Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

187
008
Intensive Care Monitoring
Kenneth Waxman, MD
Frederic S. Bongard, MD
Darryl Y. Sue, MD
Physiologic monitoring is available for appropriate indica-
tions in the ICU. Monitoring should be selected and applied
to detect pathophysiologic abnormalities in patients at high
risk of developing them and to aid in the titration of therapy
to appropriate physiologic end points.
Electrocardiography
Continuous electrocardiography permits monitoring of heart
rate, detection of arrhythmias, and evaluation of pacemaker
function. It also may help detect myocardial ischemia or elec-
trolyte abnormalities. Continuous electrocardiographic mon-
itoring is indicated for patients with potential for developing
arrhythmias—particularly those with acute myocardial
infarction, traumatic cardiac contusion, following cardiac
surgical procedures, and those with a prior history of arrhyth-
mia. It is also useful for those in whom heart rate monitoring
is indicated, such as patients at risk of hemorrhage or those
undergoing fluid resuscitation. Monitoring of the ST seg-
ments is indicated for patients at risk of myocardial ischemia,
such as those with coronary artery disease who have an injury,
illness, or operation. Monitoring of the ECG also may be use-
ful to detect certain electrolyte abnormalities such as
hypokalemia during treatment of diabetic ketoacidosis.
The cardiac electrical potential available for skin surface
monitoring is between 0.5 and 2.0 mV. Because of this low
signal level, electrocardiographic systems must have good
sensing, amplifying, and display capabilities. The electrodes
used for electrocardiographic monitoring are usually com-
posed of silver–silver chloride gel (Ag/AgCl) inside an adhe-
sive pad. Prior to placement, the skin should be clean and
dry. The stratum granulosum has an electrical resistance of
50,000 Ω/cm
3
, which can be reduced to 10,000 Ω/cm
3
simply
by cleansing, which removes oils and dead cells. Difficulties
with a low signal are often remedied by reapplying the elec-
trode after cleaning the skin.
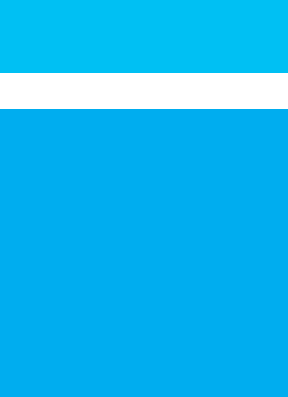
Optimal electrode placement (Figure 8–1) allows proper
detection of the electrocardiographic signals with a minimum
of extraneous noise. A “modified lead II” configuration is
appropriate for routine monitoring, with limb leads
extended proximally to lie over the shoulders. Placing them
over bony prominences reduces electrical noise from muscle
contractions.
Most electrocardiographic amplifiers and display modules
can be used for both diagnostic and monitoring applications.
The diagnostic setting permits greater amplifier bandwidth
(0.05–100 Hz) when compared with the monitor setting
(0.5–50 Hz). For routine rate and arrhythmia detection, the
monitor setting is preferred because it decreases baseline
wander, reduces unwanted interference, and improves overall
trace quality. However, because it may falsely elevate or
depress ST segments, the diagnostic mode should be selected
when myocardial ischemia is the primary concern.
Clinical Applications
A. Electrocardiographic Monitoring—Lead placement at
the shoulders and in the lead II position parallels the atria
and results in the greatest P-wave voltage of any surface lead
configuration. This facilitates recognition of arrhythmias
and inferior wall ischemia. When placed in the V
5
position
along the anterior axillary line, both anterior and lateral wall
ischemia can be detected. Because patient positioning may
make a true lead V
5
position difficult, a modified arrange-
ment (CS
5
), in which the left arm lead is placed just lateral to
the left nipple and the lower limb lead is placed over the iliac
crest, is a good alternative. When possible, leads II and V
5
should be monitored simultaneously. Esophageal leads are
better than lead II for the detection of arrhythmias, but their
use is difficult in patients who are not paralyzed and sedated,
and they are rarely used in the ICU setting.
B. Complications—Difficulties associated with electrocardio-
graphy are usually due to technical error or equipment mal-
function. Electrodes may not function properly when they are
old and dry or if they are not attached securely. Electrical noise
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
CHAPTER 8
188
accompanying the displayed electrocardiogram is usually due
to loose electrodes, broken wires, or poorly fitting contacts or
problems with associated electrical equipment. Proximity of
the patient to electrical lines (ie, power cords, etc.) produces a
potential difference through capacitive coupling known as
common-mode voltage. Typically as low as a few millivolts, cou-
pling can cause voltages as high as 20 V. Common-mode volt-
age interference usually presents as 60-Hz interference and
often can be reduced by using properly placed shielded wires,
good skin preparation, and an electrocardiographic amplifier
that offers common-mode rejection.
Proper sensitivity setting of the amplifier and recorder
is essential to make certain that large T waves are not
“double-counted” in the rate determination. Additional fil-
tering is occasionally required for patients who have
pacemakers—in whom the pacer spike is interpreted as a
QRS complex.
Goodman S, Shirov T, Weissman C: Supraventricular arrhythmias
in intensive care unit patients: Short and long-term conse-
quences. Anesth Analg 2007;104:880–6. [PMID: 17377100]
Reinelt P et al: Incidence and type of cardiac arrhythmias in criti-
cally ill patients: A single-center experience in a medical-
cardiological ICU. Intensive Care Med 2001;27:1466–73.
[PMID: 11685339]
Blood Pressure Monitoring
Because systemic blood pressure is related to both cardiac
function and the peripheral circulation, blood pressure mon-
itoring provides information related to the overall circula-
tory condition. While blood pressure monitoring is standard
and universal for critically ill patients, the type of blood pres-
sure monitoring and its frequency should be chosen based
on the individual patient’s diagnosis and condition.
Figure 8–1. Locations of the unipolar precordial leads on the body surface. (Reproduced, with permission, from
Goldschlager N, Goldman MJ: Principles of Clinical Electrocardiography, 13th ed. Originally published by Appleton
& Lange. Copyright © 1989 by The McGraw-Hill Companies, Inc.)
Midclavicular line
Anterior axillary line
Midaxillary line
Horizontal plane
of V
4-6
V
5R
V
4R
V
3R
V
1
(V
2R
)(V
1R
)
V
2
V
3
V
4
V
5
V
6
V
6R
V
7
V
7R
V
8
V
8R
V
9
V
9R
1
2
3
4
5
6
INTENSIVE CARE MONITORING
189
Blood pressure represents lateral force exerted on the vas-
culature by flowing blood. Pressure is maximal shortly after
ventricular systole (SBP). The diastolic pressure (DBP) fol-
lows cardiac diastole and is the lowest pressure in the cycle.
The mean arterial pressure (MAP) represents the standing
pressure in the arterial circuit and is calculated as follows:
Pulse pressure is the arithmetic difference between the sys-
tolic and diastolic pressures. Pulse pressures vary with stroke
volume or vascular compliance. Pulse pressures less than
30 mm Hg are common with hypovolemia, tachycardia, aor-
tic stenosis, constrictive pericarditis, pleural effusions, and
ascites. Widened pulse pressures may be due to aortic regur-
gitation, thyrotoxicosis, patent ductus arteriosus, arteriove-
nous fistula, and coarctation of the aorta. Variability of pulse
pressure and systolic pressure during the respiratory cycle has
been correlated with response to intravascular fluid repletion.
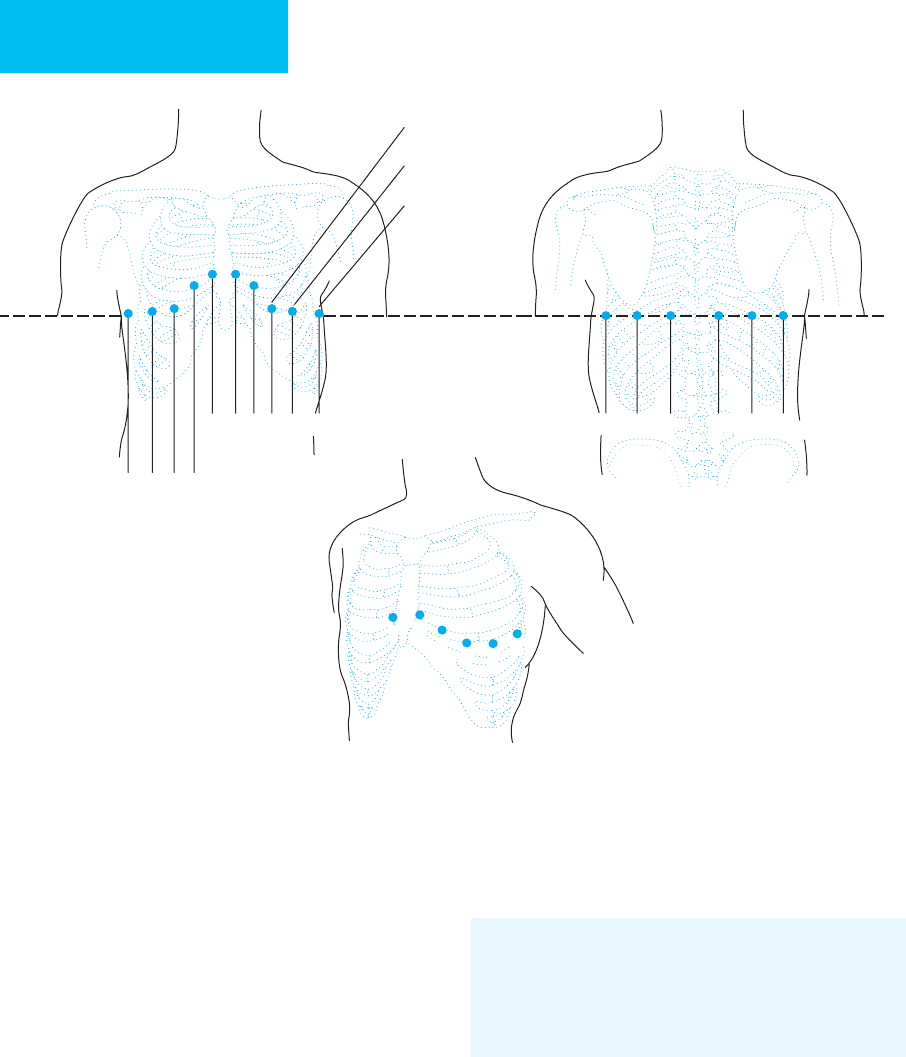
The initial upstroke and peak of the arterial waveform are
produced by left ventricular ejection. The end of systole is
marked by a brief decline in pressure until the aortic valve
closes and redirects backflowing blood into the aorta. The
“dicrotic notch” so created may be detected on recordings
obtained from aortic or proximal arterial sites. The waveform
becomes more peaked and of higher amplitude as it progresses
distally. The initial upstroke is prolonged, producing a higher
systolic and a lower diastolic pressure (Figure 8–2).
The velocity of blood flow is slowest in the largest arter-
ies because they are distensible and absorb energy from the
pressure wave front. The pulse wave travels at a rate of 7–10 m/s
in large arteries such as the subclavian artery and increases to
15–30 m/s in smaller distal arteries.
When a pressure wave front enters a small, nondistensible
artery, part of the wave may be reflected back proximally. If a
reflected wave strikes an oncoming wave, the two summate,
causing a higher pressure than would occur otherwise. This
phenomenon produces pressures in the distal peripheral
arteries that paradoxically may be more than 20–30 mm Hg
above those recorded in the aorta.
Arterial pressure depends on cardiac output (CO) and
systemic vascular resistance (SVR). The latter is calculated as
follows:
When MAP and CVP (central venous pressure) are in
millimeters of mercury and CO is in liters per minute, SVR
is expressed in dynes × seconds × cm
–5
. Evaluation of the
equation indicates that an increase in either SVR or CO will
increase mean arterial pressure.
Clinical Applications
Arterial blood pressure can be assessed either by direct
instrumentation of the vascular tree or by indirect means.
The indirect technique usually involves inflating a cuff to
occlude an artery. As the cuff is deflated and inflow resumes,
arterial pressure can be determined.
A. Noninvasive Arterial Pressure Monitoring—
1. Palpation—A blood pressure cuff is placed above an eas-
ily palpated artery and inflated until pulsation ceases. On
cuff deflation, systolic pressure is estimated as that pressure
at which pulsation resumes. This method is limited because
it underestimates true arterial pressure and does not provide
a diastolic pressure.
2. Auscultation (Riva-Rocci method)—When an occlud-
ing proximal cuff is deflated below systolic pressure, flow
begins through the compressed artery. The turbulent flow thus
created strikes the walls of the vessel, causing them to reverber-
ate (Korotkoff sounds). As long as the cuff pressure is higher
than diastolic pressure, no flow will occur during diastole. The
sound thus produced is rhythmic in nature. Once the pressure
in the cuff is below diastolic pressure, flow occurs throughout
the cardiac cycle, and the sounds disappear. A cuff 20% wider
than the diameter of the limb must be used to obtain correct
sphygmomanometric pressures. If the cuff is too narrow, the
systolic and diastolic pressures will be artificially increased,
and vice versa. Other sources of error include too-tight or too-
loose cuff application and too-rapid or too-slow cuff deflation.
SVR
(MAP CVP)
CO
=
−
× 80
MAP
(SBP DBP)
=
+×2
3
Dorsalis pedis artery
Femoral artery
Radial artery
Peripheral
Central
Aortic root
Subclavian artery
Axillary artery
Brachial artery
Figure 8–2. The shape of the arterial pressure wave
front changes as it progresses distally. The systolic peak
becomes more pronounced, as does the dicrotic notch.
(Reproduced, with permission, from Morgan GE, Mikhail
MS: Clinical Anesthesiology. Originally published by
Appleton & Lange. Copyright © 1992 by The McGraw-Hill
Companies, Inc.)

CHAPTER 8
190
Unduly slow deflation produces venous congestion, which
decreases the amplitude of the Korotkoff sounds as the cuff
pressure nears the diastolic pressure.
When compared with intraarterial pressure measure-
ments, those obtained by auscultation differ by 1–8 mm Hg
systolic and 8–10 mm Hg diastolic. At intraarterial pressures
below 120 mm Hg systolic, auscultation tends to overesti-
mate pressure, whereas above 120 mm Hg, auscultation
underestimates arterial pressure.
3. Oscillometry—The oscillometer uses two cuffs in series;
one occludes the artery proximally, whereas the other detects
the onset of pulsations. Slow deflation of the proximal cuff
produces aneroid needle oscillation or mercury column vari-
ation at systolic pressure. Oscillometry is the only noninva-
sive technique capable of indicating mean arterial pressure,
which coincides with maximum deflection of the manome-
ter. Although diastolic pressure is defined as that point at
which oscillation ceases, measurement of diastolic pressure is
in fact inaccurate. Oscillometry requires several cardiac
cycles to measure blood pressure accurately.
Automated oscillometry devices generally use single-
bladder cuffs that are alternately inflated and deflated. On
deflation, alterations in cuff pressure are sensed by a trans-
ducer inside the instrument. Pairs of oscillations and corre-
sponding cuff pressures are stored electronically to permit
measurement of the systolic and diastolic pressures. Use of
these automated devices is limited in those with irregular
rhythms or when motion cannot be minimized. In addition,
measurements tend to be unreliable in low-flow states.
4. Plethysmography—Arterial pulsations produce minute
changes in the volume of an extremity. Such alterations in
finger volume can be detected photometrically with a
plethysmograph. These devices tend to be less accurate than
alternative pressure monitoring techniques, particularly dur-
ing low-flow and stress conditions.
5. Doppler—The Doppler principle states that any moving
object in the path of a sound beam will alter the frequency of the
transmitted signal. The sound beam used to “insonate” tissue is
created by applying an electrical potential to a crystal that causes
it to oscillate in the radiofrequency spectrum. This sound is cou-
pled to the tissue of interest through an acoustic gel.
When the beam strikes moving blood cells, the frequency
of the reflected beam is altered in a manner proportionate to
the velocity of the reflecting surface. Continuous- and pulsed-
wave Doppler equipment is currently available. Continuous-
wave transducers have two crystals mounted together in a
single probe. One is continuously transmitting, and the other
is continuously receiving. Only the velocity of flow and its
direction can be determined by a continuous-wave device.
Because a Doppler shift occurs only when blood moves rela-
tive to the transducer, an angle correction must be applied:
where Δf is the frequency shift, fe is the frequency of the
insonating beam, V is blood velocity,
θ
is the incident angle
of insonation, and C is the velocity of sound in tissue.
The depth of tissue penetration by the sound beam is
inversely proportional to the frequency of insonation.
Because arteries of interest are typically superficial, a 10-
MHz probe can be used. As can be seen from the equation,
the largest frequency shift is obtained when the probe is held
parallel to the artery. Perpendicular positioning decreases the
frequency shift (cos
θ
→ 0). Doppler blood pressure meas-
urements are obtained by placing an ultrasonic probe on an
artery distal to a compressing cuff.
Doppler sounds become apparent when cuff pressure falls
below arterial pressure. Arterial pressures obtained using a
Doppler probe usually are higher than those obtained by pal-
pation and lower than those obtained by direct measurement,
although the overall correlation is excellent. An automated
device (Arteriosonde) is available for Doppler measurements.
It uses a 2-MHz insonation frequency directed at the brachial
artery. Overall accuracy is very good—especially at low pres-
sures, when ultrasonic and palpatory techniques are more
accurate than auscultation. Disadvantages include motion
sensitivity, requirement for accurate placement, and the need
to use a sonic transmission gel.
B. Invasive Pressure Monitoring—Insertion of a catheter
into an artery is the most accurate technique for pressure
monitoring. Such catheters are connected by tubing to pres-
sure transducers that convert pressure into electrical signals.
Because arterial pressure waves are themselves too weak to
generate electrical impulses, most transducers actually meas-
ure the displacement of an internal diaphragm. This
diaphragm is connected to a resistance bridge such that
motion of the diaphragm modulates an applied current. The
transducer’s sensitivity is the change in applied current for a
given pressure change.
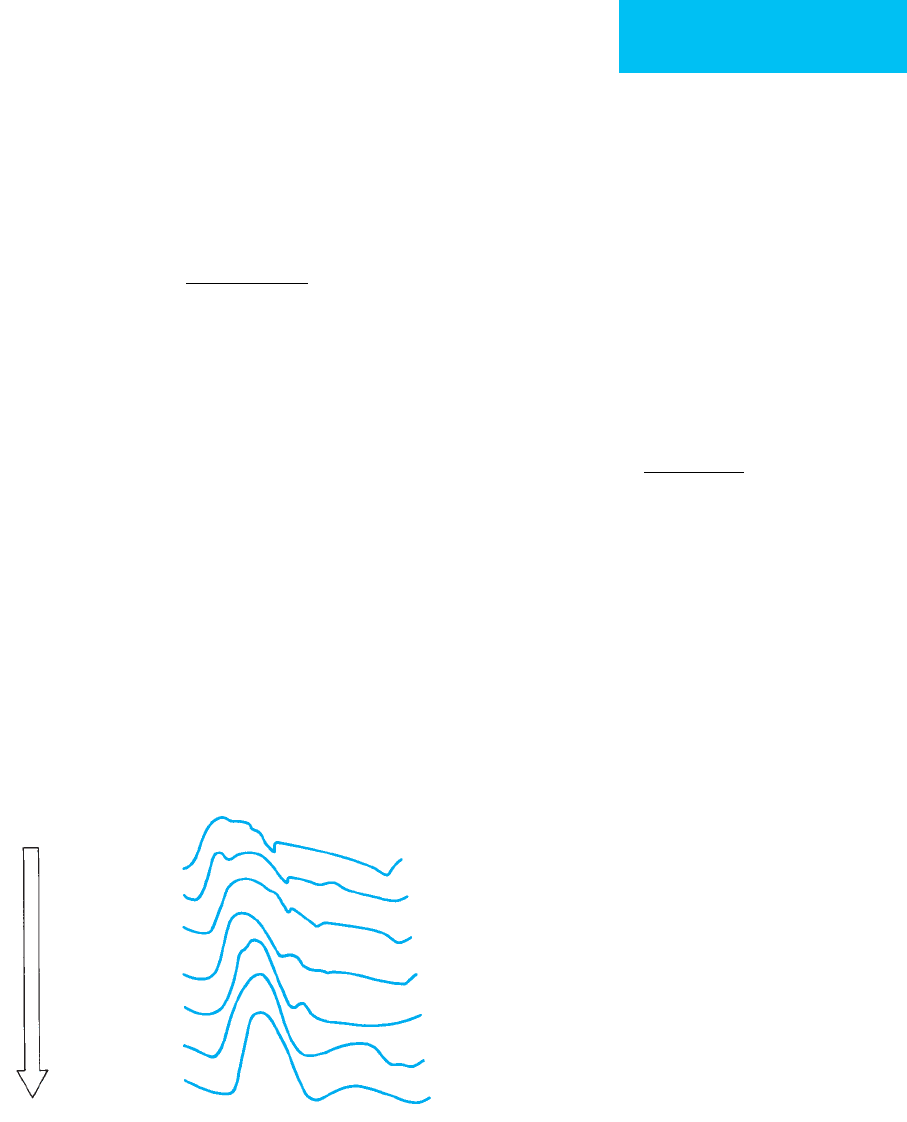
Because transducers are ultimately mechanical, they
absorb energy from the systems they monitor. If absorbed
energy in the transducer’s diaphragm is suddenly released, it
will begin to vibrate at its natural (resonant) frequency. The
tendency for this oscillation to stop depends on the damping
of the system. Oscillating frequency increases as damping
decreases. The resonant frequency is a function of the natu-
ral frequency and the damping coefficient. Classically, a sys-
tem’s damping coefficient is determined by applying and
releasing a square pressure wave (Figure 8–3).
Damping increases when compliance increases. Soft
(compliant) connecting tubing absorbs transmitted pressure
waves and damps the system. Other factors that increase
damping include air in the transducer dome or tubing, exces-
sively long or coiled tubing, connectors containing
diaphragms, and the use of stopcocks. Because air is more
compressible than water, even small bubbles increase the sys-
tem damping. Excessive damping results in underestimation
of systolic pressure and overestimation of diastolic pressure.
There is little effect on mean pressure. Underdamped systems
produce the opposite effects. Additionally, systems with
Δ
f
=
2feV
C
(cos )
θ
INTENSIVE CARE MONITORING
191
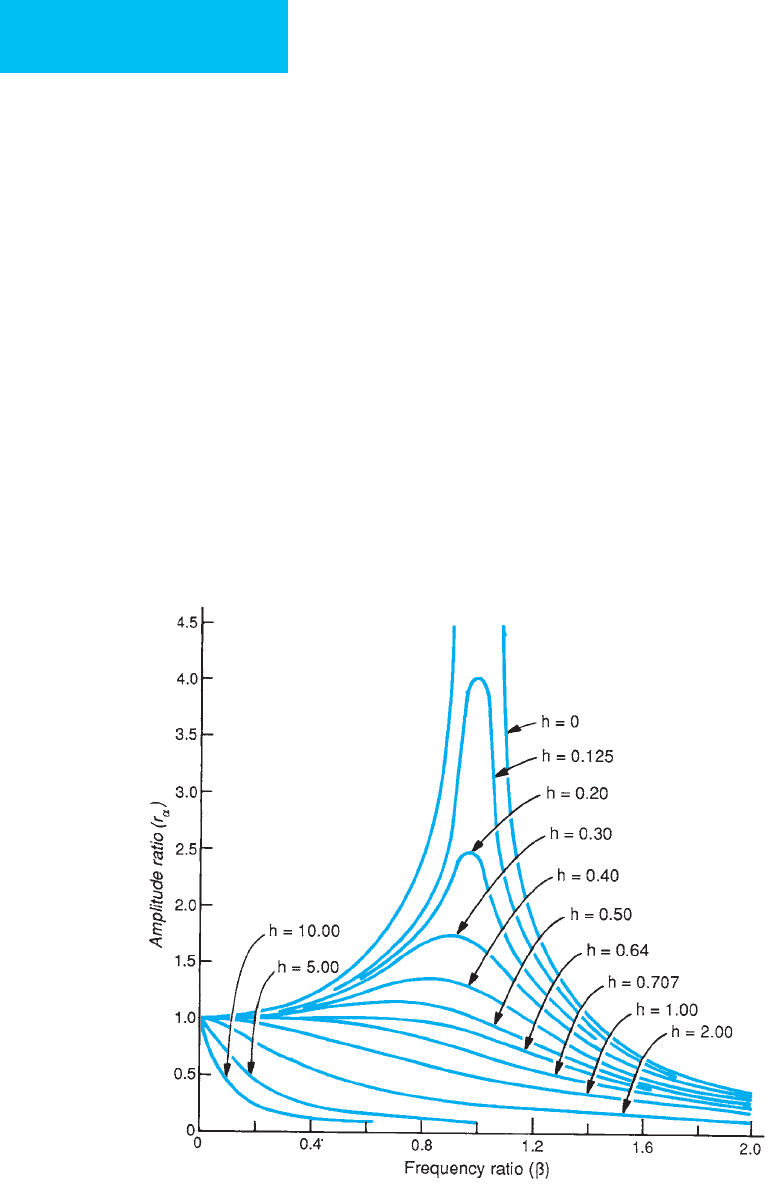
Figure 8–3. The amplitude ratio obtained by measuring the amplitude of oscillations after pressure release. Either
the listed formula or the tables then can be used to calculate the damping coefficient. (Reproduced, with permission,
from Morgan GE, Mikhail MS: Clinical Anesthesiology. Originally published by Appleton & Lange. Copyright © 1992 by The
McGraw-Hill Companies, Inc.)
CHAPTER 8
192
insufficient compliance tend to “ring” when rapid pressure
changes cause oscillations within the system. Conversely,
overdamping decreases the frequency response to the point
that rapid changes in pressure may not occur. The effect of
damping on the natural frequency of the system is illustrated
in Figure 8–4. The optimal damping coefficient is near 0.7
because there is essentially no effect on amplitude until the
measured frequency approaches the natural frequency of the
measuring system.
Clinical Applications
The arteries commonly used for invasive blood pressure
monitoring, in order of usual preference, are the radial,
ulnar, dorsalis pedis, posterior tibial, femoral, and axillary
arteries. The radial artery is preferred because of its ease of
cannulation and relatively low incidence of serious compli-
cations. The ulnar artery is the dominant artery to the hand
in 90% of patients. It connects with the radial artery through
the palmar arches in 95% of patients. Because vascular
insufficiency may result from occlusion of the dominant
artery, all patients should undergo an Allen test prior to
catheter insertion, and the results should be entered into the
medical record. However, one prospective study has demon-
strated that vascular complications were not reliably related
to results of the Allen test. Overall, there is a 10% incidence
of arterial occlusion in adults cannulated with 20-gauge
Teflon catheters for a period of 1–3 days. The use of 22-gauge
catheters seems to reduce this incidence.
For unknown reasons, women have a lower incidence of
arterial thrombosis than men. When thromboses do occur in
women, occlusions are usually temporary. Distal occlusion of
the radial artery may cause overestimation of systolic pres-
sure because of increased wave reflection, whereas proximal
occlusion usually causes reduction in pressure owing to
overdamping. Another complication of arterial catheters is
infection, most commonly limited to the skin but some-
times involving the artery as well; distal septic emboli rarely
occur. The incidence and severity of such infections can be
minimized by strict adherence to policies of daily catheter
Figure 8–4. The amplitude ratio depends on the natural frequency of the system and the damping ratio (h). A sys-
tem that operates below its natural frequency and with a damping ratio near 0.7 is desirable. (Reproduced, with
permission, from Fry DL: Physiologic recording by modern instruments with particular reference to pressure recording.
Physiol Rev 1960;40.)
INTENSIVE CARE MONITORING
193
inspection, sterile dressing changes, and limiting catheteriza-
tion to 5 days or less at any single site. Pseudoaneurysm for-
mation may be a late complication of arterial catheters. The
incidence of pseudoaneurysms may be minimized by using
smaller catheters, minimizing the duration of catheteriza-
tion, and preventing catheter infections.
Physiologic pressures are measured with reference to the
tricuspid valve, where intravascular pressure is defined as
zero. This phlebostatic axis is independent of changes in
body habitus. Postural changes affect the reference pressure
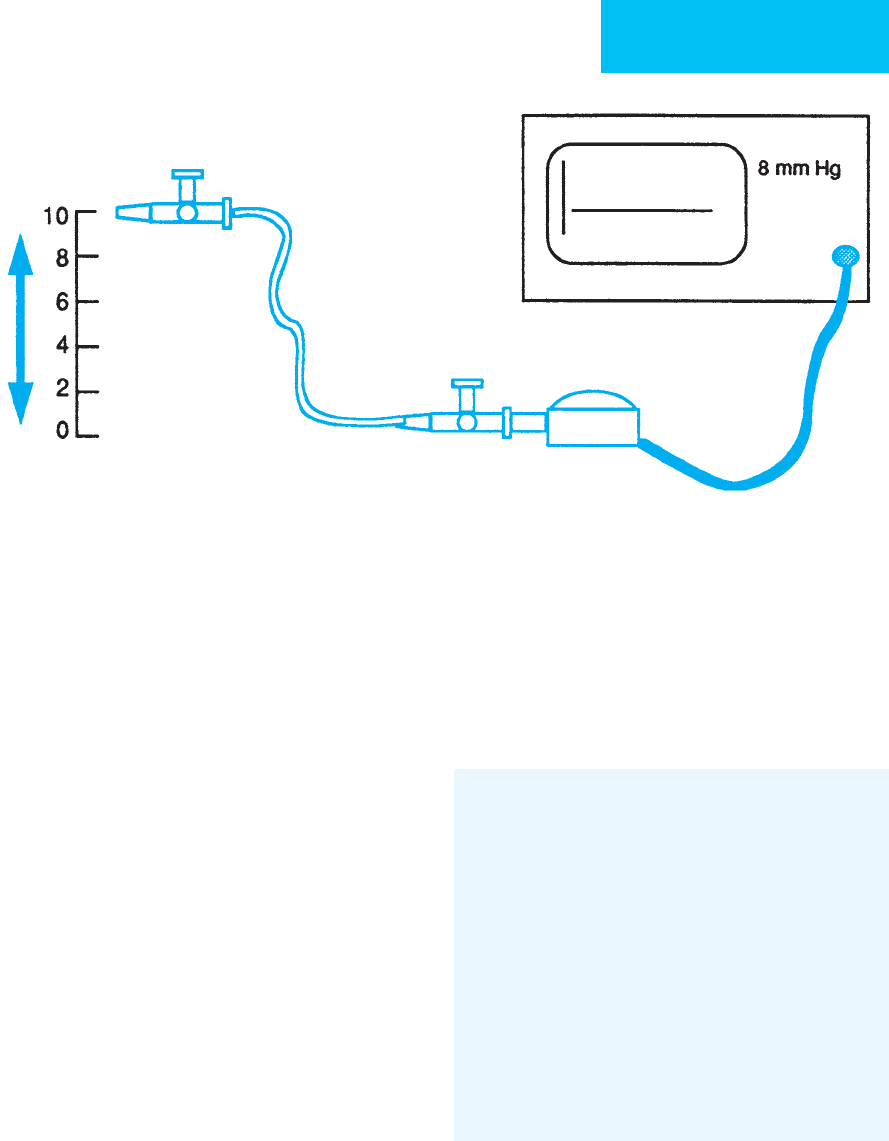
by less than 1 mm Hg. The phlebostatic point is identified as
(1) 61% of the way from the back to the front, (2) exactly in
the midline, and (3) one-quarter of the distance above the
inferior tip of the xiphoid process. A convenient method of
system calibration is to move an open stopcock attached by
fluid-filled connecting tubing to the transducer up against
the patient’s midaxillary line. The digital display on the mon-
itor indicates whether the midaxillary line is above (positive
pressure) or below (negative pressure) the transducer. The
bed is then moved up or down until the pressure reads zero
(Figure 8–5).
Calibration of the monitor for nonzero pressure can be
done internally or externally. External calibration can be
done with a mercury manometer for systemic arterial pres-
sures. A convenient method adequate for the lower pressure
range required for a pulmonary artery catheter (up to 60 cm
H
2
O) takes advantage of the fluid-filled connecting tubing.
After establishing the zero reference, move an open stopcock
connected to the transducer above the transducer a meas-
ured amount. The height above the transducer in centimeters
(cm H
2
O pressure) should be read by the monitor system in
millimeters of mercury as height in centimeters divided
by 1.36. Therefore, if the system is calibrated accurately, the
pressure reading should be about 14.8 mm Hg when the
stopcock is raised 20 cm above the transducer.
An additional use of arterial catheterization is to provide
access for arterial blood sampling. This is often indicated in
patients who require frequent sampling of blood for arterial
blood gases or other blood tests.
Araghi A, Bander JJ, Guzman JA: Arterial blood pressure monitor-
ing in overweight critically ill patients: Invasive or noninvasive?
Crit Care 2006;10:R64. [PMID: 16630359]
Bur A et al: Factors influencing the accuracy of oscillometric blood
pressure measurement in critically ill patients. Crit Care Med
2003;31:793–9. [PMID: 12626986]
Gibbs NC, Gardner RM: Dynamics of invasive pressure monitor-
ing systems: Clinical and laboratory evaluation. Heart Lung
1988;17:43–51. [PMID: 3338943]
Gunn SR, Pinsky MR: Implications of arterial pressure variation in
patients in the intensive care unit. Curr Opin Crit Care
2001;7:212–7. [PMID: 11436530]
Mignini MA, Piacentini E, Dubin A: Peripheral arterial blood pres-
sure monitoring adequately tracks central arterial blood pres-
sure in critically ill patients: An observational study. Crit Care
2006;10:R43. [PMID: 16542489]
Pittman JA, Ping JS, Mark JB: Arterial and central venous pressure
monitoring. Int Anesthesiol Clin 2004;42:13–30. [PMID:
14716195]
Central Venous Catheters
Central venous (CV) catheters are inserted via the subcla-
vian, internal jugular, or a peripheral vein in the arm.
Femoral venous catheters are not long enough to reach
“central” veins but provide similar access for intravenous
Figure 8–5. The height of the transducer must be adjusted to the phlebostatic axis to ensure accuracy of the
pressure measurements.
CHAPTER 8
194
infusions. For monitoring purposes, CV catheters provide
estimates of central venous pressure (CVP) and measure-
ment of central venous oxygen saturation (Scv
O
2
). Central
venous pressure (CVP) reflects the balance between systemic
venous return and cardiac output. In the normal heart, the
right ventricle is more compliant than the left. This differ-
ence in compliance accounts for the slope of their correspon-
ding Frank-Starling curves. The use of CVP to assess
left-sided preload causes difficulty because CVP primarily
reflects changes in right ventricular end-diastolic pressure
and only secondarily reflects changes in pulmonary venous
and left-sided pressures. The relationship between CVP and
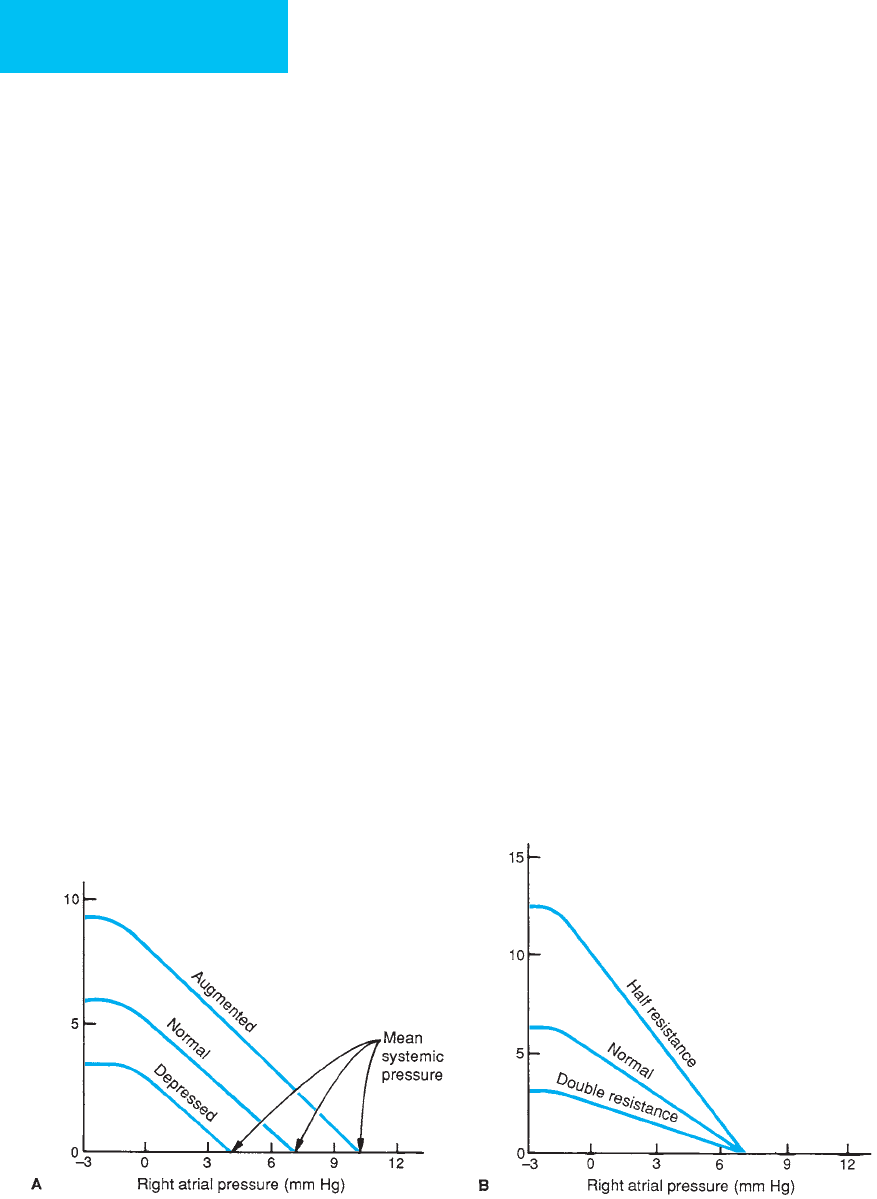
venous return is shown in Figure 8–6A. Decreasing right
atrial pressure below zero does not significantly increase
CVP because of collapse of the vasculature leading to the
chest. The figure also demonstrates that changes in mean sys-
temic pressure cause a parallel change in venous return.
Alterations in vascular resistance (decreased by anemia, arte-
riovenous fistulas, pregnancy, or thyrotoxicosis) change the
slope of the respective curves (Figure 8–6B).
A water manometer may be used to measure CVP. The
normal range of CVP is between –4 and +10 mm Hg (–5.4
and +13.6 cm H
2
O).
An electronic transducer also displays the pressure wave-
form. The bandwidth of a catheter-transducer system used to
monitor CVP can be significantly narrower than that used
for arterial pressure.
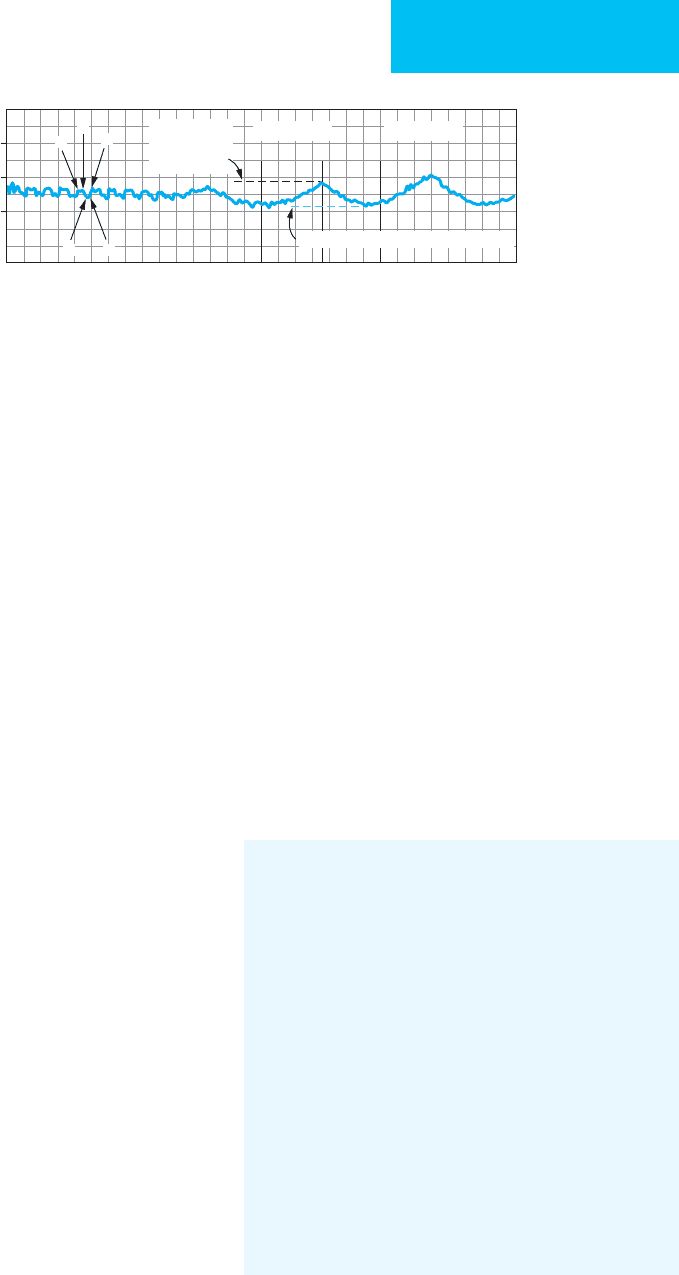
A typical CVP waveform has three positive deflections
(a, c, and v) and two descents (x and y) (Figure 8–7). The
increase in venous pressure caused by atrial contraction pro-
duces the a wave. The c wave is created when the tricuspid valve
is displaced into the right atrium during initial ventricular
contraction. The x descent corresponds to the period of ven-
tricular ejection, when blood empties from the heart; it is
inscribed when the ventricle draws down on the floor of the
atrium and decreases the CVP. The v wave is produced by the
increase in atrial pressure that takes place as venous return
continues while the tricuspid valve is closed. The y descent
occurs when the tricuspid valve opens at the conclusion of
ventricular contraction, and blood enters the right ventricle.
The a wave is absent during atrial fibrillation and is magni-
fied by tricuspid stenosis (cannon wave). The x descent also
may be absent with atrial fibrillation. The x and y descents
are both exaggerated by constrictive pericarditis. Cardiac
tamponade magnifies the x descent while abolishing the y
descent. When tricuspid regurgitation occurs, the c wave and
the x descent are replaced by a large single regurgitant wave.
Pulmonary hypertension decreases right ventricular compli-
ance and accentuates the v wave.
Clinical Applications
A. CVP Monitoring—CVP monitoring is best used for
patients without preexisting cardiac disease as one indicator
of the adequacy of venous return and cardiac filling. An
intravenous fluid challenge is employed to aid in determin-
ing whether decreased blood pressure is due to hypovolemia
or to cardiogenic failure. Measurements of CVP are affected
by ventilation because transthoracic pressure is transmitted
through the pericardium and the thin-walled venae cavae.
During spontaneous ventilation, inspiration lowers CVP, and
exhalation increases it. The situation is reversed in patients
being mechanically ventilated, in whom inspiration increases
intrathoracic pressure and elevates CVP.
Venous return (L/min)
Venous return (L/min)
Figure 8–6.
A.
Effect of mean systemic pressure on venous return.
B.
Effect of systemic vascular resistance on
venous return. (Reproduced, with permission, from Otto CW: Central venous pressure monitoring. In: Blitt CD (ed),
Monitoring in Anesthesia and Critical Care. New York: Churchill Livingstone, 1985. Copyright 1985 Elsevier.)
INTENSIVE CARE MONITORING
195
The degree of this elevation depends on the compliance
of the lungs and intravascular volume and will vary among
patients. For this reason, CVP measurements are best made
and compared at end expiration. When positive end-
expiratory pressure (PEEP) is applied, the positive pressure is
transmitted through to the right atrium, causing a decrease
in venous return and a rise in CVP. Again, the magnitude of
this effect of PEEP on CVP varies with pulmonary compli-
ance and blood volume. Some argue that the patient should
be temporarily removed from PEEP while the measurement
is taken. This is both impractical and potentially dangerous.
In critical situations, an esophageal probe can be inserted to
estimate transthoracic pressure. Subtracting the transtho-
racic pressure from the CVP provides transmural pressure,
which is a better estimate of right atrial pressure in the pres-
ence of elevated transthoracic pressure.
B. Central Venous O
2
Saturation—Mixed venous oxygen
saturation (S
–
v
O
2
) reflects the relative delivery of O
2
to the tis-
sues compared with consumption. If lower than normal,
concern should be raised about tissue hypoxia. True S
–
v
O
2
must be measured in the pulmonary artery. Central venous
O
2
saturation (Scv
O
2
) does not require a pulmonary artery
catheter, but theoretically, the value will differ from S
–
v
O
2
because Scv
O
2
obtained from a subclavian or internal jugular
vein does not reflect venous blood returning via the inferior
vena cava or coronary sinus. Generally, Scv
O
2
is about 5%
higher than S
–
v
O
2
.
In practice,however,Scv
O
2
appears to have similar predic-
tive value for end-organ hypoxia as S
–
v
O
2
. Recent studies
emphasizing early goal-directed therapy in sepsis have
emphasized a target Scv
O
2
of greater than 70% by giving
blood transfusion and cardiac inotropic drugs. Scv
O
2
can be
obtained from a small sample of blood drawn back through
the catheter or by using an oximeter-tipped CVP catheter.
C. Complications—Inadvertent arterial insertion occurs
about 2% of the time; such insertion is particularly dangerous
if large, rigid “introducer” catheters are inserted. Perforation
of the superior vena cava is associated with a 67% mortality
rate, whereas the rate associated with laceration of the right
ventricle approaches 100%. Such perforations may occur
either from guidewires or from catheter erosion—again, par-
ticularly with introducer catheters. Other structures that may
be injured on insertion include the brachial plexus, the stel-
late ganglion, and the phrenic nerve. Air emboli are uncom-
mon at insertion but more often during use or at the time of
removal when the patient is not positioned properly. Late
complications are due to catheter migration, embolization,
and infection. The incidence of cannula-related thrombosis
of the axillary and subclavian veins varies between 16.5% and
46%. Central venous catheter infections occur in approxi-
mately 5% of insertions. The organisms most commonly
involved are Staphylococcus epidermidis, 30%; Staphylococcus
aureus, 8%; streptococci, 3%; gram-negative rods, 18%; diph-
theroids, 2%; Candida species, 24%; and other pathogens, 15%.
Both colonization of central venous catheters and systemic
sepsis are reduced by routine catheter care and periodic
removal and reinsertion.
Kalfon P et al: Comparison of silver-impregnated with standard
multi-lumen central venous catheters in critically ill patients.
Crit Care Med 2007;35:1032–9. [PMID: 17334256]
Kusminsky RE: Complications of central venous catheterization.
J Am Coll Surg 2007;204:681–96. [PMID: 17382229]
Marx G, Reinhart K: Venous oximetry. Curr Opin Crit Care
2006;12:263–8. [PMID: 16672787]
Michard F, Teboul JL: Predicting fluid responsiveness in ICU patients:
A critical analysis of the evidence. Chest 2002;121:2000–8. [PMID:
12065368]
Onders RP, Shenk RR, Stellato TA: Long-term central venous
catheters: Size and location do matter. Am J Surg 2006;
191:396–9. [PMID: 16490554]
Pinsky MR, Teboul JL: Assessment of indices of preload and vol-
ume responsiveness. Curr Opin Crit Care 2005;11:235–9.
[PMID: 15928472]
Rivers E, et al. Early goal-directed therapy in the treatment of
severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
[PMID: 11794169]
Rivers E: Mixed vs central venous oxygen saturation may be not
numerically equal, but both are still clinically useful. Chest
2006;129:507–8. [PMID: 16537845]
a
c
v
yx
Inspiration Inspiration
20
10
0
Water
manometer
pressure
Mean end expiratory pressure
ExhalationExhalation
Right atrial
pressure (mm Hg)
Figure 8–7. Effect of mechanical ventilation on central venous pressure. The
a, c
, and
v
waves along with the
x
and
y
descents are shown. (Reproduced, with permission, from Otto CW: Central venous pressure monitoring. In: Blitt CD
(ed), Monitoring in Anesthesia and Critical Care. New York: Churchill Livingstone, 1985. Copyright 1985 Elsevier.)
CHAPTER 8
196
Rivers EP, Ander DS, Powell D: Central venous oxygen saturation
monitoring in the critically ill patient. Curr Opin Crit Care
2001;7:204–211. [PMID: 11436529]
Taylor RW, Palagiri AV: Central venous catheterization. Crit Care
Med 2007;35:1390–6. [PMID: 17414086]
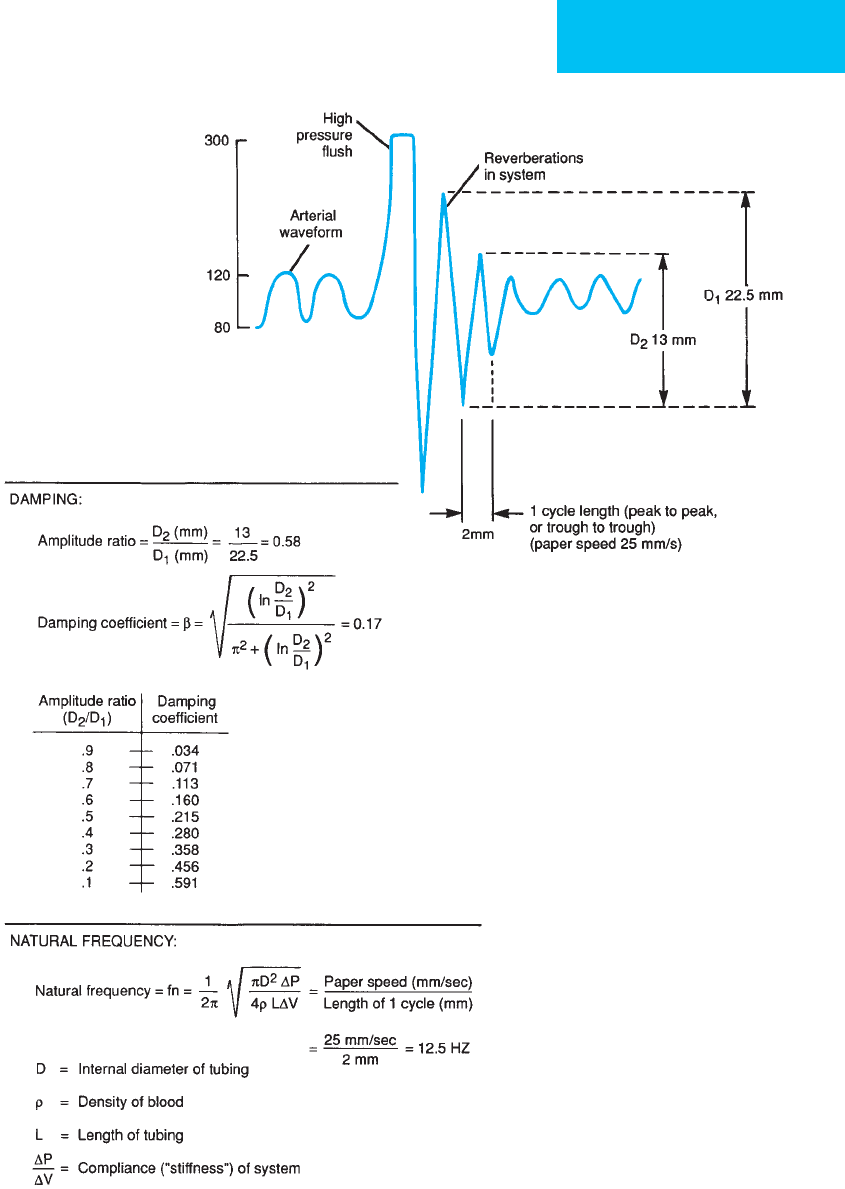
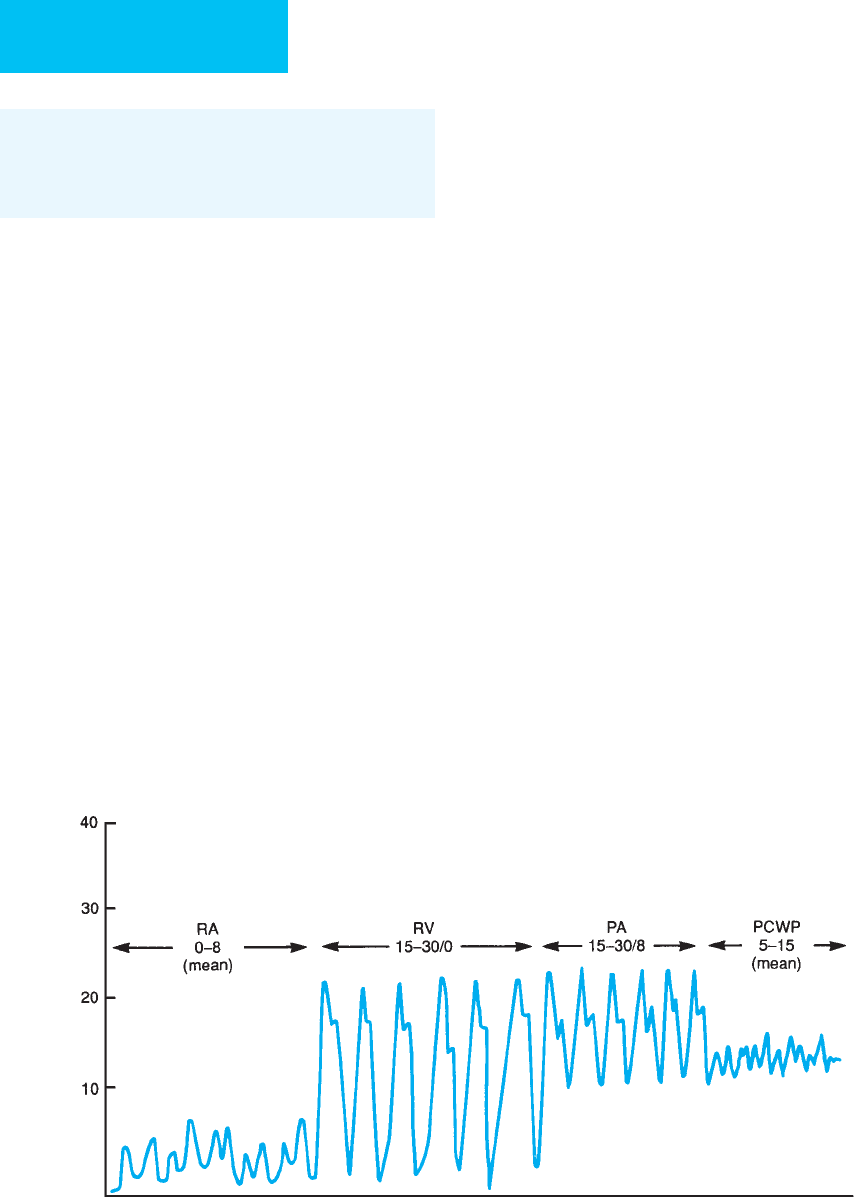
Pulmonary Artery Catheterization
Catheterization of the pulmonary artery is a useful addition
to CVP monitoring. It provides information related to left
heart filling pressures and allows sampling of pulmonary
artery blood for determination of mixed venous oxygen sat-
uration. Thermodilution cardiac output measurements are
made using a thermistor-tipped catheter.
As the balloon flotation catheter is advanced through the
heart, characteristic pressure waveforms are obtained that
indicate the position of the catheter’s distal port (Figure 8–8).
Simultaneous electrocardiographic monitoring ensures that
ventricular tachyarrhythmias will be detected as the
catheter traverses the right ventricle. After a pulmonary
capillary wedge tracing is obtained, the catheter should be
deflated and withdrawn until only 1 mL of inflation is
required to advance from a pulmonary artery to a capillary
wedge tracing. Insertion of excessive catheter length con-
tributes to intracardiac knotting. If subsequent pressure
tracings are not obtained within 15 cm of additional inser-
tion, looping should be suspected. When the catheter is
placed through either the subclavian or the jugular vein, the
typical distances required are as follows: right atrium, 10–15
cm; right ventricle, 20–30 cm; pulmonary artery, 45–50 cm;
and pulmonary capillary wedge, 50–55 cm. As the catheter
passes through the right ventricle, a wedgelike pressure trac-
ing may be obtained. This “pseudowedge” is due to engage-
ment of the catheter tip beneath the pulmonary valve or
within trabeculations. Withdrawal of 10 cm of the catheter
will solve the problem. Overinflation of the balloon, causing
it to herniate over the tip of the catheter, results in a pressure
tracing that continues to rise to high levels. The balloon
should be deflated and a short length of catheter withdrawn
before further advancement is attempted.
The final position of the catheter tip within the pul-
monary artery is critical. This may be described with refer-
ence to three lung zones that depend on the relationship of
airway and vascular pressures (Figure 8–9). In zones I and II,
mean airway pressure is intermittently greater than pul-
monary venous pressure, which results in collapse of the vas-
culature between the catheter tip and the left atrium. In this
position, observed pressures will be more indicative of air-
way pressure than of left atrial pressure. Only in zone III is
there an uninterrupted column of blood between the
catheter and the left atrium. In the supine position, zone III
assumes a more dependent position, caudal to the atrium.
Decreased airway pressures change the ventilation-perfusion
relationship, producing a relative increase in zone III.
Hypovolemia decreases vascular pressures and decreases
zone III.
Correct catheter position should be ensured by chest x-
ray. Although most catheters migrate caudally and to the
right, an occasional catheter will become wedged anterior to
the vena cava. In this position, true pulmonary capillary
pressures may be less than alveolar pressures, resulting in
spuriously elevated measurements. A lateral chest x-ray will
mm Hg
Figure 8–8. Normal pressures and waveforms obtained as a pulmonary artery flotation catheter is advanced from
the right atrium to a pulmonary artery wedge position. (Reproduced, with permission, from Morgan GE, Mikhail MS:
Clinical Anesthesiology. Originally published by Appleton & Lange. Copyright © 1992 by The McGraw-Hill Companies, Inc.)
