Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

IMAGING PROCEDURES
157
Radiographic Features
Septic pulmonary emboli appear radiographically as wedge-
shaped or rounded peripheral opacities. Septic emboli are
usually multiple and are more numerous in the lower lobes,
reflecting increased blood flow to the dependent lung. The
lesions may vary in size by virtue of variations in the timing
of embolization. Cavitation, typically thin-walled, is com-
mon, and necrotic debris may be identified within the cavity.
Hilar and mediastinal adenopathy can occur, and empyema
may occur.
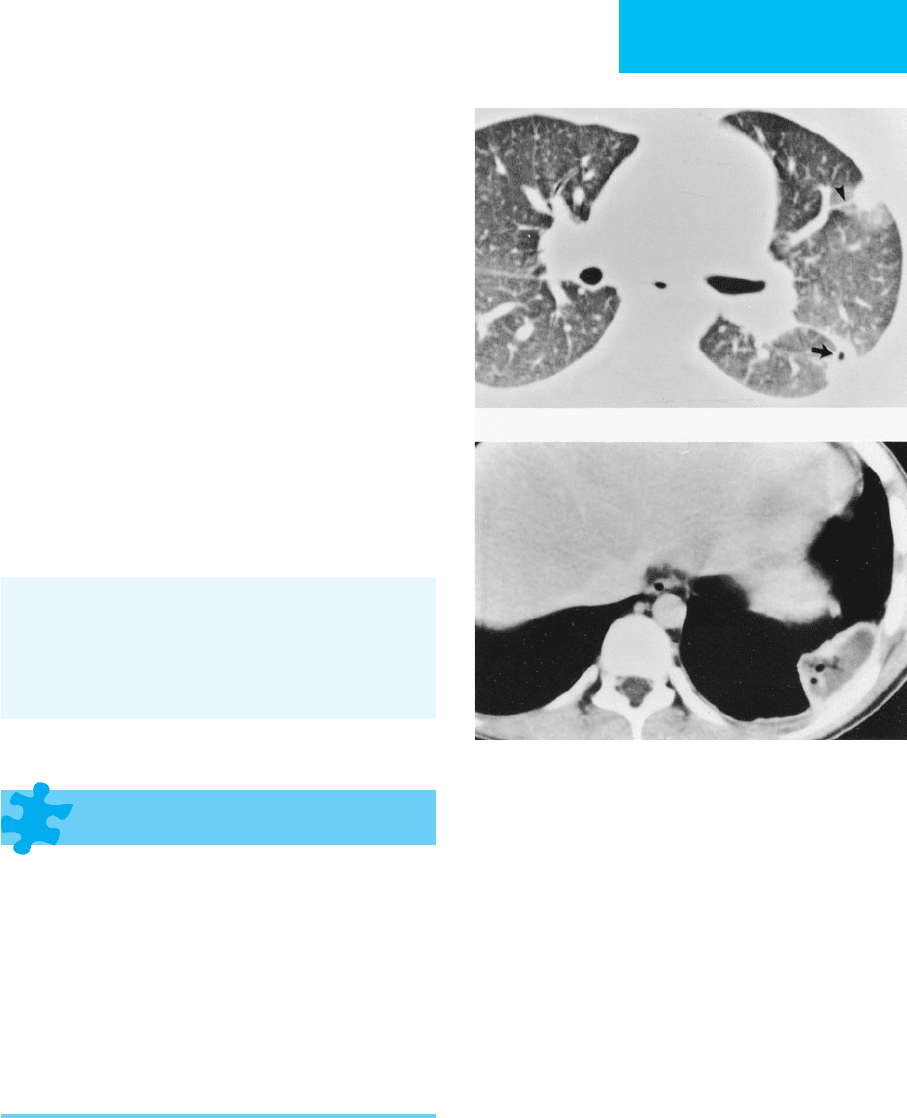
The CT features of septic emboli have been described.
Peripheral nodules with identifiable feeding vessels, wedge-
shaped peripheral opacities, and cavitation are the most diag-
nostic features. Peripheral enhancement along the margins of
the wedge-shaped densities has been reported following
administration of intravenous contrast material (Figure 7–11).
It has been suggested that CT can detect disease earlier than the
plain radiograph and that it better characterizes the extent of
disease. Moreover, the cross-sectional perspective of CT affords
better identification of embolic lesions that may be obscured
on chest radiographs by edema or other diffuse consolidations.
Han D et al: Thrombotic and nonthrombotic pulmonary arterial
embolism: Spectrum of imaging findings. Radiographics
2003;23:1521–39. [PMID: 14615562]
Huang RM et al: Septic pulmonary emboli: CT-radiographic cor-
relation. AJR 1989;153:41–5. [PMID: 2735296]
Iwasaki Y, et al: Spiral CT findings in septic pulmonary emboli. Eur
J Radiol 2001;37:190–4. [PMID: 11274848]
Pulmonary Edema
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Interstitial edema:
Kerley B (most common), A, and C lines.
Peribronchial cuffing.
Indistinct pulmonary vessels.
Hilar haze.
Alveolar edema:
Poorly marginated, coalescent opacities.
Air bronchograms.
“Butterfly” pattern.
General Considerations
Pulmonary edema—an excess of water in the extravascular space
of the lung—is a frequent cause of respiratory distress in the crit-
ically ill patient. The three main categories of pulmonary edema
are cardiac edema secondary to myocardial or endocardial dis-
ease, volume overloaded state due to renal failure or excess
administration of fluid, and increased capillary permeability,
which may result from a variety of insults to the microvascula-
ture of the lung. In the ICU patient, more than one mechanism
may contribute to the formation of edema, increasing the diffi-
culty of diagnostic interpretation on radiographs.
There are four principal mechanisms that result in the
development of edema: elevated capillary hydrostatic pressure,
decreased plasma oncotic pressure, increased capillary perme-
ability, and obstruction of lymphatic drainage. Decreased
plasma oncotic pressure and obstruction to lymphatic drainage
only rarely lead to pulmonary edema but may be contributing
factors in the setting of increased hydrostatic pressure. The
A
B
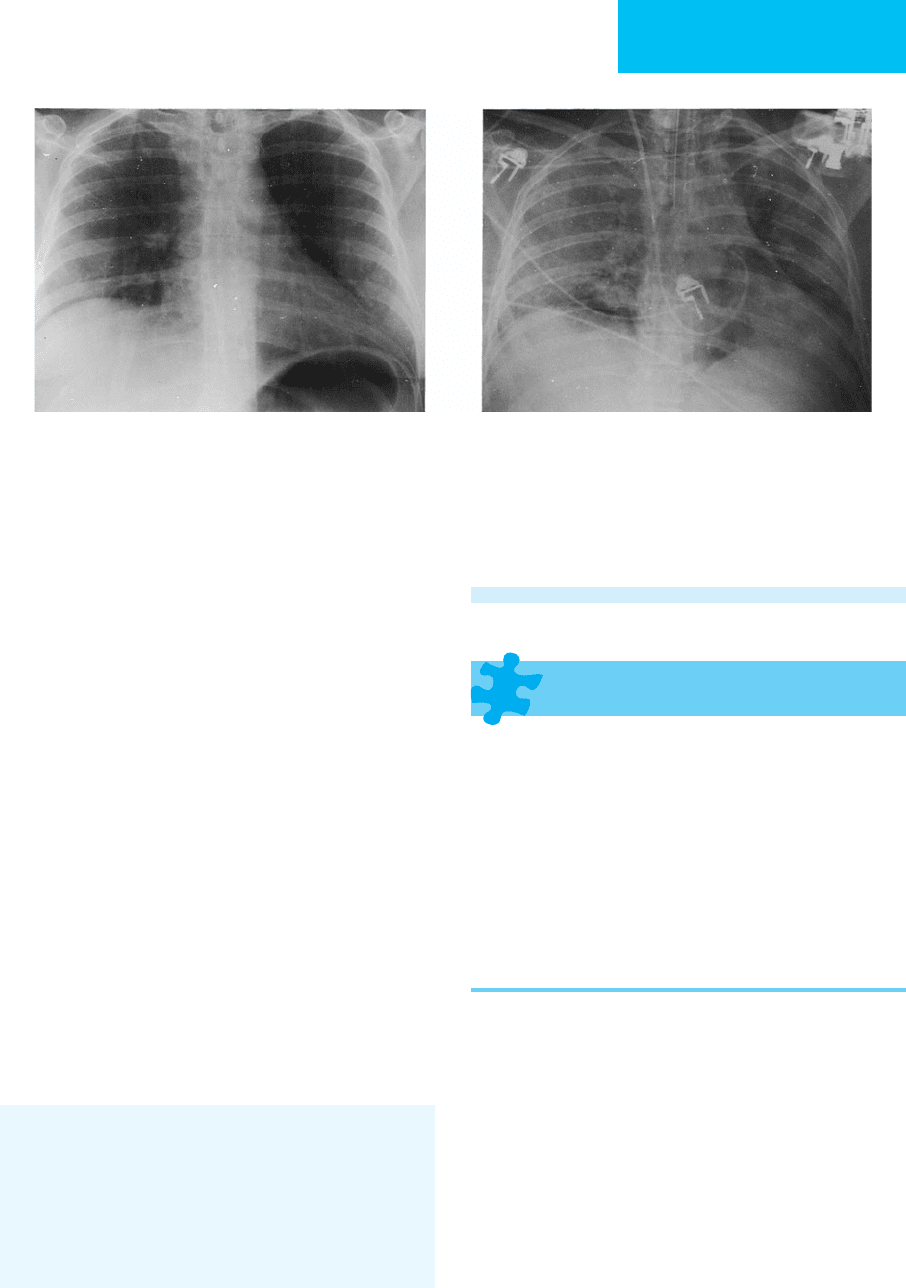
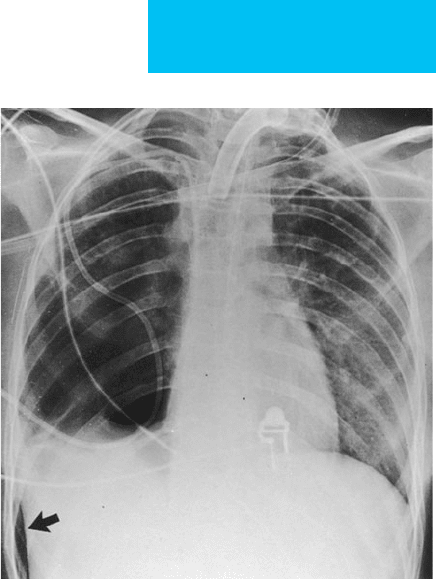
Figure 7–11. Young woman with septic emboli second-
ary to intravenous drug abuse. Blood cultures were positive
for Staphylococcus aureus. A. Peripheral nodular opacities
are present with evidence of cavitation (arrow). A feeding
vessel is identified leading to a pulmonary nodule, consis-
tent with hematogenous dissemination (arrowhead).
B. Wedge-shaped subpleural lesion is noted with periph-
eral enhancement after administration of intravenous contrast
material.
CHAPTER 7
158
most common cause of pulmonary edema is hydrostatic pres-
sure elevation due to cardiac disease. Acute myocardial infarc-
tion, acute volume overload of the left ventricle, and mitral
stenosis are common causes of cardiogenic edema.
Radiographic Features
The chest radiograph is the most commonly used noninva-
sive test in the evaluation of a patient with pulmonary
edema. Interstitial edema may be present radiographically in
the absence of clinical signs and symptoms, and the chest
radiograph may be the first indication of pulmonary edema.
A. Cardiogenic Pulmonary Edema—In the patient with heart
failure, pulmonary edema is preceded by pulmonary venous
hypertension. In patients with left ventricular failure, elevated left
ventricular end-diastolic pressure (pulmonary venous hyperten-
sion) is reflected in the pulmonary vasculature by dilation and
redistribution of pulmonary blood flow to the upper lobes. In the
normal erect patient, the upper zone vessels are smaller than the
lower zone vessels, and a significant fraction of the pulmonary
circulation, particularly to the upper lobes, is not perfused. In
conditions of increased pulmonary blood volume or left ventric-
ular failure, there is recruitment of these nonperfused reserve ves-
sels in the upper lobes, while reflex hypoxic vasoconstriction of
lower lobe vessels occurs. These and other pathophysiologic fac-
tors contribute to the phenomenon of upper lobe arterial and
venous redistribution. Vascular redistribution is often difficult to
observe on radiographs, particularly in critically ill patients imaged
in the semierect or supine position. As the pulmonary venous
pressure continues to increase, pulmonary edema develops.
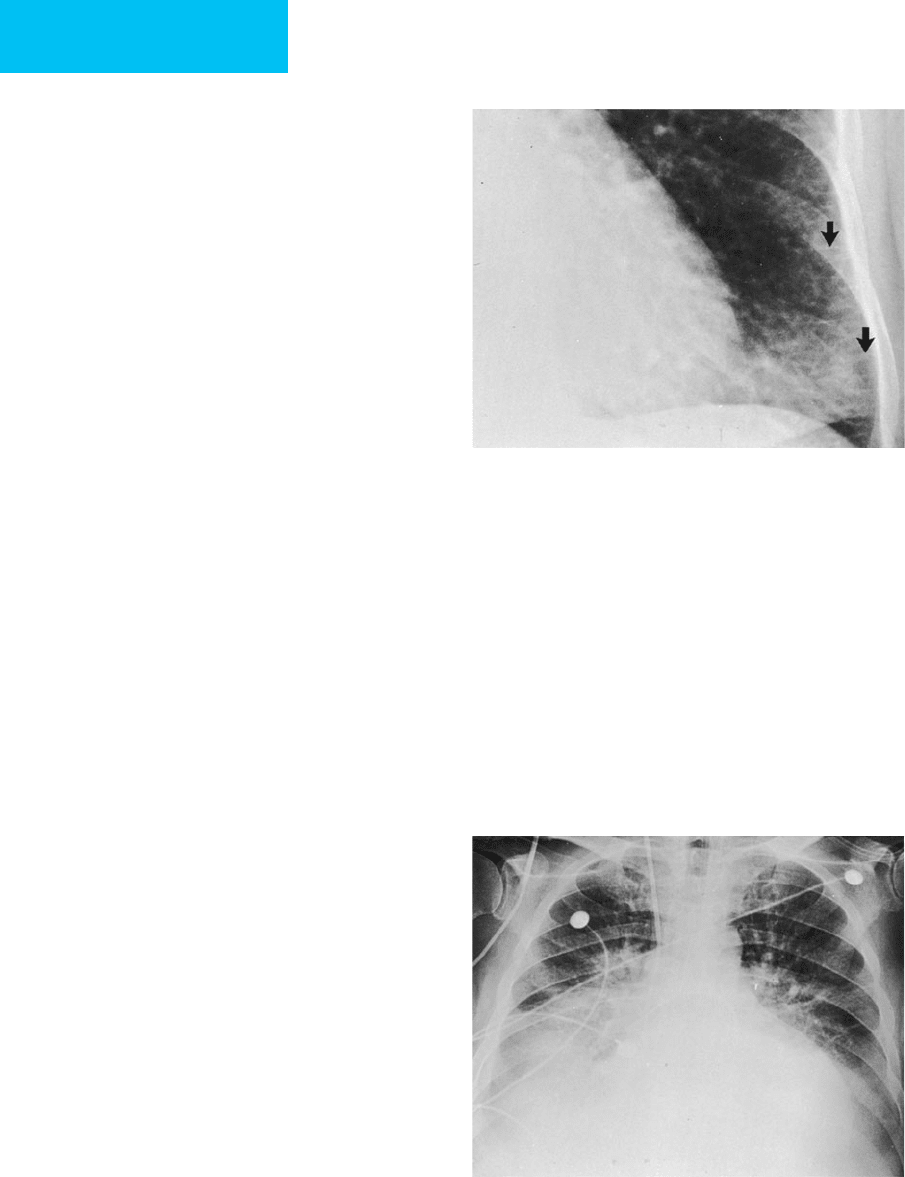
Pulmonary edema may be present within the pulmonary
interstitium, the alveoli, or both. Radiographic evidence of inter-
stitial edema includes Kerley A, B, and C lines; peribronchial cuff-
ing; hilar haze; indistinct vascular markings; and subpleural
edema. Kerley lines represent thickened interlobular septa, with
Kerley B lines being the most easily and most frequently seen.
These lines are horizontal linear densities measuring 1–2 cm in
length and 1–2 mm in width. They are located peripherally,
extend to the pleural surface, and are best seen at the lung bases on
the frontal film (Figure 7–12). Kerley A lines are longer and more
randomly oriented and are best seen in the upper lobes, directed
toward the hila. Kerley C lines are presumably a superimposition
of many thickened interlobular septa and appear as a fine reticu-
lar pattern. Other signs of interstitial edema, including peri-
bronchial cuffing, hilar haze, and indistinct vascular markings,
result from accumulation of fluid in the perivascular and peri-
bronchial interstitium. Accumulation of fluid in the subpleural
interstitium is best demonstrated along the pleural fissures.
Alveolar edema occurs as fluid fills the air spaces of the
lungs (Figure 7–13). Although interstitial edema precedes alve-
olar edema and continues to be present in the alveolar filling
stage, the interstitial component is frequently obscured by
concomitant air space edema. With filling of the air spaces, the
lung becomes opaque, with poorly defined confluent opacity.
Air bronchograms are identified as tubular lucencies repre-
senting normal patent bronchi surrounded by fluid-filled air
spaces. The butterfly pattern, appearing as a dense perihilar
opacification, has been described in volume overloaded states
and cardiogenic edema.
In general, cardiogenic pulmonary edema is bilateral and
symmetric. Atypical edema patterns may be seen in patients
with underlying acute or chronic lung disease or as a conse-
quence of gravitational forces related to patient positioning.
Destruction of the lung due to emphysema may cause a
patchy, asymmetric distribution of edema that spares regions
of bullous disease. Gravitational forces also affect the distribu-
tion of edema, with increased edema in the dependent lung.
Shifting the patient’s position can change the appearance of
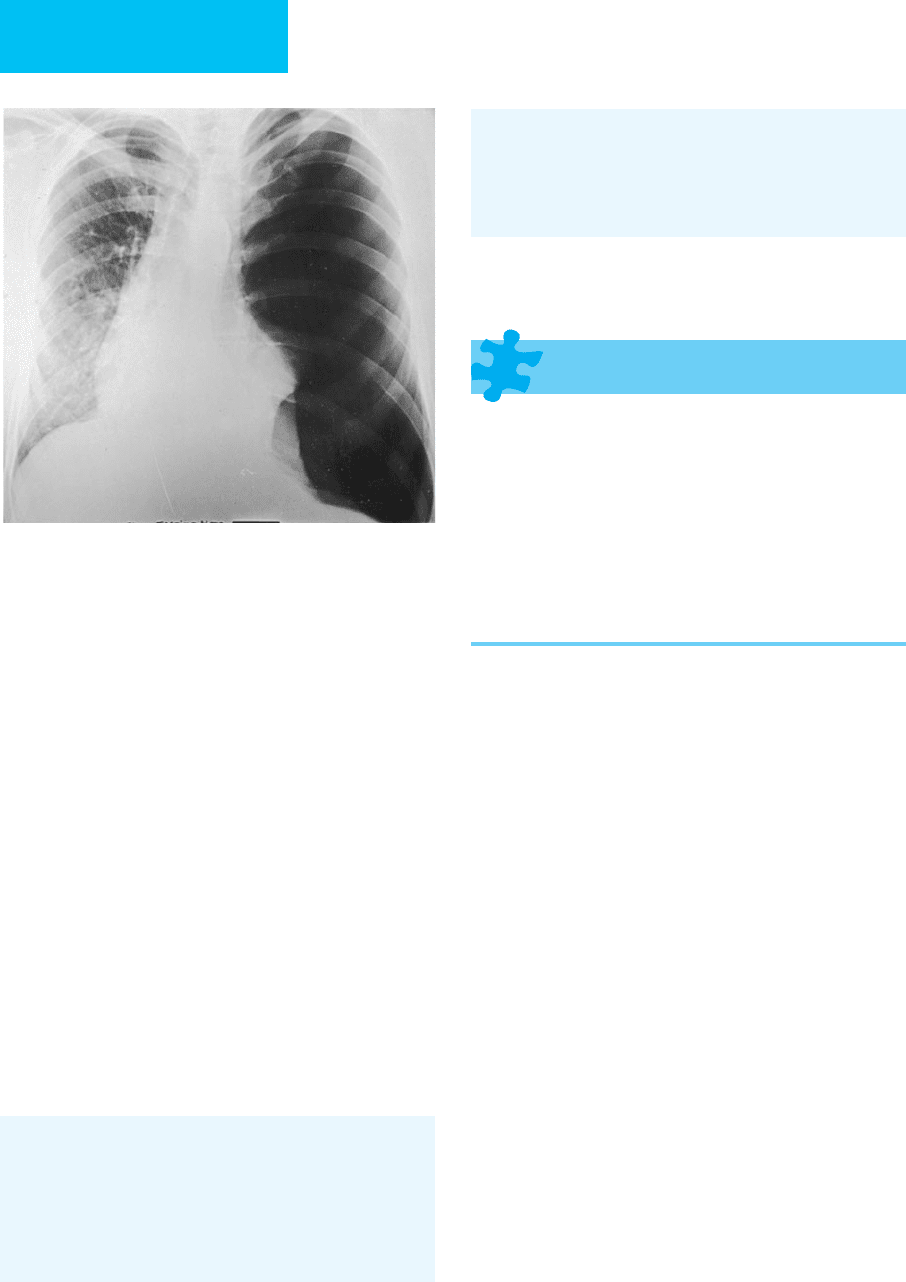
Figure 7–12. Interstitial edema. Kerley B lines are
identified at the lung bases (arrows).
Figure 7–13. Alveolar edema. Air space opacities
with vascular redistribution, perihilar haze, cardiomegaly,
and bilateral pleural effusions are secondary to cardio-
genic edema. A pulmonary artery catheter and nasogas-
tric tube are present.
IMAGING PROCEDURES
159
edema. Such maneuvers may help to distinguish atypical
edema from other air space processes such as pneumonia.
The temporal sequence of parenchymal opacification is also
crucial because the onset and resolution of hydrostatic
edema may be rapid, whereas in other conditions such as
pneumonia and ARDS, changes are more gradual.
The CT findings in heart failure have been studied and, as
predicted by the chest radiograph, include “ground glass”opac-
ities, interstitial and alveolar edema, and pleural effusions.
Small pulmonary nodules also have been described and likely
represent pulmonary vessels and regions of edema. Mediastinal
adenopathy may be present, with 35% of patients with chronic
heart failure demonstrating nodal enlargement on CT.
B. Distinguishing Cardiogenic from Noncardiogenic
Pulmonary Edema—Three principal features have been pro-
posed to distinguish cardiogenic from noncardiogenic pul-
monary edema radiographically: distribution of pulmonary
flow, distribution of pulmonary edema, and width of the vas-
cular pedicle. Ancillary features include pulmonary blood vol-
ume, peribronchial cuffing, septal lines, pleural effusions, air
bronchograms, lung volume, and cardiac size. The vascular
pedicle width is defined as the width of the mediastinum just
above the aortic arch, with normal width ranging from 43 to
53 mm in an erect patient. The vascular pedicle is enlarged in
60% of patients with cardiac failure and in 85% of patients
with renal failure or volume overload. This is in contrast to
patients with noncardiogenic capillary permeability edema,
who have a normal or narrowed vascular pedicle in 70% of
cases. The distribution of flow is also a discriminating feature
in that patients with hydrostatic edema more typically have bal-
anced flow or vascular redistribution. In contrast, patients with
capillary permeability edema usually demonstrate a normal or
balanced distribution of flow. Finally, the distribution of edema
is symmetric and perihilar or basilar in patients with cardio-
genic edema or volume overloaded states, whereas capillary
permeability edema appears patchy and peripheral.
Heart size and the presence or absence of septal lines also
may be useful criteria for differentiating cardiogenic from per-
meability edema with an accuracy of 83%. Thus, if the heart is
enlarged or of normal size and septal lines are present, cardio-
genic edema is likely, but if the heart size is of normal and sep-
tal lines are absent, permeability edema is more likely. There
may be considerable overlap. In one study, a classic hydro-
static pattern occurred in 90% of patients with hydrostatic
edema, but 40% of patients with increased permeability
edema had radiographic features consistent with hydrostatic
edema. A peripheral or patchy air space pattern was relatively
specific for capillary permeability edema. Overlapping features
may arise from differences in patient populations, including
differences in the severity of edema, underlying heart or lung
disease, and radiologic technique and patient positioning.
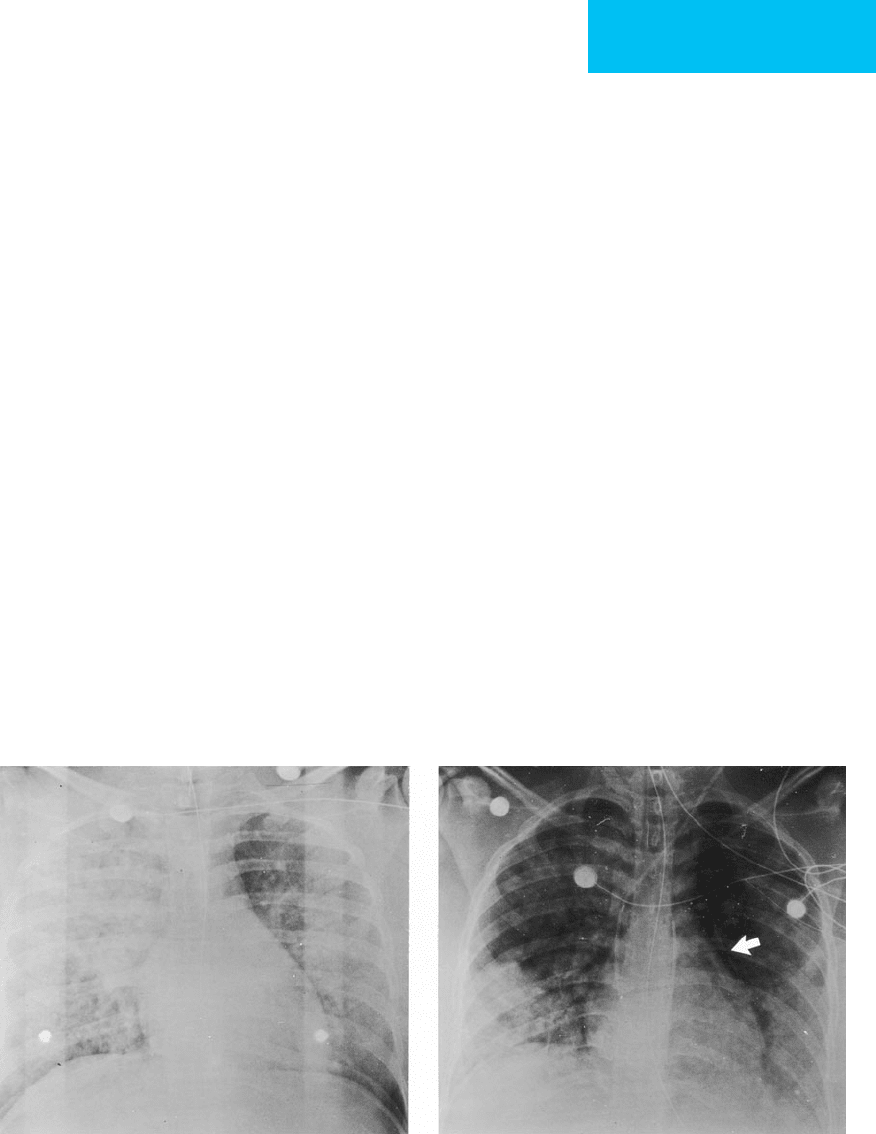
The radiographic diagnosis of edema may be complicated
by several factors. However, general guidelines can be suggested.
In general, noncardiogenic edema typically demonstrates nor-
mal cardiac size with air space opacities (Figure 7–14) and
AB
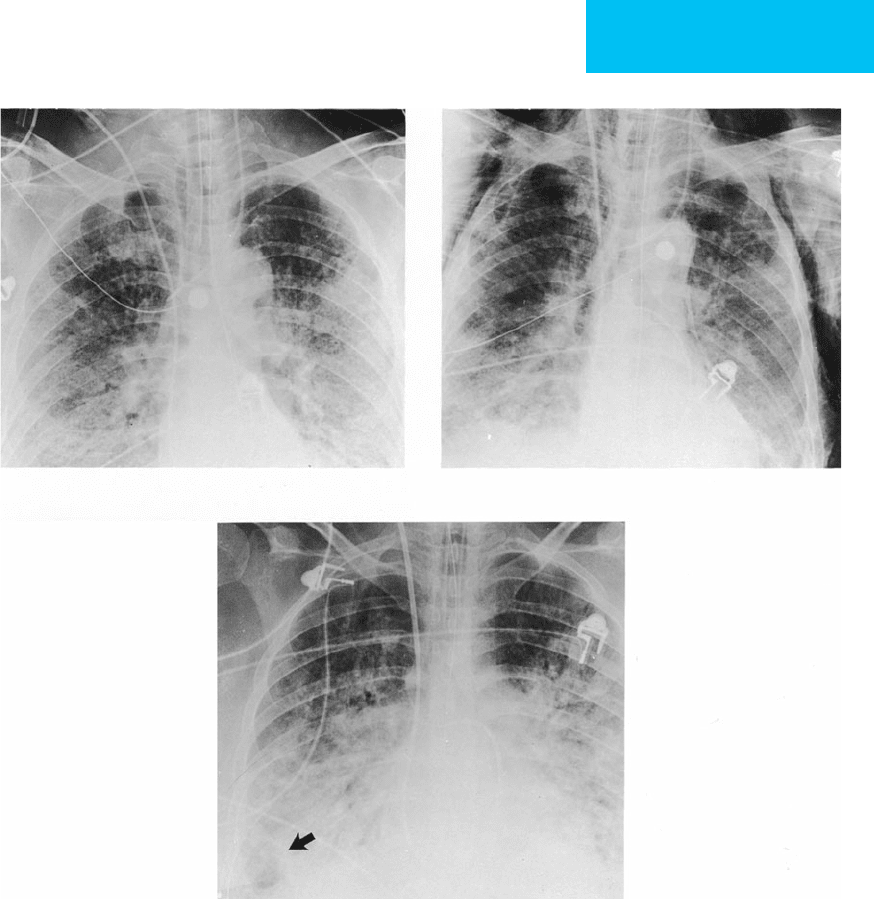
Figure 7–14. Noncardiogenic pulmonary edema secondary to near-drowning. A. Anteroposterior chest radiograph
demonstrates asymmetric air space opacities bilaterally. Heart size is normal, and there are no pleural effusions.
Endotracheal tube is high in position, and a nasogastric tube is present. B. Radiograph 48 hours after admission shows het-
erogeneous parenchymal opacification with worsening at the lung bases. A left thoracostomy tube and pulmonary artery
catheter are now present, and the endotracheal tube is in satisfactory position. There is evidence of barotrauma with pneu-
momediastinum (arrow).
CHAPTER 7
160
infrequent Kerley lines, peribronchial cuffing, or pleural effu-
sions. In contrast, hydrostatic edema is associated with cardiac
enlargement, septal lines, and frequent pleural effusions. The
accuracy of chest radiographic diagnosis depends on the inte-
gration of all available clinical and physiologic data.
Aberle DR et al: Hydrostatic versus increased permeability pul-
monary edema: Diagnosis based on radiographic criteria in crit-
ically ill patients. Radiology 1988;168:73–9. [PMID: 3380985]
Gluecker T et al: Clinical and radiologic features of pulmonary
edema. Radiographics 1999;19:1507–31. [PMID: 10555672]
Lewin S, Goldberg L, Dec GW: The spectrum of pulmonary abnor-
malities on computed chest tomographic imaging in patients
with advanced heart failure. Am J Cardiol 2000;86:98–100.
[PMID: 10867103]
Martin GS et al: Findings on the portable chest radiograph corre-
late with fluid balance in critically ill patients. Chest
2002;122:2087–95. [PMID: 12475852]
Miller RR, Ely EW: Radiographic measures of intravascular vol-
ume status: The role of vascular pedicle width. Curr Opin Crit
Care 2006;12:255–62. [PMID: 16672786]
Thomason JW et al: Appraising pulmonary edema using supine
chest roentgenograms in ventilated patients. Am J Respir Crit
Care Med 1998;157:1600–8. [PMID: 9603144]
Acute Respiratory Distress Syndrome
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Early ARDS: Decrease in lung volumes, but lungs are
generally clear. If ARDS is caused by aspiration or pneu-
monia, parenchymal opacifications may be present.
Later: Air space opacification is usually bilateral but may
be asymmetric and patchy and may progress later to
more uniform consolidation. Air bronchograms are usu-
ally present.
Late ARDS associated with collagen deposition shows
less dense parenchymal consolidations with interstitial
or “ground glass” opacities.
Complications include pulmonary interstitial emphy-
sema, pneumomediastinum, and pneumothorax.
General Considerations
ARDS is a catastrophic consequence of acute lung injury,
with damage to the alveolar epithelium and pulmonary vas-
culature resulting in increased capillary permeability edema.
Despite numerous attempts at clarification in the literature,
there is still disagreement about the best way to describe this
disorder. It is usually characterized clinically by refractory
hypoxemia, decreased lung compliance, severe acute respi-
ratory distress, and pulmonary parenchymal consolidations
on chest radiographs. A number of disorders are associated
with ARDS, including both direct insults to the lungs and
nonpulmonary systemic conditions.
Radiographic Features
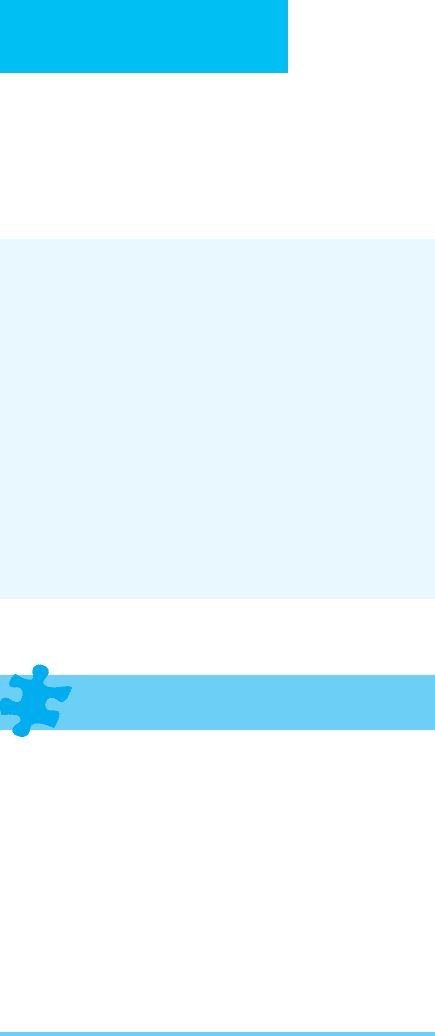
A. Chest Radiographs—The radiographic manifestations
correlate with the pathologic changes seen in the lungs and
vary with the stage of lung injury. Three stages have been
described in ARDS. Stage I (also known as the acute exuda-
tive phase) is the earliest and most transient stage of lung
injury and occurs during the first hours after the insult.
Pathologically, this stage is characterized by pulmonary cap-
illary congestion, endothelial cell swelling, and extensive
microatelectasis. Fluid leakage is confined to the intersti-
tium and is limited. Clinically, respiratory distress with
tachypnea and hypoxemia is present. In patients with ARDS
secondary to systemic insults, diffuse microatelectasis and
diminished lung compliance may result in a decrease in lung
volumes, but the lungs are generally clear. Interstitial fluid is
usually too mild to be radiographically apparent (Figure 7–15).
In primary pulmonary insults causing ARDS, such as aspira-
tion or pneumonia, parenchymal opacifications may be pres-
ent (Figure 7–16). Physiologic changes due to therapy are also
reflected on the radiograph, including volume overload and
barotrauma. The use of positive end-expiratory pressure
(PEEP) may cause improvement in aeration on the chest
radiograph without physiologic or clinical improvement. In
fact, occasionally there is paradoxical worsening of oxygena-
tion from alveolar overdistention with subsequent diversion
of pulmonary flow to poorly ventilated regions.
In stage II (also referred to as the fibroproliferative phase),
the pathologic features of hemorrhagic fluid leakage, fibrin
deposition, and hyaline membrane formation result in radi-
ographic consolidation. Air space opacification is usually bilat-
eral but may be asymmetric and patchy and may progress later
to more uniform consolidation. Air bronchograms are usually
present and become more conspicuous with severe consolida-
tion. The transition to stage II may occur 1–5 days following
the pulmonary insult depending on its type and severity. More
severe injuries result in a more rapid transition. Pleural effu-
sions are uncommon and, when present, are small.
Stage III (also referred as the fibrotic or recovery phase) is
characterized by hyperplasia of type II alveolar epithelial cells
and collagen deposition. Decreased lung compliance,
ventilation-perfusion imbalance, diffusion impairment, and
destruction of the microvascular bed result in abnormal gas
exchange and lung mechanics. Radiographically, parenchy-
mal consolidations become less dense and confluent.
Interstitial or “ground glass” opacities develop as fluid is
replaced by the deposition of collagen. Subpleural lucencies
may develop in regions of peripheral ischemia and ischemic
necrosis. The treatment of ARDS, including positive-pressure
ventilation, sometimes results in barotrauma that is mani-
fested as pulmonary interstitial emphysema, pneumomedi-
astinum, and pneumothorax (Figure 7–17).
Long-term sequelae of ARDS are variable. The overall mor-
tality rate is approximately 50%. Although long-term survivors
IMAGING PROCEDURES
161
may have complete recovery of pulmonary function, respiratory
impairment may result from pulmonary fibrosis and microvas-
cular damage. Improvement in lung function is relatively rapid
during the first 3–6 months, reaching maximum recovery
within 6–12 months following the onset of ARDS. The chest
radiograph may continue to show hyperinflation and some
residual lung opacities, but most often it returns to normal.
B. CT Scans—The CT appearance of ARDS has been
described by numerous investigators. In general, CT demon-
strates a variable and patchy distribution, with most marked
involvement in the dependent lung regions. These opacities
probably represent severe diffuse microatelectasis as well as
edema fluid and have been observed to migrate under the
influence of gravity. Air bronchograms are frequent, and
pleural effusions, typically small, occur in approximately
one-half of patients. The distribution of consolidation may
depend on the stage of ARDS. Early changes may show
patchy areas of “ground glass” opacity or consolidation dif-
fusely but not uniformly, without central or gravity depend-
ence. Later changes show more homogeneity as the lung
becomes more edematous, and gravity-dependent atelectasis
increases. On CT, barotraumatic lung cysts and infectious
complications such as cavitation or empyema are better
identified than on projectional radiographs (Figure 7–18).
Caironi P et al: Radiological imaging in acute lung injury and acute
respiratory distress syndrome. Semin Respir Crit Care Med
2006;XX:404–15. [PMID 16909374]
Desai SR et al: Acute respiratory distress syndrome caused by pul-
monary and extrapulmonary injury: A comparative CT study.
Radiology 2001;218:689–93. [PMID: 11230641]
Gattinoni L et al: What has computed tomography taught us about
the acute respiratory distress syndrome? Am J Respir Crit Care
Med 2001;164:1701–11. [PMID: 11719313]
IMAGING IN PLEURAL DISORDERS
Pleural Effusions
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Blunting of the lateral costophrenic angle (meniscus sign).
Elevation of the apparent level of the diaphragm. Increased
separation between the lung and the stomach bubble.
Homogeneous increased density of the involved
hemithorax.
Fluid capping the lung apex.
Decreased visibility of pulmonary vessels below the
diaphragm.
Increased density within the pleural fissures (“pseudo-
tumor”).
General Considerations
Pleural fluid is primarily formed on the parietal pleural sur-
face and absorbed on the visceral pleural surface, with
approximately 25 mL of fluid present normally in the pleural
space. Pleural effusion is an excess accumulation of
intrapleural fluid. A wide variety of disorders result in excess
pleural fluid. Although the chest radiograph is useful for
detecting and estimating the amount of pleural effusion, the
differentiation between transudate, exudate, empyema, and
hemorrhagic pleural effusion requires a thoracentesis.
Congestive heart failure is the most common cause of pleu-
ral effusion in the ICU population.
AB
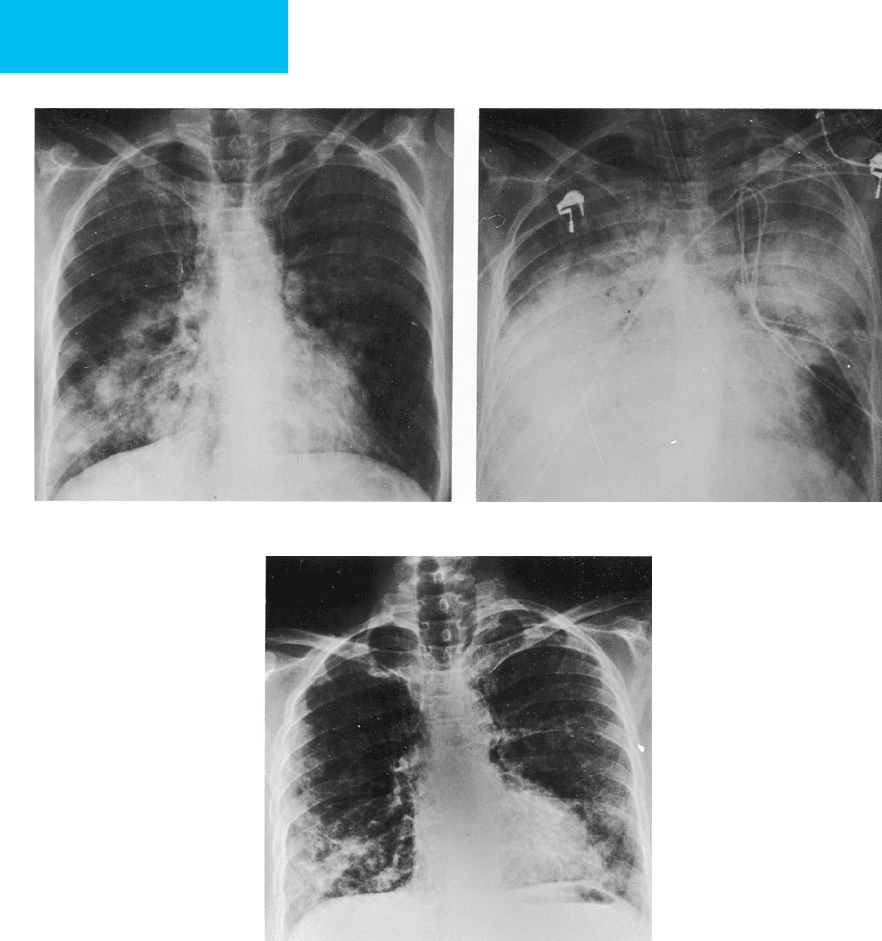
Figure 7–15. ARDS secondary to sepsis in an immunocompromised patient following bone marrow transplantation.
A. Stage I ARDS. The lungs are clear, despite marked dyspnea and hypoxemia. Lung volumes are slightly decreased.
B. Stage II ARDS. Within 24 hours, the chest radiograph shows diffuse parenchymal opacification consistent with ARDS.
CHAPTER 7
162
Radiographic Features
The distribution of fluid within the pleural space is greatly
affected by lung elastic recoil and gravity. On erect frontal and
lateral radiographs, free pleural effusions typically have a con-
cave, upward-sloping contour (the meniscus appearance). Since
the posterior costophrenic angles are usually deeper than the
lateral costophrenic angles, small pleural effusions are typically
best seen on the lateral view. Blunting of the lateral costophrenic
angle—detectable on an erect posteroanterior chest radi-
ograph—may occur with as little as 175 mL of fluid, although in
some cases as much as 525 mL will be present before blunting is
noted. Pleural effusion also may accumulate in a subpulmonary
location between the lung base and diaphragm without causing
A
B
C
Figure 7–16. ARDS secondary to pneumococcal pneumonia in a patient with a history of Hodgkin’s disease and
splenectomy several years earlier. A. Initial chest radiograph demonstrates patchy bilateral consolidation. B. Within
12 hours of admission, dense air space consolidation is present, necessitating intubation. Clinical course was consistent
with ARDS. C. Follow-up radiograph 5 weeks after admission to the ICU shows a coarse reticular pattern bilaterally.
Lung volumes are slightly decreased in comparison with the admission radiograph.
IMAGING PROCEDURES
163
blunting of the lateral costophrenic sulcus. These subpul-
monary collections simulate elevation of the diaphragm; on the
left, the distance between the gastric air bubble and the “pseu-
dodiaphragm” will be increased. The pulmonary vessels are not
seen through the basilar pulmonary parenchyma. The pseudo-
diaphragm is elevated and flattened, with the dome appearing
more lateral than normal.
Pleural effusions may extend into the fissures, with the
radiographic appearance depending on the shape and orientation
of the fissure, the location of the fluid, and the direction of the
radiographic beam. Collections of fluid in the fissures may
mimic a mass, resulting in a “pseudotumor” appearance.
Although the preceding radiographic appearances of
pleural effusion are well known and easily recognized on pos-
teroanterior and lateral chest radiographs, these projections
are infrequently obtained in the ICU patient, and recognition
of pleural effusion in the supine patient may be difficult. In
supine patients, the most dependent regions of the pleural
A
B
C
Figure 7–17. Barotrauma in ARDS. A. Chest radiograph demonstrates diffuse lung consolidation secondary to ARDS.
Parenchymal stippling is present with lucent perivascular halos secondary to pulmonary interstitial emphysema. B. On
chest radiograph 4 days later, pneumomediastinum is now identified with extensive subcutaneous emphysema. C. In
another patient with ARDS, subpleural cysts (arrow) and parenchymal stippling due to pulmonary interstitial emphy-
sema are present.
CHAPTER 7
164
space are the posterior aspects of the bases and the lung apex.
Free pleural effusions layer posteriorly, resulting in a homoge-
neous increased density of the lower involved hemithorax.
Fluid also may accumulate at the apex of the thorax, resulting
in apical capping. These findings, however, are seen frequently
only in moderate or large pleural effusions, and small effu-
sions may not be detected on supine radiographs. Although
very small accumulations of pleural effusion can be detected
on lateral decubitus views, this projection is logistically diffi-
cult to obtain in the ICU patient.
Atelectasis and lung consolidation may be difficult to dis-
tinguish from a pleural effusion because they too may result
in elevation of the hemidiaphragm and decreased visibility of
lower lobe vessels. Cross-sectional imaging using ultrasound or
CT is very helpful in detecting small amounts of pleural effu-
sion and in distinguishing complicated pleural and parenchy-
mal processes. These imaging methods are also used frequently
to guide interventional procedures, including diagnostic thora-
centesis, drainage of empyema or malignant pleural effusions,
intracavitary fibrinolytic therapy, and sclerotherapy.
Ultrasound can be performed at the bedside and can easily
detect both free pleural effusions and loculated collections
(Figure 7–19). In most situations, ultrasound is the imaging
method of choice for guiding thoracentesis and may decrease
the incidence of iatrogenic pneumothorax. The percutaneous
drainage of pleural fluid collections with small catheters
instead of large-bore thoracostomy tubes has been shown to be
effective in treating both sterile and infected effusions.
Intracavitary fibrinolytic therapy, the installation of fibrinolytic
enzymes into the pleural space, has greatly improved the effec-
tiveness of pleural fluid drainage with smaller catheters.
CT is extremely sensitive in detecting even small amounts
of free pleural effusion, demonstrating loculations, and evalu-
ating the underlying lung parenchyma. The excellent contrast
resolution of CT allows demonstrations of regions of high atten-
uation secondary to blood or proteinaceous collections and
shows calcifications that are not apparent on chest radiographs.
By virtue of the cross-sectional perspective, air-fluid levels are
easily identified. In complicated cases, intravenous contrast
administration will help to differentiate pulmonary and pleural
processes in that perfused, consolidated lung will be enhanced,
whereas pleural processes will not (see Figure 7–7). The disad-
vantages of CT are its relatively high cost and the need for trans-
porting the critically ill patient to the radiology department.
Emamian SA et al: Accuracy of the diagnosis of pleural effusion on
supine chest x-ray. Eur Radiol 1997;7:57–60. [PMID: 9000398]
Ruskin JA et al: Detection of pleural effusions on supine chest radi-
ographs. AJR 1987;148:681–3. [PMID: 3493648]
Moulton JS: Image-guided management of complicated pleural
fluid collections. Radiol Clin North Am 2000;38:345–74. [PMID:
10765394]
Qureshi NR, Gleeson FV: Imaging of pleural disease. Clin Chest
Med 2006;27:193–213. [PMID: 16716813]
Pneumothorax
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Identification of a visceral pleural line.
Absence of pulmonary vessels peripheral to visceral
pleural line.
Basilar hyperlucency in the supine patient.
Deep sulcus sign (supine patient).
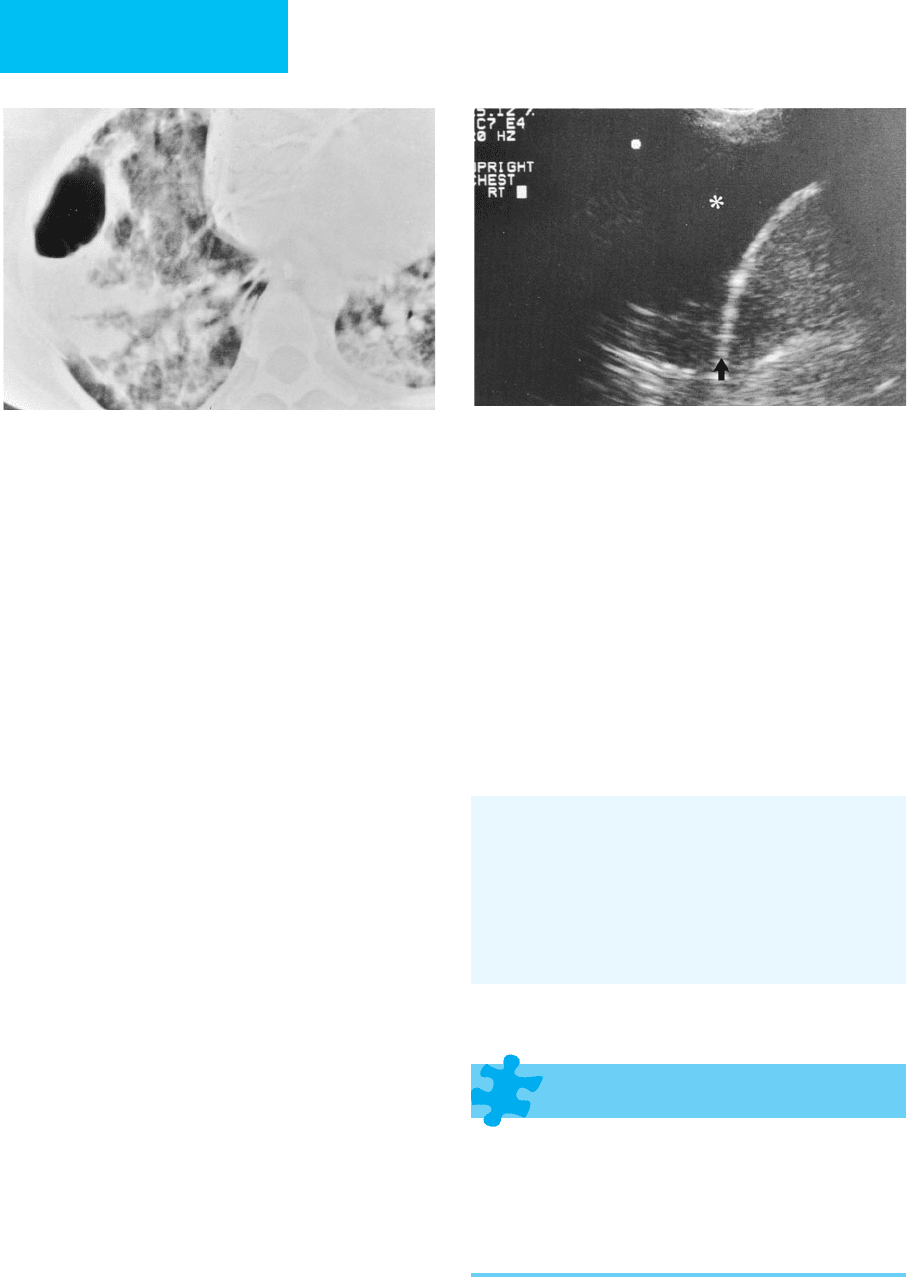
Figure 7–18. Adult respiratory distress syndrome. CT
shows heterogeneous consolidation with subpleural air
cyst secondary to barotrauma.
Figure 7–19. Pleural effusion on ultrasound. Right
pleural effusion is seen as a region of low echogenicity
(asterisk) above the hyperechoic diaphragm (arrow).
IMAGING PROCEDURES
165
General Considerations
Pneumothorax is a frequent and serious complication in
the ICU. Iatrogenic pneumothorax may develop as a
sequela of invasive diagnostic or therapeutic procedures,
including central venous catheterization, endotracheal
intubation, tracheostomy, thoracentesis, pleural biopsy,
percutaneous lung biopsy, bronchoscopy, cardiothoracic or
abdominal surgery, and interventional abdominal proce-
dures to the liver and upper abdominal viscera.
Pneumothorax also may result from blunt chest trauma or
underlying lung diseases such as COPD, asthma, cystic fibro-
sis, and interstitial lung disease. Pneumothorax can compli-
cate the course of cavitary pneumonias due to infections
with M. tuberculosis, staphylococci, Klebsiella and other
gram-negative organisms, or fungi; similarly, there is an
increased incidence of pneumothorax in patients with AIDS
who develop Pneumocystis pneumonia. Finally, in patients
receiving positive-pressure mechanical ventilation, pneu-
mothorax may result from pulmonary interstitial emphy-
sema due to barotrauma.
In a recent study of pneumothorax in ICU patients, 35 of 60
patients (58%) who developed a pneumothorax during the
study period had procedure-related pneumothoraces. Patients
with pneumothoraces due to barotrauma or who had concur-
rent septic shock or a tension pneumothorax had a higher risk of
mortality than patients with postprocedural pneumothoraces.
Radiographic Features
A. Simple Pneumothorax—As with fluid in the pleural
space, the distribution of a pneumothorax is influenced by
gravity, lung elastic recoil, potential adhesions in the pleural
space, and the anatomy of the pleural recesses. In the upright
patient, air accumulates in the nondependent region of the
pleural space, the apex. Radiographically, a pneumothorax is
identified by separation of the visceral pleural surface from the
chest wall and the absence of pulmonary vessels peripheral
to the pleural line. A pneumothorax typically is better seen
on expiratory images because of a relative decrease in lung
volumes compared with the air in the pleural space.
Imaging in the supine position alters the radiographic
appearance of pneumothorax. In this position, the least
dependent regions of the pleural space are the anteromedial
and subpulmonary regions. Pleural air in the anteromedial
space results in sharp delineation of mediastinal contours,
including the superior vena cava, the azygos vein, the heart
border, the inferior vena cava, and the left subclavian artery.
The accumulation of air in the subpulmonary region is seen as
a hyperlucent upper quadrant of the abdomen; a deep, hyper-
lucent lateral costophrenic sulcus (“deep sulcus sign”); sharp
delineation of the ipsilateral diaphragm; and visualization of
the inferior surface of the lung (Figure 7–20). Air can accumu-
late in the apicolateral pleural space in the supine patient just
as in the erect patient, especially when a large pneumothorax
is present. In the presence of lower lobe collapse, air can
accumulate in the posteromedial pleural recess. This results in
a sharp delineation of the posterior mediastinal structures,
including the descending aorta and the costovertebral sulcus.
Subtle pneumothoraces may require other projections for
detection, such as decubitus or cross-table lateral views. CT
is an excellent method for diagnosing a pneumothorax not
demonstrated on plain chest radiographs.
Several conditions may be confused with a pneumothorax.
Pneumoperitoneum may result in a hyperlucent upper
abdomen, mimicking pneumothorax. Skin folds can be con-
fused with apicolateral pneumothorax but should be recog-
nized when they extend outside the bony thorax or are traced
bilaterally. Pneumomediastinum may simulate medial pneu-
mothorax, but pneumomediastinum may cross the midline
and extend into the retroperitoneum.
B. Tension Pneumothorax—Recognition of even small
pneumothoraces is crucial to prevention of progressive accu-
mulation of pleural air collections, particularly in patients
being maintained on mechanical ventilation. Tension pneu-
mothorax occurs when the pressure of air in the pleural space
exceeds ambient pressure during the respiratory cycle. With
this pressure gradient, air enters the pleural space on inspi-
ration but is prevented from exiting the pleural space during
expiration due to a check-valve mechanism. A tension
Figure 7–20. Pneumothorax in a supine patient with
ARDS. Chest radiograph demonstrates a large right pneu-
mothorax with intrapleural air adjacent to the diaphragm
and evidence of a deep sulcus (arrow). The margin of the
right hemidiaphragm is obliterated by adjacent adhesions.
CHAPTER 7
166
pneumothorax may result in acute respiratory distress and, if
untreated, cardiopulmonary arrest and death. The diagnosis
of tension pneumothorax is made clinically, reflecting the
hemodynamic sequelae of impaired venous return to the
right side of the heart. Radiographic signs include displace-
ment of the mediastinum toward the contralateral thorax,
inferior displacement or inversion of the diaphragm, and
total lung collapse (Figure 7–21). However, significant hemo-
dynamic compromise can exist in the absence of these find-
ings. Adhesions may prevent mediastinal shift, and lung
collapse may not occur in patients with stiff lungs such as
those with ARDS. A small pneumothorax may convert to a
tension pneumothorax, particularly in patients receiving
mechanical ventilatory support. In patients with ARDS,
poorly compliant lungs and pleural adhesions may result in
difficulty identifying a pneumothorax on portable chest
radiographs, and CT may be particularly useful in the diag-
nosis of loculated pneumothorax and in guiding appropriate
chest tube placement.
Chen KY et al: Pneumothorax in the ICU: Patient outcomes and
prognostic factors. Chest 2002;122:678–83. [PMID: 12171850]
Kong A: The deep sulcus sign. Radiology 2003;228:415–6. [PMID:
12893899]
Moss HA, Roe PG, Flower CDR: Clinical deterioration in ARDS:
An unchanged chest radiograph and functioning chest drains
do not exclude an acute tension pneumothorax. Clin Radiol
2000;55:637–51. [PMID: 10964737]
Rankine JJ, Thomas AN, Fluechter D: Diagnosis of pneumothorax
in critically ill adults. Postgrad Med J 2000;76:399–404. [PMID:
10878196]
Woodside KJ et al: Pneumothorax in patients with acute respira-
tory distress syndrome: Pathophysiology, detection, and treat-
ment. J Intensive Care Med 2003;18:9–20. [PMID: 15189663]
Pulmonary Interstitial Emphysema
& Pneumomediastinum
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Pulmonary interstitial emphysema: Perivascular “halo”
(air surrounding pulmonary vessels seen on end), linear
radiolucencies radiating toward the hila, irregular radi-
olucent mottling, parenchymal cysts, or collections of
air along visceral pleural surface.
Pneumomediastinum: Linear lucencies adjacent to the
heart and aortic arch, descending aorta, and great ves-
sels. May have subcutaneous emphysema with linear
radiolucencies extending along tissue planes in the
chest wall and neck.
General Considerations
Barotrauma is a serious and frequent complication in the
ICU patient. Defined as damage secondary to the presence
of extraalveolar or extraluminal air, the incidence is highest
in patients being supported by mechanical ventilation.
Alveolar overdistention and an increased intraalveolar pres-
sure gradient from alveolus to vascular sheath allow rupture
of air into the interstitial space along the perivascular
sheaths, resulting in pulmonary interstitial emphysema.
Reduction in the caliber of pulmonary vessels—as well as
general and local alveolar overinflation—contributes to the
pressure gradient, causing alveolar rupture. Although com-
monly associated with mechanical ventilation, barotrauma
may also result from coughing, straining, trauma, pneumo-
nia, a Valsalva maneuver, anesthesia or resuscitation, partu-
rition, positive-pressure breathing, and asthma. Other
manifestations of barotraumas develop because air from
ruptured alveoli follows the path of least resistance. Air dis-
sects centrally to cause pneumomediastinum and dissects
via the cervical fascial planes, resulting in subcutaneous
emphysema in the neck and chest wall. Air also can dissect
from the mediastinum into the abdomen, leading to
retroperitoneal air and pneumoperitoneum or into the
pleural space resulting in a pneumothorax.
Barotrauma has a high incidence in patients with ARDS. In
one study of 15 patients with ARDS—all requiring positive-
pressure ventilation—radiographic evidence of pulmonary inter-
stitial emphysema was found in 87%. Although there was no
correlation with positive end-expiratory pressure or mean airway
Figure 7–21. Spontaneous tension pneumothorax. The
left lung is completely collapsed, with visualization of a vis-
ceral pleural line and hyperlucency of the thorax. The medi-
astinum is shifted to the right, and there is depression of the
left hemidiaphragm consistent with tension pneumothorax.
