Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

CARDIAC PROBLEMS IN CRITICAL CARE
477
chronic congestive heart failure and wasting. Diagnosis and
identification of the organism are essential for proper man-
agement. Clinical features of endocarditis, including fever,
heart murmur, unexplained anemia, and peripheral or
immunologic stigmata, should alert the physician. In partic-
ular, endocarditis needs to be considered in any febrile
patient with a known history of valvular heart disease, a
pathologic murmur, or a prosthetic valve. Patients with
community-acquired Staphylococcus aureus or Streptococcus
viridans bacteremia have a high incidence of endocarditis
(20% and 80%, respectively) and should be considered to
have endocarditis until proven otherwise.
The diagnosis of endocarditis is made on clinical grounds
(see Chapter 15). Positive blood cultures are found in as
many as 90% of patients, but the frequency of this finding
depends on the type of organism and the number of blood
cultures obtained. Therefore, one should obtain an adequate
number of samples of blood for culture before starting
antibiotic therapy or specify laboratory techniques to mini-
mize the effect of antibiotics on the culture results.
Obtaining cultures for fungi, anaerobic bacteria, and fastidi-
ous or slow-growing organisms may increase the likelihood
of an etiologic diagnosis in susceptible patients.
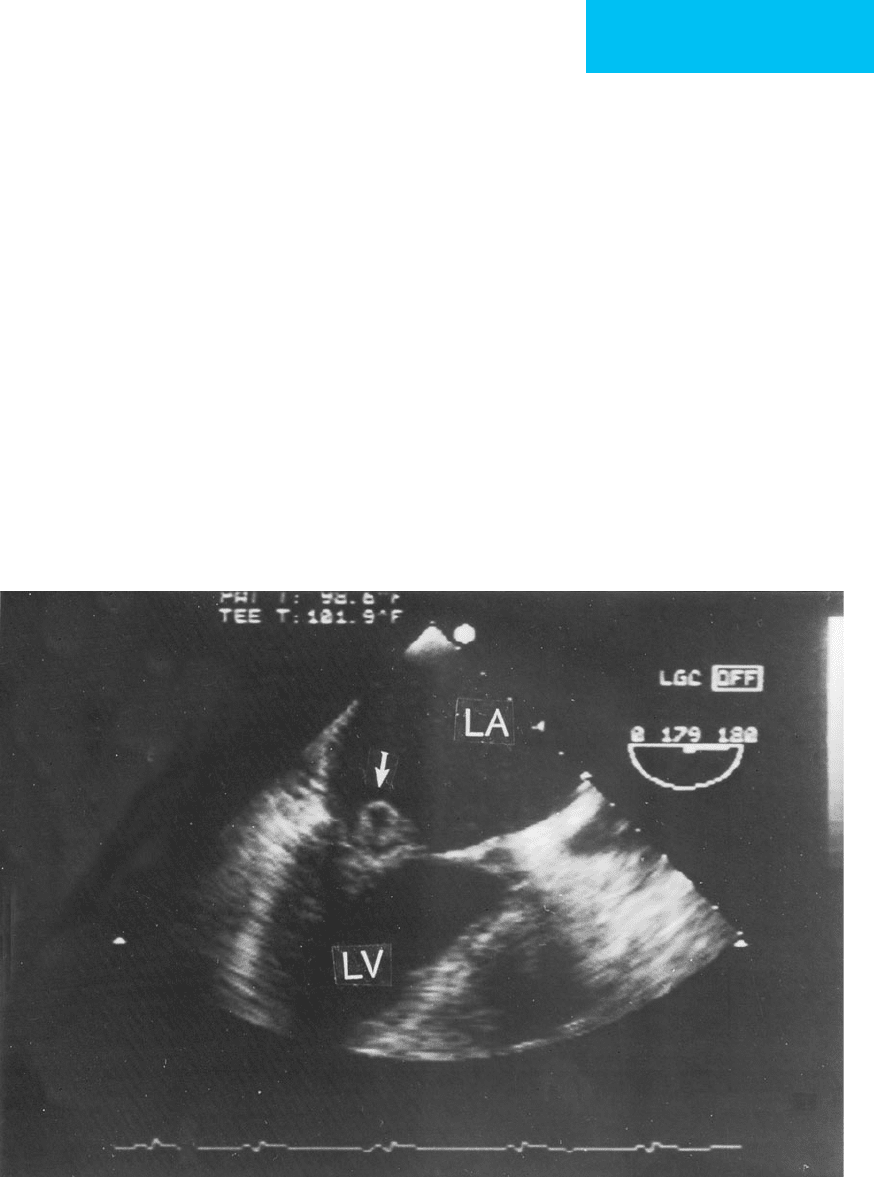
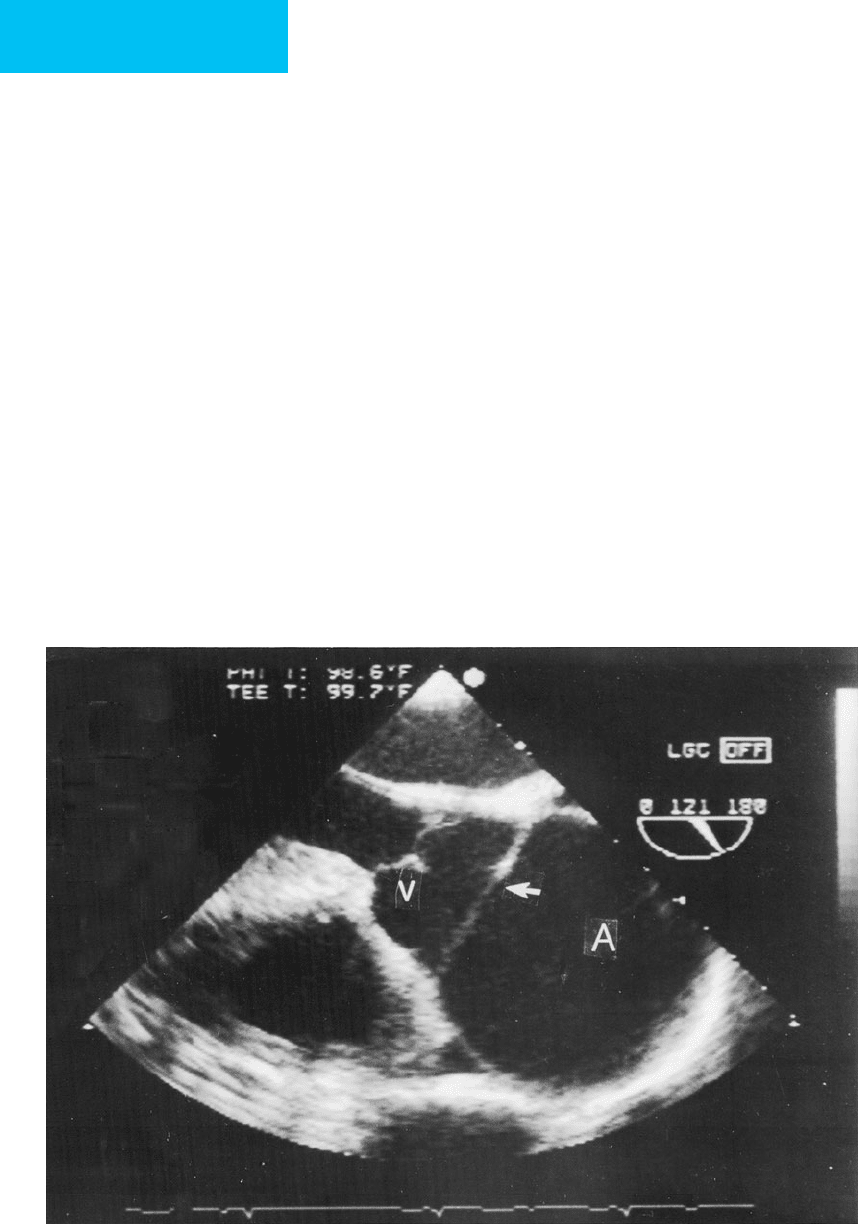
Echocardiography, especially using the transesophageal
approach, is extremely useful in detecting valvular vegeta-
tions in endocarditis and for assessing the degree of valvular
incompetence, if any (Figure 21–2).
Effective antibiotic therapy requires selection of bacterici-
dal or fungicidal drugs to which the organism is sensitive and
then delivering intravenous antibiotics in adequate quanti-
ties for a prolonged period. Fungal endocarditis is almost
never eradicated using pharmacotherapy. The duration of
therapy, in part, depends on the organism. Prosthetic valve
endocarditis often necessitates valve replacement because
antibiotics fail to eliminate the infection or because of valve
dysfunction, valve dehiscence, or ring abscess.
The outcome of both native and prosthetic valve endo-
carditis depends on cardiac function. Patients developing
congestive heart failure do quite poorly without valve
replacement. Valve replacement, even while the patient is still
Figure 21–2. Transesophageal echocardiogram demonstrating mitral valve endocarditis with a prolapsing and partial
flail mitral valve leaflet (arrow). A vegetation can be seen as well. The left ventricle and left atrium are indicated by
LV and LA, respectively. At surgery, the valve was found to be necrotic. The mitral valve was incompetent, with severe
mitral regurgitation, as seen on color-flow Doppler, but this is not shown in this still-frame image.
CHAPTER 21
478
infected or septic, can be lifesaving after congestive heart fail-
ure has developed. When to operate in cases of native valve
endocarditis depends in part on the hemodynamic conse-
quences of the infection (eg, severe valvular regurgitation,
intracardiac shunts, or congestive heart failure). Surgery is
required if antibiotic therapy fails to clear the infection, if
there are persistent fevers or a valve ring abscess, or if cul-
tures have identified a fastidious organism known to be dif-
ficult to eradicate medically. Patients who have more than
one major embolic episode with left-sided endocarditis
almost always undergo valve replacement. Larger vegeta-
tions, particularly on the left side of the heart, are associated
with higher complication rates and poorer outcomes.
In patients suspected of having infective endocarditis,
echocardiography should be performed to identify valvular
vegetations or valve destruction and to qualitatively assess the
degree of valvular regurgitation present. Echocardiography
then can be used to monitor therapy. Increase in vegetation
size, worsening of regurgitation, or the development of
mycotic aneurysms, intramyocardial abscesses, or a fistula
suggests treatment failure and the need for further interven-
tion. In patients with left-sided endocarditis, aortic valve ring
abscess, left-to-right shunts, valvular incompetence, and large
vegetations have important implications for outcome and the
need for valve surgery. Transesophageal echocardiography has
superior sensitivity for identifying valvular vegetations, valve
ring abscesses, and intracardiac shunts. It is particularly valu-
able for visualizing lesions in patients with prosthetic valve
endocarditis. For these reasons, transesophageal echocardiog-
raphy is recommended for all patients suspected of having
left-sided endocarditis, aortic valve endocarditis, or suspected
prosthetic valve endocarditis and for patients with endocardi-
tis who are hemodynamically unstable or deteriorating. The
transesophageal echocardiogram also should be used in the
preoperative and intraoperative management of these
patients to identify unsuspected pathologic findings, includ-
ing aortic-to-atrial fistulas and valve ring infection, and to
verify the adequacy of surgical repair.
Bonow RO et al: ACC/AHA 2006 guidelines for the management
of patients with valvular heart disease: A report of the American
College of Cardiology/American Heart Association Task Force
on Practice Guidelines (writing committee to revise the 1998
guidelines for the management of patients with valvular heart
disease), developed in collaboration with the Society of
Cardiovascular Anesthesiologists, endorsed by the Society for
Cardiovascular Angiography and Interventions and the Society
of Thoracic Surgeons. Circulation 2006;114:e84–231. [PMID:
16880336]
Baddour LM et al: Infective endocarditis: Diagnosis, antimicrobial
therapy, and management of complications: A statement for
healthcare professionals from the Committee on Rheumatic
Fever, Endocarditis, and Kawasaki Disease, Council on
Cardiovascular Disease in the Young, and the Councils on
Clinical Cardiology, Stroke, and Cardiovascular Surgery and
Anesthesia, American Heart Association—Executive Summary
Circulation 2005;111:e394–434. [PMID: 15956145]
Butchart EG et al: Recommendations for the management of
patients after heart valve surgery. Eur Heart J 2005;26:2463–71.
[PMID: 16103039]
Carabello BA: Aortic stenosis. N Engl J Med 2002;346:677–82.
[PMID: 11870246]
Carabello BA: Modern management of mitral stenosis. Circulation
2005;112:432–7. [PMID: 16027271]
Enriquez-Sarano M, Tajik AJ : Aortic regurgitation. N Engl J Med
2004;351:1539–46. [PMID: 15470217]
Cardiac Tamponade
ESSENTIALS OF DIAGNOSIS
Evidence of elevated pericardial pressure manifested as
elevated systemic venous pressure, decreased cardiac
output and hypotension; evidence of decreased periph-
eral perfusion.
Echocardiography: diastolic collapse of right ventricle, sys-
tolic collapse of right atrium, large pericardial effusion.
Pulmonary artery catheter monitoring: equalization of
right atrial, left atrial, and left ventricular end-diastolic
pressures.
General Considerations
Pericardial effusions occur in a variety of patients seen in the
ICU, including those with malignancy, tuberculosis, fungal
infections, myocardial infarction, trauma, acute and chronic
renal failure, thyroid disease, autoimmune conditions, and
more rarely, those with endocarditis or aortic dissection.
Patients after cardiac surgery can develop pericarditis and
pericardial effusions for several reasons. The size of the effu-
sion and the rapidity with which it develops are the major
determinants of its hemodynamic effects. Cardiac tamponade
ensues when adequate ventricular and atrial filling are pre-
vented by increased intrapericardial pressure owing to the
presence of a pericardial effusion. Left atrial, right atrial, left
ventricular end-diastolic, and right ventricular end-diastolic
pressures increase and equalize. Stroke volume, cardiac out-
put, and systemic blood pressure fall greatly, and patients may
develop shock with evidence of end-organ hypoperfusion.
Clinical Features
A. Symptoms and Signs—Symptoms and signs may reflect
the underlying cause of the pericardial effusion, especially if
there is inflammation of the pericardium with acute peri-
carditis. Chest pain that is pleuritic and positional suggests
this diagnosis. However, patients with tamponade need not
have chest pain, especially if tamponade is due to other
causes such as malignancy or uremia. When cardiac tampon-
ade develops, patients may have associated dyspnea and
orthopnea.
CARDIAC PROBLEMS IN CRITICAL CARE
479
Physical findings in cardiac tamponade include distended
neck veins, tachycardia, hypotension, and pulsus paradoxus.
Elevated pericardial pressure will cause distended neck veins
(which should be looked for in the upright position because
the meniscus may not be visible in a semisupine patient
when the pressures are markedly elevated), pulsus paradoxus
(ie, augmented respiratory variation in the pulse pressure,
usually >10 mm Hg), and usually hypotension. Although in
general the blood pressure is reduced, normal or elevated
blood pressure can be seen with tamponade in patients with
previous hypertension. Tachycardia, tachypnea, and orthop-
nea are important supporting signs suggesting elevated pres-
sures affecting the left side of the heart. Heart sounds as well
as the left ventricular impulse may be muted because the
heart is surrounded by fluid and farther away from the chest
wall. Hepatomegaly and peripheral edema may be present.
Patients rarely may present with “low pressure” cardiac tam-
ponade, in which classic signs may be absent but there is evi-
dence of reduced cardiac output. These patients have decreased
intravascular pressures relative to pericardial pressures, but the
diagnosis usually can be made by echocardiogram.
B. Laboratory Findings—Laboratory abnormalities may
identify a specific cause of pericardial effusion. If a diagnos-
tic pericardiocentesis is performed, a specific diagnosis may
be made from bacterial, fungal, or mycobacterial cultures;
cytologic examination; and other studies.
C. Electrocardiography—Electrocardiography may show
decreased voltage. Acute pericarditis may present with dif-
fusely elevated ST segments or PR depression on ECG.
Electrical alternans is an important clue supporting the
diagnosis of cardiac tamponade but is neither sensitive nor
specific.
D. Imaging Studies—The chest x-ray may show car-
diomegaly with a characteristic “water bottle” shape, but if
the development of pericardial effusion is rapid, heart size
may be only slightly increased. At the bedside, echocardio-
graphy can rapidly and accurately determine if pericar-
dial fluid is present and estimate ventricular function
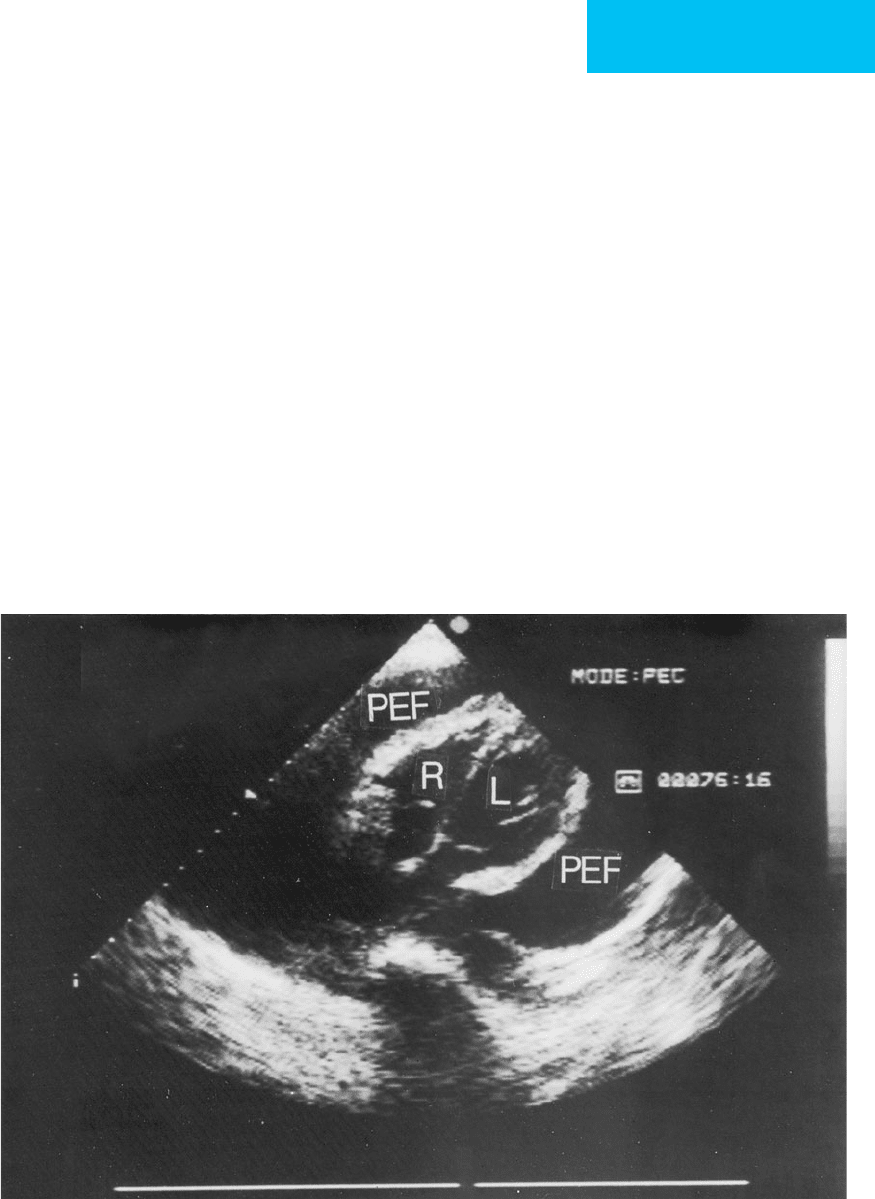
(Figure 21–3). In addition, there are several echocardio-
graphic criteria for the diagnosis of tamponade in patients
with pericardial effusions. These findings include the
Figure 21–3. Two-dimensional echocardiogram taken from the subcostal window demonstrating a large pericardial
effusion with cardiac tamponade. PEF locates the pericardial effusion surrounding the heart. R and L indicate the right
and left ventricles, respectively. Note that the chambers are quite small because of the massive pericardial effusion.
CHAPTER 21
480
“swinging heart,” right ventricular diastolic or right atrial
systolic collapse, respiratory variation in the left ventricular
and the right ventricular chamber sizes, and right atrial
indentation. Although helpful, these signs are neither sensi-
tive nor specific. Therefore, after identifying a moderate to
large pericardial effusion by echocardiography in a sympto-
matic patient, a bedside pulmonary artery catheter should be
placed to confirm the hemodynamic findings of tamponade.
Treatment
Initial treatment of cardiac tamponade consists of rapid
intravenous fluid loading and dopamine. The goal is to
increase intravascular pressures enough to overcome the
increased pericardial pressure as well as maintain adequate
systemic blood pressure. Although these agents may improve
the hemodynamic status for a short time, pericardiocentesis
when tamponade is present is essential to avoid hemody-
namic collapse and death. This procedure should be per-
formed rapidly to relieve the hemodynamic compromise and
to determine the cause of the effusion.
An intrapericardial catheter can be placed through a sub-
xiphoid approach using a wire placed through a thin-walled
needle (Seldinger technique). Positioning is done using elec-
trocardiographic guidance, echocardiographic guidance, or
fluoroscopy. The catheter should remain in place to permit
repeated aspirations of fluid. Fluid should be sent for cul-
ture, cytologic examination, and serologic testing. Patients
with moderate to large effusions and elevated filling pres-
sures but not satisfying the criteria for cardiac tamponade
should have hemodynamic measurements made before and
after pericardiocentesis to verify hemodynamic benefit as
well as to obtain fluid for diagnosis. Cardiac tamponade sec-
ondary to renal failure may benefit from injection of a non-
absorbable corticosteroid into the pericardial space after
drainage of the fluid.
In patients with malignant pericardial effusion and car-
diac tamponade, drainage followed by sclerotherapy using
bleomycin or fluorouracil may decrease the recurrence of
tamponade. Alternatively, balloon pericardiotomy may allow
drainage of fluid into the pleural or mediastinal space—thus
preventing reaccumulation of fluid, which would result in
tamponade. However, in patients whose life expectancy is
greater than 6 months (a small number of patients with
malignant pericardial effusions and tamponade) and in
those whose effusion cannot be controlled with sclerosis of
the pericardial space, pericardiectomy should be considered.
Lange RA, Hillis LD: Acute pericarditis. N Engl J Med 2004;351:
2195–2202. [PMID: 15548780]
Little WC, Freeman GL: Pericardial disease. Circulation 2006;113:
1622–32. [PMID: 16567581]
Maisch B et al: Guidelines on the diagnosis and management of
pericardial diseases executive summary: The task force on the
diagnosis and management of pericardial diseases of the
European Society of Cardiology. Eur Heart J 2004;25:587–610.
[PMID: 15120056]
Sagrista-Sauleda J et al: Low-pressure cardiac tamponade: Clinical
and hemodynamic profile. Circulation 2006;114:945–52.
[PMID: 16923755]
Spodick DH: Acute cardiac tamponade. N Engl J Med 2003;349:
684–90. [PMID: 12917306]
Hypertensive Crisis & Malignant
Hypertension
ESSENTIALS OF DIAGNOSIS
Hypertensive crisis: systemic blood pressure >240/130
mm Hg without symptoms or elevated blood pressure
with chest pain, headache, or heart failure; may have
intracranial hemorrhage, aortic dissection, pulmonary
edema, myocardial infarction, or unstable angina.
Malignant hypertension: severe hypertension associated
with encephalopathy, renal failure, or eye findings
including retinal hemorrhage, exudates, or papilledema.
General Considerations
Hypertension in adults is usually a chronic condition that, if
untreated, is a significant risk factor for the long-term devel-
opment of coronary, cerebral, and peripheral vascular disease.
Mild to moderate hypertension usually poses no immediate
danger to the patient if the pressure is below 170/110 mm Hg.
Patients with mild to moderate hypertension are often
asymptomatic, and control of their blood pressure can be
achieved using oral medications and modification of diet.
Antihypertensive treatment usually is begun on an outpatient
basis after documentation of persistent hypertension and
evaluation for potentially reversible causes.
A subset of patients present with or develop severe life-
threatening hypertension or have other coexisting medical
problems requiring urgent control of blood pressure; these
patients are defined as having a hypertensive crisis (some-
times called a hypertensive emergency). For example, patients
with acute myocardial infarction or unstable angina benefit
greatly from reduction of elevated blood pressure and lower-
ing of left ventricular afterload. Blood pressure represents a
major factor in myocardial oxygen demand. When conges-
tive heart failure owing to left ventricular dysfunction or aor-
tic or mitral regurgitation is associated with severe
hypertension, rapid lowering of blood pressure will acceler-
ate treatment of the hemodynamic dysfunction. Patients
with acute aortic dissection and elevated blood pressure have
greatly increased stress on the aorta, and urgent control of
blood pressure is mandatory. Patients with intracranial
hemorrhage—intracerebral or subarachnoid—also require
control of blood pressure and may become acutely hyperten-
sive as a result of the CNS event. Severe hypertension results
in local and systemic effects that start a cascade of events that

CARDIAC PROBLEMS IN CRITICAL CARE
481
further elevates blood pressure. Dilation of cerebral blood
vessels results in hypertensive encephalopathy, and damage
to the blood vessel wall can increase permeability, resulting
in edema or bleeding.
Malignant hypertension is defined by some as severe
hypertension associated with specific end-organ damage,
namely encephalopathy, nephropathy, or eye findings,
including retinal hemorrhages, exudates, or papilledema.
Treatment of malignant hypertension is important because
rapid and effective lowering of blood pressure is essential for
reversal of complications.
Any of the causes of hypertension can be associated with
hypertensive crisis, including essential, renovascular, or
endocrine-mediated (eg, pheochromocytoma) forms of
hypertension. Most patients who present with hypertensive
crises have preexisting hypertension.
Clinical Features
A. Symptoms and Signs—Patients with severely elevated
blood pressure are frequently asymptomatic, but most will pres-
ent with headache, confusion, stupor, seizure, or coma depend-
ing on the severity of the hypertension and the degree of
end-organ involvement. Chest pain may be due to angina pec-
toris, unstable angina, or myocardial infarction associated with
hypertension, but chest pain also should raise the possibility of
aortic dissection. In malignant hypertension, papilledema, reti-
nal hemorrhages, or exudates are present by definition and may
be accompanied by encephalopathy. Acute oliguric renal failure
as well as signs and symptoms of congestive heart failure may be
seen. The blood pressure is usually quite elevated, with diastolic
blood pressure exceeding 130 mm Hg. Ophthalmoscopic exam-
ination may demonstrate retinal hemorrhages and exudates as
well as papilledema. Patients may have evidence of congestive
heart failure. Neurologic findings owing to severe hypertension
may include focal motor or sensory abnormalities as well as
altered mental status. However, other causes of acute neurologic
impairment with hypertension must be excluded, including pri-
mary CNS events such as strokes, tumors, head injury,
encephalitis, and collagen vascular disease.
B. Laboratory Findings—Serum creatinine and urea nitro-
gen may be elevated. In those with acute hypertensive
nephropathy, urinalysis shows red blood cells, red blood cell
casts and proteinuria.
C. Electrocardiography—Electrocardiography may show left
ventricular hypertrophy, particularly with chronic hyperten-
sion. Acute ST-segment and T-wave changes may be second-
ary to hypertension but also may represent acute ischemia.
D. Imaging Studies—The chest x-ray may show car-
diomegaly and pulmonary edema. Aortic dissection should
be considered when reviewing the film. Imaging of specific
organs depends on symptoms and signs and may include
head CT scan (eg, strokes and focal neurologic findings),
renal ultrasound (eg, acute renal insufficiency), and
echocardiography (eg, aortic dissection).
Treatment
The most important consideration in patients with hyper-
tensive crisis is rapid reduction of blood pressure with a
short-acting, easily titratable agent. The goal is to prevent
permanent vascular and neurologic damage and to avoid
worsening the heart failure or causing uncontrollable
hypotension. Blood pressure should be controlled aggres-
sively in these patients, and therapy should be instituted even
while etiologic investigation is still under way. Of particular
concern, patients with strokes or other types of neurologic
dysfunction may sustain further neurologic damage if blood
pressure is lowered too abruptly or excessively. Therefore,
the initial goal of antihypertensive therapy within the first
6 hours is to lower the blood pressure by 25% of the starting
blood pressure value or to no less than 150/110 mm Hg.
Further lowering should take place more gradually.
A. Nitroprusside—Intravenous nitroprusside, which acts as
a peripheral arteriodilator, is the drug of choice in hyperten-
sive crises because it can be titrated rapidly and safely.
Excessive hypotension can be avoided by careful blood pres-
sure monitoring, usually with an arterial catheter, but a non-
invasive automated cuff manometer is usually satisfactory. If
hypotension occurs with nitroprusside therapy, discontinu-
ation of the drug results in rapid restoration of blood pres-
sure. Nitroprusside is given intravenously at a rate of
0.25–10 μg/kg per minute. Usually one begins at a low infu-
sion rate and adjusts the rate as needed every 5 minutes over
a period of 1–2 hours. Thiocyanate toxicity can occur, par-
ticularly in patients with renal failure. However, over the
first 24 hours, when control of blood pressure is essential,
this is not a major concern. After blood pressure is lowered
to a satisfactory level, institution of oral antihypertensive
drugs is begun with the goal of discontinuing nitroprusside
within 24–48 hours.
B. Other Antihypertensive Agents—Other parenteral
agents that can be used in patients with severe hypertension
include esmolol, hydralazine, labetalol, nitroglycerin (usually
a mild blood pressure–lowering agent), and enalaprilat, an
ACE inhibitor. Esmolol is a short-acting β-adrenergic blocker
indicated for short-term use. It should be avoided in patients
with bronchospasm, severe heart failure, heart block, or
bradycardia. Hydralazine is a peripheral vasodilator that can be
given orally or intravenously. Reflex tachycardia is common, and
β-adrenergic blockers are almost always given simultaneously.
Labetalol has both α- and β-adrenergic blocking effects.
Nitroglycerin has primarily venodilator effects. The degree of
lowering of blood pressure with intravenous nitroglycerin varies
from patient to patient, and there is some risk of lowering car-
diac output excessively with this drug. On the other hand, nitro-
glycerin has the advantage of being a coronary artery
vasodilator and therefore is useful in patients with hypertension
and myocardial ischemia. Enalaprilat is the only intravenous
ACE inhibitor available. It is converted to the active drug
enalapril after infusion. It has modest antihypertensive effects

CHAPTER 21
482
at the dosages recommended (starting dose 0.625 mg). Side
effects include worsening of renal failure and hyperkalemia.
Oral calcium channel blockers, including amlodipine and
diltiazem, are useful in less severe hypertension. In patients
with severe hypertension and heart failure, calcium channel
blockers and beta-blockers may result in unacceptable depres-
sion of ventricular function, in some cases worsening conges-
tive heart failure. However, β-adrenergic blockers must be
used in patients with dissecting aortic aneurysms before sys-
temic vasodilators (eg, hydralazine and nitroprusside) are
given to prevent an increase in shear stress on the aortic wall.
Diuretics may be needed in addition to the antihypertensive
medication to help relieve the volume overload associated
with treatment with many of the vasodilator drugs.
Stable patients with severe hypertension without
encephalopathy may be managed with oral agents, including
beta-blockers, calcium channel blockers, clonidine,
hydralazine, and ACE inhibitors. Combinations of drugs are
often necessary to maximize effects and minimize side effects
and toxicities.
Aggarwal M, Khan IA: Hypertensive crisis: Hypertensive emergen-
cies and urgencies. Cardiol Clin 2006;24:135–46. [PMID:
16326263]
Chobanian AV et al: The seventh report of the Joint National
Committee on prevention, detection, evaluation, and treatment
of high blood pressure: The JNC 7 report. JAMA
2003;289:2560–72. [PMID: 12748199]
Feldstein C: Management of hypertensive crises. Am J Ther 2007;14:
135–9. [PMID 17414580]
Marik PE, Varon J: Hypertensive crises. Chest 2007;131:1949–62.
[PMID: 17565029]
Complications of Cardiac Catheterization
ESSENTIALS OF DIAGNOSIS
Bleeding or thrombosis at vascular access site.
Peripheral arterial emboli from clot at access site.
CNS complications from cerebrovascular emboli.
Arrhythmias, myocardial infarction, cardiac tamponade
from myocardial perforation, aortic dissection.
General Considerations
Patients may be admitted to the ICU after cardiac catheteri-
zation for monitoring or because of complications from the
procedure. Complications may result from the underlying
cardiac problem, but complications from the cardiac
catheterization procedure itself should be anticipated.
Complications can be grouped into problems related to the
vascular access site, the aorta, and the heart.
A. Vascular Access Complications—Vascular access, partic-
ularly in an atherosclerotic vessel, can result in the development
of dissection or occlusion at the vascular site or may provide
a nidus for thrombus with or without peripheral emboliza-
tion. In addition, large hematomas may develop at the entry
site if adequate hemostasis is not achieved or if vascular
damage with a pseudoaneurysm or intimal tear has
occurred. The use of heparin, clopidogrel, aspirin, and glyco-
protein IIb/IIIa receptor inhibitors for treatment of unstable
angina and prolonged catheter placement after catheteriza-
tion have increased the risk of bleeding and the need to pay
close attention to local hemostasis. Several kinds of devices
have been developed to close arterial catheter puncture sites
when catheterization is completed, including those with
arterial sutures and devices that provide internal compres-
sion with a collagen plug. These devices have reduced the risk
of bleeding significantly.
In patients with bleeding at the access site, the hematoma
should be measured, outlined with a marker, and then
observed for any increase in size. An enlarging hematoma or
swelling at the access site indicates a need for rapid evalua-
tion to exclude or control significant bleeding. Distal periph-
eral pulses, leg temperature, and the arterial site should be
checked and findings recorded frequently. Doppler studies
are indicated if changes occur or pain develops in the distal
portion of the extremity or if a pseudoaneurysm or dissec-
tion is suspected. Patients undergoing percutaneous translu-
minal coronary angioplasty (PTCA) and stent placement
may have the arterial sheath left in place for 12–24 hours or
may undergo repeat catheterizations to treat multiple
lesions. These repeat and prolonged interventions may
increase the risk of complications and require diligent anti-
coagulation to avoid arterial thrombosis. Newer coated stents
have improved outcomes dramatically with angioplasty and
higher patency rates but require prolonged treatment with a
combination of clopidogrel and aspirin. Discontinuation of
these agents, in particular clopidogrel, can result in acute
stent thrombosis and abrupt myocardial infarction. This
complicates the management of bleeding complications after
catheterization and also poses problems for ICU patients
requiring surgical noncardiac interventions where postoper-
ative bleeding may be an issue.
B. CNS Complications—Strokes can occur during and after
cardiac catheterization because of embolization of intracar-
diac thrombi, aortic intimal plaque disruption, catheter
thrombosis and embolization, and more rarely, dissection of
carotid arteries or air injected inadvertently during catheter-
ization. Strokes owing to catheterization are not infrequent
occurrences. A careful neurologic evaluation prior to cardiac
catheterization makes evaluation after catheterization more
useful. Interpretation of neurologic findings can be compli-
cated by the use of sedation for catheterization; however, a
localizing finding such as hemiplegia or aphasia is highly
suggestive of postcatheterization embolization. A CT scan or
MRI of the head or cerebral arteriography should be per-
formed immediately to help determine whether the event is
associated with hemorrhage. In the absence of hemorrhage,
intervention with thrombolysis is an option to lyse the clot.
CARDIAC PROBLEMS IN CRITICAL CARE
483
This can be done by localized infusion during cerebral
angiography or with systemic thrombolytic agents.
Prolonged use of heparin or use of other anticoagulants dur-
ing catheterization may preclude the use of systemic throm-
bolysis, and decisions are made on an individual basis with
the help of a stroke team.
C. Other Complications—Cardiac complications related to
catheterization include myocardial infarction, arrhythmias,
cardiac tamponade, and aortic dissection. Echocardiography
should be performed with little hesitation in patients com-
plaining of dyspnea or chest pain after catheterization, and
this technique can be useful to look for new cardiac wall
motion abnormalities, aortic dissection, or the development
of a pericardial effusion.
Pericardial effusions developing after catheterization are
relatively rare but require close observation for develop-
ment of tamponade, particularly in patients who have had
interventions (eg, angioplasty) or are receiving platelet
inhibitors or anticoagulation. Tamponade with hemody-
namic collapse can develop rapidly in these situations.
Acute shortness of breath with chest pain may be due to
acute ischemia, and this must be differentiated from acute
cardiac tamponade.
Radiologic contrast medium–related problems include
histamine-mediated reactions (eg, urticaria, angioedema,
and hypotension), volume depletion and hypotension sec-
ondary to the osmotic diuresis, and acute renal failure. Close
monitoring of patients after cardiac catheterization requires
attention to electrolyte and fluid balance. Patients with dia-
betes and preexisting renal disease are at increased risk of
acute renal failure. Urticaria and other histamine reactions
can be reduced by pretreatment with antihistamines and H2-
blockers one hour before the procedure. Patients with known
allergic reactions to contrast media also should be pretreated
with corticosteroids 8–12 hours before the procedure.
Hydration before and after contrast administration is the
best way to prevent renal failure. Patients with renal insuffi-
ciency or preexisting diabetes may have a reduced risk of fur-
ther deterioration if given acetylcysteine prior to the
administration of contrast material.
Becker CR et al: High-risk situations and procedures. CIN
Consensus Working Panel. Am J Cardiol 2006;98:37–41S.
[PMID: 16949379]
Chandrasekar B et al: Complications of cardiac catheterization in
the current era: A single-center experience. Catheter Cardiovasc
Interv 2001;52:289–95. [PMID: 11246238]
McCullough PA et al: Risk prediction of contrast-induced
nephropathy. CIN Consensus Working Panel. Am J Cardiol
2006;98:27–36. [PMID: 16949378]
Marenzi G et al. N-Acetylcysteine and contrast-induced nephropa-
thy in primary angioplasty. N Engl J Med 2006;354:2773–82.
[PMID: 16807414]
Pannu N, Wiebe N, Tonelli M: Prophylaxis strategies for contrast-
induced nephropathy. Alberta Kidney Disease Network. JAMA
2006;295:2765–79. [PMID: 16788132]
Aortic Dissection
ESSENTIALS OF DIAGNOSIS
Severe chest pain without features of ischemic heart
disease in the presence of hypertension.
Widened mediastinum on chest x-ray.
Aortic dissection identified by echocardiogram, CT scan,
or MRI.
General Considerations
Acute aortic dissection is seen in patients with underlying
atherosclerotic vascular disease, hypertension, and connec-
tive tissue abnormalities such as Marfan’s syndrome. Aortic
dissection is the acute development of a tear in the intima of
the aorta. Arterial blood under high pressure enters the
intima, extending the tear and causing progressive destruc-
tion of the aortic media. This process is potentially cata-
strophic. The path the dissection takes is quite variable,
spiraling superiorly and retrograde to the aortic valve and
the coronary arteries, antegrade to the abdominal aorta, or
both. The hemodynamic manifestations and clinical findings
will depend on the path the dissection takes.
Dissections occur most frequently in the ascending aorta
near the aortic valve or in the proximal descending aorta beyond
the takeoff of the left subclavian artery. There are several classifi-
cation systems for describing the location of aortic dissection.
The easiest to understand and most relevant in terms of clinical
decision making divides aortic dissections into two types. The
proximal or ascending (type A) dissection involves the proximal
aorta but may extend beyond the aortic arch. This type is analo-
gous to the DeBakey type I and type II classification of aortic dis-
sections. Descending or distal (type B) dissection involves only
the descending portion of the aorta, similar to DeBakey type
III. Type A dissections are often lethal, causing acute aortic insuf-
ficiency, congestive heart failure, pericardial effusions, often with
tamponade, and acute myocardial infarctions. Treatment is
almost always surgical. Type B dissections are initially treated
medically but may require surgery after stabilization.
Clinical Features
A. Symptoms and Signs—The most common clinical pres-
entation of patients with aortic dissections is the abrupt onset
of severe chest or back pain. The pain is at maximum intensity
at onset. The pain tracks the progression or pathway of the dis-
section and often is described as tearing or ripping in quality.
The severity of the pain may precipitate vagal reflexes, includ-
ing hypotension and bradycardia. If the aortic valve or coro-
nary arteries are involved, congestive heart failure or myocardial
ischemia can develop acutely. Cardiac tamponade may occur
if the tear extends into the proximal aortic root, allowing blood
to enter the pericardial space. Physical findings include dimin-
ished or unequal peripheral pulses and blood pressures.
CHAPTER 21
484
A murmur of aortic regurgitation may be heard along with
findings consistent with acute pulmonary edema or tamponade.
In this age of thrombolytic therapy and anticoagulation
for acute myocardial infarction, it is critically important to
distinguish aortic dissection from myocardial ischemia.
Although both present with chest pain, the pattern of pain—
quality, location, duration, and onset—should help to distin-
guish between the two. Pain from aortic dissection is more
abrupt in onset, more often reaches maximum intensity
immediately, and is often described as tearing in quality.
Location is more often in the back than substernal. Unlike
myocardial pain, the pain of aortic dissection usually does not
respond to nitrates or beta-blockers acutely but may do so if
a reduction in blood pressure decreases the stress on the
aorta. Also unlike myocardial ischemia, aortic dissection pain
usually is unrelated to activity. In contrast, ischemic pain usu-
ally begins slowly and increases in intensity. It radiates to the
neck, jaw, and arm but never below the umbilicus. Beta-
adrenergic blockers and nitrates usually relieve ischemic pain,
although not necessarily the pain of myocardial infarction.
Ischemia and infarction often have electrocardiographic find-
ings of ST-segment and T-wave changes. On examination, the
presence of a new aortic diastolic murmur, unequal peripheral
pulses, and absence of rales in a patient with chest pain
should raise the question of aortic dissection.
If aortic dissection is a consideration, diagnostic tests
should be undertaken expeditiously because the treatment—
lowering the blood pressure, decreasing myocardial contractil-
ity with beta-blockers, and surgical repair—must be adminis-
tered urgently. Anticoagulation and thrombolytic therapy are
clearly contraindicated. Unfortunately, because aortic dissec-
tion can cause acute myocardial infarction by involving coro-
nary arteries in the dissection, the distinction between aortic
dissection and myocardial ischemia is not always clear.
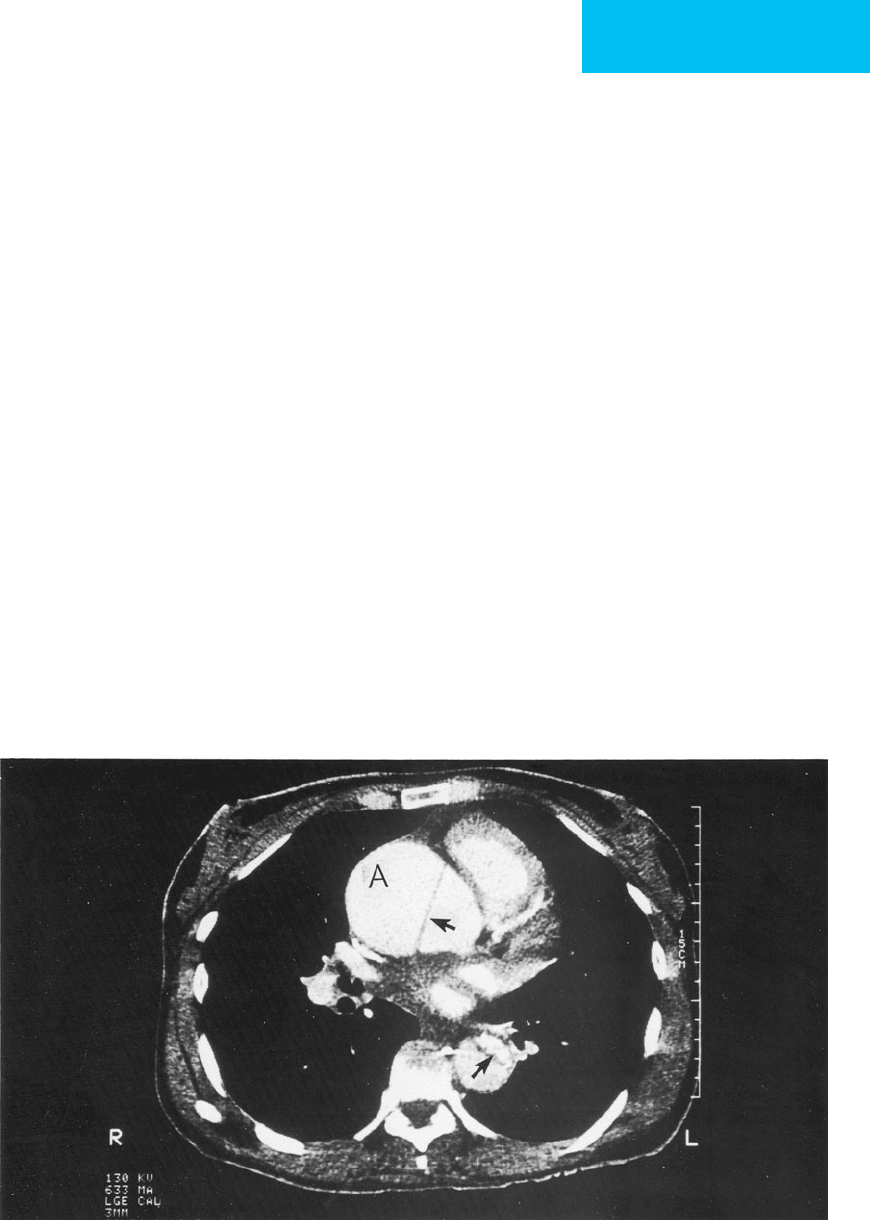
B. Imaging Studies—Initial evaluation with chest x-ray may
identify a widened mediastinum, but more definitive infor-
mation can be obtained using transthoracic echocardiogra-
phy. Although the sensitivity for identifying aortic dissection
is relatively low with transthoracic echocardiography, this test
provides other useful additional information on cardiac func-
tion, ventricular wall motion, and valvular abnormalities and
can identify the presence of pericardial effusion. In addition,
the echocardiogram can be used to measure the aortic root
size, and Doppler echocardiography can determine the degree
of aortic valvular regurgitation (Figure 21–4).
Figure 21–4. Aortic dissection and aneurysm with an intimal flap demonstrated by transesophageal echocardiogra-
phy. The aneurysm of the ascending aorta is at A. The aortic valve is at V. The arrow points to the intimal flap approxi-
mately 2 cm above the aortic valve in the proximal ascending aorta.
CARDIAC PROBLEMS IN CRITICAL CARE
485
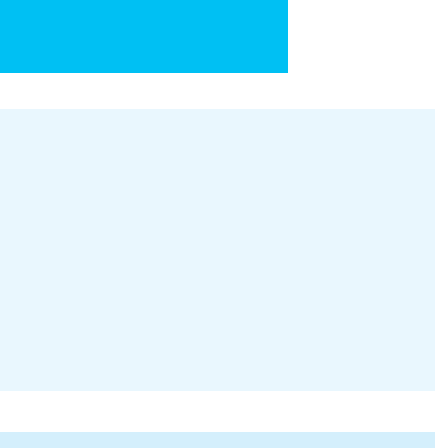
Transesophageal echocardiography, MRI, and CT scan are
80–100% sensitive and specific for the diagnosis of aortic dissec-
tion. MRI is probably the most sensitive and specific procedure,
but the availability of transesophageal echocardiography and
the ability to monitor the patient more closely during echocar-
diography than during MRI or CT scanning are important con-
siderations. Monitoring patients during MRI scanning can be
difficult, and unstable or hypotensive patients should undergo
transesophageal echocardiography at the bedside instead. One
of these tests should make the diagnosis rapidly (Figure 21–5).
If the imaging technique identifies aortic dissection, therapy is
based on the location of the dissection and the extent of aortic
involvement. Further studies may be indicated to assess coro-
nary anatomy and aortic valve function. Cardiac catheterization
may be needed to help guide the surgical intervention.
Treatment
In general, type A aortic dissections require surgery because
medical management alone for proximal ascending aortic
dissection has a high short-term and 1-year mortality rate.
Type B aortic dissections that involve the descending portion
of the thoracic aorta only are managed medically unless there
is compromise of the renal or mesenteric circulations.
Complicated dissections involving the arch and arch vessels
have high surgical and medical mortality rates, making ther-
apeutic decisions more difficult.
Immediate management of all aortic dissections
requires aggressive medical and pharmacologic therapy to
reduce systolic blood pressure and to decrease the peak
systolic velocity of aortic blood flow and thereby reduce
sheer forces on the aortic wall. The goals of therapy
include control of pain, reduction of systolic blood pres-
sure to 100–120 mm Hg (as long as renal, myocardial, and
cerebral perfusion is maintained), and stabilization of the
patient’s hemodynamic variables to permit a thorough
diagnostic evaluation. Beta-adrenergic blockers are used
aggressively to decrease the force of ventricular contrac-
tion. Heart rate is used as a guide to the degree of beta-
blockade, and enough β-adrenergic blockade should be
given to lower the heart rate to 55–65 beats/min.
Nitroprusside is used to control blood pressure initially
and is adjusted as required when beta-blockade is
achieved. Calcium channel blockers, because of their neg-
ative inotropic and antihypertensive properties, are ideal
alternatives in patients who are unable to tolerate beta-
blockers. Hydralazine and other direct vasodilators should
not be given to control blood pressure in the absence of β-
adrenergic blockade. Although blood pressure will fall, the
force of aortic blood flow may increase, further increasing
stress on the damaged aortic wall.
Survival rates approach 80–90% when appropriate ther-
apy is instituted rapidly in both type A and type B aortic dis-
sections. Outcome is determined in part by the degree of
damage to vital organs (eg, kidneys, brain, heart, and bowel),
the underlying condition of the aorta, and the extent of the
repair needed.
Figure 21–5. Aortic dissection and aneurysm with an intimal flap as demonstrated by ultrafast CT scan in the same
patient as shown by transesophageal echocardiography in Figure 21–4. The arrows point to the intimal flap. The
aneurysm is marked by an A.
CHAPTER 21
486
Ince H, Nienaber CA: Diagnosis and management of patients with
aortic dissection. Heart 2007;93:266–70. [PMID 17228080]
Khan IA, Nair CK: Clinical, diagnostic, and management perspec-
tives of aortic dissection. Chest 2002;122:311–28. [PMID:
12114376]
Mukherjee D, Eagle KA: Aortic dissection: An update. Curr Probl
Cardiol 2005;30:287–325. [PMID: 15973249]
Shiga T et al: Diagnostic accuracy of transesophageal echocardio-
graphy, helical computed tomography, and magnetic resonance
imaging for suspected thoracic aortic dissection: Systematic
review and meta-analysis. Arch Intern Med 2006;166:1350–6.
[PMID: 16831999]
Tsai TT, Nienaber CA, Eagle KA: Acute aortic syndromes.
Circulation 2005;112:3802–13. [PMID: 16344407]
ATRIAL ARRHYTHMIAS
Critically ill patients—particularly those with pulmonary
disease and respiratory failure—are at high risk for develop-
ing atrial arrhythmias. Atrial distention, electrolyte imbal-
ances, hypoxemia, and high catecholamine levels all
contribute to electrical instability and increased atrial auto-
maticity. Identifying the type of supraventricular arrhythmia
is essential in choosing the correct treatment. A 12-lead ECG
permits more careful evaluation of P-wave morphology and
axis than a single-lead ECG from the bedside monitor or
“rhythm strip.” The morphology of the ST segments and T
waves should be examined for evidence of ischemia. The PR
interval and initial activation of the QRS segment can iden-
tify the presence of an atrioventricular (AV) nodal bypass
tract and show evidence of preexcitation.
Treatment is directed primarily toward eliminating or
reversing the precipitating or exacerbating causes.
Correction of alkalosis, hypokalemia, hypomagnesemia, or
hypoxemia will increase the likelihood of rate control and
eventual conversion to sinus rhythm. The major goal of acute
treatment is to slow the ventricular rate so as to improve car-
diac output and blood pressure. In the setting of hemody-
namic compromise (eg, hypotension, syncope, chest pain, or
electrocardiographic evidence of ischemia), rapid treatment
using electrical cardioversion may be indicated. This treat-
ment also should be performed immediately if the ventricu-
lar rate is extremely rapid or the patient will not tolerate
prolonged tachycardia because of other conditions such as
aortic or mitral stenosis, hypertrophic cardiomyopathy, or
unstable angina. The high likelihood of recurrence of these
arrhythmias makes rhythm identification and appropriate
pharmacologic treatment important even if initially cor-
rected by electrical cardioversion.
AV Nodal or Reentrant Tachycardia
AV nodal reentrant (circus movement) tachycardias are
rhythm disturbances that depend on the properties of the AV
node for initiation and propagation. The arrhythmia results
from an endless circle of electrical impulses conducted down
one pathway and up another with slow and fast pathways
cooperating to facilitate and maintain the circuit. Alteration of
refractoriness or conduction velocities in either pathway in the
AV node can stop the arrhythmia immediately. The arrhyth-
mia can be prevented by altering the electrical properties of
the involved pathways or by decreasing the frequency of the
premature atrial contractions that often initiate the cycle.
AV nodal reentrant tachycardias usually have ventricular
rates of 140–220 beats/min, and AV conduction is usually 1:1
but rarely 2:1. The P wave may not be obvious if atrial and
ventricular depolarization occur simultaneously, although a
retrograde P wave may be seen. The differential diagnosis
includes sinus tachycardia, atrial tachycardia, atrial flutter, and
orthodromic AV reentry using an accessory pathway. If the
diagnosis is unclear, adenosine (6–12 mg intravenously) usu-
ally will stop either AV nodal reentry or AV reentry causing the
ventricular rate to fall all at once to the underlying sinus rate
and rhythm. A brief intervening period of sinus bradycardia or
complete heart block may occur. Sinus tachycardia will slow
gradually in response to adenosine and then return to the pre-
treatment rate. If the rhythm is atrial tachycardia, atrial flutter,
or atrial fibrillation, increasing AV block with adenosine usu-
ally will make the diagnosis apparent.
AV nodal reentrant tachycardias are treated effectively
with adenosine (6–12 mg IV bolus), verapamil (5 mg IV
bolus), diltiazem (0.25 mg/kg infusion given over 2 minutes),
or β-adrenergic blockers (eg, metoprolol, 5 mg intravenously
up to a total of three doses given every 5 minutes if needed).
These drugs alter conduction velocity through the AV node.
Because of adenosine’s extremely short half-life (measured in
seconds), it is the drug of choice for acute treatment of narrow-
complex tachyarrhythmias, but it is not useful in preventing
recurrences. Therefore, if the risk of recurrence is great in
patients with an underlying predisposing medical condition,
one of the other drugs can be administered to decrease the
likelihood of recurrence and can be tried if adenosine fails to
convert the patient to sinus rhythm. In patients with com-
promised ventricular function, digoxin may be a more
appropriate long-term drug than either calcium channel
blockers or β-adrenergic blockers, both of which are myocar-
dial depressants.
Procainamide is effective in treating atrial arrhythmias by
preventing premature atrial beats and decreasing atrial auto-
maticity. When the AV reentry tachycardia uses concealed
retrograde conduction through a bypass tract, procainamide
also may help by slowing conduction through the bypass
tract. A bypass tract may be suspected when the ventricular
rate exceeds 200 beats/min in an adult or when a baseline
ECG demonstrates a short PR interval and evidence of pre-
excitation. Digoxin, β-adrenergic blockers, and calcium
channel blockers can be dangerous in patients with bypass
tracts who have atrial fibrillation because these drugs block
AV nodal conduction and thereby facilitate conduction
through the bypass tract. The ventricle is bombarded by an
increased number of impulses from the atria, resulting in a
very rapid ventricular rate. Ventricular fibrillation may
