Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CARDIAC PROBLEMS IN CRITICAL CARE
497
Sotalol
Sotalol is a class II (β-adrenergic blocker) and class III antiar-
rhythmic drug that is excreted renally and therefore must be
monitored carefully in patients with changing renal function.
It is an effective agent for atrial and ventricular arrhythmias,
but—like most antiarrhythmic agents—it has proarrhythmic
effects, occurring particularly while therapy is being initiated.
It can cause significant bradycardia and heart block when used
in conjunction with digoxin or calcium channel blockers.
Calcium Channel Blockers
These drugs can be categorized into three subclasses:
verapamil-like drugs, diltiazem-like drugs, and nifedipine-like
drugs. Some of the toxic effects are the logical result of their
therapeutic mechanisms and may be beneficial in certain set-
tings. For example, slowing of the heart rate in patients with
ischemia is a desirable effect of some of the calcium channel
blockers. However, verapamil and diltiazem also can slow AV
nodal and sinus node conduction excessively, resulting in
bradyarrhythmias and hypotension. Because they are myocar-
dial depressants, these drugs may precipitate or exacerbate
congestive heart failure. The bradycardiac effects of diltiazem
and verapamil can be augmented by concomitant use of β-
adrenergic blockers or digoxin. In contrast, nifedipine and
other drugs in its dihydropyridene class of calcium channel
blockers have no effect on the AV node but can cause reflex
tachycardia and hypotension from vasodilation. Calcium
administered intravenously may reverse some of the toxic
effects of the calcium channel blockers, at least temporarily.
Beta-Adrenergic Blockers
Beta-adrenergic blockers are extremely useful drugs for con-
trolling hypertension, treating atrial arrhythmias, and allevi-
ating myocardial ischemia. In a patient with myocardial
dysfunction, β-adrenergic blockers can precipitate profound
heart failure and block the normal tachycardiac response to
hypotension and low cardiac output. Despite this, however,
these drugs have been shown to improve long-term survival
in patients with chronic congestive heart failure, including in
patients with class III to IV heart failure.
These drugs are myocardial depressants, block the AV
node, and by blocking the action of catecholamines,
decrease the sinus nodal rate. In patients with conduction
system disease, β-adrenergic blockers may cause profound
bradycardia. The effects of Beta-adrenergic blockers and cal-
cium channel blockers on the myocardium, the sinus node,
and the AV node can be additive, resulting in severe
hypotension and heart block. Beta-adrenergic agonists may
be used to counteract the excessive depressant effects of β-
adrenergic blockers.
ACE Inhibitors
ACE inhibitors (eg, captopril, enalapril, benazepril, lisinopril)
are commonly used vasodilators valuable in the treatment of
congestive heart failure and hypertension. These drugs can
cause hyperkalemia even in patients without overt renal dis-
ease. Therefore, potassium levels must be observed carefully
when initiating or maintaining therapy with ACE inhibitors.
Rapidly developing renal failure may occur in patients with
renal artery stenosis when ACE inhibitors are started.
Angioedema is a significant and concerning side effect that
should result in terminating this entire class of drug from the
patient’s medical regimen. Cough is another side effect that
patient’s may find bothersome with this class of medica-
tions. In fact, the cough may be confused with the cough
owing to heart failure but responds fairly quickly to removal
of the drug. Angiotensin-receptor blockers have effects simi-
lar to those of ACE inhibitors and may be substituted for
management of the cough complaint. As with other antihy-
pertensive agents, profound hypotension may develop when
starting ACE inhibitors, particularly in patients who are
hypovolemic. In critically ill patients, the benefits and side
effects of these drugs need to be considered carefully.
Darbar D, Roden DM: Future of antiarrhythmic drugs. Curr Opin
Cardiol 2006;21:361–7. [PMID: 16755206]
Gheorghiade M et al: Digoxin in the management of cardiovascu-
lar disorders. Circulation 2004;109:2959–64. [PMID: 16735690]
Kowey PR et al: Classification and pharmacology of antiarrhyth-
mic drugs. Am Heart J 2000;140:12–20. [PMID: 10874257]
Zimetbaum P: Amiodarone for atrial fibrillation. N Engl J Med
2007;356:935–41. [PMID: 17329700]
Zipes DP, Jalife J (eds): Cardiac Electrophysiology from Cell to
Bedside, 4th ed. Philadelphia: Saunders, 2004.
498
Atherosclerotic coronary artery disease is the leading cause of
death in the United States. Each year approximately 1.5 million
patients experience a myocardial infarction. Approximately
20% of these individuals die before they reach the hospital,
and an additional 7–15% die during hospitalization. This
chapter will consider the major coronary artery disease
syndromes: angina pectoris, acute coronary syndromes
(unstable angina and non-ST-segment-elevation myocar-
dial infarction), and acute ST-segment-elevation myocardial
infarction.
Physiologic Considerations
Coronary Anatomy
The right and left coronary arteries arise from ostia in the
right and left sinuses of Valsalva. Their function is to deliver
oxygen and nutrients and to remove toxic metabolites. The
origin of the left coronary artery is called the left main coro-
nary artery and divides into the left anterior descending coro-
nary artery, which feeds the anterior wall of the left ventricle
and the left ventricular septum, and the left circumflex artery,
which supplies the lateral and posterior walls of the left ven-
tricle. The right coronary artery supplies the right ventricular
free wall and in 90% of cases gives off the posterior descending
artery, which, in turn, provides the blood supply for the pos-
terior right ventricle as well as the inferior left ventricular wall
and septum. The coronary artery that gives rise to the poste-
rior descending artery is referred to as dominant. Thus 90% of
people have a right-dominant circulation. The remaining 10%
have a posterior descending artery that originates from the
left circumflex coronary artery. Coronary collateral vessels
span the area between the right and left coronary artery terri-
tories. These vessels are very small and difficult to demon-
strate even during cardiac catheterization. However, as
coronary stenoses develop in the major epicardial coronary
arteries, collateral vessels may increase in size and number
and provide a protective effect by allowing increased blood
supply from the opposite coronary circulation.
Coronary Blood Flow
Coronary blood flow at rest is ordinarily 70–100 mL/min per
100 g of heart tissue. Approximately 80% of the coronary flow
occurs during diastole. As a consequence, coronary blood
flow is highly dependent on diastolic blood pressure and
resistance to coronary flow within the coronary circulation.
In the absence of disease and with a constant myocardial
oxygen requirement (M
VO
2
), coronary blood flow is kept con-
stant by autoregulation of the coronary vasculature by both
myogenic and metabolic factors. Diastolic perfusion pressure
provides the driving pressure for coronary blood flow.
Metabolic factors, particularly adenosine, affect regional
myocardial blood flow. As tissue oxygen decreases, ADP is
converted to AMP and then to adenosine by the enzyme 5′-
nucleotidase. Adenosine then diffuses out of the cell and
causes relaxation of local vascular smooth muscle. This action
of adenosine is terminated by its deamination to inosine.
Myocardial Oxygen Consumption
Over 90% of the heart’s energy is derived from aerobic
metabolism, primarily from oxidation of fatty acids. The
absence of oxygen forces a transition to anaerobic metabo-
lism of glucose and glycogen. Myocardial O
2
requirements
are multiple: 20% of the M
VO
2
is used to support the basal
metabolism of the heart, less than 5% is used to support elec-
trical activity, and approximately 15% is used to move cal-
cium into the sarcoplasmic reticulum. The most important
determinant of M
VO
2
is myocardial contractility, accounting
for 60% of M
VO
2
.
A. Heart Rate and Systolic Blood Pressure—An impor-
tant concept about coronary artery disease is the relation of
M
VO
2
to the heart rate (HR) and systolic blood pressure
(SBP). HR × SBP is commonly referred to as the double prod-
uct. The double product is proportional to M
VO
2
and can be
used as a measure of myocardial work and thus myocardial
O
2
consumption. The inotropic state of the myocardium is
another important determinant of M
VO
2
and myocardial
22
Coronary Heart Disease
Kenneth A. Narahara, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CORONARY HEART DISEASE
499
work. However, it is somewhat difficult to measure clinically;
fortunately, the heart rate and systolic blood pressure usually
provide sufficient information for clinical decision making.
B. Balance of Oxygen Demand and Supply—Myocardial
ischemia represents an imbalance between myocardial oxy-
gen demand and myocardial blood supply. A fixed coronary
artery stenosis will limit coronary blood supply. In this cir-
cumstance, demand for coronary blood flow may increase,
but the stenosis will limit the available blood flow. Hence
demand will exceed supply, and myocardial ischemia will
result. The ability of the coronary artery to respond to sym-
pathetic stimulation and other local factors also can result in
an inadequate blood supply through coronary artery spasm.
However, coronary artery spasm (ie, variant angina and
Prinzmetal’s angina) is seldom the sole cause of inadequate
coronary blood flow. More often, fixed coronary artery
stenoses exist in combination with some degree of coronary
spasm or vasoconstriction to cause a myocardial O
2
demand-
supply imbalance.
Myocardial Ischemia (Angina Pectoris)
ESSENTIALS OF DIAGNOSIS
Complaint of heavy, pressure-like or viselike discomfort;
sometimes choking, a constricting feeling in the throat,
or a sensation of strangling; discomfort located diffusely
in substernal region, left arm, jaw, or neck—rarely local-
ized to a single point.
Discomfort lasts 30 seconds to 15 minutes.
May be provoked by exertion, emotional distress, eat-
ing, and cold.
Should decrease with rest and may be relieved in 1–2
minutes after sublingual nitroglycerin.
General Considerations
Resistance to blood flow in the coronary arteries becomes
significant when there is sufficient narrowing of the coronary
artery diameter by atherosclerotic plaques (diameter
decreased by more than 50%). The physiologic consequence
is that coronary artery blood flow becomes fixed at some
value rather than increasing to meet increased myocardial
demands. Coronary blood flow may be adequate to supply
the myocardium at rest but becomes insufficient during
exertion when the myocardial oxygen demand increases.
This explains why, in patients with stable angina pectoris,
symptoms are seen with exercise and disappear with rest.
Clinical Features
The diagnosis of angina pectoris is typically a clinical one.
Pain with the qualities described below should be considered
the primary diagnostic criterion—that is, the history is the
most important diagnostic clue to ischemic heart disease and
myocardial ischemia (angina pectoris).
A. Symptoms—There are six major features of the clinical
manifestations of myocardial ischemia (angina pectoris): the
quality of the discomfort (patients do not always complain of
“pain”), the location, the duration, provoking factors,
sources of relief, and actions taken by the patient during the
episode.
1. Quality of discomfort—Patients with myocardial
ischemia frequently describe the discomfort as a heavy,
pressure-like, or viselike sensation. They may describe chok-
ing or a constricting feeling in the throat. Indigestion or a sen-
sation of strangling is also frequently described. The patient
should be asked about “discomfort” because many patients do
not perceive angina or myocardial ischemia as “pain.”
2. Location of discomfort—The discomfort of myocar-
dial ischemia usually is located in the substernal region but
also may be located in the arms (the left more often than the
right), the jaw, the neck, the left interscapular region, or
occasionally, the epigastrium. It is often useful to ask the
patient to define the extent of the pain with one finger. The
pain of myocardial ischemia is not likely to be localized to a
single point.
3. Duration of discomfort—Angina pectoris usually lasts
30 seconds to 15 minutes. Longer episodes of ischemic pain
are associated with unstable angina or myocardial infarction.
4. Provocation of discomfort—Exertion, emotional dis-
tress, eating, cold weather, and sexual activity are frequent
initiating events.
5. Relief of discomfort—Pain from myocardial ischemia
should decrease with rest or a reduction in exertion.
Sublingual nitroglycerin should relieve angina within 1–2
minutes, and this feature can be used both for diagnosis and
for treatment.
6. Actions taken by the patient—Angina pectoris is not
relieved by inspiration or movement of the upper extremities
or torso nor by antacids or food. Pain relief achieved in this
way should make one think of other disorders.
B. Physical Findings—During an episode of angina, an S
3
gallop, pulmonary rales, or the murmur of mitral regurgita-
tion may appear. However, these findings are more likely to
be noted during stress testing, when the patient’s chest pain
is provoked with a physician present.
C. Electrocardiography—
1. Resting ECG—If ST-segment and T-wave changes (ie, ST-
segment depression, T-wave inversion, or both) are present
during an episode of pain and return to normal with spon-
taneous relief of pain or after administration of nitroglyc-
erin, the diagnosis of myocardial ischemia is confirmed.

CHAPTER 22
500
2. Exercise stress ECG—The resting ECG frequently is
normal in patients with myocardial ischemia owing to coro-
nary artery disease or coronary artery spasm because the
pain usually has subsided by the time the patient reaches
medical attention. For this reason, stress testing during bicy-
cle or treadmill exercise is frequently employed to reproduce
the supply and demand imbalance that triggers myocardial
ischemia. The patient is asked to walk on a treadmill or pedal
on a bicycle as the work load is increased progressively.
Continuous electrocardiographic monitoring permits detec-
tion of ST-segment depression. Exercise causes an increase in
heart rate and blood pressure (an increase in the double
product); thus patients with a fixed (and inadequate)
myocardial blood supply owing to coronary artery disease
frequently will experience angina with ST-segment depres-
sion as myocardial work exceeds a fixed O
2
supply.
D. Imaging Studies
1. Stress testing—Specialized forms of exercise stress test-
ing, including thallium scintigraphy and stress ventriculog-
raphy, have been introduced to diagnose myocardial
ischemia in patients who have resting ECGs that would make
the diagnosis of myocardial ischemia difficult on the basis of
exercise electrocardiography. For example, patients with rest-
ing ST-segment and T-wave abnormalities owing to left ven-
tricular hypertrophy, from administration of digitalis
glycosides, or from prior myocardial infarction may have a
stress ECG that is difficult or impossible to interpret with
precision. In these circumstances, the use of myocardial per-
fusion scanning with thallium-201 or technetium-99m ses-
tamibi may be useful. These perfusion agents are taken up by
viable myocardium in proportion to coronary blood flow. As
coronary blood flow requirements increase (such as during
exercise), myocardium supplied by normal coronary vessels
will have a normal uptake of the tracer. Conversely, areas of
myocardium served by stenotic coronary arteries will have
reduced coronary blood flow during exercise. As a conse-
quence, the reduced uptake of the perfusion agent will
appear as a “cold spot.”
Exercise ventriculography using echocardiography, cine-
CT scanning, or radionuclide angiography can identify the
presence of myocardial ischemia by the development of a
new or worsened wall motion abnormality during stress. As
myocardial O
2
requirements outstrip the available supply,
regional wall motion abnormalities will develop as nutrient
flow to the myocardium remains fixed in the face of an
increasing metabolic demand. Initially, a localized wall
motion abnormality will appear or will worsen (if a previous
infarction is present). Next, the global left ventricular ejec-
tion fraction will fall. Although these tests are substantially
more expensive than the standard electrocardiographic stress
test, they may provide a definitive noninvasive means of
diagnosing myocardial ischemia.
2. Coronary angiography—Anatomic diagnosis of coro-
nary atherosclerosis is made by injection of radiopaque
contrast material directly into the coronary arteries. Patients
are taken to the catheterization laboratory, where careful
hemodynamic monitoring can be performed. Significant
atherosclerotic lesions are seen as a reduction in the diame-
ter of the coronary artery, and the anatomic information can
be used to decide whether medical therapy or interventional
procedures such as coronary angioplasty or coronary artery
bypass surgery might be useful.
Differential Diagnosis
Other causes of chest pain that may have features suggestive
of angina pectoris include pericarditis (pain is often posi-
tional and related to respiration); esophageal spasm (related
to meals and swallowing); chest wall pain (often reproduced
by applying pressure to the chest wall); aortic dissection
(classically “tearing” in quality and radiating to the back;
pulses in the arms may be unequal); GI pain from esophagi-
tis, gastritis, cholecystitis, and cholelithiasis (often associated
with meals and, for esophagitis and gastritis, relieved by
antacids); and hyperventilation.
Treatment
The treatment of myocardial ischemia is directed at both
reducing myocardial O
2
consumption (myocardial O
2
demand and double product) and increasing myocardial
blood supply. Initially, medical therapy is used in an attempt
to reduce myocardial O
2
consumption (eg, use of beta block-
ade to reduce heart rate and blood pressure) or to increase
myocardial O
2
supply by using coronary vasodilators such as
calcium channel blocking agents or either short-acting (sub-
lingual nitroglycerin) or long-acting nitrates (isosorbide
dinitrate).
More aggressive therapy, such as percutaneous translumi-
nal coronary angioplasty and coronary artery bypass surgery,
increase coronary blood supply directly. While effective in
reaching this goal, as well as in relieving angina, these strate-
gies are invasive and cause a variable degree of morbidity. To
date, with the exception of patients with left main coronary
artery disease or three-vessel coronary artery disease in the
presence of left ventricular dysfunction, neither coronary
angioplasty nor coronary bypass surgery will reduce the
mortality rate from coronary artery disease. The high cost
and stress on the health care network of these procedures
would suggest that the management of myocardial ischemia
with medical therapy is a reasonable first step.
A. Long-Acting Nitrates—Nitrates are the oldest form of
anti-ischemic therapy. Their continued use is a testament to
their efficacy as well as their safety. Therapy with long-acting
nitrates aims to improve coronary blood flow. Twenty mil-
ligrams of isosorbide dinitrate three times a day is a typical
starting dose. Although lower doses may be used, they usu-
ally have little more than a placebo effect in patients with
coronary artery disease. After initial dosing with 20 mg three
times daily for 3–5 days, the dose can be increased to either

40 or 60 mg three times daily. A target dose of at least 40 mg
three times daily would be a reasonable therapeutic goal,
assuming that the patient does not suffer from headaches or
symptoms of hypotension. Alternatively, extended-release
isosorbide mononitrate in a dose of 30–120 mg once or twice
daily may enhance compliance.
“Nitrate headaches” occur frequently during the first few
days of therapy with isosorbide dinitrate. The patient should
be encouraged to continue the medication (perhaps with
administration of acetaminophen) because the headaches fre-
quently subside with time and the antianginal efficacy of the
long-acting nitrates persists. Doses of isosorbide dinitrate
larger than 60 mg three times daily generally are not necessary
for therapy of angina pectoris and produce a smaller incre-
mental improvement in symptoms compared with the
increase from 20 to 40 or 60 mg three times daily. However, in
the treatment of unstable angina or for patients who have
severe angina pectoris that is not amenable to revasculariza-
tion, such high doses of long-acting nitrates may be useful in
providing an asymptomatic or moderately symptomatic state.
B. Beta-Adrenergic Blockade—β-adrenergic blockers are
particularly effective in the treatment of patients who have
coexisting angina and hypertension. Likewise, the combina-
tion of β-blocker therapy with a long-acting nitrate may be
hemodynamically desirable because the long-acting nitrates
tend to produce a modest reflex tachycardia that can be
blunted or eliminated by beta blockade. In the treatment of
exertional angina, beta blockade can be particularly advanta-
geous because it will block catecholamine-induced increases
(from exercise or emotional stress) in heart rate and blood
pressure.
Initial therapy with β-blockers can commence with meto-
prolol, 50 mg twice daily (or 50–100 mg of sustained-release
metoprolol daily); atenolol, 50 mg once daily; or betaxolol,
10 mg once daily. In the elderly patient, these initial doses
should be reduced at the initiation of therapy. Titration of
the dose upward can commence after four to five half-lives
have elapsed, that is, 2–3 days for metoprolol, 3–4 days for
atenolol, and 5–7 days for betaxolol or extended-release
metoprolol (eg, Toprol XL). Upward titration of the dose of
β-blocker should be considered if the resting heart rate or
blood pressure are not affected by the initial dose of therapy.
As a general rule, patients who may be operating machin-
ery or driving automobiles should be warned of the possibil-
ity of drowsiness or lethargy when taking β-blockers.
Frequently, the administration of longer-acting agents such
as extended-release forms of metoprolol or betaxolol at bed-
time can be useful in reducing symptoms of fatigue and
reduced attentiveness during the daytime.
Concern is frequently raised about the use of beta block-
ade in patients with diabetes. However, if the patient does not
suffer from episodes of hypoglycemia, judicious therapy with
beta blockade is often rewarded by substantial reduction in
angina pectoris. In addition, β-blocker use in diabetic
patients with coronary artery disease is associated with a
reduction in mortality. The major concern regarding the
coadministration of beta blockade with hypoglycemic agents
is blunting of the symptoms of hypoglycemia. However, this
effect is related primarily to a reduction of tachycardia;
diaphoresis and hunger are not blunted by β-blocker ther-
apy. Of course, β-blockers should be avoided in the brittle
type 1 diabetic or in diabetics with a history of ketoacidosis.
C. Calcium Channel Blocking Agents—
1. Dihydropyridines—This class of calcium antagonists is
characterized by both a systemic and coronary vasodilator
effect. The dihydropyridines have no effect on sinoatrial (SA)
or atrioventricular (AV) nodal function. Therefore, coad-
ministration of a dihydropyridine with β-blockers for the
combined therapy of angina and hypertension is fre-
quently highly effective. Both agents tend to lower blood
pressure, and the bradycardic effect of beta blockade will
prevent any reflex tachycardia that may be engendered by the
dihydropyridine.
Nifedipine, the first-generation dihydropyridine, had a
relatively short half-life and frequently caused symptoms of
vasodilation, including flushing, headaches, and peripheral
edema. Sustained-release nifedipine is still used for refrac-
tory hypertension in doses of 30–90 mg/day or more.
However, for the treatment of coronary artery disease,
nifedipine and the second-generation dihydropyridines have
been superseded.
Amlodipine and felodipine are “long acting” dihydropyri-
dine calcium channel antagonists. Amlodipine has an inher-
ently long half-life of over 30 hours, whereas felodipine gains
its once-a-day dosing from an enteric coating that results in
the gradual release of the agent. Amlodipine is approved for
both angina and hypertension; felodipine is approved for
hypertension only.
Amlodipine is the only calcium channel blocking agent
that can be used safely in patients with impaired left ventric-
ular function. Hence the agent can be used for antianginal
treatment in addition to nitrates and β-blockers, particularly
when coexisting hypertension is present. The starting dose
for amlodipine is 2.5–5 mg/day with a recommended maxi-
mum of 10 mg/day. Higher doses of amlodipine may afford
additional antianginal and antihypertensive effects, but side
effects such as peripheral edema become more pronounced.
Given the long half-life of amlodipine, the dose of this agent
should not be increased more than once weekly.
2. Verapamil—Verapamil is a vasodilating calcium channel
blocking agent that, in addition to causing coronary artery
vasodilation, has a negative chronotropic effect. Conduction
through both the SA node and the AV node can be slowed by
this agent. Verapamil has a side-effect profile similar to that
of nifedipine. In addition, verapamil causes constipation,
and the patient’s bowel habits should be evaluated carefully.
Many clinicians will start patients on stool softeners or pro-
phylactic milk of magnesia when commencing therapy with
verapamil.
CORONARY HEART DISEASE
501
CHAPTER 22
502
Verapamil is a fairly potent peripheral vasodilator and
therefore is an effective antihypertensive agent. Additionally,
with its bradycardic effect, it may be particularly useful in
patients with ischemic heart disease who are intolerant of
β-blockers, such as those with asthma or type 1 diabetes. It
should be recalled that, on balance, verapamil exerts the
greatest negative inotropic effect of the currently available
calcium channel blockers and should be avoided in patients
with a history of congestive heart failure or a known reduc-
tion in ejection fraction. Short-acting verapamil typically is
administered in a dosage of 80–120 mg every 8 hours.
However, the long-acting verapamil preparations generally
are preferred for the sake of compliance and convenience.
Long-acting verapamil should be initiated at a dosage of
180 mg once daily with upward titration to 240 mg/day.
Titration can occur at weekly intervals for symptoms of
angina or control of hypertension. Patients should be
warned to avoid chewing or crushing the long-acting
preparations of verapamil because the entire daily dose may
be released rapidly. Long-acting verapamil should be initi-
ated at a dosage of 120 mg/day in the elderly or in under-
weight patients.
3. Diltiazem—Diltiazem has a modest effect on heart rate
and blood pressure in normotensive patients. Like all cal-
cium channel blocking agents, it exerts a coronary vasodi-
lating effect. Diltiazem’s antianginal properties are the
result of both coronary vasodilation and a reduction in the
product of heart rate and systolic blood pressure.
Diltiazem has a favorable side-effect profile characterized
by minor occurrences of dyspepsia, rash, and edema.
Because diltiazem depresses SA and AV nodal function, con-
comitant administration of β-blockers warrants careful
attention to the heart rate.
Starting dosages for diltiazem are 60 mg every 8 hours,
and this can be increased to 120 mg every 6–8 hours. Long-
acting preparations of diltiazem have been introduced.
Therapy with these sustained-release preparations can be
initiated at a dosage determined by therapy with the short-
acting preparation (eg, patients who tolerate 60 mg every
8 hours can be converted directly to 180 mg/day of the long-
acting preparation). Frequently, clinicians initiate therapy
with 180 mg of the sustained-release compound and
increase the dose weekly up to 360 mg/day. For elderly and
underweight patients, a starting dose of 120 mg/day may be
preferable.
Like all calcium channel blocking agents currently mar-
keted (with the exception of amlodipine), diltiazem should
be avoided in patients with reduced left ventricular func-
tion. A large multicenter trial demonstrated that the
administration of diltiazem to patients with left ventric-
ular ejection fractions of less than 0.40 or with pul-
monary congestion after acute myocardial infarction is
associated with an approximately 1.4-fold increase in car-
diovascular death. Similar results have been seen in trials
with verapamil.
Ben-Dor I, Battler A: Treatment of stable angina. Heart
2007;93:868–74. [PMID: 17569815]
Fox K et al: Guidelines on the management of stable angina pec-
toris: Executive summary. The Task Force on the Management
of Stable Angina Pectoris of the European Society of
Cardiology. Eur Heart J 2006;27:1341–81. [PMID: 16735367]
Gibbons RJ et al: ACC/AHA 2002 guideline update for the manage-
ment of patients with chronic stable angina: Summary article. A
report of the American College of Cardiology/American Heart
Association Task Force on Practice Guidelines (Committee on
the Management of Patients with Chronic Stable Angina).
Circulation 2003;107:149–58. [PMID: 12515758]
Hemingway H et al: Incidence and prognostic implications of sta-
ble angina pectoris among women and men. JAMA
2006;295:1404–11. [PMID: 16551712]
Acute Coronary Syndromes: Unstable
Angina and Non-ST-Segment-Elevation
Myocardial Infarction
ESSENTIALS OF DIAGNOSIS
Increase in the frequency, severity, or duration of stable
angina or angina occurring at a lower threshold (unsta-
ble angina with low-risk characteristics).
Prolonged (>20 minutes) angina at rest now resolved,
plus diabetes, age over 65, deep T-wave inversions in
more than three leads, angina on walking one to two
blocks on the level or climbing one flight of stairs at a
normal pace in the past 2 weeks, nocturnal angina, or
pathologic Q waves (unstable angina with intermediate-
risk characteristics).
Ongoing (>20 minutes) chest pain, ST-segment depression
= 1 mm or more, angina plus heart failure, or angina plus
hypotension (unstable angina with high-risk characteristics).
Any of the preceding plus cardiac enzyme markers of
myocardial necrosis (troponin I, troponin T, or CK-MB)
(non-ST-segment-elevation myocardial infarction).
General Considerations
Patients with non-ST-segment-elevation (non-Q-wave)
myocardial infarctions represent the severe end of the spec-
trum of the pathology associated with unstable angina.
Fissuring or rupture of an atherosclerotic plaque precedes
unstable angina. If the plaque disruption can be stabilized
spontaneously or through medical intervention, unstable
angina develops. If not, then non-ST-segment-elevation
myocardial infarction may occur.
The American College of Cardiology/American Heart
Association (ACC/AHA) has issued guidelines for the manage-
ment of unstable angina pectoris and non-ST-segment-
elevation myocardial infarction (non-STEMI). The intensity

CORONARY HEART DISEASE
503
of medical therapy and interventional procedures, as well as
the urgency of starting treatment, should be guided by both
symptoms and objective findings.
Clinical Features
A. Symptoms and Signs—The signs and symptoms of
unstable angina and non-STEMI are the same as those of sta-
ble angina pectoris. The distinction between stable angina
and unstable angina or non-STEMI is in the longer duration
of the pain episodes, the reduced amount of exertion
required to produce angina (including pain at rest), and the
increased frequency of chest discomfort.
B. Diagnostic Testing—As in stable angina, patients with
unstable angina frequently have normal ECGs. However, the
presence of new ST-segment depression, T-wave inversion,
or both that resolve spontaneously or with the administra-
tion of sublingual nitroglycerin identifies a category of
patients at high risk for subsequent cardiac events, including
myocardial infarction or death. Chest pain with ST-segment
depression now can be managed by specific therapy defined
by large randomized clinical trials.
A non-STEMI is diagnosed when markers of myocardial
necrosis (ie, elevated levels of troponins or CK-MB) are pres-
ent in the absence of ST-segment elevation on the ECG.
C. Evaluation of the Stabilized Patient—In patients
whose symptoms become well controlled on antianginal
therapy after an episode of unstable angina pectoris, three
approaches may be followed: (1) Perform coronary arteriog-
raphy with the anticipation of elective coronary artery angio-
plasty or coronary artery bypass surgery. If catheterization
and revascularization can be accomplished within 48 hours
of presentation, this approach can reduce morbidity and
mortality in patients with troponin-positive non-STEMIs
and in patients with unstable angina with 1 mm or more of
labile ST-segment depression on presentation. (2) Treat the
patient conservatively with increased doses of antianginal
medications. (3) Perform a functional test to select patients
most likely to benefit from more invasive therapies.
A “low level” stress test can be used in ACC/AHA low-
and intermediate-risk unstable angina patients to identify
those who are at high or low risk for development of subse-
quent myocardial infarction, further unstable angina, and
death after an initial episode of unstable angina. These exer-
cise stress tests, which are limited either by workload (5–7
mets [ie, five to seven times the resting metabolic rate]) or
heart rate (<120 beats/min or less than 65% of predicted
maximum heart rate), are used to determine whether
ischemia is present at levels of exercise likely to be encoun-
tered in ordinary daily activities. Safety is the primary reason
for limiting the test to a lower target workload or heart rate
than might be the goal for diagnosis of angina in a patient
with chest pain. Furthermore, it makes little sense intuitively
to challenge with a conventional stress test a patient who has
recently had symptoms with minimal exertion.
A negative low-level stress test is associated with a rela-
tively good outcome, with over 70% of patients with a nega-
tive study having no or mild angina pectoris in the ensuing
6 months to 1 year. Conversely, a positive low-level stress test,
with development of ST-segment depression or chest pain, is
associated with a greater than 80% incidence of subsequent
undesirable outcomes (eg, recurrent unstable angina,
myocardial infarction, or death). Thus the low-level stress
test can be used to identify patients at high risk and therefore
more likely to benefit from early aggressive management of
ischemic heart disease.
Treatment
Patients who experience an increase in the frequency or
duration of angina pectoris or a marked decline in the
amount of exertion required to provoke chest pain are can-
didates for hospitalization. This will both reduce the work of
the heart (hospitalization itself) and initiate or intensify
pharmacologic therapy for ischemic heart disease.
A. Aspirin—Over two decades ago, two major studies
attested to the importance of aspirin in the therapy of unsta-
ble angina pectoris. Both the Veterans Administration and
the Canadian Cooperative trials demonstrated a 50% reduc-
tion in deaths and myocardial infarctions in patients with
unstable angina who take one to four 325-mg aspirin tablets
a day. The observation that patients with unstable angina or
non-STEMI have large amounts of thrombus in patent but
atherosclerotic coronary arteries at the time of coronary
angioscopy or coronary arteriography provides the patho-
physiologic basis for this remarkably successful and inexpen-
sive form of therapy. Patients with true allergies to aspirin
can substitute clopidogrel, 75 mg/day.
B. Beta-Blockers—The prevention of the ischemia that
underlies unstable angina pectoris and non-STEMI is accom-
plished most easily by reducing the work of the heart. By low-
ering both the heart rate and blood pressure, β-blockers
perform this task efficiently and inexpensively. In patients with
high-risk characteristics of unstable angina or evidence of a
non-STEMI, intravenous administration of β-blocking agents
followed by oral β-blockers is appropriate and desirable.
Metoprolol should be administered intravenously in 5-mg
increments more than 2 minutes apart to a total dose of 15 mg
(or more if better control of the heart rate is desired). Following
intravenous loading of β-blockers, oral metoprolol, 50 mg twice
daily, or oral atenolol, 50 mg once daily, should be initiated.
For patients with contraindications to beta blockade (eg,
bronchospastic lung disease), calcium channel blocking
agents may be substituted. Calcium channel blockers,
angiotensin-converting enzyme (ACE) inhibitors, or
angiotensin II receptor blockers may be added to beta block-
ade if additional antihypertensive therapy is required.
C. Nitrates—Oral nitrates may be initiated as 20-mg isosor-
bide dinitrate three times per day with a target dose of 40–60 mg

CHAPTER 22
504
three times per day. Long-acting isosorbide mononitrate can
be initiated at a dosage of 20 mg/day with a target dosage of
60–120 mg/day. These agents usually are administered to
low- and intermediate-risk patients who need additional
anti-ischemic therapy after β-blockers.
Intravenous nitrate therapy may be particularly useful in
the patient with high-risk unstable angina pectoris who has
ongoing pain or the non-STEMI patient with hypertension
that is difficult to control. Patients receiving intravenous
nitroglycerin should be monitored closely, and the rate of
infusion should be titrated to relieve pain as well as to meet
blood pressure goals while avoiding hypotension.
D. Thrombolytic Therapy—There is no role for throm-
bolytic therapy in unstable angina or non-STEMI. Trials
designed to test the efficacy of thrombolytic therapy in these
settings are negative (thrombolytics increased morbidity and
mortality).
E. Clopidogrel—The thienopyridine clopidogrel is an
antiplatelet agent that inhibits platelet aggregation induced by
adenosine diphosphate (ADP), whereas aspirin blocks the
thromboxane-mediated payway. The CURE trial randomized
12,562 patients with acute coronary syndromes to clopidogrel
75 mg/day (after a 300-mg oral loading dose) or a placebo.
Clopidogrel therapy was associated with a substantial reduc-
tion in the composite endpoint of death from cardiovascular
causes, nonfatal myocardial infarction, or stroke. Although
approved for all forms of acute coronary syndromes, the ben-
efit of this agent was demonstrated only in patients with
unstable angina and ST-segment depression and patients with
non-STEMIs.
F. Anticoagulation—The ESSENCE and TIMI 11B trials
have provided convincing evidence supporting the use of the
low-molecular-weight heparin enoxaparin in high-risk
unstable angina pectoris and non-STEMI patients. While
also approved for use in intermediate-risk unstable angina, a
close look at the data suggests that the greatest benefit from
this agent occurs in patients with pain at rest and 1 mm or
more of ST-segment depression or who have elevated tro-
ponins or CK-MB. The dose of enoxaparin is 1 mg/kg subcu-
taneously every 12 hours for 48–72 hours.
Intravenous unfractionated heparin can be given for non-
STEMI as well as for intermediate- and high-risk unstable
angina. However, given the advantages of low-molecular-
weight heparin, unfractionated heparin seems most useful as
an adjunct to the glycoprotein IIb/IIIa inhibitors or in renal
failure, where enoxaparin is not desired because it is cleared
by the kidneys.
Recently, the synthetic pentasaccharide fondaparinux,
which also binds to activated factor Xa, has been shown to
reduce ischemic events in acute coronary syndromes much
the same as enoxaparin. Fewer bleeding events were observed.
G. Glycoprotein IIb/IIIa Receptor Inhibitors—This class
of drugs blocks the affinity of the glycoprotein IIb/IIIa recep-
tor for fibrinogen on platelets activated by products released
from plaque rupture. In this manner, platelet plugging and
clot formation in atherosclerotic lesions are retarded or
inhibited.
Like enoxaparin, the glycoprotein IIb/IIIa receptor
antagonists (ie, eptifibatide and tirofiban) are indicated for
the treatment of intermediate- and high-risk unstable
angina and for non-STEMI patients. Eptifibatide is
approved for use in preventing complications of percuta-
neous revascularization. Both agents are administered with
unfractionated heparin at a dose titrated to result in a
twofold increase in the partial thromboplastin time.
Eptifibatide is initiated with an intravenous bolus of 180
μg/kg, followed by an infusion of 2 μg/kg per minute for
72–96 hours. Tirofiban is given as an intravenous loading
dose of 0.4 μg/kg per minute for 30 minutes, followed by an
infusion of 0.1 μg/kg per minute for 48–96 hours.
Both glycoprotein IIb/IIIa receptor antagonists reduce the
combined endpoint of death or myocardial infarction or the
need for urgent revascularization. Like enoxaparin, the great-
est benefit from these agents appears to be conferred on the
more ill patients (ie, those with prolonged chest pain, 1 mm
or more of ST-segment depression, or elevated troponins or
cardiac enzymes). The decision to use these costly agents may
hinge on the likelihood of side effects of bleeding.
H. Coronary Angioplasty and Coronary Artery Bypass
Grafting—Debate continues regarding the advantages of
conservative compared with aggressive management of
these patients. The clinician may elect to initiate or enhance
the therapy of patients with low-risk unstable angina and
simply follow the patient symptomatically with or without
hospitalization. This option is based on the observation
that low-risk patients have a risk of serious events (eg,
death and myocardial infarction) that is similar to that
borne by patients with stable angina. Even intermediate-
risk unstable angina pectoris patients who stabilize their
symptoms on medical therapy are at risk only for an
increased rate of recurrent unstable angina during the
ensuing year. Hence, for stabilized patients, watchful wait-
ing appears to carry little risk and may avoid unneeded
revascularization procedures.
Recurrent ischemic pain despite adequate medical ther-
apy should prompt urgent coronary angiography in anticipa-
tion of coronary bypass grafting or coronary angioplasty.
This recommendation also applies to patients with recurrent
pain during treatment of non-STEMI.
Data from TACTICS and TIMI 18 suggest that patients
with rest pain plus ST-segment depression or those who have
a non-STEMI may benefit from an early (but not emergent)
cardiac catheterization in anticipation of expeditious coro-
nary revascularization.
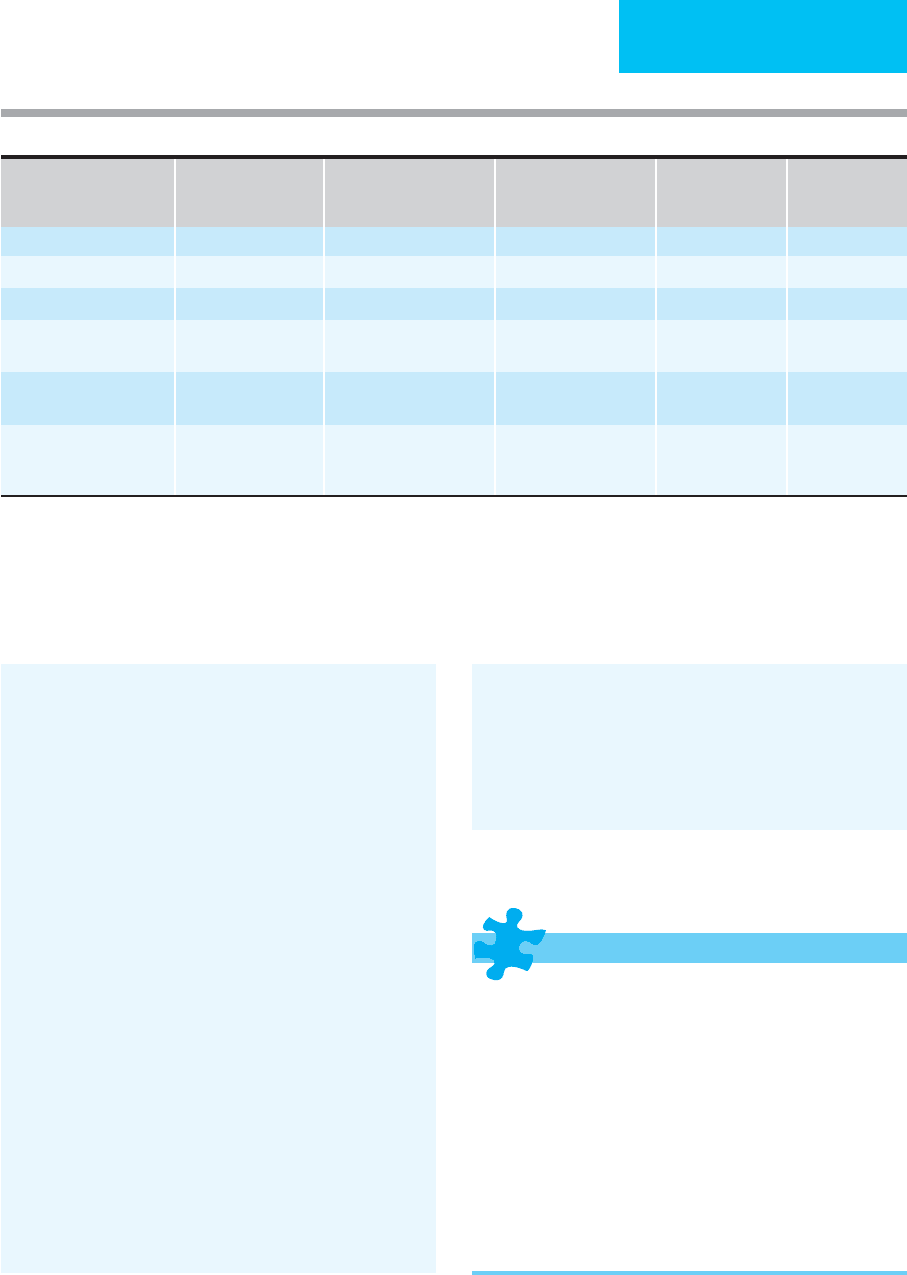
Table 22–1 outlines basic evidence-based treatment
strategies for acute coronary syndromes. The terms low,
intermediate, and high risk refer to ACC/AHA guideline esti-
mates of risk for adverse outcome (eg, recurrent unstable
angina, myocardial infarction, and death).
CORONARY HEART DISEASE
505
Allen LA et al: Comparison of long-term mortality across the spec-
trum of acute coronary syndromes. Am Heart J 2006;151:
1072–8. [PMID: 16644337]
Ayala TH, Schulman SP: Pathogenesis and early management of
non-ST-segment-elevation acute coronary syndromes. Cardiol
Clin 2006;24:19–35. [PMID: 16326254]
Braunwald E et al: ACC/AHA 2002 guideline update for the man-
agement of patients with unstable angina and non-ST-segment-
elevation myocardial infarction. A report of the American
College of Cardiology/American Heart Association Task Force
on Practice Guidelines (Committee on the Management of
Patients with Unstable Angina). Circulation 2002;106:
1893–900. [PMID: 12356647]
Cannon CP: Acute coronary syndromes: Risk stratification and ini-
tial management. Cardiol Clin 2005;23:401–9. [PMID 16278114]
Cannon CP et al, for the TACTICS-TIMI 18 Investigators:
Comparison of early invasive and conservative strategies in
patients with unstable coronary syndromes treated with the gly-
coprotein IIb/IIIa inhibitor tirofiban. N Engl J Med 2001;344:
1879–87. [PMID: 11419424]
The CURE Trial Investigators: Effects of clopidogrel in addition to
aspirin in patients with acute coronary syndromes without ST-
segment elevation. N Engl J Med 2001;345:494–502. [PMID:
11519503]
de Winter RJ et al: Early invasive versus selectively invasive man-
agement for acute coronary syndromes. N Engl J Med
2005;353:1095–104. [PMID: 16162880]
Fitchett DH et al: Randomized evaluation of the efficacy of enoxa-
parin versus unfractionated heparin in high-risk patients with
non-ST-segment-elevation acute coronary syndromes receiving
the glycoprotein IIb/IIIa inhibitor eptifibatide: Long-term
results of the Integrilin and Enoxaparin Randomized
Assessment of Acute Coronary Syndrome Treatment (INTER-
ACT) trial. Am Heart J 2006;151:373–9. [PMID: 16442903]
Tricoci P et al: Clopidogrel to treat patients with non-ST-segment-
elevation acute coronary syndromes after hospital discharge.
Arch Intern Med 2006;166:806–11. [PMID: 16606819]
Yusuf S et al: Comparison of fondaparinux and enoxaparin in
acute coronary syndromes. N Engl J Med 2006;354:1464–76.
[PMID: 16537663]
Acute Myocardial Infarction with ST-
Segment Elevation
ESSENTIALS OF DIAGNOSIS
Precordial chest pain with or without radiation to the
left arm, shoulder, or jaw.
Pain may be identical in quality and description to that
of angina pectoris but may last from 10 minutes to sev-
eral hours.
Greater than 1 mm ST-segment elevation in two con-
tiguous leads with or without Q-wave formation.
Confirmation by serial changes in ECGs plus elevation of
cardiac enzymes (ie, CK-MB, troponin I, or troponin T).
Complications may include arrhythmias, pulmonary
edema, hypotension and shock, ventricular rupture, and
pericarditis.
Non-STEMI
(Elevated Troponin)
High-Risk UAP (Chest
Pain and ≥ 1 mm ST-
Segment Depression
High-Risk UAP (<1 mm
ST-Segment Depression)
Intermediate-
Risk UAP
Low-Risk UAP
Aspirin + + + + +
β-Adrenergic blockers + + + + +
Clopidogrel +
∗
+
∗
Low-molecular-weight
heparin (enoxaparin)
+
†,‡
+
†,‡
IIb-IIIa inhibitor and
unfractionated heparin
+
§
+
§
Consider cardiac catheteri-
zation and revasculariza-
tion within 48 hours
+ +
Note: Recurrent chest pain in the hospital is an indication for expeditious catheterization and intervention.
∗
For 30 days.
†
Avoid if creatinine ≥ 2.5 mg/dL.
‡
Substitute IIb-IIIa inhibitor + unfractionated heparin if urgent catheterization is planned.
§
Avoid if creatinine ≥ 4 mg/dL; adjust dose if creatinine ≥ 2.
Table 22-1. Treatment of unstable angina pectoris (UAP) or non-ST-segment-elevation myocardial infarction (non-STEMI)

CHAPTER 22
506
General Considerations
Coronary thrombosis is the immediate cause of acute
myocardial infarction in over 90% of patients with this syn-
drome of acute myocardial infarction with ST-segment ele-
vation (STEMI). Although early autopsy investigations
suggested a variety of other causes of acute myocardial
infarction—including coronary vasospasm and emboli—
over 86% of those with acute myocardial infarction had
coronary artery thrombi when coronary angiography was
performed within 4 hours of the onset of symptoms.
Current concepts of acute myocardial infarction support
the view that the nidus for thrombosis is an atherosclerotic
plaque in a coronary artery. The plaque itself may or may not
result in stenosis of the artery severe enough to cause symp-
toms, although more severe atherosclerotic stenoses may be
associated with exertional angina. The pathophysiologic
sequence of events then probably includes plaque rupture
with exposure of the subintimal components of the plaque to
coronary blood flow. Platelet activation occurs as the con-
tents of the atherosclerotic plaque (including cholesterol and
calcium) interact with circulating blood components.
Platelet activation releases thromboxane A
2
, a vasoconstric-
tive substance that may lead to localized vasospasm, which
further impedes coronary artery blood flow. The net result of
these events is interruption of coronary blood flow by
thrombus formation followed by myocardial necrosis if ther-
apy is not effective.
New information regarding the treatment of unstable
angina and non-STEMI appears almost weekly. The thera-
pies of unstable angina, non-STEMI, and STEMI are now
driven by large clinical trials that define current pharmaco-
logic and revascularization strategies.
Clinical Features
A. Symptoms—Acute myocardial infarction is classically
associated with precordial chest pain with or without radia-
tion to the left arm, shoulder, or jaw. The pain is identical to
that described in the section on angina pectoris but often
more severe. The only deviation is duration. The chest pain
of myocardial infarction lasts from 10–15 minutes to several
hours. The pain is poorly responsive to nitroglycerin and
may require morphine for relief. Diaphoresis, syncope, and
lightheadedness may be present. Dyspnea and orthopnea
may be associated with acute congestive heart failure and
pulmonary edema.
B. Signs—During myocardial infarction, an S
3
gallop, pul-
monary rales, or the murmur of mitral regurgitation may
appear. Myocardial infarction may be associated with
decreased intensity of S
1
and S
2
. Patients should be examined
carefully for murmurs of mitral regurgitation and for the pres-
ence of pericardial friction rubs. Rales and wheezes may indi-
cate acute pulmonary edema from congestive heart failure.
C. Laboratory Findings—Venous blood should be obtained
routinely to measure the cardiac-specific CK-MB and
troponin I or troponin T on admission to hospital and every
6–8 hours thereafter for the first 24 hours. Daily CK-MB and
troponin levels may be useful during the balance of the
patient’s hospital stay to detect silent recurrent myocardial
necrosis. A partial thromboplastin time should be obtained
on admission and repeated if unfractionated heparin therapy
is indicated. Arterial blood gases should be measured if
hypoxemia is suspected from physical findings, chest x-ray,
or pulse oximetry.
D. Electrocardiography—By definition, acute STEMI is
associated with specific electrocardiographic findings.
However, with modern management, the classic electrocar-
diographic changes of ST-segment elevation followed by T-
wave inversion with development of Q waves may be
retarded or even abolished. A substantial proportion of
patients with myocardial infarction will not develop Q waves
after initial ST-segment elevation and may demonstrate only
T-wave changes or no changes in their ECGs. The develop-
ment of Q waves portends a worse prognosis.
E. Imaging Studies—Imaging studies should not delay
prompt management of acute myocardial infarction.
1. Chest x-ray—The chest x-ray should be reviewed for car-
diomegaly, pulmonary edema, and pleural effusions. In
upright chest x-rays, fullness and congestion of vessels lead-
ing to the upper lung fields sometimes is taken as evidence of
mild pulmonary edema from heart failure.
2. Echocardiography—Echocardiography is useful in
defining coexisting heart disease—especially valvular or con-
genital disease—identifying pericardial effusion, evaluating
unexplained tachycardia, and assessing ventricular function.
Patients with acute myocardial infarction should have an
echocardiogram if there is hypotension or shock. Other indi-
cations for echocardiography include suspicion of ventricu-
lar septal rupture or severe mitral regurgitation (both
potentially requiring surgery), a large myocardial infarction
as judged from CK-MB or troponin elevation, suspected
pericardial effusion, or left ventricular dysfunction that may
be worsened by β-adrenergic blockade or calcium channel
antagonists.
An evaluation of left ventricular function by echocardio-
graphy or radionuclide ventriculography should be per-
formed in almost all patients after an acute myocardial
infarction to help define prognosis and guide appropriate
prophylactic therapy. ACE inhibitors given after myocardial
infarction will prolong survival, and the greater the degree
of reduction in ejection fraction or severity of heart failure
as defined by New York Heart Association (NYHA) func-
tional class, the greater is the benefit from the routine use of
these agents. Similar statements can be made for the β-
blocker carvedilol in patients with NYHA class II and class III
symptoms.
3. Pulmonary artery catheterization (right-sided
heart catheterization)—Right-sided heart catheteriza-
tion allows the determination of right atrial, right ventricular,
