attributed automatically
to old age, and it is important to look for potentially reversible
causes of symptoms. Moreover, treatable conditions should not
be undertreated for fear of side effects of medication.
Improvement or maintenance of functional status is the
major goal of medical care in the geriatric population.
Functional disability occurs faster and takes longer to correct
in the elderly, necessitating early preventive measures. Active
efforts should be made to maintain functional level even dur-
ing intensive care. Even small changes in function can make
large differences in the quality of life. For example, regaining
the ability to oppose the thumb to other fingers may enable a
geriatric patient to become independent in feeding.
Prevention of iatrogenic diseases is also important. For exam-
ple, close attention should be paid to prevent the develop-
ment of pressure ulcers. A pressure ulcer can develop in just
few hours, and the mortality rate of those who develop the
lesions in the first 2 weeks of intensive care has been reported
to be as high as 73%. Other iatrogenic problems in the ICU
include aspiration pneumonia, sepsis, GI bleeding, delirium,
drug toxicity and interactions, and renal insufficiency.
Multiple concurrent illnesses, cognitive and sensory
impairments, age-related changes in physiology and phar-
macodynamics, increased vulnerability to delirium, and
complications from immobility make management of acute
illness in the elderly a clinical challenge for all physicians and
other health care providers who care for patients in this age
group.
Physiologic Changes with Age
The Aging Heart
Heart disease is the leading cause of death in people over
75 years of age and the fourth most prevalent chronic disease
in the elderly. Nearly 30% of elderly people have some abnor-
mality affecting the heart. Moreover, occult cardiac disease can
cause marked functional impairments in otherwise apparently
healthy elderly people. Coronary atherosclerosis increases
exponentially with age and, in the elderly, can present as heart
failure, pulmonary edema, arrhythmias, or exercise intoler-
ance rather than as angina or obvious myocardial infarction.
In healthy subjects, the resting heart rate does not change
with age, but the maximum heart rate with exercise decreases
with age (Table 19–1). It can be calculated by the following
formula: 208 – (0.7 × age). Age-related changes in collagen
and elastin contribute to progressive stiffness and loss of
recoil of elastic tissues. In the systemic arteries, this process
contributes to an increase in systolic blood pressure. Systolic
pressure rises approximately 6–7 mm Hg per decade, but
diastolic pressure changes little with age and even may fall
starting in the sixth decade. In addition, the systolic pressure
may be underestimated by the cuff sphygmomanometer in
the elderly. Resistance to blood flow leads to increased left
ventricular wall tension and compensatory left ventricular
hypertrophy. The myocardium is also affected by changes in
collagen and elastin that cause stiffness of the left ventricle
that can result in diastolic dysfunction. The left ventricular
filling rate during early diastole declines markedly with age
(approximately a 50% reduction between age 20 and age 80).
Enhanced active filling in late diastole during atrial contrac-
tion compensates for decreased passive diastolic filling, and
this explains the vulnerability of older persons to congestive
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 19
444
heart failure when atrial fibrillation or flutter occurs.
Decreased filling also makes the elderly more vulnerable to
small decreases in venous filling with volume loss or when
given opioids, diuretics, or positive-pressure ventilation. On
the other hand, systolic function is relatively preserved in the
healthy elderly.
Despite these disturbances, cardiac output at rest remains
relatively constant across the life span. During low- and
medium-intensity exercise, increases in stroke volume com-
pensate for the lower heart rates observed in the elderly. This
increase in stroke volume with exercise is the result of an
increase in end-diastolic volume by as much as 30% (Frank-
Starling law). However, with high-intensity exercise, a decline
in cardiac output is observed owing largely to the age-related
decline in maximum heart rate. This hemodynamic profile is
strikingly similar to that observed in younger patients who
exercise in the presence of β-adrenergic blockade. Since
β-adrenergic modulation of pacemaker cells partly explains
the increased heart rate during exercise, this observation led
to the hypothesis—later confirmed—that diminished response
to β-adrenergic modulation is one of the most notable age-
related changes in the cardiovascular system. Chronotropic
and inotropic responses of the aging heart to norepinephrine,
isoproterenol, and dobutamine are diminished. Virtually all
studies show higher mean circulating blood norepinephrine
and epinephrine levels in the elderly than in younger persons.
Both arterial dilation and venous dilation in response to
β-adrenergic stimulation decrease with age. This deficiency
in arterial dilation in addition to any age-related structural
changes within the large vessels may contribute to increased
vascular impedance in advancing age.
The Aging Lung
Cross-sectional population studies consistently show a pro-
gressive age-related decline in pulmonary function. The
decrements in flow rates and lung volumes are not uniform
throughout life but tend to accelerate with age. Given the
large individual differences in the elderly, longitudinal stud-
ies would be preferable for observing the change in pul-
monary function, which is influenced not only by age but
also by environmental factors such as smoking, air pollution,
infections, and other comorbid conditions.
Age-related changes in collagen and elastin produce a
decrease in lung compliance, but this is not physiologically
significant. However, rigidity of the chest wall with aging has
measurably negative mechanical implications resulting in
significantly increased work of breathing. Starting around
age 35 years, there is a decrease in forced vital capacity (FVC)
averaging 14–30 mL per year and a decrease in forced expi-
ratory volume in 1 second (FEV
1
) averaging 23–32 mL per
year for nonsmoking men. Nonsmoking women show
slightly lesser rates of decline (FVC 15–24 mL per year and
FEV
1
19–26 mL per year). All expiratory flow rates decrease
with age and tend to fall faster in men, taller individuals, and
those with increased airway reactivity. The decrease in FVC is
associated with an elevation in functional residual capacity
(FRC) and residual volume (RV). Only minor changes occur
in total lung capacity.
Age-related changes in lung structure and chest wall
mechanics lead to premature closure of terminal airways. This
phenomenon occurs predominantly in the dependent parts of
the lungs that are the best perfused, accounting for increasing
ventilation-perfusion mismatching that results in a progressive
decrease in arterial oxygen tension (Pa
O
2
) and an increased
alveolar-arterial oxygen difference—P(
A
–a)
O
2
—with age. The
following equation predicts Pa
O
2
at sea level in the adult:
Pa
O
2
(mm Hg) = 100 – 0.325 × age (years)
The normal value for the P(
A
–a)
O
2
at rest for a given age
can be calculated as follows:
P(
A
–a)
O
2
(mm Hg) = (age + 10) × 0.25
Based on this formula, a 90-year-old subject will have a
predicted Pa
O
2
of 71 mm Hg and a maximum normal
P(
A
–a)
O
2
of 25 mm Hg at sea level.
Changes in position also influence the Pa
O
2
.Pa
O
2
is 6–10
mm Hg lower in the supine position than in the upright posi-
tion in the elderly. Postoperative hypoxemia is especially com-
mon in the elderly, in whom it may persist for several days.
There is no significant change in arterial pH or P
CO
2
with age.
Ventilatory control is also affected by age and is more
striking compared with the changes in lung volumes and
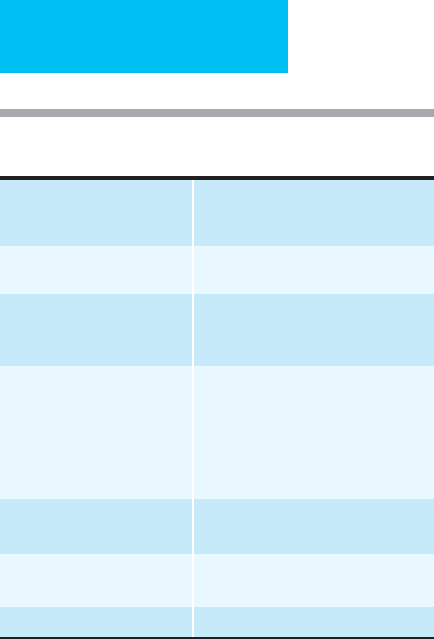
Table 19–1. Summary of age-related change in cardiac
physiology.
Heart rate At rest: unchanged
Maximal heart rate with
exercise: decreases
Stroke volume At rest: unchanged
With exercise: increases
Ejection fraction At rest: unchanged
With exercise: fails to increase as
much as in younger subjects
Cardiac output At rest: unchanged
Low- and medium-intensity exercise:
unchanged
High-intensity exercise: fails to
increase as much as in younger
subjects
Early diastolic left ventricular
filling rate
Decreases
Late diastolic left ventricular
filling rate (atrial ”kick”)
Increases
Ventricular compliance Decreases
CARE OF THE ELDERLY PATIENT
445
flow rates. The ventilatory response to hypoxemia is reduced
by half in healthy elderly men 64–73 years of age, whereas the
response to hypercapnia is reduced by 40%. Reasons for
these decreased responses are unclear. Suggested explana-
tions include altered central or peripheral chemoreceptor
function as well as reduction in neuromuscular inspiratory
output.
Right atrial, pulmonary artery, and pulmonary capillary
wedge pressures are unchanged in the healthy elderly at rest.
In contrast, the older person’s increases in pulmonary artery
and pulmonary capillary wedge pressures with exercise are
significant, and increases in pulmonary artery resistance are
highly significant with age.
There is a reduction in the effectiveness of cough and
mucociliary clearance with aging and a decline in the cellular
and humoral components of pulmonary immunity. These
changes predispose the older population to pulmonary
infections. Similarly, a diminished gag reflex, dyscoordina-
tion of swallowing, prolonged periods in the supine position,
and sedation contribute to an increased risk of aspiration.
Table 19–2 summarizes these findings.
The Aging Kidney
Many cross-sectional and longitudinal studies of large
human populations have shown a steady decline in creati-
nine clearance with age. As in any other area, the decline in
renal function with age is highly variable among individuals.
In general, changes owing to disease and to aging are in the
same direction and are additive. With aging, there is a loss of
nephrons at a rate of 0.5–1% per year. By the seventh decade
of life, there is a 30–50% loss of functioning glomeruli owing
to age alone. This loss occurs primarily in the renal cortex,
with relative sparing of the medulla. A progressive reduction
in renal plasma flow also has been demonstrated with age. A
50% reduction has been shown between young adulthood
and the eighth decade, averaging 10% per decade.
The major clinically relevant renal functional defect aris-
ing from these histologic and physiologic changes is a pro-
gressive decline, after maturity, in the glomerular filtration
rate (GFR). Age-adjusted normative standards for creatinine
clearance have been established. The rate of decline has been
estimated as 8 mL/min/1.73 m
2
per decade after the fourth
decade (or 0.8 mL/min per year). This rather drastic age-
related loss of renal function is not completely reflected in
the serum creatinine because of the proportionate decline in
skeletal muscle mass. Therefore, in order to make an estima-
tion of the glomerular filtration rate in the elderly, the serum
creatinine value should be incorporated in the Cockcroft and
Gault formula that takes into account the age, sex, and
weight of the patient:
Estimated creatinine clearance =
In women, the result should be multiplied by 0.85. For
obese individuals (body mass index [BMI] ≥ 30), ideal rather
than actual body weight should be used.
For the preceding reasons, dosage adjustments of medica-
tions excreted primarily by the kidneys should not be based
on serum creatinine values but rather on measured or esti-
mated creatinine clearance. Drugs that are excreted predom-
inantly through kidneys and have low therapeutic indices
(eg, digoxin, procainamide, and vancomycin) require close
monitoring of serum levels.
Since medullary nephrons, which are relatively spared
compared with cortical nephrons, have reduced concentrat-
ing ability, the elderly tend to excrete more free water. They
release more antidiuretic hormone in response to hyper-
tonicity, yet water retention is less than in younger individu-
als because of reduced end-organ response in older persons.
Older individuals tend to have diminished thirst perception
and diminished awareness of volume contraction. The
response to aldosterone is impaired, and the ability to con-
serve sodium is limited.
The age-related decline in other renal functions such as
urine concentration and dilution, tubular secretion and
reabsorption, and hydrogen ion secretion render the elderly
more susceptible to disorders of fluid, electrolyte, and acid-
base imbalance. Low renin and aldosterone levels can con-
tribute to hyperkalemia and hyponatremia.
Management of the Elderly Patient
in the ICU
Clinical Presentation of Disease in the Elderly
Elderly patients may present with multiple pathologic
processes in different organ systems. Various studies have
found an average of three to four medical conditions in
ambulatory older patients and five to nine medical diagnoses
among elderly patients in chronic care facilities.
[140 age (years)] body weight (kg)
72 se
−×
×
rrum creatinine (mg/dL)
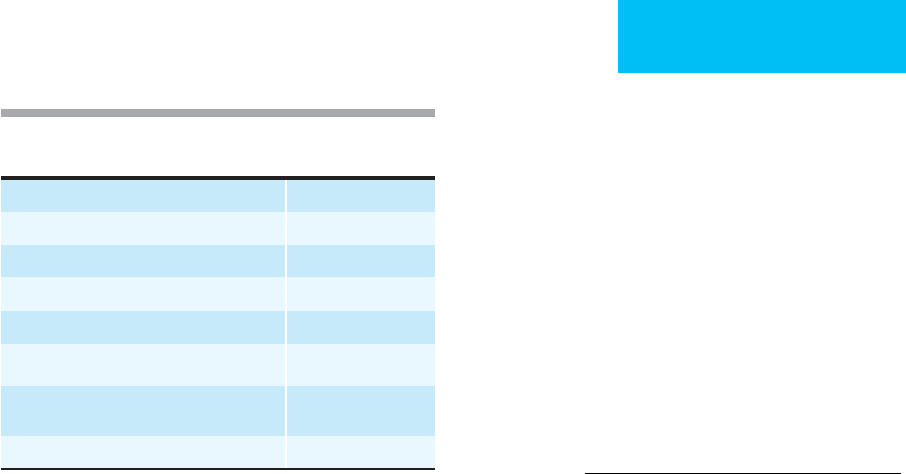
Forced vital capacity (FVC) Decreases
Forced expiratory volume in 1 second (FEV
1
) Decreases
Residual volume Increases
Arterial P
O
2
Decreases
Alveolar-arterial oxygen difference Increases
Arterial P
CO
2
Unchanged
Ventilatory response to hypoxia or
hypercapnia
Decreases
Mucociliary clearance Decreases
Table 19–2. Summary of age-related changes in
pulmonary physiology.

CHAPTER 19
446
Owing in part to the progressive decrease in physiologic
reserve with age and comorbidity, the elderly may have
unusual presentations of diseases. The onset of a disease in
the elderly generally affects the most vulnerable organ system
first. This explains the frequent apparent lack of relation
between the presenting symptom and the underlying disease.
Thus delirium, functional impairment, frequent falls, incon-
tinence, and syncope could be the presenting manifestations
of a variety of illnesses such as congestive heart failure, pneu-
monia, myocardial infarction, urinary tract infection, or GI
bleeding. Moreover, painless myocardial infarction may
occur in up to 30% of cases. This emphasizes the need for a
thorough evaluation when searching for the cause of non-
specific symptoms.
Drug Therapy
Iatrogenic illness is common and often preventable in the
elderly. The incidence of iatrogenic problems among acutely
hospitalized geriatric patients is close to one in three. By far
the most common iatrogenic disorders in the elderly are
adverse drug reactions. Changes in pharmacokinetics and
pharmacodynamics and polypharmacy predispose geriatric
patients to adverse reactions and drug interactions.
Pharmacokinetics is the study of the time course of
absorption, distribution, metabolism, and excretion of drugs
and their metabolites from the body. Absorption and metab-
olism are minimally affected by aging. Distribution is affected
by changes in body composition. For example, aging is asso-
ciated with an increased percentage of fat (50% increase in
men and 25% increase in women from age 40 to age 80) and
a concomitant decrease of total body water. Thus medications
that distribute in the water space (ie, hydrophilic drugs such
as digoxin and theophylline) have a lower volume of distribu-
tion and tend to reach higher levels in a shorter time in an
older patient. On the other hand, drugs that are lipid-soluble
(ie, lipophilic drugs such as the psychotropics) will have a
larger volume of distribution, resulting in progressive accu-
mulation of these drugs. The net effect of this will be to
increase the half-life of these drugs and prolong the duration
of action. This effect is further compounded by impaired
drug excretion because both renal and, to a lesser extent,
hepatic function tend to decrease with age.
In addition, some plasma protein levels may alter with age.
For example, serum albumin often falls with chronic comor-
bid conditions, resulting in higher free drug levels and a
potential for greater pharmacologic effect at the same dosage
or total serum level for protein bound drugs (eg, phenytoin).
As discussed earlier, renal function tends to decrease with
age, but concurrent changes in muscle mass keep the serum
creatinine constant at approximately 1 mg/dL, often masking
the declining renal function. Thus measurement of creati-
nine clearance or estimation with the Cockcroft and Gault
formula should be used to assess the GFR and make the nec-
essary adjustment in dosages of drugs excreted by the kid-
neys (see Chapter 4).
Cytochrome P450 enzymatic activity tends to decrease
with age. Warfarin and theophylline are examples of drugs
eliminated by this system. On the other hand, normal aging
does not significantly impair the conjugation capacity of the
liver. There is also a decrease in hepatic blood flow with age.
Compared with renal function, hepatic function is extremely
difficult to quantitate. Only sparse data are available on
hepatic drug metabolism in aging human subjects, and evi-
dence for altered hepatic metabolism in humans is largely
indirect and frequently inconsistent. For example, in studies
with antipyrine (a useful model compound for the study of
drug metabolism), large individual variation frequently
exceeds the effect of age such that only 3% of the variance in
metabolic clearance is explained by age alone.
Pharmacodynamics is the study of the physiologic
response to a drug or combination of drugs and is based on
drug-receptor interactions. For reasons that are not well
understood, the aging process appears to be associated with
an altered sensitivity of receptors for many commonly used
medications. In general, elderly subjects are more sensitive to
some medications, including warfarin, narcotics, sedatives,
and anticholinergic medications, and less sensitive to others,
such as β-adrenergic agonists and antagonists. However,
given the marked heterogeneity of the elderly as a group,
careful individualization should be the general rule when
drawing conclusions about such matters.
Because of multiple diseases and polypharmacy in the eld-
erly, the clinician always should check for possible drug-drug
and drug-disease interactions before prescribing any new
medication. The probability of a significant drug-drug inter-
action is nearly 7% for patients using more than 5 drugs and
24% for those using more than 10 medications. Special atten-
tion should be paid when prescribing medications with long
half-lives or with anticholinergic or potential CNS side effects.
Adverse drug effects can mimic almost any clinical syn-
drome in geriatrics and should be considered in the differen-
tial diagnosis of vague symptoms or deterioration of
function. For example, timolol eye drops—a β-blocker used
for glaucoma treatment—may be absorbed systemically and
can cause cardiac decompensation in a patient with poor
cardiac function.
Hydration and Nutrition
Hydration status is a major concern in the hospitalized eld-
erly. One of the most common reasons for electrolyte abnor-
malities or fluid disturbances in this population is
dehydration. Contributing factors may include laxative or
diuretic use, the presence of fever or infection, decreased
ability to recognize or express thirst, and limited access to
water. There is also an age-related decline in urine concen-
trating ability, which can lead to frequent urination and fluid
loss. Accurate fluid balance assessment is essential in nutri-
tional screening because alterations in hydration state may
contribute to inaccurate anthropometric and biochemical
markers. Because of the high prevalence of congestive heart
