Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


BLEEDING & HEMOSTASIS
417
have been associated with thrombocytopenia following
desmopressin therapy because of increased binding of aber-
rant vWF to platelets. If the response to desmopressin is
unknown and a patient is actively bleeding, factor replace-
ment with blood products is preferable. Desmopressin also
stimulates release of tissue plasminogen activator, so antifib-
rinolytic therapy is often administered simultaneously.
Aminocaproic acid and tranexamic acid are two commer-
cially available antifibrinolytic agents that may be useful for
managing bleeding in patients with a wide variety of bleed-
ing disorders. The use of antifibrinolytics in combination
with desmopressin often eliminates the need for any blood
product administration for patients with vWD or mild
hemophilia A with minor bleeding or after dental proce-
dures. Antifibrinolytic therapy also may be useful as an
adjunct to factor replacement in any inherited coagulation
disorder unless there are contraindications such as hema-
turia, uncontrolled DIC, or use of prothrombin complex
concentrates. For acute bleeding, aminocaproic acid usually
is given as an intravenous infusion at a rate of 1 g/h until
bleeding is controlled (maximum 24 g in 24 hours), followed
by a maintenance dose of 6 g intravenously or orally every 6
hours for 7–10 days. The suggested dose of tranexamic acid
is 10 mg/kg intravenously or 25 mg/kg orally three or four
times a day beginning 1 day before surgery or at the onset of
acute bleeding and to be continued for 2–8 days.
Current Controversies and Unresolved Issues
Current recommendations regarding factor replacement for
inherited coagulation disorders stem primarily from anec-
dotal experience rather than from carefully designed clinical
trials comparing one regimen with another. The optimal
level of factor activity, the precise interval between doses, and
the duration of therapy are somewhat arbitrary and for most
of the rare disorders reflect a lack of clinical experience.
Genetic heterogeneity contributes further to the lack of firm
data to support current recommendations.
Because of the risks of bleeding, infections, and other
transfusion-related complications, elective surgery should be
avoided when possible. There is a body of literature demon-
strating the success of surgery in hemophiliacs and others
with inherited coagulation defects, but clearly, surgery in
such patients poses significant risks and increases the
demand for scarce resources, including blood products.
Current screening for infectious diseases and processing
of factor concentrates to eliminate many (but not all) infec-
tious agents has significantly decreased the risk of transmis-
sion of infectious diseases from plasma-derived products. All
patients with hemophilia and related coagulation disorders
should be vaccinated against hepatitis B. The development of
recombinant factors VIII and IX has contributed to a marked
decrease in virus-associated illnesses in these patients (no
documented cases of HIV and hepatitis B or C since 1985
and 1990, respectively), and human albumin–free products
have been developed to reduce further the possible transmission
of Creutzfeldt-Jakob disease. However, recombinant factors
are two to three times more expensive than plasma-derived
factors, are not always available owing to limited production
capacity, and may be associated with a higher rate of
inhibitor development compared with plasma concentrates.
Hemophilia patients who acquired HIV infection prior to
the widespread availability of screening and purified factors
have been treated successfully with antiretroviral therapy, but
there appears to be an increased risk of spontaneous bleed-
ing in these patients.
The development of inhibitors to factors continues to be
a problem for patients with severe hemophilia; recombinant
factors do not eliminate this risk (estimated at 10–15%).
Recombinant factor VIIa and activated prothrombin com-
plex concentrates (aPCCs) can be used to control hemor-
rhage by bypassing factors VIII and IX in patients with
inhibitors, but both may be associated with thromboem-
bolism. Porcine factor VIII is no longer used owing to con-
tamination with porcine parvovirus. Protein A sepharose
immunoadsorption may transiently lower factor VIII
inhibitors, allowing time for other immunosuppressive ther-
apies to work. Optimal management of inhibitors remains a
challenge in management of severe hemophilia.
Factor IX replacement (recombinant or purified plasma-
derived) can cause anaphylaxis in 5% of patients with severe
hemophilia B. Further replacement therapy in these patients
is risky. Recombinant factor VIIa is the only available thera-
peutic option for these patients.
Research in gene therapy is ongoing for patients with
severe hemophilia A and B. Results from preliminary trials
are promising, but this approach remains experimental.
Gene therapy may not prevent inhibitor development, how-
ever, and patients who are undergoing treatment for HIV
infection or who have hepatitis may not respond to this
approach.
Acquired Coagulation Disorders
ESSENTIALS OF DIAGNOSIS
Absence of a personal (if newly acquired) or family his-
tory of bleeding disorder.
Abnormal screening coagulation tests.
Clinical situation leading to decreased production or
increased destruction of coagulation factors or presence
of an anticoagulant.
General Considerations
Acquired coagulation disorders result from four basic mech-
anisms: vitamin K deficiency, liver disease, consumption of
factors, or inhibition of factor activity or fibrin polymeriza-
tion. Unlike inherited disorders, acquired coagulation disor-
ders are often characterized by multiple factor deficiencies as

CHAPTER 17
418
well as platelet defects (quantitative and qualitative). In addi-
tion, many of the clinical symptoms and signs result from the
underlying disease process; the coagulopathy is just one of
many processes contributing to the overall clinical picture.
A. Vitamin K Deficiency—Vitamin K is a cofactor necessary
for the synthesis of functional factors II (ie, prothrombin),
VII, IX, and X and proteins C and S. Vitamin K is found in
dietary sources (green vegetables) and is synthesized by bac-
teria in the intestinal lumen. It is fat-soluble, requiring bile
salts for absorption in the intestine. Vitamin K deficiency is
most likely to occur in patients who have disruption of both
dietary and bacterial sources of vitamin K (eg, patients who
are receiving broad-spectrum antibiotics who are not eating),
who have biliary obstruction or fat malabsorption, or who
are taking warfarin derivatives that inhibit metabolism of
vitamin K in the liver and induce a vitamin K–depleted state.
Vitamin K stores also may be depleted in patients with acute
or chronic liver disease. By unclear mechanisms, certain
antibiotics—particularly certain cephalosporins—and high
doses of aspirin are known to induce a deficiency of vitamin
K–dependent coagulation factors that is reversible with
administration of vitamin K. Cholestyramine, mineral oil,
and other cathartics may interfere with vitamin K absorption
when taken for a prolonged period. Normal newborns have
low levels of vitamin K–dependent factors that fall further
during the first few days of life. Deficiency of vitamin K
results in progressive depletion of all the vitamin K–dependent
factors as they are metabolized. Factor VII has the shortest
biologic half-life and is depleted first, followed by proteins
C and S and then factors IX, X, and II. Bleeding owing to vita-
min K deficiency is uncommon unless the deficiency is severe
(PT >25–30 seconds) or vascular injury is present.
B. Liver Disease—Coagulation disorders associated with
liver disease are complex. With the exception of vWF and
factor VIII, all the coagulation factors and other regulatory
proteins (eg, α
2
-antiplasmin, proteins C and S, and
antithrombin) are synthesized in hepatocytes. The liver is
also the site of clearance of activated coagulation factors and
degradation products of fibrin and fibrinogen and is respon-
sible for regeneration of vitamin K after it participates in
synthesis of the vitamin K–dependent coagulation factors.
Liver disease from any cause may result in multiple abnor-
malities, including decreased synthesis of all the coagulation
factors (with the exception of factor VIII), abnormal synthe-
sis of factors and proteins (eg, dysfibrinogenemia), abnormal
vitamin K metabolism resulting in functional vitamin K defi-
ciency, impaired fibrin polymerization owing to increased
fibrin degradation products, and accelerated fibrinolysis. In
addition, thrombocytopenia (owing to multiple mecha-
nisms, including inadequate synthesis of thrombopoietin in
the liver and hypersplenism, among others), defective
platelet function, or both may complicate severe liver disease.
Advanced cirrhosis is often associated with abnormalities of
blood vessels (eg, esophageal and gastric varices) and other
defects (eg, gastritis, ulcer disease, and esophageal tears),
which are the major sites of bleeding in patients with liver
disease. Hemostatic abnormalities exacerbate bleeding from
these sites and contribute to epistaxis, ecchymoses, and
increased bleeding with invasive procedures. In general, the
presence of a coagulopathy is a sign of advanced liver disease,
although passive congestion of the liver owing to right-sided
heart failure may be associated with coagulation distur-
bances without irreversible liver dysfunction.
C. Consumption of Coagulation Factors—Consumption
of coagulation factors may result from massive internal or
external blood loss or from DIC. Occasional patients who
have massive blood loss will develop a clinically significant
deficiency of multiple hemostatic factors, but DIC is the
most typical condition associated with consumption of coag-
ulation factors.
DIC occurs as a result of abnormal activation of coagula-
tion because of vascular injury, direct release of procoagulant
materials into the circulation, or both. There also may be
decreased quantity or function of naturally occurring antico-
agulants (ie, thrombomodulin–protein C pathway) in
patients with sepsis-associated DIC or in patients following
resuscitation for cardiac arrest. Consumption of coagulation
factors and platelets is accompanied by secondarily acceler-
ated fibrinolysis and results in a generalized bleeding ten-
dency associated with mucosal bleeding, ecchymoses, and
oozing from sites of vascular trauma, including venipuncture
and surgical sites. Fibrin deposition in the microcirculation
may contribute to some of the clinical sequelae of DIC, such
as tissue hypoxia. Rarely, purpura fulminans complicates
DIC. As a result of widespread arterial and venous thrombo-
sis, patients with purpura fulminans may have skin necrosis
and gangrene of the distal extremities and digits. The condi-
tions in which DIC occurs are complex (Table 17–5), with
multiple pathophysiologic mechanisms contributing to the
overall outcome of patients. DIC itself contributes to
multiple-organ-system failure and death in patients with
severe systemic disorders, particularly sepsis. Localized con-
sumption of coagulation factors and platelets owing to mas-
sive internal bleeding may mimic DIC but is not associated
with intravascular fibrin generation or generalized fibrinoly-
sis. In this situation, depletion of coagulation factors and
platelets may be accompanied by elevated circulating fibrin
degradation products and may result in a serious bleeding
tendency, but it is not associated with microvascular throm-
bus formation. Primary systemic fibrinolysis is extremely
rare and results in rapid destruction of fibrin clots, destruc-
tion of circulating fibrinogen, and consumption of plas-
minogen and its inactivators. Systemic fibrinolysis
accompanies DIC and may contribute significantly to clini-
cal bleeding. Primary fibrinolysis can be confused with DIC
but usually is not associated with thrombocytopenia and
generalized consumption of coagulation factors.
D. Inhibitors of Coagulation—Infrequently, inhibitors of
coagulation develop and may result in a serious bleeding
diathesis. Inhibitors directed against factor VIII are encountered
BLEEDING & HEMOSTASIS
419
most frequently as a complication of treatment for severe
hemophilia A and also may be associated with pregnancy,
collagen vascular diseases, malignancy, or certain drug reac-
tions. Inhibitors may occur as an isolated condition. The
abrupt development of factor V inhibitors following surgical
procedures has been reported and may cause unexpected
severe postoperative bleeding. These inhibitors appear to be
related to the use of topical bovine thrombin preparations con-
taining bovine factor V intraoperatively that may crossreact
with human factor V. Inhibitors to other coagulation factors,
including vWF and factor XIII, have been described. These
inhibitors are immunoglobulins with neutralizing activity
directed against specific factors and result in a clinical picture
consistent with a factor deficiency state. Other types of
inhibitors include substances that inhibit fibrin polymerization
without immunologic specificity for the fibrin molecule (eg,
fibrin degradation products or myeloma proteins). The lupus
anticoagulant typically prolongs the aPTT and therefore may
be confused with factor deficiencies or other inhibitors, but it is
not associated with bleeding. Heparin is a therapeutic inhibitor
of coagulation, accelerating the rate of antithrombin-mediated
inactivation of thrombin and other coagulation factors that act
as serine proteases (ie, factors VII, IX, and X).
Clinical Features
The clinical history, physical examination, and screening lab-
oratory abnormalities are usually sufficient to determine the
nature of the coagulation defect.
A. Symptoms and Signs—Patients with acquired coagula-
tion disorders occasionally may have spontaneous bleeding
but more commonly have excessive bleeding with surgical or
other invasive procedures or exacerbations of bleeding from
GI or other sites. Other clinical features reflect the underly-
ing disorder. Patients with liver disease may have bleeding
from esophageal varices as well as signs of hepatic dysfunc-
tion. In DIC, bleeding is a common finding, but ongoing
coagulation may be manifested as intravascular thrombosis
with skin necrosis and gangrene (ie, purpura fulminans).
Features of the disease causing DIC—particularly sepsis—
may predominate.
B. Laboratory Findings (See Table 17–6)—The PT and
the aPTT may be prolonged in all the acquired coagulation
defects as a result of multiple factor deficiencies. A 1:1 dilu-
tion test that fails to correct the abnormal PT or aPTT indi-
cates the presence of an inhibitor (including heparin and
lupus anticoagulants). Complete correction of the prolonged
PT and aPTT within 24 hours of administration of intra-
venous vitamin K confirms the presence of vitamin K defi-
ciency; vitamin K administration therefore is both diagnostic
and therapeutic. The diagnosis of DIC is based on the pres-
ence of prolonged PT and aPTT, thrombocytopenia, and ele-
vated fibrin degradation products or D-dimer in the
presence of an appropriate underlying condition.
Hypofibrinogenemia may be present in very severe cases,
but—because fibrinogen is an acute-phase reactant—fib-
rinogen levels are often normal. None of these tests is sensi-
tive or specific enough to determine conclusively whether
DIC is present. Circulating fibrin monomers (protamine sul-
fate test) and degradation products of cross-linked fibrin (D-
dimer test) confirm the presence of increased thrombin or
plasmin generation, and both are usually present in DIC;
they also may be positive occasionally in patients with liver
disease. Laboratory findings also vary as the condition of the
patient changes. Despite numerous attempts to standardize
the diagnostic criteria for DIC, DIC remains a clinical diag-
nosis, and assessment of the consequences of DIC is the
most critical aspect of management.
Coagulation defects owing to liver disease may be con-
fused with DIC because of the presence of accelerated fibri-
nolysis, decreased clearance of fibrin and fibrinogen
degradation products, thrombocytopenia, and prolongation
of both the PT and the aPTT. Therefore, differentiating DIC
from the coagulopathy of severe liver disease may be difficult,
and clinical experience is required to interpret the often
complex laboratory abnormalities. Schistocytes may be
found on peripheral blood smear; when present, DIC must
be distinguished from microangiopathic hemolytic anemia.
This disorder, which can be due to thrombotic thrombocy-
topenic purpura–hemolytic uremic syndrome, chemother-
apy, malignant hypertension, and the HELLP (hemolysis,
elevated liver enzymes, low platelets) syndrome, results from
endothelial injury with subsequent platelet activation,
thrombin generation, and fibrinolysis. Thrombocytopenia,
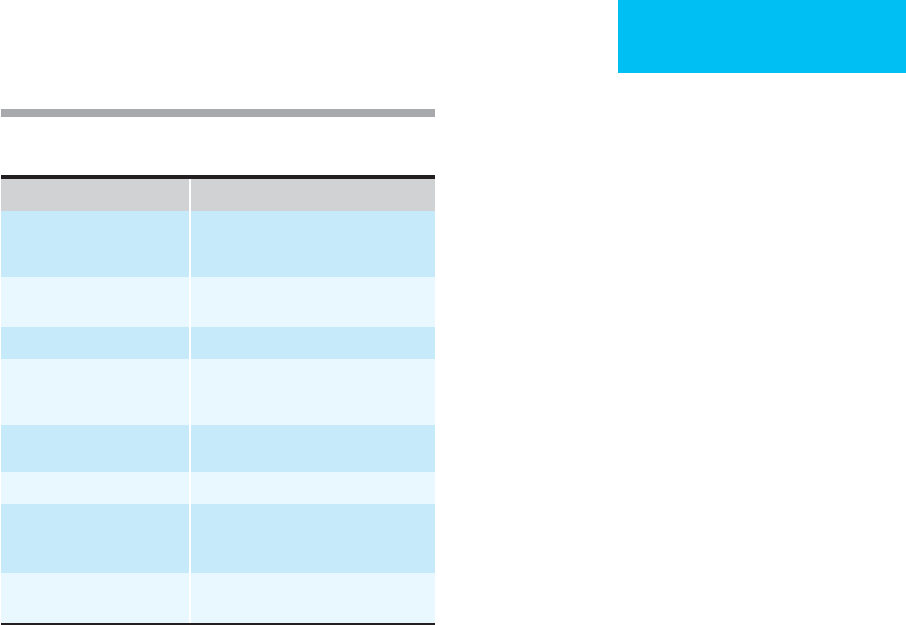
Cause Examples
Infections Bacterial sepsis (gram-negative and
gram-positive), viremia, rickettsiae,
malaria, tuberculosis
Trauma Massive tissue injury, head trauma, fat
embolism, burns
Malignancy Adenocarcinomas, acute leukemia
Obstetrical complications Abruptio placentae, amniotic fluid
embolism, retained dead fetus, septic
abortion, placenta previa, eclampsia
Vascular disorders and
prosthetic devices
Giant hemangioma (Kasabach-Merritt
syndrome), aortic aneurysm
Toxins Snake venoms, drugs
Immunologic disorders Severe allergic reaction, hemolytic
transfusion reaction, transplant
rejection
Metabolic disorders Hypotension, hypoxia, hyperthermia,
hypothermia, cardiac arrest
Table 17–5. Causes of disseminated intravascular
coagulation (DIC).
CHAPTER 17
420
hemolytic anemia, and fragmented red blood cells are the
hallmarks of microangiopathic hemolytic anemia, without
prolongation of coagulation times in most cases.
Differential Diagnosis
Inherited coagulation defects, thrombocytopenia, platelet
dysfunction, and accelerated fibrinolysis all may result in
bleeding at sites of vascular injury. Prolonged screening
coagulation tests may be abnormal owing to technical error
(including obtaining blood samples through heparinized
lines or inadequate quantity of blood in the tube) because of
inhibitors that do not cause bleeding (eg, lupus anticoagu-
lant) and deficiencies of factors that are not important for in
vivo hemostasis (eg, the contact factors, factor XII, high-
molecular-weight kininogen, and prekallikrein). Finally,
impaired surgical hemostasis, mucosal abnormalities, and
primary vascular abnormalities may result in clinical bleed-
ing regardless of coagulation status.
Treatment
Treatment of the underlying disease state, avoidance of inva-
sive procedures, and replacement of deficient factors during
acute bleeding episodes are the mainstays of treatment.
Vitamin K
1
(phytonadione), 1–10 mg orally or subcuta-
neously (not intramuscularly), should be administered to
patients at risk for vitamin K deficiency as both a diagnostic
and therapeutic strategy. The American College of Chest
Physicians recommends different dosing ranges of vitamin K
depending on the elevation of the PT and the bleeding status
or risk of the patient. Weekly administration (10 mg) reduces
the risk of vitamin K deficiency in patients who are poorly
nourished, receiving antibiotics, or who have malabsorption.
Intravenous vitamin K administration works more rapidly
but rarely may cause severe allergic reactions. Larger doses
may be required to reverse massive overdoses of warfarin.
Fresh-frozen plasma administration is necessary to correct
multiple factor deficiencies, but this treatment may be compli-
cated by the large volume required to achieve adequate hemo-
static levels, especially if factors are being consumed rapidly.
The quantity of fresh-frozen plasma administered must be
individualized, but in general, 30–40% of plasma volume (eg,
1000–1200 mL) is required to achieve adequate levels of all the
deficient factors; this amount must be readministered every
6–8 hours to maintain adequate levels of factor VII. Many
patients will not tolerate such a high volume of fresh-frozen
plasma replacement, so only partial correction may be possi-
ble—yet, if increased consumption of factors is present, even
more frequent administration may be needed.
A. Liver Disease—Management of liver disease complicated
by bleeding is difficult owing to the presence of multiple
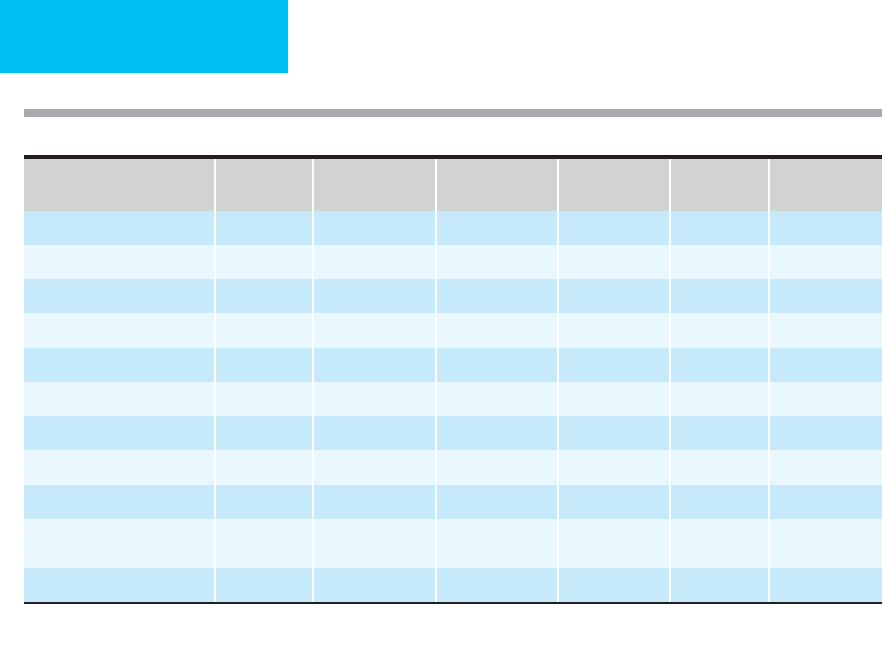
Laboratory Abnormality
Vitamin K
Deficiency
Liver Disease DIC
Specific Factor
Inhibitors
Lupus
Inhibitors
Primary
Fibrinolysis
PT prolonged + + + +
∗
(+)
aPTT prolonged + + + +
∗
+
1:1 dilution does not correct +
†
+
Thrombin time prolonged + + +
Thrombocytopenia + + (+)
FDP elevated + + + +
D-dimers present (+) +
Protein C/S decreased + + (+)
Antithrombin decreased + +
Red blood cells Targets,
macrocytes
Schistocytes,
microspherocytes
Hypofibrinogenemia (+) (+)
∗
Pattern of clotting time prolongation depends on specific factor to which inhibitor is directed.
†
May require incubation.
Key: + common; (+) occasional
Table 17–6. Laboratory diagnosis of acquired coagulopathies.

BLEEDING & HEMOSTASIS
421
pathologic processes. Factor replacement with fresh-frozen
plasma, platelet concentrates for thrombocytopenia, and cry-
oprecipitate for severe hypofibrinogenemia is a reasonable
intervention for serious bleeding but must be accompanied
by attempts to correct vascular and mucosal defects that
often are the main reasons for bleeding. The volume of fresh-
frozen plasma required to completely reverse prolonged clot-
ting times is substantial (>1000 mL), which limits its efficacy.
Prothrombin complex concentrate provides essential coagu-
lation factors in a much smaller volume, but because it is
associated with increased thromboembolic complications
and DIC (particularly with severe liver disease owing to
decreased clearance of activated clotting factors present in
the complex), it should be used only in life-threatening
bleeding. Vitamin K
1
administration (10–20 mg) may
improve the PT and aPTT in some patients and should be
tried. Desmopressin may shorten the bleeding time in some
patients with platelet dysfunction complicating cirrhosis, but
its efficacy has not been determined for control of bleeding
in liver disease. Treatment with desmopressin may exacer-
bate hyponatremia and hypotension and should be used with
caution. Antifibrinolytic agents have been advocated for
patients with evidence of accelerated fibrinolysis, but their
safety and efficacy in patients with advanced liver disease
have not been proved.
B. Disseminated Intravascular Coagulation—Patients
with DIC have diverse underlying conditions (see Table
17–5) and heterogeneous complications (both hemorrhagic
and thrombotic). Management should be directed primarily
at the underlying disorder. If serious bleeding is present, or if
an invasive procedure is required, factor replacement with
fresh frozen plasma to shorten the PT to within 2–3 seconds
of normal, cryoprecipitate to maintain fibrinogen levels
greater than 100 mg/dL, and platelet concentrates to raise the
platelets to greater than 50,000/μL should be attempted, but
these efforts may be compromised by short survival of the
hemostatic factors. Prophylactic administration of factors
and platelets in the absence of bleeding is not effective, and
coagulation factor concentrates should be avoided because
activated factors present in the concentrate may increase
intravascular coagulation.
Interruption of the primary pathologic coagulation of
DIC with heparin is controversial. DIC complicating acute
leukemia may be associated with marked bleeding owing to
impaired platelet production and may necessitate the use of
low-dose heparin (eg, 5–10 units/kg per hour) to achieve
adequate platelet counts with platelet concentrates, although
controlled studies have demonstrated that heparin adminis-
tration increases platelet transfusion requirements without
decreasing complications associated with DIC. Patients with
solid tumors and chronic DIC are more likely to experience
thrombotic complications than bleeding and may benefit
from long-term administration of heparin. Patients with
overt thromboembolism or purpura fulminans should be
treated with heparin, but because of an increased risk of
adrenal hemorrhage, the initial dose should be relatively low
and adjusted based on clinical response. Although secondary
fibrinolysis often contributes to the bleeding diathesis,
antifibrinolytic agents generally are contraindicated in the
presence of DIC because of the potential for unopposed
intravascular coagulation, which may result in significant
thrombotic complications. If marked symptomatic fibrinol-
ysis is present and there is no evidence of thrombotic com-
plications, however, antifibrinolytic therapy may be
attempted in combination with low-dose heparin to control
bleeding.
C. Circulating Inhibitors—Circulating inhibitors pose sub-
stantial difficulties in management of the bleeding patient.
As in patients with hemophilia A with factor VIII inhibitors,
strategies include high-dose factor replacement, decreasing
the titer of the inhibitor by immunosuppression or plasma-
pheresis, or using factors that bypass the need for the factor
being inhibited (eg, use of activated prothrombin complex
concentrates or recombinant factor VIIa). When high con-
centrations of fibrin and fibrinogen degradation products
are present, treatment of the underlying process (eg, sepsis-
induced DIC) is more useful than specific hemostatic ther-
apy. Myeloma proteins that inhibit fibrin polymerization
should be definitively treated with chemotherapy, but
plasmapheresis may be used as a temporizing measure.
Current Controversies and Unresolved Issues
Despite our understanding of the multiple processes that con-
tribute to bleeding in patients with liver disease, management
of bleeding has not been subject to careful clinical study to
determine optimal treatment strategies. Recombinant factor
VIIa (rFVIIa) has been shown to improve outcome from
acute variceal bleeding in a small preliminary trial, but its pre-
cise role in the management of bleeding in liver disease has
not been defined by clinical studies. The use of thrombopoi-
etin to improve thrombocytopenia is under investigation.
DIC is a syndrome that occurs in diverse clinical condi-
tions and is usually diagnosed on the basis of a combination
of laboratory abnormalities in the appropriate situation.
Several confirmatory laboratory tests have been proposed as
essential for the diagnosis, but the lack of a “gold standard”
combined with lack of standardization for the newer tests has
resulted in conflicting data on their usefulness. Management
of DIC is directed primarily against the underlying condi-
tion, but interventions to interrupt the state of pathologic
coagulation and fibrinolysis seem to be logical because these
processes may contribute significantly to the pathologic
state. Nevertheless, it has been difficult to demonstrate a clear
benefit of anticoagulation or antifibrinolytic therapy in any
situation complicated by DIC above and beyond that of
aggressive supportive care and treatment of the underlying
disease, with the possible exceptions of purpura fulminans
and thromboses associated with solid tumors. The use of
rFVIIa to treat bleeding associated with DIC may increase
CHAPTER 17
422
thrombotic sequelae and is not recommended by the manu-
facturer. However, control of refractory bleeding with rFVIIa
without thrombotic complications has been reported in sev-
eral patients with DIC. The use of activated protein C has
been shown to reduce hospital mortality in patients with
severe sepsis; however, this benefit was seen in patients both
with and without DIC. It is not known whether this benefit
is due to its anti-inflammatory properties, profibrinolytic
properties, or antithrombotic properties. Other strategies
aimed at interrupting important steps in the pathogenesis of
DIC such as the use of antithrombin concentrate and
inhibitors of the tissue factor pathway are under investiga-
tion for treatment of DIC. Antifibrinolytic therapy has
proven to be useful in the management of some of the inher-
ited coagulation disorders as an adjunct to factor replace-
ment. Because the acquired coagulation disorders are often
more complex, disruption of fibrinolysis has been attempted
infrequently. Potential complications of such therapy, such as
unmasking an underlying thrombotic diathesis, have limited
its role in the management of acquired coagulation disor-
ders. There is some evidence, however, that patients with
severe liver disease may have excessive fibrinolysis as a major
contributor to bleeding. Future studies to determine the effi-
cacy and safety of antifibrinolytic therapy are necessary
before it can be recommended.
Inherited Platelet Dysfunction
ESSENTIALS OF DIAGNOSIS
Lifelong history of easy bleeding.
Prolonged bleeding time out of proportion to platelet
count.
Normal platelet count or mild thrombocytopenia.
Normal coagulation times.
General Considerations
Platelets are involved in multiple aspects of normal hemosta-
sis. Defects in platelet membrane constituents, granules,
metabolism, or coagulant function give rise to defective
adhesion, aggregation, secretion, or procoagulant activity
(Table 17–7). These disorders are generally rare, usually fol-
low autosomal recessive inheritance patterns, and result in
varying degrees of bleeding associated with prolongation of
the bleeding time or defective or absent platelet aggregation
in response to platelet agonists. The most severe defects have
onset in the neonatal period or in early childhood with
ecchymoses, epistaxis, and other mucosal bleeding, but
milder defects may be manifest only after surgery or trauma.
Thrombocytopenia is present in some platelet disorders and
may contribute to the bleeding tendency. Other congenital
abnormalities (eg, albinism) also may be present.
Clinical Features
A clinical history of lifelong bleeding, accompanied by a pro-
longed bleeding time in the presence of normal platelet
count (or mild thrombocytopenia), PT, and aPTT, should
suggest the possibility of an inherited platelet disorder. A
peripheral smear made from fresh non-anticoagulated blood
may uncover morphologic platelet abnormalities or absence
of platelet aggregation. Platelet aggregation studies using a
wide variety of platelet agonists (including ristocetin) are
helpful for identifying the specific defect. Confirmation of
the specific diagnosis may require specialized studies avail-
able only in research laboratories.
Differential Diagnosis
A prolonged bleeding time in the absence of a history of clini-
cal bleeding is unreliable as an indicator of platelet dysfunction
or as a predictor of future bleeding. In the presence of bleeding,
a prolonged bleeding time may suggest the diagnosis of vWD
or an acquired disorder of platelet function (eg, uremia, drug
therapy, cardiopulmonary bypass, or myeloproliferative disor-
ders) rather than an inherited defect. Mucosal bleeding, ecchy-
moses, and posttraumatic bleeding may result from severe
coagulation disorders, accelerated fibrinolysis, thrombocytope-
nia, or vascular injury or from multiple hemostatic defects.
Adult onset of a severe bleeding tendency makes the diagnosis
of an inherited disorder of platelet function very unlikely.
Treatment
Serious bleeding usually requires transfusion of normal
platelets. Alloimmunization to HLA antigens and to platelet-
specific antigens may result in refractoriness to platelet trans-
fusions, so efforts to decrease alloimmunization are
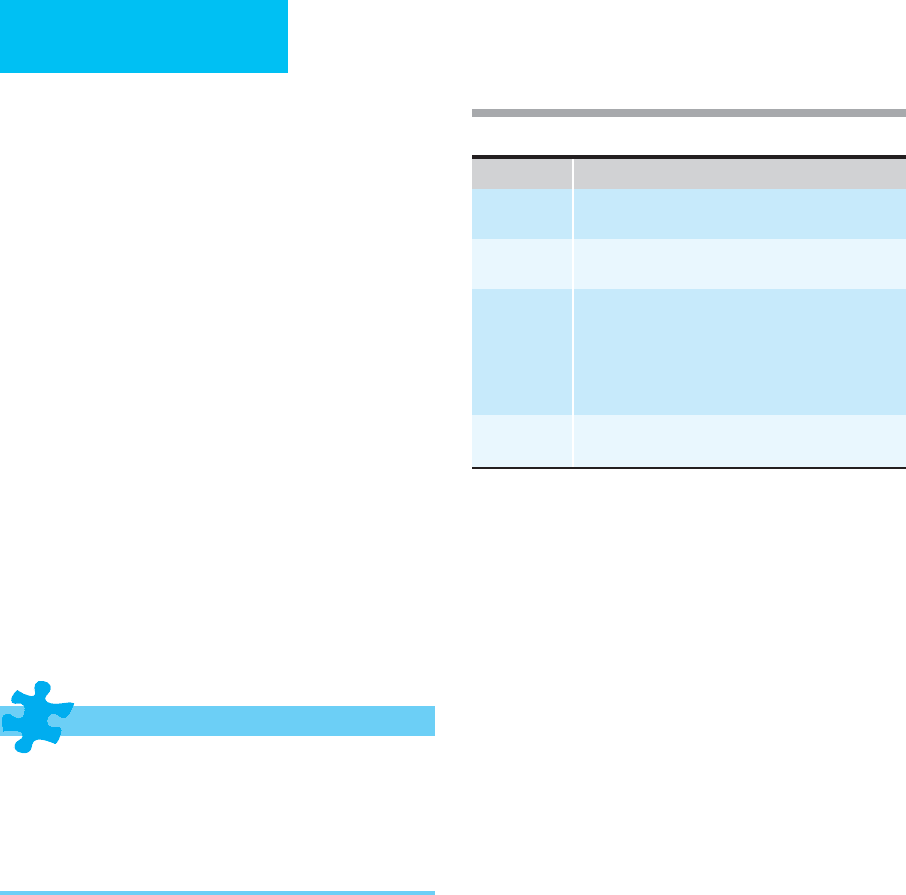
Function Disorder
Adhesion Bernard-Soulier syndrome (GP Ib deficiency)
von Willebrand disease.
Aggregation Glanzmann’s thrombasthenia (GP IIb/IIIa deficiency)
Afibrinogenemia
∗
Secretion/
signal
transduction
Gray platelet syndrome (alpha granule deficiency)
Storage pool deficiency (delta granule defects)
Arachidonic acid pathway abnormalities
Defective calcium mobilization
Wiskott-Aldrich syndrome (defective cytoskeletal
regulation)
Procoagulant
activity
Decreased platelet factor III activity
Scott syndrome (asymmetry of platelet phospholipids)
∗
Defect is extrinsic to platelet but affects platelet function, with
exception of platelet-type von Willebrand disease.
Table 17–7. Inherited disorders of platelet function.
BLEEDING & HEMOSTASIS
423
recommended (eg, limiting transfusions to life-threatening
situations, use of leukocyte-poor platelet preparations, or
administration of HLA-matched platelets). For unclear rea-
sons, some defects respond to therapy with desmopressin.
Antifibrinolytic agents (eg, aminocaproic acid or tranexamic
acid) may be useful for control of minor mucosal bleeding or
as adjuncts to platelet transfusions. Hormonal suppression of
menses is indicated for control of menorrhagia. Antiplatelet
agents are contraindicated, and surgical procedures should
be avoid whenever possible. Antifibrinolytic agents (eg,
epsilon-amino caproic acid and tranexamic acid) may be
helpful for controlling bleeding, as they do in inherited coag-
ulation disorders.
Current Controversies and Unresolved Issues
Optimal therapy of inherited platelet disorders is hampered
by the infectious risk of platelet concentrates and by the risk
of alloimmunization to HLA antigens and platelet-specific
antigens that renders further transfusions ineffective. The
risk of antibody formation is highest in patients with mem-
brane protein defects because of the presence of these pro-
teins on normal platelets. Bone marrow transplantation can
completely correct the bleeding tendency in patients with
inherited platelet disorders but remains experimental
because of potential lethal toxicity. Desmopressin releases
vWF and factor VIII from the endothelium, but it also may
shorten the bleeding time in some patients with a wide vari-
ety of platelet disorders independent of vWF and factor VIII
levels; its mechanism of action in these intrinsic platelet dis-
orders has not been established. Corticosteroid therapy prior
to surgery may improve hemostasis via an effect on vascular
integrity and may be indicated for control of bleeding in
patients with inherited platelet disorders who have no con-
traindications to steroid use.
Acquired Platelet Dysfunction
ESSENTIALS OF DIAGNOSIS
Mucosal bleeding, ecchymoses, or excessive surgical
bleeding in the absence of thrombocytopenia.
Abnormal bleeding time.
Normal coagulation times.
Clinical condition or medication associated with platelet
dysfunction.
General Considerations
Acquired platelet dysfunction may result from defects in
platelet adhesion, aggregation, secretion, or procoagulant
function. Drugs, liver or renal disease, cardiopulmonary
bypass, antiplatelet antibodies, acquired vWD, dysproteine-
mias, and myeloproliferative or lymphoproliferative disorders
(acute and chronic) may be associated with impairment of
platelet function, as measured by the bleeding time or by
abnormal tests of platelet aggregation. The clinical impor-
tance of the laboratory abnormalities in these diverse clinical
conditions is not always clear. Bleeding depends not only on
the severity of the defect but also on the presence of vascular
injury and other hemostatic defects. Typical manifestations
reflect impaired platelet function with mucocutaneous
bleeding and excessive posttraumatic bleeding. Petechiae are
rare unless thrombocytopenia is also present. Spontaneous
soft tissue hematomas and joint bleeding are rare.
Thromboxane A
2
is an important mediator of platelet
secretion and aggregation. Aspirin irreversibly acetylates and
inactivates cyclooxygenase, thus preventing the production of
prostaglandins, including thromboxane A
2
. Most individuals
who take aspirin will have a slight prolongation of baseline
bleeding time that may persist for several days, but marked
prolongation or clinical bleeding owing to platelet dysfunc-
tion is rare at doses used in most clinical situations, although
chronic use may be accompanied by easy bruising and
mucosal bleeding. Patients with other hemostatic defects,
however, may experience marked prolongation of bleeding
time and clinical bleeding if they take aspirin. Increased GI
tract bleeding is common in patients chronically taking high
doses of aspirin, but this is due to its irritant effect on the
mucosa rather than its effect on platelet function. The effect
of aspirin on bleeding following major surgery or invasive
procedures is controversial. While other nonsteroidal anti-
inflammatory agents reversibly inhibit cyclooxygenase, these
rarely prolong the bleeding time or induce clinical bleeding
even in patients with severe coagulation defects.
Dextran is used occasionally for its antiplatelet effect in
preventing postoperative deep vein thrombosis without
increasing postoperative blood loss. Ticlopidine and clopido-
grel are newer antiplatelet agents that inhibit ADP-induced
platelet aggregation and prolong the bleeding time, and these
occasionally may cause increased mucosal bleeding or bruis-
ing. Both agents appear to have irreversible effects on platelet
function, requiring 7 days for normal platelet function to
appear after withdrawal of the drugs (see Table 39–2).
Platelet glycoprotein IIb/IIIa inhibitors are used for treat-
ment of acute coronary ischemia, usually in combination
with anticoagulants or fibrinolytic agents, and work by pre-
venting fibrinogen-mediated platelet aggregation. β-lactam
antibiotics given at high doses for a prolonged period of time
may affect platelet function and can cause bleeding. However,
most patients with overt bleeding have multiple contributing
problems and can be managed without discontinuing the
antibiotic. Many other drugs have been linked to prolonga-
tion of the bleeding time but rarely result in clinical bleeding.
Renal failure is frequently associated with abnormal
platelet function, as measured by the bleeding time and by
platelet aggregation tests. Impaired platelet function appears
to result from biochemical alteration of intrinsically normal
platelets, although the precise mechanisms have not been

CHAPTER 17
424
elucidated. Severe anemia seen with renal failure can con-
tribute to prolongation of the bleeding time. Bleeding mani-
festations attributed to uremia include purpura, epistaxis,
and menorrhagia, but the risk of bleeding does not correlate
well with laboratory assessment of platelet function. With
adequate dialysis and generally improved care of uremic
patients in the past 25 years, bleeding may not be increased
significantly compared with those without renal failure.
Cardiopulmonary bypass induces both thrombocytope-
nia and transient platelet dysfunction. Platelet activation
while the platelets circulate through the bypass circuit results
in a state of functional “refractoriness” that usually reverses
within the first few postoperative hours. Multiple mecha-
nisms appear to be responsible for the observed changes
in platelet membranes, granule content, and functional
activity following bypass. Modest transient coagulation factor
deficiencies—owing mainly to hemodilution coupled with
heparin and protamine use—may result in prolongation of
coagulation times. Bleeding following cardiopulmonary
bypass therefore may result from multiple defects in hemo-
stasis, including inadequate surgical hemostasis.
Acquired hematologic disorders cause platelet dysfunc-
tion through production of intrinsically abnormal platelets
(eg, myeloproliferative disorders, myelodysplastic syn-
dromes, acute leukemias, or hairy cell leukemia), or through
production of abnormal substances that interfere with
platelet function (eg, immunoglobulins in myeloma or
Waldenström’s macroglobulinemia; rarely, immune-
mediated thrombocytopenia), or from abnormalities in vWF
(acquired vWD, seen in aortic stenosis, myeloproliferative
and lymphoproliferative disorders, collagen vascular dis-
eases, and angiodysplasia). Clinical bleeding is more often
the result of associated hemostatic defects or other hemato-
logic abnormalities, such as severe anemia, thrombocytope-
nia, marked leukocytosis, or hyperviscosity. Thrombotic
sequelae also may result from abnormal platelet function,
particularly in the myeloproliferative disorders.
Clinical Features
A. Symptoms and Signs—Mucosal bleeding, ecchymoses, or
excessive posttraumatic or surgical bleeding in the absence of
thrombocytopenia or abnormal coagulation times should sug-
gest the possibility of an acquired defect of platelet function.
B. Laboratory Findings—In most cases, the underlying
condition of the patient and medication use are obvious, and
minimal laboratory evaluation is needed to confirm the pres-
ence of platelet dysfunction. The bleeding time is a readily
available in vivo test of platelet function that will identify
most patients with significantly abnormal platelet function.
In vitro platelet aggregation studies require significant tech-
nical experience for reliable results and should be reserved
for patients with bleeding suggestive of platelet dysfunction
and an unexplained prolongation of the bleeding time—or a
very suggestive history of bleeding without prolongation of
the bleeding time. Bleeding time and platelet aggregation
studies are influenced by multiple factors, and while they are
useful for diagnosis in patients with significant bleeding, they
are not reliable indicators of the risk of future bleeding.
Differential Diagnosis
Inherited disorders of platelet function usually are readily dif-
ferentiated from acquired disorders by the presence of a long
history of bleeding and the absence of underlying conditions
associated with acquired platelet dysfunction. Mucosal bleed-
ing, ecchymoses, or excessive posttraumatic and surgical
bleeding may result from severe coagulation disorders,
thrombocytopenia, excessive fibrinolysis, vascular injury, or
multiple hemostatic defects. Prolongation of the bleeding
time may result from severe anemia, thrombocytopenia,
improper technique, or insignificant platelet dysfunction, and
in the absence of bleeding suggestive of platelet dysfunction,
it is not a reliable indicator of future risk of bleeding.
Treatment
Impaired platelet function in the absence of clinical bleeding
usually requires no specific therapy even when invasive pro-
cedures are performed. If bleeding is present, or if the nature
of an invasive procedure is such that any increased risk of
bleeding is unacceptable, a number of therapeutic options
are available depending on the underlying cause of the
platelet dysfunction. Withdrawal of aspirin or other suspect
drugs is usually adequate for management of drug-induced
platelet dysfunction. Desmopressin may be useful for man-
agement of bleeding in patients with a wide variety of disor-
ders of platelet function, including uremia, cardiopulmonary
bypass, and liver disease. Cryoprecipitate infusions and cor-
rection of severe anemia with red blood cell transfusions or
epoetin alfa (ie, erythropoietin), aggressive dialysis, and con-
jugated estrogens are other strategies for controlling bleeding
in uremic patients with platelet dysfunction. Aprotinin is a
plasmin inhibitor that reduces significant postoperative
bleeding following cardiopulmonary bypass and also may
decrease bleeding after liver transplantation.
Platelet transfusions are indicated in the treatment of
severe bleeding when platelet dysfunction is due to drugs,
cardiopulmonary bypass, or acquired intrinsic abnormalities
of platelets (eg, leukemias, myelodysplasias, and myeloprolif-
erative disorders) but are not helpful for management of
bleeding in uremia. Avoidance of aspirin and other
antiplatelet agents, correction of vascular defects, and treat-
ment of the underlying disease process are the most impor-
tant strategies for prevention and treatment of bleeding
associated with platelet dysfunction.
Current Controversies and Unresolved Issues
The bleeding time has enjoyed widespread use as a screening
test for patients requiring surgical procedures and as a diag-
nostic test in bleeding patients. The bleeding time may be
affected by technique, the site and depth of the incision, the

BLEEDING & HEMOSTASIS
425
presence of anemia, and characteristics of the supporting
connective tissues regardless of the functional status of the
platelets. A recent review of hundreds of studies of bleeding
time produced no convincing evidence that the bleeding
time is a useful predictor of bleeding in any clinical situation.
Its main value is in diagnosing conditions associated with
impaired platelet function, but even when platelet dysfunc-
tion is present, the bleeding time does not correlate well with
clinical bleeding.
Desmopressin acetate has proved to be useful in shorten-
ing the bleeding time in a wide variety of platelet disorders,
and it may decrease clinical bleeding as well. Conflicting
reports on its efficacy and a lack of understanding of its
mechanism of action in diverse diseases have limited its
widespread use. In addition, a few case reports have sug-
gested that desmopressin may contribute to thrombotic
complications, particularly in elderly patients with cardio-
vascular disease. Antifibrinolytic agents may prove to have a
role as adjuncts to other therapies for treatment of acquired
platelet disorders, but the potential for thrombotic complica-
tions must be appreciated when considering their use.
Thrombocytopenia
ESSENTIALS OF DIAGNOSIS
Mucocutaneous bleeding; petechiae in severe cases.
Decreased platelet count.
Absence of other hemostatic defects.
Associated condition leading to thrombocytopenia.
General Considerations
Thrombocytopenia may result from decreased production,
increased destruction or utilization, or sequestration of
platelets in the spleen (Table 17–8). Decreased production
usually affects all hematopoietic cells and rarely results in
isolated thrombocytopenia. Mechanical destruction of
platelets is often accompanied by evidence of hemolysis with
anemia, reticulocytosis, and red blood cell fragmentation on
peripheral blood smear, as well as clinical manifestations of
the underlying disease process. Immunologic destruction of
platelets may occur as an isolated problem (eg, autoimmune
thrombocytopenic purpura) or may result from drugs, trans-
fusions, or disease states associated with the production of
autoantibodies (eg, chronic lymphocytic leukemia, systemic
lupus erythematosus, or HIV infection). Splenomegaly from
any cause may result in thrombocytopenia and is often
accompanied by anemia and leukopenia.
Clinical Features
The history and physical examination with attention to
bleeding symptoms, medication usage, splenomegaly, and
symptoms and signs of underlying disorders often will reveal
clues to the diagnosis.
A. Symptoms and Signs—Mucocutaneous bleeding is the
most common bleeding manifestation of thrombocytopenia.
Petechiae usually occur only with severe thrombocytopenia
and may reflect the platelet’s essential role in the mainte-
nance of endothelial tight junctions. Spontaneous soft tissue
hematomas and hemarthroses are distinctly unusual. The
risk of serious bleeding depends on the cause and severity of
the thrombocytopenia, the presence of other hemostatic
defects or vascular injury, and the condition of the patient. In
general, patients with thrombocytopenia owing to consump-
tion, destruction, or splenic sequestration are at less risk for
serious bleeding than patients with decreased production of
platelets because decreased platelet survival results in pro-
duction of a younger, more functional population of
platelets. The most feared complication of severe thrombo-
cytopenia is CNS hemorrhage, which is rare unless the
platelet count is less than 10,000/μL and there are other pre-
disposing factors, such as leukemic infiltration, marked
leukocytosis, or other vascular injury. Bleeding manifesta-
tions associated with various degrees of thrombocytopenia
are shown in Table 17–9.
B. Laboratory Findings—Review of the complete blood
count and peripheral blood smear is essential to evaluate asso-
ciated abnormalities in other blood cell lines and to exclude
the possibility of pseudothrombocytopenia owing to in vitro
platelet clumping in the presence of EDTA anticoagulant.
Other instances of artifactual thrombocytopenia may be due
to platelet satellitism around neutrophils or may occur when
many giant platelets are present that may not be counted as
platelets by automated cell counters. Isolated thrombocytope-
nia is most often the result of immunologic destruction of
platelets but may be found in some patients with mild hyper-
splenism, acute alcohol intoxication, or early acute leukemia
and in the rare patient with isolated amegakaryocytic throm-
bocytopenia. The presence of fragmented red blood cells sug-
gests the possibility of intravascular mechanical trauma to
cells, as seen with DIC, thrombotic thrombocytopenic
purpura–hemolytic uremic syndrome, eclampsia (ie, HELLP
syndrome), or mechanical prosthetic heart valves. Abnormal
white blood cells may indicate the presence of leukemia or
lymphoma. The combination of nucleated red blood cells and
immature white blood cells in the peripheral smear, a leuko-
erythroblastic picture, suggests the possibility of bone marrow
infiltration from myelofibrosis or metastatic carcinoma.
Macrocytosis and pancytopenia should suggest the possibility
of vitamin B
12
or folate deficiency.
The PT and aPTT should be determined to detect condi-
tions such as DIC or thrombocytopenia associated with liver
failure. Bone marrow biopsy and aspiration are useful for
evaluation of platelet production and should be performed
when the diagnosis is not certain or if confirmation of a spe-
cific diagnosis (eg, leukemia, aplastic anemia, or metastatic
carcinoma) is essential to proper management.
CHAPTER 17
426
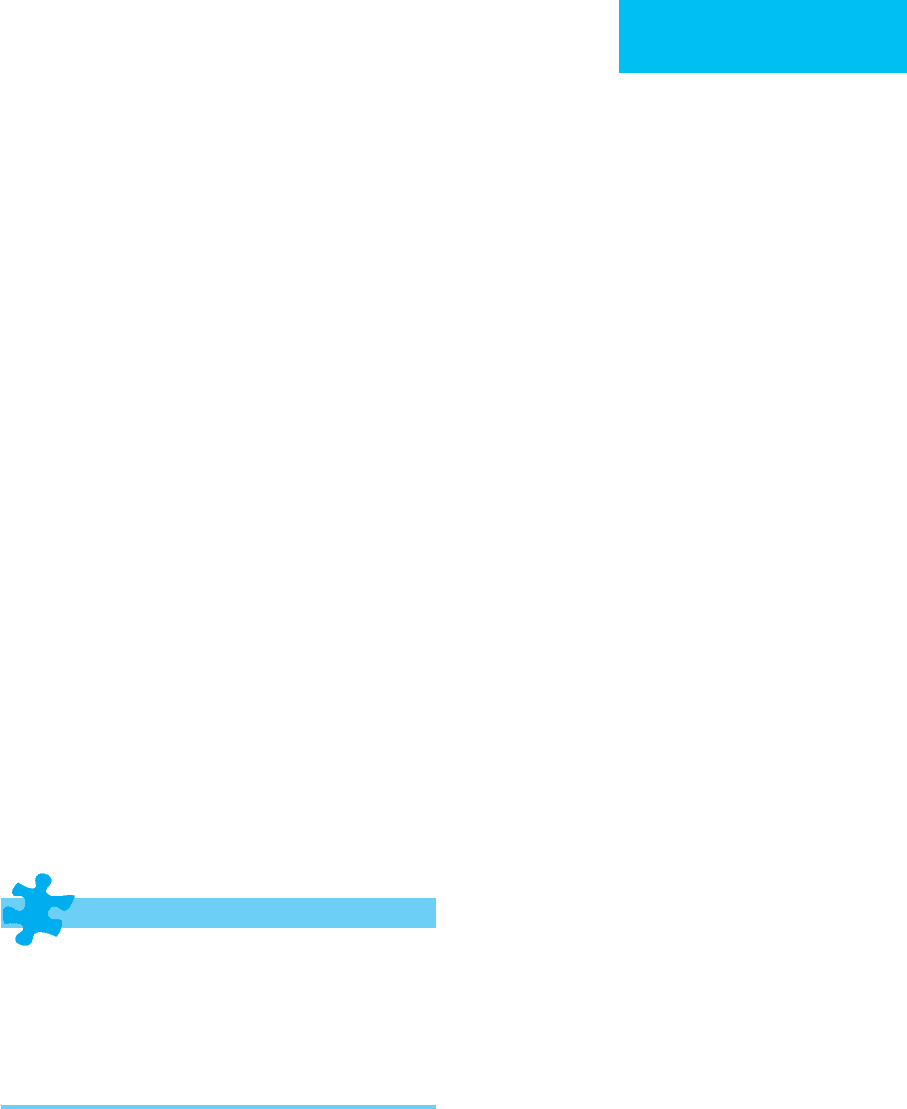
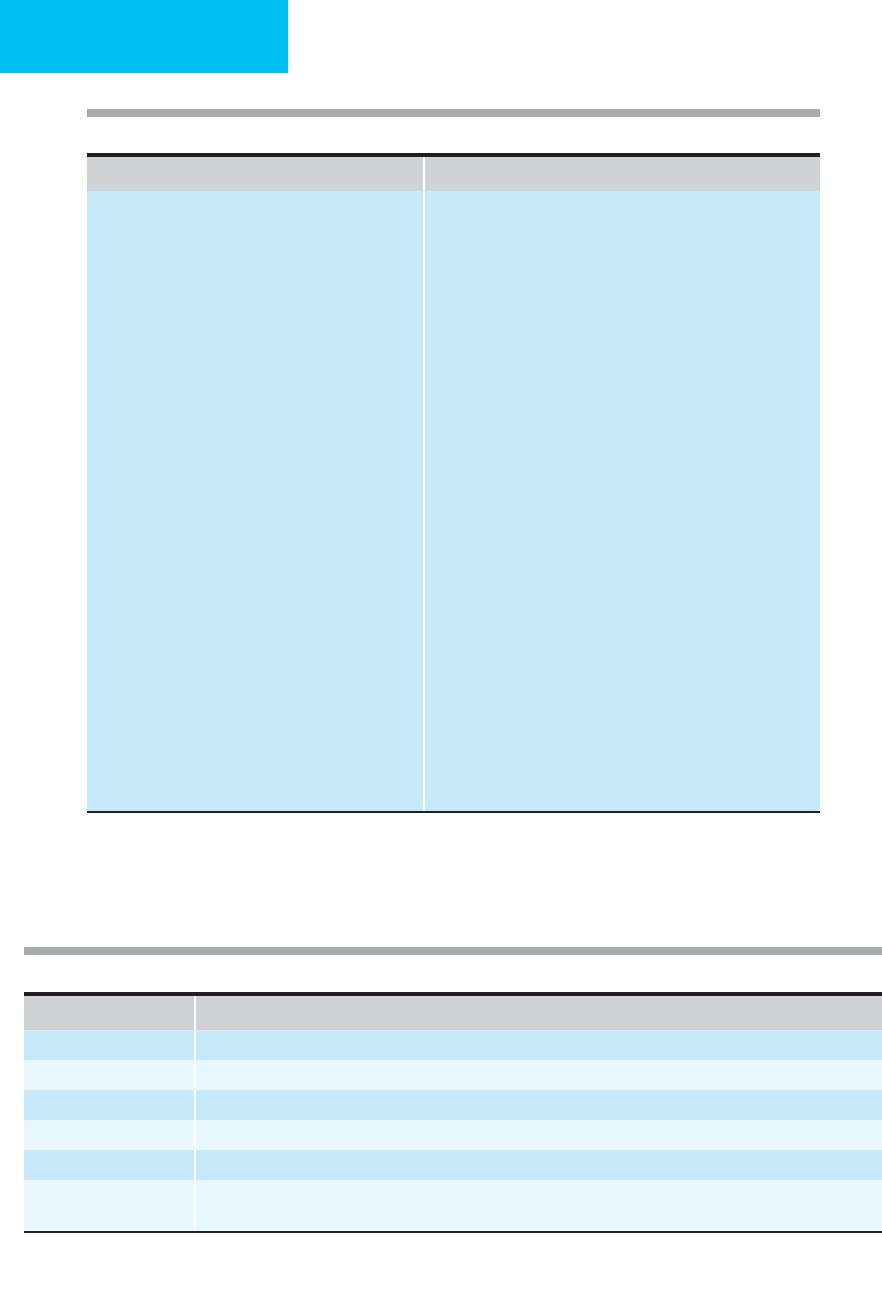
Decreased Production Increased Destruction or Utilization
Marrow infiltration or replacement
Leukemia, lymphoma, metastatic carcinoma
Aplastic anemia
Myelofibrosis
Granulomatous disease
Toxic or environmental exposures
Alcohol
Radiation
Chemotherapy
Chemicals
Thiazide diuretics
Ineffective hematopoiesis
Vitamin B
12
or folate deficiency
Myelodysplastic syndromes
Paroxysmal nocturnal hemoglobinuria
Infections
Viral: HIV, hepatitis, cytomegalovirus
Fungal: histoplasmosis
Acid fast organisms:
M tuberculosis,
M avium-intracellulare.
Bacterial sepsis
Acquired amegakaryocytic thrombocytopenia
Congenital thrombocytopenia
Thrombocytopenia–absent radius syndrome
Wiskott-Aldrich syndrome
May-Hegglin anomaly
Bernard-Soulier syndrome
Alport syndrome
Neonatal rubella or CMV infection
Maternal thiazide use
Mechanical
Abnormal heart valves
Vascular devices
Disseminated intravascular coagulation
Vasculitis
Cardiopulmonary bypass
Thrombotic thrombocytopenic purpura
Hemolytic uremic syndrome
Renal transplant rejection
Giant cavernous hemangioma (Kassabach-Merritt syndrome)
Fat embolism
Burns (>10% body surface)
Snake bite (crotalid)
Sequestration (hypersplenism, hypothermia)
Massive transfusion
Immunologic
Drug-induced antibodies or immune complexes
Systemic lupus erythematosus
Antiphospholipid antibody syndrome
Neoplastic diseases (chronic lymphocytic leukemia,
Hodgkin’s disease)
Posttransfusion purpura
Neonatal alloimmune thrombocytopenia
Viral-associated (HIV, infectious mononucleosis,
cytomegalovirus)
Pregnancy
HELLP syndrome (hemolysis, elevated liver enzymes,
low platelets associated with eclampsia)
Autoimmune thrombocytopenia
Probably immune
Malaria
Bacterial sepsis
Artifactual thrombocytopenias: Anticoagulant-dependent platelet clumping, pseudothrombocytopenia, platelet
satellitism, giant platelets.
Table 17–8. Causes of thrombocytopenia.
Platelet count (per μL) Clinical manifestations
>100,000 No increase in bleeding
50,000–100,000 Minimal bleeding even with surgery unless platelet dysfunction is present
30,000–50,000 Increased bleeding with surgery or trauma
∗
20,000–30,000 Occasionally associated with easy bruising or other minor spontaneous bleeding
∗
10,000–20,000 Epistaxis, petechiae, menorrhagia, gum bleeding
<10,000
Increased gastrointestinal blood loss, spontaneous life-threatening bleeding
†
(eg, intracranial hemorrhage, hematuria,
melena, hematemesis)
∗
Minimal in patients with immune thrombocytopenia or other consumptive disorders.
†
Life-threatening hemorrhage ususally occurs only with underlying vascular defect or if a second hemostatic defect is present
(including aspirin ingestion).
Table 17–9. Bleeding manifestations associated with thrombocytopenia.
