Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

IMAGING PROCEDURES
167
pressure, in all but one of the patients barotrauma was noted
when peak airway pressure was greater than 40 cm H
2
O. Other
studies report an incidence of about 50% and suggest that
PEEP does contribute to the development of barotrauma.
Decreased compliance of the lungs in patients with ARDS
necessitates higher ventilatory pressures to maintain adequate
oxygenation, which results in an increased risk of barotrauma.
Pulmonary diseases that increase lung compliance also may
promote barotrauma because there is greater overdistention of
the lung.
Radiographic Features
Radiographic findings of pulmonary interstitial emphy-
sema include visualization of perivascular air along pul-
monary vessels seen on end (producing a perivascular
“halo”), linear radiolucencies radiating toward the hila,
irregular radiolucent mottling, parenchymal cysts (pneu-
matoceles), and linear or rounded collections of air along
the visceral pleural surface (subpleural air cysts).
Pulmonary interstitial emphysema may be difficult to
detect and to distinguish from air bronchograms.
Moreover, pulmonary interstitial emphysema is usually not
apparent radiographically unless present in conjunction
with pulmonary opacification.
Pneumomediastinum may be recognized radiographi-
cally by linear lucencies adjacent to the heart and aortic arch,
descending aorta, and great vessels. Visibility of the wall of a
main bronchus, air outlining the thymus, and air between
the parietal pleura and diaphragm also have been described.
Pneumomediastinum is usually easier to identify than pul-
monary interstitial emphysema and is often the first evidence
of barotrauma. Subsequent dissection of air from the medi-
astinum along fascial planes may result in subcutaneous
emphysema, with linear radiolucencies extending along tis-
sue planes in the chest wall and neck (see Figure 7–17). Less
often, dissection of air along the descending aorta into the
retroperitoneum will occur, with rare rupture into the
abdomen giving rise to pneumoperitoneum. In such
instances, clinical correlation is essential to exclude a perfo-
rated abdominal viscus. Early diagnosis of pulmonary inter-
stitial emphysema may alert clinicians to pneumothorax, a
potentially catastrophic consequence of barotrauma.
Although other manifestations of barotrauma are usually
self-limited, even a small pneumothorax may progress to
tension pneumothorax in critically ill patients, particularly
in patients being maintained with mechanical ventilators. As
previously discussed, pneumothorax in the supine patient
may be difficult to diagnose and must be considered or it will
be missed. Occasionally, tension pneumomediastinum may
occur, although this is usually of greater clinical likelihood in
pediatric patients. Concomitant pulmonary interstitial
emphysema will result in further respiratory embarrassment
secondary to compression of lung parenchyma by interstitial
air and decreases in both ventilation and perfusion.
Pneumopericardium arises infrequently secondary to
barotrauma but may progress to tension, in which there is
increased intrapericardial pressure and impairment in
venous return and cardiac function.
Kemper AC, Steinberg KP, Stern EJ: Pulmonary interstitial emphy-
sema: CT findings. AJR 1999;172:1642. [PMID: 10350307]
Trotman-Dickenson B: Radiology in the intensive care unit (part 2).
J Intensive Care Med 2003;18:239–52. [PMID: 15035758]
Webb WR, Higgins CB: Thoracic Imaging: Pulmonary and
Cardiovascular Radiology. Philadelphia: Lippincott Williams &
Wilkins, 2005.
IMAGING OF THE ABDOMEN & PELVIS
General Principles
Imaging of the gastrointestinal tract generally should begin
with plain radiographs because these are readily obtained
and provide useful information regarding perforation,
bowel obstruction, and ileus. However, because the overall
sensitivity of plain radiographs remains low, further imag-
ing with CT may be necessary to confirm suspected pneu-
moperitoneum or intraabdominal abscess and to inspect
the features of the small and large bowel walls and sur-
rounding fat. Imaging of abdominal and pelvic solid
organs, including the gallbladder and urinary bladder,
should begin with ultrasound because it is nonionizing and
portable to the ICU.
Gastrointestinal Perforation
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Lucency over the liver or abdomen.
Lucency under a hemidiaphragm on upright views.
“Double-wall sign.”
Visualization of the falciform ligament.
“Football sign.”
“Inverted-V sign.”
“Triangle sign.”
General Considerations
In the ICU, bowel perforation usually results from an upper
abdominal source, such as a penetrating gastric or duodenal
ulcer; a lower gastrointestinal tract source, such as diverticulitis
or toxic megacolon; or from complications of upper and
lower endoscopic procedures. Other causes of perforation
include severe intestinal inflammation, bowel obstruction,
bowel infarction, or neoplasm.
CHAPTER 7
168
Radiographic Features
An experienced abdominal radiologist may identify even small
amounts of free air on a supine abdominal radiograph, finding
small bubbles or generalized increased lucency over the abdomen,
right upper quadrant, or subhepatic space. Other signs include
the “double-wall sign” of Rigler, the “triangle sign,” the “football
sign,” or the falciform ligament sign (Figure 7–22). For less expe-
rienced readers, a second view must be added to the supine radi-
ograph to increase sensitivity. Most commonly, this is an upright
abdominal film in which air rises to outline the thin curvilinear
hemidiaphragm. However, to obtain this view properly is nearly
impossible in the ICU. Useful alternatives include the left lateral
decubitus view (where the patient maintained in the left-side-
down position for at least 5–10 minutes), allowing free air to rise
toward the right subphrenic space. A right lateral decubitus view
is usually nondiagnostic because of confusion arising from the
adjacent stomach bubble. In immobile patients, a cross-table lat-
eral view may be obtained, in which the patient remains supine,
but the x-ray beam is tangential to the anterior abdominal wall.
However, small amounts of free air may be missed on this view. If
plain films are equivocal and perforation is suspected, an abdom-
inal CT (Figure 7–23) offers an excellent means of detecting even
tiny amounts of free air and possibly localizing a source.
Differential Diagnosis
Pneumoperitoneum has a variety of causes and is not synony-
mous with bowel perforation, its most serious and surgically
urgent cause. In the ICU, the most common reason for pneu-
moperitoneum is probably the postoperative state.
Pneumoperitonem may persist for up to 14 days after surgery,
the amount of air decreasing progressively and never increasing
over time. Other forms of pneumoperitoneum requiring urgent
attention include peritonitis caused by gas forming microorgan-
isms. Benign causes include dissection of gas from the thoracic
cavity in patients with COPD receiving mechanical ventilation.
Bhalla S, Menias CO, Heiken JP: CT of acute abdominal aortic disor-
ders. Radiol Clin North Am 2003;41:1153–69. [PMID: 14661663]
Gore RM et al: Helical CT in the evaluation of the acute abdomen.
AJR 2000;174;901–13. [PMID: 10749221]
Grassi R et al: Gastro-duodenal perforations: Conventional plain
film, US and CT findings in 166 consecutive patients. Eur J
Radiol 2004;50:30–6. [PMID: 15093233]
Pinto A et al: Comparison between the site of multislice CT signs
of gastrointestinal perforation and the site of perforation
detected at surgery in forty perforated patients. Radiol Med
(Torino) 2004;108:208–17. [PMID: 15343135]
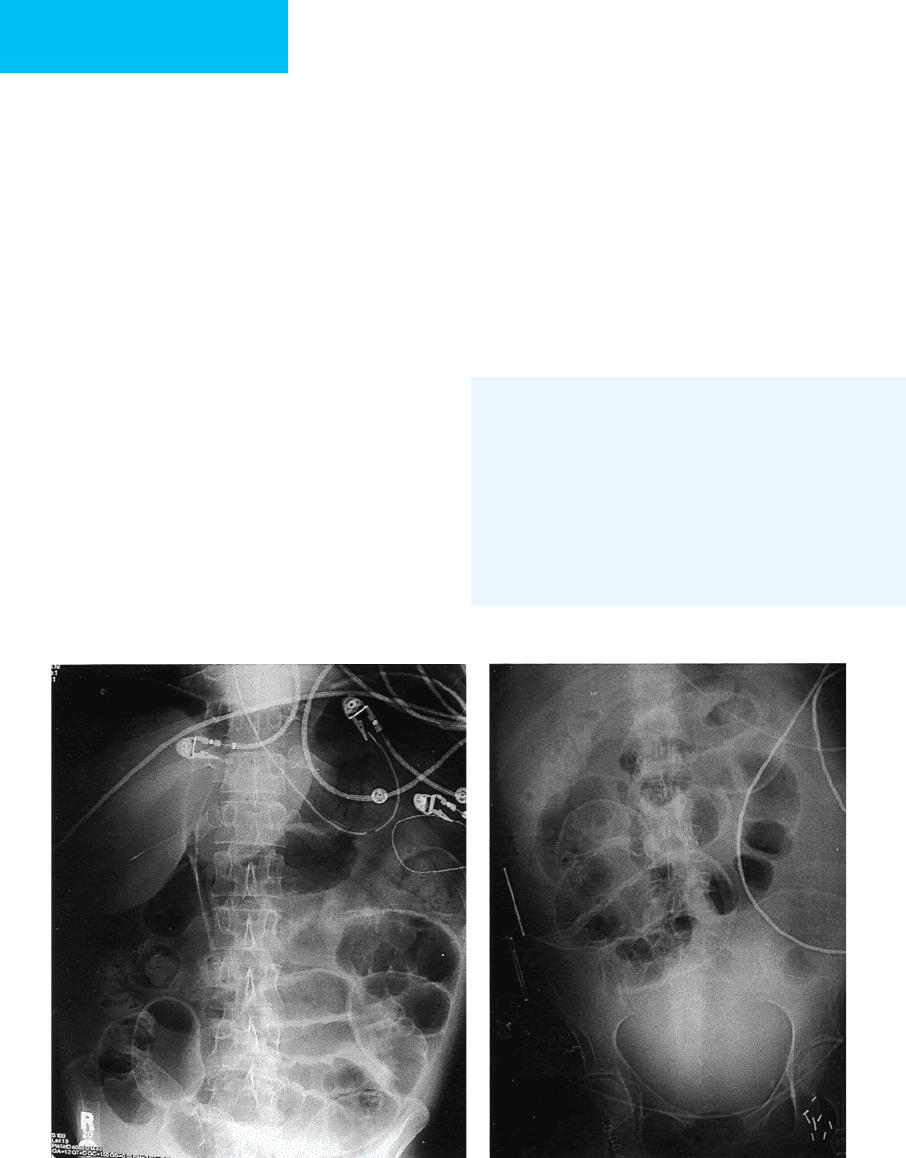
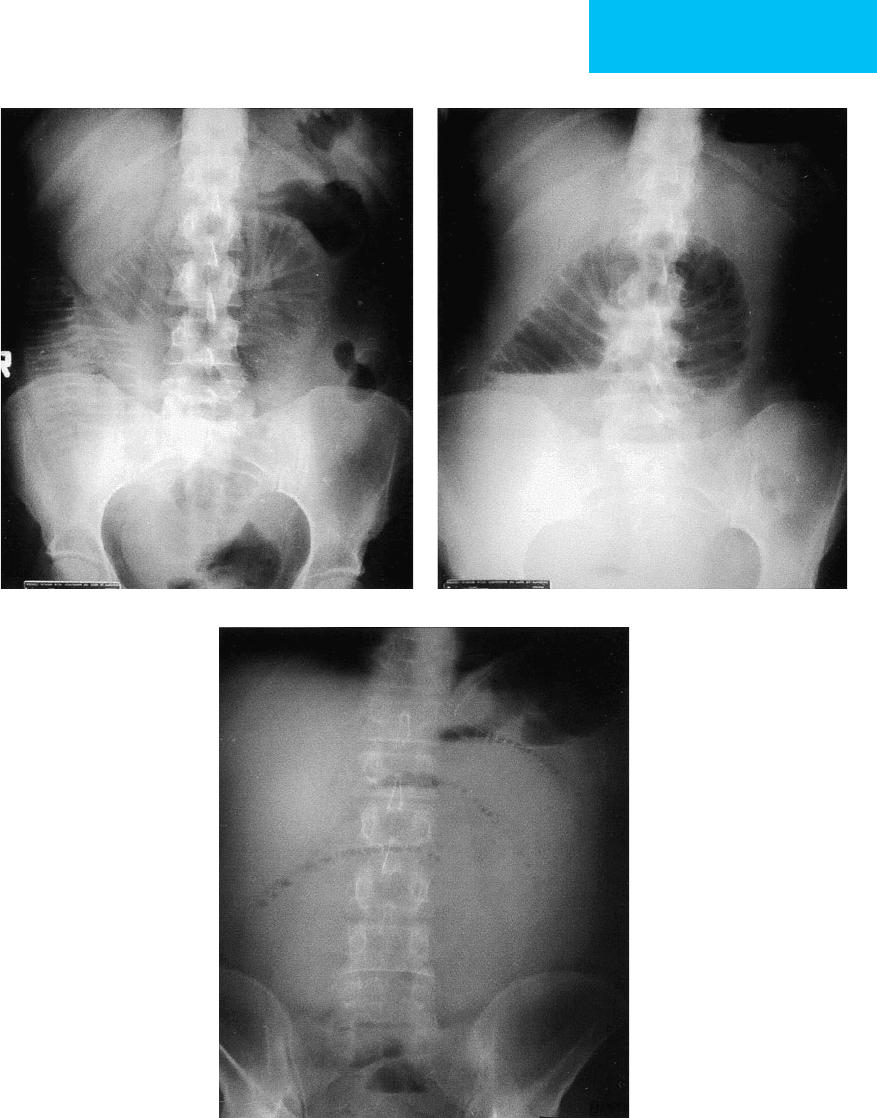
AB
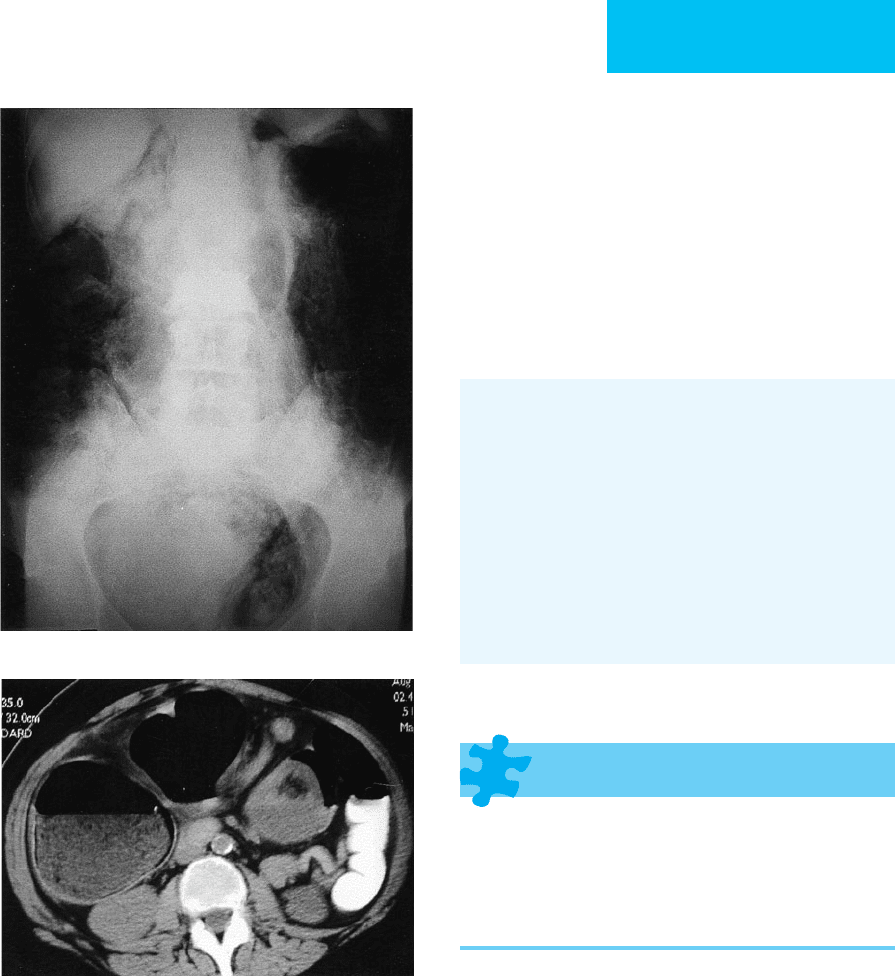
Figure 7–22. A: Pneumoperitoneum in a 72-year-old man with perforated sigmoid diverticulitis. On a supine radi-
ograph, there is lucency over the right upper quadrant with visualization of falciform ligament. Both sides of small
bowel wall are visualized (Rigler’s sign) with characteristic triangles. B. Pneumoperitoneum in an 80-year-old man
after recent abdominal surgery. Supine radiograph demonstrates a more subtle example of Rigler’s sign.
IMAGING PROCEDURES
169
Bowel Obstruction
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Asymmetric dilation of proximal bowel loops.
Normal or collapsed distal bowel loops.
Small bowel obstruction: Dilated U-shaped loops with
air-fluid levels (upright or decubitus films) or a single
loop with air-fluid levels at different heights.
Large bowel obstruction: Cecal distention, absence of
rectal gas, or “triple flexure” and “coffee bean” signs of
sigmoid volvulus.
CT scan: Excellent for detecting bowel obstruction and
confirming the cause.
General Considerations
Mechanical obstruction of the bowel is a relatively common
occurrence in hospitalized patients. In the general population,
bowel obstructions account for approximately 20% of acute
abdominal conditions. Obstruction usually results from extrin-
sic compression but can occur from luminal obstruction.
Without prompt attention, bowel obstruction may progress to
bowel infarction because of disruption of venous outflow and
subsequent arterial blood supply. Bowel infarction may progress
to mucosal ulceration, necrosis, and perforation. Mortality rates
for untreated obstruction have been as high as 60%.
Approximately three-fourths of bowel obstructions are
related to the small bowel (enteric) and one-fourth to the
colon. Small bowel obstructions are most commonly due to
adhesions from prior abdominal surgery. Adhesions can
form rapidly, sometimes within 4–10 days after surgery, or
may develop manifestations many years later. Other causes of
small bowel obstruction include hernias (external and internal),
primary and metastatic tumors, intussusception, inflamma-
tory bowel disease, abscesses, and trauma.
Large bowel obstructions are most often (60%) caused by
primary carcinomas of the distal (left) colon. Metastatic
tumor or invasion from cancers of surrounding organs,
diverticulitis, sigmoid volvulus, and fecal impaction also may
cause a distal colonic obstruction.
Radiographic Features
A. Plain Abdominal Radiographs—An abdominal series that
includes supine plus upright or decubitus views of the
abdomen is only 50–60% sensitive for small bowel obstruction.
Objective evidence of small bowel obstruction includes asym-
metric dilation (luminal diameter >3 cm) of small bowel prox-
imal to the site of obstruction, with normal or decompressed
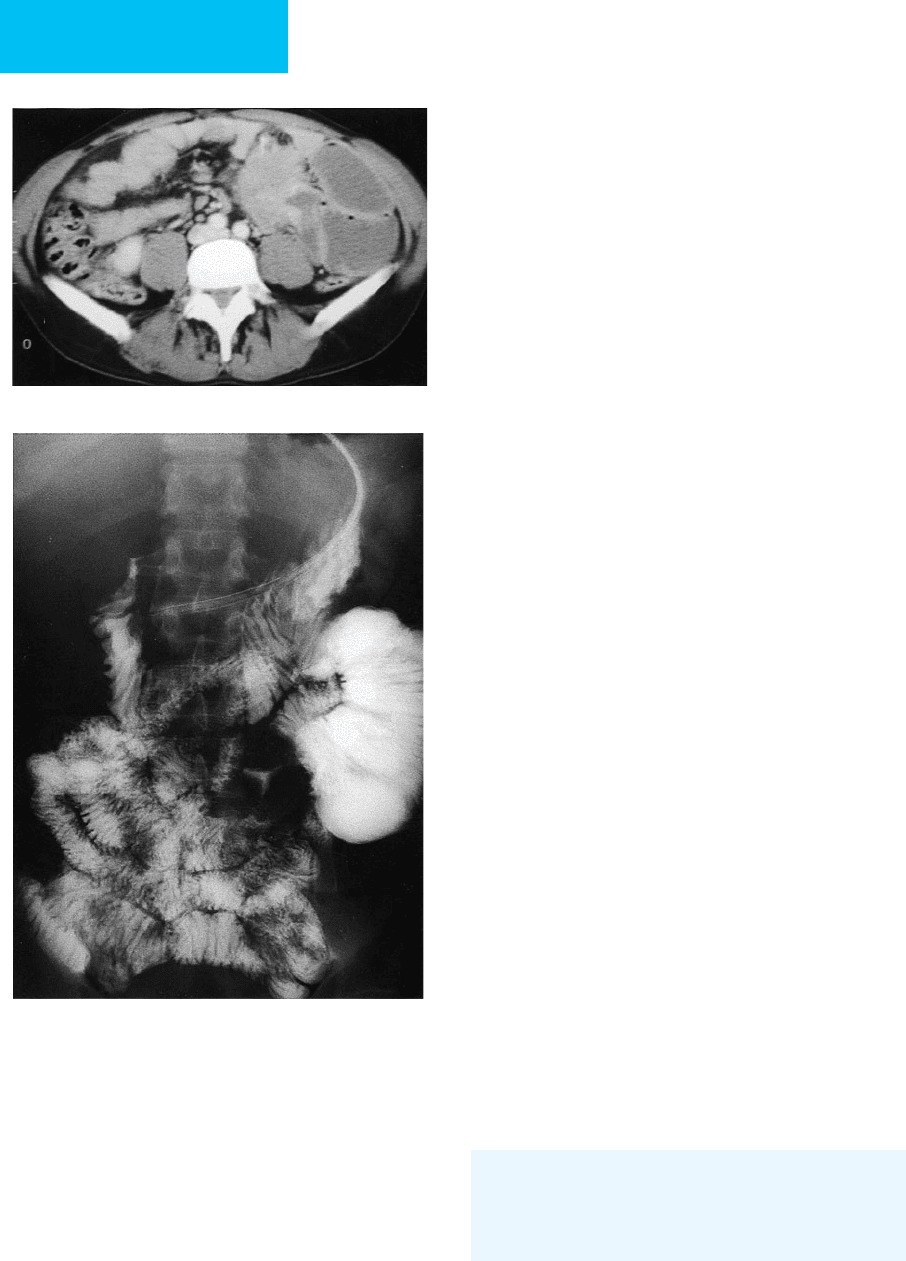
A
B
Figure 7–23. A. Pneumoperitoneum and pneu-
moretroperitoneum in a 76-year-old man after biliary
stent placement because of obstruction from pancre-
atic cancer. A supine radiograph shows characteristic
air under the diaphragm and surrounding liver. The
psoas muscles and kidneys are also outlined by gas,
confirming the presence of pneumoretroperitoneum.
B. Abdominal CT demonstrates ectopic gas and confirms
the diagnosis of pneumoperitoneum in the patient in
Figure 7–21.
CHAPTER 7
170
small bowel loops distally and normal to absent colonic gas.
However, these findings may not be seen in all patients who
present with a small bowel obstruction. More valuable is the
relative change in distention over time, and for this reason,
comparison of a series of studies is prudent. Other radi-
ographic signs include an inverted U-shaped loop of dilated
small bowel with air-fluid levels, multiple air-fluid levels, and
dynamic loops (air-fluid levels at varying heights in different
limbs of a loop). In some cases, a “string of pearls sign” can be
seen (Figure 7–24).
On a single supine film of the abdomen, dilated small
bowel loops may be mostly fluid-filled, with a minimal
amount of gas, or may be completely devoid of gas. In this
case, the film will be nonspecific, and additional views or CT
may be required. Diagnosis of small bowel obstruction may
be difficult because the presence of radiographic signs will
depend on the site, duration, and degree of obstruction.
Bowel distal to a complete obstruction takes 12–48 hours to
evacuate all its gas. Serial plain films sometimes are required
to capture these changes because films may be nonspecific if
imaging is performed too early.
Because of the limited utility of plain radiographs, helical
CT is now the preferred method for evaluating suspected
small bowel obstruction (Figure 7–25). In patients who can-
not undergo CT or if CT is unavailable, serial radiographs
may be taken after ingestion of enteric contrast material.
Although water-soluble contrast agents are preferred, espe-
cially for patients who are surgical candidates, they are
hypertonic and become progressively more dilute, limiting
the ability of the study to accurately identify the site of
obstruction. Barium is preferred in nonsurgical patients
because progressive dilution does not occur, and the site of
obstruction is more easily identified. However, in high-grade
obstructions, barium may thicken and become difficult to
evacuate. The high density of retained barium also degrades
CT images because of a beam-hardening artifact that results
in a nondiagnostic CT examination. Given these problems,
CT is the initial imaging procedure of choice if small bowel
obstruction is suspected.
In general, colonic obstruction (Figure 7–26) tends to occur
distally because most obstructing colon cancers occur in the dis-
tal large bowel. A single supine radiograph often fails to identify
the site of obstruction, and supplementary views—an upright
view, a right lateral decubitus view, or a prone view—may be
necessary to work up a possible obstruction and distinguish it
from an ileus. In large bowel obstruction, the cecum distends to
a greater degree than does the remainder of the colon regardless
of the site of obstruction. This follows from Laplace’s law, which
states that the pressure required to distend the walls of a hollow
structure is inversely proportional to its radius. The cecum has
the largest radius of any part of the large bowel. Generally, the
upper limits of normal for the transverse diameter of a large
bowel loop is 6 cm; for the cecum, it is 9 cm. However, these are
rough estimates only and may not hold true for a given patient.
Again, one must interpret, if possible, the relative change in dis-
tention with comparison studies over time. Perforation is a
dreaded complication of obstruction. The overall risk of cecal
perforation is low—approximately 1.5%—but may increase to
14% with delay in diagnosis. There is an increased risk of cecal
perforation if the luminal diameter exceeds 9 cm and persists
for more than 2–3 days.
B. Computed Tomography—Over the last 10 years, several
investigators have emphasized the value of CT scanning in
detecting bowel obstruction. Helical and multidetector CT
can produce multiplanar images to help determine whether
obstruction is present, the severity and level of obstruction,
the cause of obstruction, and whether strangulation or
ischemia is present. Current helical and multidetector tech-
nology permits evaluation of the abdomen and pelvis in 20
seconds to 2 minutes. Oral and intravenous contrast material
may not be required if experienced radiologists interpret the
scans. In most cases of small bowel obstruction, a transition
point between dilated and nondilated bowel can be demon-
strated. Identification of the transition zone and the cause of
obstruction, when not apparent on axial images, may be
aided by the multiplanar reformatting possible on current
CT scanners and image-processing workstations. Although
adhesions themselves are too thin to be imaged, most other
common causes of small bowel obstruction—including her-
nia, tumor, intussusception, postradiation fibrosis, and gall-
stone ileus—may be identified. The accuracy of CT is
90–95% in high-grade bowel obstruction but somewhat less
in low-grade obstruction.
Furukawa A et al: Helical CT in the diagnosis of small bowel
obstruction. Radiographics 2001;21:341–55. [PMID: 11259698]
Lappas JC, Reyes BL, Maglinte DD: Abdominal radiography
findings in small-bowel obstruction: Relevance to triage for
additional diagnostic imaging. AJR 2001;176:167–74.
[PMID:11133561]
Mak SY et al: Small bowel obstruction: Computed tomography
features and pitfalls. Curr Probl Diagn Radiol 2006;35:65–74.
[PMID: 16517290]
Nicolaou S et al: Imaging of acute small-bowel obstruction. AJR
2005;185:1036–44. [PMID: 16177429]
Thompson WM et al: Accuracy of abdominal radiography in acute
small-bowel obstruction: Does reviewer experience matter? AJR
2007;188:W233–8. [PMID: 17312028]
Ileus
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Diffuse symmetric dilation of small and large bowel.
May be focal when adjacent to an inflammatory source.
Colonic ileus (Ogilvie’s syndrome) may be seen alone or
in conjunction with small bowel ileus.
IMAGING PROCEDURES
171
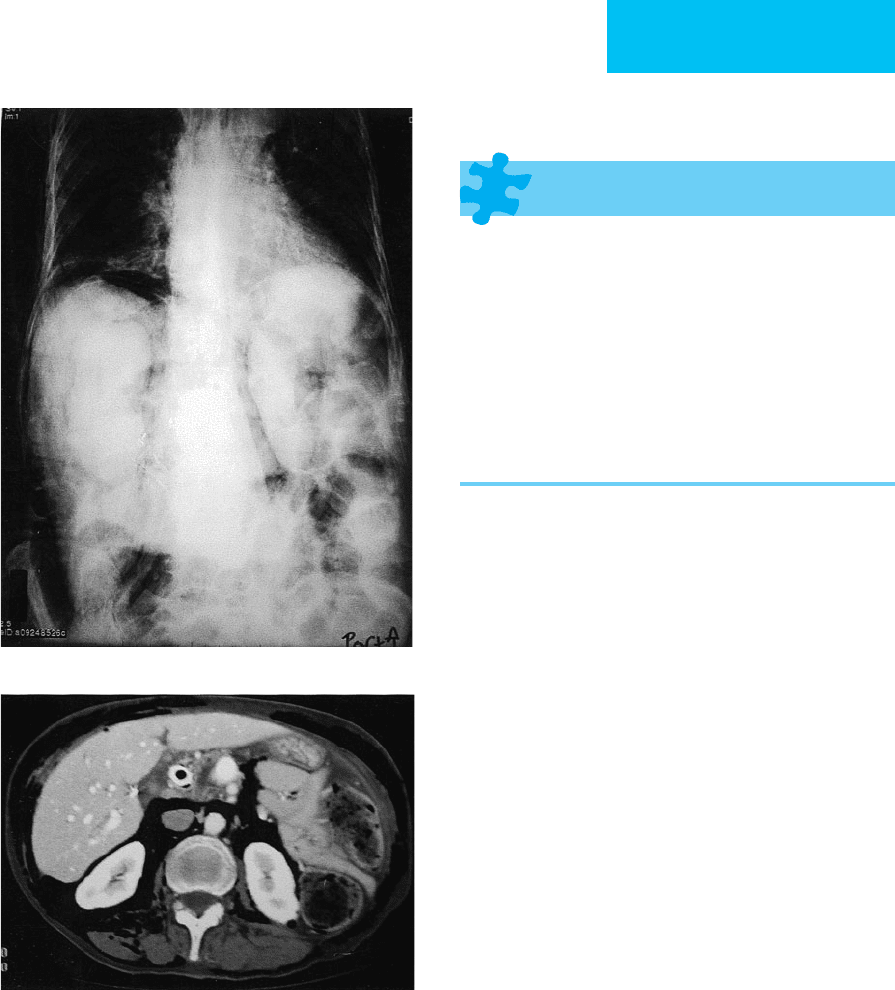
AB
C
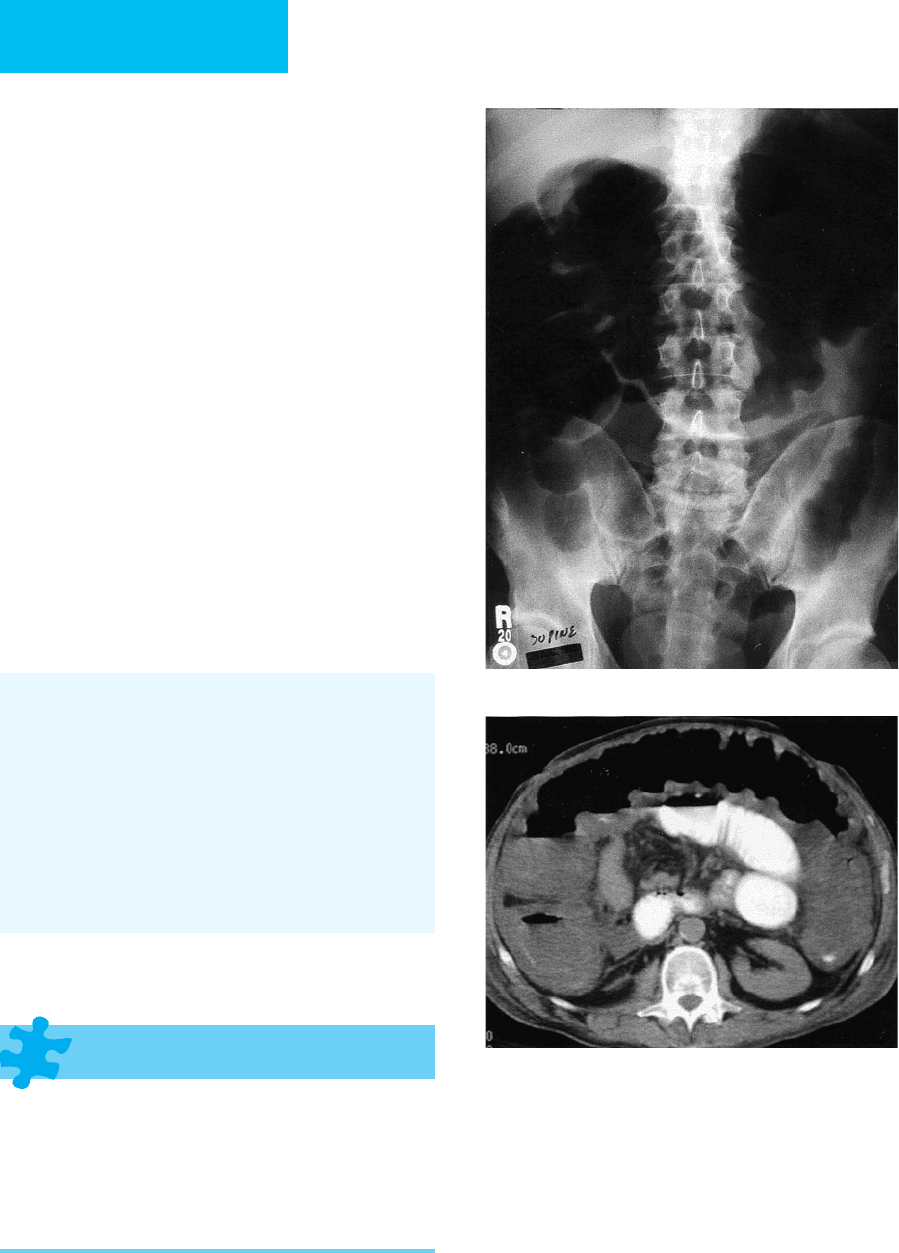
Figure 7–24. A. Small bowel obstruction. Because of their widespread availability, conventional upright and supine
radiographs are a good first step in suspected small bowel obstruction, although sensitivity and specificity are low.
A supine radiograph demonstrates asymmetric dilation of the proximal small bowel (note plicae circulares) without
significant gas in the colon. B. In the same patient, an upright abdominal radiograph demonstrates a prominent
air-fluid level from proximal small bowel obstruction. C. The “string of pearls sign” in small bowel obstruction; an
upright radiograph demonstrates numerous air-fluid levels.
CHAPTER 7
General Considerations
Ileus is generalized dysfunction of bowel related to an
underlying disorder, usually most severe in the 2–4 days
following abdominal surgery with extensive bowel manip-
ulation. Dysfunction due to humoral, metabolic, and neu-
ral factors contributes to the overall process. Other
common causes include abdominal infections, peritonitis,
active inflammatory bowel disease, opioid or chemother-
apy use, electrolyte imbalances, visceral pain syndrome
(biliary or ureteral colic, ovarian torsion), and myocardial
infarction.
Radiographic Features
In the generalized form of ileus, the small and large
bowel are dilated but generally to a lesser degree than
seen in moderate to severe bowel obstruction (Figure 7–27).
In many cases, there is a significant overlap with clinical
and radiologic features of small bowel obstruction, and
differentiation on the basis of a single study may not be
possible. Serial radiographs, contrast studies with water-
soluble contrast agents or barium, or CT may be
required.
An intraabdominal inflammatory event (acute pancreatitis)
or trauma may produce a focal form of ileus. The dysfunc-
tional segment of bowel may lose peristaltic activity and
enlarge. This is known as a sentinel loop.
Colonic ileus—also known as intestinal pseudo-
obstruction or Ogilvie’s syndrome—usually presents in
elderly, debilitated, or bedridden patients with major
underlying systemic abnormalities, severe infection,
cardiac disease, or recent surgery. Progressive large
bowel distention is variably accompanied by small bowel
distention. Massive cecal distention compromises blood
flow and may be complicated by perforation, with a
mortality rate of 30–45%. As in the small bowel, colonic
ileus is not always diffuse and may be segmental, typi-
cally in the cecum. In cecal ileus, there is massive dila-
tion of the cecum. If the cecum is mobile, this condition
may be difficult to distinguish from cecal volvulus, and
a contrast examination may be necessary to make the
differentiation.
Conservative treatment, consisting of nasogastric tube,
rectal tube, or colonoscopic decompression, is successful in
78% of patients. Alternatively, surgical cecostomy may be
necessary. Percutaneous cecostomy may be offered to high-
risk patients.
Nunley JC, FitzHarris GP: Postoperative ileus. Curr Surg
2004;61:341–5. [PMID: 15276337]
Saunders MD, Kimmey MB: Colonic pseudo-obstruction: The
dilated colon in the ICU. Semin Gastrointest Dis 2003;14:20–7.
[PMID: 12610851]
∂
A
B
172
Figure 7–25. A. CT is excellent for diagnosing small
bowel obstruction and for detecting a cause (eg, mass,
intussusception, or hernia). In this patient, a large
leiomyosarcoma caused a high-grade small bowel
obstruction. B. In certain situations, following luminal
contrast material through the small bowel (small bowel
follow-through) may be helpful for detecting small
bowel obstruction. This study from the same patient
demonstrates an abrupt tapering of the bowel lumen
with dilated proximal bowel due to the mass.
IMAGING PROCEDURES
173
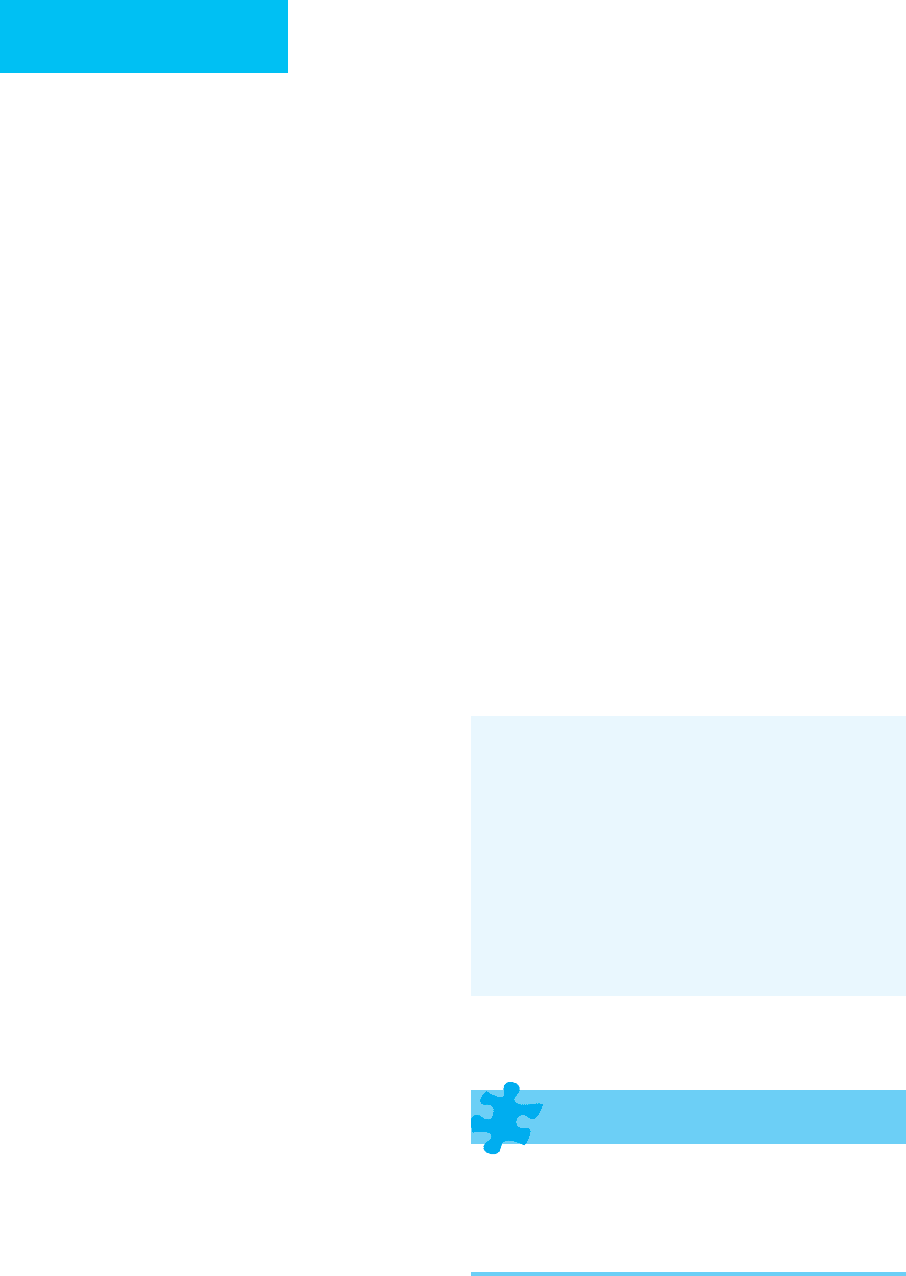
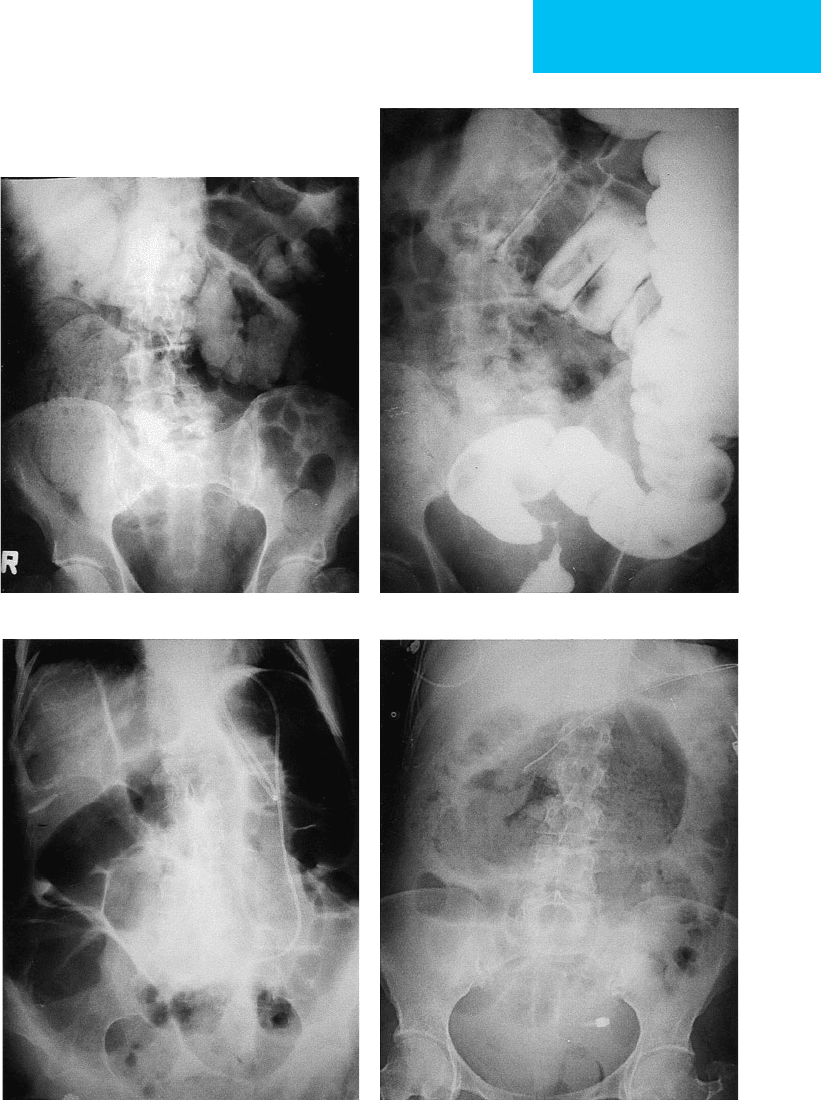
AB
CD
Figure 7–26. Large bowel obstruction. A. Most large bowel obstructions occur distally and are due to tumors or
diverticulitis. In this patient, the large bowel is diffusely dilated and filled with stool. B. A single-contrast barium
enema depicts a short segment annular carcinoma causing sigmoid colon obstruction. C. Sigmoid volvulus. On plain
radiograph, the dilated sigmoid colon may project over the right upper quadrant with a “coffee bean” appearance. The
remainder of the colon is dilated. D. Cecal volvulus. On plain radiographs, the dilated cecum is filled with stool and
projects over the midabdomen or sometimes the left upper quadrant. The small bowel is diffusely dilated.
CHAPTER 7
Intestinal Ischemia
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Plain films: Early: normal or nonspecific dilation of
bowel; later: focal, edematous, thick-walled bowel
loops, gas in the superior mesenteric and portal veins,
pneumatosis intestinalis, ileus, and gasless abdomen.
Abdominal CT: bowel wall thickening, pneumatosis;
portal venous gas usually sign of infarction.
CT or MRA provides excellent evaluation of the larger
mesenteric arteries and veins.
Conventional angiography is infrequently needed but
may be confirmatory in some situations.
General Considerations
Early diagnosis of bowel ischemia and infarction remains diffi-
cult because of limited clinical and radiologic sensitivity.
Vascular insufficiency must be considered in elderly patients or
for any patient with atherosclerotic vascular disease, hypoten-
sion, cardiac failure, or arteritis. In young patients, vasculitis, a
hypercoagulable state, pregnancy, illicit use of cocaine, or
embolic sources (eg, patent foramen ovale) must be suspected.
Morbidity and mortality rates remain high (30–80%).
Ischemia has a variety of underlying causes, including
mesenteric arterial occlusion (ie, thrombus, embolus, or dis-
section), venous occlusion (ie, hypercoagulable states or
malignancy), nonocclusive mesenteric ischemia (ie,
vasospasm, myocardial infarction, or shock), and mechanical
obstruction, including colonic pseudo-obstruction. Any por-
tion of the small bowel may be affected; the cecum and dis-
tal left colon are the large bowel segments affected most
commonly. Rectal ischemia is infrequent because of the rec-
tum’s dual blood supply, but it may be seen in patients who
have had prior radiation therapy to that area.
Clinical symptoms are variable. Generally, abdominal
pain out of proportion to physical findings, and bloody
diarrhea may be suggestive of ischemic colitis. Segmental
ischemia often resolves spontaneously, but fibrotic strictures
may develop. Infarcted bowel must be surgically resected. In
selected patients, clots identified on IV contrast-enhanced
CT may be treated with angiographic interventional tech-
niques, including thrombolysis or stent placement.
Radiographic Features
A. Plain Radiographs—Edematous, thick-walled bowel,
pneumatosis intestinalis, and portal venous gas are the most
specific signs of ischemia and infarction but are insensitive.
More commonly, plain films are normal, show lack of
abdominal gas, or suggest focal ileus or small bowel obstruc-
tion (Figure 7–28).
B. Computed Tomography—Helical CT is important for
detecting early changes of ischemia. A high-quality helical CT
is usually performed with oral contrast material to opacify
and distend the small bowel along with rapid IV contrast
material injection (3 mL/s) to optimize opacification of the
superior mesenteric artery and vein. The CT features of
intestinal ischemia vary with its cause, chronicity, and sever-
ity. Bowel wall thickening is a sensitive but nonspecific early
finding and may be accompanied by a “target sign” appear-
ance of bowel caused by submucosal edema. Indirect signs of
ischemia include focal ascites, bowel distention, and mesen-
teric edema. In more advanced stages of bowel ischemia, the
presence of gas within the bowel wall or within the superior
mesenteric or portal vein makes the prognosis more grave.
Colonic ischemia generally results from hypoperfusion or
hypotension, and mesenteric thrombosis is rare. CT angiog-
raphy using newer-generation multidetector helical scanners
∂
174
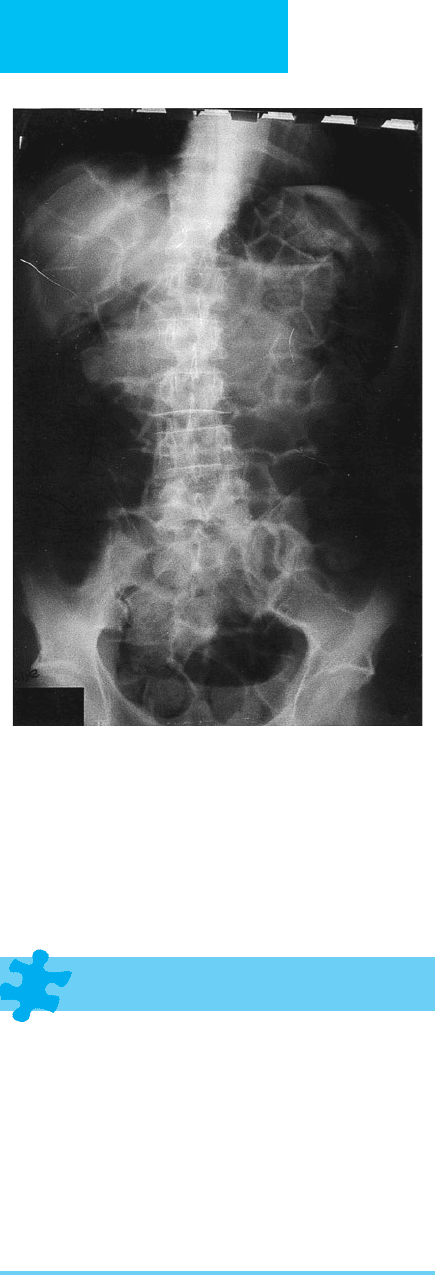
Figure 7–27. Ileus. Plain abdominal radiograph
demonstrates mild diffuse gaseous dilation of both the
small and the large bowel. No transition point is present.
IMAGING PROCEDURES
175
allows excellent vascular and intestinal wall assessment, aided
by three-dimensional image processing (eg, multiplanar,
volume-rendered, and maximum-intensity projection views).
Thrombus in the major mesenteric vessels may be detected.
However, a normal CT does not exclude ischemia, and if a
strong clinical suspicion is present—especially in patients
with vasculitis—angiography or surgery may be required.
C. Catheter Angiography—Angiography may be both diag-
nostic and therapeutic. Vasodilators may be used in conjunc-
tion with thrombolytic agents in certain patients. While
angiography remains the diagnostic standard in patients
with vasculitides given its unparalleled spatial resolution,
multidetector CT and modern MR scanners have narrowed
the resolution gap. Angiography has a limited role in colonic
ischemia because low-blood-flow states rather than occlu-
sion of the vasculature are most often the cause.
Bradbury MS et al: Mesenteric venous thrombosis: Diagnosis and
noninvasive imaging. Radiographics 2002;22:527–41. [PMID:
12006685]
Horton KM, Fishman EK: Multidetector CT angiography in the
diagnosis of mesenteric ischemia. Radiol Clin North Am
2007;45:275–88. [PMID: 17502217]
Kirkpatrick ID, Kroeker MA, Greenberg HM: Biphasic CT with mesen-
teric CT angiography in the evaluation of acute mesenteric ischemia:
Initial experience. Radiology 2003;229:91–8. [PMID: 12944600]
Nehme OS, Rogers AI: New developments in colonic ischemia.
Curr Gastroenterol Rep 2001;3:416–9. [PMID: 11560800]
Shih MC, Hagspiel KD: CTA and MRA in mesenteric ischemia: 1.
Role in diagnosis and differential diagnosis. AJR 2007;
188:452–61. [PMID: 17242255]
Colitis
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Colonic wall thickening and nodularity associated with
paralytic ileus.
Infiltration of pericolonic fat, often seen on CT.
Plaque-like filling defects are suggestive of pseudomem-
branous colitis.
General Considerations
Inflammatory bowel disease, ischemia, and infections are the
most common causes of colitis. Patients present with pain,
bloody diarrhea, cramping, fever, and leukocytosis.
Infectious colitis may be bacterial, viral, fungal, or parasitic.
Stool cultures, serologic tests, or colonic biopsy may be
required.
Pseudomembranous colitis—the most common cause of
colitis in hospitalized populations—is a complication of
antibiotic therapy. Clostridium difficile produces an entero-
toxin that causes mucosal ulceration and edema and the
development of pseudomembranes. The process may be
focal or diffuse.
Figure 7–28. Colonic ischemia. A. Plain radiograph
demonstrates mottled lucency of the wall of the ascend-
ing colon consistent with pneumatosis. B. Abdominal CT
is excellent for confirmation of pneumatosis.
A
B
CHAPTER 7
176
Neutropenic colitis is typically seen in patients undergo-
ing chemotherapy or bone marrow transplantation with
myelosuppression. Although involvement can be diffuse, it
typically affects the ascending colon, cecum, appendix, and
terminal ileum. If cecal inflammation is present, then the
term typhlitis (or necrotizing enterocolitis) is used.
Radiographic Features
Although usually normal or nonspecific, plain radiographs
may reveal colonic fold thickening and nodularity. Features
of paralytic ileus may be present. Contrast studies such as a
barium enema should be avoided but can be performed care-
fully with water-soluble agents only if absolutely necessary
(Figure 7–29). Although abdominal CT is an excellent test, it
may be normal in early infectious colitis. In more advanced
cases of infectious colitis and in pseudomembranous colitis,
mural thickening is more severe, averaging 15–20 mm, with
a target or halo pattern. An accordion-like pattern reflecting
haustral thickening may be produced in addition to peri-
colonic inflammatory changes and lymphadenopathy. In
neutropenic colitis (typhlitis), similar features are present,
but most commonly in the right colon. Occasionally in
advanced cases, pneumatosis intestinalis and frank perfora-
tion may develop.
Horton KM, Corl FM, Fishman EK: CT evaluation of the colon:
Inflammatory disease. Radiographics 2000;20:399–418. [PMID:
10715339]
Kawamoto S et al: Pseudomembranous colitis: Spectrum of imag-
ing findings with clinical and pathologic correlation.
Radiographics 1999;19:887–97. [PMID: 10464797]
Ramachandran I et al: Pseudomembranous colitis revisited:
Spectrum of imaging findings. Clin Radiol 2006;61:535–44.
[PMID: 16784938]
Thoeni RF, Cello JP: CT imaging of colitis. Radiology
2006;240:623–38. [PMID: 16926320]
Zalis M, Singh AK: Imaging of inflammatory bowel disease: CT
and MR. Dig Dis 2004;22:56–62. [PMID: 15292695]
Toxic Megacolon
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Gaseous colonic distention, which may be diffuse or
segmental.
Effacement of haustra, edematous folds (thumbprinting),
relative paucity of feces.
Common complication of a number of inflammatory
conditions, notably ulcerative colitis.
Figure 7–29. A. Colitis. Plain radiograph demon-
strates mild dilation and severe fold thickening
(thumbprinting) of transverse colon in this case of
pseudomembranous colitis. B. Abdominal CT also
demonstrates mural colonic thickening with associated
infiltration of the pericolonic fat.
A
B
