Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

INTENSIVE CARE MONITORING
197
demonstrate when the catheter has assumed this position.
Indicators of proper tip placement include (1) a decline in
pressure as the catheter moves from the pulmonary artery
into the “wedged” position, (2) ability to aspirate blood from
the distal port (eliminating the possibility of overwedging),
and (3) a decline in end-tidal CO
2
concentration with infla-
tion of the balloon (produced by a rise in alveolar dead
space). In a patient receiving positive end-expiratory pres-
sure (PEEP), another indicator of correct positioning is an
increase pulmonary capillary wedge pressure less than 50%
of any increase in PEEP. This is so because normal lung and
chest wall compliances are approximately equal at end expi-
ration. Therefore, intrathoracic pressure will increase by 50%
of PEEP, and pulmonary capillary wedge pressure also will
increase by at most 50%. Lung disease (decreased lung com-
pliance generally) will distort this relationship, but almost
always to less than 50%. If the pulmonary capillary wedge
pressure rises more than 50% of the PEEP, repositioning
must be considered.
The pulmonary capillary wedge (pulmonary capillary
occlusion) pressure (PCWP) estimates left ventricular end-
diastolic pressure and thus serves as an estimate of left ven-
tricular preload. Because the pulmonary vasculature is a
low-resistance circuit, the pulmonary artery end-diastolic
pressure in normals is usually only 1–3 mm Hg higher than
the mean pulmonary capillary wedge pressure and has been
used to estimate left ventricular pressure when the pul-
monary capillary wedge pressure is not available—but this is
unreliable and inconsistent in the case of lung disease, pul-
monary hypertension, or tachycardia. Normal values for pul-
monary artery catheter pressures are shown in Figure 8–8.
Pulmonary capillary filtration pressure (P
cap
) is a measure
of the potential difference that drives fluid from the pulmonary
vasculature into the perivascular interstitial and alveolar spaces.
The contribution of hydrostatic and osmotic pressure differ-
ences to fluid filtration is described by Starling’s law. The equa-
tion relating mean PA pressure, PCWP, and P
cap
is
P
cap
= PCWP + 0.4 × (PA – PCWP)
Adult respiratory distress syndrome (ARDS) widens the
PA-to-PCWP gradient and increases P
cap
, contributing to
pulmonary edema.
Clinical Applications
A. Pressure Measurements—In most instances, PCWP is
an accurate indicator of left ventricular end-diastolic pres-
sure. Correlation between CVP and PCWP may be poor in
critically ill patients with cardiopulmonary disease because
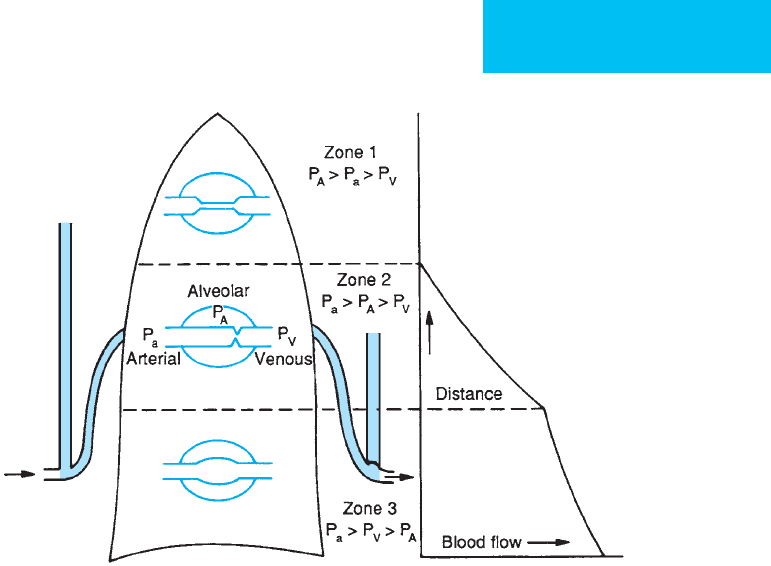
Figure 8–9. The effect of airway pressure on the pulmonary vasculature is divided into three zones. A pulmonary
artery flotation catheter should wedge in zone III, where there is a continuous column of blood between the pul-
monary capillary and the left atrium. (Reproduced, with permission, from West JB, Dollery CT, Naimark A: Distribution of
blood flow in isolated lung: Relation to vascular and alveolar pressures. J Appl Physiol 1964;19:713.)
CHAPTER 8
198
of differences between right and left ventricular function. In
this group, both absolute values and relative changes in CVP
are unreliable because alterations in the pulmonary vascular
bed affecting the right side of the heart do not equally affect
the left ventricle. This is of particular importance following
pulmonary embolization, which increases right ventricular
afterload without affecting left ventricular end-diastolic
pressure. CVP and pulmonary systolic and diastolic pres-
sures are all elevated, whereas PCWP is decreased because of
the decline in forward flow.
PCWP correlates best with left atrial pressure (LAP) when
the latter is less than 25 mm Hg. However, PCWP will be
lower than LAP in hypovolemic patients, whose pulmonary
vasculature collapses during peak inspiration. When LAP
increases to more than 25 mm Hg—which may occur after
acute myocardial infarction with decreased left ventricular
compliance—PCWP tends to underestimate left-ventricular
end-diastolic pressure (LVEDP). As left ventricular function
deteriorates, the contribution that atrial contraction makes to
left ventricular filling is increased, and LVEDP can be signifi-
cantly higher than PCWP. Several conditions affect the accu-
racy of PCWP as an indicator of LVEDP. In mitral stenosis,
left atrial pressure at end diastole may be significantly higher
than left ventricular pressure. This is diagnosed by the pres-
ence of large v waves on a PCWP tracing. Large left atrial
myxomas also elevate PCWP. Aortic regurgitation produces
an underestimation of LVEDP by PCWP because the mitral
valve closes early despite increasing left ventricular pressure.
Mitral regurgitation results in accentuation of LVEDP
because of backward flow during systole. Pericardial tampon-
ade restricts filling of all four cardiac chambers and results in
an equalization of CVP and PCWP because all such pressures
are under the restrictive influence of the tamponade. Positive
end-expiratory pressure (PEEP) adversely affects the ability of
PCWP to monitor left ventricular preload. High positive air-
way pressures (PEEP >15 mm Hg) can result in pulmonary
vascular collapse, causing PCWP to reflect airway pressure
instead of left atrial pressure (conversion from zone III to
zone I). As with CVP, an esophageal pressure transducer per-
mits calculation of transmural rather than transthoracic pres-
sures. However, because pulmonary compliance is not
disturbed uniformly, the pressure obtained through the
esophageal probe may not correctly reflect the pressure that
surrounds the pericardium.
While PCWP often closely estimates LVEDP, these values
may not accurately reflect true LV preload, which is a func-
tion of LV end-diastolic volume and stretch of myocardium.
Patients with LV hypertrophy, diastolic heart failure, and LV
ischemia have distorted relationships between LVEDP and
ventricular preload. Consequently, a single PCWP measure-
ment may be less helpful than therapeutic trials of volume
loading or diuretics with serial measurements.
B. Mixed Venous Oxygen Saturation—Mixed venous oxy-
gen saturation (S
–
v
O
2
) is obtained from blood from the pul-
monary artery drawn out of the distal port of the catheter.
Pulmonary artery blood should be withdrawn slowly to
avoid inadvertently pulling “pulmonary capillarized” blood
with a misleadingly higher O
2
saturation.
Mixed venous oxygen saturation is an indicator of sys-
temic oxygen utilization. Normally, peripheral oxygen con-
sumption (
.
V
O
2
) is independent of oxygen delivery (D
O
2
).
Therefore, as cardiac output and oxygen delivery decline,
peripheral oxygen extraction increases to keep consumption
constant. This results in decreased mixed venous oxygen sat-
uration. Conversely, sepsis may cause a reduction in periph-
eral oxygen consumption, thereby increasing mixed venous
oxygen saturation.
The partial pressure of oxygen in mixed venous blood is
normally about 40 mm Hg, resulting in a hemoglobin satu-
ration of 75%. Oxygen content can be calculated for both
arterial and venous hemoglobin saturations (%Sat Hb) using
the following formula:
C
XO
2
= 1.34 × Hb × %Sat + (0.0031 × P
XO
2
)
If hemoglobin concentration is in grams per deciliter,
oxygen content is expressed in milliliters per deciliter.
Dissolved oxygen (0.0031
× P
O
2
) contributes minimally to
oxygen content but may become significant in patients who
are profoundly anemic. The normal arteriovenous oxygen
content difference—C(a–v)
O
2
—is 5 mL/dL. Hypovolemia and
cardiogenic shock both increase the difference (>7 mL/dL),
whereas sepsis decreases it (<3 mL/dL). Left-to-right intrac-
ardiac shunts produce a significant step-up in hemoglobin
saturation in the right ventricle and therefore decrease the
C(a–v)
O
2
gradient.
Mixed venous saturation can be obtained continuously
from pulmonary artery catheters with integral fiberoptic
oximetry capabilities. Dual oximetry combines mixed
venous and arterial pulse oximetry (Spa
O
2
) to provide con-
tinuous estimates of oxygen extraction and intrapulmonary
shunting. From continuous oximetry data, the ventilation-
perfusion index (
.
V/
.
QI) can be calculated by the following
equation:
where P
AO
2
is alveolar oxygen tension, calculated from the
alveolar gas equation.
.
V/
.
QI correlates well with shunt (
.
Qs/
.
Qt)
over a wide range of parameters and clinical conditions.
C. Complications—Complications of pulmonary arterial
catheterization may occur both on insertion and subse-
quently. The incidence of a pneumothorax with either the
subclavian or internal jugular approach is 2–3%. Catheter
knotting is related to the size of the catheter and the insertion
length. Smaller catheters knot more frequently, as do those
with excessive redundancy in the ventricle. The incidence of
catheter-induced transient right bundle branch block is
V
QI
Hb Sp P
H
aO AO
=
+×− + ×
×
1 32 1 0 0031
132
22
.()(. )
.
bbS PvO AO×− + ×()(. )1 0 0031
22
INTENSIVE CARE MONITORING
199
between 0.1% and 0.6% and is thought to be caused by direct
trauma to the bundle of His. The incidence increases to as
high as 23% in patients with preexisting left bundle branch
block. Ventricular arrhythmias also may occur, although they
are usually transient and do not require treatment. Other
complications that may occur during insertion include tra-
cheal laceration, innominate artery injury, and bleeding.
Pulmonary artery rupture may occur at the time of place-
ment, as a result of laceration by the catheter tip, or subse-
quently, from overinflation of the balloon in the distal
pulmonary artery. The overall incidence of rupture is sub-
stantially less than 1%. Contributory factors include distal
position of the catheter, decreased vessel diameter (primary
pulmonary hypertension), systemic anticoagulation, and
prolonged balloon inflation. Hemoptysis is usually the pre-
senting sign. The need for complete removal of the catheter
is debatable because the requirements for monitoring are
compounded by the complication. The catheter should be
withdrawn to a more proximal site and the patient posi-
tioned with the affected side down to optimize ventilation-
perfusion relationships. Emergency thoracotomy is required
in rare cases when uncontrolled bleeding occurs.
Air embolism occurs most commonly with tubing
changes and transducer calibrations. Approximately 20 mL/s
of air is required in adults before symptoms appear, with
75 mL/s required to produce hemodynamic collapse and
death. The precipitating cause is mechanical obstruction of
right ventricular outflow by the air embolus. Patients should
be placed in the left decubitus and steep Trendelenburg posi-
tion. This puts the outflow tract in a dependent location and
allows the air to rise in the ventricle. Aspiration of air through
the pulmonary artery catheter has been reported with varying
results. Obstruction of the pulmonary vasculature by the
embolus results in hypoxemia, increased pulmonary artery
pressure, and right ventricular dysfunction. Passage of air
through a patent foramen ovale may cause cerebral emboliza-
tion and stroke.
Thromboemboli may originate from the tip or body of
the catheter and can result in pulmonary emboli. Catheters
left in place for long periods may cause subclavian or jugular
venous thrombosis. Other complications include infective
endocarditis, sepsis, aseptic thrombotic endocarditis, and
rupture of the chordae tendineae.
The avoidance of sepsis from pulmonary arterial
catheters is identical to the protocols for central venous
catheters. Daily sterile catheter care, dressing changes, and
regular rotation of insertion sites are critical to minimize
catheter-related infections.
Binanay C et al: Evaluation study of congestive heart failure and
pulmonary artery catheterization effectiveness: The ESCAPE
trial. JAMA 2005;294:1625–33. [PMID: 16204666]
Harvey S et al: Assessment of the clinical effectiveness of pul-
monary artery catheters in management of patients in intensive
care (PAC-Man): A randomised, controlled trial. Lancet
2005;366:472–7. [PMID: 16084255]
National Heart, Lung, and Blood Institute Acute Respiratory
Distress Syndrome (ARDS) Clinical Trials Network:
Pulmonary-artery versus central venous catheter to guide treat-
ment of acute lung injury. N Engl J Med 2006;354:2213–24.
[PMID: 16714768]
Pinsky MR, Vincent JL: Let us use the pulmonary artery catheter
correctly and only when we need it. Crit Care Med
2005;33:1119–22. [PMID: 15891346]
Sakr Y et al: Use of the pulmonary artery catheter is not associated
with worse outcome in the ICU. Chest 2005;128:2722–31.
[PMID: 16236948]
Shah MR et al: Impact of the pulmonary artery catheter in criti-
cally ill patients: Meta-analysis of randomized clinical trials.
JAMA 2005;294:1664–70. [PMID: 16204666]
Summerhill EM, Baram M: Principles of pulmonary artery
catheterization in the critically ill. Lung 2005;183:209–19.
[PMID: 16078042]
Cardiac Output
The bedside technique of measuring cardiac output by ther-
modilution added a new dimension to ICU monitoring.
When a known quantity of hot (or cold) solution (indicator)
is injected into the circulation, a time-temperature curve
may be produced that allows calculation of flow. The area
under the time-temperature curve is inversely proportional
to cardiac output. This is calculated using the Stewart-
Hamilton indicator dilution equation:
where V
I
is the volume of injectate (mL) and T
B
,T
I
,S
I
,S
B
,C
B
,
and C
I
are temperature, specific gravity, and specific heat of
blood (B) and indicator (I), respectively.
Either iced or room-temperature thermal boluses can be
used, although the use of iced fluid slightly improves the
signal-to-noise ratio. Room-temperature boluses generally
are adequate except when cardiac output is very low. For best
results, the difference between the blood’s temperature and
that of the injectate should be at least 12°C, which is easily
achieved with room-temperature injectate. Bolus injection
speed and warming of the indicator as it passes through the
catheter have only minimal effects (±3%). When technique is
optimal, measurement repeatability is within 10%. Severe
cardiac arrhythmias may reduce repeatability and yield
results that may not accurately reflect average cardiac output.
Timing of injection with a particular phase of respiration
(end expiration) improves consistency of measurements.
Excessive patient movement also may produce erratic results.
SC
SC
for D W
II
BB
5
×
×
= 108.
Cardiac output
V(T T)SC
SC
IBI II
BB
=
× − ×××
×
60
CHAPTER 8
200
Continuous thermodilution cardiac output measure-
ments can be obtained using special pulmonary artery
catheters. In one type, the right ventricular segment of the
catheter warms the blood by a small amount above body
temperature. A sensitive downstream thermistor records the
change in temperature. In another type, blood flow is esti-
mated by how much electric current is needed to maintain a
segment of the catheter at a temperature slightly above body
temperature. Blood flow is directly related, but in a complex
manner, to the amount of energy needed for a constant tem-
perature. These methods correlate well with conventional
bolus thermodilution but may differ in systematic or nonsys-
tematic fashion.
Other Methods to Measure Cardiac Output
A. Indicator Dilution Cardiac Output—This technique
relies on dilution of a colored dye. A bolus of dye is injected
intravenously through a central venous catheter while
peripheral arterial blood is withdrawn. The arterial sample is
continuously passed through a densitometer. The area under
the dye curve is calculated, and a modification of the
Stewart-Hamilton equation is applied. This techniques is
rarely used in the ICU.
B. Doppler Ultrasound—Doppler devices measure ascend-
ing aortic flow and calculate cardiac output. A continuous-
wave Doppler probe is placed in the sternal notch to measure
the velocity of aortic blood flow. A separate A-mode pulsed
Doppler probe is centered in the third or fourth anterior
intercostal space to measure the cross-sectional diameter of
the aortic root. The stroke volume is the product of the
cross-sectional area and the average blood velocity. Cardiac
output is calculated by multiplying the heart rate and the
stroke volume. Potential sources of error include (1) mis-
alignment of the Doppler beam, which produces errors in
measurement of blood velocity, (2) the assumption that the
aorta is circular, and (3) the assumption that aortic blood
flow is laminar. Each of these factors accounts for a cardiac
output error that approaches 15% when compared with
determinations obtained by other means. The difference
between suprasternal Doppler ultrasound cardiac output
and standard thermodilution has been reported to range
from –4.9 to +5.8 L/min. An esophageal probe is now avail-
able that measures descending aortic flow. An insertion
depth of about 30 cm is required to reach the esophageal
“window.” The aortic root is sized using an A-mode pulsed
Doppler, and a single measurement of ascending aortic flow
is performed with a continuous-mode suprasternal probe.
The esophageal probe is then calibrated against the cardiac
output obtained by the suprasternal technique. This method
yields results as good as those obtained with the suprasternal
technique and offers the added advantage of providing data
continuously. A recently developed transtracheal probe uses
a pulsed Doppler probe attached to the distal end of an endo-
tracheal tube. Controlled studies have shown good accuracy,
but extensive clinical experience is wanting.
C. Thoracic Bioimpedance—This noninvasive technique
measures stroke volume by passing a small alternating cur-
rent (2.5–4.0 mA) through the chest at radiofrequency
70–100 kHz. Four pairs of electrodes (one transmitter and
one sensor) are required. Two pairs are placed at the base of
the neck and two at the level of the xiphoid process in the
midcoronal plane. The change in thoracic impedance is due
to blood flow, ventilation, and body movement. Respiratory
variations occur much more slowly than those associated
with blood flow and can be eliminated by the computer algo-
rithm. Similarly, motion artifacts can be rejected by special
circuitry. The majority of systolic blood flow is due to pul-
satile blood flow in the descending thoracic aorta. Stroke vol-
ume is obtained by analyzing the impedance change over a
cardiac cycle. Heart rate is determined at the same time and
multiplied by stroke volume to yield cardiac output. Other
parameters obtained include ejection velocity index, thoracic
fluid index, and ventricular ejection time. The thoracic fluid
index is thought to correlate with extravascular lung water,
whereas ejection time has been used as a parameter of car-
diac function.
Because bioimpedance cardiac output measurements are
noninvasive, they can be repeated frequently. The volume of
electrically participating tissue (VEPT) is critical in determi-
nation of the stroke volume. Although changes in body habi-
tus are included in the nomogram used to calculate VEPT,
small changes can produce significant error. Similarly, elec-
trode placement is important. A 2-cm change in the distance
between the sensing electrodes will produce a 20% variation
in recorded cardiac output. Overall correlation with ther-
modilution in adults has been only fair. The method is fur-
ther limited by inaccuracies caused by dysrhythmias.
Furthermore, readings are difficult during patient move-
ment, including shivering. Cardiac output is overestimated
when preload is reduced; in low-flow states, when inotropes
are required; and with aortic insufficiency. Underestimation
is produced by hyperdynamic sepsis, hypertension, and
intracardiac shunts.
D. Fick Method—Cardiac output may be calculated by relat-
ing oxygen consumption to arterial and mixed venous oxy-
gen saturation using Fick’s equation:
Calculation of cardiac output using Fick’s equation is the
reference with which all other techniques are compared. The
Cardiac output
V
Ca vO
O
=
−×
2
2
10()
Cardiac output
indicator dose(mg)
average
=
×60
cconcentration time×
INTENSIVE CARE MONITORING
201
arteriovenous oxygen content difference requires that a pul-
monary artery catheter be placed to obtain mixed venous
blood. Oxygen consumption is calculated by measuring the
oxygen content difference between inspired and exhaled gas.
A modification of this technique substitutes mixed venous
CO
2
(rebreathing), arterial P
CO
2
, and expired volume of CO
2
for the corresponding oxygen values in the Fick equation.
E. Pulse Waveform Analysis—A noninvasive method that
shows some promise despite varying reported accuracy uses
algorithmic analysis of the arterial pulse waveform. The
waveform bears a certain relationship with stroke volume
but is modified a great deal by the capacitance, impedance,
and other characteristics of upstream and downstream arte-
rial beds. The aortic impedance plays a major role in this
relationship and is likely to differ between patients. Thus
“calibration” of a noninvasive system (or one using an arte-
rial catheter) using the arterial waveform with thermodilu-
tion cardiac output has been necessary. Recently, several
commercially available systems have been reported to have
adequate agreement with conventional measurements.
Sources of Error
Use of correct temperatures and volumes is the most impor-
tant factor contributing to accurate thermodilution cardiac
output results. If the amount of indicator injected is less than
the amount used in calculation, the fall in indicator temper-
ature will be less than anticipated, and the cardiac output
will be falsely elevated. Cardiac output also will be falsely
elevated if the injectate is warmer than that used in the cal-
culation. The latter problem has been largely overcome with
the introduction of new cardiac output computers that
measure the injectate’s temperature and automatically enter
the value into the calculation.
Right-to-left intracardiac shunt will result in loss of the
indicator, causing a falsely elevated cardiac output. Left-to-
right shunts permit recirculation of indicator that has
already passed through the lungs. This produces multiple
peaks in the time-temperature curve that cannot be inter-
preted by the cardiac output computer, resulting in a bad
curve alert. When tricuspid regurgitation occurs, blood and
indicator mix, resulting in prolongation of transit time. The
curve produced has a slow upstroke and decay, thereby
increasing the area underneath it. This causes sporadic read-
ings and underestimation of the true cardiac output.
Derived Parameters
Cardiac output measurements may be combined with sys-
temic arterial, venous, and pulmonary artery pressure deter-
minations to calculate a number of hemodynamic variables
useful in assessing the overall hemodynamic status of the
patient (Table 8–1). Oxygen transport parameters also may
be calculated (see below).
Cholley BP, Payen D: Noninvasive techniques for measurements of
cardiac output. Curr Opin Crit Care 2005;11:424–9. [PMID:
16175028]
Pulse Oximetry
Pulse oximetry affords a noninvasive estimate of arterial oxy-
gen saturation using the change in light absorption across a
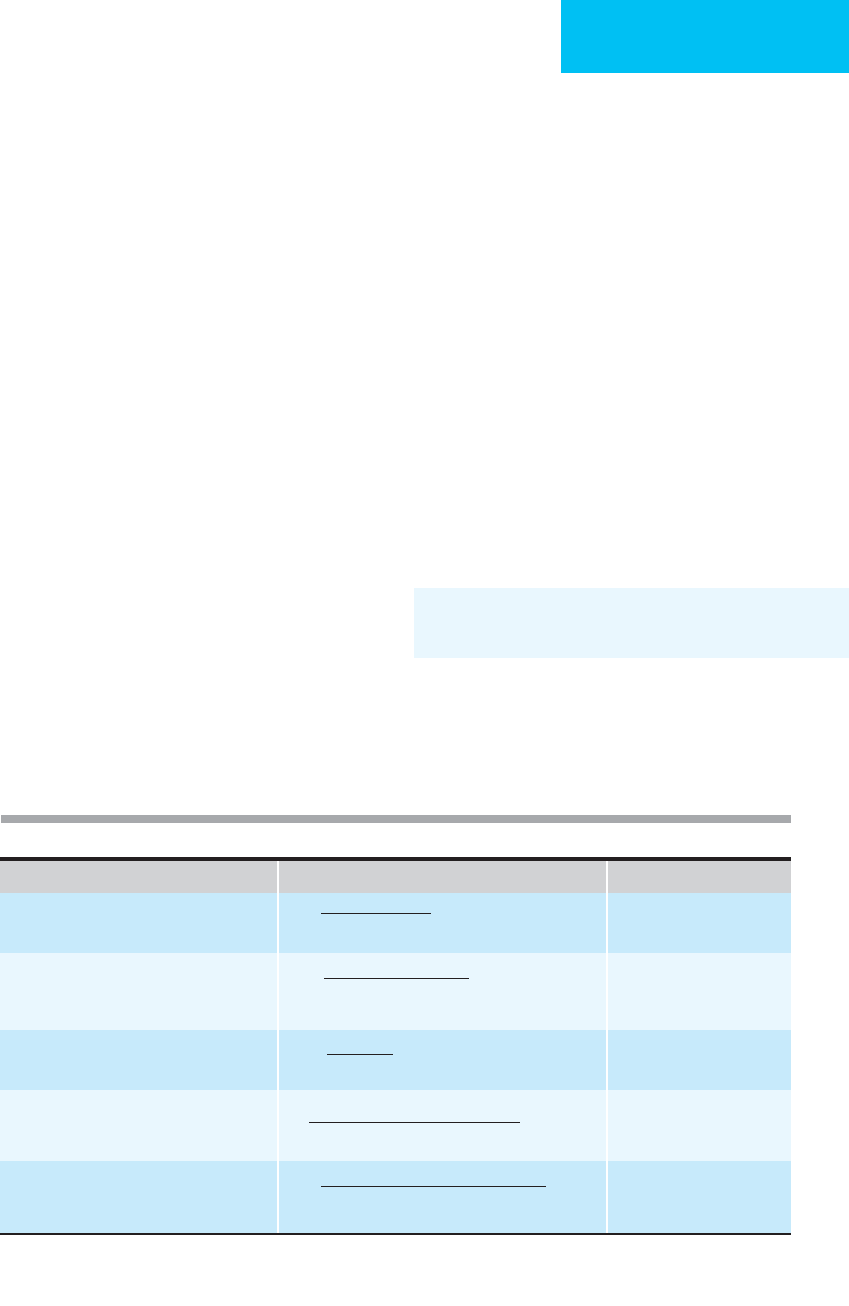
Table 8–1. Hemodynamic calculations and normal ranges.
Formula Normal Range
Stroke volume, mL 60–90 ml
Stroke volume index, mL/m
2
30–65 ml
Cardiac index, L/min/m
2
2.8–4.2 L/min/m
2
Systemic vascular resistance, dyne-s/cm
5
1200–1500 dyn-s/cm
5
Pulmonary vascular resistance, dyne-s/cm
5
100–300 dyn-s/cm
5
CO = cardiac output; BSA = body surface area; BP = systemic blood pressure; CVP = central venous pressure; PAP = pul-
monary artery pressure; PAWP = pulmonary artery wedge pressure.
1000 × CO (L/min)
HR (beats/min)
Stroke volume (mL/beat)
BSA (m
2
)
CO (L/min)
BSA (m
2
)
[Mean BP (mm Hg) – CVP (mm Hg)]
× 80
CO (L/min)
[Mean PAP (mm Hg) – PAWP (mm Hg)]
× 80
CO (L/min)

CHAPTER 8
202
vascular bed during the arterial pulse. In the ICU, pulse
oximetry has important uses and has become a standard of
care in many institutions. There are, however, a number of
issues that should be understood and considered with this
monitoring technique. In particular, the reliability of this
method may be limited in patients with severe hypoxemia,
abnormal arterial pulsations, and hypoperfusion of the site
of measurement.
When light of a particular wavelength is transmitted
through a clear solvent containing solute that absorbs light at
that wavelength, the amount of light absorbed is the product
of solute concentration, path length, and the extinction coef-
ficient (determined by the solute and the wavelength). For a
hemoglobin solution, the relative concentrations of oxy- and
deoxyhemoglobin can be determined in a spectrophotome-
ter because the extinction coefficients are different for these
two hemoglobin species at certain wavelengths.
Pulse oximetry uses the beat-to-beat changes in light
absorption through a vascular bed to estimate arterial O
2
sat-
uration, discarding any nonvariable light absorption by con-
sidering only the difference between peak and nadir light
intensities. The method determines O
2
saturation by a com-
plex calculation that includes several important assump-
tions. With the use of two light-emitting diodes (LEDs)
producing light in the red and infrared ranges, pulse oxime-
try is able to estimate oxyhemoglobin as a proportion of the
sum of oxyhemoglobin plus deoxyhemoglobin—the so-
called functional oxyhemoglobin saturation. Pulse oximeters
are “calibrated” by comparison of arterial blood oxygen sat-
uration in volunteers to calculated values; the devices use a
“look-up table” to translate the measured proportion to the
displayed saturation. Pulse oximetry is subject to artifact-
caused errors. Movement of the oximeter probe, extraneous
incident light (especially if pulsatile), variations in arterial
pulsation, dependent position, venous pulsations, and other
factors may result in incorrect O
2
saturation readings. Pulse
oximeters are most commonly transmission pulse oximeters,
in which light is passed through tissue (ear or fingertip) to a
sensor on the opposite side, but they may be reflectance pulse
oximeters, in which light passes through tissue but is
reflected back to a sensor on the same side as the light source.
Validity
The accuracy of pulse oximetry is generally considered good
in the range of normoxia to mild hypoxemia. However, accu-
racy may be suspect during more severe hypoxemia, such as
when arterial O
2
saturation is below 75%. In this range, dif-
ferences between measured O
2
saturation and pulse oximetry
saturation range from 5–12%.
A. Patient Factors—Patients in the ICU frequently have
hypotension, poor distal extremity perfusion, and impaired
oxygen delivery—or are being given pharmacologic vasopres-
sors or vasodilators. These factors affect blood flow to the site
of pulse oximetry and vary the contour and intensity of the
beat-to-beat pulse used to calculate O
2
saturation. Most
devices are programmed to avoid reporting O
2
saturation
when low perfusion or a poor pulse signal is being measured.
In some of the few studies considering these issues in the ICU,
failure of the pulse oximeter to measure O
2
saturation was not
infrequent in patients with hemodynamic instability
(12–15%). However, other studies have demonstrated that
some pulse oximeters continue to measure and report O
2
sat-
uration despite very poor blood flow and severe hypotension.
These results may not be reliable, and there is concern that
pulse oximeter O
2
saturation under these conditions may be
misleadingly high. Pulse oximeter technology continues to
evolve. The latest-generation devices have improved resist-
ance to motion artifact and low perfusion. These are expected
to be more reliable and accurate in the ICU setting.
B. Abnormal Hemoglobins—The pulse oximeter cannot
measure carboxyhemoglobin nor accurately measure oxyhe-
moglobin in the presence of carboxyhemoglobin. The oxy-
gen saturation displayed is essentially equal to the difference
between total hemoglobin and deoxygenated hemoglobin
(100% – the percentage of deoxyhemoglobin), but the relative
concentrations of oxy- and carboxyhemoglobin are
unknown. Other substances in the blood may or may not
affect pulse oximetry. Bilirubin has little effect on pulse
oximetry; methemoglobin, generated in the presence of oxi-
dizing agents such as nitrites and sulfonamides, usually
increases the difference between functional O
2
saturation and
oxyhemoglobin, but a sufficiently high methemoglobin con-
centration also may have the peculiar effect of causing the
pulse oximeter to read 85% regardless of other conditions. A
number of dyes such as indocyanine green and methylene
blue also have effects on the accuracy of measurement.
Clinical Applications
Pulse oximetry has widespread usefulness in the ICU, espe-
cially in adjusting inspired oxygen, during weaning from
mechanical ventilation, and in testing different levels of
PEEP, inverse I:E ratio, or other mechanical ventilator adjust-
ments. Other uses include monitoring during procedures
such as bronchoscopy, gastrointestinal endoscopy, cardiover-
sion, hemodialysis, and radiography. Pulse oximetry is par-
ticularly accurate in following O
2
saturation in patients who
have mild to moderate hypoxemia (O
2
saturation >75%) but
without severe hypoperfusion or hypotension. It cannot be
regarded as a complete substitute for arterial blood gas deter-
minations partly because of the lack of P
O
2
and pH determi-
nations but also because of the relationship between P
O
2
and
O
2
saturation when the latter is above 90–95%. Results of
pulse oximetry should be interpreted cautiously in patients
with carboxyhemoglobinemia or methemoglobinemia.
Keogh BF, Kopotic RJ: Recent findings in the use of reflectance
oximetry: A critical review. Curr Opin Anaesthesiol
2005;18:649–54. [PMID: 16534307]
McMorrow RC, Mythen MG: Pulse oximetry. Curr Opin Crit Care
2006;12:269–71. [PMID: 16672788]

INTENSIVE CARE MONITORING
203
Airway CO
2
Monitoring
A disposable colorimetric device that detects CO
2
can con-
firm endotracheal tube placement and position. When the
device tests positively for CO
2
, this confirms that the endo-
tracheal tube is in the trachea. However, a negative result is
not as reliable, and alternative means for checking tube
placement must be used.
Continuous airway CO
2
monitoring uses a rapidly
responding infrared CO
2
analyzer. Capnography is a continu-
ous display or recording of CO
2
concentration during each
breath. Other devices may display the end-tidal CO
2
fraction
or partial pressure (P
ETCO
2
).
The infrared analyzer uses an appropriate wavelength of
infrared light for which the CO
2
concentration is propor-
tionate to the absorption of the light. It has the advantage of
relatively low cost, real-time sampling, reliability, ease of cal-
ibration, and acceptable response time.
Capnography shows a continuous display of expired and, if
desired, inspired CO
2
concentration or partial pressure. The
expired CO
2
waveform can give a qualitative assessment of the
degree of ventilation-perfusion mismatching. For example,
the steepness of the slope of the “alveolar plateau” indicates
more severe
.
V/
.
Q mismatching because it demonstrates empty-
ing of progressively less well ventilated lung units compared
with a waveform showing a flatter alveolar plateau in a patient
with less severe
.
V/
.
Q mismatching. The inspiratory segment
also should be inspected to confirm that the inspired gas is free
of CO
2
as a result of malfunction of the ventilator’s expiratory
valve or some other component.
End-Tidal and Mixed Expired P
CO
2
In normal subjects at rest and breathing at a normal tidal vol-
ume and respiratory rate, P
ETCO
2
is close numerically to arte-
rial P
CO
2
, with the usual difference between Pa
CO
2
and
P
ETCO
2
0–4 mm Hg (P[a–
ET
]
CO
2
). In patients with respira-
tory failure, contribution to expired gas from dead space and
high
.
V/
.
Q lung units decreases CO
2
concentration during
expiration and at end expiration. The P(a–
ET
)
CO
2
becomes
increasingly large, with a strong correlation between
P(a–
ET
)
CO
2
and the dead space–tidal volume ratio. The
P
ETCO
2
should not be used as a substitute for Pa
CO
2
in
patients with lung disease. Furthermore, P(a–
ET
)
CO
2
cannot
be assumed to remain constant in the face of lung disease
and mechanical ventilation.
The mixed expired CO
2
fraction or partial pressure (P
–
ECO
2
)
is usually determined from collection of expired gas for several
minutes. This should be distinguished from P
ETCO
2
sampled at
the end of a single breath. The mixed expired CO
2
fraction can
be used with Pa
CO
2
to calculate the dead space–tidal volume
ratio (V
D
/V
T
) using the modified Bohr equation:
In addition, if minute ventilation is measured,
where P
B
is barometric pressure.
Volumetric Capnography
Capnography records CO
2
concentration against time dur-
ing expiration. If CO
2
is plotted against expired volume, then
a semiquantative estimate of dead space:tidal volume ratio is
obtained. Equipment for doing volumetric capnography can
be built into mechanical ventilators. Volumetric capnogra-
phy has been used to help diagnose pulmonary embolism
and theoretically should be applicable to other situations
where dead space:tidal volume ratio is useful (eg, weaning,
ARDS, and asthma).
Validity
As described earlier, end-tidal P
CO
2
should not be used as an
accurate estimate of Pa
CO
2
. Patients with either worsening of
gas exchange function (increased Pa
CO
2
) or improvement in
function (decreased Pa
CO
2
) can have a fall in P
ETCO
2
.The
former occurs because of an increase in P(a–
ET
)
CO
2
; the lat-
ter represents a parallel fall in both P
ETCO
2
and Pa
CO
2
.
However, among the relatively few reports involving ICU
patients—most of whom were receiving mechanical ventila-
tion—some indicate that Pa
CO
2
and P
ETCO
2
track together rel-
atively well, with mean differences less than 5 mm Hg and no
change in difference during weaning or extubation. In COPD
patients, the difference was considerably higher (as much as 9
mm Hg) but, again, relatively constant. In contrast, other stud-
ies have found that P(a–
ET
)
CO
2
varies considerably, and while
there was correlation with V
D
/V
T
, there was a lack of a con-
stant value for P(a–
ET
)
CO
2
that would allow “tracking” of
Pa
CO
2
from P
ETCO
2
alone. In particular, one study demon-
strated that both increases and decreases in P(a–
ET
)
CO
2
may
result from mechanical ventilator adjustments.
Clinical Applications
Airway CO
2
monitoring has the advantage of being nonin-
vasive, and studies are available that indicate a decrease in
the number of arterial blood gases obtained when this
modality is used. However, it is clear that the critically ill
patient with respiratory failure will have the largest and
most unpredictable difference between Pa
CO
2
and P
ETCO
2
;
in these patients, P
ETCO
2
is an unreliable estimate of Pa
CO
2
.
On the other hand, the difference between Pa
CO
2
and
P
ETCO
2
can be used as a measure of dead space:tidal volume
ratio and therefore as a measure of the severity of gas
exchange derangement.
Although studies are lacking on the benefit of routine mon-
itoring of airway CO
2
, capnography and P
ETCO
2
monitoring
V L /min STPD V L/min,BTPS
P
CO E
2
0 826(,). ( )=× ×
EECO
B
2
P
V
V
Pa P
Pa
D
T
CO ECO
CO
=
−
22
2
CHAPTER 8
204
have been used in several clinical situations. First, airway CO
2
monitoring can provide rapid noninvasive assurance of correct
endotracheal tube placement. The capnogram should show
increasing CO
2
concentration during expiration, and P
ETCO
2
should be a plausible value. Second, P
ETCO
2
has been used dur-
ing cardiopulmonary resuscitation as a measure of the effec-
tiveness of artificial circulatory assistance; a very low P
ETCO
2
suggests that venous blood is not adequately returning to the
central circulation. Third, the combination of arterial and end-
tidal P
CO
2
provides an estimate of the inefficiency of ventila-
tion (V
D
/V
T
). Some researchers have suggested that
P(a–
ET
)
CO
2
can be used to titrate the optimal amount of PEEP.
While the smallest difference in P(a–
ET
)
CO
2
has correlated with
the highest degree of tissue oxygen delivery, this measurement
has not proved ideal in all studies. Finally, it has been suggested
that capnography can help in weaning patients from mechani-
cal ventilation, but the predictive value of airway CO
2
monitor-
ing in this clinical situation is unclear.
Belpomme V et al: Correlation of arterial P
CO
2
and P
ETCO
2
in pre-
hospital controlled ventilation. Am J Emerg Med 2005;
23:852–9. [PMID: 16291440]
Kallet RH et al: Accuracy of physiologic dead space measure-
ments in patients with acute respiratory distress syndrome
using volumetric capnography: Comparison with the meta-
bolic monitor method. Respir Care 2005;50:462–7. [PMID:
15807908]
Moon SW et al: Arterial minus end-tidal CO
2
as a prognostic fac-
tor of hospital survival in patients resuscitated from cardiac
arrest. Resuscitation 2007;72:219–25. [PMID: 17101205]
Verschuren F et al: Volumetric capnography as a screening test for
pulmonary embolism in the emergency department. Chest
2004;125:841–50. [PMID: 16117730]
Transcutaneous Blood Gases
Using transcutaneous blood gas monitors, partial pressures
of oxygen and carbon dioxide may be measured in the tissue
beneath heated skin electrodes. This monitoring technique
has value because it reflects tissue levels, but it cannot yet be
employed as a substitute for blood gas monitoring.
Principle
The Clark electrode, similar to that used in blood gas analyz-
ers, has been modified to be used on the skin surface. The
skin in the area of the electrode is heated to 43–45°C. This
heating is necessary to make the skin permeable to oxygen,
but it has the additional effect of increasing perfusion in the
tissues beneath the probe. Since transcutaneous P
O
2
(Ptc
O
2
)
reflects the oxygen tension level of the tissue beneath the
probe, values may be affected either by arterial oxygenation
or by systemic and regional perfusion. At relatively normal
cardiac output and with normal regional blood flow, Ptc
O
2
values reflect arterial P
O
2
values. In adults, the ratio of
transcutaneous-to-arterial P
O
2
is normally about 0.8,
whereas in children it tends to be higher. (Values in neonates
may be very close to equal.) However, when either cardiac
output or regional perfusion is decreased, the ratio of
transcutaneous-to-arterial P
O
2
is decreased in proportion to
the level of decreased perfusion. Hence transcutaneous oxy-
gen monitoring may be used as a monitor of both oxygena-
tion and perfusion. A low Ptc
O
2
value is an indicator that the
patient is either hypoxemic or in a low-flow state (or has
reduced regional perfusion).
Transcutaneous P
CO
2
(Ptc
CO
2
) has been measured using
a modified P
CO
2
electrode attached to the skin surface. In
contrast to Ptc
O
2
,however,CO
2
is more soluble than O
2
,so
tissue stores of CO
2
act as a buffer, reducing the dependence
of Ptc
CO
2
on blood flow and metabolism. In theory, Ptc
CO
2
should mirror Pa
CO
2
more closely than Ptc
O
2
reflects Pa
O
2
,
and there is no need to heat the skin at the monitoring site.
Newly designed sensors with heaters have been studied
recently. Results have been variable.
Both Ptc
O
2
and Ptc
CO
2
devices should be calibrated
against known P
O
2
and P
CO
2
. Because of the heating of the
Ptc
O
2
electrode site, the location must be changed every 4–6
hours to minimize the risk of thermal injury.
Clinical Applications
Many neonatal ICUs routinely employ Ptc
O
2
monitoring and
have found good correlation with arterial blood gases except in
patients with severe cardiac compromise. In adults, Ptc
O
2
measurement is best used as a measure of tissue hypoperfusion.
A reduction of Ptc
O
2
may be an early indicator of low flow, par-
ticularly if pulse oximetry does not indicate severe hypoxemia.
Kagawa S, Severinghaus JW: Errors in monitoring transcutaneous
P
CO
2
on the ear. Crit Care Med 2005;33:2414–5. [PMID:
16215403]
Kagawa S et al: Initial transcutaneous P
CO
2
overshoot with ear
probe at 42
º
C. J Clin Monit Comput 2004;18:343–5. [PMID:
15957625]
Respiratory Mechanics
Measured parameters are tidal volume, vital capacity, airway
pressure, and intrathoracic pressure. From these, respiratory
system and lung compliance, airway resistance, and work of
breathing can be estimated. Modern mechanical ventilators
often are equipped to measure airway pressure, tidal volume,
inspiratory flow, and other derived values. They may be able
to display in real time flow-volume or pressure-volume
loops. A discussion of respiratory compliance and resistance
is found in Chapter 12.
Tidal Volume
In the ICU, tidal volume is measured most commonly in
patients who have endotracheal tubes and require mechanical
ventilation. Respiratory inductive plethysmography provides

INTENSIVE CARE MONITORING
205
a noninvasive estimate of tidal volume. Tidal volume should
be monitored frequently in patients receiving mechanical
ventilation. When volume-preset modes are used, a difference
in expired volume compared with preset volume indicates
that there is a leak in the ventilator circuit, that inspiratory
flow demand is extremely high, or that inspiratory peak pres-
sure exceeds the preset limit. In pressure-controlled ventila-
tion, tidal volume is used to adjust the level of set airway
pressure, and any change in expired tidal volume indicates a
change in lung or chest wall compliance or airway resistance.
During spontaneous respiration, tidal volume monitoring
using noninvasive measurement can be employed to help
identify patients with obstructive sleep apnea or abnormal
breathing patterns (Cheyne-Stokes respiration).
Maximum Inspiratory and Expiratory Airway
Pressure
Inspiratory and expiratory maximum pressures are deter-
mined by a manometer connected either to a mouthpiece or
to tubing adapted to fit onto the endotracheal tube. These
pressures are measured correctly starting at functional resid-
ual volume so that lung and chest wall elastic recoils are
neutralized, and the pressures reflect only respiratory mus-
cle strength. In practice, this detail is often omitted. Normal
maximum inspiratory pressure is more than –80 to –100 cm
H
2
O; maximum expiratory pressure in normal individuals
exceeds 120–150 cm H
2
O. Maximum negative inspiratory
and positive expiratory pressures are useful in assessment of
respiratory failure in patients with neuromuscular disor-
ders. Studies support the use either of the average of maxi-
mum inspiratory and expiratory pressures or of vital
capacity in roughly predicting the onset of hypercapnia in
these patients when pressures fall by about 70% or when
vital capacity is less than about 55% of predicted. These
direct measures are notably better than extrapolations of
respiratory muscle strength from measurements of the
strength of the extremities.
Intrathoracic (Intraesophageal) Pressure
Intrathoracic pressure requires a pressure sensor within the
chest—almost always a balloon placed in the lower third of the
esophagus and connected to a suitable manometer. The bal-
loon must be filled carefully with a small amount of air so that
the changes in intrathoracic pressure are faithfully recorded
without the confounding effects of the balloon’s compliance.
Care must be taken to position the balloon within the chest
and not in the stomach. Systems for measuring esophageal
pressure are available commercially. Esophageal pressure is
used most often to determine lung or chest wall compliance or
work of breathing, but it also can be helpful in identifying
auto-PEEP. A potential use is to “correct” pulmonary artery or
pulmonary artery wedge pressures for large swings in
intrathoracic pressure during the respiratory cycle.
Lung and Chest Wall Compliance
Calculation of compliance of the respiratory system (chest
wall and lungs together) is reviewed in Chapter 12. The com-
ponents of respiratory system compliance can be subdivided
into chest wall and lung compliances. Lung compliance (C
L
)
is calculated as the ratio of change in volume (ΔV) to change
in pressure (ΔP), where ΔV is usually the tidal volume and
ΔP is the difference between end-inspiratory and end-
expiratory transpulmonary pressure. Transpulmonary pres-
sure is the pressure difference between the pressure in the
airway and the esophageal pressure. Normal lung compliance
is about 200 mL/cm H
2
O at end-expiratory volume. If chest
wall compliance (C
CW
) is desired, the formula 1/C
RS
= 1/C
L
+ 1/C
CW
can be used, where
RS
is the respiratory system).
Decreased lung compliance has been used as a criterion of
ARDS in some clinical studies but is not usually required for
its clinical diagnosis. Low lung or chest wall compliance sug-
gests increased work of breathing and could suggest that
weaning would be difficult or inappropriate. On occasion,
abnormal chest wall compliance as a cause of respiratory fail-
ure is not identified unless measured. If low chest wall com-
pliance is found to contribute to respiratory failure, a very
different approach to treatment may be warranted.
Work of Breathing
The work required for breathing is derived from the for-
mula for mechanical work: W = force × distance. For
breathing in which the force is applied over a predeter-
mined volume, substitute pressure for work, and for dis-
tance, substitute change in volume. Thus work of
breathing is the product of ΔP ×ΔV. Work of breathing can
be calculated for the patient-ventilator system, with the
result indicating the work being done by the mechanical
ventilator for a particular tidal volume. The same work, of
course, would be done by the patient breathing sponta-
neously, but this is usually not relevant because the patient
is unlikely to breathe at the same rate, tidal volume, and I:E
ratio. For spontaneous breathing, tidal volume should be
measured nonintrusively, and the pressure difference
between end expiration and end inspiration is measured
inside the thorax (esophageal pressure). Thus a setup for
measuring mechanical work of breathing generally meas-
ures tidal volume (noninvasive or through the endotra-
cheal tube) and esophageal pressure.
Work of breathing calculated from tidal volume and
esophageal pressure may underestimate actual work being
performed by a significant amount. Some of the difference
arises from nonuniform expansion of the lung or chest wall
or compression of intrathoracic gas, and the calculation does
not consider the expiratory work of breathing. In practice,
work of breathing is rarely measured for clinical purposes.
Theoretically, increased work of breathing should be a good
predictor of the success of weaning from mechanical ventila-
tion and could provide a guide to maximizing respiratory
CHAPTER 8
206
muscle strength, maximizing lung and chest wall compliance,
and minimizing airway resistance. In the area of research in
critically ill patients, work of breathing has been used to
characterize an excessive burden on the respiratory muscles
from high resistance in the ventilator circuit, poorly func-
tioning expiratory and inspiratory valves, development of
auto-PEEP, and other factors.
Bigatello LM, Davignon KR, Stelfox HT: Respiratory mechanics
and ventilator waveforms in the patient with acute lung injury.
Respir Care 2005;50:235–45. [PMID: 15691393]
Durbin CG Jr: Applied respiratory physiology: Use of ventilator
waveforms and mechanics in the management of critically ill
patients. Respir Care 2005;50:287–93. [PMID: 15691397]
Gattinoni L, Eleonora C, Caironi P: Monitoring of pulmonary
mechanics in acute respiratory distress syndrome to titrate ther-
apy. Curr Opin Crit Care 2005;11:252–8. [PMID: 15928475]
Haitsma JJ: Physiology of mechanical ventilation. Crit Care Clin
2007;23:117–34. [PMID: 17368160]
Jonson B: Elastic pressure-volume curves in acute lung injury and
acute respiratory distress syndrome. Intensive Care Med
2005;31:205–12. [PMID: 15605228]
Stahl CA et al: Dynamic versus static respiratory mechanics in
acute lung injury and acute respiratory distress syndrome. Crit
Care Med 2006;34:2090–8. [PMID: 16755254]
Respired Gas Analysis
Measurement of respired gases includes determination of
CO
2
output (
.
V
CO
2
) and O
2
uptake (
.
V
O
2
). In the steady state,
these are considered equivalent to CO
2
production and O
2
consumption. The ratio
.
V
CO
2
/
.
V
O
2
is the respiratory gas
exchange ratio, which is equal to the respiratory quotient
(RQ) in the steady state.
.
V
CO
2
and
.
V
O
2
are measured by comparing inspired and
expired gas concentrations of O
2
and CO
2
and knowing the
inspired or expired minute ventilation. Gas concentrations
are measured using O
2
and CO
2
analyzers. Oxygen analyzers
measure P
O
2
using an electrochemical method to generate
current proportionate to P
O
2
. Infrared CO
2
analyzers are
highly reliable and accurate. Both inspired and expired gas
concentrations are needed.
The product of mixed expired CO
2
fraction (F
–
ECO
2
) and
expired minute ventilation is
.
V
CO
2
(L/min) expressed at stan-
dard temperature and pressure, dry (STPD). For
.
V
O
2
(L/min), the calculation is more complex, having to take into
account the inspired oxygen fraction and the small but sig-
nificant difference between inspired and expired minute ven-
tilation owing to the gas exchange ratio.
Automated instruments allow for continuous measure-
ment of
.
V
CO
2
and
.
V
O
2
and often report these results in tables
or graphs. Indirect calorimetry uses
.
V
O
2
and an estimate of
the substrate mix being used for energy production (RQ) to
estimate the energy expenditure or caloric requirement of
the patient:
.
V
O
2
and
.
V
CO
2
also can be measured using the Fick equa-
tion with knowledge of arterial and mixed venous O
2
and
CO
2
contents (mL/dL or mL/L of blood) and cardiac output
(thermodilution or other technique). For critically ill
patients, this requires a pulmonary artery catheter, and most
commonly it has been an intermittent calculation. However,
with continuous cardiac output technology, continuous
mixed venous oximetry, and arterial pulse oximetry, a con-
tinuously calculated oxygen consumption is now possible.
Validity
Carbon dioxide output (
.
V
CO
2
) determination is generally
satisfactory in the ICU, including patients receiving mechan-
ical ventilation. With high inspired O
2
,CO
2
analyzers require
adjustment according to the manufacturer’s instructions, but
this does not detract from accuracy.
On the other hand,
.
V
O
2
is calculated most often using the
difference between inspired and expired fraction of O
2
and
an adjustment that accounts for the small difference between
inspired and expired minute ventilation. This formula is very
sensitive to inspired O
2
concentration, especially when F
IO
2
>
0.50. In fact, some investigators are suspicious of
.
V
O
2
deter-
minations from expired gas when F
IO
2
exceeds 0.21, and
many commercial systems are not reliable when F
IO
2
is
greater than 0.30–0.40.
Calculation of oxygen consumption by the Fick equation
also has significant inherent inexactness. Intermittent ther-
modilution measurements of cardiac output have signifi-
cant variance, as do measurements of arterial and venous
saturation, as well as hemoglobin. Any errors in these
measurements are increased geometrically during calcula-
tion of oxygen consumption—so-called mathematical cou-
pling. However, the importance of this limitation to the
accuracy of this methodology in clinical practice is a matter
of controversy.
Clinical Applications
Monitoring of oxygen delivery and oxygen consumption
allows titration of ICU interventions to specific physiologic
end points for individual patients. However, it is not clear
that providing “supranormal” oxygen delivery improves out-
come for critically ill patients with shock, sepsis, trauma, or
hemorrhage. One important exception is during the early
phase of sepsis and septic shock, in which attention to oxy-
gen delivery (assessed using central venous oxygen satura-
tion) increases survival.
Oxygen uptake by indirect calorimetry in the ICU also
may be used to determine metabolic requirements so that
appropriate caloric requirements as well as substrate
kcal/day V (L/min) 1440 min/dayO
2
=×
×+×(3.82 1.23 RQ) kcal/L V
OO
2
