Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CARE OF THE ELDERLY PATIENT
447
failure in this population, intravenous fluid administration
must be individualized and approached cautiously.
As stated earlier, aging is associated with a change in body
composition with increase in fat content and a concurrent
decrease in muscle mass and total body water. Decrease in
muscle mass and a reduction in physical activity result in a
fall in total energy expenditure with increasing age. Energy
requirements may decrease by about a third between the ages
of 30 and 80 years. However, during periods of stress such as
trauma, surgery, or infection, daily energy requirements may
be more than doubled. In addition to the total energy intake,
attention should be paid to macronutrient and micronutri-
ent requirements.
The elderly are particularly vulnerable to malnutrition.
The reported incidence of malnutrition in elderly hospital-
ized patients varies from 17% to 65%. As the duration of
hospital stay increases, the likelihood of malnutrition rises.
In the elderly, a functional nutritional assessment should
include evaluation of sight, taste, smell, dentition, degree of
cognitive impairment, presence of depression, swallowing
abnormalities, respiratory dysfunction, hand-to-mouth coor-
dination, level of assistance required at meals, and perhaps
drug-appetite and drug-nutrient interactions.
Whenever possible, feeding should be started as soon as
possible in hospitalized or postoperative elderly patients. The
enteral route is greatly preferred, but parenteral nutritional
support can be used, if needed. Increased mortality occurs in
underweight people, but mortality is not clearly increased in
overweight elderly patients.
Special Considerations
The current disease-oriented model of acute medical care
promotes a sequential approach to diagnosis and treatment
that generally ignores the practice of restorative care until
after the patient is discharged from the hospital. In the frail
elderly, this approach may lead to a decline in functional
abilities despite effective treatment of acute medical illnesses.
The high rate of delirium and psychological decompensa-
tion in the acutely hospitalized elderly may lead to excessive
bed rest with accompanying loss of mobility, muscle atrophy,
contractures, pressure sores, greater tendency to fall, throm-
boembolism, incontinence, anorexia, constipation, and lack
of motivation. This has been called the “cascade of illness and
functional decline.”
Since the physiologic characteristics of the aging popula-
tion include both a decreased functional reserve and large
individual variation, medical management should be indi-
vidualized with the focus on maintenance of functional sta-
tus, protection from the hazards of immobility, and low risk
of complications from treatment.
Delirium
Approximately one-third to one-half of elderly patients will
have a delirious episode during the course of hospitalization
for medical or surgical care. It can be as high as 70% in ICUs.
Delirium is often unrecognized and is associated with pro-
longed hospitalization, greater need for nursing home place-
ment, and increased mortality. The presence of altered level
of consciousness, easy distractibility, rambling conversation,
illogical flow of ideas, unpredictable switching from subject
to subject, perceptual disturbances, and psychomotor agita-
tion or retardation should clue the clinician to the diagnosis
of delirium. Risk factors are listed in Table 19–3. Prior cog-
nitive impairment is the most frequent independent risk
factor for delirium. Other factors that predispose to the
development of delirium include unfamiliar surroundings,
social isolation, structural brain disease, concurrent chronic
illness, sleep deprivation, and alcohol or drug abuse. Delirium
could be the presenting symptom of a variety of illnesses
(Table 19–4). Early diagnosis is important because most
patients can recover if the underlying cause is recognized and
treated. The use of sedatives, psychotropic drugs, or physical
restraints to treat delirium could worsen the existing situa-
tion, placing the patient at higher risk for aspiration pneu-
monia, pressure ulcers, and other immobility-related
complications (cascade effect).
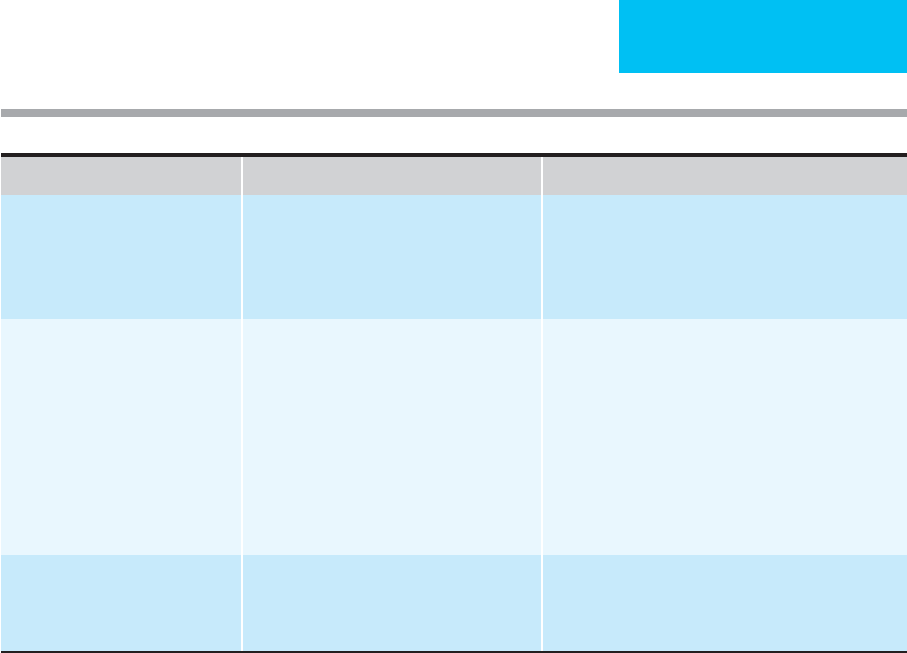
Prior cognitive impairment
Fracture on admission
Age over 80 years
Infection
Male sex
Impaired activities of daily living (ADLs)
Sensory impairment (blindness, deafness)
Polypharmacy (psychoactives, anticholinergics etc.)
Dehydration
Immobility
Bladder catheters
Table 19–3. Risk factors for delirium.
Decreased cardiac output Fecal impaction
Congestive heart failure Hypothermia and hyperthermia
Acute myocardial infarction Metabolic disorders
Acute blood loss Electrolyte abnormalities
Dehydration Acid-based disturbances
Infections Hypoxia
Fractures Hypercapnia
Stroke Hypoglycemia and hyperglycemia
Poorly controlled pain Azotemia
Drugs Transfer to unfamiliar surroundings
Urinary retention
Table 19–4. Common causes of delirium.

CHAPTER 19
448
The DSM-IV criteria for diagnosis of delirium include
the following: (1) disturbances of consciousness (ie, reduced
clarity of awareness of the environment) in conjunction with
reduced ability to focus, sustain, or shift attention, (2) a
change in cognition (such as memory deficit, disorientation,
or language disturbance) or the development of a perceptual
disturbance that is not better accounted for by a preexisting,
established, or evolving dementia, (3) development of the
disturbance during a brief period (usually hours to days) and
a tendency for fluctuation during the course of the day, and
(4) evidence from the history, physical examination, or labo-
ratory findings that the disturbance is caused by a general
medical condition. The Confusion Assessment Method is a
validated tool to assess delirium. With appropriate training,
it can achieve more than 95% sensitivity and specificity in
the diagnosis of delirium, even in groups with a high preva-
lence of dementia. In contrast with dementia, delirium gen-
erally has an abrupt onset, disturbance of consciousness,
fluctuations during the course of the day, and frequently, an
identifiable and potentially reversible cause.
The decreased attention span seen in delirium can be
assessed by several bedside tests. A simple test is the A test, in
which the interviewer vocalizes letters at a rate of one per
second, and the patient indicates by a sign every time the let-
ter A is mentioned. In the one-tap, two-taps test, the patient is
instructed to tap twice each time the interviewer taps once
and vice versa. More complex tests include spelling the word
world backward or subtracting 7 from 100 each time until 72
is reached (ie, 100, 93, 86, 79, 72). These tests are often abnor-
mal in patients with delirium.
Delirium is indicative of diffuse brain dysfunction and
has been associated with four classes of diseases: (1) primary
cerebral diseases, such as CNS infections, brain tumors, and
stroke, (2) systemic illnesses that secondarily affect brain
function, including cardiac disease, pulmonary failure,
hepatic dysfunction, uremia, deficiency states, anemia,
endocrine disturbances, systemic infections, and inflamma-
tory diseases, (3) intoxication with exogenous substances (eg,
alcohol, illicit drugs, prescribed medications, and industrial
toxins), and (4) withdrawal from dependency-producing
agents (eg, alcohol, barbiturates, and benzodiazepines).
The approach to patients with delirium includes a
focused history and physical examination, review of medica-
tions, and basic laboratory studies such as complete blood
count, serum electrolytes, serum urea nitrogen, glucose, and
urinalysis. Further specialized tests can be done in individual
patients. These include chest radiography, electrocardiogra-
phy, pulse oximetry, selected drug levels, selected cultures,
vitamin B
12
level, thyroid function tests, brain imaging, lum-
bar puncture, and electroencephalography.
Treatment of delirium should include identification and
treatment of the underlying cause and review of the medica-
tion regimen. Neuroleptics, opioids, or any medication with
high anticholinergic or sedative side effects should be discon-
tinued or reduced in dosage whenever possible. When avail-
able, constant observation is preferable to restraints. A
well-lighted and predictable environment, use of eyeglasses
and hearing aids, frequent reorientation by family and care-
givers, simple explanations of any procedure or confusing
stimuli, encouragement to stay awake during the daytime, and
nursing routines that permit uninterrupted nighttime sleep
are all valuable in the management of delirium. Finally, it may
be necessary to treat agitated behavior with medication.
Generally, the lowest effective doses of one of the atypical
antipsychotics (eg, risperidone or olanzapine) should be used
because of the low incidence of extrapyramidal side effects.
Complete resolution of symptoms can take days to months.
Communicating with the Elderly Patient
Many elderly patients have hearing and vision problems that
interfere with communication and cause difficulty in orien-
tation and adaptation to a new environment. Being able to
see and hear properly becomes critical when one must cope
with new experiences such as ventilatory support devices and
other invasive interventions.
Communication problems generate great anxiety in the
patient and frustration in the caregiver. There is a risk of mis-
labeling the patient as “confused” and disregarding the patient’s
role as a participant in health care decisions. The elderly patient
who reacts to an unfamiliar situation by becoming “agitated” is
at risk for the use of physical restraints or psychotropic medica-
tions. This causes worsening of the clinical status and may lead
to the cascade effect described earlier. The importance of efforts
to maximize communication with the elderly individual thus is
emphasized, especially in the ICU setting.
Adequate vision makes communication easier, especially
for those who have impaired hearing or comprehension. Eye
contact helps the caregiver to assess the extent to which the
older person hears and understands what is being said. If the
patient wears glasses, they should be clean and within reach
of the patient. The head of the bed should be elevated so that
the patient can see the speaker’s lips and eyes. A glare-free
light source coming from behind the patient helps the
patient to see the face and lips of the speaker. If the patient
has a hearing impairment, background noise should be
reduced by turning the television or radio off, by closing the
door, and by asking others in the area to be quiet. The
speaker should lean forward so that the lips can be seen, but
shouting should be avoided. Most elderly people suffer from
a selective high-frequency hearing loss with decreased ability
to identify high-frequency tones and pitches in the conso-
nants s, f, t, hard g, and j. Increasing the volume of sound is
of little help, and shouting may be misinterpreted as hostility
or anger. The manner of speaking should be natural and not
distorted by exaggerated lip movements. When it is necessary
to repeat a comment or question, it is better to rephrase than
to say the same thing in a louder voice. If the patient has a
hearing aid, it should be properly in place and in good work-
ing condition. Older people are often not aware of their hear-
ing inadequacies, and their perceptions of what they have
heard may not be accurate. Therefore, an attempt should be

CARE OF THE ELDERLY PATIENT
449
made to determine whether the patient has properly inter-
preted what has been communicated.
Health care personnel and family members should not
whisper or speak together in low tones near a hearing-
impaired older adult. A few words may be heard that will
result in misinterpretation, increasing the possibility of
unwarranted fears, paranoid behavior, or hostility. Glasses
and hearing aids should be worn consistently during the day.
If the patient is able to talk, dentures should be in place to
facilitate clear speech.
Immobility
Elderly patients are particularly vulnerable to the untoward
effects of immobility. Contractures, pressure ulcers, and
deconditioning can develop rapidly. Some of the other con-
sequences of immobility include muscle atrophy, deep
venous thrombosis, increased calcium mobilization from
bone, atelectasis, hypostatic pneumonia, constipation, func-
tional fecal and urinary incontinence, and loss of motivation.
Pressure ulcers are a common and frequent complication
of immobility. Any disease process leading to immobility
(eg, severe congestive heart failure, respiratory failure, delir-
ium, fractures, complicated postoperative course, or spinal
cord injury) places the elderly patient at high risk for devel-
opment of a pressure ulcer. Sites commonly involved are the
sacrum, ischial tuberosities, hip, heel, elbow, knee, ankle, and
occiput. More than 50% of pressure ulcers occur in persons
over age 70. Their prevalence among patients expected to be
confined to a bed or a chair for at least 1 week is as high as
28%. Pressure ulcers generally occur within the first 2 weeks
of hospitalization. Moreover, the development of pressure
sores has prognostic implications; the mortality rate among
those who develop pressure ulcers during the first 2 weeks has
been as high as 73%. Sepsis is the most serious complication
of pressure ulcers. Among bacteremic patients with a pres-
sure ulcer as the probable source of infection, the in-hospital
mortality rate can be as high as 60%.
Frequent repositioning (whether supine or in the sitting
position) has been the primary method of preventing pres-
sure ulcers. The evidence of structural changes in experimen-
tal animal models has led to the recommendation for
repositioning every 2 hours. Repositioning should be per-
formed so that a person at risk is positioned without pressure
on vulnerable bony prominences. This is accomplished in
practice by positioning patients horizontally with the
back resting partially over pillows that maintain the body at
a 30-degree angle to the support surface. Additional pillows
between the legs and supporting the arms will aid in main-
taining optimal positioning. A person with limited ability to
change position who must sit in a chair or have the head of
the bed elevated should not remain in this position for more
than 2 hours at a time. To diminish the shearing forces over
the sacral area, the head of the bed should not be elevated
more than 30 degrees. Particulate matter (eg, food crumbs)
should be removed from the bed. Sheets should be loose, and
tucking of the sheet at the foot of the bed should be avoided
so that movement is not restricted and the feet can assume
their natural position. Heels and elbows should be protected
by raising them with pillows to avoid direct pressure over
bony prominences. Patients should be lifted, not dragged.
The skin should be patted dry, not rubbed. Moisture control
depends on timely skin care. The evaluation and manage-
ment of urinary and fecal incontinence are of crucial impor-
tance in these patients.
In high-risk patients, pressure-relieving devices such as
constant low-pressure supports, alternating-pressure sup-
ports, or pressure-relieving cushions may be needed.
Attention also should be directed toward proper nutrition,
hydration, and pain control.
Educational programs aimed at physicians, nurses, and
other caregivers; family members; and the patients them-
selves have beneficial results. One study found that when
physicians ordered preventive measures for high-risk
patients, the incidence of pressure ulcers was half that for
patients for whom such orders were not written.
Bed rest also results in immobility and loss of weight-
bearing forces on joints. These effects cause changes in peri-
articular and articular structures that result in joint
contractures and changes similar to those of osteoarthritis.
Changes in periarticular tissues occur within days. Muscles
that bridge the immobilized joint shorten. These changes
produce decreased range of motion that can be permanent,
depending on the length of immobilization.
Bed rest is accompanied by progressive cardiovascular
deconditioning with exaggeration of the hemodynamic
changes normally seen with standing, as manifested by
orthostatic intolerance and decreased exercise tolerance.
Although orthostatic hypotension is not always documented,
signs and symptoms of orthostatic intolerance such as tachy-
cardia, nausea, diaphoresis, and syncope are common after
prolonged bed rest. A decrease in coordination, as measured
by pattern tracing and a marked increase in body sway in a
standing position, has been documented after several weeks
of bed rest.
The rate of decrease in muscular strength may be as high
as 5% per day and varies with the degree of immobility. Leg
muscles tend to lose strength about twice as fast as arm mus-
cles. For some elderly patients who normally use 100% of
their quadriceps muscle strength just to stand up, a loss of 5%
per day results in significant loss of function in a short time.
Given the numerous complications resulting from immo-
bility, early mobilization of the elderly patient in the ICU set-
ting should be a high priority. The rate of loss of muscle
strength will slow when active contraction of muscles is
encouraged, particularly if resistance is added. Simple
devices such as elastic fabrics (Theraband) make exercise
against resistance available for patients in beds or chairs.
Active movement in bed and full range-of-motion exercises
should be encouraged in alert patients. For other patients,
passive full range of motion should be done on every nurs-
ing shift.
CHAPTER 19
450
Intermittent sitting—and standing when possible—will
reduce the frequency of orthostatic hypotension. The sitting
position also improves oxygenation and diminishes cardiac
work because cardiac output and stroke volume decrease in the
sitting position. Finally, rehabilitation service consultation may
be useful in the management of elderly patients in the ICU.
REFERENCES
Aalami OO et al: Physiological features of aging persons. Arch Surg
2003;138:1068–76. [PMID: 14557122]
Bressler R, Bahl JJ: Principles of drug therapy for the elderly patient.
Mayo Clin Proc 2003;78:1564–77. [PMID: 14661688]
Ely EW et al: Delirium as a predictor of mortality in mechanically
ventilated patients in the intensive care unit. JAMA 2004;291:
1753–62. [PMID: 15082703]
Fick DM et al: Updating the Beers criteria for potentially inappropri-
ate medication use in older adults. Arch Intern Med 2003;163:
2716–24. [PMID: 14662625]
Inouye SK et al: The role of adherence on the effectiveness of non-
pharmacologic interventions: Evidence from the Delirium
Prevention Trial. Arch Intern Med 2003;163:958–64. [PMID:
12719206]
Luckey AE, Parsa CJ: Fluid and electrolytes in the aged. Arch Surg
2003;138:1055–60. [PMID: 14557120]
Lyder CH: Pressure ulcer prevention and management. JAMA 2003;
289:223–6. [PMID: 12517234]
Marik PE: Management of the critically ill geriatric patient. Crit Care
Med 2006;34:S176–82. [PMID: 16917421]
McNicoll L et al: Detection of delirium in the intensive care unit:
Comparison of confusion assessment method for the intensive
care unit with confusion assessment method ratings. J Am Geriatr
Soc 2005;53:495–500. [PMID: 15743296]
Mick DJ, Ackerman MH: Critical care nursing for older adults:
Pathophysiological and functional considerations. Nurs Clin
North Am 2004;39:473–93. [PMID: 15331298]
Rellos K et al: Outcome of critically ill oldest-old patients (aged 90
and older) admitted to the intensive care unit. J Am Geriatr Soc
2006;54:110–4. [PMID: 16420206]
Rosenthal RA, Kavic SM: Assessment and management of the geri-
atric patient. Crit Care Med 2004;32:S92–105. [PMID: 15064668]
Sevransky JE, Haponik EF: Respiratory failure in elderly patients.
Clin Geriatr Med 2003;19:205–24. [PMID: 12735123]
Suttner SW, Piper SN, Boldt J: The heart in the elderly critically ill
patient. Curr Opin Crit Care 2002;8:389–94.

451
0020
Critical Care of the
Oncology Patient
∗
Darrell W. Harrington, MD
Darryl Y. Sue, MD
Several complications of cancer may require critical care for
palliative management. These include (1) acute CNS disor-
ders (eg, spinal cord compression and increased intracranial
pressure), (2) severe metabolic disorders (eg, hypercalcemia,
hypocalcemia, tumor lysis syndrome, hyponatremia, hyper-
glycemia, hypoglycemia, and hypokalemia with ectopic
adrenocorticotropic hormone [ACTH] production),
(3) orthopedic disorders (eg, pathologic fracture), (4) uro-
logic disorders (eg, hematuria, hemorrhagic cystitis, and
acute obstructive uropathy), (5) general surgical disorders
(eg, GI bleeding, bowel perforation, bowel obstruction,
extrahepatic biliary obstruction, and intraabdominal abscess
formation), (6) malignant effusions (eg, pericardial effusion
with cardiac tamponade and pleural effusion with lung
compression), (7) complications of chemo- and radiother-
apy, and rarely, (8) superior vena cava syndrome. CNS disor-
ders, metabolic disorders, and superior vena cava syndrome
are addressed in this chapter.
CENTRAL NERVOUS SYSTEM DISORDERS
Spinal Cord Compression
ESSENTIALS OF DIAGNOSIS
Axial (back) pain that may radiate to arms or legs or
bandlike discomfort around the chest.
History of malignancy (may be initial presentation of
cancer).
Neurologic deficits (ie, motor, sensory, or autonomic).
Abnormal images of spine: MRI (preferred), plain x-rays,
CT scan, CT or planar myelography.
General Considerations
Spinal cord compression from epidural metastases is a
potentially devastating complication in cancer patients. It
occurs in about 5% of cancer deaths and therefore will
develop in about 25,000 of the annual 500,000 cancer deaths.
The most common primary tumors that cause spinal cord
compression are cancers of the lung, breast, and prostate;
lymphomas; and multiple myeloma. Cord compression also
can be seen in patients with leukemia (chloroma) and a wide
range of other solid tumors. It may present as the first and
only manifestation of cancer, but it is postulated that pro-
longed survival from initial diagnosis of cancer will increase
the incidence of spinal cord compression.
Epidural spinal cord compression develops via two mecha-
nisms: (1) by metastatic spread to the vertebral bodies, from
where the tumor expands and erodes into the epidural space,
and (2) by cancerous involvement of the paravertebral region
with extension into the epidural space through the interverte-
bral foramina. Bone scans and spine x-rays may be normal in
the latter cases but usually are abnormal in the former. Vertebral
body metastases account for epidural spinal cord compression
in approximately 85% of patients with solid tumors and 25% of
patients with lymphomas. In the 70% of cancer patients with
metastases at death, metastases to the spine are found in 40%.
Epidural metastases extend from the paravertebral region in the
remainder. In addition to spinal cord compression, sudden irre-
versible spinal dysfunction may occur from vascular compro-
mise, resulting in spinal cord infarction.
The thoracic spine occupies 47% of the total length of the
spine but is the affected area in approximately 70% of
patients, the lumbar spine occupies 30% and is affected in
20%, and the cervical region occupies 22% and is affected in
10% of patients. Spinal cord involvement may occur at mul-
tiple levels in 10–38% of patients. The greater chance of tho-
racic spine involvement may be related to the presence of
physiologic kyphosis and the narrower spinal canal in this
region. Metastases never traverse the intervertebral disks and
rarely traverse the dura.
∗
Darrell W. Harrington, MD, and Hassan J. Tabbarah, MD, were the
authors of this chapter in the second edition.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.

CHAPTER 20
452
Clinical Features
A. Symptoms and Signs—The clinical presentation of
epidural spinal cord compression is well known and depends
on the level of spinal involvement. Axial pain is the most
common presenting symptom (prodromal phase), occurring
in 95% of adults and 80% of children with epidural spinal
cord compression. Therefore, spinal cord compression
should be considered in any patient with cancer and axial
pain. The local pain corresponds to the site of the lesions and
is described as dull and aching. Tenderness over the affected
spinal element is usually readily elicited. Approximately 15%
of patients will develop paraplegia despite a long duration of
painful symptoms (compressive phase), because spinal cord
compression was not anticipated. Pain may persist for several
weeks or months before symptoms of radiculopathy are
manifested. Cervical or lumbar disease usually but not
always presents as unilateral radiculopathy, whereas thoracic
disease produces bilateral symptoms resulting in a bandlike
distribution of pain. Radicular pain may be accompanied by
sensory or motor loss, as determined by the involved nerve
root, and may be easily confused with disk herniation. Pain is
usually worse at night and is aggravated by movement,
coughing, or the Valsalva maneuver. Because midthoracic
back pain is less likely to be due to benign causes, any patient
localizing pain and tenderness to this area regardless of a his-
tory of malignancy should be evaluated carefully.
Neurologic deficits seen in spinal cord compression usu-
ally begin with motor impairment. These are seen more com-
monly in the distal part of the body or the lower extremities
owing to the greater frequency of thoracic and lumbar spine
involvement. Anterior spinal cord compression is more com-
mon than posterior involvement. Accordingly, patients usu-
ally have more motor than sensory disability, at least in the
early stages. Sensory impairment follows, parallels the devel-
opment of motor deficit, and is present in half of patients at
the time of diagnosis of spinal cord compression. Autonomic
dysfunction occurs later and is present in half of cases.
The neurologic deficit is caused either by mechanical
compression by the tumor on the spinal cord or cauda
equina or by destruction of a vertebral body sufficient to
make it collapse and compress the spinal cord. Once spinal
cord compression occurs, progression may be very rapid.
Therefore, the presence of myelopathy is a neurologic emer-
gency. Disease presentation and progression depend on the
level of spinal involvement. For example, high cervical cord
lesions (C3–5) may be life-threatening because both quadri-
plegia and respiratory muscle impairment are common fea-
tures. Involvement of the thoracic cord typically is
characterized by identification of a sensory level on the
trunk. In addition, lower extremity weakness and autonomic
dysfunction may accompany thoracic cord compression. The
specific site of lumbosacral spinal cord compression is less
easily determined by physical examination. Patients may
present with radiculopathy and loss of associated reflexes or
with isolated autonomic dysfunction as seen in the conus
syndrome. It is important that each patient have a complete
neurologic examination, paying close attention to subtle
asymmetries in muscle strength and reflexes. It is important
to note that patellar and ankle reflexes provide information
only about L4 and S1 nerve roots, respectively. Therefore,
normal reflexes of the lower extremity should not be used to
exclude the presence of significant myelopathy.
B. Laboratory Findings—A histologic diagnosis of malig-
nancy is rarely necessary in a patient with a known preexist-
ing malignancy. However, it is prudent to specifically identify
malignancy causing spinal cord compression in an individual
without an underlying history of cancer. This is so because
localized infection causing spinal cord compression may
mimic malignancy. In the presence of complete blockage of
the spinal canal and to avoid worsening of neurologic status,
only a few drops of cerebrospinal fluid (CSF) should be
removed and sent for cytologic examination and protein
determination. Additional studies are sent to exclude infec-
tion. Lumbar puncture otherwise should be reserved for
patients suspected of concomitant leptomeningeal dissemi-
nation of tumor. CSF may have elevated protein, normal or
low glucose, and a lymphocytic pleocytosis.
C. Imaging Studies—MRI is the diagnostic study of choice
to evaluate spinal cord compression, but plain x-rays of the
involved area and planar or CT myelography are potentially
useful or necessary (especially if MRI is unavailable or cannot
be performed). It is critical that imaging should be acquired
as early as possible and should not be delayed more than a few
hours in patients with neurologic symptoms and signs.
The most important attribute of MRI is its ability to eval-
uate directly the full length of the cord, thus making it possi-
ble for multiple levels of compression to be identified and to
determine whether these lesions are related or unrelated to
bony erosion or bone destruction by tumor. At least 35% of
patients who present with focal symptoms have evidence of
subclinical epidural compression at other sites along the
spine. MRI also can determine the number of segments and
vertebrae involved, the location of a compressive mass, if
present (anterior, posterior, or encircling), and perhaps the
percentage loss of bone mass. Imaging of the entire spine is
usually not done because of the length of time needed (as
much as 3 hours), but not taking the time may miss lesions
that cause later neurologic compromise. MRI is comparable
to myelography and CT scanning with contrast material in
detecting leptomeningeal metastasis. However, MRI may be
inadequate in patients who may have had previous spinal
surgery because metal-induced artifacts may be seen or the
patient’s movements cannot be controlled.
Vertebral metastases can be seen on unenhanced T
1
-
weighted images as foci of low signal intensity (dark) that
contrast with the adjacent high signal intensity (bright) of
normal adult bone marrow. The administration of gadolin-
ium results in normalization of the tumor, making its appear-
ance similar to that of the marrow. Vertebral metastases rarely
cross the disk space, as often seen in infection. However, it

CRITICAL CARE OF THE ONCOLOGY PATIENT
453
sometimes may be difficult to distinguish between malig-
nancy and infection with MRI. Diffuse bone marrow
involvement may make interpretation by MRI difficult. This
is also true in younger patients with relatively little fatty mar-
row. MRI is superior to CT scanning with and without
intrathecal contrast material (CT myelogram).
Plain x-rays may be helpful in localizing the anatomic
origin of compression symptoms. Hematologic malignancies
less often are manifested by abnormal plain spine x-rays than
solid tumors. The most common findings include loss of
pedicles, destruction of the vertebral body, and vertebral
body collapse. Plain x-rays will, however, be unsuccessful in
identifying up to 20% of vertebral body lesions and also will
fail to demonstrate paravertebral masses that spare vertebral
body destruction but encroach on the epidural space via the
intervertebral foramina. The overall diagnostic sensitivity of
plain spine films is about 83%.
CT scans can assess the extent of a paravertebral mass,
detect small areas of bone destruction, quantify the extent
and characterize the direction of spinal cord impingement,
and assess response to treatment. CT scans cannot investigate
multiple levels of involvement without extensive scanning
and may miss the area of maximal impingement if CT scan
“cuts” are too widely spaced.
CT myelography remains an important diagnostic
method for epidural spinal cord compression, especially
when MRI is unavailable. Water-soluble contrast media are
preferred. Once a complete block of the spinal canal is
demonstrated by a lumbar myelogram, a C1–2 or suboccipi-
tal myelogram should be done to define the upper level of
block. Myelography may disclose silent epidural metastasis.
Lumbar myelography may cause further deterioration of neu-
rologic findings in approximately 14% of patients even with
the removal of only a small amount of CSF. Myelography has
been associated with complications such as headaches, seizures,
allergic reactions, and deterioration of neurologic status.
The role of radionuclide bone scans is unclear in the set-
ting of suspected epidural spinal cord compression. Bone
scans are less accurate than plain spine x-rays in predicting
epidural involvement. Moreover, bone scans often will suggest
multiple areas of abnormality without identifying the level
associated with pain or neurologic deficit. Bone scans may
not reflect the extent of vertebral involvement. These studies
are reserved for patients with skeletal pain, negative plain x-
rays, and a low suspicion for spinal cord compression.
Differential Diagnosis
The differential diagnosis of spinal cord compression includes
intervertebral disk herniation, vascular disease (eg, hemor-
rhage or infarction), infectious processes such as epidural
abscess, benign neoplasms (eg, meningioma, neurilemoma,
and chordoma), neurologic disorders (eg, multiple sclerosis
and amyotrophic lateral sclerosis), transverse myelitis, lep-
tomeningeal carcinomatosis, and paraneoplastic syndromes
(eg, necrotizing myelopathy and carcinomatous neuropathy).
Treatment
Early recognition, diagnosis, and treatment of epidural
spinal cord compression are of utmost importance. Either
the presence of neurologic symptoms or radiographic evi-
dence of epidural compression is sufficient to justify begin-
ning treatment. Cord compression diagnosed after the onset
of myelopathy has the most profound impact on the patient’s
quality of life. The drastic difference is between 2 and 6
months of ambulatory survival versus 2–6 months of bed or
wheelchair confinement with a urinary catheter, potential
urosepsis, pneumonia, and decubiti—and dependence on
professional care or family members. In one study, 70% of
patients with malignant spinal cord compression had pro-
gression of symptoms from initial symptoms and onset of
treatment. Reasons for delay included lack of recognition by
the patient but also delays in diagnostic evaluation.
Although median survival after treatment for spinal cord
compression is short, two factors appear to predict a good
prognosis for recovery of function: a normal pretreatment
neurologic examination and urgent appropriate treatment.
Other prognostic factors include the rate and onset of pro-
gression of neurologic dysfunction, histologic features of the
primary tumor (eg, myeloma, lymphoma, breast, and
prostate have a better prognosis), the presence of vertebral
collapse, and the location of the compressing lesion (anterior
or posterior). In general, if patients are ambulatory before
the start of treatment, two-thirds will remain ambulatory
after treatment. If patients are paraparetic before treatment,
one-third will be ambulatory after treatment, but if patients
are paraplegic (especially if unresponsive to dexamethasone
therapy), only a few—if any—will become ambulatory after
treatment. The most commonly used treatment regimen
consists of high-dose corticosteroid therapy plus external-
beam radiation. Surgery is used selectively either as initial
treatment or when specifically indicated.
A. Corticosteroids—To reduce edema of the cord adjacent
to the tumor, corticosteroids are used frequently in the treat-
ment of spinal cord compression. These should be started as
soon as the diagnosis is suspected. Delaying therapy while
awaiting formal studies is unnecessary and may lead to fur-
ther progression of the neurologic deficit. These drugs clearly
improve the initial rate of neurologic recovery and often lead
to stabilization of the neurologic deficit. Randomized trials
support the benefit of corticosteroids in those treated subse-
quently with radiotherapy. The optimal dose of corticos-
teroids is not known, but almost all recommendations
support “high doses” in the range of 16–100 mg dexametha-
sone. Some studies have shown both a higher likelihood of
benefit from the highest dosages and more complications of
therapy. One recommendation is to vary the dose with the
degree of neurologic impairment. With pain or radiculopa-
thy alone, dexamethasone, 16 mg intravenously, followed by
4–6 mg intravenously or orally every 6 hours, is adequate.
Patients with rapidly progressive symptoms or significant
CHAPTER 20
454
myelopathy should be treated with dexamethasone, 100 mg
intravenously, followed by 24 mg intravenously every 6 hours.
Therapy should be continued until benefit is demon-
strated from definitive therapy (ie, radiation or surgery)
or neurologic deficits are considered irreversible. Tapering of
corticosteroids is accomplished by reducing the dose by
about one-third every 3–4 days over a period of 2–3 weeks.
Corticosteroids should be reinstituted if neurologic deficits
recur. Patients failing to improve after a 7-day trial at 100
mg/day should be rapidly tapered to the lowest dose that will
maintain stable neurologic function. Such steroid regimens
do not appear to be toxic, although vaginal burning may
occur with rapid intravenous administration of dexametha-
sone. Conversely, corticosteroids may result in serious and
fatal complications when used in high doses for more than 40
days or when given to patients with serum albumin concen-
tration of less than 2.5 g/dL.
B. Radiation Therapy—Radiation therapy alone produces
neurologic improvement in 30–50% of patients with epidural
spinal cord compression. Pain relief is obtained in the major-
ity of patients with radiation therapy. Radiation-sensitive
tumors such as hematologic malignancies and seminomas
have the best outcome, breast and prostate cancer have mod-
erately good outcomes, and lung and renal cancer, sarcomas,
and melanoma are radioresistant and have the worst out-
comes. Radiation therapy and surgical therapy appear to be of
equal effectiveness in the treatment of radiosensitive tumors.
The usual dose of radiation is 3000–4000 cGy over a period of
3–4 weeks. There are few differences reported between vari-
ous radiotherapy protocols (ie, dose, number of fractions, and
total duration). Complications of radiation therapy include
radiation myelopathy and impaired wound healing in
patients who undergo subsequent surgery.
C. Surgery—The surgical approach selected—laminectomy,
anterior surgical decompression, or posterolateral surgical
decompression—depends on several variables, including the
specific element of vertebral involvement, cord level, and sta-
bility of the spine. The concept that surgery is not indicated
in the treatment of spinal cord compression is based on ret-
rospective analysis of several surgical series that compared
decompressive laminectomy followed by radiation therapy
with radiation therapy alone. No difference in neurologic
outcome was reported initially. Better understanding of the
pathogenesis of cord compression combined with advances
in operative technique and materials have resulted in
improved outcomes after surgical decompression. For exam-
ple, in 54 patients with cord compression in whom laminec-
tomy or vertebral body resection was performed, all 54
improved, and 23 of 25 patients surviving for 2 years
remained ambulatory. The 30-day mortality rate in this
series was 6%, and the morbidity rate was 15%.
Surgery is a major procedure associated with a significant
rate of complications. Therefore, surgery should be used only
in patients who have less extensive disease and longer life
expectancy. In the absence of medical contraindication,
surgery may be considered (1) when the diagnosis is not
known or is in doubt, (2) when there is spinal instability or
bone deformity, (3) when there is failure to respond to radi-
ation therapy, (4) when there is a history of previous radia-
tion therapy up to cord tolerance, (5) when there is high
cervical spinal cord compression (because of the danger of
respiratory failure), (6) in the presence of a radioresistant
tumor, especially when the onset of signs is rapid and com-
plete block is present, (7) when atlantoaxial compression is
present, (8) when a solitary spinal cord metastasis is present,
and (9) as a form of primary treatment before radiation ther-
apy. When possible, it is recommended that adjuvant
chemotherapy be delayed for 3–6 weeks after surgical ther-
apy to minimize wound complications.
Table 20–1 offers an approach to the patient with known
or suspected malignancy that presents with back pain and
possible spinal cord compression.
Conway R, Graham J, Kidd J, Levack P. Scottish Cord Compression
Group: What happens to people after malignant cord compres-
sion? Survival, function, quality of life, emotional well-being
and place of care 1 month after diagnosis. Clin Oncol (R Coll
Radiol) 2007;19:56–62. [PMID: 17305255]
Graham PH et al: A pilot randomised comparison of dexam-
ethasone 96 mg vs 16 mg per day for malignant spinal-cord
compression treated by radiotherapy: TROG 01.05 Superdex
study. Clin Oncol (R Coll Radiol) 2006;18:70–6. [PMID:
16477923]
Husband DJ, Grant KA, Romaniuk CS: MRI in the diagnosis and
treatment of suspected malignant spinal cord compression. Br J
Radiol 2001;74:15–23. [PMID: 11227772]
Loblaw DA et al: Systematic review of the diagnosis and manage-
ment of malignant extradural spinal cord compression: The
Cancer Care Ontario Practice Guidelines Initiative’s Neuro-
Oncology Disease Site Group. J Clin Oncol 2005;23:2028–37.
[PMID: 15774794]
Patchell RA et al: Direct decompressive surgical resection in the
treatment of spinal cord compression caused by metastatic can-
cer: A randomised trial. Lancet 2005;366:643–8. [PMID:
16112300]
Prasad D, Schiff D: Malignant spinal-cord compression. Lancet
Oncol 2005;6:15–24. [PMID: 15629272]
Increased Intracranial Pressure Due
to Malignancy
ESSENTIALS OF DIAGNOSIS
Mental deterioration, lethargy, somnolence, or confusion.
Changes in heart rate and blood pressure.
Pupillary changes.
Neurologic deficits, focal or nonfocal.
Abnormal brain CT or MRI diagnostic or suspicious of
intracranial tumor or metastases.
CRITICAL CARE OF THE ONCOLOGY PATIENT
455
General Considerations
Increased intracranial pressure (ICP) can cause neurologic
damage either directly or indirectly by way of herniation of
the cerebellar tonsil or uncus or by secondary vascular com-
promise. It is essential that prompt management be insti-
tuted in order to prevent loss of cerebral function or death.
The closed cranium means that any increase in volume of
any intracranial component must result in increased pres-
sure. A tumor increases ICP by adding its bulk or localized
edema to the normal components of brain tissue, CSF, and
vessels within the cranium.
Increased ICP can result from primary or metastatic
tumors. At least one-fourth of patients dying from malig-
nancy will have brain metastases discovered at autopsy.
Hematogenous spread is the most common route of dissem-
ination. Thus most lesions (approximately 80%) are supra-
tentorial. The most common cancers found include lung,
renal, breast, and melanoma. Brain metastases from chorio-
carcinoma, melanoma, and breast cancer more often
undergo hemorrhagic transformation. The metastatic
tumors may be single or multiple and should be distin-
guished from diffuse infiltrative processes that also may
cause increased ICP. Leukemic meningitis and diffuse
leukemic infiltration also can cause increased ICP but with-
out the focal neurologic or radiographic findings usually
seen in primary or metastatic brain tumors. In diffuse
processes, ICP increases without evidence of other concomi-
tant findings (eg, localizing findings from a mass lesion).
Brain edema results from leakage of plasma into the
parenchyma through dysfunctional capillaries (ie, vasogenic
edema). Studies on the formation, speed, and resolution of
brain edema have concluded that increased capillary perme-
ability occurs within the brain tumor itself and not in the
surrounding brain tissue. This increased capillary permeabil-
ity varies depending on the histology of the tumor and its
size. Brain edema occurs preferentially in the cerebral white
matter. Vascular endothelial growth factors may contribute
to dysfunction of tight junctions. It is not clear how brain
edema results in neurologic dysfunction, but it is thought to
be related to ischemia from a mass effect or from metabolic
abnormalities in the surrounding extravascular fluid.
Untreated, metastatic brain tumors ultimately lead to
progressive neurologic dysfunction and death. The median
survival in this setting is 4–6 weeks.
Clinical Features
A. Symptoms and Signs—Headache, nausea, vomiting,
mental deterioration, lethargy, somnolence, and confusion
are key findings in patients with increased ICP. Flexor or
extensor posturing may occur. In addition, decrease in
Other Clinical Findings Diagnostic Studies Treatment
Normal neurologic examination
Normal plain spine x-rays
MRI for high-risk tumors or in the presence
of other metastatic disease. If MRI is not
available, then CT, CT with myelography, or
myelography.
Observe closely for low-risk primary tumors.
Treatment depends on MRI or CT findings.
Normal neurologic examination
Abnormal plain spine films
None.
MRI, or CT with myelography.
Radiation therapy to symptomatic vertebral metastases
without further imaging. Advantages: No delay in treat-
ment, no further expense. Disadvantages: May miss
other sites of disease that may become symptomatic
later and compromise further radiotherapy because of
overlapping radiation therapy ports. Disadvantages
reduced if x-ray of entire spine is obtained, radiation
port includes two segments above and below lesions, or
bone scan is performed to document that disease is lim-
ited to one area of the spine.
Treatment depends on MRI or CT findings.
Abnormal neurologic examination
Abnormal or normal plain spine x-rays
MRI of symptomatic area to identify adjacent
levels of involvement.
If MRI is unavailable, consider CT with
myelography.
Treatment (radiation therapy) depends on MRI or CT
findings. Consider selective surgery.
Table 20–1. Management of patients with back pain and suspected malignancy.

CHAPTER 20
456
heart rate, increase in blood pressure, and abnormal respira-
tory pattern (Cushing’s triad) often can be present but are
late findings. Cerebellar masses may, however, have a
reversed clinical picture. Dilation of one or both pupils sug-
gests rapid and significant increases in ICP. Focal neurologic
deficits and abnormal reflexes may be found. Early diagnosis
is usually based on the timely observation of subtle alter-
ations in the mental status or state of consciousness of the
patient.
B. Laboratory Findings—Lumbar puncture for diagnosis is
to be discouraged because removal of fluid from the
intrathecal sac may result in an acute drop in infratentorial
pressure, thereby precipitating or worsening herniation.
C. Imaging Studies—Head CT scan and MRI are the most
useful diagnostic tests. The size and location of a tumor mass
or masses, the amount of peritumoral edema, shifts in
intracranial structures, and ventricular size can be deter-
mined easily. No test is completely accurate in predicting risk
of herniation. MRI is more sensitive than CT scan for find-
ing tumor, especially when evaluating lesions of the posterior
fossa. However, CT scan may better detect bony involvement
of the skull. Both non-contrast- and contrast-enhanced CT
scans are recommended because the combination not only
may detect hemorrhagic lesions (non-contrast-enhanced)
but also may allow detection of small lesions (contrast-
enhanced).
Differential Diagnosis
The differential diagnosis of increased ICP includes metabolic
encephalopathy (eg, hypo- and hypernatremia, hypercal-
cemia, uremia, hypoxemia, hypoglycemia, and thyroid dys-
function), CNS infection, cerebrovascular disease (especially
intracranial hemorrhage), drug-induced encephalopathy (eg,
sedatives and analgesics), and nutritional deficiencies.
Treatment
A. Medical Treatment—If signs of cerebral herniation are
evident, emergent reduction of ICP is warranted. Emergent
maneuvers include elective intubation and hyperventilation
to maintain Pa
CO
2
between 25 and 30 mm Hg, followed by
administration of mannitol, 1–1.5 g/kg intravenously every
6 hours. Some recommend following serum osmolality as a
guide to dosing mannitol. Use of mannitol should be avoided
when definitive therapy (surgery or radiation) is delayed. In
any case, hypotonic fluids may be harmful and should not be
given. Early corticosteroid (eg, dexamethasone) administra-
tion and fluid restriction appear to be the best means of
achieving a decrease in ICP and brain edema. The specific
mechanism of action of corticosteroids on brain edema is
not known. These agents may either decrease edema produc-
tion or increase edema resorption. Corticosteroids appear to
decrease tumor capillary permeability and alter the exchange
of sodium and water across the endothelial cells and decrease
CSF production at the choroid plexus. Corticosteroid
administration may result in symptomatic improvement
within 4–5 hours, but more commonly such improvement
occurs gradually over several days, with 70% of patients
showing late significant clinical improvement. Dexamethasone
is administered at a dosage of 16 mg/day in four divided
doses, and the dosage may be increased to 100 mg/day. Some
patients must remain on corticosteroids for long periods and
whenever they undergo definitive treatment such as sur-
gery or radiation. Patients are subject to the risks and side
effects of high-dose corticosteroids if administered for long
enough time.
Preemptive antiseizure medications are frequently
administered, but their value is controversial. Because
patients with malignancy have a high risk for venous throm-
boembolism, deep venous thrombosis prophylaxis is recom-
mended despite the theoretical risk of hemorrhage from
primary or metastatic brain tumor.
B. Surgical and Radiation Treatment—Surgery and radi-
ation therapy are important methods of treatment of pri-
mary and metastatic brain tumors either as initial or as
adjunctive therapy. Candidates for surgical resection should
be patients with solitary lesions and limited systemic disease.
Radiation therapy usually involves the whole brain and
requires an average of 3000 cGy. Most recently, radiosurgery
has evolved as a new technique to deliver a single large dose
of radiation to a specific target. Local control rates appear to
be equal to those achieved with surgery. Radiosurgery is
especially useful in patients with multiple or poorly accessi-
ble lesions.
Aoyama H et al: Stereotactic radiosurgery plus whole-brain radia-
tion therapy vs stereotactic radiosurgery alone for treatment of
brain metastases: A randomized, controlled trial. JAMA
2006;295:2483–91. [PMID: 16757720]
Chang JE, Robins HI, Mehta MP: Therapeutic advances in the
treatment of brain metastases. Clin Adv Hematol Oncol
2007;5:54–64. [PMID: 17339829]
Kaal EC, Niel CG, Vecht CJ: Therapeutic management of brain
metastasis. Lancet Neurol 2005;4:289–98. [PMID: 15847842]
Khuntia D et al: Whole-brain radiotherapy in the management of
brain metastasis. J Clin Oncol 2006;24:1295–304. [PMID:
16525185]
Klos KJ, O’Neill BP: Brain metastases. Neurologist 2004;10:31–46.
[PMID: 14720313]
Langer CJ, Mehta MP: Current management of brain metastases,
with a focus on systemic options. J Clin Oncol 2005;23:6207–19.
[PMID: 16135488]
Mehta MP, Khuntia D: Current strategies in whole-brain radiation
therapy for brain metastases. Neurosurgery 2005;57:S33–44;
discusssion S1–4. [PMID: 16237287]
Peacock KH, Lesser GJ: Current therapeutic approaches in patients
with brain metastases. Curr Treat Options Oncol 2006;7:
479–89. [PMID: 17032560]
Tsao MN et al: Whole brain radiotherapy for the treatment of mul-
tiple brain metastases. Cochrane Database Syst Rev
2006;3:CD003869. [PMID: 16856022]
