Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


CARDIAC PROBLEMS IN CRITICAL CARE
487
follow. Class Ic and class III antiarrhythmic agents such as
flecainide and amiodarone also can be helpful for medical
management of patients with bypass tracts. The develop-
ment of transvenous radiofrequency ablation of bypass
tracts obviates the need for long-term pharmacologic ther-
apy for most patients and has largely replaced surgical abla-
tion. AV nodal reentry arrhythmias without bypass tracts
and atrial flutter are also treated effectively with transvenous
ablation techniques.
Atrial Tachycardia
Atrial tachycardia is an automatic rhythm (repetitive single
focus) and does not depend on the AV node and reentry to
continue. Atrial tachycardia is less common than AV nodal
reentrant rhythms and usually has a regular ventricular rate
of 140–220 beats/min, although AV block may cause the ven-
tricular rate to be considerably slower. The P waves have uni-
form morphology and relationship to the QRS complex.
Although calcium channel blockers, beta-blockers, and
digoxin usually will not terminate these atrial arrhythmias,
they will decrease the ventricular response rate by slowing AV
nodal conduction and therefore can effectively improve
hemodynamics. Slowing of the ventricular rate may be help-
ful in identifying underlying atrial activity on the ECG so
that a distinction can be made between atrial tachycardia, AV
nodal reentry, atrial flutter, and atrial fibrillation. After the
ventricular rate is controlled, conversion to sinus rhythm can
be attempted with class Ia, Ic, or III antiarrhythmic agents or
electrical cardioversion. Radiofrequency ablation can be con-
sidered in selected patients when the focus of the arrhythmia
can be localized and the arrhythmia occurs frequently.
Atrial Flutter
Atrial flutter is a macroreentrant arrhythmia and in many
ways behaves like atrial tachycardia. Atrial flutter always
should be considered when a patient presents with supraven-
tricular tachycardia with a rate of approximately 150
beats/min. The atrial flutter rate usually is approximately 300
beats/min, but because of normal delays in conduction
through the AV node, the ventricular response rate is slower
than the atrial rate, with only every other (2:1 AV block) or
every third (3:1 AV block) beat effectively conducted to the
ventricle. Increasing the degree of AV nodal block with drugs
(adenosine) or by carotid massage brings out the underlying
flutter waves on the ECG and establishes the diagnosis.
Drugs that increase AV nodal block usually—though not
always—can control the ventricular rate at rest, but conver-
sion to sinus rhythm usually requires either antiarrhythmic
drugs or, more commonly, electrical cardioversion. Ibutilide,
sotalol, or amiodarone can be tried. In general, atrial flutter
is more resistant to pharmacologic conversion than AV nodal
reentrant tachycardia. However, unlike atrial fibrillation and
atrial tachycardia, atrial flutter can be converted using fairly
small amounts of electrical energy, usually less than 50 J.
Atrial flutter also can be converted to sinus rhythm with
overdrive pacing using a transvenous right atrial pacemaker
electrode or an esophageal pacemaker electrode. Atrial flutter
is a rhythm that is amenable to radiofrequency ablation, with
success rates approaching those for other supraventricular
tachycardias. Given the difficulty of treating atrial flutter and
converting it with medical therapy, ablation provides effec-
tive long-term treatment.
A subset of patients with atrial tachyarrhythmia may
develop bradycardia after electrical cardioversion or drug
therapy. Patients with tachy-brady syndrome pose a particu-
lar problem in designing therapy and may require temporary
pacing if cardioversion is attempted. They also may require a
permanent pacemaker to generate an adequate ventricular
rate when receiving necessary drug therapy to control the
tachyarrhythmias.
Atrial Fibrillation
Atrial fibrillation is a chaotic arrhythmia probably owing to
multiple reentry circuits within the atria that results in loss
of atrial contraction and an irregular, often rapid ventricu-
lar rate. Because of the rapid but unpredictable bombard-
ment of the AV node by the atrial fibrillatory impulses and
variable penetration of the impulses through the AV node to
the ventricle, the ventricular rate is highly variable. An irreg-
ularly irregular ventricular rate with the absence of P waves
is the hallmark of atrial fibrillation and makes it easily dis-
tinguishable from the other more organized and regular
atrial arrhythmias. Patients with acute atrial fibrillation may
develop hypotension, myocardial ischemia, decreased perfu-
sion of vital organs, and acute congestive heart failure.
Those with chronic atrial fibrillation have an increased risk
of atrial mural thrombus formation, usually in the left atrial
appendage, with the risk of subsequent systemic emboliza-
tion. Atrial fibrillation is very common in patients with
mitral stenosis, lung disease, sepsis, and hyperthyroidism, as
well as in any form of heart disease or after cardiac surgery.
Therapy is directed at slowing the ventricular rate initially,
followed, in appropriate patients, by conversion of atrial fibril-
lation to sinus rhythm. Slowing of the ventricular rate can be
achieved with β-adrenergic blockers, calcium channel block-
ers, or digoxin, all of which increase the AV nodal refractory
period. Control of the ventricular rate is particularly impor-
tant in patients with ischemia and chest pain, congestive heart
failure, mitral stenosis, and hypotension. Intravenous diltiazem
can be given at a dose of 5–10 mg followed by a continuous infu-
sion. Alternatively, intravenous digoxin is effective when given at
a dosage of 0.125–0.25 mg every 4–6 hours until the desired rate
is achieved or until 1–1.5 mg has been given. In some patients,
combinations of these drugs are necessary, but excessive AV
nodal blockade should be avoided. The goal of rate control is to
lower the ventricular rate to about 80–100 beats/min.
Ibutilide, an intravenous short-acting class III antiar-
rhythmic agent, can be used to convert atrial fibrillation to
normal sinus rhythm. When given before direct current (DC)

CHAPTER 21
488
cardioversion, it increases the likelihood of success. It has
proarrhythmic effects, including torsade de pointes, that
necessitate close monitoring during its infusion and for sev-
eral hours thereafter. Intravenous magnesium is given fre-
quently prior to ibutilide to reduce this risk. Combined use
with amiodarone may increase heart block or arrhythmias.
Sotalol, a class III antiarrhythmic with β-adrenergic blocking
properties, also can be used. These agents can be continued to
help maintain normal sinus rhythm. Long-term use of sotalol
and amiodarone, however, may result in bradycardia, which
may be prolonged with amiodarone because of the 32-day
half-life.
Today, conversion to sinus rhythm is only rarely
attempted using class Ia antiarrhythmic drugs such as
quinidine or procainamide. Before administering class Ia
drugs, the ventricular response rate must be well controlled
because acceleration of the ventricular rate may occur when
these drugs are given. This problem is also seen with atrial
flutter and atrial tachycardia. It also should be noted that
the administration of quinidine may result in nearly a dou-
bling of the serum digoxin level. Thus, a patient with atrial
fibrillation whose ventricular rate is controlled with
digoxin and who has no evidence of digoxin toxicity may
develop digoxin toxicity when quinidine is given.
Procainamide therefore may be a better short-term choice
in the critically ill patient receiving digoxin. Neither quini-
dine nor procainamide is well tolerated as a long-term oral
medication, and both also have significant proarrhythmic
effects. They are being replaced by the newer class agents
Ic agents flecainide and propafenone, which can be used
safely in patients without coronary disease, left ventricular
hypertrophy, or left ventricular dysfunction, and by the
class III agent dofetilide. The latter is safe in patients with
left ventricular dysfunction but does require initial in-
patient monitoring for excessive QT-interval prolongation.
Sotalol is also effective, but it too carries a risk of QT-
interval prolongation and torsades de pointes, necessitating
initial monitoring for safest administration. Amiodarone is
probably the most effective medication for maintaining
sinus rhythm, but its myriad of potentially dangerous side
effects indicate the need for caution in using it to treat an
arrhythmia that is not lethal.
Electrical cardioversion of atrial fibrillation to sinus
rhythm is effective at least acutely but generally requires higher
amounts of electrical energy than other atrial arrhythmias,
often more than 200 J. Newer biphasic defibrillators have a
higher success rate and require less energy. In a hemodynam-
ically unstable patient with rapid atrial fibrillation, electrical
cardioversion is the appropriate first treatment. Patients with
acute myocardial infarction, hypertrophic cardiomyopathy,
severe systolic left ventricular dysfunction, critical aortic
stenosis, or recent major surgery are patients who would
benefit from rapid restoration of normal sinus rhythm but
who might not tolerate the hypotensive episode or further
hypotension caused by the antiarrhythmic agents used to
chemically treat the atrial fibrillation.
Atrial fibrillation poses a risk of embolization because the
noncontracting atria are potential sites for thrombus forma-
tion, and the risk of embolization increases with cardiover-
sion. The greatest risk of embolization is associated with
atrial enlargement and atrial fibrillation of long duration.
Therefore, patients who have had atrial fibrillation for more
than 2–3 days should be anticoagulated for 3–4 weeks before
conversion is attempted. Alternatively, it has been shown to
be safe to undertake cardioversion if a transesophageal
echocardiogram performed while the patient is on anticoag-
ulation demonstrates no atrial thrombi and anticoagulation
is continued for 4 weeks after cardioversion. This approach
allows fairly prompt cardioversion of patients in whom the
duration of atrial fibrillation is unknown and avoids leaving
the patient in atrial fibrillation for several additional weeks.
Patients without mitral stenosis who develop acute atrial fib-
rillation can be cardioverted within the first few days without
anticoagulation.
Patients with atrial fibrillation who cannot be converted
to sinus rhythm are managed by controlling their ventricular
rates. Anticoagulation with warfarin should be considered
in patients with chronic atrial fibrillation because of the
increased frequency of embolic strokes even in the absence
of intrinsic heart disease. Patients at higher risk for embolic
events include the elderly; those with ischemic, valvular, or
hypertensive heart disease; diabetics; and patients with a
history of stroke or TIA. Aspirin may be an alternative in
otherwise healthy younger patients with lone atrial fibrilla-
tion or in those with contraindications to anticoagulation
with warfarin.
Multifocal Atrial Tachycardia
Multifocal atrial tachycardia is an atrial arrhythmia that can
be confused with atrial fibrillation, but it is managed quite
differently. This arrhythmia generally is seen in patients with
severe lung disease and respiratory failure. The hallmark of
this atrial tachycardia is an irregular ventricular rate but with
multiple atrial foci (P waves with different morphologic
appearances). Atrial fibrillation also has an irregular ventric-
ular response, but P waves are absent.
Treatment of the underlying lung disease and respiratory
failure usually corrects the arrhythmia. Once the precipitat-
ing pulmonary process resolves, sinus rhythm often returns.
Multifocal atrial tachycardia responds poorly to digoxin,
with neither slowing of the ventricular rate nor conversion to
sinus rhythm. Verapamil may be effective sometimes in slow-
ing ventricular rate and decreasing the frequency of ectopic
atrial beats.
VENTRICULAR ARRHYTHMIAS
Management of ventricular arrhythmias in the ICU is often
more complicated than management of atrial arrhythmias
because the treatment is sometimes worse than the disease,
and because these arrhythmias may be poorly tolerated by

CARDIAC PROBLEMS IN CRITICAL CARE
489
critically ill patients. Rapid ventricular arrhythmias (eg, ven-
tricular tachycardia) require immediate treatment, particu-
larly in patients who have severe underlying cardiac disease.
Almost all antiarrhythmic agents used for the treatment of
ventricular arrhythmias may facilitate arrhythmias (proar-
rhythmic effect) and have a variety of other unpleasant or
life-threatening side effects. Therefore, treatment of ventric-
ular arrhythmias should be limited to those known to cause
hemodynamic compromise or those that occur in the setting
of underlying myocardial disease. In general, the more malig-
nant the arrhythmia appears—that is, the more rapid the
rate, the longer the duration of the arrhythmia, the more fre-
quent the occurrence, and the greater the hemodynamic
compromise (eg, hypotension or syncope)—the more
important it is to treat. In addition, the presence of ventricu-
lar tachycardia always should raise the question of ischemia
with underlying coronary artery disease.
The nuances of evaluation and management of sudden
cardiac death and nonsustained and sustained ventricular
tachycardia in the presence or absence of ventricular dys-
function are beyond the scope of this text. However, develop-
ment of significant ventricular arrhythmia justifies and
necessitates consultation with an electrophysiologist to
determine whether medical therapy is indicated, to assess
drug efficacy, and to consider more definitive treatment,
including implantable defibrillators and transvenous abla-
tion. The development of sudden cardiac death and sus-
tained ventricular tachycardia in patients without known
cardiac disease should result in a careful search for cardiac
disease, particularly ischemia. Cardiac catheterization with
coronary arteriography may be indicated.
Ventricular Ectopy (Premature Ventricular
Contractions)
Treatment of asymptomatic ventricular ectopy (ie, premature
ventricular contractions [PVCs]) is usually not indicated, par-
ticularly in light of many studies demonstrating both the lack
of efficacy and potential catastrophic side effects resulting
from treatment of non-life-threatening ventricular arrhyth-
mias in certain populations. Ventricular ectopy is often benign
and requires no treatment. However, development of PVCs
may be a clue to the presence of digoxin toxicity or electrolyte
or other metabolic imbalance—particularly hypokalemia but
also hypomagnesemia, alkalosis, hyperkalemia, hypoxemia,
and ischemia. Correcting these abnormalities often eliminates
the PVCs. High catecholamine states, including treatment in
an ICU, recent surgery, and prolonged pain, can result in
PVCs. Beta-adrenergic blockade may help to reduce the fre-
quency of PVCs in these patients.
Unifocal PVCs, bigeminy, and couplets (paired PVCs)
usually do not require treatment even in a patient with
myocardial ischemia. Antiarrhythmic therapy should be
reserved for patients with sustained or nonsustained ventric-
ular tachycardia accompanied by hemodynamic compro-
mise. However, the indications for short-term therapy of
PVCs are less rigorous than the indications for long-term
antiarrhythmic treatment, and short-term therapy to sup-
press PVCs may be appropriate while a patient is medically
unstable in the ICU. In patients with congestive heart failure
and ventricular ectopy, PVCs may not generate an adequate
stroke volume, and frequent PVCs may result in a reduced
cardiac output. Suppression of the ectopy therefore may be
indicated to increase cardiac output. This goal often can be
achieved with administration of intravenous lidocaine.
Procainamide and quinidine are alternatives that are essen-
tially no longer used. Their long- and short-term toxicity
generally outweighs any perceived benefit.
Lidocaine toxicity is seen most often in elderly patients
and those with decreased liver function or congestive heart
failure, and the proarrhythmic effects of lidocaine are mini-
mal. Both quinidine and procainamide can cause torsade de
pointes and worsening of ventricular arrhythmias; use of
these agents calls for close monitoring and careful consider-
ation of indications for therapy. The use of beta-blockers,
particularly in a patient who has evidence of a high-
catecholamine state (eg, tachycardia, agitation, and hyper-
tension), may result in a reduction in PVCs, heart rate, and
blood pressure.
Ventricular Tachycardia
Ventricular tachycardia is defined as three or more consecu-
tive ventricular beats and is most commonly a reentrant type
of tachycardia. Nonsustained ventricular tachycardia lasts for
less than 30 seconds and terminates spontaneously, in con-
trast to sustained ventricular tachycardia. Myocardial
ischemia is the most common situation in which ventricular
tachycardia is seen, but valvular heart disease, myocarditis,
and other forms of heart disease also predispose to this
arrhythmia. Patients with prolonged QT intervals with or
without administration of quinidine or another drug that
prolongs the QT interval (such as a tricyclic antidepressant)
may have a form of ventricular tachycardia known as torsade
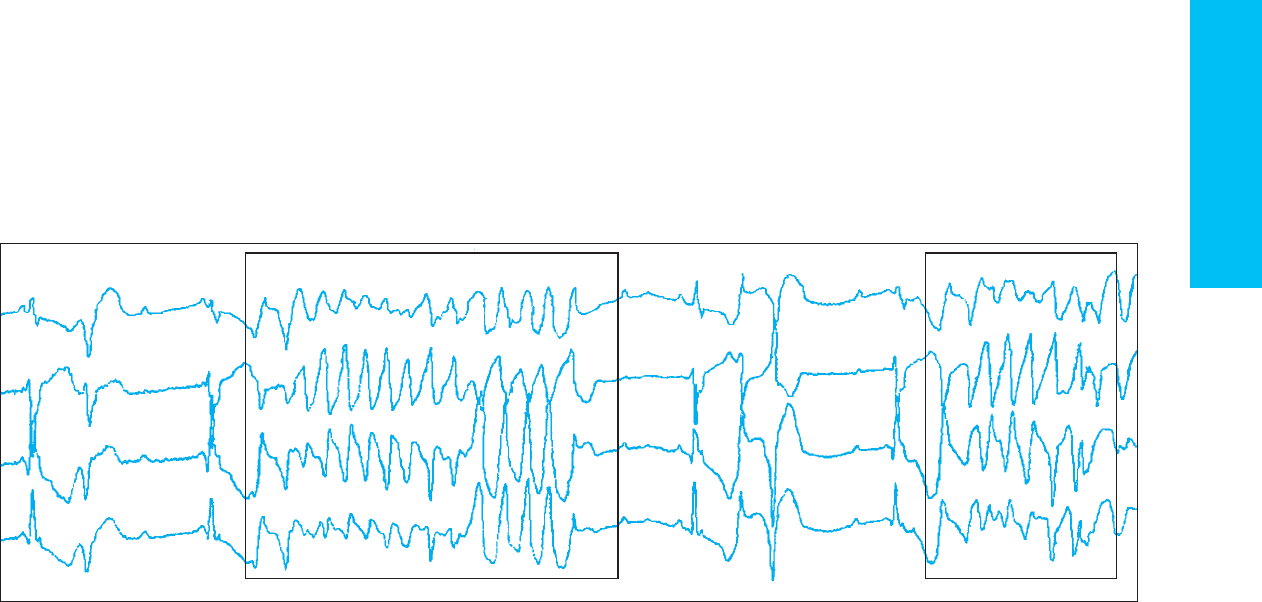
de pointes. This arrhythmia presents as ventricular tachycar-
dia marked by a pattern of multiform ventricular beats with
the axis shifting with each beat, yielding an undulating QRS
pattern (Figure 21–6). Rapid ventricular tachycardia often
deteriorates into ventricular fibrillation.
In the presence of underlying cardiac disease, ventricular
tachycardia often deserves therapy. Nonsustained ventricular
tachycardia in the setting of acute ischemia or infarction
justifies antiarrhythmic suppression at least over the first
24–48 hours. A similar arrhythmia in a healthy 20-year-old
postoperative patient might be observed without therapy, or
the patient might be given a β-adrenergic blocker to decrease
the effects of excess catecholamines. Electrolyte imbalances
(particularly hypokalemia, hypomagnesemia, and alkalosis)
and hypoxemia increase ventricular irritability and therefore
may predispose to ventricular arrhythmias. In addition,
there is evidence that magnesium administration may
decrease or prevent ventricular arrhythmias even in the
CHAPTER 21
490
Figure 21–6. Four-channel ECG demonstrating torsade de pointes. This multiform ventricular tachycardia changes its axis with changing height and
direction of the QRS complex shifting over the episode. The arrhythmia was initiated by a premature ventricular contraction during a period of high-
degree heart block. Note that not all the P waves are conducted to the ventricle and that the ventricular rate is quite slow.
CARDIAC PROBLEMS IN CRITICAL CARE
491
absence of hypomagnesemia. Digoxin toxicity, alcohol with-
drawal, and ischemia also must be considered in ICU
patients who develop ventricular arrhythmias.
As a general rule, patients with sustained ventricular
tachycardia that produces hemodynamic instability with
syncope, obtundation, hypotension, congestive heart failure,
or chest pain should be electrically cardioverted immediately
using 100–200 J. Persistent myocardial ischemia or hypoten-
sion that occurs while trying various pharmacologic agents
puts the patient at risk of further deterioration and ventric-
ular fibrillation. As the ventricle becomes more ischemic, sta-
bilization becomes more difficult, and intractable ventricular
fibrillation and death may ensue.
Pharmacologic conversion of ventricular tachycardia can
be used in patients with ventricular tachycardia who are tol-
erating this rhythm without chest pain, hypotension, or con-
gestive heart failure. Initial therapy is lidocaine administered
by an intravenous bolus of 1–2 mg/kg, followed by an intra-
venous infusion of 1–4 mg/min. Procainamide can be given
intravenously as a loading dose (500–1000 mg given at a rate of
50 mg/min), followed by an intravenous infusion (2–4 mg/min)
as an alternative if lidocaine fails. Intravenous amiodarone is an
effective alternative that is being used more frequently, and it is
now recommended as the initial antiarrhythmic medication for
refractory ventricular arrhythmia in Advanced Cardiac Life
Support (ACLS). Amiodarone has a fairly complicated load-
ing schedule: 150 mg is given over 10 minutes followed by 1
mg/min for 6 hours and then 0.5 mg/min for 18 hours.
Loading of amiodarone can be repeated if ventricular tachy-
cardia recurs. Bretylium, another class III antiarrhythmic
agent, is no longer available. Overdrive pacing to suppress
ventricular arrhythmias is helpful in occasional patients.
Patients with torsade de pointes or polymorphic ventricu-
lar tachycardia with a long QT interval are treated differently.
Antiarrhythmic drugs that prolong the QT interval should
not be given including class Ia (eg, quinidine or pro-
cainamide), class Ic (eg, flecainide or propafenone), and some
class III agents (eg, amiodarone or sotalol). These drugs
should be stopped if the arrhythmia occurs during their use.
Isoproterenol or ventricular overdrive pacing may be helpful
in suppressing the initiating ectopic beats and shortening the
QT interval; this is unlike other ventricular arrhythmias in
which β-adrenergic agonists may exacerbate the arrhythmia.
Indications for implantable defibrillators in the treatment
of ventricular arrhythmias are changing rapidly. They are not
generally placed in the acute setting for the management of
ICU-related ventricular arrhythmias. Patients with reduced
left ventricular function after myocardial infarction or owing
to cardiomyopathy, patients with complex ventricular
arrhythmias and depressed left ventricular function, and
patients at high risk for sudden arrhythmic death owing to
underlying heart disease are appropriate candidates. The
presence of an implantable cardiac defibrillator in an ICU
patient can complicate management of the arrhythmias,
including pacemaker-mediated tachycardia; inappropriate
shocks in an ICU setting in the presence of a variety of atrial
tachycardias could lead to inappropriate therapies. In an
emergency when there are incessant inappropriate
implantable cardiac defibrillator shocks, placement of a mag-
net over the implantable cardiac defibrillator usually will
inhibit the defibrillator from delivering therapy. Patients
with implantable cardiac defibrillators and increasing
arrhythmias in the ICU should have their device interrogated
by an electrophysiologist to determine the extent and type of
arrhythmia and to potentially modify the programming of
the device to better control the rhythm.
HEART BLOCK
Heart block occurs when one or more segments of the car-
diac conduction system transmit impulses at an inadequate
rate. Heart block can be divided into (1) sinus node prob-
lems including sinus arrest, sinus node Wenckebach, and
some forms of sinus bradycardia; (2) AV nodal block includ-
ing first-degree AV block, and second-degree Mobitz type I
block (Wenckebach); and (3) infranodal block including
bundle branch block, Mobitz type II AV block, and third-
degree heart block. Both Mobitz type II block and third-
degree heart block also can occur in the AV node, but they
are more commonly manifestations of infranodal disease. In
addition to degeneration caused by aging of the conduction
system, heart block can be induced iatrogenically with med-
ications or may be due to myocardial ischemia or infarction;
metabolic abnormalities; enhanced vagal tone from tracheal
irritation, suction, or intubation; abdominal distention; or
severe vomiting. Heart block sometimes can be confused
with other cardiac dysrhythmias.
It is important to determine whether the arrhythmia is
due to an inadequate impulse formation or poor conduction
from the atrium to the ventricles (default) or to a fast nodal
or ventricular rate relative to the atrial rate (usurpation).
Accelerated idioventricular rhythms, junctional tachycardia,
and isorhythmic dissociation are not due to heart block but
rather result from an acceleration of AV nodal or infranodal
pacemakers. Since there is no heart block, speeding of the
atrial rate will entrain the ventricles normally.
Heart block is managed differently depending on whether
the ventricular rate is adequate or there is clinically significant
bradycardia. Treatment of heart block should focus on several
issues: (1) identification of reversible causes, (2) the hemody-
namic consequences of the arrhythmia, (3) the potential to
progress or recur, and (4) the patient’s underlying medical
condition. For example, the management of patients with
second-degree heart block secondary to the combined use of
a calcium blocker and a β-adrenergic blocker for hyperten-
sion is different from management of a similar degree of heart
block owing to intrinsic conduction system disease. Time, cal-
cium, and perhaps isoproterenol may obviate the need for
even temporary pacing support in the former, but permanent
pacing probably will be required for the latter.
External cardiac pacing may be used for short periods of
time, permitting stabilization with adequate ventricular rates

CHAPTER 21
492
and decreasing the urgency of the need for temporary trans-
venous pacing. Temporary transvenous pacing should be
used in patients who are hemodynamically compromised by
heart block. Indications for both temporary and permanent
pacing in coronary artery disease are discussed in Chapter 22.
Heart Block & Conduction Disturbances
Sinus Bradyarrhythmias
The name sick sinus syndrome has been given to a variety of
bradyarrhythmias arising in the sinus node including sinus
arrest and symptomatic sinus bradycardia. When seen in
association with alternating bradycardia and supraventricu-
lar tachycardia, the term tachy-brady syndrome is sometimes
used. Many patients with sinus bradyarrhythmias have
intrinsic heart disease, but digoxin, beta-blockers, calcium
channel blockers, and other drugs may precipitate bradycar-
dia with syncope, hypotension, and heart failure. In patients
with drug-related bradyarrhythmias, discontinuation of the
drug is necessary; in others with symptomatic bradycardia, a
pacemaker may be necessary. As described earlier, treatment
of supraventricular tachycardia associated with alternating
bradycardia may require drug treatment of the tachycardia
(eg, digoxin and beta-blockers) and a pacemaker (because of
drug-induced bradycardia).
AV Block
Temporary or permanent alteration of conduction through
the AV node or bundle of His is classified as AV block.
Patients with prolonged PR intervals (>210 ms) have first-
degree AV block; this can be due to intrinsic conduction sys-
tem disease, increased vagal tone, or more commonly,
cardiac medications or ischemia. First-degree AV block is
usually benign. Second-degree AV block is diagnosed when
atrial impulses are conducted intermittently through to the
ventricles. In Mobitz type I second-degree AV block
(Wenckebach block), the PR interval lengthens on successive
beats prior to a nonconducted atrial beat (P wave without a
following QRS complex). The electrocardiographic pattern
that emerges is grouped beating in which the number of ven-
tricular complexes is equal to the number of P waves
minus 1. This rhythm is usually due to increased vagal tone
and is seen often in conjunction with reversible ischemia of
the AV node. Treatment of symptomatic or severe bradycar-
dia with Mobitz type I block is begun with atropine.
Isoproterenol and dopamine may be tried; a temporary pace-
maker is necessary occasionally if the ventricular response is
inadequate and prolonged.
Mobitz type II second-degree AV block is usually due to
disease in the infranodal conduction system. The PR interval
is constant in conducted beats. The QRS interval is usually
mildly prolonged secondary to the infranodal conducting
system disease. In the nonconducted or blocked beats, a P
wave is seen without a QRS interval. This form of block may
occur in a pattern or may occur randomly. Several P waves
without accompanying ventricular beats may be seen (3:1 or
4:1 block). A temporary pacemaker is often necessary with
this type of block because of the higher likelihood of pro-
gression to complete AV block, and the escape pacemaker
with type II block, which originates in the ventricle, may not
generate an adequate ventricular rate.
During complete heart block (ie, third-degree AV block),
no atrial impulses are conducted to the ventricles because of
usually infranodal or severe AV nodal conduction system dis-
ease. There is no relationship between P waves and the QRS
interval (AV dissociation). The prolonged QRS interval indi-
cates that ventricular activation is initiated by a ventricular
pacemaker (automatic focus). Ventricular rates of 25–40
beats/min are seen with these ventricular escape rhythms
and usually are inadequate to maintain acceptable cardiac
output and blood pressure. Temporary and often permanent
pacing is required in adults with type II second-degree heart
and third-degree heart block.
Malfunction of Permanent Artificial
Pacemakers
Permanent pacemakers are used to support cardiac electrical
activity and maintain adequate heart rate by providing elec-
trical stimulation to the cardiac chambers. Pacemaker leads
are placed transvenously, although occasionally they may be
placed epicardially in association with other cardiac surgery.
Pacemakers have become increasingly more complex and
sophisticated in the last 10–15 years. In addition to the famil-
iar single-lead pacemakers, which sense and pace in the ven-
tricular chamber, pacemakers now are often dual-chamber,
sensing and pacing in both the atrium and the ventricle, and
sometimes they have an additional left ventricular lead for
cardiac resynchronization to treat congestive heart failure.
Pacemakers can be programmed to interrupt arrhythmias by
overdrive pacing or by administering ectopic beats.
Pacemakers can have rate-responsive features that allow the
heart rate to increase in response to increased physiologic
demand. When the pacemaker’s rate-responsive sensor is
minute ventilation (measured by transthoracic impedance),
inappropriate tachycardia may be observed during mechani-
cal ventilation.
Because of these added features, assessing pacemaker
function has become extremely complex and requires knowl-
edge of the type of pacemaker, understanding of the algo-
rithms the pacemaker uses, and information about the mode
in which the pacemaker is functioning. For example, for a
rate-responsive pacemaker, knowing the rate at which the
pacemaker should be inhibited involves not only knowing its
backup settings but the ramp used to adjust the pacing rate
and the stimulus to which it is responding.
In a critically ill patient, the major concerns about perma-
nent pacemaker function are (1) that the electrical impulse
from the pacemaker results in stimulation and electrical acti-
vation in the heart, (2) that the pacemaker is providing an
CARDIAC PROBLEMS IN CRITICAL CARE
493
adequate heart rate to meet the patient’s needs, and (3) that
the pacemaker is sensing the intrinsic cardiac activity and
not competing with it. A properly functioning pacemaker is
able to sense the intrinsic electrical activity of the heart so
that the pacemaker-generated rhythm and intrinsic rhythm
are not competing with each other. Failure to sense the
intrinsic rhythm raises the possibility of pacemaker-induced
arrhythmia; for example, ventricular tachycardia may result
from a pacemaker-triggered QRS interval occurring on a T
wave from the intrinsic rhythm.
In general, in the absence of battery failure, pacemaker
failure is almost always due either to lead malfunction from
wire fracture, loss of insulation, or fibrosis at the endocardial
contact site or to dislodgment in the cardiac chamber or dis-
connection at the connection between the pacemaker and
the pacemaker lead. Lead malfunctions produce problems
with both sensing and capturing, but often the malfunction
is intermittent, occurring when the lead is moved in a partic-
ular way, making detection difficult. Interrogation of the
pacemaker using the programming device provided by the
manufacturer will produce information about the pace-
maker’s settings as well as lead impedance, thresholds, ampli-
tude of sensed electrical activity, and strength of the battery.
This information often can differentiate lead malfunction
from component malfunction. Unfortunately, the older the
pacemaker, the less information can be derived from the pro-
grammer, and the older the pacemaker, the more likely it is
that malfunction will occur.
Programmability of the pacemaker, the ability to change
the rate of pacing or the relationship of ventricular to atrial
activation, allows manipulation of the patient’s hemodynam-
ics. For example, in a febrile or septic patient or one with
heart failure, increasing the ventricular rate may be needed to
increase cardiac output. In patients who develop atrial tach-
yarrhythmias, changing the pacemaker function to ignore the
atrial activity sometimes can allow much better rate control.
Blomstrom-Lundqvist C et al: ACC/AHA/ESC guidelines for the
management of patients with supraventricular arrhythmias:
Executive summary. A report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines and the European Society of Cardiology Committee
for Practice Guidelines (Writing Committee to Develop
Guidelines for the Management of Patients with Supraventricular
Arrhythmias). Developed in collaboration with NASPE-Heart
Rhythm Society. J Am Coll Cardiol 2003;42: 1493–531. [PMID:
14563598]
Delacrétaz E: Supraventricular tachycardia. N Engl J Med 2006;354:
1039–51. [PMID: 16525141]
Fuster V et al: ACC/AHA/ESC 2006 guidelines for the management
of patients with atrial fibrillation: Executive summary. A report
of the American College of Cardiology/American Heart
Association Task Force on Practice Guidelines and the
European Society of Cardiology Committee for Practice
Guildines. Developed in collaboration with the European Heart
Rhythm Association and the Heart Rhythm Society. Circulation
2006;114:e257–354. [PMID: 17695733]
Gregoratos G et al: ACC/AHA/NASPE 2002 guideline update for
implantation of cardiac pacemakers and antiarrhythmia
devices: Summary article. A report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines (ACC/AHA/NASPE Committee to Update the 1998
Pacemaker Guidelines). J Am Coll Cardiol 2002;40:1703–19.
[PMID: 12427427]
Holdgate A, Foo A: Adenosine versus intravenous calcium channel
antagonists for the treatment of supraventricular tachycardia in
adults. Cochrane Database Syst Rev 2006;4:CD005154. [PMID
17054240]
Jarcho JA: Biventricular pacing. N Engl J Med 2006;355:288–94.
[PMID: 16855269]
Naccarelli GV et al: Old and new antiarrhythmic drugs for con-
verting and maintaining sinus rhythm in atrial fibrillation:
Comparative efficacy and results of trials. Am J Cardiol 2003;91:
15–26D. [PMID: 12670638]
Trappe HJ, Brandts B, Weismueller P: Arrhythmias in the intensive
care patient. Curr Opin Crit Care 2003;9:345–55. [PMID:
14508146]
Zimetbaum P: Amiodarone for atrial fibrillation. N Engl J Med 2007;
356:935–41. [PMID: 17329700]
Zipes DP et al: ACC/AHA/ESC 2006 guidelines for management
of patients with ventricular arrhythmias and the prevention of
sudden cardiac death. A report of the American College of
Cardiology/American Heart Association Task Force and the
European Society of Cardiology Committee for Practice
Guidelines (Writing Committee to Develop Guidelines for
Management of Patients with Ventricular Arrhythmias and the
Prevention of Sudden Cardiac Death). Developed in Collaboration
with the European Heart Rhythm Association and the Heart
Rhythm Society. Circulation 2006;114:e385–484. [PMID:
16935995]
CARDIAC PROBLEMS DURING PREGNANCY
Pregnant patients with cardiac disorders may pose difficult
management problems. One always must consider the
impact of therapy on both the patient and the fetus. It is
often possible to pick a medication that will achieve the
desired clinical effect without injuring the fetus. However,
when the issue of fetal injury secondary to medication arises,
the risks need to be defined and the patient advised.
Knowledge of which medications cross the placenta and have
known teratogenic effects is mandatory. Ultimately, it is the
patient and physician who need to make the decision about
fetal risks to be accepted or avoided.
Common cardiac problems that occur in pregnant
women and may lead to admission to the ICU include valvu-
lar heart disease, arrhythmias, congestive heart failure, and
pulmonary hypertension.
Valvular Heart Disease During Pregnancy
Valvular heart disease may be unsuspected in a woman of
childbearing age who has been previously healthy.
Rheumatic heart disease resulting in mitral stenosis is seen
with increased frequency in regions that have large Hispanic
and Asian populations.
CHAPTER 21
494
Clinical Features
Women with mitral stenosis often are asymptomatic until the
normal increase in blood volume and cardiac output occurring
during pregnancy leads to elevated left atrial pressures and pul-
monary venous hypertension. Tachycardia or atrial fibrillation
is seen often in the acute presentation. These patients present
with signs and symptoms mimicking asthma and, if heart dis-
ease is unsuspected, become progressively worse owing to
drug-induced tachycardia from treatment with β-adrenergic
agonists. Atrial fibrillation also may result in atrial thrombus
formation, so the initial presentation may be a stroke.
The rapid heart rate does not allow time for atrial emptying,
and left atrial pressures therefore rise, resulting in pulmonary
edema. The presence of a diastolic murmur and opening snap
consistent with mitral stenosis and an echocardiogram showing
decreased mitral valve area and increased right ventricular pres-
sure should lead to appropriate management.
Treatment
When mitral stenosis is the dominant cardiac lesion, β-
adrenergic blockers should be used to slow the heart rate and
allow more time for ventricular filling. In general, cardiose-
lective β-adrenergic blockers such as atenolol are preferred
because they cross the placental barrier less effectively than
noncardioselective beta-blockers such as propranolol. If
atrial fibrillation rather than sinus tachycardia is present,
digoxin also can be used to slow the ventricular rate.
Although calcium channel blockers such as diltiazem and
verapamil also will slow heart rate, their effects on the fetus
need to be considered. In pregnant patients with tight mitral
stenosis and especially those with atrial fibrillation, anticoag-
ulation is important to reduce the risk of a stroke. Depending
on the stage of pregnancy, unfractionated heparin or low-
molecular-weight heparin may be most appropriate.
Returning the patient to normal sinus rhythm may
improve cardiac function by allowing better rate control, and
restored atrial contraction will aid in left ventricular filling.
Cardioversion must be done with the patient fully anticoag-
ulated—with plans to continue anticoagulation—and it is
necessary to demonstrate that atrial thrombi are not present
by transesophageal echocardiography. Finally, in patients
with severe mitral stenosis who continue to have severe con-
gestive heart failure symptoms despite medical therapy, per-
cutaneous valvuloplasty can be considered. Patients should
be chosen based on appropriate valve morphology and the
absence of significant mitral regurgitation. Fetal age and via-
bility should be considered in the timing of the intervention,
and neonatologists and obstetricians should be involved in
weighing the risk and benefit to the fetus.
In patients with other types of valvular heart disease,
management is directed toward maximizing the patient’s
cardiac output. However, some of the unloading agents used
to treat left ventricular dysfunction and left-sided valvular
regurgitation may decrease blood supply to the placenta and
therefore to the fetus. Thus the risks of treatment must be
weighed carefully. Fetal monitoring can be used to help assess
the impact of therapy.
Arrhythmias During Pregnancy
Atrial and ventricular arrhythmias are often benign.
However, sustained rapid atrial or ventricular tachycardia
has the potential to impair uterine blood flow resulting in
compromised fetal oxygenation. Late in pregnancy, when
systemic venous return is limited by compression of the infe-
rior vena cava by the enlarged uterus, a tachyarrhythmia may
result in profound hypotension and syncope. Therefore,
pregnant women who complain of dizziness or syncope must
be evaluated and monitored carefully, usually in an inpatient
setting. Because of toxic side effects and potential effects on
the fetus, antiarrhythmic drugs should be used only for doc-
umented sustained arrhythmias, with drugs and dosages
chosen to minimize effects on the fetus. Beta-blockers and
digoxin generally are safe in pregnancy.
Congenital Heart Disease and Pulmonary
Hypertension During Pregnancy
Pregnancy in patients with cyanotic congenital heart disease
is associated with a high incidence of fetal loss as well as
maternal death. Pulmonary hypertension, atrial tach-
yarrhythmias, inability to increase cardiac output with
increased demand, and hypoxemia all result in inadequate
cardiac output to the mother and the fetus. Postpartum,
acute exacerbation of pulmonary hypertension and sudden
death occur frequently. Treatment during the pregnancy is
supportive, including restricting activity, avoiding volume
overload, and treating polycythemia. A controlled elective
delivery using an epidural block or cesarean section to mini-
mize myocardial demand should be considered. Inhaled nitric
oxide or intravenous prostacyclin can be used to help manage
the worsening pulmonary hypertension seen after delivery in
patients with Eisenmenger’s syndrome with cyanosis.
Elkayam U, Bitar F: Valvular heart disease and pregnancy: I. Native
valves. J Am Coll Cardiol 2005;46:223–30. [PMID: 16022946]
Elkayam U, Bitar F: Valvular heart disease and pregnancy: II.
Prosthetic valves. J Am Coll Cardiol 2005;46:403–10. [PMID:
16053950]
Elkayam U et al: Pregnancy-associated cardiomyopathy: Clinical
characteristics and a comparison between early and late presen-
tation. Circulation 2005;111:2050–5. [PMID: 15851613]
van Mook WN, Peeters L: Severe cardiac disease in pregnancy: II.
Impact of congenital and acquired cardiac diseases during preg-
nancy. Curr Opin Crit Care 2005;11:435–48. [PMID 16175030]
TOXIC EFFECTS OF CARDIAC DRUGS
Cardiac medications have changed the treatment of patients
with heart disease dramatically, improving the quality and
duration of life, but these drugs have side effects both major

CARDIAC PROBLEMS IN CRITICAL CARE
495
and minor. Some of the toxic effects are extensions of a
drug’s therapeutic effects, whereas others are idiopathic or
autoimmune in nature. In some patients, toxicity may
develop only when metabolic changes occur that result in
decreased clearance of the drug, but reactions may occur
unpredictably even when drugs levels are in the therapeutic
range. Thus drug levels that produce a desirable drug effect in
one patient may produce a life-threatening side effect in
another. Toxicity also may develop when several drugs inter-
act. Both the toxic and the therapeutic effects of drugs, their
interaction with other drugs, and drug metabolism should be
understood and considered in making treatment decisions
and in evaluating patients receiving cardiac medications.
Discussed below are some of the more common and
important side effects of frequently used cardiac medica-
tions. The key to treating critically ill patients with cardiac
drugs is always to consider the possible or likely side effects
and interactions of the drugs, especially when the patient has
unexplained problems.
Digoxin
Pharmacology
Digoxin is a glycoside that inhibits Na
+
-K
+
ATPase and
thereby changes the intracellular Na
+
concentration. By alter-
ing the amount of Na
+
available for the Na
+
-Ca
2+
exchanger,
the net effect of digoxin is to increase the intracellular cal-
cium. Similarly, the effect of digoxin on Na
+
-K
+
ATPase also
alters the transmembrane potential of other cells and there-
fore affects cell excitability, conduction velocity, and refrac-
tory periods. Various cell types are affected differently; this
accounts for the differing effects of digoxin on atrial, AV
nodal, and ventricular tissue. Digoxin, like other cardiac gly-
cosides, also has neurally mediated effects that alter auto-
nomic balance and sympathetic output.
In appropriate doses, digoxin functions as an inotropic
agent, increasing contractility. Its clinically important elec-
trophysiologic effect is to block the AV node, thereby
decreasing the ventricular response rate in atrial fibrillation
and inhibiting reentrant supraventricular tachycardia.
Digoxin has a fairly long half-life of 36–48 hours. It also has
a relatively narrow therapeutic range. Digoxin is cleared pri-
marily by the kidneys with, perhaps, some clearance through
the GI tract.
In critically ill patients, rapidly changing renal function
and the requirement for multiple other drugs make the
development of digoxin toxicity more frequent. Electrolyte
abnormalities such as hypokalemia, hypomagnesemia, and
hypercalcemia enhance digoxin toxicity. Serum levels of
digoxin are affected by a variety of drugs. Quinidine alters
the renal clearance and volume of distribution of digoxin.
Therapeutic levels of quinidine double digoxin serum con-
centrations. Therefore, the dose of digoxin should be
reduced by half when instituting quinidine therapy.
Amiodarone, verapamil, and propafenone have similar
effects on renal clearance of digoxin and digoxin serum level,
although the magnitude of the effect is smaller. Periodic
determination of drug levels with appropriate dose reduc-
tion or cessation can avoid the worse complications.
Toxicity
Digoxin serum levels generally are considered therapeutic in
the range of 0.8–2 ng/mL, which, unfortunately, overlaps with
the range in which toxicity may be seen. Toxicity is rare in
patients with serum levels under 1.4 ng/mL but is seen with
increased frequency when serum levels exceed 2 ng/mL. The
positive inotropic effect of digoxin increases in a dose-related
manner, and this effect persists even in the face of high drug
levels. The toxic effects of digoxin can be broken down into
systemic and electrolyte effects and mild and severe arrhyth-
mias. With mild toxicity, the patient may develop nausea,
visual disturbances, and decreased appetite. At higher serum
levels of digoxin, as the Na
+
-K
+
ATPase is poisoned, hyper-
kalemia develops that may lead to cardiac arrest. Arrhythmias
seen at low levels of toxicity reflect the effect of digoxin on
automaticity, resulting in paroxysmal atrial tachycardia, junc-
tional tachycardia, and ventricular ectopy (particularly
bigeminy). Because digoxin increases AV nodal block, the
atrial tachycardias are associated with heart block.
Treatment
Treatment depends on the severity of toxic manifestations.
Withholding digoxin and correcting hypoxemia, hypokalemia,
and the acid-base disturbances that exacerbate digoxin toxi-
city usually correct arrhythmias over time. Marked bradycar-
dia in the setting of atrial fibrillation can be treated with
atropine in mild cases and temporary pacing in more severe
situations. Lidocaine or phenytoin often can control the less
serious ventricular arrhythmias. Electrical cardioversion may
be necessary acutely to treat sustained ventricular tachycar-
dia from digoxin toxicity when drugs and other measures
have failed, but there is an increased risk of arrhythmic com-
plications because of increased ventricular automaticity
caused by digoxin. Using less electrical energy (fewer joules)
may decrease the risk.
In cases of severe digoxin toxicity that include the devel-
opment of hyperkalemia, severe bradyarrhythmia, recurrent
ventricular tachycardia, or ventricular fibrillation, digoxin
immune Fab (ovine) can be lifesaving. This preparation is a
sheep antibody fragment that has a high affinity for digoxin,
rapidly binding to the drug and reversing its effect. The Fab
fragments have a lower molecular weight than complete anti-
bodies and thus have a greater rate and volume of distribu-
tion. The Fab-digoxin complexes are excreted in the urine,
thus enhancing renal clearance of the drug. Digoxin anti-
body is indicated in the setting of life-threatening digoxin
toxicity or when the ingestion of large amounts of digoxin
makes the development of toxic side effects likely. The dosage
of digoxin immune Fab depends on the digoxin level and the

CHAPTER 21
496
estimated volume of distribution. However, if the desired
effect is not achieved with the calculated dose, treatment
with the maximum dose is indicated in life-threatening situ-
ations. Side effects from digoxin immune Fab are minimal.
The drug is expensive, and its use therefore is reserved for
patients with severe life-threatening digoxin toxicity. In most
patients, prevention of digoxin toxicity is preferable and
achievable with forethought. For example, for elderly
patients or critically ill patients in the ICU with acute renal
failure or cardiogenic shock, digoxin should not be given as a
standing order for more than 1 day without careful review
and adjustment if necessary.
Antiarrhythmic Drugs
Lidocaine
Because lidocaine is metabolized by the liver, hypotension,
right-sided heart failure, and liver failure may result in
decreased clearance of this drug. Lidocaine has minimal
proarrhythmic and myocardial depressant effects. Its side
effects are primarily neurologic consisting of acute onset of
agitation, tremulousness, psychosis, and seizures.
Withdrawal of the drug and time are the treatments. If indi-
cated, another antiarrhythmic agent can be used when lido-
caine is discontinued.
Procainamide and Quinidine
Procainamide, used for treatment of both atrial and ventric-
ular arrhythmias, is cleared by the kidneys. Both the drug
and its by-product, N-acetyl procainamide (NAPA), accu-
mulate in patients with renal failure. Procainamide is a
myocardial depressant and can cause hypotension. It also can
cause QT-interval prolongation with the development of
polymorphic ventricular tachycardia similar to the effects of
quinidine. Unlike quinidine, procainamide does not alter
serum digoxin levels. A number of noncardiac side effects are
caused by procainamide, the most important being agranu-
locytosis and the development of a lupus-like syndrome.
Agranulocytosis is reversible, but the patient may present
with sepsis. The lupus-like syndrome is generally a late devel-
opment in the course of prolonged administration with man-
ifestations such as fever, pleuropericarditis, and arthralgias.
There are serum antihistone antibodies associated with this
drug-induced syndrome as well. This side effect may be seen
more frequently in patients who metabolize the drug slowly
(slow acetylators). The syndrome is reversible with discontin-
uation of the drug.
Quinidine should not be used as a routine drug in the
ICU and virtually never should be started as a new agent.
Quinidine, a class Ia agent whose indications are similar to
those of procainamide, has less myocardial depressant effects
but is only available orally. Its proarrhythmic effects are well
known, with QT-interval prolongation resulting in ventricu-
lar tachycardia and syncope. GI side effects are frequent, and
the development of nausea and diarrhea often limits its use.
Neurologic side effects include tinnitus, hearing loss, and
confusion. Autoimmune thrombocytopenia or hemolytic
anemia occasionally develops unexpectedly, resulting in
hemorrhage or death. Quinidine-induced thrombocytopenia
is treated as autoimmune thrombocytopenia.
If polymorphic ventricular tachycardia (torsade de
pointes) develops during treatment with quinidine or pro-
cainamide, the drug should be stopped, and other class Ia and
Ic agents should be avoided. Beta-adrenergic agonists such as
isoproterenol can be used to speed up the heart rate and
shorten the QT interval. Overdrive pacing with a transvenous
pacing wire also can be used in patients with recurrent ven-
tricular tachycardia until the offending drug is cleared or
metabolized. When monitoring the QT interval during
administration of quinidine or procainamide, the drug
should be discontinued if the QT interval exceeds 500 ms.
Flecainide
Flecainide is a class Ic antiarrhythmic agent that is well toler-
ated, with minimal noncardiac side effects. It is proarrhyth-
mic, however, and can cause significant and sustained
ventricular tachycardia that is resistant to other antiarrhyth-
mic agents. Flecainide slows conduction throughout the con-
ducting system, which can result in bradycardia as well as
heart block. It is poorly tolerated by patients with depressed
left ventricular function and should not be used for those
patients.
Amiodarone
Amiodarone is a powerful antiarrhythmic agent with mini-
mal proarrhythmic effects. However, it has a number of car-
diac and noncardiac side effects that are magnified by its long
half-life. Resulting toxicities can last from days to months
depending on the duration of therapy and the dose.
Amiodarone slows conduction throughout the heart, result-
ing in bradycardia and heart block, which may require per-
manent pacing. GI side effects include nausea and decreased
appetite resulting in weight loss and necessitating dose
reduction or termination of therapy. Either hypo- or hyper-
thyroidism can result from amiodarone’s effect on iodine
metabolism. Deposits in the skin can result in darkening of
skin especially in sun-exposed areas. Intracytoplasmic lamel-
lar deposits can occur in several parts of the eyes, most com-
monly causing corneal epithelial opacities in more than 70%
of patients and lens opacities in 50–60%. Neither impairs
visual acuity, and amiodarone treatment can be continued.
Pulmonary fibrosis is a frightening and potentially life-
threatening complication that can further compromise
patients who already have significant cardiac impairment.
Baseline and follow-up pulmonary function tests are manda-
tory to monitor the development of pulmonary involvement.
Amiodarone interacts with and changes the metabolism of a
myriad of drugs. Its interactions with digoxin, β-adrenergic
blockers, calcium channel blockers, and warfarin should be
monitored carefully.
