Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


397
0016
Surgical Infections
Timothy L. Van Natta, MD
∗
General Considerations
Persistent fever in the postoperative patient is always con-
cerning. Potential causes include infection, atelectasis,
deep venous thrombosis, and drug reactions. The surgical
wound and urinary tract are common infections sites.
While management of these problems is relatively straight-
forward, diagnosis and treatment of other inflammatory
and infectious processes can be problematic. It is often dif-
ficult to differentiate between systemic inflammatory
response syndrome (SIRS) and sepsis. Documentation of a
discrete infection is required for diagnosis of the latter.
Infection types and sites not thought of are unlikely to be
identified. An organized diagnostic approach pays divi-
dends, particularly when based on analysis by body region
and through monitoring the presence and duration of
indwelling devices. Early diagnosis of infection portends
optimal outcomes, preempting sepsis and its attendant
complications—provided antimicrobial agents and adjunc-
tive measures are used rationally.
Sepsis may be the reason for ICU admission, or it may
complicate another critical illness. A surgical patient can
present anywhere along a spectrum from SIRS to sepsis to
severe sepsis (ie, sepsis associated with organ dysfunction)
to septic shock to multiple organ dysfunction syndrome
(MODS). A patient’s course often devolves along these
stages despite the physician’s best efforts. However,
prompt application of goal-directed therapy raises the
likelihood of course reversal before irrevocable organ
damage occurs.
Balk RA, Ely EW, Goyette RE: Sepsis Handbook, 2d ed. Nashville,
TN: Thomson Advanced Therapeutics Communications and
Vanderbilt School of Medicine, 2004.
Prevention of Surgical Infections in the ICU
Surgical infections can be prevented through proper use of
prophylactic antibiotics. To be effective, the appropriate antibi-
otic must be administered within 1 hour before the operation
so that tissue levels are high at incision time. Antibiotics with
24-hour dosing are attractive in this regard because no postop-
erative doses are necessary. Prophylactic antibiotics have no
value beyond the first 24 hours following surgery. Their contin-
ued use puts patients at risk for antibiotic-associated
Clostridium difficile colitis, infection by multidrug-resistant
bacteria (eg, methicillin-resistant Staphylococcus aureus,
vancomycin-resistant Enterococcus, and Acinetobacter species),
and fungal infections. No less important, this practice adversely
affects the bacterial ecology in the ICU. Continuing “prophy-
lactic” antibiotics for the duration of drain and chest tube pres-
ence cannot be condoned. Furthermore, antibiotics cannot
compensate for suboptimal surgical conduct.
Invasive procedures in the ICU require strict sterile tech-
nique. This demands that one don a cap, mask, sterile gloves
and gown; generously prepare the area with chlorhexidine;
and meticulously drape the field. Once percutaneous
catheters are in place, making connections and sampling
must be done fastidiously. Chlorhexidine-laden catheter-site
dressings are effective in preventing infections and should be
used routinely. Of course, clinical crises can demand expedi-
tious, nonsterile placement of intravenous and other
catheters. These should be removed as soon as feasible and
never beyond 24 hours from time of placement. When cen-
tral venous access is necessary but central pressure monitor-
ing is not, conversion from a central line to a percutaneously
inserted central catheter (PICC line) lessens infection risk.
When central access is no longer required, a change from
central to peripheral access should be accomplished as soon
as practical. Other devices, such as ventriculostomy drains,
chest tubes, epidural catheters, arterial lines, and urinary
catheters, should be removed as soon as their utility wanes.
The ICU team should take daily stock of all such devices and
think critically about the continued value of each.
∗
James A. Murray, MD, and Howard Belzeberg, MD, were the
authors of this chapter in the second edition.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 16
398
Other preventive measures are noteworthy. It has been
established that postoperative hyperglycemia is directly asso-
ciated with increased infection rates. The goal should be to
strive for glucose levels of 80–110 mg/dL and certainly to
prevent levels from exceeding 150 mg/dL. In the ICU, hourly
glucose monitoring and aggressive insulin use are commonly
required to achieve this goal. Insulin drips are frequently
necessary, and there should be no reluctance to use them on
a protocol-driven basis. Judicious use of steroids and other
immunosuppressive medications is an important adjunct as
well. For patients with diseases requiring these agents, the
intensivist must balance their use with the need to prevent
and/or treat infections. The same can be said for transfusion
of blood and blood products. As the immunosuppressive
nature of blood transfusion has become increasingly recog-
nized, the elevated risk of surgical infection must be weighed
against the desire to optimize oxygen delivery.
Malnutrition clearly puts patients at risk for infections, and
nutritional support is a signal feature of intensive care. For
many reasons, including lower infection rates, enteral feeding
is preferred over the intravenous route. However, the latter has
the advantage of prompt delivery of full nutritional support.
There should be no hesitation to initiate parenteral nutrition
should tube feedings be unsuccessful or impractical.
Currently, numerous immune-enhanced formulas are avail-
able. Some of the purported benefits are simply due to their
increased protein content, but additionally, there may be clin-
ically significant benefits to increased provision of certain
amino acids (eg, glutamine, arginine, and glycine), nucleic
acids, and omega-3 fatty acids. This is an area of particularly
intense research activity, and critical care physicians should
follow this work closely.
Furnary AP et al: Continuous insulin infusion reduces mortality in
patients with diabetes undergoing coronary artery bypass graft-
ing. J Thorac Cardiovasc Surg 2003;125:1007–21. [PMID:
12771873]
Hill GE et al: Allogeneic blood transfusion increases the risk of
postoperative bacterial infection: A meta-analysis. J Trauma
2003;54:908-14. [PMID: 12777903]
Diagnosis of Surgical Infection in the ICU
Despite the highly technical atmosphere of the ICU, assiduous
physical examination remains the cornerstone for timely diag-
nosis of surgical infections. The presence of complex devices
and dressings, along with the patient’s relative immobility, can
inhibit thorough physical assessment. Diagnostic delays are
commonly attributable to an intubated patient’s inability to
communicate. Fever and leukocytosis often prompt early eval-
uation by CT scan. Negative or equivocal imaging studies are
not uncommonly followed by a revealing physical evaluation
that could have obviated the trip to radiology.
Clues to presence of infection can be subtle. Examples
include unexplained hyperglycemia and gradual worsening of
hepatic, pulmonary, and/or renal functional indices.
Additionally, stagnant or falling nutritional markers such as
prealbumin may signify infection rather than inadequate pro-
vision of calories and nutrients. Immunosuppressed individ-
uals may not manifest the usual signs of infection, and index
of suspicion should be high if the clinical course is not pro-
ceeding smoothly. For these and other critically ill patients,
both overt and subtle indicators of infection warrant blood,
sputum, and urinary cultures. More sophisticated evaluations
also generally will be necessary. It can be quite difficult to dif-
ferentiate true infection from bacterial or fungal colonization.
It takes experience and discipline to react appropriately when
confronted with culture results in critically ill patients.
Fortunately, there are many tools for diagnosing infec-
tions even when their existence is not forthcoming from
physical examination or culture data. Critical care specialists
are increasingly using bedside ultrasound and echocardiog-
raphy. Pleural, pericardial, peritoneal, and soft tissue fluid
collections can be identified and sampled safely. Diagnostic
peritoneal lavage, though largely supplanted by emergency
department ultrasonography for trauma, still has an occa-
sional role in determining the presence of peritonitis in
patients too unstable for travel to the radiology suite.
Intensivists routinely perform fiberoptic endoscopy of all
sorts. This allows accurate and timely diagnosis of pneumo-
nia and infectious esophagitis and colitis. Diagnostic
laparoscopy and pleuroscopy now can be done at bedside.
Imaging studies play a crucial role in the diagnosis of
infection in the critically ill. Ultrasound, CT, and MRI are
sometimes complementary and sometimes competing. It is
often productive to discuss clinical scenarios in depth with
radiology colleagues before sending the patient for one type
of scan or another. This avoids unnecessary excursions from
the ICU and limits suboptimal studies, redundancy, expense,
and patient risk. Of the three, MRI probably is the least use-
ful in evaluation of the unstable ICU patient. In some cases,
though, particularly when CNS infection is a concern, MRI
may be superior. CT scanning and ultrasound, besides pro-
viding high-quality images, allow therapeutic abscess
drainage. To a large extent, this has replaced surgical explo-
ration for management of abdominal and pelvic infections.
Nuclear medicine studies, when selected appropriately, also
serve an important purpose. For example, indium-labeled
white blood cell scans, though of limited utility early in the
postoperative period, can pinpoint the site of infection later
in a patient’s course when other methods have failed.
Beaulieu Y: Bedside echocardiography in the assessment of the crit-
ically ill. Crit Care Med 2007;35:S235–49. [PMID: 17446784]
Nicolaou S et al: Ultrasound-guided interventional radiology in
critical care. Crit Care Med 2007;35:S186–97. [PMID: 17446778]
Treatment of Surgical Infection in the ICU
Significant progress has been made over the past decade rel-
ative to treatment. Advances are attributable to two major
areas: improvement in use of antimicrobial agents and

SURGICAL INFECTIONS
399
advancement in interventional radiology techniques. A
handful of new antibacterial and antifungal agents have been
introduced recently. While these agents have broadened ther-
apeutic options, multidrug-resistant pathogenic strains con-
tinually threaten the ICU patient. By employing newer agents
rationally and using older agents more effectively, the clini-
cian stands a better chance against problematic organisms.
The change to once-daily dosing of aminoglycosides, for
instance, addresses several issues. Higher doses given over
broader time intervals provide greater peak blood levels. This
enhances bacterial killing, whereas low or undetectable
trough levels limit renal and other toxicity. Renal toxicity is a
largely saturable process. Despite high peak levels, only so
much aminoglycoside can be taken up by renal cells per unit
time. Later in the interval, when renal cells could absorb
more antibiotic, there is little available to produce toxic
effects. Other antibiotics work much better when some con-
tinuous minimum level is maintained. Since there appears to
be no augmentation of bacterial killing by pushing levels
higher, lower doses given more frequently (or even by con-
tinuous infusion) provide a persistent satisfactory level to
achieve optimal bactericidal effect. Penicillins and
cephalosporins exemplify this strategy. As newer agents are
introduced, these principles should be borne in mind.
Newer antibiotics have improved options for treating
surgical infections caused by multidrug-resistant strains.
Examples include linezolid to treat methicillin-resistant S.
aureus (MRSA) and tigecycline to combat difficult gram-
negative rods such as Acinetobacter baumannii. To retain
their efficacy, they must be used with discretion. While
broad agents are often necessary at the onset of infection,
there should be a rapid taper to narrower agents once cul-
ture data are available. Again, it is particularly important to
differentiate between bacterial colonization and true infec-
tion so as not to overuse new agents and diminish their
capabilities.
It is worthwhile at times to also consider alternative
routes of antibiotic administration. These include intrathe-
cal, inhalational, enteral, and intracavitary drug delivery.
Several antimicrobial classes have bioavailability via the
enteral route that rivals that of parenteral delivery.
Examples include quinolones and fluconazole. Once tube
feedings are well tolerated, a switch from parenteral to
enteral delivery can be made confidently, limiting adminis-
trative costs and allowing removal of intravenous catheters
that may, in turn, become infected. Finally, a broader array
of antifungal and antiviral agents has become available in
recent years, enhancing treatment options while in many
cases reducing renal and other toxicity. On occasion, a crit-
ically ill patient whose infection is not responding to mul-
tiple antibiotics must be started presumptively on a
systemic antifungal agent despite lack of supportive culture
data. Close collaboration with infectious disease consult-
ants is necessary in these cases.
Duration of antimicrobial coverage is continually
debated. While there is a trend toward limiting treatment
duration, some infections are particularly hard to treat given
the difficulty of antibiotic penetration into the tissues
involved. Examples include endocarditis, osteomyelitis,
sinusitis, and otitis media. When presence of one of these
infections is certain, prolonged antibiotic courses generally
are necessary and accepted. For most other surgical infec-
tions, however, shorter durations are preferable. It has been
well established that peritonitis following perforated diverti-
culitis or appendicitis (after surgical source control) should
be discontinued once fever, leukocytosis, and ileus have
resolved. If these occur even as early as postoperative day 3,
it is reasonable to stop antibiotics then. Failure to meet these
criteria by days 5, 6, or 7 usually means an abscess has
formed. Continued or additional antibiotics likely will be
ineffective, and one should proceed with an abdominopelvic
CT scan searching for a drainable abscess. In most cases,
abscesses thus identified can be treated definitively by CT- or
ultrasound-guided aspiration via percutaneous, transrectal,
or transvaginal routes. This obviates a return to the operat-
ing room and its attendant morbidity. Occasionally, multiple
abscesses are identified, not all of which are amenable to
image-guided drainage. Options then are limited to continu-
ing conservative (ie, broad antibiotic) treatment versus reop-
eration. This decision hinges on the patient’s status. If
substantial leukocytosis or left shift persists, but the patient is
eating well and lacks marked constitutional symptoms, pro-
longed antibiotic therapy may be successful. This is unusual,
though, and most patients with multiple postoperative
abscesses must be taken back to the operating room.
These concepts involving intraabdominal infection are
not new. Limiting duration of treatment and earlier pursuit
of imaging studies have been applied recently to other infec-
tions, however, such as pneumonia. The common goal is to
get the most out of available agents by preserving their effi-
cacy, limiting toxicity and microbial resistance during ther-
apy, and slowing emergence of resistant strains that might
affect future patients. Every institution and its individual
ICUs have their own unique bacterial ecology. This limits
somewhat the broad applicability of treatment guidelines.
Review of institutional antibiograms on a quarterly basis can
positively influence empirical coverage of apparent pneumo-
nias and bloodstream infections while spotlighting emerging
resistance patterns. Antibiotic “crop rotation” has been
employed as a means to stem development of resistant
strains within ICUs, although this concept remains contro-
versial. What is probably more important is for the inten-
sivist to employ all means at his or her disposal to rapidly
identify the site of infection and its causative organism(s),
allowing the most rapid application of the narrowest effec-
tive agent(s). An organized approach to patient assessment
by body region is helpful.
Bennett KM et al: Implementation of antibiotic rotation protocol
improves antibiotic susceptibility profile in a surgical intensive
care unit. J Trauma 2007;63:307–11. [PMID: 17693828]

CHAPTER 16
400
Evaluation and Management of Infection
by Body Site
Head and Neck
CNS infections, including meningitis, ventriculitis, and
intracerebral abscess, must be considered in patients who
have sustained head injury or have undergone neurosurgical
procedures. Patients with skull base and paranasal fractures
are included in this group. Use of intraparenchymal cerebral
pressure (ICP) monitors and ventriculostomy catheters, while
applied appropriately along guidelines for severe head injury
management, is associated with serious infection risk.
Previously, antibiotic prophylaxis was used for the duration of
ICP monitor presence and for 5–7 days following diagnosis of
skull base or paranasal sinus fractures. It is now recognized
that this exerts pressure toward infection by multidrug-
resistant organisms. Controlled data are lacking as to appro-
priate antibiotic use in these patients, but it is clear that the
indiscriminant use of antibiotics in these settings is associated
with difficult-to-treat secondary infections. With regard to
transcranial pressure monitors, it is hoped that with sterile
technique at placement, fastidious fluid sampling, prudent
antibiotic use, and device removal as early as feasible, occur-
rence of serious infections will diminish.
Another important consideration is infection in and
around the eye. As mentioned earlier, ocular inflammation
often goes unnoticed in the complex ICU patient. Problems
not considered go undiagnosed, and any abnormal ocular
finding should prompt early ophthalmologic consultation as
appropriate. Periorbital cellulitis is of particular concern
because therapeutic delay can result in the catastrophic com-
plication of cavernous sinus thrombosis.
Given the ubiquitous use of nasogastric tubes, paranasal
sinusitis remains a risk. There may or may not be associated
purulent nasal drainage. It is important to remember this not
infrequent but often undiagnosed infection in the febrile
critically ill patient. CT scan is far superior to plain films for
making this diagnosis. Surgical drainage sometimes must
augment antibiotics to clear this infection. It is best to avoid
this condition altogether by choosing the oral over the nasal
route for enteral decompression and feeding in orotracheally
intubated patients. Dental abscess, simple or complicated,
should be considered in the febrile, critically ill patient, par-
ticularly when dentition is poor. These and pharyngeal infec-
tions can evolve into life-threatening necrotizing infections
that can descend transcervically into the chest (ie, acute
necrotizing mediastinitis). The cervical component of this
process is not difficult to recognize given neck edema,
induration, and erythema, but the thoracic component can
have protean manifestations. New and unexplained pleural
fluid noted on chest x-ray is an important early finding.
Central line infections contribute significantly to mor-
bidity and mortality in surgical patients. In the United States,
about 200,000 nosocomial bloodstream infections occur annu-
ally, the majority of which are associated with the presence of
intravascular catheters. Internal jugular and femoral venous
catheters previously carried higher infection rates than those
in the subclavian position, but recent preventive strategies
have perhaps neutralized this difference. Such measures
include perfect sterile technique at placement, chlorhexidine
site preparation, selection of catheters with antibacterial
coatings, use of antiseptic site dressings, and device removal
as early as possible. Application of catheter-site antibiotic
ointments should be avoided because they encourage devel-
opment of infection by resistant bacteria and fungi. Rotation
of catheter sites on a scheduled basis is not helpful, and
catheter changes over a guidewire should be kept to a mini-
mum. In certain situations, vascular access may be exceedingly
difficult. Despite development of fever or leukocytosis, risk-
benefit analysis may favor guidewire exchange over attempting
placement at a new site. However, the removed catheter tip
should be sent for culture. A positive culture mandates
immediate removal of the catheter that replaced the original
one. Infection also can be introduced via the catheter hub,
and those accessing the catheter must maintain strict sterile
technique.
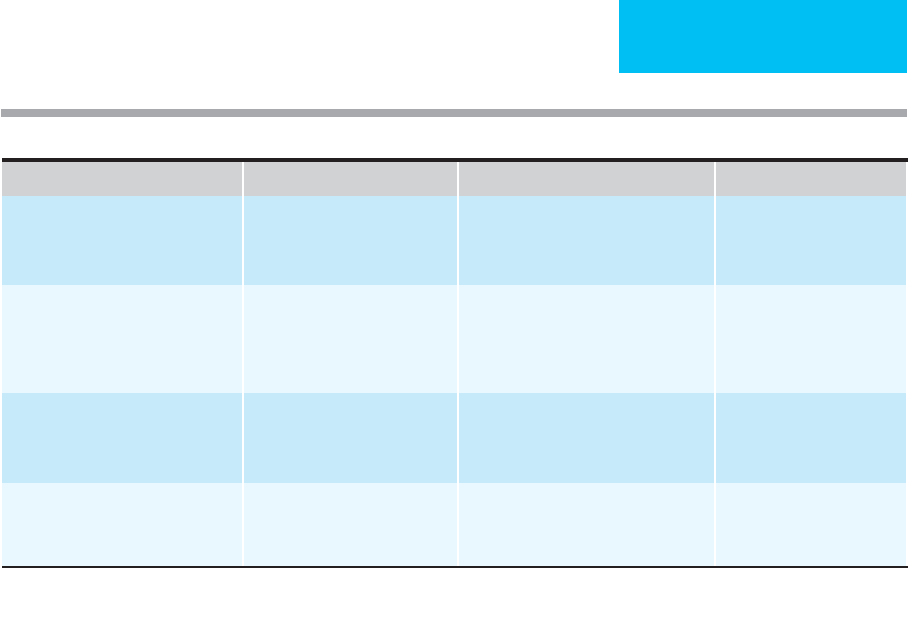
Treatment of head and neck infections is summarized in
Table 16–1.
Gilbert DN et al (eds): The Sanford Guide to Antimicrobial Therapy,
37th ed. Sperryville, VA: Antimicrobial Therapy, Inc., 2007.
Kuminsky RE: Complications of central venous catheterization.
J Am Coll Surg 2007;204:681–96. [PMID: 17382229]
Taylor RW, Palagiri AV: Central venous catheterization. Crit Care
Med 2007;35:1390–6. [PMID: 17414086]
Chest
Ventilator-associated pneumonia (VAP) is the most com-
mon infection in the surgical ICU. VAP is defined as pneu-
monia occurring at least 48–72 hours following
endotracheal intubation. There is debate as to whether or
not VAP independently increases mortality, but it clearly
lengthens ICU stay, increases patient days on the ventilator,
and adds tremendously to health care expenditures.
Antibiotic therapy for VAP is often complex and prolonged,
adversely affecting an ICU’s bacterial ecology. Over recent
years, much effort has been expended to better characterize
the pathophysiology, diagnosis, and proper treatment of
VAP. There is no diagnostic “gold standard,” and treatment
is complicated by undisciplined antibiotic administration
with vague treatment endpoints. The Centers for Disease
Control and Prevention original criteria for pneumonia (ie,
fever, leukocytosis, positive sputum Gram stain, and new or
changing pulmonary infiltrate) have proven insufficient for
diagnosis of VAP in the complicated, critically ill patient. In
patients with a markedly abnormal chest x-ray because of
acute respiratory distress syndrome (ARDS), it is often
impossible to identify a new infiltrate superimposed on the
background of noncardiogenic pulmonary edema.
Although VAP diagnosis and treatment remain problematic,
SURGICAL INFECTIONS
401
its causes have become better understood. Presence of an
endotracheal tube (ETT) allows contaminated oropharyn-
geal secretions to circumvent natural protective barriers.
The endotracheal tube, impaired host immunity, and lurk-
ing environmental pathogens conspire to produce VAP in
the critically ill surgical patient. Negative effects of blood
transfusion, hyperglycemia, and malnutrition, so commonly
seen in the ICU, elevate risks further.
There has been a strong push lately to improve the preven-
tion and management of VAP. Influential multidisciplinary
societies (eg, the American Thoracic Society and the Infectious
Disease Society of America) have promulgated clinical guide-
lines. These ICU “bundles” promote consistency in approach
within and across institutions. Prevention strategies include
head-of-bed elevation 30–45 degrees (or reverse Trendelenburg
position when thoracic spine stability is in question) and
avoidance of gastric distention to minimize aspiration of gas-
tric contents, use of ETTs with suction ports to remove secre-
tions pooling above the ETT cuff, use of sleeved suction
catheters, and improved oral hygiene. Selective gut decontami-
nation has been advocated, but its value is questionable because
enteric organisms generally are not responsible for VAP. The
most common offending organisms are MRSA and species of
the genera Pseudomonas, Acinetobacter, and Stenotrophomonas.
Minimizing transfer of these pathogens from one patient to
another is another key to prevention. Finally, since the inci-
dence of VAP correlates with a patient’s duration of intubation,
any prevention program should include an aggressive strategy
for liberation from the ventilator.
Diagnosis of pneumonia is usually not difficult in the
emergency department. History, physical findings, and
chest x-ray generally suffice. For the intubated ICU patient,
development of fever, leukocytosis, and apparent purulent
sputum raise the question of pneumonia, but establishing a
confident diagnosis may be difficult. Both chest x-ray and
tracheal sputum aspirate analysis lack specificity in these
patients. A normal chest x-ray excludes the diagnosis. When
the chest x-ray is abnormal, the next step is to obtain a reli-
able sputum sample for performance of quantitative analy-
sis. Preferred methods are use of a protected-specimen
brush (PSB) and bronchoalveolar lavage (BAL).
Commonly used thresholds for confirming pneumonia are
10
3
colony-forming units (cfu)/mL for PSB and 10
4
cfu/mL
for BAL. These techniques, which require bronchoscopy,
are expensive and time-consuming. However, they more
firmly establish the correct diagnosis and direct appropri-
ate antibiotic therapy. More recently, catheters have been
developed that allow reliable sampling by the respiratory
therapist, eliminating need for bronchoscopy. Both PSBs
and mini-BAL sets are available and are enjoying wider use.
The goals are to distinguish between infection and colo-
nization and, if infection is present, to determine the
offending organism(s) as soon as possible so that treatment
can be tailored specifically.
Diagnosis Organisms Initial Antibiotics Adjunctive Therapy
Meningitis and ventriculitis
S. pneumoniae, S. aureus,
coliforms,
P. aeruginosa,
Acinetobacter
sp.
Vancomycin 500–750 mg IV q6h +
cefepime or ceftazidime 2 g IV q8h
or
meropenem 2 g IV q8h + vancomycin
1 g IV q6–12h
Removal of intracerebral
device, intrathecal antibiotic
administration
Periorbital cellulitis
S. pneumoniae, Haemophilus
influenzae, Moraxella catarrhalis,
S. aureus, group A
Streptococcus
sp.
Nafcillin-oxacillin 2 g IV q4h (if MRSA,
vancomycin 1 g IV q12h) + ceftriaxone
2 g IV q24h + metronidazole 1 g IV q12h
IV heparin for cavernous sinus
thrombosis if present
Paranasal sinusitis Gram-negative bacilli,
S. aureus
Imipenem 500 mg IV q6h
or
meropenem
1 g IV q8h
or
ceftazidime 2 g IV q8h
or
cefepime 2 g IV q12h (for possible
MRSA, add vancomycin 1 g IV q12h)
Removal of nasoenteric tube,
aspiration of fluid from sinus
Central line infection
S. aureus
(MSSA, MRSA),
S. epidermidis,
enterococci
Vancomycin 1 g IV
or
linezolid 600 mg
IV q12h
Removal of catheter, vein
resection if suppurative
thrombophlebitis
Data from Gilbert DN et al (eds): The Sanford Guide to Antimicrobial Therapy, 37th ed. Sperryville, VA: Antimicrobial Therapy, Inc., 2007.
Table 16–1. Summary of head and neck infections in adult surgical patients.

CHAPTER 16
402
Aggressive treatment should immediately follow acquisi-
tion of a good sputum sample. Antibiotic selection depends
on the prevailing organisms within an individual ICU.
Offending bacteria change over time, justifying quarterly
analysis of cultures and resistance patterns. In general, initial
therapy should cover MRSA and the difficult gram-negative
rods. It is important to start broadly because delays in appro-
priate coverage may lead to increased mortality. Once reliable
microbiologic data are available, antibiotic coverage should
be tailored immediately to the narrowest bactericidal agent
to which the organism is sensitive. Previously, it was recom-
mended that two antibiotics with different mechanisms of
action should be used to treat the multidrug-resistant gram-
negative rods. This was extrapolated from the neutropenic
cancer patient population and applied to other groups.
Supportive data are lacking for the surgical ICU population,
and single-agent therapy appears to be satisfactory. When
final microbiologic data do not support the diagnosis of VAP,
and the patient is not deteriorating, it is reasonable to stop
antibiotics altogether. If culture results are equivocal and/or
the patient’s condition is worsening, it is appropriate to con-
tinue broad antibiotic coverage, but a firm endpoint of about
7 days should be selected early. In the majority of cases, cul-
ture and sensitivity results will guide selection of the narrow-
est appropriate antibiotic, and duration of therapy can be
determined by the patient’s response.
Antibiotics with high enteral bioavailability often can be
converted safely from intravenous to enteral administration
early in the treatment process. Inhaled administration of
antimicrobials should be considered in some instances.
Pneumonia can be difficult to treat, even with the correctly
chosen and delivered agent, and courses of 10–14 days are
often necessary. Patients with blood and respiratory cultures
growing the same organism have a more serious infection
and generally will need a longer antibiotic course. However,
improvement should be seen within 1 week, and if this has
not occurred, a prolonged antibiotic course is not likely to be
effective. Failure of a timely response should prompt a search
for complications of pneumonia such as pulmonary abscess
or empyema or consideration of an alternative infection
diagnosis. CT scanning is important in this assessment.
Another important surgical infection is empyema, or pus
in the pleural space. Indicative findings on pleural fluid
analysis are pH less than 7.20, organisms present on Gram
stain, and a positive culture. Ultrasound is helpful to guide
safe aspiration of pleural fluid. Surgical patients at risk are
those who have had VAP, blunt or penetrating trauma, tho-
racostomy tube placement, or thoracotomy. CT scan defines
the empyema’s extent. Treatment options include thoracos-
tomy tube placement, instillation of tissue plasminogen acti-
vator (tPA), video-assisted thoracoscopic surgery (VATS) or
open thoracotomy with lung decortication, and open
drainage. Choice of treatment is influenced by the duration
of the process, the pleural fluid distribution, and the patient’s
condition. The three stages of empyema are the early exuda-
tive stage, the intermediate fibrinopurulent stage, and the late
organization stage. A simple empyema in its early stage often
can be well managed with a chest tube and antibiotics.
Beyond antibiotics, the goals are to drain all the infected fluid
and eliminate all free intrapleural space. Generally, the
admonition of “no space, no problem” applies. The chest
tube does not always have to be of large caliber. A single loc-
ulated collection not draining adequately via a well-placed
thoracostomy tube may respond to dissolution by a throm-
bolytic agent. This can be effective, but it is best done in col-
laboration with the surgeon who would operate if
thrombolytics fail because subsequent operative intervention
can be rendered much more difficult.
Multiple loculated fluid collections and more advanced
empyema stages are best dealt with surgically (VATS or tho-
racotomy). For the critically ill or severely debilitated patient,
rib resection and drainage may be the best approach, allow-
ing the space to heal from the inside out as the thoracostomy
tube is slowly withdrawn over weeks to months. A special
empyema subset is that occurring early after pneumonec-
tomy. The majority of these are due to a breakdown of the
bronchial stump. The problem is manifested by a productive
cough, dyspnea, and sepsis. The first maneuver is to place a
thoracostomy tube to drain the infected fluid that will
diminish the septic focus and prevent spread of infection to
the remaining lung. Open thoracostomy with bronchial
repair and muscle or omental flap coverage are required then
to correct the process. Eventually, the chest can be closed over
a pleural space filled with antibiotic solution, with expecta-
tion of success in most cases.
Two other major chest infectious processes are mediastini-
tis and endocarditis. Mediastinitis can occur as a postopera-
tive infection following median sternotomy, as a result of
spontaneous or iatrogenic esophageal perforation, or as a
descending necrotizing process originating from oropharyn-
geal or odontogenic infection. Sternal wound infection after
cardiac surgery can be superficial, responding to antibiotics
and local wound care. Associated life-threatening mediastini-
tis occurs in just over 1% of cardiac surgery patients, with the
incidence in children approximating that in adults. One adult
group at higher risk is diabetic women undergoing bilateral
internal thoracic artery harvest. Fever, leukocytosis, sternal
instability, and wound erythema and drainage warn of this
problem, and a new pleural effusion adds to the probability.
Treatment includes administration of intravenous antibiotics,
surgically evacuating all purulent fluid and necrotic soft tissue
and bone, and either reclosing the sternum over an inflow-
outflow antibiotic delivery system or filling the defect with
pedicled muscle or omental flaps. Esophageal perforation
occurs most commonly now as a complication of endoscopy.
Small tears occasionally can be managed with antibiotics with
or without stent placement, provided that there is no free flow
of diagnostic contrast agent into the mediastinum or pleural
space. Most esophageal perforations require thoracoscopic or
open pleural drainage, mediastinal debridement, and
esophageal repair over a bougie when feasible. Generally, tears
in the upper two-thirds of the esophagus are approached via
SURGICAL INFECTIONS
403
right posterolateral thoracotomy and those in the distal third
by way of left posterolateral thoracotomy.
Acute necrotizing mediastinitis (ANM) is third major
form of mediastinitis. It is a destructive, life-threatening
process usually originating in the oropharyngeal region and
extending transcervically into the mediastinum along con-
tinuous fascial planes. While the cervical component is easy
to recognize, mediastinal involvement is less obvious, caus-
ing significant diagnostic delays. Management includes
prompt institution of broad-spectrum intravenous antimi-
crobials to cover oropharyngeal aerobes and anaerobes,
immediate contrast-enhanced cervicothoracic CT scanning,
and urgent surgical therapy directed at the oropharyngeal,
cervical, and thoracic components. Tracheostomy should be
applied selectively. Occasionally, mediastinal involvement
confined to the upper anterior mediastinal aspect may be
amenable to drainage via the transcervical approach, but the
potential for rapid, diffuse spread deeper into the medi-
astinum must be anticipated and dealt with accordingly.
Minimally invasive approaches have been reported, but gen-
erally they are inadequate to treat this process. A team of sur-
geons including otolaryngologists and thoracic surgeons
(and maxillofacial surgeons in the presence of odontogenic
infection) serves the patient best. At the outset, surgeons
should acknowledge the likely need for multiple operations.
Endocarditis can be seen in surgical patients. This diag-
nosis is particularly likely in the febrile patient with a posi-
tive blood culture and new murmur. Other classic signs of
endocarditis (eg, splinter hemorrhages, Osler’s nodes, and
Janeway’s lesions) are often absent in acute endocarditis.
Risk factors include intravenous drug abuse (IVDA), poor
dental hygiene, long-term hemodialysis, diabetes mellitus,
mitral valve prolapse, and rheumatic heart disease. In the
ICU, endocarditis can occur in patients admitted for other
reasons but who require multiple intravascular catheters.
Enterococci, though overwhelmingly associated with bac-
teremia rather than endocarditis, can be a cause of endo-
carditis in this patient group, and the organisms are
commonly resistant to many antibiotics. Previously, viridans
streptococci led the list of causative bacteria. In most recent
series, S. aureus predominates. Polymicrobial endocarditis is
unusual and generally associated with IVDA. Blood cultures
positive for Streptococcus bovis suggest a colon lesion in
older patients, warranting colonoscopy. Endocarditis
involves native valves 75–93% of the time, with prosthetic
valve infection comprising the remainder. As for the latter,
infections occurring within 2 months of surgery are thought
to be hospital-acquired. If onset exceeds 12 months from
time of surgery, the endocarditis is considered community-
acquired. Between 2 and 12 months, valve infection can be
either origin.
Echocardiography is the primary diagnostic modality
for endocarditis. Transthoracic echocardiography (TTE)
has sensitivity as low as 70% but a specificity approaching
98% for identification of the characteristic vegetations.
When suspicion remains high despite a negative TTE, or
additional detail is required for operative planning, trans-
esophageal echocardiography (TEE) is indicated. TEE sen-
sitivity for endocarditis is around 95%, with a negative
predictive value around 92%. Despite its more invasive
nature, TEE offers a much better view of the cardiac inte-
rior. TEE is particularly valuable for assessment of pros-
thetic valves and evaluation for myocardial abscess. The
latter is associated with conduction system disturbances.
Surgery is indicated urgently to address acute valvular
incompetence, myocardial abscess, or continued septic
embolization despite apparently adequate antibiotic cover-
age. Sometimes multiple cultures are negative in the febrile
patient with a positive echocardiogram. If the laboratory is
alerted to this situation, special culture techniques can be
employed to capture fastidious organisms. For patients
undergoing surgery, the polymerase chain reaction (PCR)
can be run to identify otherwise unculturable organisms
obtained from valve tissue or peripheral emboli.
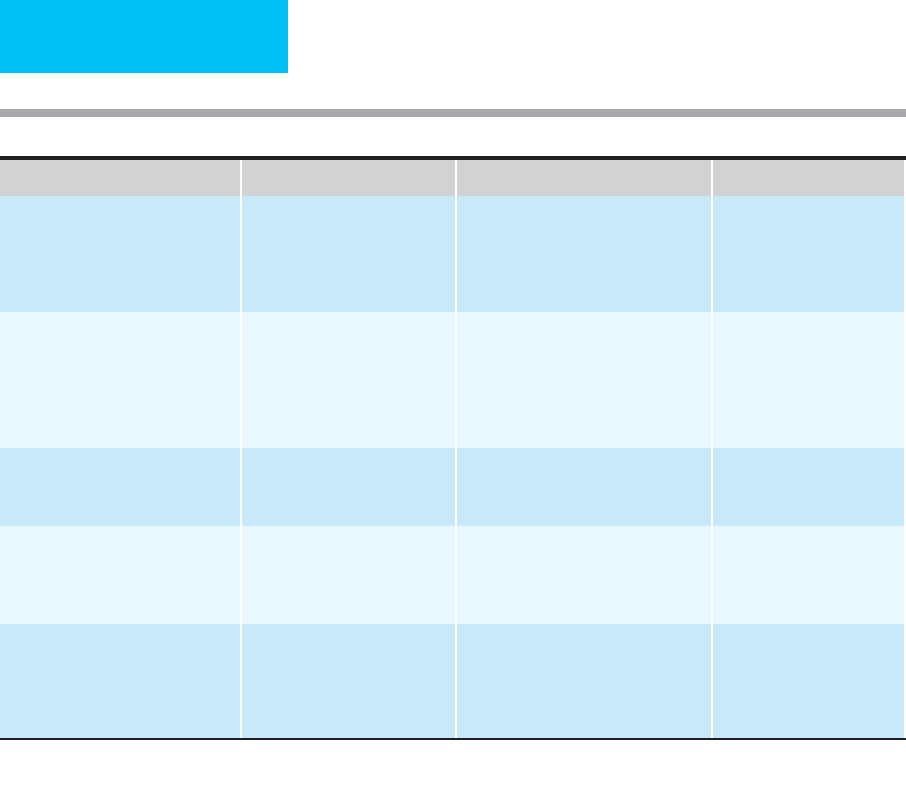
Treatment of thoracic infections is summarized in
Table 16-2.
American Thoracic Society: Executive summary: Guidelines for
the management of adults with hospital-acquired, ventilator-
associated, and healthcare-associated pneumonia. Am J Respir
Crit Care Med 2005;171:388–416. [PMID: 15699079]
Cocanour CS et al: Decreasing ventilator-associated pneumonia in
a trauma ICU. J Trauma 2006;61:122–30. [PMID: 16832259]
Freeman RK et al: Descending necrotizing mediastinitis: An analy-
sis of the effects of serial surgical debridement on patient mor-
tality. J Thorac Cardiovasc Surg 2000;119:260–7. [PMID:
10649201]
Gilbert DN et al (eds): The Sanford Guide to Antimicrobial Therapy,
37th ed. Sperryville, VA: Antimicrobial Therapy, Inc., 2007.
Light RW: Parapneumonic effusions and empyema. Proc Am
Thorac Soc 2006;3:75–80. [PMID: 16493154]
Minei JP et al: Guidelines for prevention, diagnosis and treatment
of ventilator-associated pneumonia (VAP) in the trauma
patient. J Trauma 2006;60:1106–13. [PMID: 16688078]
Mylonakis E, Calderwood SB: Infective endocarditis in adults.
N Engl J Med 2001;345:1318–30. [PMID: 11794152]
Pierracci FM, Barie PS: Strategies in the prevention and manage-
ment of ventilator-associated pneumonia. Am Surg 2007;73:
419–32. [PMID: 17520992]
Abdomen and Pelvis
This broad class includes infections of the GI mucosa or full
bowel thickness, visceral infarction, abscesses, and diffuse
peritonitis. Infections also occur secondary to mechanical
blockage of the biliary tract (eg, ascending cholangitis and
cholecystitis), urinary tract (eg, pyelonephritis and cystitis),
and female internal genitalia (eg, tubo-ovarian abscess and
pelvic inflammatory disease). Peritonitis occurs in primary,
secondary, and tertiary forms. Primary (spontaneous) bacte-
rial peritonitis truly can be spontaneous (eg, Pneumococcal
peritonitis seen in young girls) or more commonly a compli-
cation in cirrhotic patients with ascites or in those receiving
CHAPTER 16
404
peritoneal dialysis. Tuberculous and other granulomatous
forms of peritonitis also are included in this group. In these
instances, there is no leak of organisms from the GI tract.
Secondary peritonitis occurs when there is perforation of a
hollow viscus, such as in duodenal ulcer, anastomotic leak,
appendicitis, or diverticulitis. The further along the GI tract
a perforation occurs, the higher is the bacterial density.
Whereas gastroduodenal perforations are best described as
causing chemical peritonitis complicated by the presence of
bacteria, colonic perforation delivers an enormous load of
bacteria into a peritoneal space that secondarily becomes an
altered, low-pH environment. Sometimes perforations are
contained by surrounding structures such as omentum or
adjacent bowel loops. This produces focal rather than diffuse
peritonitis that is often amenable to antibiotic therapy with
or without percutaneous drainage. Surgical therapy can be
postponed or even avoided altogether. Patients often can be
spared the two-stage emergency procedure with its associ-
ated temporary colostomy. Examples include perforated
appendicitis and diverticulitis with abscess. Diffuse second-
ary peritonitis, on the other hand, requires urgent operative
intervention.
Two phases of secondary peritoneal infections have been
described. Initially, hundreds of bacterial species exit into the
peritoneum on colonic perforation, but within short order
these numbers are reduced to two or three pathogenic
species (simplification). These organisms are predictable
because only a few species can survive in the unusual envi-
ronment of peritonitis: obligate anaerobes such as
Bacteroides fragilis and endotoxin-producing members of the
family Enterobacteriaceae that includes facultative anaerobes
such as Escherichia coli. These bacteria work together (syner-
gism) to produce both abscess formation and systemic sepsis.
Included in this synergistic relationship are Enterococcus
species, at least with regard to abscess formation and wound
infection. However, Enterococcus is of questionable impor-
tance when the other two groups are surgically reduced and
then eliminated by appropriate antibiotics and host defenses.
Diagnosis Organisms Initial Antibiotics Adjunctive Therapy
Ventilator-associated pneumonia (VAP)
S. pneumoniae, S. aureus,
P. aeruginosa, Acinetobacter
sp.,
Stenotrophomonas maltophilia,
coliforms, anaerobes
Imipenem 500 mg IV q6h
or
meropenem
1 g IV q8h (+ vancomycin 1 g IV q12h if
ICU MRSA pneumonia rate high)
or
cefepime 2 g IV q8h
or
high-dose
piperacillin-tazobactam + vancomycin
Prevention, quantitative
sputum cultures, ICU
antibiogram
Empyema
S. pneumoniae, S. aureus
(consider MRSA),
S. pyogenes,
S. milleri, H. influenzae,
Bacteroides
sp.,
Enterobacteriaceae
Cefotaxime 1–2 g IV q4–12h
or
ceftriax-
one 1–2 g IV q24h (+ clindamycin
450–900 mg IV q8h for possible anaer-
obes)
or
nafcillin-oxacillin 2 g IV q4h
(MSSA)
or
vancomycin 1 g IV q12h
(MRSA)
Thoracostomy tube,
intrapleural thrombolytics,
VATS, thoracotomy
Mediastinitis after sternotomy
S. aureus,
possible MRSA Vancomycin 1 g IV q12h Surgical debridement, medi-
astinal inflow-outflow
catheters
Other mediastinitis MRSA/MSSA, coliforms,
Bacteroides
sp., and other
anaerobes
Piperacillin-tazobactam 3.375 g IV q6h
(
or
ceftazidime 2 g IV q8h + metronidazole
15 mg/kg IV q12h
or
a carbapenem IV)
+ vancomycin 1 g IV q12h
Surgical debridement
Endocarditis
S. aureus, S. epidermidis
(prosthetic valve),
viridans
strep,
S. bovis,
enterococci
Vancomycin 1 g IV q12h + gentamicin
1–1.5 mg/kg IV q8h × 14 days
or
(for
penicillin-sensitive organisms) penicillin
G 18–30 million units in divided doses IV
q4h + gentamicin
Valve repair or replacement,
myocardial debridement
Data from Gilbert DN et al (eds): The Sanford Guide to Antimicrobial Therapy, 37th ed. Sperryville, VA: Antimicrobial Therapy, Inc., 2007.
Table 16–2. Summary of thoracic infections in adult surgical patients.

SURGICAL INFECTIONS
405
Wound infection is largely eliminated by the practice of leav-
ing the cutaneous portion of the surgical wound open to
allow healing by secondary intention. Addition of ampicillin
or other antienterococcal antibiotics (part of the old main-
stay of “triple antibiotic coverage”) is now considered
anachronistic. Since the mid-1990s, appropriate antibiotic
treatment of secondary peritonitis has included metronida-
zole to cover most strains of B. fragilis and a non-
antipseudomonal third-generation cephalosporin to cover
the important Enterobacteriaceae organisms. This remains a
reasonable combination today, although some single-agent
strategies have shown equivalent efficacy. Intraoperative
peritoneal cultures are of little value because the important
pathogens are predictable from the pathophysiology.
Overall, the management goals for secondary peritonitis
as outlined by Wittmann, Schein, and Condon in the mid-
1990s remain true today. Supportive treatment includes pro-
vision of appropriate antibiotics, treatment of hypovolemia
and shock, optimizing tissue oxygenation, nutritional sup-
port, and support of failing organ systems. Surgical measures
include early source control, mechanical cleansing of the peri-
toneal cavity, recognition and avoidance of abdominal com-
partment syndrome, and identification and drainage of
persistent or recurrent infection. As discussed earlier, antibi-
otic treatment is necessary only until there is absence of fever,
normalization of leukocytosis, and resolution of ileus.
Presence of any of these beyond 5–7 days prompts a search for
undrained infection, not addition of extra antibiotics. Culture
of fluid collected with image-guided drainage may be of value
to direct adjunctive antibiotic therapy at this stage.
Tertiary peritonitis is an entity occurring late in the
course of treatment for secondary peritonitis. In patients
with persistent multiple-organ dysfunction after seemingly
appropriate treatment of intestinal perforation, diligent
searches for undrained infection are usually undertaken.
Abdominal or pelvic collections revealed by CT scan are
tapped, only to demonstrate organisms of low pathogenicity.
Unfortunately, the finding of organisms like S. epidermidis,
Candida albicans, and even A. baumannii only confirms the
existence of tertiary peritonitis rather than suggesting defin-
itive antimicrobial treatment. This really only identifies one
more organ that is failing, the peritoneum. Drainage of such
collections and intensifying antibiotic coverage probably
provide little benefit. Optimization of nutritional support
and oxygen delivery are at least as effective as seemingly more
direct measures.
There are a number of other life-threatening intraabdom-
inal infections besides peritonitis. Examples include ascend-
ing cholangitis, gangrenous cholecystitis, and necrotizing
pancreatitis. Acute biliary obstruction in and of itself does not
require urgent intervention. However, when coupled with
fever, leukocytosis, and hemodynamic changes, biliary tract
decompression in needed emergently. Causative bacteria are
predictably enteric organisms, primarily anaerobes and gram-
negative rods, and antibiotic selection is straightforward in
most cases. High blood levels of appropriate antimicrobials
are more helpful than high biliary concentrations. More
important than antibiotic therapy is prompt biliary drainage
via endoscopic retrograde cholangiopancreatography (ERCP).
When ERCP is either unavailable or unsuccessful, percuta-
neous or surgical drainage is required. Gangrenous cholecys-
titis, identified by the presence of air in the gallbladder wall
noted on imaging studies, requires urgent cholecystectomy.
Other forms of cholecystitis, including the acalculous form
complicating critical illness, can be treated by percutaneous
transhepatic cholecystostomy tube placement. The transhep-
atic route prevents spillage of any purulent fluid into the peri-
toneal cavity. Interval cholecystectomy can be performed
when the patient’s condition has improved.
Pancreatic infections can be particularly difficult to sort
out. Severe pancreatitis without sepsis can produce fulminate
SIRS and ARDS that can be confused with sepsis. Presence of
air bubbles within an edematous or necrotic pancreas indi-
cates infection requiring an aggressive surgical approach. In
the absence of this finding, the deteriorating patient with
necrotizing pancreatitis should undergo CT-guided fine-
needle aspiration for Gram stain and culture of the most
prominently involved area. Although this risks introducing
infection to sterile pancreatic necrosis, high mortality can be
expected if true infection is missed and surgery is withheld.
Recently, a number of minimally invasive approaches have
been reported for the surgical management of this problem.
As for other necrotizing infections, however, the need for
multiple surgical interventions should be anticipated. When
infection is not present, the value of pancreatic necrosectomy
in the critically ill is controversial. The value of prophylactic
systemic antibiotics (eg, carbapenems), widely employed
previously, has been debated recently. Other pancreatic infec-
tions, such as infected pseudocyst, often are amenable to per-
cutaneous drainage. Creative combinations of endoscopic
and transcutaneous drainage can eliminate the need for
complex open surgery in many cases.
Other important surgical infections of the abdomen and
pelvis include a variety of abscesses (eg, subdiaphragmatic,
hepatic, splenic, and perinephric), and complications of
blunt and penetrating trauma, gastroenteritis, bowel
ischemia, inflammatory bowel disease (ie, Crohn’s and ulcer-
ative colitis), vasculitis, antibiotic-associated colitis, and sex-
ually transmitted diseases in women. Appropriate treatment
includes attention to the primary causes.
Whether owing to hemorrhage, SIRS, or septic shock, vis-
ceral and peritoneal edema can produce a dangerous rise in
intraabdominal pressure. Physical findings include abdomi-
nal distention, respiratory distress, and measured urinary blad-
der pressures exceeding 30 mm Hg. Patients on mechanical
ventilation manifest progressive elevation of peak inspiratory
pressures and an increasing P
CO
2
. Urine output falls, probably
owing to compression of renal veins. Decompressive laparo-
tomy is indicated to prevent a downhill spiral toward irre-
versible organ dysfunction and death.
Treatment of abdominal and pelvic infections is summa-
rized in Table 16-3.
CHAPTER 16
406
Marshall JC, Innes M: Intensive care unit management of intraab-
dominal infection. Crit Care Med 2003;31:2228–37.
Wittmann DH, Schein M, Condon RE: Management of secondary
peritonitis. Ann Surg 1996;224:10–8. [PMID: 8678610]
Soft Tissues of the Extremities and Torso
Serious soft tissue infection is another common reason for
surgical ICU admission. Cellulitis and soft tissue abscesses
can occur in patients admitted to the ICU for other conditions.
ICU clinicians commonly care for patients with compli-
cated diabetic foot infections either because of the com-
plexity of the infection or for acute management of
advanced cardiovascular disease so frequently seen in these
patients. Necrotizing fasciitis affecting the extremities and
Fournier’s gangrene are two life-threatening infectious
processes often faced by intensivists. Less commonly seen
but equally lethal is suppurative thrombophlebitis. Most of
these infections are caused by multiple organisms working
synergistically to produce tissue destruction, bacteremia,
Diagnosis Organisms Initial Antibiotics Adjunctive Therapy
Primary peritonitis Enterobacteriaceae,
S. pneumoniae,
enterococci,
anaerobes,
S. aureus,
∗
S. epider-
midis,
∗
P. aeruginosa
∗
Cefotaxime 2 g IV q4–8h
or
ticarcillin-
clavulanate 3.1 g IV q6h
or
piperacillin-
tazobactam 3.375 g IV q6h
or
ampicillin-sulbactam 3 g IV q6h
or
ceftriaxone 2 g IV q24h or ertapenem
1 g IV q24h
Removal of PD catheter as
indicated
Secondary peritonitis Enterobacteriaceae,
Bacteroides
sp., enterococci,
P. aeruginosa
Ceftriaxone 1–2 g IV q24h + metronida-
zole 1 g IV q12h
or
imipenem 500 mg IV
q6h
or
meropenem 1 g IV q8h
Surgical source control, peri-
toneal washout, prevention
and treatment of abdominal
compartment syndrome
Tertiary peritonitis
S. epidermidis, Candida
sp.,
vancomycin-resistant enterococci
(VRE),
Acinetobacter
sp.
Antimicrobial agents of questionable
benefit
Supportive care, optimization
of O
2
delivery, nutritional
therapy, percutaneous or sur-
gical drainage
Biliary tract infection, including
ascending cholangitis (AC)
Enterobacteriaceae, enterococci,
Bacteroides
sp.,
Clostridium
sp.
Ceftriaxone 1–2 g IV q24h + metronida-
zole 1 g IV q12h
or
piperacillin-
tazobactam 3.375–4.5 g IV q6–8h
or
ampicillin-sulbactam 3 g IV q6h
or
ticarcillin-clavulanate 3.1 g IV q6h or
carbapenems IV
ERCP with sphincterotomy ±
stent placement, percuta-
neous transhepatic biliary
drainage, or surgical common
bile duct decompression
for AC
Pancreatic infections Enterobacteriaceae, enterococci,
S. aureus, S. epidermidis,
anaerobes,
Candida
sp.
Same as for biliary tract infection,
guided by fine-needle aspiration results
Prophylactic antimicrobials
controversial for sterile pan-
creatic necrosis, surgical
drainage/debridement, ERCP
with stent PD stent place-
ment, nutritional support
Pelvic inflammatory disease
Neisseria gonorrhoeae, Chlamydia
trachomatis, Bacteroides
sp.,
Enterobacteriaceae,
Streptococcus
sp.
(Cefotetan 2 g IV q12h
or
cefoxitin 2 g
IV q6h + doxycycline 100 mg IV/PO
q12h)
or
(clindamycin 900 mg IV q6h +
gentamicin 4.5 mg/kg IV q24h, then
doxycycline 100 mg PO bid × 14 days)
Several alternative antibiotic
regimens available
∗
Peritoneal dialysis (PD).
Data from Gilbert DN et al (eds): The Sanford Guide to Antimicrobial Therapy, 37th ed. Sperryville, VA: Antimicrobial Therapy, Inc., 2007.
Table 16–3. Summary of abdominal and pelvic infections in adult surgical patients.
