Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


as spasm, rupture, tumor, achalasia, and reflux can be con-
fused with aortic symptomatology. Tortuosity and athero-
sclerosis of the aorta may have a similar appearance on chest
x-ray. Tumors may widen the mediastinal silhouette, and
pulmonary diseases such as pleural effusions and pulmonary
emboli can cause densities on radiographs that may be diffi-
cult to differentiate from aortic disease. When this occurs,
CT scanning or MRI can be of value. Minor ruptures of the
aortic vasa vasorum can widen the aortic shadow without
actually producing aortic disruption.
Treatment
A. General Measures—The disease extent and, if applicable,
the site of intimal injury should be determined based on clin-
ical examination and studies already available. Patients who
are exsanguinating may require immediate operation based
on chest x-ray findings alone. Others should be evaluated rap-
idly and, if ascending aortic disease or aortic transection is
confirmed, repaired immediately. Many elderly patients with
type B dissections or asymptomatic small (<5 cm) aneurysms
may best be managed initially with medical therapy.
Regardless of disease type, patient age, or initial treat-
ment, vigorous continuous medical control of shear forces
with antihypertensives and negative inotropes is essential if
there is residual abnormal aorta. Patients with aortic transec-
tions and localized aneurysms frequently have curative sur-
gery with no remaining diseased aorta. Commonly, when an
aortic dissection is present, only a portion of the aorta is
repaired, and residual disease requires vigorous treatment
and long-term follow-up.
Since diseases of the thoracic aorta can cause morbidity
and mortality owing to complex disease, significant comor-
bidities, and acuteness of presentation, they provide a logical
potential application for newer catheter-based therapies that
have proliferated in the past decade for the treatment of car-
diovascular disorders. Indeed, endovascular stent grafts have
been used in both elective and emergent settings for thoracic
aortic dissection, aneurysmal disease, and blunt injury to the
thoracic aorta. Furthermore, percutaneous fenestration of
the intimal flap has been performed successfully to restore
perfusion to end organs when ischemia results from dissec-
tion. As long-term results of these therapies become available
and as new technology develops, the indications for the use
of percutaneous-based therapies in diseases of the thoracic
aorta will become clearer.
B. Blood Pressure Control—Rapid, continuous control of
blood pressure and pulse pressure should be pursued aggres-
sively immediately following diagnosis. Systolic blood pres-
sure should be kept below 110 mm Hg systolic. The force of
left ventricular contraction (dP/dt) should be minimized by
administering negative inotropes.
An intraarterial monitoring line is vital during the early
phases of treatment because of the potential for rapid alter-
ations in blood pressure. The arterial line should be used
until documented continuous blood pressure control is
accomplished.
Central venous pressures should be monitored and fluid
status optimized. Patients with severe blood loss, intraperi-
cardial blood and tamponade, or end-organ ischemia may
require volume replacement. Cardiovascular function is fre-
quently labile, and inotropes and vasopressors may be
required while definitive diagnosis is established.
A single, ideal drug applicable to every situation does not
exist, but several aspects of the many available antihyperten-
sives are useful. The rapidity of onset, half-life, potency, dis-
tribution, metabolism, degradation products, side effects, and
physiologic effects all should be considered. Use of a short-
acting vasodilator (eg, IV nitroprusside) in combination with
a negative inotropic agent (eg, IV esmolol) effectively reduces
both blood pressure and the force of blood ejection.
Vasodilators commonly used include nitroprusside,
hydralazine, and nitroglycerin. Nitroprusside is well toler-
ated, extremely potent, rapid-acting, and has a short half-life.
Its disadvantages include an increase in dP/dT when used
alone, elevation of pulmonary shunt, and creation of a toxic
metabolite (cyanide) with prolonged high-dose use.
Hydralazine is longer-acting and available orally, making it a
suitable agent for long-term use. Nitroglycerin decreases car-
diac output and blood pressure through direct venodilation
but has little effect on arterial relaxation. Thus its usefulness
for disorders of the thoracic aorta is limited, and it should
not be regarded as a first-line agent.
β-Blockers are available in short-acting (eg, esmolol) and
long-acting (eg, atenolol) forms. As such, they are usually a
part of both short- and long-term management. Of the many
β-blockers available, esmolol offers the advantage of an
extremely short half-life, allowing precise and frequent dos-
ing adjustments toward optimal blood pressure. Labetalol is
also an efficacious agent because of its blockade of both
β-adrenergic and β-adrenergic receptors. With this said, for
acute blood pressure control, β-blocker therapy combined
with sodium nitroprusside, as needed, is regarded as the
therapy of choice.
Calcium blockers produce both decreased blood pressure
and decreased contractility. They are of greatest benefit in
long-term management. Their relatively long half-life limits
use acutely during unstable periods.
Central sympatholytics include trimethaphan, clonidine,
methyldopa, and reserpine. They are used less commonly but
do have a role in acute and chronic care as adjuncts to stan-
dard drug regimens.
Nienaber CA, Eagle KA: Aortic dissection: New frontiers in diag-
nosis and management: I. From etiology to diagnostic strate-
gies. Circulation 2003;108:628–35.
Nienaber CA, Eagle KA: Aortic dissection: New frontiers in diag-
nosis and management: II. Therapeutic management and
follow-up. Circulation 2003;108:772–8.
Hagan PG et al: The International Registry of Acute Aortic
Dissection (IRAD): New insights into an old disease. JAMA
2000;283:897–903. [PMID: 10685714]
Karmy-Jones R, Jurkovich GJ: Blunt chest trauma. Curr Probl Surg
2004;41:211–380. [PMID: 15097979]
CARDIOTHORACIC SURGERY
517
CHAPTER 23
518
Leurs LJ et al: Endovascular treatment of thoracic aortic diseases:
Combined experience from the EUROSTAR and United
Kingdom Thoracic Endograft registries. Thoracic Endograft
Registry Collaborators. J Vasc Surg 2004;40:670–9; discussion
679–80. [PMID: 15472593]
Svensson LG, Crawford ES: Aortic dissection and aortic aneurysm
surgery: Clinical observations, experimental investigations, and
statistical analyses. Curr Probl Surg 1992;29:817–911 (part I)
[PMID: 1464240]; 29:913–1057 (part II) [PMID: 1291195];
30:1–163 (part III).
Postoperative Arrhythmias
ESSENTIALS OF DIAGNOSIS
Variable heart rate.
Regular or irregular rhythm.
Electrocardiographic abnormalities.
Altered peripheral perfusion.
General Considerations
Significant cardiac dysrhythmias occur in up to one-third of
postoperative cardiac surgical patients. Age is the most con-
sistently identified predictor of postoperative arrhythmias,
although many other risk factors exist, including valvular
disease, cardiomyopathy, ischemia, reperfusion, adequacy of
myocardial protection, metabolic derangements, adrenergic
states, medications, temperature, and mechanical irritants.
Arrhythmias should be classified first by ventricular rate.
The rhythm then is subclassified according to its origin—
supraventricular or ventricular—by establishing the rate of
the atrium and evaluating the status of the atrioventricular
(AV) conduction system. Bradycardias include sinus brady-
cardia, heart block, sinus arrest, and slow junctional
rhythms. Tachycardias include (1) supraventricular arrhyth-
mias (eg, atrial fibrillation, atrial flutter, premature atrial
contractions, paroxysmal atrial tachycardia, and fast junc-
tional rhythms) and (2) ventricular tachycardia, flutter, fib-
rillation, and premature ventricular contractions.
Conduction defects include heart block, bundle branch
block, and preexcitation. Sometimes, the origin of a rapid
arrhythmia is indeterminate and should be referred to as a
nonspecific wide complex tachycardia.
Etiology
The etiology of perioperative arrhythmias is multifactorial.
Mechanistically, they can be separated into ectopic foci and
reentrant circuits. Both originate either from abnormal car-
diac tissue affected by ischemia, hypertrophy, dilation, car-
diomyopathy, and scar or from normal cardiac tissue
induced by inotropes, endogenous catecholamines, auto-
nomic stimulation, and metabolic derangements.
A. Intrinsic Factors—Age is associated with supraventricu-
lar arrhythmias and heart block in both cardiac and other
thoracic surgical patients. The etiology of this association is
unclear, but the incidence in patients over 65 years of age is
high enough to warrant prophylactic therapy in many cases.
To this end, β-blockers (eg, sotalol) and amiodarone are
commonly used agents. Although routine preoperative pro-
phylaxis against postoperative arrhythmias (particularly
atrial fibrillation) remains controversial, it is increasingly
supported by emerging data. Intrinsic cardiac disease,
including cardiomyopathy, acute coronary insufficiency,
valvular heart disease, congenital lesions, pulmonary hyper-
tension, ventricular outflow obstruction, and ventricular
failure, also increases the incidence and severity of arrhyth-
mias in both the preoperative and postoperative periods.
Cardiomyopathy, both ischemic and nonischemic, as well
as dilated and nondilated, frequently causes both atrial and
ventricular rhythm irregularity and is one of the more com-
mon presenting complaints. Surgical therapy (excluding
aneurysm resection and endocardial ablation) frequently
does not eliminate the cause. Atrial arrhythmias can result
from primary involvement of atrial muscle or secondary
dilation of atrial chambers by ventricular failure. Ectopic foci
and reentrant circuits are the primary underlying causes, but
the metabolic complications of diuresis and inotropes fre-
quently contribute. Ventricular rhythm disturbances develop
by these same mechanisms and are often life-threatening.
Acute coronary arterial insufficiency frequently presents
with severe arrhythmias (particularly ventricular) or heart
block. They can recur or present postoperatively from resid-
ual or recurrent ischemia and reperfusion injury.
Valvular heart disease frequently has residua that predis-
pose to arrhythmias despite correction of the valvular lesion.
The conduction system is anatomically close to valvular
structures and is easily interrupted.
Endocarditis is particularly likely to be associated with
heart block pre- and postoperatively. Aortic disease leads to
left ventricular hypertrophy or ventricular dilatation, both of
which predispose to reentrant circuits or arrhythmic foci.
Mitral and tricuspid valve disease most commonly causes
atrial arrhythmias, primarily fibrillation. These should be
expected to recur with almost 100% certainty in the postop-
erative period.
Congenital lesions frequently are associated with abnor-
malities of the location and function of the conduction sys-
tem and with chamber enlargement or hypertrophy. All these
factors contribute to ectopic foci and reentry. Wolff-
Parkinson-White syndrome is a common congenital lesion
of the conduction system predisposing to reentrant AV
rhythms. Gross anatomic disease is also occasionally associ-
ated with specific rhythm changes. In particular, Ebstein’s
anomaly may be complicated by Wolff-Parkinson-White
syndrome, tetralogy of Fallot is associated with right ventric-
ular arrhythmic foci, and certain types of transposition result
in abnormal conduction anatomy and an increased incidence
of perioperative heart block. Pulmonary and pulmonary

CARDIOTHORACIC SURGERY
519
vascular abnormalities are superimposed on all these lesions
and result in right ventricular enlargement and hypertrophy,
tricuspid regurgitation, and secondary atrial arrhythmias.
B. Extrinsic Factors—Mechanical irritants (eg, chest tubes,
central catheters, blood, and tamponade), metabolic
derangements (eg, hypo- or hypermagnesemia, -kalemia,
-phosphatemia, and -calcemia), adrenergic or vagotonic
states, and cardiovascular drugs are frequent in the postoper-
ative period and can induce and aggravate arrhythmias.
Clinical Features
The approach to the diagnosis of rhythm disturbances in the
postoperative period is similar to that presented elsewhere.
However, because of the unique perioperative factors that
contribute to arrhythmias, an organized, rapid, and complete
evaluation is crucial.
A. Symptoms and Signs—Patients with cardiac arrhyth-
mias in the perioperative period have findings identical to
those seen in nonsurgical patients. They may have more pro-
found and acute circulatory compromise owing to residual
anesthetic agents, cardiopulmonary bypass effects, ongoing
hemorrhage, metabolic derangements, volume shifts,
hypothermia, and residual cardiac disease.
B. Electrocardiography—Unique to cardiac surgical
patients is the frequent presence of ventricular or atrial pac-
ing wires, which can provide valuable information and man-
agement options. Twelve-lead surface electrocardiographic
tracings should be compared with preoperative and earlier
postoperative examinations for evidence of ischemia, rhyth-
micity, conduction abnormalities, QRS-complex and ST-
segment abnormalities, and QT-interval prolongation.
If the rhythm cannot be diagnosed conclusively, an atrial
ECG should be obtained by attaching one or more of the
atrial pacing wires (if not in use for pacing) to the electrocar-
diographic machine or bedside monitor. A predetermined
configuration on the 12-lead machine is usually used, and
the tracings based on the atrial wires will emphasize the atrial
portion of the rhythm despite its small muscle mass.
Signal-averaged ECGs and programmed electrical stimu-
lation are beyond the scope of this text but should be pur-
sued on an individual basis to establish a diagnosis, stratify
risk, and evaluate the effects of treatment.
C. Laboratory Findings—Arterial blood gases and elec-
trolytes should be obtained to exclude acidosis, alkalosis, and
electrolyte abnormalities. Serum potassium and calcium lev-
els merit particular attention.
Invasive Hemodynamic Monitoring
Invasive hemodynamic monitoring with arterial lines and
flow-directed pulmonary artery catheters typically is per-
formed to assist with management after cardiac surgery.
Analysis of these data is invaluable in the diagnosis and man-
agement of postoperative arrhythmias. Furthermore,
confirmation of appropriate waveforms (eg, pulmonary cap-
illary wedge pressure and pulmonary artery pressure) with
the pulmonary artery catheter may decrease the suspicion of
mechanical irritation from the catheter, significantly con-
tributing to the arrhythmias.
Differential Diagnosis
Problems peculiar to postoperative cardiac surgical patients
that may lead to arrhythmias include hypovolemia, bleeding,
pericardial tamponade, tension pneumothorax, thrombosis
or dehiscence of a prosthetic valve, coronary ischemia, and
hypoxia. Care must be exerted to ensure that the bedside
monitor is working correctly and that observed rhythms are
not due to electrical interference.
Treatment
A. Antiarrhythmics—Arrhythmias are frequent postopera-
tively, and prophylaxis with a variety of agents appears effec-
tive. In particular, β-blockers reduce the incidence and
severity of atrial arrhythmias and probably prevent some
ventricular arrhythmias. Although there is conflicting evi-
dence, magnesium appears to have some antiarrhythmic
effects and may reduce the incidence of atrial fibrillation,
atrial flutter, and ventricular arrhythmias as well. Calcium
channel blockers may have similar benefits, but these agents
are less well studied in the postoperative context.
Amiodorone, a class III agent, has been shown recently, albeit
in a very small study, to reduce the incidence of postopera-
tive arrhythmias when administered perioperatively. Further
discussion of the medical treatment of arrhythmias is found
in detail in Chapter 22.
B. Cardioversion—In addition to pharmacologic measures,
preparation should be made for rapid cardioversion in
patients at high risk for severe ventricular arrhythmias.
Patients who have had ventricular fibrillation perioperatively
may require immediate cardioversion. Equipment should be
ready at the bedside and attached to the patient. Much of the
morbidity of severe ventricular arrhythmias can be avoided
by immediate cardioversion.
The rhythm type and chamber of origin—atrial, junc-
tional, or ventricular—should be established. If the atrial
arrhythmia is fast and poorly tolerated (ie, symptomatic),
immediate electrical conversion is warranted. To convert
atrial fibrillation or flutter, high-energy shock usually is
required and always should be synchronized. Overdrive atrial
pacing may be performed at the bedside using the atrial epi-
cardial pacing wires. This is most effective for supraventricu-
lar tachyarrhythmias such as atrial flutter and paroxysmal
atrial or AV junctional reentrant circuits. Rapid atrial pacing
also can interrupt a reentrant circuit such as atrial fibrilla-
tion, thereby restoring sinus rhythm, although less effec-
tively. When performing overdrive pacing, great vigilance
must be exercised to ensure that the atrial leads—rather than
the ventricular leads—are attached to the generator.
CHAPTER 23
520
Ventricular tachycardia frequently can be terminated
with low-energy synchronized cardioversion. Ventricular fib-
rillation should be treated immediately with high-energy
defibrillation, usually unsynchronized. Both defibrillation
and cardioversion can worsen the existing rhythm, so one
must be prepared to increase electrical output rapidly and
defibrillate again. If the rhythm is bradycardiac or becomes
so following electrical or chemical conversion, ventricular
pacing should be instituted immediately. After an adequate
heart rate is obtained with ventricular pacing, the patient can
be converted to atrial or AV sequential pacing if wires are
available. If wires are not available or do not function, tem-
porary transvenous pacing (eg, balloon-guided or pacing
pulmonary artery catheter wires) can be attempted.
C. Supportive Measures—If prophylaxis has been unsuc-
cessful, the first objective is to maintain adequate oxygen
delivery and pH control with optimal ventilation.
Circulatory support with cardiopulmonary resuscitation
(CPR) may be necessary while preparations are made for
electrical cardioversion. CPR procedures in cardiac surgery
patients are similar to those followed under other circum-
stances. Closed chest compressions are effective in cardiac
surgery patients and should be used when indicated, as in
any other resuscitation effort. If a pulse is obtained with
CPR, continued efforts at external electrical conversion can
be pursued, but if perfusion is inadequate or external electri-
cal conversion is unsuccessful, open cardiac massage and
internal paddle defibrillation should be considered.
After initial control with electrical conversion in unstable
patients—and primarily in stable patients—the rhythm
should be evaluated for type and probable causes. Many
rhythms are caused by temporary derangements and are best
treated by eliminating the primary cause. Almost all antiar-
rhythmic drugs have adverse side effects even when used
appropriately, and many (perhaps all) are proarrhythmic.
Careful consideration of the risks and benefits of drug ther-
apy is vital because the complications of therapy sometimes
are worse than the underlying arrhythmia. The safest thera-
pies are to optimize electrolytes, decrease sympathetic stim-
ulation, remove mechanical causes, treat ischemia, and allow
some temporary arrhythmias (owing to reperfusion) to
resolve spontaneously with careful monitoring.
Atrial arrhythmias are particularly common and usually
cannot be allowed to persist because they are accompanied by
symptomatic tachycardia. The rate of conduction of atrial fib-
rillation and flutter through the AV node can be blocked with
digoxin, β-blockers, and calcium channel blockers singly or in
combination. After adequate rate control is established, con-
version of the arrhythmia can be accomplished with a class Ia
antiarrhythmic agent (eg, procainamide or quinidine). The
risk of treating relatively benign atrial arrhythmias with class
I agents should be appreciated because there is a chance of
inducing ventricular arrhythmias.
Ventricular arrhythmias in the postoperative period
require individual evaluation of the circumstances, prior
therapy, and risks of drug treatment. Unless a specific cause
is found and removed, most arrhythmias will recur, requir-
ing drug or device therapy to block the effects. For this rea-
son, symptomatic ventricular arrhythmias (eg, tachycardia
or fibrillation) almost always should be corrected.
Kerstein J et al: Giving IV and oral amiodarone perioperatively for
the prevention of postoperative atrial fibrillation in patients
undergoing coronary artery bypass surgery: The GAP study.
Chest 2004;126:716–24.
Knotzer H et al: Postbypass arrhythmias: Pathophysiology, prevention,
and therapy. Curr Opin Crit Care 2004;10:330–5. [PMID: 15385747]
Mathew JP et al: A multicenter risk index for atrial fibrillation after
cardiac surgery. Investigators of the Ischemia Research and
Education Foundation, Multicenter Study of Perioperative
Ischemia Research Group. JAMA 2004;291:1720–9. [PMID:
15082699]
Palin CA, Kailasam R, Hogue CW Jr: Atrial fibrillation after cardiac
surgery: Pathophysiology and treatment. Semin Cardiothorac
Vasc Anesth 2004;8:175–83. [PMID: 15375479]
Piotrowski AA, Kalus JS: Magnesium for the treatment and pre-
vention of atrial tachyarrhythmias. Pharmacotherapy 2004;24:
879–95. [PMID: 15303452]
Bleeding, Coagulopathy, & Blood
Product Utilization
ESSENTIALS OF DIAGNOSIS
Excessive chest tube output.
Hypovolemia.
Bleeding from needle puncture sites.
GI or endotracheal tube bleeding.
Rash, hematuria.
Abdominal or groin distention.
Respiratory compromise.
Neurologic event.
Evidence of tamponade.
General Considerations
Hypocoagulable and hypercoagulable states are known com-
plications of all major surgery but are particularly common
following cardiovascular surgery. Both may adversely affect
outcome. Factors contributing to a hypocoagulable state
include the underlying pathology and anatomy of the heart
or great vessel disease itself and a variety of intrinsic coagu-
lation abnormalities owing to hepatic failure, uremia, drugs,
and cardiopulmonary bypass. Hypercoagulability results
from intravascular stasis, endothelial injury, implanted for-
eign bodies, and derangement of the normal anticoagulant
factors by blood loss, surgical complications, cardiopul-
monary bypass, and drugs.

CARDIOTHORACIC SURGERY
521
Etiology
A number of causes combine to make both bleeding and
excessive coagulation two of the most common complica-
tions of cardiovascular surgery. Both are reviewed here
because of the delicate balance between normal coagulation
and pathologic bleeding or clotting. Factors favoring coagu-
lation and decreased bleeding are complicated by the seque-
lae of excessive thrombosis: myocardial infarction, stroke, or
peripheral embolus.
A. Hypocoagulability—The frequency of blood product
administration varies widely among institutions, but the
incidence of blood and coagulation factor loss in cardiotho-
racic surgery patients is significant at all centers. The major-
ity of coronary, valvular, congenital, and ascending aortic or
arch aortic surgeries performed by current techniques use
total cardiopulmonary bypass and systemic anticoagulation
with heparin, with or without hypothermia. This remains
true even with the recent increased popularity of minimally
invasive techniques (“keyhole” surgery) and “beating heart”
(ie, off-pump) surgery. Descending thoracic aortic surgery is
performed frequently using partial bypass or the “clamp and
sew” technique, both of which eliminate or reduce the need
for anticoagulation with heparin. Total cardiopulmonary
bypass circuits consist of priming solutions, pumps, cannu-
las, tubing, reservoirs, filters, and oxygenators. Each of these
components causes a variety of coagulation changes, includ-
ing dilution of all blood components by priming solution,
consumption and impairment of clotting factors and
platelets by contact with component surfaces, release of
cytokines and complement, blood and factor injury by direct
air contact in the operative field, and injury by turbulence
and mechanical stress. Additionally, many operations use
hypothermia, which further decreases the activity of existing
clotting factors. The length of cardiopulmonary bypass and
the degree of hypothermia employed are related to the sever-
ity of these changes.
In addition to these deleterious changes are the effects
produced by heparin. High-dose heparin (100 units/kg) is
necessary for current bypass circuits to prevent circuit
thrombosis. With the use of heparin-bonded bypass circuits,
lower-dose heparin may be as efficacious, although this is
currently the focus of active investigation. The majority of
heparin’s effects are counteracted by protamine administra-
tion after weaning from cardiopulmonary bypass.
Protamine, however, is itself a weak anticoagulant, and the
heparin-protamine complex thus formed impairs platelet
and factor function until cleared from the bloodstream by
the reticuloendothelial system. Occasionally, heparin-
induced antibodies or protamine intolerance complicates the
perioperative course and requires specific therapy as out-
lined below. The development of bypass circuits with
improved biocompatibility (eg, heparin-bonded circuits)
may decrease the heparin—and thus the protamine—
requirements. Further, there is ongoing investigation of
heparin alternatives, particularly direct thrombin inhibitors
(eg, bivalirudin), for use in cardiac surgery. Partial bypass
circuits and shunts that do not require an oxygenator (eg, left
atrial to femoral or descending aorta) can be accomplished
with little or no heparin in many instances. This is particu-
larly important in traumatic aortic injuries, where anticoag-
ulation is usually contraindicated.
Numerous risk factors identify patients more likely to
have hemorrhagic complications and require transfusion
therapy. Platelet inhibitors commonly used for treatment
and prevention of cardiovascular disorders include newer
agents such as the platelet glycoprotein IIb/IIIa receptor
inhibitors (eg, abciximab), although aspirin remains the
most commonly used medication. Platelet function is
reduced dramatically by aspirin for up to 10 days following a
single dose. Nonsteroidal anti-inflammatory agents have
similar effects but usually are more transient. Heparin ther-
apy preoperatively can result in heparin-antibody-platelet
complexes with subsequent thrombocytopenia or occasional
thrombotic complications. Warfarin therapy preoperatively
typically is reversed by withholding warfarin for several days
until measured coagulation tests are normal. Thrombolytics
usually are combined with both heparin and antiplatelet
therapy and have the additional effect of depleting fibrino-
gen levels. Antibiotics occasionally result in vitamin
K–dependent factor loss. High-dose penicillin-like antibi-
otics can cause profound platelet dysfunction.
A number of systemic diseases cause specific defects.
Uremia primarily affects platelet function, and hepatic failure
(primary or secondary to alcohol or congestive heart failure)
results in decreased levels and delayed restoration of clotting
factors. Cyanotic disease is believed to cause factor and
platelet dysfunction. Thrombocytopenia and factor defi-
ciency frequently occur with septicemia associated with endo-
carditis. Von Willebrand’s disease and other inherited platelet
and factor abnormalities usually can be identified by a careful
preoperative history. Poor tissues are associated with malnu-
trition, age, organ failure, advanced endocarditis, and connec-
tive tissue disease. Transfusion reactions are sometimes
difficult to detect but can cause severe coagulopathies.
Reoperations and procedures requiring multiple suture
lines, work on abnormal tissue, and extensive operative dis-
sections increase the risk for bleeding. These include all reop-
erations, aortic dissections and aneurysms, multiple-valve
and combined procedures, complex congenital heart disease,
and patients who require ventricular support.
Prolonged cardiopulmonary bypass, hypothermia, circu-
latory arrest, a history of massive intraoperative blood loss,
and perioperative cardiovascular collapse all decrease the
level and function of platelets and clotting factors. A history
of heparin resistance or a protamine reaction frequently her-
alds a fibrinolytic state, intravascular coagulation, or severe
platelet or factor deficiency.
Recent efforts to modify the bypass circuit with heparin
bonding or to improve surgical techniques (eg, by minimally
invasive or “beating heart” surgery) appear to ameliorate the
inflammation and coagulation abnormalities after cardiac

CHAPTER 23
522
surgery. However, even with these advances, current tech-
niques are only partially effective; thus coagulation abnor-
malities continue to be a major cause of morbidity after
cardiac surgery.
B. Hypercoagulable States—Hypercoagulable states are
classically explained by Virchow’s triad of stasis, endothelial
injury, and systemic hypercoagulability. Stasis is present dur-
ing low-flow states, periods of immobility, during certain
arrhythmias, and intraoperatively during vessel or chamber
cannulation or clamping. The risk of major arterial thrombo-
sis and deep venous thrombosis appears to be low in patients
who have undergone full anticoagulation. In procedures such
as descending aortic replacement with heparinless shunts or
without bypass, the risk is similar to that of other thoraco-
tomy and vascular surgery patients. Endothelial injury (ie,
abnormal endothelium) is ubiquitous in cardiovascular sur-
gery and includes coronary anastomotic sites, vascular clamp
sites, tears in aortic dissection patients, conduits, valves,
intravascular or cardiac patches, and numerous arterial and
venous catheters. Systemic hypercoagulability occurs after all
types of major surgery presumably owing to coagulation fac-
tor activation and derangements of factor levels. Naturally
occurring anticoagulants, including proteins A, C, and S and
antithrombin III, are also frequently depleted, particularly in
patients receiving heparin, warfarin, or thrombolytics. In
addition to coagulation abnormalities caused by the disease
process and its treatment, both inherited and acquired hyper-
coagulable states (eg, activated protein C resistance), which
are being recognized increasingly, also may coexist and con-
tribute to a perioperative hypercoagulable state.
Hypercoagulability is less common than hypocoagulabil-
ity but has dramatic consequences. Liver disease, either pri-
mary or secondary (eg, congestive hepatopathy), also may
result in anticoagulant factor depletion. Antifibrinolytics (eg,
aprotinin) and desmopressin can result in a hypercoagulable
state, and their use should be evaluated critically. Heparin-
induced thrombocytopenia (HIT) is an increasingly recog-
nized phenomenon in cardiac surgery and may be a
significant contributor to associated morbidity and mortal-
ity. HIT can result in thromboembolic complications with
significant associated morbidity and mortality. Patients with
prior deep venous thrombosis, pulmonary embolism, or
thrombophlebitis are especially prone to recurrent thrombo-
sis, and early anticoagulation should be considered. Patients
undergoing coronary endarterectomy appear to have an
increased risk of graft thrombosis and usually are started on
antiplatelet agents immediately after surgery. Areas of stasis
are always at risk for thrombosis. These include the deep
veins in immobile patients and the left atrium in those with
atrial fibrillation or akinetic endocardium after a myocardial
infarction. The presence of intravascular foreign bodies may
increase the risk of thrombosis. Catheters, patches, valves,
conduits, balloon pumps, and ventricular assist devices may
cause thrombosis and embolism.
In summary, hemostatic and coagulation abnormalities
are very common in cardiac surgical patients and clearly
contribute to associated morbidity and mortality. The etiol-
ogy often is complicated, involving myriad interrelating fac-
tors. Nonetheless, appreciation of these causative factors is
important to optimize care of the cardiac surgical patient.
Clinical Features
A. Chest Tube Output—Chest tube output varies widely
among patients and over time in individuals. It should be
considered in the context of chest x-ray findings, hemody-
namics, previous outputs, surgical findings, and the patient’s
history. Chest tube output is frequently miscalculated as a
result of autotransfusion, multiple tubes and containers, and
in unrecorded intervals such as during patient transport.
These possible errors should be considered, and a repro-
ducible technique of recording and reporting outputs should
be established. Many valid definitions of excessive chest tube
output exist; in the descriptions that follow, output greater
than 200 mL/h for 2 hours is considered significant, whereas
output greater than 400 mL/h for 2 hours is considered
severe. Chest tube output during the first 2 hours following
operation is extremely variable owing to retained blood in
the pleural space and lack of drainage during transport.
Increased drainage can be expected during this period.
Greater than 200 mL/h of drainage after the initial period
may indicate the need for reexploration. The average chest
tube output over 24 hours is approximately 1200 mL in pri-
mary low-risk coronary artery bypass graft patients, but it
may be significantly higher after more complex procedures.
If chest tubes are clotted or do not communicate with the
bleeding site, cardiovascular instability consistent with hypo-
volemia frequently will be the presenting sign. Inadequate
resuscitation of prior or ongoing severe bleeding presents in
a similar fashion.
Patients with excessive drainage from chest tubes
should be thoroughly examined for diffuse oozing from
other sites such as needle punctures, wounds, and nasogas-
tric tubes. A generalized rash and hematuria should alert
one to the possibility of hemolysis owing to a transfusion
reaction. Other findings suggestive of bleeding include
abdominal or groin distention, respiratory compromise
owing to intrapleural blood, low cardiac output owing to
tamponade, and neurologic changes from hypoperfusion
or intracranial hemorrhage.
B. Thrombosis—An uncommon result of a relative hyperco-
agulable state is prosthetic valve thrombosis. Although most
common in patients not adequately anticoagulated chroni-
cally, valve thrombosis can occur at any time in the hospital
course and requires immediate diagnosis. A new murmur
suggesting outflow or inflow obstruction or valvular insuffi-
ciency should be investigated immediately with echocardio-
graphy. Hemodynamic changes may be severe.
Arterial occlusions owing to primary thrombosis or sec-
ondary to embolus may be subtle or dramatic and are quite
common. The arteries at highest risk for primary thrombosis
are recent coronary or peripheral grafts, peripheral cannula-
tion sites, and arteries with preexisting stenosis. An arterial
CARDIOTHORACIC SURGERY
523
embolus will have a similar presentation, but multiple emboli
commonly occur with combined neurologic, coronary, GI,
and peripheral findings. Subtle neurologic changes are sensi-
tive indicators of arterial thrombi or emboli. Findings associ-
ated with arterial occlusion under normal circumstances may
be blurred by perioperative low-flow states, systemic
hypothermia, and preexisting arterial disease.
Venous thrombosis or venous embolism (ie, pulmonary
embolism) is not seen commonly following cardiac surgery
presumably because of systemic anticoagulation during car-
diopulmonary bypass. Since lower extremity edema follow-
ing cardiac surgery is common, owing to increased
extravascular water and venectomy incisions, lower extrem-
ity venous duplex ultrasound examination is critical for diag-
nosis when deep venous thrombosis is suspected. In
congenital disease, systemic and pulmonary venous patches
and conduits are potential sites for thrombosis.
C. Imaging Studies—The routine postoperative chest x-ray
should be reviewed in any patient with suspected bleeding.
Changes in mediastinal width (corrected for technique),
pleural accumulations, and other lesions causing hemody-
namic compromise can be diagnosed rapidly.
D. Laboratory Findings—Activated clotting times (ACTs)
are obtained routinely to determine the adequacy of antico-
agulation during bypass and to assess its reversal by prota-
mine. A normal ACT is between 100 and 120 seconds.
Anticoagulation during bypass increases it to over 400 seconds.
Limited anticoagulation usually falls in the range of
150–250 seconds.
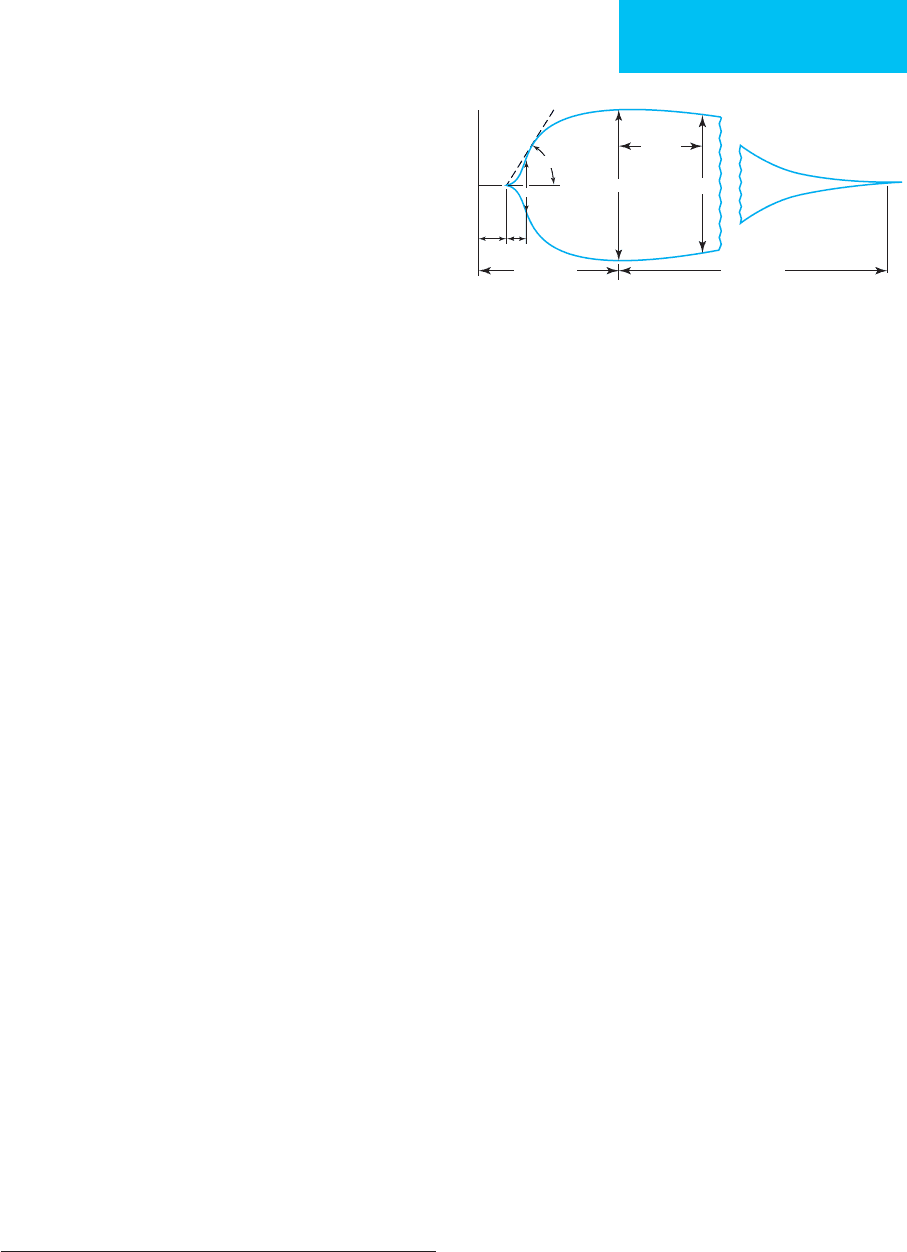
Thromboelastography gives a rapid assessment of the
adequacy of the coagulation cascade and can help to predict
the subgroup of patients whose bleeding is due to an under-
lying disorder. Thromboelastography also can identify
unsuspected hypercoagulable patients. Five parameters are
measured (Figure 23–2). The specific cause of an abnormal
thromboelastogram can be further investigated by routine
coagulation tests (described below).
Platelet counts should be obtained in patients with long
or complex bypass runs and those with excessive bleeding.
However, platelet dysfunction is common perioperatively
despite adequate platelet numbers and is probably the most
common cause of excessive bleeding. Unfortunately, no sim-
ple reproducible test of in vivo platelet function is currently
available. Template bleeding time can provide some infor-
mation but is not recommended on a routine basis. It
should be obtained in patients with a history of bleeding or
refractory postoperative blood loss. A very prolonged tem-
plate bleeding time (>8 minutes) is suggestive of significant
platelet dysfunction.
Routine coagulation tests—international normalized
ratio (INR),
∗
partial thromboplastin time (PTT), thrombin
time (TT), fibrinogen level, and fibrinogen degradation
products (FDPs)—should be obtained in any patient with
severe bleeding who will be receiving factor replacement. The
INR is frequently mildly elevated early postoperatively in all
patients, but an INR greater than 1.7 in a patient with exces-
sive bleeding should be corrected. TT is extremely sensitive
to the presence of heparin, whereas PTT accurately reflects
the level of heparin activity. Fibrinogen deficiency and elevated
FDPs usually indicate excessive fibrinolysis consistent with
consumption coagulopathy. Using the preceding guidelines,
MA
A
60
60 min
FibrinolysisThrombosis
ρ
K
20 mm
α°
Figure 23–2. Quantification of thrombelastograph vari-
ables: r = reaction time (time from sample placement in
the curette until thrombelastograph tracing amplitude
reaches 2 mm [normal range 6–8 min]). This represents
the rate of initial fibrin formation and is related function-
ally to plasma clotting factor and circulating inhibitor
activity (intrinsic coagulation). Prolongation of the r time
may be a result of coagulation factor deficiencies, antico-
agulation (heparin), or severe hypofibrinogenemia.
A small r value may be present in hypercoagulability syn-
dromes. K = clot formation time (normal range 3–6 min),
measured from r time to the point where the amplitude
of the tracing reaches 20 mm. The coagulation time rep-
resents the time taken for a fixed degree of viscoelastic-
ity to be achieved by the forming clot as a result of fibrin
buildup and cross-linking. It is affected by the activity of
the intrinsic clotting factors, fibrinogen, and platelets.
Alpha angle (α°; normal range 50–60°) = angle formed
by the slope of the thrombelastograph tracing from the
r to the K value. It denotes the speed at which solid clot
forms. Decreased values may occur with hypofibrinogene-
mia and thrombocytopenia. Maximum amplitude
(MA; normal range 50–60 mm) = greatest amplitude on
the thrombelastograph trace and is a reflection of the
absolute strength of the fibrin clot. It is a direct function
of the maximum dynamic properties of fibrin and
platelets. Platelet abnormalities, whether qualitative or
quantitative, substantially disturb the MA. A
80
(normal
range = MA – 5 min) = amplitude of the tracing 60 min-
utes after MA is achieved. It is a measure of clot lysis or
retraction. The clot lysis index (CLI; normal range >85%)
is derived as A
80
/MA × 100 (%). It measures the ampli-
tude as a function of time and reflects loss of clot
integrity as a result of lysis. (Reprinted, with permission,
from Mallett SV, Cox DJA: Thromboelastography. Br J
Anaesth 1992;69:307–13.)
∗
The INR is the equivalent of the prothrombin time (PT) corrected
for the wide interlaboratory variation in reagents and PT results.

CHAPTER 23
524
the results of routine coagulation tests are used to direct
therapy at the specific defects outlined below.
To monitor the proper perioperative anticoagulation in
patients with artificial valves and other indications for sys-
temic anticoagulation, the INR is obtained on a daily basis
before and after beginning warfarin therapy. The INR is
superior to the PT because it minimizes interlaboratory
reagent variation. Appropriate levels for given circumstances
are outlined below. In occasional patients at high risk for
thrombosis or those who may need further invasive proce-
dures postoperatively, heparin is started when deemed safe,
and anticoagulation is maintained at a level appropriate for
the relative risks using PTT assays or the ACT. When HIT is
suspected based on clinicopathologic findings, antibodies to
heparin–platelet factor 4 complex should be sought (ie, HIT
antibody test), and heparin administration is stopped
immediately.
Differential Diagnosis
Bleeding is usually easy to diagnose while chest tubes are in
place if they are not clotted and if they communicate with the
bleeding site. If the patient is hypothermic on arrival to the
ICU owing to surgical techniques, then core rewarming over
the first 1–2 hours can be associated with progressive vasodi-
lation, hemodynamic changes, and a fluid requirement that
can be mistaken for ongoing bleeding. Pleural accumulations
of blood or serous fluid are common, and their drainage can
be alarming but benign, as can mediastinal collections.
Hemolysis is rarely confused with significant bleeding but
should be considered. Intrinsic cardiac dysfunction and con-
gestive heart failure may present with hypotension, hemodi-
lution, and congestion similar to hypovolemia or tamponade,
as can any other cause of shock and hypotension.
Arterial thromboembolic complications easily can be
confused with poor perfusion owing to low-output states
and vasoactive drugs. Vascular spasm is particularly common
with mammary artery grafts and can mimic occlusion.
Spasm of peripheral vessels may be observed. Cholesterol
emboli from an atherosclerotic aortic wall are probably
much more common than thromboemboli owing to dissem-
inated clotting. Cholesterol emboli usually present immedi-
ately postoperatively and are frequently multiple.
Treatment
A. Bleeding—If postoperative bleeding is apparent, one
must immediately ensure the availability of adequate sup-
plies of blood products. Careful fluid balances are crucial and
should be reported in a reproducible fashion at appropriate
intervals. Patients should be rapidly stratified according to
the level of bleeding. Bleeding less than 200 mL/h frequently
stops without additional therapy as the effects of cardiopul-
monary bypass and anticoagulation resolve. Bleeding greater
than 300 mL/h only rarely resolves spontaneously. Severe
bleeding (>400 mL/h) frequently requires operation. If the
patient is hemodynamically stable, evaluation for a nonsurgical
cause of bleeding may be undertaken provided that prepara-
tion for mediastinal exploration is begun and sufficient
blood products are available.
If patients can be stabilized and bleeding is less than mas-
sive, a check for residual heparin can be performed with an
ACT in a few minutes. Protamine then should be adminis-
tered if the ACT is elevated above baseline. A platelet count
should be checked, although an adequate number does not
equate with adequate function. Thromboelastography can
provide an overview of the level of coagulation, and if it is
normal, one should suspect a surgical cause for the bleeding.
Routine coagulation tests can be obtained to guide specific
factor therapy and to rule out ongoing fibrinolysis.
B. Transfusion—Transfusion therapy is guided by the
hemostatic laboratory profile, which should be easily and
rapidly obtained. Usually, platelets are the initial therapy
because they augment platelet function, supply fresh-
frozen plasma, and provide a source of fibrinogen with the
same number of donor exposures. If platelet concentrate
fails to correct the deficit or severe factor deficiencies are
documented, an elevated INR is usually treated with fresh-
frozen plasma, and a diminished fibrinogen is treated with
cryoprecipitate.
C. Other Agents—Antifibrinolytics such as aminocaproic
acid (4–5 g in 250 mL of diluent over 1 hour intravenously,
followed by 1 g/h as a continuous infusion) can be added if
fibrinolysis is significant; however, most agents should be
given preoperatively for full effect. Patients felt to be at high
risk for bleeding should be treated prophylactically.
Desmopressin acetate (0.3 μg/kg intravenously over 15–30
minutes) is particularly effective in the treatment of patients
with platelet deficiency owing to uremia or von Willebrand’s
disease, but it may cause increased graft thrombosis.
Conjugated estrogens and serine protease inhibitors also may
be helpful in treatment of uremic bleeding, although consid-
eration always must be given to the risks and benefits of these
pharmacologic therapies. Recently, recombinant factor V11a
has become available to assist with hemorrhagic complica-
tions following cardiac surgery. Although it has been used
with success in both the adult and the pediatric population,
an evidence-based approach guiding its use is not yet avail-
able. Similar to published reports, we have found it useful in
the setting of continuing hemorrhage and coagulopathy
despite ongoing transfusion of usual products in the absence
of surgical bleeding.
If correction of the clotting mechanism does not stop the
hemorrhage, immediate surgical exploration is mandatory
irrespective of the patient’s hemodynamic status.
D. Thrombosis—Clinical (eg, chest pain and hemodynamic
changes) and electrocardiographic (eg, ST-segment changes)
evidence for coronary graft thrombosis is not infrequently
due to graft spasm, particularly with arterial conduits (mam-
mary arteries). In unresolved cases, echocardiography should
be obtained to evaluate wall motion in the suspect arterial
CARDIOTHORACIC SURGERY
525
territory. Antispasmodics should be instituted (eg, calcium
channel blocking agents, nitroglycerin, or phosphodiesterase
inhibitors) while diagnostic evaluation continues. Many cen-
ters give antispasmodics (eg, calcium channel blockers) pro-
phylactically in an attempt to avoid spasm. If wall motion
abnormalities are documented and persist with antispas-
modics, angiography may be indicated to confirm graft
patency. Reexploration of grafts then is considered on an
individual basis.
Peripheral thromboembolism is not uncommon in open-
heart surgery and occurs in the presence of a left ventricular
thrombus, preexisting vascular disease, and injuries from
prior angiography. Additionally, peripheral emboli and
thrombosis are frequent in patients with intravascular pros-
theses or devices, particularly intraaortic balloon pumps and
prosthetic valves. All unnecessary foreign bodies should be
removed as soon as possible. Patients should be stratified
according to risk of thrombosis, and those who subsequently
have a thromboembolism despite one level of anticoagulation
should be increased to the next level of anticoagulation, and a
thorough evaluation of why they failed should be undertaken.
Patients with a high risk of thrombosis, delayed onset of long-
acting anticoagulants (eg, warfarin), or evidence of current
thromboembolism should be treated with rapid-onset anti-
coagulants (eg, heparin) with appropriate consideration of
the risk of bleeding in the perioperative period.
All patients with unexplained or recurrent thrombotic
episodes should be evaluated for acquired or inherited
thrombophilias, including (at least) resistance to activated
protein C (eg, factor V Leiden or HR
2
haplotype), heterozy-
gosity or homozygosity for factor V Leiden or G20210A
prothrombin mutation, hyperhomocysteinemia, factor VIII
levels, and the presence of lupus anticoagulant. If HIT is
suspected, all heparin should be eliminated. If ongoing
anticoagulation is needed, then direct thrombin inhibitors
or platelet inhibitors can be used until warfarin levels are
adequate. Antithrombin III deficiency can be treated tem-
porarily with fresh-frozen plasma and long term with war-
farin. The treatment of protein A, C, or S deficiency is
approached on an individual basis. Hyperhomocysteinemia
is treated indefinitely with folic acid, supplemented with
vitamins B
6
and B
12
if homocysteine levels do not normal-
ize on folic acid alone.
Doty JR et al: Atheroembolism in cardiac surgery. Ann Thorac
Surg 2003;75:1221–6. [PMID: 12683567]
Greinacher A: The use of direct thrombin inhibitors in cardiovas-
cular surgery patients with heparin-induced thrombocytope-
nia. Semin Thromb Hemost 2004;30:315–27. [PMID:
15282654]
Karkouti K et al: Recombinant factor VIIa for intractable blood
loss after cardiac surgery: A propensity score-matched case-
control analysis. Transfusion 2005;45:26–34. [PMID: 15647015]
Levy JH: Pharmacologic preservation of the hemostatic system
during cardiac surgery. Ann Thorac Surg 2001;72:S1814–20.
[PMID: 11722115]
Seligsohn U, Lubetsky A: Genetic susceptibility to venous throm-
bosis. N Engl J Med 2001;344:1222–31. [PMID: 11309638]
Warkentin TE, Greinacher A: Heparin-induced thrombocytope-
nia: Recognition, treatment, and prevention. The Seventh ACCP
Conference on Antithrombotic and Thrombotic Therapy. Chest
2004;126:S311–37.
Cardiopulmonary Bypass, Hypothermia,
Circulatory Arrest, & Ventricular Assistance
ESSENTIALS OF DIAGNOSIS
Decreased peripheral perfusion.
Altered end-organ function.
Hypothermia.
Coagulopathy.
Hemolysis.
Edema, localized or generalized.
General Considerations
More than 30 years ago, the introduction of cardiopul-
monary bypass—and therefore the ability to interrupt and
alter the circulation locally and systemically—revolutionized
the approach to cardiothoracic and other major surgery of
vascular structures. Continued advances in technique have
made cardiopulmonary bypass well tolerated, but untoward
effects still occur, particularly at the extremes of age. Despite
the recent popularity of minimally invasive and off-pump
techniques in cardiac surgery, full cardiopulmonary bypass is
still used for the majority of cardiac surgical procedures in
the United States. An understanding of the pitfalls of car-
diopulmonary bypass are crucial to realizing its benefits.
Both total and partial bypass circuits are used on a rou-
tine basis and are primed with crystalloid, colloid, or blood if
estimated hemodilution will be severe. Total cardiopul-
monary bypass begins with drainage of systemic venous
blood into a reservoir via a venous cannula. A separate
pump-driven cardiotomy suction device can be added to
return shed blood from the operative field to the same reser-
voir. Blood then is actively pumped through an
oxygenator/heat exchanger and back to the systemic circula-
tion via the arterial cannula. A number of additional special-
ized circuits deliver cardioplegia, provide pulmonary venous
and collateral drainage (vents), or perfuse localized areas.
Arterial and venous cannulas are usually placed in the
ascending aorta and right atrium, but a number of locations
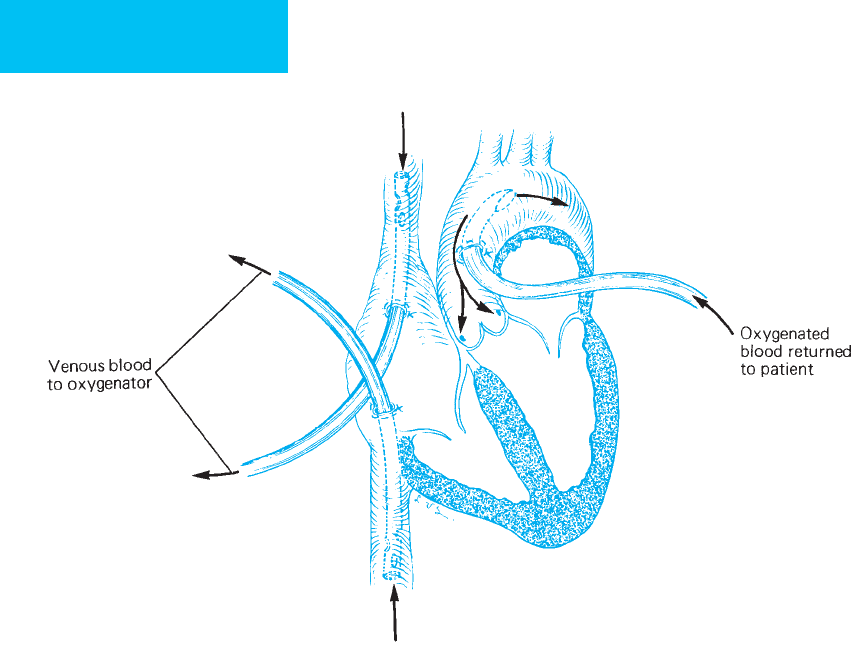
are used on an individual basis (Figure 23–3). Partial bypass
circuits include venovenous bypass (usually with oxygenator),
left atrioarterial or right atriopulmonary bypass or ventric-
ular assist (usually without oxygenator), and simple arte-
rioarterial and venovenous shunts, with or without pumps
CHAPTER 23
526
or oxygenators. Severe adverse effects of cardiopulmonary
bypass strictly owing to the circuit itself are rare but include
massive air embolism, aortic dissection from cannulas or
clamps, general or localized venous congestion from kinked
or misplaced return lines; severe hypoxia from oxygenator
dysfunction; and a number of unusual but significant events.
One or more lesser effects of the cardiopulmonary bypass cir-
cuit are nearly universal. Microscopic air, platelet, and cho-
lesterol emboli; direct blood cell trauma; and endothelial
injury may occur secondary to mechanical pump or cannu-
lation injury.
Blood contact with the artificial surfaces of the circuit
causes a variety of undesirable effects, including systemic
inflammation (ie, elaboration of cytokines and leukocyte
activation), complement activation, coagulation abnormali-
ties, and endothelial cell activation. Indeed, these changes
contribute to the morbidity and mortality of cardiac sur-
gery. Full anticoagulation with heparin (300 units/kg) is
required in all circuits to prevent widespread coagulation,
although lower anticoagulation protocols may prove equally
efficacious as the biocompatibility of the circuits improves
(ie, heparin bonding). Partial-bypass circuits—and some
full-bypass circuits with heparin-bonded components—
frequently can be maintained with little or no systemic anti-
coagulation depending on flow, component surfaces, and
the effects of the pump, filters, and special devices. Circuit
priming solutions and added fluids cause hemodilution,
which is frequently helpful in diminishing blood cell loss
but may be excessive in patients with low blood volumes. In
selected patients with generous prebypass blood cell vol-
umes, whole blood or blood components may be removed
prior to bypass for retransfusion postoperatively. This
restores coagulation factor activity and reduces homologous
blood product utilization.
Perfusion during total cardiopulmonary bypass is almost
always nonpulsatile, and flow is maintained at a level to
ensure adequate end-organ perfusion based on metabolic
demands. Perfusion during partial bypass or ventricular sup-
port may be pulsatile or nonpulsatile depending on the cir-
cuit and device. Flows in these local circuits are determined
by arterial resistances in the native perfused and mechani-
cally perfused beds, left- and right-sided pressures during
ventricular support, inflow limitations, technical considera-
tions, and device capabilities. Measured pump flows are
felt to be more crucial than blood pressure in patients
without vascular stenoses. Typical flows at normothermia
Figure 23–3. Cannulation sites used commonly in connecting the extracorporeal circuit. Venous blood is drained
through tubes introduced into both venae cavae. Oxygenated blood is returned to the arterial system through a tube in
the aorta. (Reproduced, with permission, from Way LW (ed), Current Surgical Diagnosis & Treatment, 10th ed. Originally
published by Appleton & Lange. Copyright © 1991 by The McGraw-Hill Companies, Inc.)
