Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


ETHICAL, LEGAL, & PALLIATIVE/END-OF-LIFE CARE CONSIDERATIONS
217
Although rarely necessary, a legal decision can be sought
from the courts, such as in situations in which (1) the state
of the patient’s decision-making capacity is in doubt, or
(2) the surrogate decision maker cannot make or refuses to
make the decision, or (3) the health care team feels that the
surrogate’s decision is not in the patient’s best interests, or
(4) the surrogate’s decision is contrary to the patient’s
advance directive.
Shared Decision Making
Decision making in the ICU should be a shared responsibil-
ity between the physician and the patient or surrogate deci-
sion maker. The physician should avoid making
independent paternalistic medical decisions for the patient
involving life support measures even though doing so might
seem to be in the patient’s best interests. The physician is
singularly qualified to determine the medical futility of a
specific treatment, but only the patient or surrogate decision
maker can decide quality-of-life issues, that is, whether pro-
longation of life would be meaningful and valuable to the
patient. The physician should seek input from other mem-
bers of the patient’s health care team, including nurses and
other care providers.
Advance Care Planning
In an attempt to support the fundamental ethical principle of
patient autonomy, legislation has been enacted to facilitate
the process by which the patient’s wishes may be carried out
when he or she is no longer able to make decisions. That is, a
legal declaration by the patient gives the physician and health
care team advance notice of what he or she wants to be done
or not done under various future circumstances. Federal leg-
islation requires hospitals and skilled nursing facilities that
receive Medicare or Medicaid funding to inform all patients
of their right to complete such an advance directive. These
documents exist in most states, but the legal requirements
and implications vary in different jurisdictions.
The living will is the most common document by which
the patient may request or refuse life-sustaining treatment if
he or she becomes terminally ill and no longer able to make
medical decisions or becomes permanently unconscious.
Such documents are not legally binding in all states but
serve as guides for the physician and surrogate decision
maker. A legally binding natural advance death declaration
health care directive can include the decision to forego basic
life support measures of artificially administered nutrition
and hydration.
The advance health care directive appoints a health care
agent (“attorney-in-fact”) to act in the patient’s best interests
when the patient can no longer do so. Such an advance direc-
tive is most helpful when the patient has expressed his or her
wishes in writing in some detail rather than merely using
general terms such as “no heroic measures.” Ideally, individ-
uals executing these directives should discuss their intentions,
beliefs, and value systems with their health care agent, family,
and physician, in addition to completing the advance direc-
tive document. It is also important that these wishes and the
directive be reviewed on a regular basis, particularly each
time the patient is hospitalized.
Medicolegal Aspects of Decision Making
Critical care practices have been influenced by court actions
that were pursued to resolve ethical conflicts regarding
individual patients. While the actions are not legally bind-
ing outside those jurisdictions, they are used as legal prece-
dents to guide behavior and to aid in arriving at future
court decisions.
A number of cases have strengthened the ethical principle
of patient autonomy and have helped to clarify the role of the
surrogate decision maker in exercising the process of “substi-
tuted judgment” when acting for the patient. For example, in
1976, the New Jersey Supreme Court allowed the family of
Karen Quinlan to withdraw her from mechanical ventilation
because it agreed with her parents that this treatment would
not allow her to return to a cognitive and sapient life but
would merely keep her in a persistent vegetative state.
Similarly, legal decisions surrounding the care of Nancy
Cruzan in Missouri in 1990 ultimately acknowledged that
her parents as surrogate decision makers, based on past com-
ments the patient had made, could refuse life-sustaining
treatment, including nutrition and hydration.
Patient autonomy was further strengthened by the legal
determination in 1991 concerning the care of Helga Wanglie,
who was in a persistent vegetative state on a ventilator in
Minneapolis. The hospital had requested permission from
her husband to discontinue life support treatment based on
the medical decision that Ms Wanglie had no chance for
recovery, that is, that the treatment was futile. Her husband
refused, deciding that based on her religious beliefs,
Ms Wanglie would have wished to continue living. The court
affirmed Mr. Wanglie’s decision and refused to appoint an
independent conservator to replace him as decision maker.
More recently, the decision to withdraw nutrition and
hydration from Terri Schiavo, a woman in a persistent vege-
tative state following a cardiac arrest, was marked by pro-
tracted conflict between the patient’s husband and her
parents that went on for 15 years. The decision to withdraw
treatment was contested in the local, state, and federal judi-
cial systems, and even by Congress, before the treatment was
finally withdrawn, allowing the patient to die according to
her wishes shared in the past with her husband. This case
illustrates the value of advance care planning for everyone
and making one’s wishes in end-of-life care known to the
family rather than debating them later in the courts.
These precedents reaffirm the principle of patient auton-
omy, but ethical conflicts nonetheless remain, particularly
for individuals who stress the principle of justice and the fair
allocation of medical resources.

CHAPTER 10
218
Withholding & Withdrawing Life Support
Based on the ethical principles discussed in the preceding
paragraphs, the patient or the surrogate decision maker can
request that life support treatments be withheld or with-
drawn. Current judgment does not distinguish an ethical or
legal difference between the act of withholding and the act of
withdrawing life support measures. Nevertheless, the patient,
the family, and the health care team may find it more diffi-
cult to withdraw life support than to withhold it. In addition,
Orthodox Jewish tradition does not permit the withdrawing
of life support measures, including nutrition or hydration,
feeling that this would be equivalent to suicide. There is usu-
ally less concern about the more passive act of withholding
treatment.
Decisions to withhold or withdraw treatment are best
made in advance of a life-threatening situation, allowing the
patient and family to consider the potential outcome of life
support measures. This is particularly important in patients
who are terminally ill or who have an illness that is severe
and irreversible.
“Do Not (Attempt) Resuscitate (Resuscitation)”
(DNR/DNAR) Orders
In the event of cardiac or respiratory arrest in a hospitalized
patient, cardiopulmonary resuscitation (CPR) is initiated
automatically. In some cases, it may be desired to forgo CPR,
in which case a “do not resuscitate” order is written. This
decision is made jointly by the patient (or surrogate) and the
physician, but either party may initiate discussion about the
decision. In general, physicians should initiate discussions
about CPR and DNR/DNAR—ideally, before the patient
becomes critically ill and before the disease progresses to a
life-threatening stage despite optimal therapy. Some writers
have advocated use of the term “allow natural death” (AND)
as more descriptive of the intent of this order.
The physician should choose an appropriate setting for
this discussion with the patient and family, allowing ample
time for discussion. The DNR/DNAR order should be pre-
sented in a positive light, emphasizing the continuation of
supportive treatment, relief of physical suffering such as pain
and dyspnea, and support for emotional suffering. It should
be made clear that such a decision does not mean that the
health care team is “giving up” but that the focus of therapy
is altered, emphasizing comfort while avoiding futile or
unnecessary treatment.
When the outcome is bleak, the discussion should focus
not only on whether CPR should be initiated but also on
whether life support measures should be withheld or with-
drawn. The “do not resuscitate” decision does not, by itself,
imply any decisions about other medical treatment, includ-
ing ICU admission, surgery, or other treatment. Thus, if the
patient’s outcome is likely to be poor, offering CPR may give
the patient and family false hope about the likelihood of a
good outcome. A better approach is to discuss whether to
withhold or withdraw life support measures when a crisis
develops if such measures are judged to be futile. The treat-
ment plan thus should be presented in an atmosphere that
will allow the patient, family, and health care team to “hope
for the best, but prepare for the worst.”
There may be situations in which a physician recom-
mends that a DNR order be written, but the patient or fam-
ily disagrees and wishes CPR to be initiated at the time of
cardiac or respiratory arrest. In this situation, several steps
can be taken. First, the physician and patient (or surrogate)
should continue the discussion, with clarification about the
reasons for each person’s decision, misconceptions about
CPR, and the continuation or discontinuation of other med-
ical care. Second, the American Medical Association (AMA)
Council on Ethical and Judicial Affairs has decided that a
physician who determines that CPR may be futile may initi-
ate a DNR order against the patient’s wishes. In this situa-
tion, the patient must be informed of the decision and its
reasons. Third, in the event of disagreement, the patient
should be transferred to the care of another physician able to
reconcile the wishes of the patient with his or her own med-
ical judgment.
Once the decision for a DNR order is made by the patient
or physician, institutional policies and procedures should
govern how such an order should be written in order to avoid
miscommunication. Major points of the discussion with the
patient and family should be documented in the medical
record, including who participated, the decision-making
capacity of the patient, the medical diagnosis and prognosis,
and the reasons for the DNR decision.
Withholding or Withdrawing Treatment
A. A Stepwise Approach—Decisions to withhold or with-
draw life support treatment must not be made hastily.
Several steps are recommended: (1) The physician should
have a clear understanding of the patient’s diagnosis, physio-
logic and functional status, and any coexisting morbid states.
(2) The physician should seek unanimity among the health
care team for the decision to withhold or withdraw life sup-
port measures. (3) The next step is to seek informed consent
from a legally competent patient. If the patient is not legally
competent, the surrogate decision maker must be contacted.
It is wise to include the family and the patient’s referring or
primary care physician in the process, although the patient
or the surrogate decision maker holds responsibility for the
ultimate decision. (4) If a decision cannot be made in a
timely fashion and life support measures are imminently
required, the physician might consider recommending a lim-
ited trial of the life support measure—for example, ventila-
tory support for the next 72 hours, with reassessment at that
time. In the absence of a firm decision, life support measures
should be initiated or continued.
Physicians and other health care workers may fear that
their actions in withholding or withdrawing life support may
subject them to litigation or even criminal prosecution.

ETHICAL, LEGAL, & PALLIATIVE/END-OF-LIFE CARE CONSIDERATIONS
219
While no one is immune from criticism or challenge, health
care workers who act thoughtfully and rationally, with con-
cern for the patient and in the open company of their peers,
should not fear legal retribution.
B. Establish a Treatment Plan—Once a decision has been
made to withhold life support measures, a specific treatment
plan should be formulated with emphasis on providing com-
fort and support and continually adjusting the plan to meet
the changing needs of the patient. A DNR order should not
automatically preclude care for a patient in the ICU. All
efforts should be made to avoid giving the patient and fam-
ily a feeling of abandonment. Forgoing treatment does not
mean forgoing care. It may be helpful to involve the services
of a medical social worker or chaplain to make certain that
the patient and family receive appropriate emotional and
spiritual support and attention to their physical comfort.
C. Withdraw Life Support—When a decision to withdraw
life support measures has been made, the order should be
executed in a timely manner, paying close attention to the
emotional needs of the patient and family.
After the life support measure is discontinued—for
example, disconnecting the patient from mechanical
ventilation—the family should be allowed access to the
patient to the extent possible, and attention should be given
to their emotional and physical needs. If the dying process is
prolonged, the patient may be transferred to a separate room
for more privacy. Medications appropriate to control pain,
dyspnea, and other symptoms should be administered liber-
ally. Nursing care and physician attention should be as dili-
gent as before the decision was made. The primary training
and practice of critical care clinicians are to prevent and treat
life-threatening medical crises, but they also must be pre-
pared to provide palliative care, administering to the dying
patient and his or her family. A large body of educational
resources is available to assist the health care team in provid-
ing palliative care in the critical care setting.
Organ Donation
Organ transplantation has progressed rapidly in recent years
and now offers hope to patients who otherwise would die
because of failure of a vital organ. One of the limiting factors,
however, is the short supply of donor organs from individu-
als who have suffered irreversible cessation of brain stem
function.
In order to establish the diagnosis of death by neurologic
criteria, that is,“brain death,” a physician who has no conflict
of interest must verify by appropriate clinical evaluation that
the patient has suffered irreversible cessation of all brain
function. Such a diagnosis must be made in the absence of
hypothermia, drug effect, or metabolic intoxication that can
temporarily suppress the CNS. It also must be made with
caution in patients in shock because reduced brain perfusion
may make the examination unreliable. Guidelines have been
published by the American Academy of Neurology.
Because of the possibility that some patients may become
candidates for organ donation, physicians and health care
professionals in the ICU should be aware of the processes by
which donations can be made. Some patients already may
have disclosed in an advance directive that they wish to
donate body organs or tissues under these circumstances.
Otherwise, authorization for such organ donation must be
obtained from the surrogate decision maker or appropriate
family member unless the religious beliefs of the patient pre-
clude such donation (eg, Christian Science, Orthodox
Judaism, or Jehovah’s Witnesses).
Organ donation is a sensitive issue that health care
providers are often reluctant to raise, particularly at a time
when the potential donor patient’s family is suffering the
impending loss of their loved one. It is therefore necessary to
discuss these issues in a sensitive and timely manner once the
family has accepted the irreversibility of the brain damage.
Legislation in some states requires that such a discussion take
place. In the absence of any known family members or other
appropriate surrogate decision maker, the institution may be
permitted to arrange a donation in accordance with statutory
guidelines. It is important that all health care personnel be
familiar with the policies and procedures for organ donation
in order to identify potential transplant donors.
Role of the Health Care Professional
Education
All health care professionals who work in the critical care set-
ting should be intimately familiar with the ethical and legal
principles that influence their medical decision making. A
number of professional bodies have published position state-
ments on the ethical implications of critical care, and some
of these resources are listed in the references at the end of this
chapter and in the appendix of Web sites. Copies of these
statements should be readily available to critical care person-
nel. Skilled legal resources also should be available.
Discussions with patients concerning life support meas-
ures are potentially within the purview of all health care
workers, so this education should be offered to the entire
medical staff and all hospital medical personnel. The
patient’s primary physician ideally should initiate discussion
about advance directives and decisions concerning treatment
long before a crisis occurs. Such discussions can be encour-
aged through public education and by taking advantage of
opportunities to document decisions such as when preparing
wills and other estate planning instruments.
Communication Skills
In addition to possessing knowledge about the ethics of crit-
ical care medicine, health care workers should be skilled in
communicating these principles and their conflicts to
patients and families as well as among the health care team.
The physician traditionally assumes the role of the leader of
CHAPTER 10
220
that team, but critical care nurses and respiratory care prac-
titioners often develop close relationships with patients and
their families as well and can aid in the process.
Communication is aided by allowing ample time for dis-
cussing these issues in an appropriate setting—ideally, long
before a critical decision must be made. This would allow
general discussion of such sensitive issues as whether to ini-
tiate or withhold CPR or other life support measures and
other decisions about which the patient may wish to express
a preference.
Medical institutions should establish mechanisms by
which ethical conflicts can be resolved satisfactorily. This
might include the availability of ethics and/or palliative care
consultations, patient care conferences, and resources such as
patient advocates, medical social workers, and the hospital’s
retained legal advisers or others who are knowledgeable
about critical care and ethical issues.
Compassion Fatigue
Critical care professionals, by the nature of their work, are
subject to significant emotional distress in the care of criti-
cally ill and/or dying patients. This can result in compassion
fatigue, by which the emotional strain on the professional
caregivers begins to affect their decision making, care deliv-
ery, and sometimes their personal lives. Signs and symptoms
of compassion fatigue can include feelings of anger toward
the patient and family resulting in avoiding them and thus
stifling communication and empathy. This is best addressed
and/or avoided by providing an open and collegial atmos-
phere within the health care team, allowing members to dis-
cuss their feelings about caring for the patient and family.
Development of Institutional Policies
Institutional policies and procedures should be drafted to aid
the health care worker in responding to ethical issues in the
critical care arena and other areas of the hospital. A number
of such policies are listed in Table 10–2. They are designed as
much to prevent ethical conflicts as to aid in resolving them.
Guidelines for formulating these policies may be found in
the references listed below. Some state hospital associations
are also a resource for such policies.
REFERENCES
AMA Council on Ethical and Judicial Affairs: Medical futility in end-
of-life care. JAMA 1999;281:937–41. [PMID: 10078492]
AMA Council on Ethical and Judicial Affairs: Ethical considerations in
the allocation of organs and other scarce medical resources among
patients. Arch Intern Med 1995;155:29–40. [PMID: 7802518]
Berger JT: Ethical challenges of partial do-not-resuscitate (DNR)
orders: Placing DNR orders in the context of a life-threatening
conditions care plan. Arch Intern Med 2003;163:2270–75.
[PMID: 14581244]
Curtis JR et al: Missed opportunities during family conferences
about end-of-life care in the intensive care unit. Am J Respir Crit
Care Med 2005;171:844–9. [PMID: 15640361]
Meisel A, Snyder L, Quill T and the ACP-ASIM End-of-life Care
Consensus Panel: Seven legal barriers to end-of-life care. JAMA
2000;284:2495–2501. [PMID: 11074780]
Moreno R, Afonso S: Ethical, legal and organizational issues in the
ICU: Prediction of outcome. Curr Opin Crit Care 2006;12:
619–23. [PMID: 17077698]
Morrison RS, Meier D: Palliative care. N Engl J Med 2004;350:
2582–90. [PMID: 15201415]
Perkins HS: Controlling death: The false promise of advance direc-
tives. Ann Intern Med 2007;147:51–7. [PMID: 17606961]
Rubenfeld GD: Principles and practice of withdrawing life-
sustaining treatments. Crit Care Clin 2004;20:435–51. [PMID:
15183212]
Schneiderman LJ et al: Effect of ethics consultations on nonbenefi-
cial life-sustaining treatments in the intensive care setting: A ran-
domized, controlled trial. JAMA 2003;290:1166–72. [PMID:
12952998]
Snyder L, Leffler C, Ethics and Human Rights Committee, American
College of Physicians: Ethics Manual, 5th ed. Ann Intern Med
2005;142:560–82. [PMID: 15809467]
Szalados JE: Discontinuation of mechanical ventilation at end-of-
life: The ethical and legal boundaries of physician conduct in ter-
mination of life support. Crit Care Clin 2007;23:317–37, xi.
[PMID: 17368174]
Thompson BT et al, American Thoracic Society, European
Respiratory Society, European Society of Intensive Care Medicine,
Society of Critical Care Medicine, Societede Reanimation de
Langue Francaise: Challenges in end-of-life care in the ICU:
Statement of the 5th International Consensus Conference in
Critical Care, Brussels, Belgium, April 2003, Executive summary.
Crit Care Med 2004;32:1781–4. [PMID: 15286559]
Tonelle MR: Waking the dying: Must we always attempt to involve
critically ill patients in end-of-life decisions? Chest
2005;127:637–42. [PMID: 15706007]
White DB et al: Decisions to limit life-sustaining treatment for criti-
cally ill patients who lack both decision-making capacity and sur-
rogate decision-makers. Crit Care Med 2006;34:2053–9. [PMID:
16763515]
Manno EM, Wijdicks EF: The declaration of death and the with-
drawal of care in the neurologic patient. Neurol Clin
2006;24:159–69. [PMID: 16443137]
Table 10–2. Institutional policies to help prevent or
resolve ethical conflicts in critical care.
Intensive care unit admission and discharge criteria
Methods for resolving ethical conflicts
Do not resuscitate orders
Guidelines for withholding and withdrawing life support
Care of the dying patient
Definition of and procedure for determining brain death
Requesting organ or tissue donation
Organizational ethics

ETHICAL, LEGAL, & PALLIATIVE/END-OF-LIFE CARE CONSIDERATIONS
221
APPENDIX 10A
Web Sites for Health Care Ethics
Information & Policies
These Web sites were operational as of April 7, 2008:
American Medical Association: www.ama-assn.org
The Hastings Center for Bioethics: www.thehastingscenter
.org
Medical College of Wisconsin Center for the Study of Ethics:
www.mcw.edu/bioethics
University of Pennsylvania Center for Bioethics, American
Journal of Bioethics Online: www.ajobonline.com
University of Pittsburgh Consortium Ethics Program:
www.pitt.edu/~cep
University of Toronto Joint Center for Bioethics: www.
utoronto.ca/jcb
University of Washington School of Medicine Ethics in
Medicine: http://depts.washington.edu/bioethx/toc.html
Center to Advance Palliative Care (CAPC): www.capc.org
Center for Ethics in Health Care: www.ohsu.edu/ethics
StopPain.org: www.stoppain.org
The EPEC Project: www.epec.net
End-of-Life Physician Education Resource Center:
www.eperc.mcw.edu
Five Wishes (advance care planning): www.agingwithdignity
.com
Southern California Cancer Pain Initiative: http://
sccpi.coh.org

222
00
The diagnosis and management of shock are among the
most common challenges the intensivist must deal with.
Shock may be broadly grouped into three pathophysiologic
categories: (1) hypovolemic, (2) distributive, and (3) car-
diac. Failure of end-organ cellular metabolism is a feature
of all three. Hemodynamic patterns vary greatly and consti-
tute the diagnostic features of the three types of shock.
HYPOVOLEMIC SHOCK
ESSENTIALS OF DIAGNOSIS
Tachycardia and hypotension.
Cool and frequently cyanotic extremities.
Collapsed neck veins.
Oliguria or anuria.
Rapid correction of signs with volume infusion.
General Considerations
Hypovolemic shock occurs as a result of decreased circulat-
ing blood volume. The most common cause is trauma result-
ing in either external hemorrhage or concealed hemorrhage
from blunt or penetrating injury. Hypovolemic shock also
may occur as a result of sequestration of fluid within the
abdominal viscera or peritoneal cavity.
The severity of hypovolemic shock depends not only on
the volume deficit but also on the age and premorbid status
of the patient. The rate at which the volume was lost is a crit-
ical factor in the compensatory response. Volume loss over
extended periods, even in older, more severely compromised
patients, is better tolerated than rapid loss. Clinically, hypov-
olemic shock is classified as mild, moderate, or severe
depending on the blood volume lost (Table 11–1). While
these classifications are useful generalizations, the severity of
preexisting disease may create a critical situation in a patient
with only minimal hypovolemia.
Hypovolemic shock produces compensatory responses in
virtually all organ systems.
A. Cardiovascular Effects—The cardiovascular system
responds to volume loss through homeostatic mechanisms
for maintenance of cardiac output and blood pressure. The
two primary responses are increased heart rate and periph-
eral vasoconstriction, both mediated by the sympathetic
nervous system. The neuroendocrine response, which pro-
duces high levels of angiotensin and vasopressin, enhances
the sympathetic effects. Adrenergic discharge results in
constriction of large capacitance venules and small veins,
which reduces the capacitance of the venous circuit.
Because up to 60% of the circulating blood volume resides
in the venous reservoir, this action displaces blood toward
the heart to increase diastolic filling and stroke volume. It
is probable that venular constriction is the single most
important circulatory compensatory mechanism in hypo-
volemic shock.
Precapillary sphincter and arteriolar vasoconstriction
results in redirection of blood flow. The greatest decrease
occurs in the visceral and splanchnic circuits. Flow to bowel
and liver decreases early in experimental shock. Intestinal
perfusion is depressed out of proportion to reductions in
cardiac output. Reduction in flow to the kidneys accounts for
the decline in glomerular filtration and urine output,
whereas decreased skin flow is responsible for the cutaneous
coolness associated with hypovolemia. The cutaneous vaso-
constrictive response diverts flow to critical organs and has
the further effect of reducing heat loss through the skin. The
reduced diameter of the small, high-resistance vessels
increases the velocity of flow and decreases the viscosity of
blood as it reaches the ischemic vascular beds, thus permit-
ting more efficient microcirculatory flow.
Increased flow velocity in the microcirculation may
have the additional benefit of improving oxygen delivery
11
Shock & Resuscitation
Frederic S. Bongard, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
SHOCK & RESUSCITATION
223
while reducing tissue acidosis. A countercurrent exchange
mechanism has been postulated in which oxygen diffuses
from arterioles into adjacent venules. Normally, the
amount of arterial oxygen lost by this mechanism is
small. However, as flow decreases through dilated arteri-
oles, more oxygen can leave the slowly flowing arterial
blood and diffuse to the venous circuit. Arteriolar con-
striction increases flow velocity and decreases blood resi-
dence time. This effectively reduces the peripheral oxygen
shunt. In a similar fashion, CO
2
diffuses from the post-
capillary venules into the arterioles. In the absence of
arteriolar vasoconstriction, such diffusion could increase
the volume of CO
2
reaching the tissues and result in
worsening of tissue acidosis.
The balance of fluid shifts between the intravascular and
extravascular spaces is governed by Starling’s law, which
relates net transvascular flux to differences in hydrostatic and
osmotic pressure:
.
Q = K[(P
c
− P
i
) − σ(Π
c
−Π
i
)]
where Q is fluid flux, (P
c
– P
i
) is the hydrostatic pressure gra-
dient, (Π
c
– Π
i
) is the osmotic pressure gradient, K is the per-
meability coefficient, and σ is the reflection coefficient.
Under normal circumstances, intravascular hydrostatic
pressure (P
c
) is greater than interstitial hydrostatic pres-
sure (P
i
), and fluid tends to move from the capillaries into
the interstitium. Interstitial osmotic pressure (Π
i
) is usu-
ally less than the intravascular osmotic pressure (Π
c
),
favoring the movement of fluid back into the capillary.
This results in a small net movement of water, Na
+
, and K
+
out of the capillaries. When hypovolemia occurs, intravas-
cular pressure falls, facilitating the movement of fluid and
electrolytes from the interstitium back into the vascular
space. The degree of this translocation is limited because as
fluid moves back into the capillaries, the albumin remain-
ing in the interstitium exerts an increased extravascular
osmotic pressure. Compensatory vasoconstriction facili-
tates this process because fluid can be recovered more
easily if the vascular space is collapsed than if it is dilated.
The degree of such translocation is probably limited to a
total of 1–2 L. This vascular refill accounts not only for
the decrease in intravascular osmotic pressure, but it is also
primarily responsible for the decline in hematocrit
observed in hypovolemic patients before resuscitation is
started.
Increased heart rate and contractility are important
homeostatic responses to hypovolemia. Both the direct
adrenergic response and the epinephrine secreted by the
adrenal medulla are responsible for these reflexes. Cardiac
output is the product of heart rate and stroke volume. It is
supported both by tachycardia and by translocated fluid.
Because blood pressure is the product of systemic vascular
resistance and cardiac output, peripheral vasoconstriction is
an essential factor in supporting blood pressure.
B. Metabolic Effects—Tissue metabolic pathways require
ATP as an energy source. Normally, ATP is produced
through the Krebs cycle via the aerobic metabolism of
glucose. Six molecules of oxygen are consumed when six
molecules of glucose are used to convert six molecules of
ADP into six molecules of ATP, CO
2
, and water. When
oxygen is not available, ATP is generated through anaero-
bic glycolysis, which not only yields smaller quantities of
ATP for the amount of glucose consumed but also pro-
duces lactic acid. This latter product is largely responsible
for the acidosis of ischemia. The point at which tissues
change from aerobic to anaerobic metabolism is defined
as the anaerobic threshold. This theoretic point varies
between tissues and clinical situations. .The most impor-
tant factor influencing the conversion to anaerobic gly-
colysis is oxygen availability.
The delivery of oxygen depends on the quantity of oxygen
present in the blood and the cardiac output. The former,
defined as the oxygen content, is calculated as follows:
Ca
O
2
= 1.34 × Hb × Sa
O
2
+ (0.0031 × Pa
O
2
)
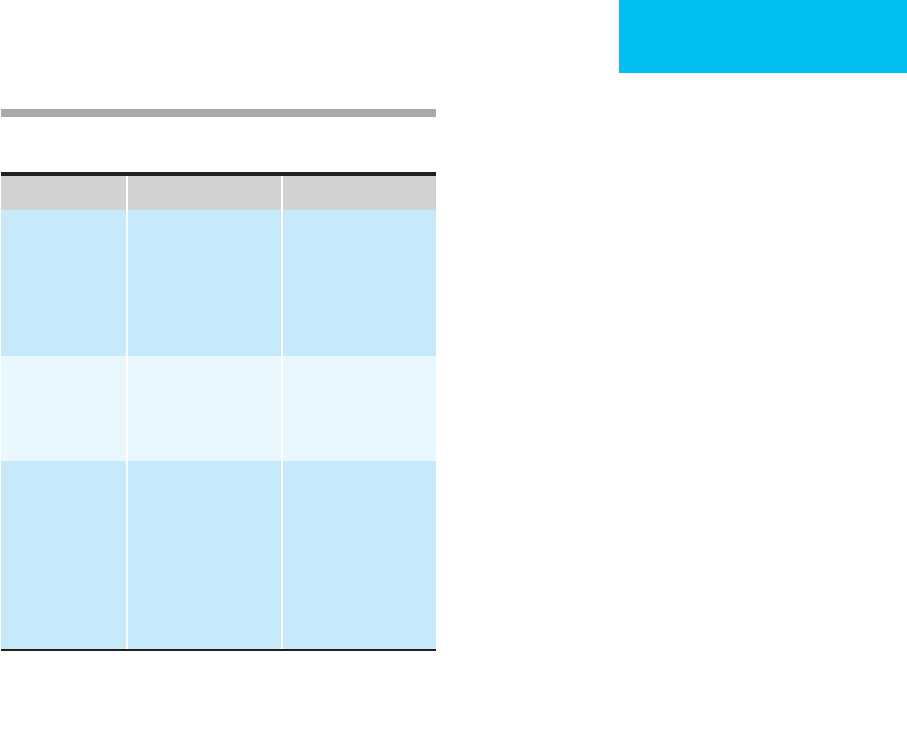
Pathophysiology Clinical Features
Mild (<20% of
blood volume)
Decreased perfusion of
organs that are able to
tolerate ischemia (skin,
fat, skeletal muscle,
bone). Redistribution of
blood flow to critical
organs.
Subjective complaints
of feeling cold. Postural
changes in blood pres-
sure and pulse. Pale,
cool, clammy skin. Flat
neck veins.
Concentrated urine.
Moderate (deficit =
20–40% of blood
volume)
Decreased perfusion of
organs that withstand
ischemia poorly (pan-
creas, spleen, kidneys).
Subjective complaint of
thirst. Blood pressure is
lower than normal in
the supine position.
Oliguria.
Severe (deficit >
40% of blood
volume)
Decreased perfusion of
brain and heart.
Patient is restless, agi-
tated, confused, and
often obtunded. Low
blood pressure with a
weak and often thready
pulse. Tachypnea may
be present. If allowed
to progress, cardiac
arrest results.
From Holcroft JW, Wisner DH: Shock and acute pulmonary failure
in surgical patients. In: Current Surgical Diagnosis and
Treatment, 9th ed. Way LW (editor). Originally published by
Appleton & Lange. Copyright © 1991 by the McGraw-Hill
Companies, Inc.
Table 11–1. Pathophysiology and clinical features of
hypovolemia.

CHAPTER 11
224
where Ca
O
2
is arterial oxygen content (in milliliters per
deciliter), Hb is hemoglobin concentration (in grams per
deciliter), Sa
O
2
is hemoglobin saturation of arterial blood (in
percent), and Pa
O
2
is partial pressure of dissolved oxygen in
arterial blood (in millimeters of mercury).
The principal determinants of oxygen content are the
concentration of hemoglobin and its saturation. Although
Pa
O
2
is the most commonly used indicator of oxygenation,
the dissolved oxygen component contributes only minimally
to oxygen content in patients with normal hemoglobin con-
centration and saturation. When anemia is profound, the rel-
ative contribution of dissolved oxygen increases. Systemic
oxygen delivery is defined as follows:
D
O
2
= Ca
O
2
× CO × 10
where D
O
2
is systemic oxygen delivery (in milliliters per
minute), Ca
O
2
is arterial oxygen content (in milliliters per
deciliter), and CO is cardiac output (in liters per minute).
Normally, D
O
2
is in excess of 1000 mL/min. When cardiac
output falls with hypovolemic shock, D
O
2
declines as well.
The extent depends not only on the cardiac output but also
on the fall in hemoglobin concentration. As oxygen delivery
declines, most organs increase their extraction of oxygen
from the blood they receive and return relatively desaturated
blood to the venous circuit. Systemic oxygen consumption is
calculated by rearranging Fick’s equation:
.
V
O
2
= (a − v)D
O
2
× CO × 10
Systemic oxygen consumption is typically 200–260 mL O
2
per minute for a 70-kg patient under baseline conditions. The
arteriovenous oxygen content difference—(a – v)D
O
2
—is
approximately 5 ± 1 mL/dL under these conditions. With
hypovolemia, oxygen consumption remains remarkably con-
stant, although peripheral oxygen extraction increases, result-
ing in an increase in (a – v)D
O
2
to values typically greater than
7 mL/dL. The oxygen extraction ratio (O
2
ER), which is defined
as
.
V
O
2
/D
O
2
, is also augmented. Increased (a – v)D
O
2
and O
2
ER
are metabolic hallmarks of hypovolemic shock.
Tissues vary greatly in their ability to increase oxygen
extraction. The normal extraction ratio is near 0.3 and may
increase to as much as 0.8 in conditioned athletes. The heart
and brain maximally extract oxygen under normal circum-
stances, making them extremely flow-dependent. Peripheral
oxygen consumption (
.
V
O
2
) remains essentially constant dur-
ing hypovolemia until a critical threshold is reached, at
which point increased extraction can no longer keep pace
with delivery. There is conflicting evidence about whether
oxygen consumption decreases in the face of reduced oxygen
delivery in humans. This so-called pathologic supply
dependence may, however, occur in patients with distributive
shock and with acute respiratory distress stndrome (ARDS).
When circulating blood volume falls sufficiently, oxygen
delivery declines, and death occurs below a critical D
O
2
of
less than 8–10 mL O
2
per minute.
Compensated shock occurs when system oxygen delivery
falls below D
O
2,crit
, and anaerobic metabolism becomes more
prevalent. Cell function is maintained as long as the combina-
tion of aerobic and anaerobic metabolism provides adequate
ATP. Tissues vary greatly in their resistance to hypoxia. While
the brain may tolerate only brief intervals, skeletal histiocytes
may withstand up to 2.5 hours of ischemia. Significantly, the
gut appears to be very sensitive to decreased perfusion.
Uncompensated shock, which results in tissue damage, occurs
when combined aerobic and anaerobic metabolism is not
adequate to sustain cellular function. Loss of cellular mem-
brane integrity results in cell swelling and ultimate cell death.
C. Neuroendocrine Effects—Adrenergic discharge and the
secretion of vasopressin and angiotensin are neuroendocrine
compensatory mechanisms that together produce vasocon-
striction, translocation of fluid from the interstitium into the
vascular space, and maintenance of cardiac output.
1. Secretion of aldosterone and vasopressin—
Together these hormones increase renal retention of salt and
water to assist in maintaining circulating blood volume.
2. Secretion of epinephrine, cortisol, and glucagon—
These hormones increase the extracellular concentration of
glucose and make energy stores available for cellular metab-
olism. Fat mobilization is increased. Serum insulin levels are
decreased.
3. Endorphins—Although their exact role is unclear, these
endogenously occurring opioids are known to decrease pain.
They promote deep breathing, which might increase venous
return by decreasing intrathoracic vascular resistance.
Endorphins have a vasodilatory effect and actually may
counteract the sympathetic influence.
D. Cellular and Immunologic Effects—Although sepa-
ration of shock and resuscitation into cellular and
immunologic effects is somewhat artificial, the distinction
provides a useful framework for the subsequent discus-
sion of resuscitation.
1. Cellular effects—Injured cells die by either apoptosis
or necrosis. Apoptosis requires energy and is a more con-
trolled than simple necrosis. Although apoptosis is required
for homeostasis, an increase in apoptosis may indicate cellu-
lar injury and organ dysfunction. Recent research has shown
that the type of resuscitation fluid used may have a signifi-
cant effect on the extent of apoptosis. Additionally, the extent
of apoptosis varies between cell types and may be particu-
larly significant in the CNS and brain.
Recent research has shown that the fluid used for resus-
citation also has an effect on cellular function. Some of the
factors thought to exert an influence include (1) the elec-
trolyte composition of the fluid used, (2) tonicity, (3) duration
of resuscitation, (4) type of cells exposed, (5) concurrent
inflammation or infection, (6) presence of additional
periods of shock or infection/contamination (“second hit”),
and (7) timing of resuscitation.

SHOCK & RESUSCITATION
225
2. Immunologic effects—Hypovolemic shock initiates a
series of inflammatory responses that may have deleterious
effects. Stimulation of circulating and fixed macrophages
induces the production and release of tumor necrosis factor
(TNF), which, in turn, leads to production of neutrophils,
inflammation, and activation of the clotting cascade.
Neutrophils are known to release free oxygen radicals, lyso-
somal enzymes, and leukotrienes C
4
and D
4
. These mediators
may disrupt the integrity of the vascular endothelium and
result in vascular leaks into the interstitial space. Activated
complement and products of the arachidonic acid pathway
serve to augment these responses.
Adhesion molecules are glycoproteins that cause leuko-
cyte recruitment and migration after hemorrhagic shock.
The most frequently involved cell adhesion molecules are the
selectins, integrins, and immunoglobulins. Although the
roles of the adhesion molecules are still under investigation,
some authorities have reported a correlation between the
severity of injury and the release of soluble cell adhesion
molecules (SCAMs). Others also have noted a relationship
between the development of multiple-organ failure and the
expression of SCAMs. The feasibility of using monoclonal
antibodies to SCAMs—as well as pathway blockade—is
under study. Isotonic crystalloid resuscitation fluids, as well
as some artificial colloids, have been demonstrated to pro-
duce an oxidative burst and the expression of adhesion mol-
ecules on neutrophils in a dose-dependent manner. Natural
colloids, such as albumin, did not create such a burst, and the
use of hypertonic saline has been shown to suppress some
neutrophil functions.
Oxygen metabolites, including superoxide anions, hydro-
gen peroxide, and hydroxyl-free radicals, are produced when
oxygen is incompletely reduced to water. These radical inter-
mediates are extremely toxic because of their effects on lipid
bilayers, intracellular enzymes, structural proteins, nucleic
acids, and carbohydrates. Phagocytes normally generate oxy-
gen radicals to assist in killing ingested material.
Antioxidants protect surrounding tissue if these compounds
leak from the phagocytes. Ischemia, followed by reperfusion,
has been shown to accelerate the production of toxic oxygen
metabolites independently of the activity of inflammatory
cells. This ischemia-reperfusion syndrome may lead to exten-
sive destruction of surrounding tissue and may play a signif-
icant role in determining the ultimate outcome of an episode
of hypovolemic shock.
Animal experiments have identified a number of other
potentially important immunologic responses to hypov-
olemia, including failure of antigen presentation by Kupffer
cells in the liver and translocation of bacteria from the gut
into the systemic circulation. This latter mechanism may
explain the occurrence of sepsis after hypotension without
other sources of infection.
E. Renal Effects—Blood flow to the kidneys decreases
quickly with hypovolemic shock. The decline in afferent flow
causes glomerular filtration pressure to fall below the critical
level required for filtration into Bowman’s capsule. The kid-
ney has a high metabolic rate and requires substantial blood
flow to maintain its metabolism. Therefore, sustained
hypotension may result in tubular necrosis.
F. Hematologic and Thrombotic Effects—When hypov-
olemia is due to loss of fluid volume without loss of red
blood cells, which occurs with emesis, diarrhea, or burns, the
intravascular space becomes concentrated, with increased
viscosity. This sludging may lead to microvascular thrombo-
sis with ischemia of the distal bed.
G. Neurologic Effects—Sympathetic stimulation does not
cause significant vasoconstriction of the cerebral vessels.
Autoregulation of the brain’s blood supply keeps flow con-
stant as long as arterial pressure does not decrease to less
than 70 mm Hg. Below this level, consciousness may be lost
rapidly, followed by decline in autonomic function.
H. Gastrointestinal Effects—Hypotension causes a decrease
in splanchnic blood flow. Animal models have shown a rapid
decrease in gut tissue oxygen tension, which may lead to the
ischemia-reperfusion syndrome or to translocation of intes-
tinal bacteria. Increased concentrations of xanthine oxidase
occur within the mucosa and also may be responsible for
bacterial translocation. Pentoxifylline has aroused recent
interest as a potential agent for increasing intestinal
microvascular blood flow after periods of ischemia.
Clinical Features
A. Symptoms and Signs—The findings associated with
hypovolemic shock vary with the age of the patient, the pre-
morbid condition, the extent of volume loss, and the time
period over which such losses occur. The physical findings
associated with different degrees of volume loss are summa-
rized in Table 11–1. Heart rate and blood pressure measure-
ments are not always reliable indicators of the extent of
hypovolemia. Younger patients can easily compensate for
moderate volume loss by vasoconstriction and only minimal
increases in heart rate. Furthermore, severe hypovolemia can
result in bradycardia as a preterminal event. Orthostatic
blood pressure testing is often helpful. Normally, transition
from the supine to the sitting position will decrease blood
pressure by less than 10 mm Hg in a healthy person. When
hypovolemia is present, the decline is greater than 10 mm Hg,
and the pressure does not return to normal within several
minutes. Older patients who present with apparently normal
blood pressures while supine often become hypotensive
when brought to an upright position. Such testing must be
used with caution in patients who have sustained multiple
injuries because potentially unstable vertebral injuries may
be present.
Decreased capillary refilling, coolness of the skin, pallor,
and collapse of cutaneous veins are all associated with
decreased perfusion. The extent of each depends on the
severity of the underlying shock. These findings are not spe-
cific to hypovolemic shock and may occur with cardiac shock

CHAPTER 11
226
or shock from pericardial tamponade or tension pneumoth-
orax. Collapsed jugular veins are commonly found in hypo-
volemic shock, although they also may occur with cardiac
compression in a patient who is not adequately fluid-
resuscitated. Examination of the jugular veins is best per-
formed with the patient’s head elevated to 30 degrees. A
normal right atrial pressure will distend the neck veins
approximately 4 cm above the manubrium.
Urine output is usually markedly decreased in patients
with hypovolemic shock. Oliguria in adults is defined as
urine output of less than 0.5 mL/kg per hour. If oliguria is
not present in the face of clinical shock, the urine should be
examined for the presence of osmotically active substances
such as glucose and radiographic dyes.
B. Laboratory Findings—Laboratory studies may be useful
in determining the cause of hypotension. However, resuscita-
tion of a patient in shock should never be withheld pending
the results of laboratory determinations.
The hematocrit of a patient in hypovolemic shock may be
low, normal, or high depending on the cause and duration of
shock. When blood loss has occurred, evaluation prior to
capillary refill by interstitial fluid will yield a normal hemat-
ocrit. On the other hand, if the patient has bled slowly, if
recognition is delayed, or if fluid resuscitation has been insti-
tuted, the hematocrit will be low. When hypovolemia results
from loss of nonsanguineous fluid (eg, emesis, diarrhea, or
fistulas), the hematocrit is usually high. A crude way to esti-
mate the extent of blood loss is to assume that the intravas-
cular space is a single compartment and that the change in
hemoglobin concentration is proportional to the extent of
blood loss and fluid replacement with nonsanguineous flu-
ids. Where H
i
is the (presumed) initial hematocrit, H
f
is the
final hematocrit, and EBV is the approximate circulating
blood volume (approximately 70% of the body weight in an
adult), the estimated blood loss (EBL) may be calculated as
EBL = EBV
× ln(H
i
/H
f
).
Lactic acid accumulates in patients with shock that is
severe enough to cause anaerobic metabolism. Both the extent
of elevation of arterial lactic acid and the rate at which it is
cleared with volume resuscitation and control of bleeding are
useful markers of the presence of ischemia and its resolution.
Failure to clear elevated arterial lactic acid is an indication of
inadequate resuscitation. If arterial lactic acid concentration
remains elevated despite seemingly appropriate fluid resusci-
tation, other causes of hypoperfusion should be sought.
Other nonspecific findings include decreased serum
bicarbonate and a minimally increased white blood cell
count. Base excess, calculated from an arterial blood gas
determination, indicates that portion on an acidosis that is
metabolic in nature. Some laboratories use the term base
deficit, which is simply the negative absolute value of the base
excess. Like lactic acid, base deficit should resolve with ade-
quate resuscitation.
C. Hemodynamic Monitoring—Assessment of central
venous pressure is seldom required to make the diagnosis of
hypovolemic shock. Because the decreased volume allows
venous collapse, insertion of central venous monitoring
catheters can be particularly hazardous. If the patient’s blood
pressure and mental status do not respond to fluid adminis-
tration, a continued source of bleeding should be suspected.
Central venous pressure monitoring may be useful in older
patients with a known or suspected history of congestive
heart failure because excessive fluid administration may rap-
idly result in pulmonary edema. In extreme cases, a pul-
monary artery flotation catheter may be required to optimize
fluid status.
Capnographic monitoring will reflect a decrease in end-
tidal CO
2
. This is produced by a decrease in blood flow to the
lungs. When compared with arterial blood gases, a widening
of the arterial–end-tidal CO
2
gradient is apparent. If pul-
monary function is normal, only minimal changes in arterial
hemoglobin saturation will be present. Hence pulse oximetry
indicates normal saturation. The introduction of noninvasive
transcutaneous tissue oxygen probes, which use near-infrared
spectroscopy to measure subcutaneous tissue oxygen tension
(St
O
2
), holds promise as a simple bedside method for deter-
mining the adequacy of resuscitation. A pilot study showed
that trauma patients who maintained St
O
2
above 75% within
the first hour of ED arrival had an 88% chance of surviving
without multiple-organ dysfunction.
Differential Diagnosis
Shock owing to hypovolemia may be confused with shock
from other causes (Table 11–2). Cardiac shock produces
signs similar to those found with hypovolemia, with the
exception that neck veins are usually distended. Absence of
such distention may be due to inadequate fluid resuscitation.
Central venous pressure monitoring will help to make the
differentiation. Following trauma, peripheral vasodilation
owing to spinal cord injury may produce shock that is rela-
tively resistant to fluid administration. Hypovolemia is the
primary cause of shock in trauma victims, and it should
never be assumed that other causes are responsible until fluid
in adequate amounts has been administered.
Alcoholic intoxication may make the diagnosis of hypov-
olemia difficult. Serum ethanol elevation causes the skin to be
warm, flushed, and dry. The patient usually makes dilute
urine. These patients may be hypotensive when supine, with
exaggerated postural blood pressure changes. Hypoglycemic
shock owing to excessive insulin administration is not uncom-
mon in the ICU. The patients are cold, clammy, oliguric, and
tachycardiac.A history of recent insulin administration should
arouse suspicion of hypoglycemic shock. After samples have
been taken for blood glucose determinations, intravenous
administration of 50 mL 50% glucose should improve the
situation.
Treatment
A. General Principles—Unlike acute posttraumatic situa-
tions, resuscitation of patients with hypovolemic shock in
