Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


SURGICAL INFECTIONS
407
and sepsis. Suppurative thrombophlebitis and type 2
necrotizing fasciitis are generally monomicrobial. For the
most part, antibiotic treatment is important but secondary
to aggressive surgical debridement.
Cellulitis is an infection of soft tissues that retain their
blood supply and viability. There is edema and erythema, but
appropriate antibiotic therapy will resolve the infection in
most cases. Abscesses and fasciitis are associated with loss of
blood supply, tissue necrosis, and collections of bacteria,
leukocytes, and cellular debris. Surrounding tissues contain
an abscess, whereas fasciitis involves and spreads along facial
planes. Necrotizing fasciitis is a virulent process frequently
associated with septic shock and carries a high mortality.
Diabetic foot infections can present anywhere along this
range from cellulitis to fasciitis, with associated dry or wet
gangrene. Limited infection often responds to antibiotics,
but surgical debridement or amputation is required in the
face of abscesses, wet gangrene, osteomyelitis, or fasciitis.
These infections are associated with the neuropathy and vas-
culopathy of diabetes. In these patients, a distinction should
be made between macrovascular and microvascular disease.
Peripheral pulse assessment and documentation of ankle-
arm indices are essential to the evaluation of these patients,
although the latter can be inaccurate if the arteries are calci-
fied and noncompressible. At any rate, stenoses and occlu-
sions of named arteries may be amenable to percutaneous
and/or surgical amelioration, allowing salvage of tissue and
resolution of infection. Presence of wet gangrene, radi-
ographic evidence of soft tissue emphysema or osteomyelitis,
and signs of sepsis influence urgency of surgical manage-
ment of these infections. Surgeons must strike a balance
between being too radical with tissue resection and avoiding
serial operations that only postpone amputation.
Ultrasound and CT scanning define the character and
extent of soft tissue abscesses. Most abscesses will not resolve
with antimicrobial therapy alone; a combined approach with
image-guided or surgical drainage is usually required. It can
be difficult to distinguish between cellulitis and abscess on
the one hand and life-threatening necrotizing fasciitis on the
other. Classic “hard signs” of fasciitis include skin necrosis
and bulla formation, palpable crepitance and soft tissue gas
on radiography, and hypotension. However, some or all of
these may be absent. Pain out of proportion to clinical find-
ings is also an important clue to the diagnosis. CT scanning,
with its greater sensitivity than plain films, is currently used
widely to help with the diagnosis of these difficult cases.
When available, frozen-section analysis of a musculofascial
biopsy obtained at bedside under local anesthesia can estab-
lish the diagnosis in difficult cases.
There are two major categories of necrotizing fasciitis.
Type 1 is polymicrobial with involvement of at least one
anaerobic species such as C. perfringens. Facultative anaer-
obes from the Enterobacteriaceae family and nontypable
streptococci generally are involved as well. A subclass of type 1
necrotizing fasciitis is Fournier’s gangrene. This fulminate
infection involves the skin and soft tissues of the scrotum,
perineum, and penis. It spreads along the fascial planes and
can involve the thighs and wall of the torso. The majority of
patients with Fournier’s have diabetes mellitus. Type 2 is
monomicrobial, most commonly owing to group A β-hemolytic
streptococci (ie, GAS or Streptococcus pyogenes), the so-called
flesh-eating bacteria. Increasingly, community-acquired
MRSA is producing necrotizing fasciitis, including the pedi-
atric population. Antecedent varicella infection is a risk fac-
tor in about half these patients.
Necrotizing fasciitis has a mortality ranging from
20–60% in developed countries. Risk of death is elevated in
association with immunosuppression, IVDA, streptococcal
toxic shock syndrome, advanced patient age, and presence of
significant comorbidities. Delays in medical and surgical
therapy are deleterious to patient survival. Initial antibiotic
therapy includes high-dose intravenous penicillin, semisynthetic
β-lactam antibiotics, and clindamycin. The latter should
cover most strains of community-acquired MRSA, but van-
comycin should be considered pending final culture and sen-
sitivity results. Whether the fasciitis is type 1 or type 2 cannot
be determined confidently at the outset. Hemodynamically
unstable patients require early, aggressive crystalloid replace-
ment of intravascular volume. In general, central venous
pressure monitoring guides this volume resuscitation and
directs rational addition and titration of vasoactive medica-
tions such as norepinephrine and vasopressin.
The mainstay of treatment for necrotizing fasciitis is
prompt radical debridement of all involved skin, subcuta-
neous tissue, muscle, and fascia. Defining the limits of this
resection is difficult and requires experience, but insufficient
initial debridement can compromise patient survival.
Immediate amputation, even hip disarticulation, may be neces-
sary to effect survival in advanced cases. It is important, when
possible, to have a compassionate but frank discussion with the
patient and family as to the possible extent of surgery before
embarking on an operation for necrotizing fasciitis. General
comprehension of this illness’s severity should not be assumed.
Just as in ANM and necrotizing pancreatitis discussed earlier,
the need for multiple operations should be anticipated.
Adjunctive measures such as hyperbaric oxygen therapy and
intravenous immunoglobulin administration have been
advised for treatment of necrotizing fasciitis, but their use has
not been rigorously verified in controlled studies.
An uncommon but similarly life-threatening infection
seen in burn and other surgical ICUs is suppurative throm-
bophlebitis. Inflammatory superficial thrombophlebitis
occurs quite often after placement of peripheral vein
catheters. Fortunately, its infectious counterpart is unusual. It
should be suspected, though, in the febrile ICU patient whose
site of infection is elusive. All former sites of intravenous
access should be examined carefully for induration, erythema,
tenderness, centrally projecting red streaks, and purulent
drainage. The latter cinches the diagnosis, whereas the other
signs may indicate vein exploration under local anesthesia.
CHAPTER 16
408
If the vein is infected, it must be excised urgently in a distal-
to-proximal direction, stopping only when normal, patent
vein is encountered or all infected vein clearly has been
removed. On occasion, infection extends from peripheral
veins into central ones, and thoracotomy with central vein
resection may be a necessary lifesaving measure.
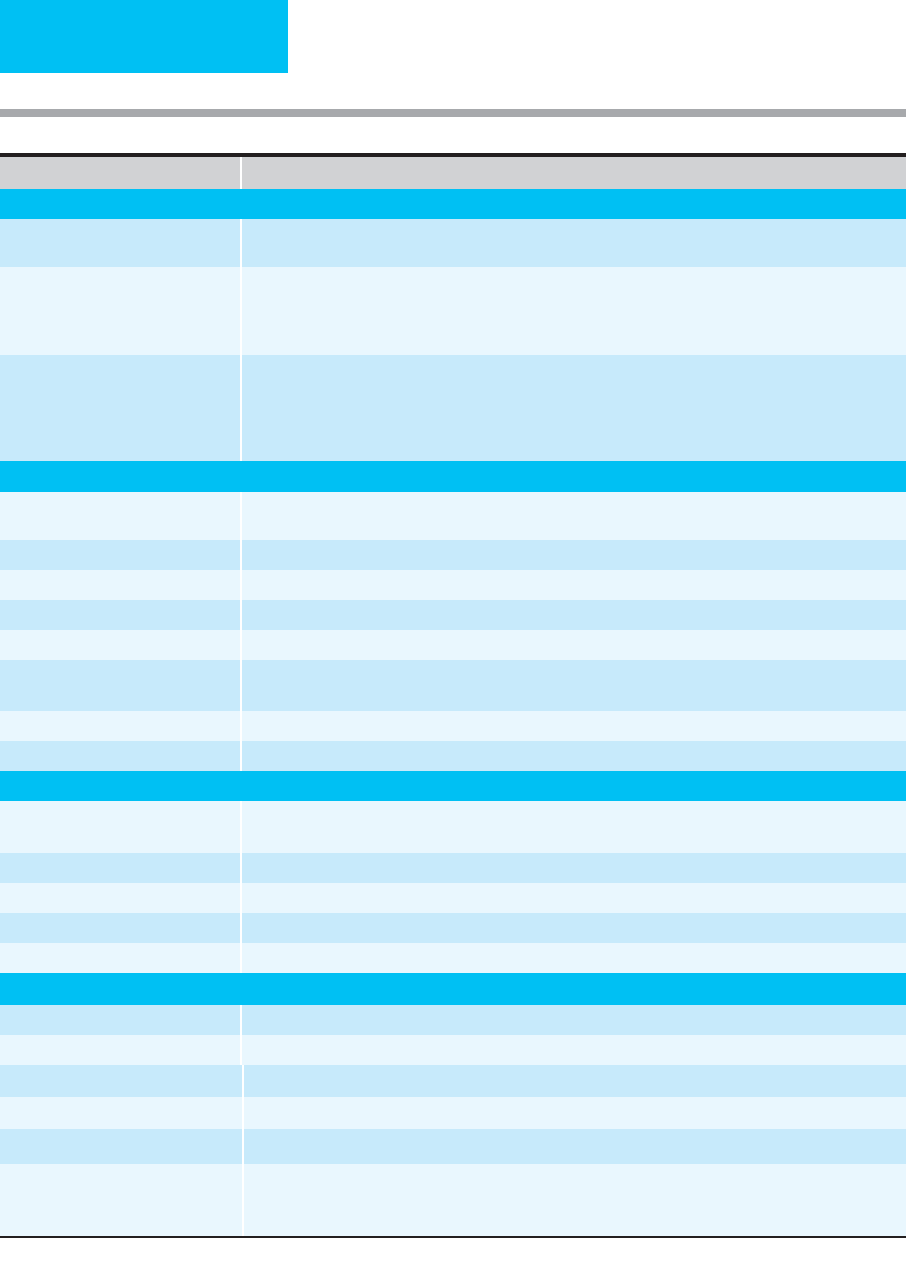
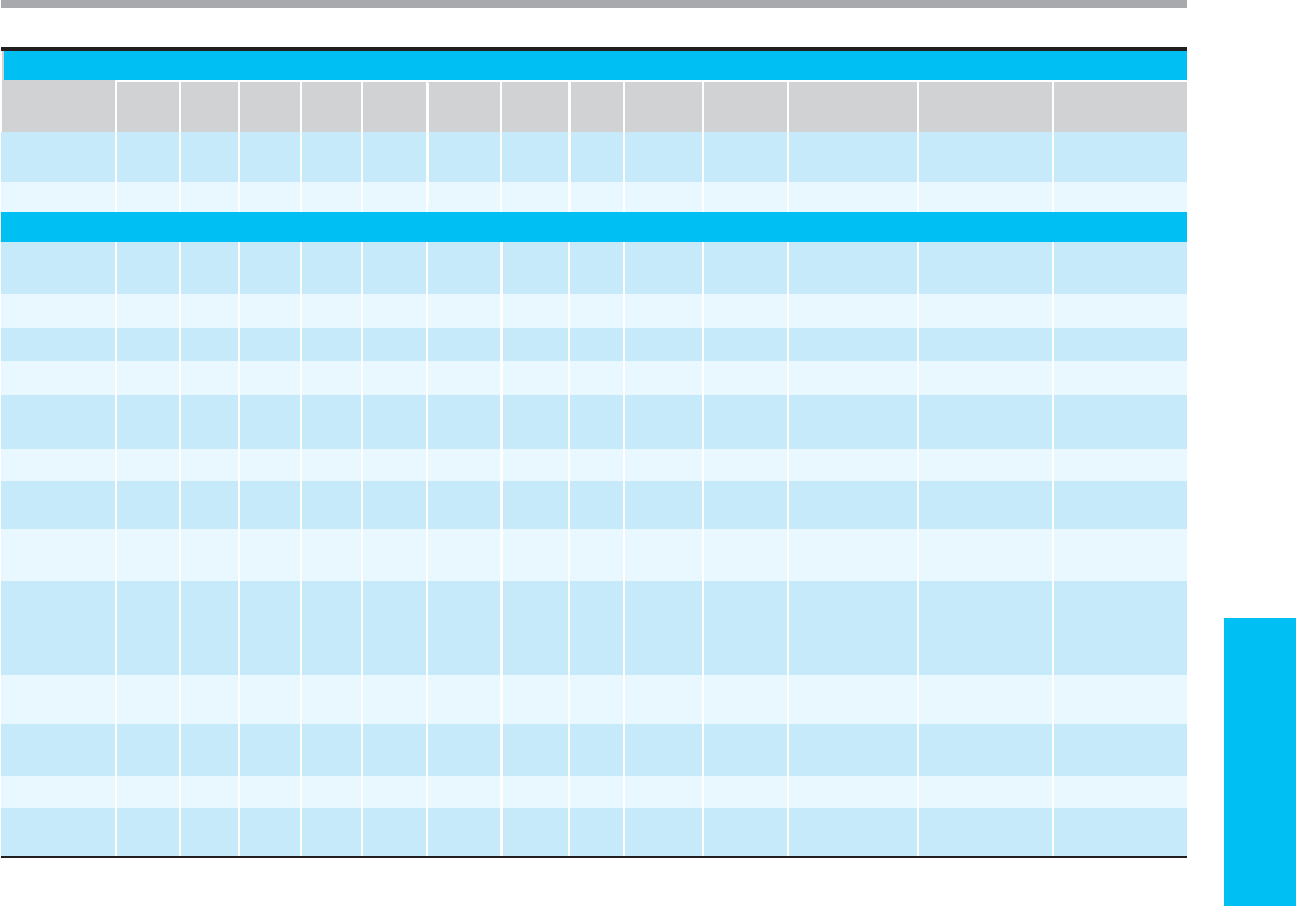
Treatment of soft tissue infections is summarized in
Table 16-4.
Golger A et al: Mortality in patients with necrotizing fasciitis. Plast
Reconstr Surg 2007;119:1803–7. [PMID: 17440360]
Rieger UM et al: Prognostic factors in necrotizing fasciitis and
myositis: Analysis of 16 consecutive cases at a single institution
in Switzerland. Ann Plast Surg 2007;58:523–30.
Table 16–4. Summary of soft tissue infections in adult surgical patients.
Diagnosis Organisms Initial Antibiotics Adjunctive Therapy
Diabetic foot infection
S. aureus
(assume MRSA), group
A strep
(S. pyogenes),
group B
strep
(S. agalactiae),
coliforms,
anaerobes
Vancomycin 1 g IV q12h + β-lactam with
β-lactamase inhibitor
or
carbapenem IV
Surgical debridement,
vascular surgical evaluation as
indicated
Cellulitis and soft tissue abscess
S. pyogenes,
group B, C, and G
strep,
S. aureus,
Enterobacteriaceae
Penicillin G 1–2 million units IV q6h
or
nafcillin-oxacillin 2 g IV q4h; vancomycin
1 g IV q12h for facial cellulitis; for
diabetics, linezolid 600 mg IV q12h
or
vancomycin 1 g IV q12h + carbapenem
IV
Consider necrotizing fasciitis
Type 1 necrotizing fasciitis Aerobes, anaerobes including
Clostridium sp.
Penicillin G 24 million units/24 h in
divided IV doses q4–6h + clindamycin
900 mg IV q8h + vancomycin 1 g IV
q12h + ceftriaxone 2 g IV q24h
Goal-directed therapy for
sepsis, prompt and aggressive
surgical debridement
Type 2 necrotizing fasciitis
S. pyogenes
(GAS),
S. aureus
(community-acquired MRSA)
Penicillin G 24 million units/24 h in
divided IV doses q4–6h + clindamycin
900 mg IV q8h
Goal-directed therapy for
sepsis, prompt and aggressive
surgical debridement
Suppurative thrombophlebitis
S. aureus, S. pyogenes,
Enterobacteriaceae
Vancomycin 1 g IV q12h (MRSA),
nafcillin-oxacillin 2 g IV q4h (MSSA),
carbapenem IV
or
extended-spectrum
penicillin (Enterobacteriaceae)
Removal of intravascular
device, excision of entire
involved vein
Data from Gilbert DN et al (eds): The Sanford Guide to Antimicrobial Therapy, 37th ed. Sperryville, VA: Antimicrobial Therapy, Inc., 2007.
409
17
Bleeding & Hemostasis
Elizabeth D. Simmons, MD
Bleeding is a common problem in critically ill patients in the
ICU. A rational approach to diagnosis and treatment of
bleeding requires an understanding of the major elements
of the hemostatic system, currently available laboratory tests
of hemostatic function, and specific disorders of hemostasis.
Bleeding disorders generally are categorized into defects of
coagulation and fibrinolysis, defects of platelets, and defects
of vascular integrity, but critically ill patients who are bleed-
ing may have defects in multiple arms of the hemostatic sys-
tem. Furthermore, defective hemostasis may result in
thrombosis as well as bleeding.
Normal Hemostasis and Laboratory Evaluation
A. Normal Hemostasis—The major elements of hemostasis
are outlined in Table 17–1. A complex interaction of vascular
endothelium, platelets, red blood cells, coagulation factors,
naturally occurring anticoagulants, and fibrinolytic enzymes
results in formation of blood clot at the site of vascular
injury and activation of repair mechanisms to promote heal-
ing of the injured blood vessel. Vascular injury results in
platelet adhesion and aggregation, activation of coagulation
factors ultimately resulting in cleavage of fibrinogen to fib-
rin, and formation of a stable blood clot consisting of cross-
linked fibrin polymers, platelets, and red blood cells.
Simultaneously, naturally occurring anticoagulants and fib-
rinolytic enzymes are activated, a process that limits the
amount of clot formed and degrades clot once the vessel is
repaired. The latter aspects of hemostasis serve to confine
clot formation to the site of vascular injury while permitting
continued blood flow through the affected blood vessel. The
precise factors that regulate the balance between clot forma-
tion and breakdown are not fully understood.
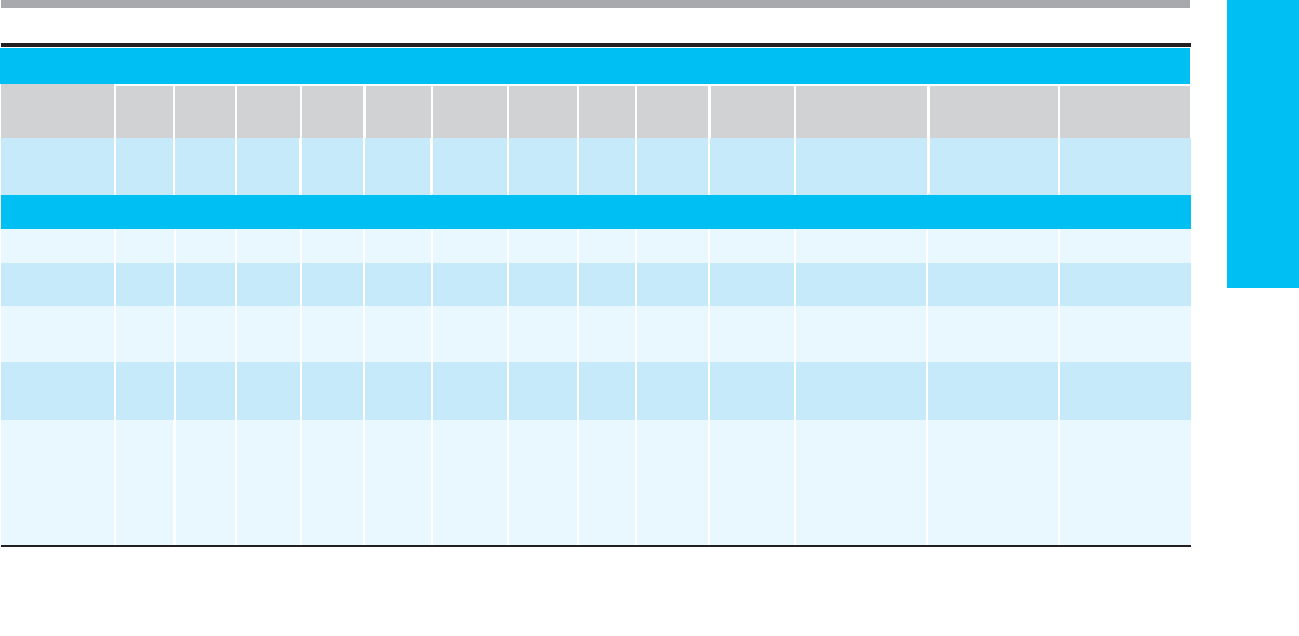
B. Laboratory Tests of Hemostasis (See Table 17–2)—
There are several generally available laboratory tests for eval-
uation of the function of the hemostatic system. Currently
available screening laboratory tests detect clinically signifi-
cant defects (quantitative and qualitative) of most but not all
of the important elements of hemostasis. The history should
dictate the choice of tests to determine the adequacy of hemo-
static function. A highly suggestive history for a bleeding dis-
order calls for sophisticated or specialized laboratory testing,
whereas abnormal test results may not be predictive of future
risk of bleeding in the absence of a significant bleeding history.
1. Tests of coagulation—Calcium and phospholipid are
required for normal coagulation to occur. In the laboratory,
measurement of coagulation times (eg, prothrombin time
and partial thromboplastin time) involves mixing decalcified
plasma (collected in citrate) and a phospholipid substitute
(thromboplastin), adding calcium, and determining the time
for visible clot formation using an automated system.
Different phospholipid reagents activate different parts of
the coagulation cascade, and an activating agent is added for
performance of the activated partial thromboplastin time
(aPTT). Prothrombin time (PT) generally is reported as the
international normalized ratio (INR), which compares
observed results against a reference thromboplastin to mini-
mize interlaboratory variability owing to differing sensitivi-
ties of thromboplastin reagents. The thrombin time (TT) is
performed by adding excess thrombin to decalcified plasma
(phospholipid is not required).
Standard coagulation times are not prolonged until factor
activities drop to less than 20–50% of normal (depending on
the specific factor deficiency). Therefore, a mixture of patient
plasma with normal plasma in equal quantities (1:1 dilution)
should normalize a prolonged coagulation time if due solely
to one or more factor deficiencies. Failure of a prolonged
coagulation time to correct after 1:1 dilution with normal
plasma implies the presence of a circulating inhibitor of
coagulation, including heparin. Detection of some factor
inhibitors may require incubation of the mixture prior to
performing the assay.
In vitro assessment of coagulation depends on the action
of factor XII, high-molecular-weight kininogen, and
prekallikrein (the contact factors), whereas in vivo hemostasis
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 17
410
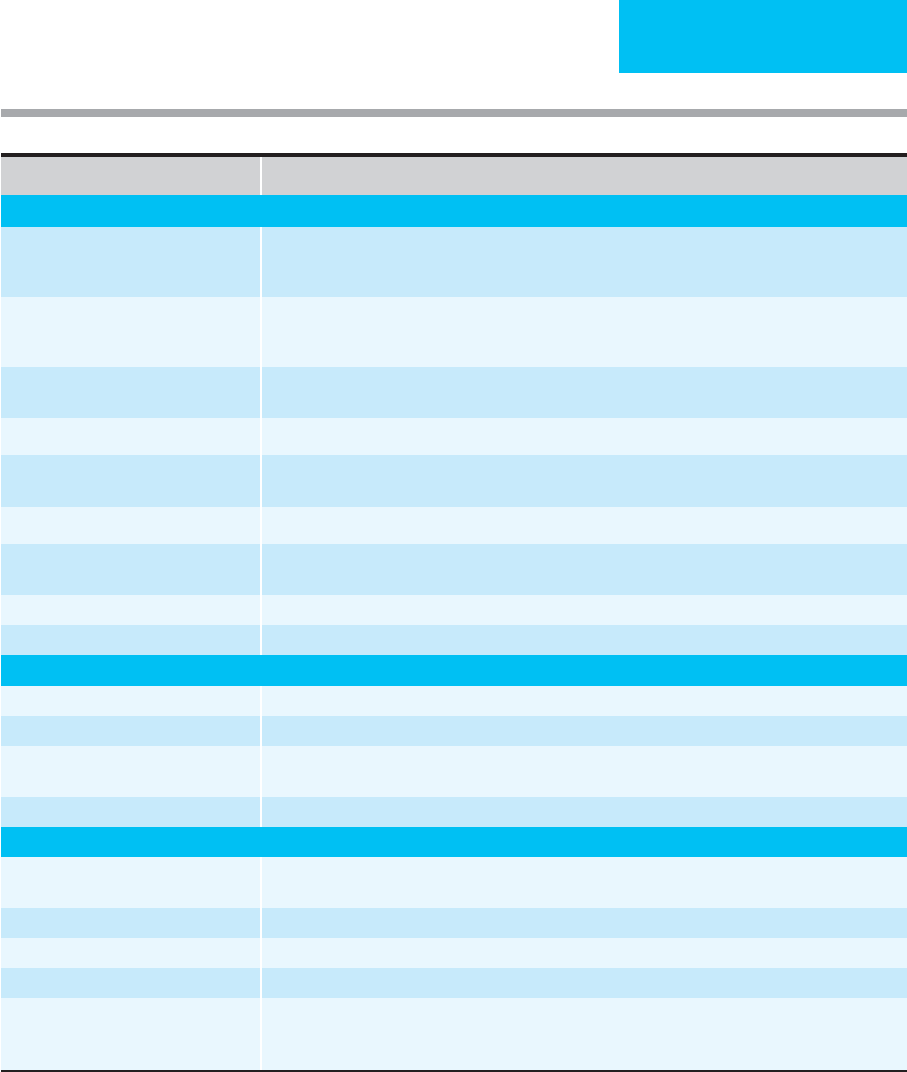
Element Participation in Hemostasis
Endothelium
Procoagulant Release of von Willebrand factor (vWF), factor VIII, tissue factor, plasminogen activator inhibitor, and platelet
activating factor in response to injury; maintains tight interendothelial junctions to prevent blood extravasation.
Anticoagulant Negative charge repels platelets and coagulation factors; produces prostacyclin; releases tissue plasminogen
activator in response to vessel injury; provides thrombomodulin for thrombin-mediated activation of protein
C; provides heparin-like molecules which interact with antithrombin III and accelerate its inactivation of
thrombin and other serine proteases.
Platelets Adhere to exposed subendothelium via vWF and aggregate in response to activation (via fibrinogen-glycoprotein
IIb/IIIa interaction); secrete agonists which stimulate further platelet aggregation; provide phospholipid for produc-
tion of thromboxane A
2
and for coagulation reactions; provide surface on which coagulation reactions are local-
ized; secrete coagulation factors (V, vWF), which increase local concentration; provide contractile machinery for
clot retraction; perhaps maintain interendothelial tight junctions by secretion of metabolically active substances.
Coagulation factors
Proenzymes In response to vascular injury, sequential activation (VII, IX, X, II) results in generation of thrombin and cleav-
age of fibrinogen to fibrin.
Thrombin In addition to cleavage of fibrinogen, activates platelets, factors V, VIII, and XIII, and protein C.
Fibrinogen Cleaved by thrombin to fibrin, which polymerizes to insoluble fibrin clot.
Factor XIII After activation by thrombin, cross-links fibrin polymers to stabilize clot.
Cofactors Factors V and VIII, both activated by thrombin, act as cofactors for X and IX, respectively.
Tissue factor Integral membrane constituent of vascular endothelial cells and stimulated monocytes; acts as receptor for
factor VII; initiates blood coagulation.
Calcium, phospholipid Necessary for several steps in coagulation.
Contact factors Factor XII, HMW kininogen, and prekallikrein are important for in vitro hemostasis only.
Anticoagulants
∗
Protein C Vitamin K-dependent anticoagulant, inactivates factors V and VIII after activation by thrombin bound to throm-
bomodulin on endothelial surfaces.
Protein S Vitamin K-dependent cofactor for protein C.
Thrombomodulin Receptor for thrombin, initiates activation of protein C pathway.
Antithrombin (AT) Inactivates thrombin and other serine proteases of the coagulation cascade.
Tissue factor pathway inhibitor (TFPI) Inhibits tissue factor/factor VIIa complex.
Fibrinolytic system
Tissue plasminogen activator Cleaves fibrin-bound plasminogen to plasmin.
Urokinase Plasminogen activator found in urine and in plasma when fibrinolysis is stimulated.
Table 17–1. Normal hemostasis.
Plasminogen Once activated to plasmin, lyses fibrin and fibrinogen.
Plasminogen activator inhibitor-1 (PAI-1) Prevents activation of plasminogen by tissue plasminogen activator.
Alpha
2
-antiplasmin Inactivates circulating plasmin and prevents lysis of fibrin and fibrinogen.
Blood elements and rheology Laminar flow prevents contact of cellular elements with endothelium; free flow prevents accumulation of factors
at uninjured sites and dilutes concentration of activated factors; dislodges platelet plugs if not firmly attached to
subendothelium; provides inhibitory plasma proteins other than antithrombin to inactivated coagulation factors.
∗
Precise physiologic role in hemostasis not well defined: Other serine proteinase inhibitors (Serpin): alpha
2
-macroglobulin, alpha
1
-proteinase
inhibitor, C1 esterase inhibitor, protein C inhibitor, heparin cofactor II.
BLEEDING & HEMOSTASIS
411
appears to occur normally even with complete deficiency of
any of these proteins. Factor XI likewise is essential for in
vitro coagulation, but factor XI deficiency generally is associ-
ated with a very mild bleeding tendency. Specific coagulation
factor deficiencies can be identified using known deficient
plasma in a modification of the 1:1 dilution test when clini-
cally indicated.
Standard screening coagulation tests (ie, PT, aPTT, and
TT) do not detect mild coagulation factor deficiencies, factor
XIII deficiency, defects in fibrinolysis, or abnormalities of
platelets, blood vessels, or supporting connective tissue.
They are not useful for determining deficiencies of the nat-
urally occurring anticoagulants or for evaluating patients
with thrombotic disorders (except for patients with lupus
Test (normal range) Significance of Abnormal Test
Coagulation
Prothrombin time (PT)
(10–13 seconds) expressed as the
international normalized ratio (INR) (1.0)
Deficiencies of or inhibitors to extrinsic and common pathway factors: VII, X, V (<50%), II (<30%),
fibrinogen (<100 mg/dL).
Activated partial thromboplastin time
(aPTT) (25–40 seconds)
Deficiencies of or inhibitors of contact factors, intrinsic and common pathway factors: XII, HMW kininogen,
prekallikrein, XI (<50%), VIII, IX (<20%), X, V, II (<30–50%), fibrinogen (<100 mg/dL). Decreased value
may indicate increased concentration of factor (especially VIII) or hypercoagulable condition.
Thrombin time (TT) (10 seconds) Deficiency or defect of fibrinogen, inhibitors of thrombin action (heparin), or inhibitors of fibrin polymer-
ization (FDP, myeloma proteins).
Reptilase time Deficiency or defect of fibrinogen. Similar to thrombin time but unaffected by heparin.
Stypven time (Russell viper
venom time)
Differentiate factor X from factor VII deficiency (abnormal in factor X deficiency).
Dilute Russell viper venom time Detect lupus anticoagulant; affected by heparin.
1:1 dilution test (corrects to normal) Failure to correct consistent with inhibitors to specific factors or to phospholipid; heparin effect.
Correction to normal consistent with factor deficiency (some inhibitors may require incubation).
Factors assays (60% to >100%) Deficiencies of one or more coagulation factors.
5 M urea clot stability Deficiency of factor XIII.
Platelets
Platelet count (150,000–400,000/μL) Quantitative abnormalities of platelets.
Bleeding time (3–10 minutes) Impaired platelet function, thrombocytopenia, severe anemia, improper technique.
Aggregation (qualitative) Impaired platelet aggregation in response to platelet agonists; can localize defect based on pattern of
abnormal aggregation.
Ristocetin cofactor assay Decreased quantity or function of vWF in patient plasma.
Fibrinolysis
Fibrin(ogen) degradation products
(FDP) (<10 μg/mL)
Accelerated fibrinolysis.
Fibrinogen (150–400 mg/dL) Deficiency of fibrinogen.
Euglobulin lysis time (>2 hours) Accelerated fibrinolysis.
Protamine sulfate test Positive test indicates presence of circulating fibrin monomers.
D-dimer test Positive test indicates presence of cross-linked FDP, formed only if activation of factor XIII has resulted in
cross-linkage of fibrin polymers. Elevated in DIC, fibrinolysis, deep vein thrombosis, and pulmonary
embolism.
Table 17–2. Tests of hemostatic function (average normal values given).

CHAPTER 17
412
anticoagulants and contact factor deficiencies). Coagulation
times shorter than normal occur frequently, particularly if
there are higher than normal levels of any of the factors
measured by the test (especially factor VIII), which may
mask deficiencies of other factors.
2. Platelets—The platelet count can be determined by
automated cell counter or by estimation on a peripheral
blood smear (normal, 10–20 platelets/high-power field
[hpf]). The bleeding time is an in vivo test of platelet func-
tion. Bleeding time is affected by platelet number, platelet
function, position and depth of the incision, maintenance of
constant pressure above the site of the incision, medications,
hemoglobin concentration, and renal function. In thrombo-
cytopenic patients, the bleeding time varies as a function of
the cause as well as the degree of thrombocytopenia.
Although the bleeding time is useful in diagnosis of disor-
ders of platelet function, it may not be reliable as a predictor
of clinical bleeding. Other tests of platelet function include
in vitro platelet aggregation in response to various agonists
(eg, thrombin, epinephrine, adenosine diphosphate, and ris-
tocetin) for evaluation of patients suspected of having sig-
nificant disorders of platelet function rather than number.
3. Fibrinolysis—Elevated fibrin and fibrinogen degrada-
tion products and decreased fibrinogen concentration may
reflect excessive intravascular fibrinolysis, but these measure-
ments are not specific. The protamine sulfate test and the D-
dimer test may be useful to confirm the presence of
disseminated intravascular coagulation (DIC) as the cause of
elevated fibrin degradation products. The euglobulin lysis
time, which measures the action of plasminogen activators
and plasmin in blood, may be useful for confirming the pres-
ence of excessive fibrinolysis. Specific assays for elements of
the fibrinolytic system are available if clinically indicated.
Inherited Coagulation Disorders
ESSENTIALS OF DIAGNOSIS
Personal and family history of bleeding disorder.
Abnormal screening coagulation tests.
Abnormal specific factor assays.
General Considerations
Inherited coagulation disorders result from a decrease in
quantity or function of a single coagulation factor, although
there are some cases of familial multiple coagulation factor
deficiencies. The inheritance pattern may be autosomal or X-
linked, dominant or recessive, or may be the result of a new
mutation, so a negative family history does not preclude the
presence of an inherited disorder of coagulation. A personal
history of bleeding may be absent if the defect is mild or if
there has been no prior challenge to the hemostatic system
(eg, major surgery or trauma). In addition, some coagulation
defects are variable over time, with fluctuations both in
bleeding manifestations and in laboratory abnormalities.
Nevertheless, most of the inherited disorders of blood coag-
ulation result in a typical clinical bleeding history accompa-
nied by characteristic reproducible laboratory abnormalities
(Table 17–3).
von Willebrand disease (vWD) is the most common inher-
ited bleeding defect in humans, but prevalence figures vary
widely because of variable expression and penetrance of the
genetic abnormality. The disease results from inheritance of
an autosomal dominant (rarely, autosomal recessive) decrease
in the quantity or function of von Willebrand factor (vWF).
vWF is essential in platelet adhesion and serves as a carrier for
the procoagulant factor VIII protein. Clinical manifestations
typically reflect impaired platelet function, with epistaxis,
easy bruising, menorrhagia, and excessive bleeding after sur-
gery, trauma, or dental procedures. Severe deficiencies (<1%
activity) are rare and may result in bleeding similar to that
seen in hemophilia A. vWD is heterogeneous in severity and
is subject to variability over time and within families. During
pregnancy, vWF levels increase, often sufficiently to permit
adequate hemostasis at childbirth.
Hemophilia A, which accounts for 80% of all hemophil-
ias, results from inheritance of an X-linked recessive muta-
tion in the factor VIII gene, giving rise to severe (<1%
activity), moderate (1–5% activity), or mild (>5% activity)
factor VIII deficiency. The incidence of hemophilia A is
approximately 1 in 5000 men. Hemophilia A does occur in
women, owing either to early X chromosome inactivation of
the normal X in a heterozygous female or to inheritance of
two abnormal X chromosomes (one from an affected father
and one from a carrier mother).
Clinical manifestations depend on the severity of the
deficiency (70% of patients have severe deficiency) but typi-
cally include lifelong spontaneous hemarthroses and soft tis-
sue hematomas, hematuria, and if severe, increased epistaxis,
gum bleeding, and ecchymoses. Postoperative or dental
bleeding is severe and prolonged. CNS hemorrhage occurs in
about 3% of patients and may be fatal. The severity of the
deficiency is generally constant within a family and over time
in an individual, but it varies between families.
Hemophilia B results from inheritance of an X-linked
recessive mutation in the factor IX gene. The pathophysiology
and clinical manifestations are virtually identical with those
of hemophilia A, although severe deficiency is present in only
50%. Hemophilia B is much less common than hemophilia A,
with an estimated incidence of 1 in 50,000 men.
Inherited deficiencies of all the other coagulation factors
have been reported (see Table 17–3), but these are rare. All are
autosomally inherited, usually recessive, and often result from
consanguineous parentage. Clinical severity correlates with
the degree of factor deficiency but is typically milder and
more variable than in hemophilias A and B. Combined defi-
ciencies of multiple coagulation factors are rare. Deficiencies
of factor XII, prekallikrein, and high-molecular-weight
kininogen cause prolongation of the aPTT but are not asso-
ciated with excessive bleeding or thrombosis.
BLEEDING & HEMOSTASIS
413
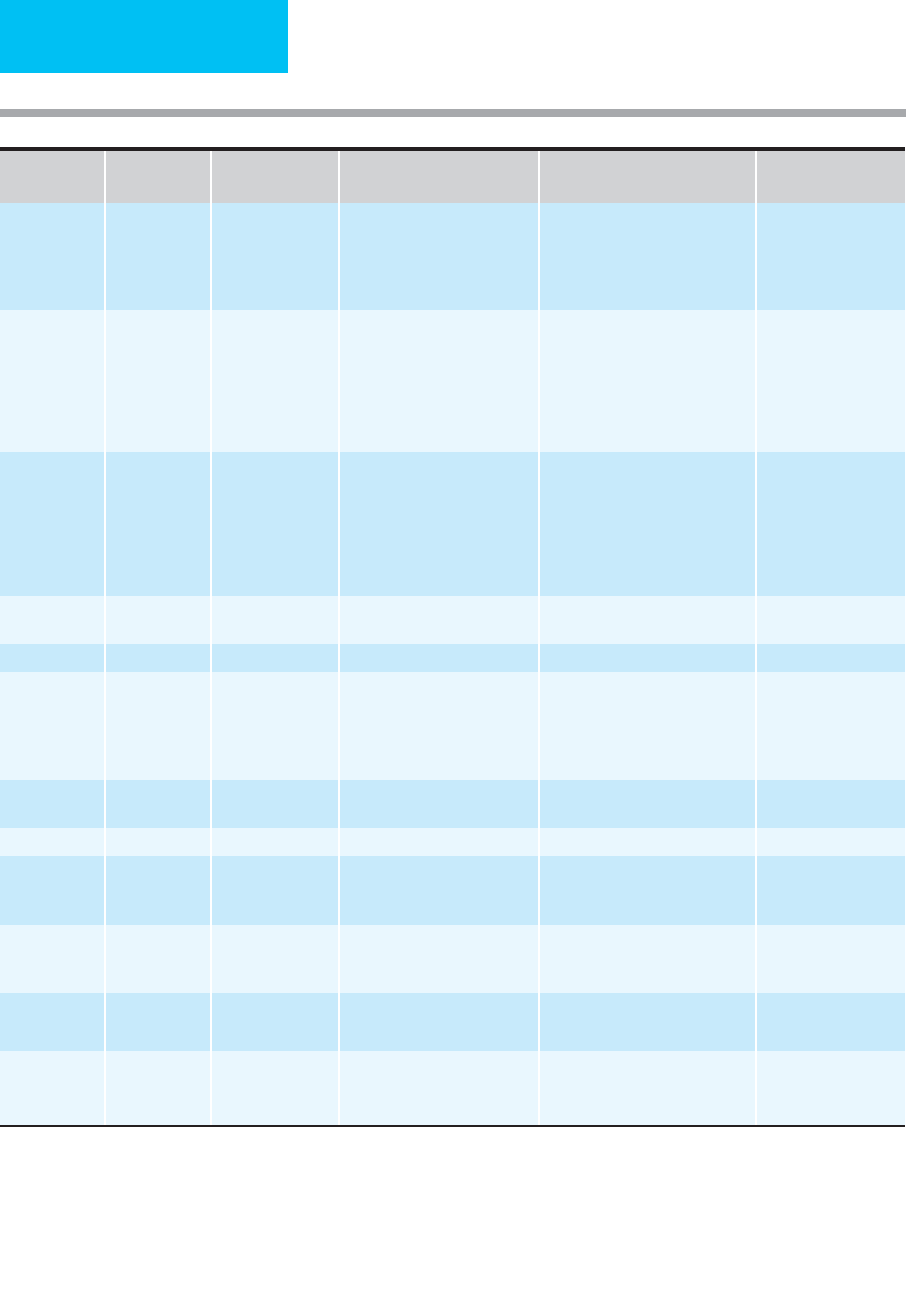
Table 17–3. Clinical manifestations of inherited coagulation factor deficiencies.
(
continued
)
Factor Deficiency
vWF VIII IX II V VII X XI XIII Fibrinogen
Dysfibrinogenemia
Combined Factor
V/VIII deficiency
Multiple Vitamin K-
dependent factors
Inheritance AD/AID/
AR
XR XR AR AR AR AIR AR AR AR AD AR AR
Incidence 1:100 1/10 K 1/40 K Rare Rare Rare Rare Rare
∗
Rare Rare Rare Rare Rare
Clinical manifestations
Severity
(most cases)
Mild 70%
severe
50%
severe
Mild Mild,
variable
Moderate,
variable
Moderate Mild Severe Mild Mild Moderate to severe Variable, not well-
described
Easy bruising + (+) (+) (+) + + + (+) + +
Epistaxis + (+) (+) (+) + + + (+) + + + +
Menorrhagia + (+) + + + (+) + + + +
Soft tissue
hematomas
+ + (+) (+) + + (+) + (+) +
Hemarthrosis • + + (+) (+) + + + (+) + +
Intracranial
hemorrhage
+ + • + + + + •
Gastrointestinal
hemorrhage
+ + (+) + + + (+)
Bleeding with
trauma, surgery,
or dental
procedures
+ + + + + (+) (+) (+) + • (+) + +
Umbilical stump
bleeding
• • + + • (+)
Spontaneous
abortions
+ + + +
Male infertility +
Poor wound
healing
(+) (+) + +
CHAPTER 17
414
∗
Factor XI deficiency much more common in Ashkenazic Jews (5–11% heterozygous).
†
Specific factor assays are available for the diagnosis of all the inherited factor deficiencies.
Key: Inheritance: AD, autosomal dominant; AR, autosomal recessive, XR, X-linked recessive; AIR, autosomal incompletely recessive; AID, autosomal incompletely dominant
Frequency of clinical manifestations: + common; (+) occasional; • rare
Thromboembolic
complications
+ + (with rx)
Laboratory abnormalities
PT prolonged + + + + + + + +
aPTT prolonged + + + + (+) + + + + + +
Thrombin time
prolonged
+ +
Bleeding time
prolonged
+ (+) (+) (+)
Other laboratory
tests
†
Risto-
cetin
cofactor,
factor
VIII
assay
Stypven
time
Stypven
time
5 M urea Reptilase time,
euglobulin lysis,
fibrinogen immuno-
electrophoresis
Low protein C/S
Table 17–3. Clinical manifestations of inherited coagulation factor deficiencies. (continued)
Factor Deficiency
vWF VIII IX II V VII X XI XIII
Fibrinogen
Dysfibrinogenemia
Combined Factor
V/VIII deficiency
Multiple Vitamin K-
dependent factors

BLEEDING & HEMOSTASIS
415
Clinical Features
A. Symptoms and Signs—Bleeding may occur sponta-
neously, but patients sometimes will give a history of bleed-
ing only after surgery, trauma, or dental extractions. In those
with vWD, platelet function is affected, so easy bruising and
menorrhagia may be prominent complaints. On the other
hand, patients with hemophilia often have spontaneous
hemarthroses, soft tissue hematomas, and hematuria. Physical
findings may reflect recent bleeding or may show evidence of
chronic bleeding such as decreased range of joint motion.
B. History—A detailed personal and family history of bleed-
ing often will uncover the nature of the coagulation disorder
and suggest its inheritance pattern. A family history of con-
sanguinity is pertinent for the rare autosomal recessive disor-
ders, and Ashkenazic Jewish ancestry may suggest the
possibility of factor XI deficiency.
C. Laboratory Findings—Laboratory abnormalities may
suggest an underlying hereditary bleeding disorder, but it is
important to remember that not all prolonged coagulation
tests indicate a bleeding diathesis, and some inherited bleed-
ing disorders are associated with normal coagulation tests.
There may be variability over time in some disorders, such as
vWD. The extent of laboratory evaluation for an inherited
coagulation disorder should be determined by the clinical his-
tory. Table 17–3 outlines the typical laboratory features of the
inherited coagulation disorders. Functional assays for factors
II, V, VII, VIII, IX, X, XI, and XII using known deficient
plasma in a modification of the 1:1 dilution test confirm spe-
cific factor deficiencies. Clot stability in 5 M urea with and
without the addition of normal plasma is the screening test of
choice for diagnosis of factor XIII deficiency and can be con-
firmed with a specific factor assay. The diagnosis of vWD is
based on finding low vWF antigen, abnormal ristocetin cofac-
tor activity, and low factor VIII activity (usually <10%).
Quantitative deficiency of vWF can be differentiated from
qualitative defects by electrophoretic analysis of vWF multi-
mers. Determining the subtype of vWD by multimer analy-
sis is important for proper management of bleeding
episodes.
Differential Diagnosis
Bleeding associated with abnormal coagulation tests also
may result from acquired coagulation disturbances, includ-
ing liver disease, vitamin K deficiency, DIC, inhibitors of spe-
cific factors, or therapeutic anticoagulation. Abnormal
coagulation tests may result from a deficiency of one of the
contact factors or from the presence of antiphospholipid
antibodies (lupus anticoagulant), neither of which causes
bleeding but may be associated with thrombosis. Mild coag-
ulation factor deficiencies may be associated with normal
or minimally prolonged clotting times and may result in
bleeding only if major vascular injury occurs. Bleeding in the
presence of normal coagulation times suggests the presence
of an underlying vascular defect, abnormal supporting con-
nective tissue, thrombocytopenia or platelet dysfunction,
excessive fibrinolysis, or factor XIII deficiency. Acquired
inhibitors to coagulation factors may be found in patients
with inherited factor deficiencies as a consequence of
replacement therapy and may be suspected in those who do
not respond adequately to factor replacement. An inhibitor
of coagulation can be confirmed by performing a 1:1 dilu-
tion test with normal plasma (preincubation may be neces-
sary to demonstrate the inhibitor).
Treatment
Factor replacement is appropriate for patients with inherited
coagulation disorders who have active bleeding or who
require surgical or dental procedures. The activity level nec-
essary for adequate hemostasis varies for each factor and
with the type of bleeding or planned procedure. General
guidelines for factor replacement are outlined in Table 17–4.
Aspirin and intramuscular injections should be avoided.
Surgical procedures should be performed only in centers
with adequate blood bank, coagulation laboratory, and
hematology consultation services. Treatment strategies for
patients with inhibitors complicating factor deficiencies
include desmopressin (for minor bleeding), high-dose fac-
tor replacement, use of products that bypass the factor
inhibitor (eg, activated prothrombin complex concentrate
with factor VIII inhibitor bypassing activity, recombinant
factor VIIa, and porcine factor VIII), and techniques to
lower the titer of the inhibitor (eg, plasmapheresis, intra-
venous immune globulin, immunosuppression, and induc-
tion of immune tolerance).
Adjuncts to factor replacement include desmopressin
acetate, antifibrinolytic agents such as aminocaproic acid and
tranexamic acid, and topical hemostatic agents such as fibrin
glue and fibrillar collagen preparations applied directly to
local areas of mucosal bleeding, such as epistaxis.
Desmopressin by intravenous (0.3 μg/kg over 15–30 minutes)
or intranasal (1.5 mg/mL in each nostril) administration
increases circulating levels of vWF and factor VIII by 2 to 5
times baseline within 15–30 minutes by releasing these factors
from endothelial storage sites. Desmopressin is useful for
most patients with vWD and in patients with mild to moder-
ate hemophilia A. Repeated infusions within 1–2 days may be
less effective, however, limiting the usefulness of desmo-
pressin in patients requiring sustained increases in vWF, fac-
tor VIII, or both. On the other hand, use of desmopressin may
completely eliminate the need for blood products in mild
bleeding episodes or during minor dental or surgical proce-
dures and may decrease the amount of blood products
required for major bleeds or surgical procedures. A test dose
of desmopressin should be administered about 1 week before
a planned surgical procedure to determine if a patient with
vWD or hemophilia A is responsive. Severe hemophiliacs and
those with qualitative abnormalities of vWF are rarely respon-
sive to desmopressin. Some subtypes of vWD (eg, type 2B)
CHAPTER 17
416
Factor
Deficiency
t
1/2
Hemostatic
Level
1
Preferred Sources
2
Dose
Interval Between
Doses
vWF 12 hours 25–50%
a. Desmopressin
3
b. Humate-P
c. Cryoprecipitate
4
a. 0.3 μg/kg IV/30 minutes or
1.5 mg/mL nasal spray
b. 30 units/kg
a. 24–48 hours
b. 12 hours for 2 days,
then 24 hours
VIII 9–18 hours 25–30% a. Purified factor VIII
b. Recombinant factor VIII
c. Desmopressin
5
a. 10–15 units/kg (minor),
30–40 units/kg (major)
b. 10 units/kg (minor); 15–25
units/kg (moderate); 40–50
units/kg, then 20–25 units/kg
(major); 50 units/kg (surgery)
12 hours (6–12 hours
following major surgery)
IX 20–25 hours 15–30% a. Purified factor IX
b. Recombinant
factor IX
c. Purified prothrombin
complex concentrates (PCC )
a. 10–20 units/kg
b. 100 units/kg, then 7.5
units/kg/h
c. 20–30 units/kg, then 15
units/kg (minor); 40–60
units/kg, then 20–25 units/kg
(major bleeding or surgery)
24 hours
II 3 days 20–40% a. Plasma
b. Purified PCC
a. 15 mL/kg, then 5–10 mL/kg
b. 20 units/kg, then 10 units/kg
24 hours
V 36 hours 25–30% FFP, PCC 15–20 mL/kg, then 10 mL/kg 12–24 hours
VII 4–7 hours 15–20% a. Plasma
b. Purified PCC
c. Recombinant factor VII
d. Factor VII concentrate
a. 20 mL/kg, then 5 mL/kg
b. 30 units/kg, then 10–20
units/kg
c. 15–30 μg/kg
d. 30–40 units/kg
a/b. 4–6 hours
c/d. 12 hours
X 40 hours 10–20% a. Plasma
b. Purified PCC
a. 15–20 mL/kg, then 10 mL/kg
b. 20–30 units/kg
24 hours
XI 80 hours 10–20% Plasma 15–20 mL/kg, then 5 mg/kg 48 hours
XIII 9–12 days 3–5% a. Plasma
b. Cryoprecipitate
c. Factor XIII concentrate
a. 15–20 mL/kg
b. 1 bag/10 kg
c. 10–20 units/kg
20–30 days
Fibrinogen 3–4 days a. Plasma
b. Cryoprecipitate
c. Fibrinogen concentrate
a. 15–20 mL/kg
b. 1 bag/10 kg
c. 20–30 mg/kg
48 hours
Combined
factors V/VIII
36 hours (V)
9–18 (VIII)
25–30% a. Plasma
b. Desmopressin (as in VIII)
a. 15–20 mL/kg 12 hours
Multiple Vitamin
K-dependent
factors
Varies by factor
(II, VII, IX, X)
Varies by factor a. Plasma
b. PCC
c. Oral Vitamin K
a. 15–20 mL/kg
b. 10–30 units/kg
c. chronic, high dose
Monitor levels
1
Estimated level required for normal hemostasis. Higher levels required for major bleeding or surgery (factors VIII and IX: 100%, factor XIII: 25–50%).
2
Plasma, fresh frozen (FFP) or fresh (FP), may be used interchangeably except for replacement of factors V and VIII.
3
Desmopressin is thrombogenic; use with caution in older patients with vascular disease; may induce fibrinolysis, often used in combination
with antifibrinolytic agents. Must give a test dose to determine efficacy; not effective for vWD type 2b, platelet-type vWD.
4
Use only if factor concentrate is unavailable.
5
In mild hemophilia A, may reduce or eliminate need for factor VIII replacement for minor surgery, dental work, or acute bleeding episodes.
Same dose as in vWD.
Table 17–4. General principles of factor replacement for inherited coagulation disorders.
