Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

IMAGING PROCEDURES
177
General Considerations
Toxic megacolon is a complication of many different types of
ischemic, inflammatory, or infectious conditions of the colon
but is most closely associated with ulcerative colitis. Patients
are usually in extremis, complaining of fever and bloody diar-
rhea. Tachycardia and abdominal pain may be present.
Clinical features are accompanied by thickened colonic haus-
tra on plain radiographs. Due to the transmural nature of the
inflammation, the neuromuscular and neurohumoral tone of
the colon is disrupted. Without treatment, the mortality rate
is nearly 20%.
Radiographic Features
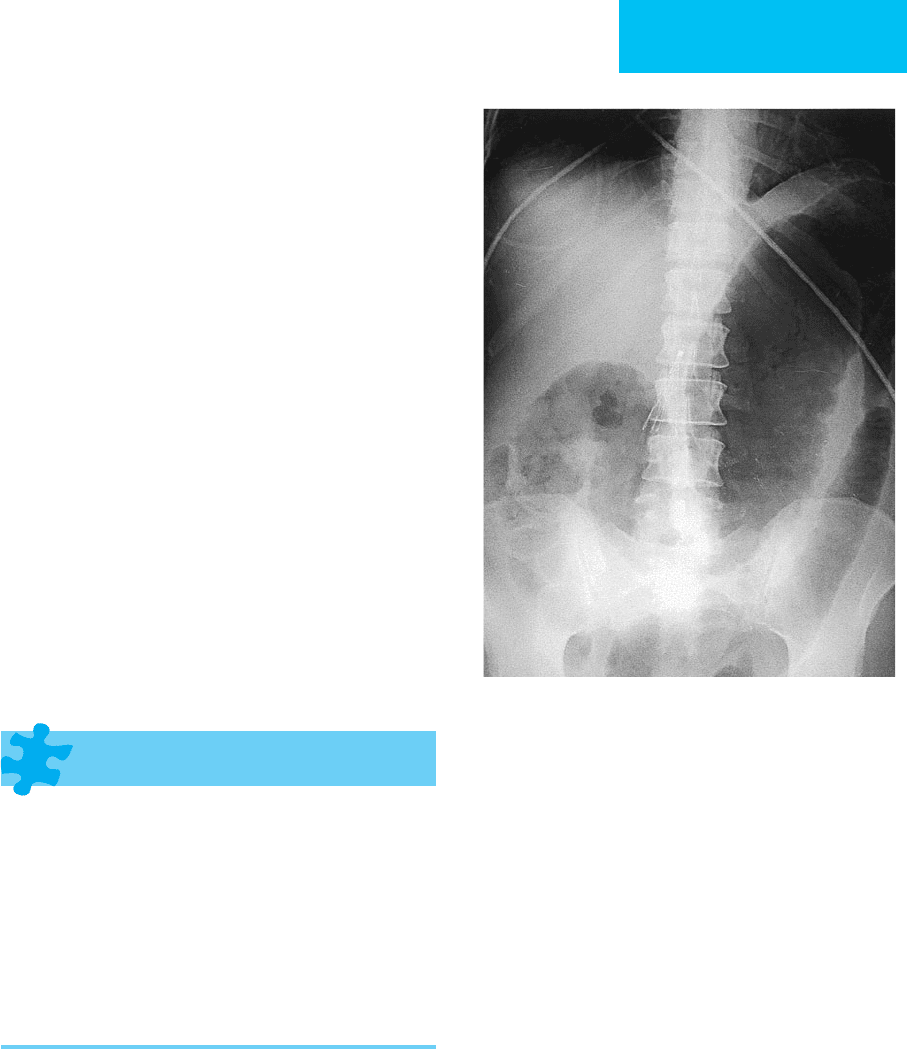
Generally, plain radiographs will reveal varying degrees of
colonic dilation (generally >6.5 cm) with or without associated
fold thickening. Thickened or effaced haustra are present, with
edematous or inflamed folds, and there is a paucity of feces. An
enema is contraindicated if toxic megacolon is suspected
(Figure 7–30). These features are more clearly seen on abdom-
inal CT imaging, and complications such as perforation and
gas within the colonic wall are easier to detect. The pericolonic
fat is usually infiltrated, and both colon and fat are sometimes
hyperemic.
Intraabdominal Abscess
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Plain film: Usually invisible except when abscess is gas-
filled or produces a mass effect.
Ultrasound: Well-circumscribed collection of variably
echogenic fluid.
Abdominal CT: Well-circumscribed fluid-filled mass,
which may contain gas. Wall is of variable thickness and
enhancement.
Radionuclide scintigraphy: Radionuclide-tagged white
blood cell scan may be useful in search of occult abscess
or other sources of infection.
General Considerations
Over the past 25 years, imaging has revolutionized the diag-
nosis and management of abdominal and pelvic abscesses,
often precluding the need for laparotomy and for incision
and drainage in the vast majority of patients.
Intraabdominal abscesses typically are caused by perfo-
rated appendicitis in the young and diverticulitis in the
elderly. Overall, most cases are iatrogenic, occurring after
intraabdominal surgery. Hematogenous seeding of bacteria
may be responsible for liver and, especially, splenic abscesses.
The mortality remains high, ranging from 80% to 100% with-
out treatment and up to 30% in patients receiving appropri-
ate therapy.
Radiographic Features
A. Plain Radiographs—These may be helpful in evaluating
the gastrointestinal tract but are not generally able to localize
an abscess. On occasion, the abscess will appear as a gasless
fluid collection mimicking a mass with defined radiodense
contours that displaces bowel or bladder.
B. Ultrasound—Ultrasound is an excellent means for bed-
side evaluation of defined areas such as the upper quadrants,
Figure 7–30. Toxic megacolon. Plain radiograph demon-
strates diffuse dilation and severe thickening of mucosal folds
(thumbprinting) of the colon. There is no stool. The patient
was in extremis with a severe flare of ulcerative colitis.
CHAPTER 7
178
the paracolic gutters, and the pelvis. Features that suggest
an infected fluid accumulation on sonography include
rounded or ovoid collections with thick walls, with variable
internal echoes and without evidence of central vascularity,
as demonstrated by color, power, or spectral Doppler sig-
nals. Focal bright echoes with variable shadowing within
collections may suggest the presence of gas. However, these
signs are not specific for infected fluid; a hematoma or
seroma may appear identical. On the other hand, nonin-
fected collections generally have angular margins, conform
to anatomic spaces, and tend to lack significant internal
echogenicity.
Ultrasound is especially valuable for evaluating the sub-
diaphragmatic regions or the low pelvis. However, one
should bear in mind its limitations. Ultrasound will not
reliably evaluate the retroperitoneum and retroperitoneal
organs such as the pancreatic body and tail. Evaluation of
complex collections in postoperative patients or in patients
with open abdominal incisions or surgical dressings is likely
to be suboptimal. Imaging of abscesses within organs may
be difficult.
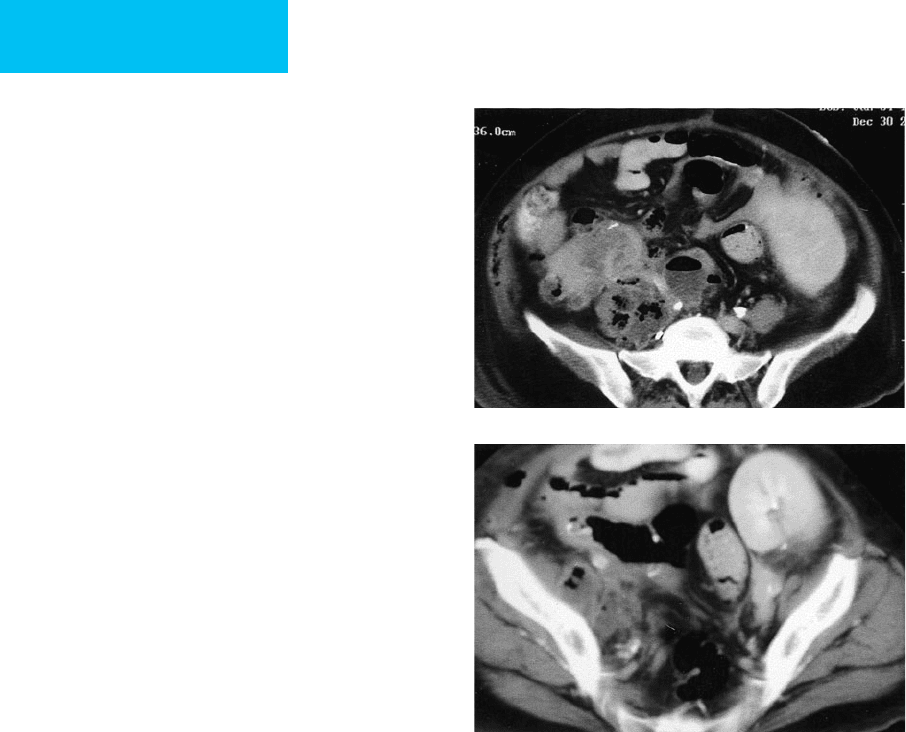
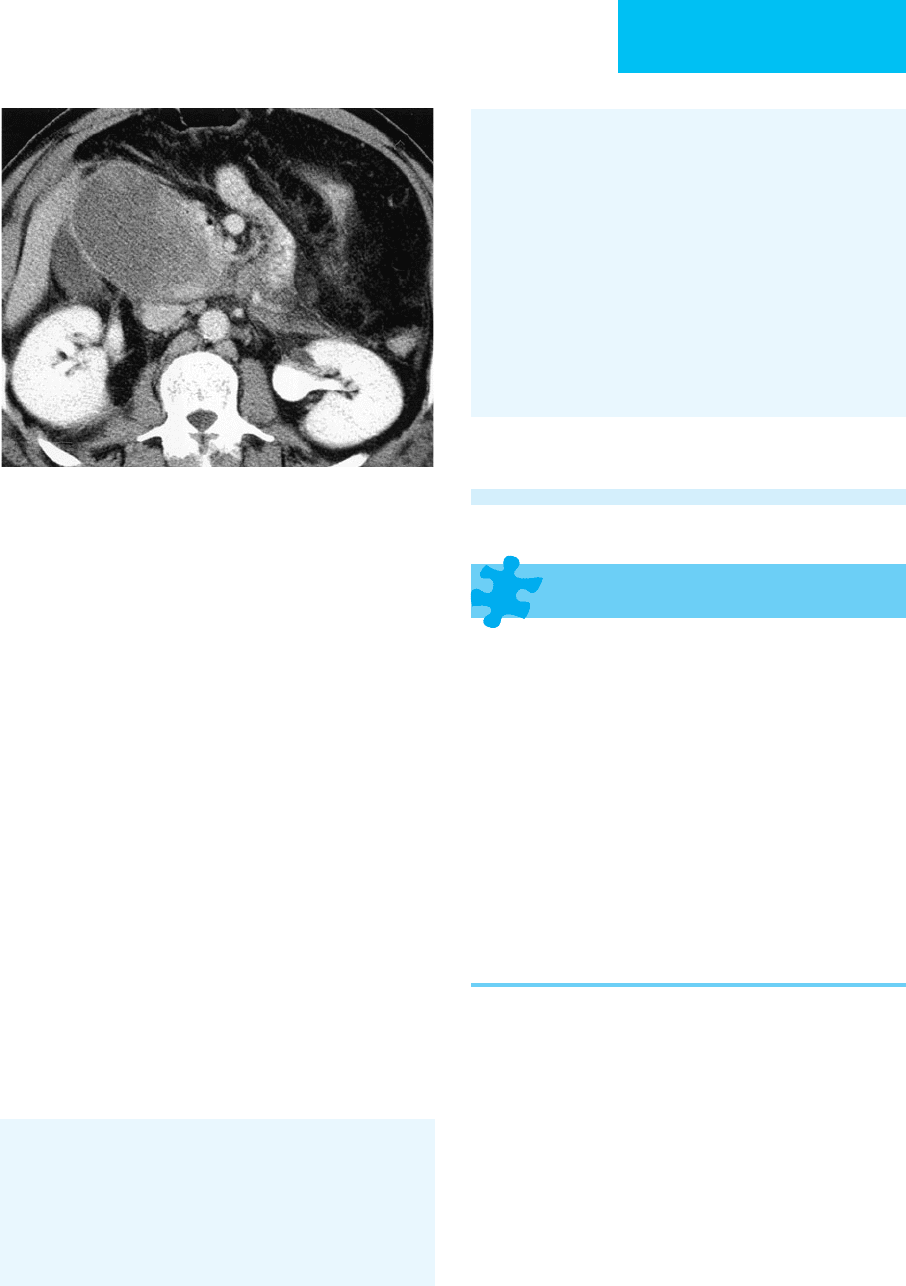
C. Computed Tomography—CT is the method of
choice for evaluation of an intraabdominal abscess
(Figure 7–31). Although preparation with oral and IV
contrast agents is preferred for optimal diagnosis in most
patients, contrast material is not always required when
using the latest-generation equipment. This is especially
true in obese patients because of inherent contrast pro-
vided by intraabdominal fat. Actual scanning time with a
multidetector helical scanner is typically on the order of
20–40 seconds.
Abscesses generally appear as round or ovoid collections
with thick surrounding rims. Intraluminal gas due to
anaerobic bacterial infection may be present in up to 50%
of collections. If IV contrast material is given, enhancement
of the surrounding rim may be noted in up to 50% of
abscesses. Abscesses under the diaphragm and surrounding
the liver or kidney may have crescentic margins. However,
in many cases, the CT signs of an abscess are nonspecific.
Necrotic tumors may have an identical appearance, and
percutaneous aspiration may be required to distinguish
between them.
D. Radionuclide Scintigraphy—Although unnecessary in
the vast majority of patients, nuclear medicine studies with
indium (
111
In)–labeled or gallium citrate (
67
Ga)–labeled
white blood cells are useful for the detection of occult
abscesses, especially in patients with fever of unknown origin.
Both indium oxine–labeled and gallium citrate–labeled cells
are injected intravenously, and scans are typically obtained
48–72 hours later. Although gallium is highly sensitive for
the detection of intraabdominal abscess (80–90%), speci-
ficity is limited by intestinal secretion at 48–72 hours.
Overall, indium-labeled white blood cell scans are more
accurate for abdominal applications.
E. Algorithm for Imaging the Patient with Suspected
Abdominal Abscess—In patients without localizing signs
or symptoms and varying degrees of suspicion of abdominal
abscess, the test of choice is helical or multidetector CT with
IV and oral contrast. This study helps to exclude potential
peritoneal and retroperitoneal sources of infection. CT is
necessary for adequate visualization of the pancreas, psoas
muscles, other retroperitoneal structures and complex col-
lections. CT is superior to other imaging methods in patients
A
B
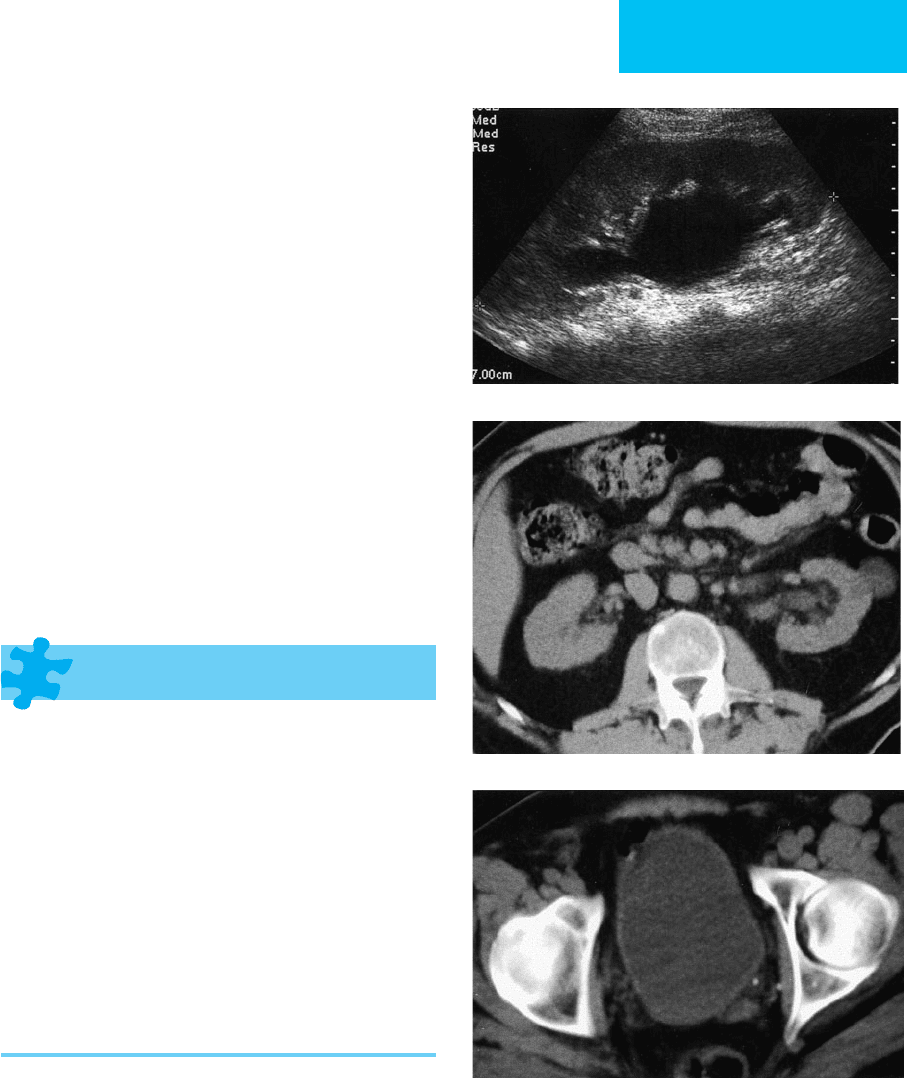
Figure 7–31. Psoas abscess. Young woman with pain
and fever 1 month after renal and pancreas transplanta-
tion. A. CT demonstrates a multiloculated right psoas
abscess with air and gas tracking into the right psoas
sheath. B. Air in the right abdominal wall is from a
recent biopsy.
IMAGING PROCEDURES
179
with ileus, open incisions, dressings, indwelling catheters,
and drains. If symptoms are localized to the upper abdomi-
nal quadrants or to the pelvis, ultrasound is an excellent
choice for diagnosis and can be performed quickly at the
bedside. Furthermore, bedside percutaneous incision and
drainage may be performed with sonographic guidance.
Scintigraphy has a limited role in diagnosing abscess in an
acutely ill patient.
F. Percutaneous Image-Guided Drainage—Percutaneous
drainage has revolutionized the management of infected
fluid collections. Expanded criteria render only a small
minority of collections unsuitable for such drainage.
General criteria include a fluid collection at least 2–3 cm in
diameter and safe access to the collection without inter-
vening blood vessels, pleura, bladder, or bowel. One should
confirm with CT or sonographic Doppler that the collec-
tion in question is not a pseudoaneurysm. Fluid collections
may be multiloculated or communicate with the gastroin-
testinal, biliary, or genitourinary tracts. Solid organ and
tubo-ovarian abscesses may be drained safely, although the
latter frequently respond to antibiotics and needle aspira-
tion alone.
A number of catheter types and sizes are available.
Noninfected serous collections usually can be drained with
6–8F catheters, whereas infected, thick purulent collections
may be drained with 10–14F catheters. Multiple catheters or
larger catheters (16–18F) occasionally may be needed for
multiloculated noncommunicating thick-walled collections.
Guidance for drainage procedures includes ultrasound, fluo-
roscopy, or CT. Ultrasound is especially versatile because cav-
itary probes (endovaginal or endorectal) can help diagnose
deep pelvic abscesses and guide transrectal or transvaginal
drainage. Catheters should be left to gravity drainage and
flushed gently with 5 mL of normal saline at 8-hour intervals
to ensure patency. Drainage output should be recorded on
the nursing flow sheet.
Catheter position may be confirmed by fluoroscopic
injection of contrast material or by ultrasound or CT.
General criteria for catheter removal include resolution of
symptoms and signs, decrease in net catheter output to
under 10 mL/day, and closure of the cavity as determined by
follow-up imaging studies.
Gerzof SG et al: Percutaneous catheter drainage of abdominal
abscesses: A five year experience. N Engl J Med 1981;305:653–7.
[PMID: 7266601]
Gerzof SG et al: Expanded criteria for percutaneous abscess
drainage. Arch Surg 1985;120:227–32. [PMID: 3977590]
VanSonnenberg E et al: Percutaneous abscess drainage: Update.
World J Surg 2001;25:362. [PMID: 11343195]
Yu SC et al: Treatment of pyogenic liver abscess: Prospective, ran-
domized comparison of catheter drainage and needle aspira-
tion. Hepatology 2004;39:932–8. [PMID: 15057896]
Acute Pancreatitis
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Plain radiographs: Gallstones, ileus of regional bowel (sen-
tinel loop), transverse colon ileus (colon cutoff), pancreatic
calcifications (chronic pancreatitis), and pleural effusion.
Ultrasound: Peripancreatic fluid, enlarged pancreas with
variable echogenicity, localized fluid collections,
cholelithiasis, choledocholithiasis, biliary tract obstruction.
Helical CT: Pancreatic enlargement, necrosis, or hemor-
rhage; thoracic and intraabdominal fluid or fluid collec-
tions; cholelithiasis; choledocholithiasis.
General Considerations
Imaging studies in acute pancreatitis help to confirm the
diagnosis, suggest possible causes (eg, choledocholithiasis or
pancreas divisum), detect features suggesting chronicity, and
demonstrate the extent of complications, such as abscess,
pseudocyst, hemorrhage, and necrosis. Imaging findings may
add to prognostic information derived from clinical and
serum laboratory parameters.
Acute pancreatitis is caused mainly by alcohol abuse or
choledocholithiasis. In the ICU, iatrogenic causes such as
postoperative state, medications (eg, antiretrovirals,
chemotherapeutic agents), or endoscopic retrograde cholan-
giopancreatography may cause acute pancreatitis. Other
causes include trauma, hypercalcemia, hypertriglyceridemia,
peptic ulcer disease, and structural congenital anomalies.
By imaging criteria, acute pancreatitis may be subdivided
broadly into acute interstitial (edematous) pancreatitis and
acute necrotizing or hemorrhagic pancreatitis. While acute
interstitial pancreatitis is usually self-limited and requires
supportive care, acute necrotizing pancreatitis is difficult to
manage and carries a significant risk of high morbidity and
mortality. In up to 60% of patients, peripancreatic and pan-
creatic fluid collections are present. Pseudocysts, which are
collections of pancreatic juice and debris, are lined by a
fibrous capsule and by definition have been present for at
least 4 weeks. In the acute phase, the behavior of a phlegmon
or nonliquified inflammatory pancreatic tissue is difficult to
predict, although most resolve. If a pancreatic abscess is
detected, prompt percutaneous or surgical debridement must
be performed because it is associated with a high mortality.
Radiographic Features
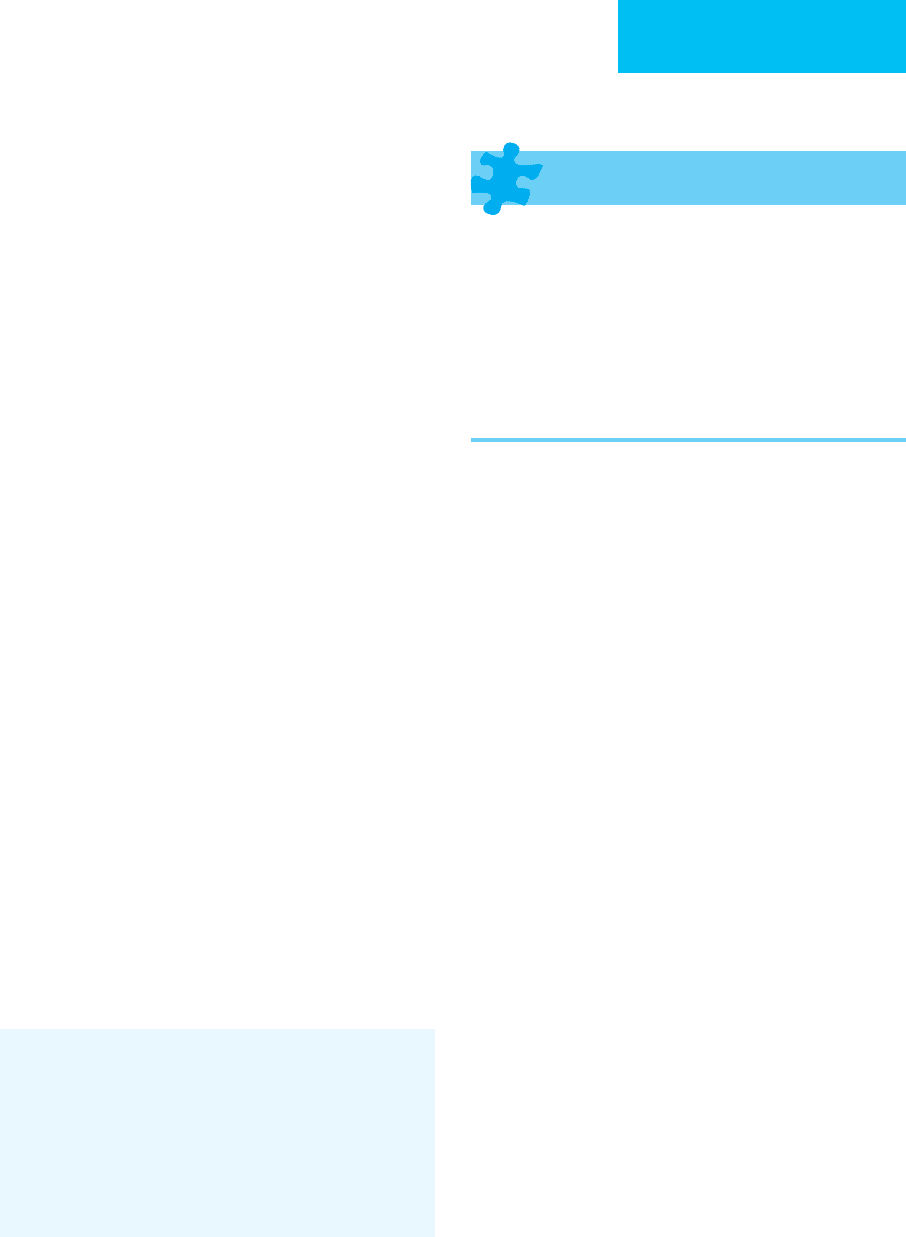
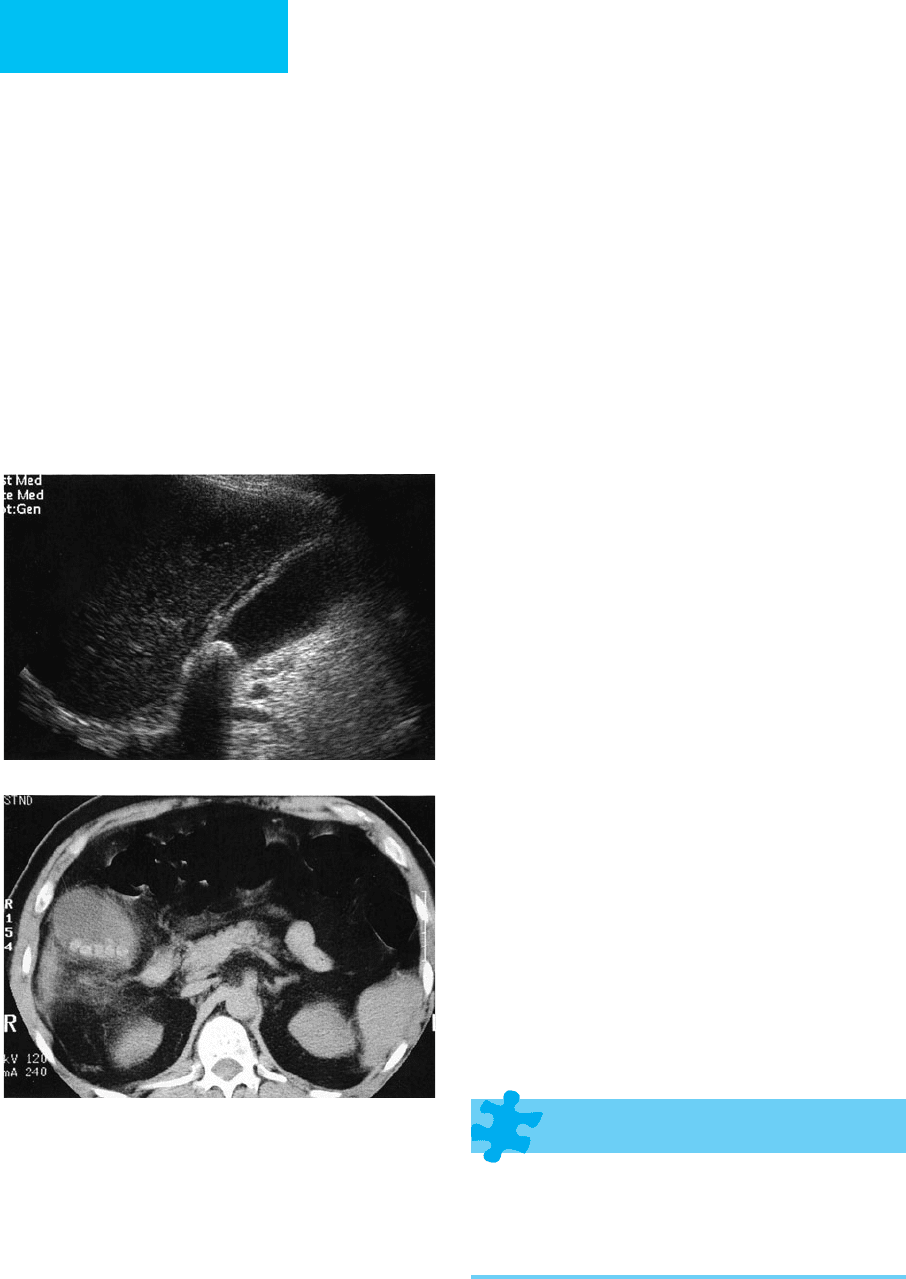
A. Plain Abdominal Radiographs—Several indirect signs in a
patient with acute back or epigastric pain suggest acute
pancreatitis (Figure 7–32). However, none of the following are
CHAPTER 7
180
specific for pancreatitis: (1) duodenal ileus—gas in the second
portion of the duodenum—reported in up to 50% of patients,
(2) jejunal ileus—focal gaseous distention of a jejunal loop
(“sentinel-loop sign”), (3) transverse colon ileus—gaseous dis-
tention of the transverse colon with a paucity of gas in the
descending colon—compatible with the “colon cutoff sign,” and
(4) left-sided pleural effusion, reported in 10–15% of patients.
B. Fluoroscopic Contrast Studies—Upper gastrointestinal
studies may be indicated to look for peptic ulcer disease.
Although they are not indicated for the diagnosis of acute
pancreatitis, one sometimes may observe a widening of the C-
loop with thickening of the duodenal folds due to edema.
C. Ultrasound—An ultrasound examination may be neces-
sary to confirm or exclude the presence of gallstones within
the gallbladder or common duct. Sonographic imaging of
the pancreas may reveal diffuse edema.
D. Abdominal CT—Current CT techniques allow detailed
pancreatic imaging tailored to the particular clinical situation.
In the setting of acute pancreatitis, a single or multidetector
helical CT may be performed, imaging the pancreas with a
minimum of 3-mm collimation with IV contrast enhance-
ment in the “pancreatic phase,” approximately 40 seconds
after bolus contrast material injection in patients with normal
cardiac output. In addition to highly detailed pancreatic
images, the remainder of the abdomen and pelvis should be
imaged to exclude distant complications, including fluid col-
lections and phlebitis. CT is the single best imaging method
for pancreatic evaluation because it provides excellent evalua-
tion and the ability to treat complications percutaneously.
Uncomplicated acute pancreatitis has an extremely vari-
able presentation. The pancreas may be normal or edema-
tous, increasing the attenuation of the intrapancreatic fat. The
peripancreatic fat planes may become infiltrated by edema
and products of the nonspecific inflammatory response. In
patients with severe pancreatitis, sections of the gland
undergo necrosis and may become hemorrhagic or infected.
On CT, lack of diffuse and homogeneous pancreatic enhance-
ment with IV contrast material reflects poor parenchymal
perfusion and is typical of necrotizing pancreatitis. In areas of
necrosis, the pancreas becomes ill-defined, with a severe peri-
pancreatic inflammatory response and local and distant free
and contained fluid. Splenic vein thrombosis may be present,
and other complications such as pseudoaneurysm formation
and pseudocyst formation may be seen at local and distant
sites (Figure 7–33). A proposed CT grading system is used in
some centers to estimate the amount of pancreatic injury and
to predict outcome. Hemorrhagic complications are well seen
because recent hemorrhage (<1 week) is usually of high
attenuation compared with surrounding tissue. Over time as
the hematoma ages, its attenuation gradually decreases.
A pancreatic abscess, which may complicate acute pancre-
atitis in up to 9% of patients, implies a poor prognosis, with
reported mortality rates of 40–70% in the pre-CT era. Prompt
CT diagnosis and treatment have reduced the mortality rate to
20%. CT appearance of a pancreatic abscess can be variable
and can range from a contained fluid collection to a more typ-
ical rim-enhancing lesion with central low attenuation and gas
collection. The latter findings are present in only 20–30% of all
pancreatic abscesses, and percutaneous aspiration is usually
necessary for confirmation. The presence of gas bubbles also
may suggest a fistulous communication with bowel.
Figure 7–32. Acute pancreatitis. A. Plain film demon-
strates focal dilated “sentinel loops” resulting from localized
ileus. B. Abdominal CT in the same patient shows peripan-
creatic stranding and a fatty liver from recent ethanol abuse.
A
B
IMAGING PROCEDURES
181
Treatment
Acute pancreatitis complicated by necrosis or infection often
can be treated successfully by aggressive percutaneous catheter
drainage with large-bore catheters. In more complex or severe
cases, percutaneous management may help to temporize a
critically ill patient until surgical debridement is possible.
The management of pseudocysts is complex. Generally,
pseudocysts may be managed expectantly because most will
regress over time. By definition, a true pseudocyst has a
mature fibrous wall developed over at least 4 weeks.
Indications for percutaneous drainage or internal drainage
into the stomach are the following: infection; enlargement;
pain; bowel, bile, or urinary obstruction; and diameter greater
than 5 cm. For noninfected pseudocysts, success rates for
internal or external drainage are high. For the 20–30% of
pseudocysts communicating with the pancreatic duct, external
drainage will be difficult, and a cyst gastrostomy performed
percutaneously, surgically, or laparoscopically may be better.
Superinfection of a previously sterile pseudocyst occurs
in less than 5% of cases. As with most fluid collections, iden-
tification of infection within a pseudocyst requires clinical
suspicion and confirmation by percutaneous aspiration.
Successful drainage of an infected pseudocyst uses the same
principles of drain placement and management as for most
intraabdominal abscesses.
Arvanitakis M et al: Computed tomography and magnetic reso-
nance imaging in the assessment of acute pancreatitis.
Gastroenterology 2004;126:715–23. [PMID: 14988825]
Balthazar EJ: Acute pancreatitis: Assessment of severity with clinical
and CT evaluation. Radiology 2002;223:603–13. [PMID: 12034923]
Casas JD et al: Prognostic value of CT in the early assessment of
patients with acute pancreatitis. AJR 2004;182:569–74. [PMID:
14975947]
Kwon RS, Scheiman JM: New advances in pancreatic imaging.
Curr Opin Gastroenterol 2006;22:512–9. [PMID: 16891882]
Memis A, Parildar M: Interventional radiological treatment in
complications of pancreatitis. Eur J Radiol 2002;43:219–28.
[PMID: 12204404]
Maher MM et al: Acute pancreatitis: The role of imaging and inter-
ventional radiology. Cardiovasc Intervent Radiol 2004;27:208–25.
[PMID: 15024494]
Miller FH et al: MRI of pancreatitis and its complications: 1. Acute
pancreatitis. AJR 2004;183:1637–44. [PMID: 15547203]
Nichols MT et al: Pancreatic imaging: Current and emerging tech-
nologies. Pancreas 2006;33:211–20. [PMID: 17003640]
Shankar S et al: Imaging and percutaneous management of acute
complicated pancreatitis. Cardiovasc Intervent Radiol
2004;27:567–80. [PMID: 15578132]
IMAGING OF ACUTE GALLBLADDER & BILIARY
TRACT DISORDERS
Acute Calculous Cholecystitis
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Plain films: 15–20% of gallstones are radiopaque; dis-
tended gallbladder may be present in the right abdomen
and produce a rounded radiodensity; gas may be present
in the lumen or wall in emphysematous cholecystitis.
Ultrasound: Thickening of gallbladder wall (>3 mm),
intraluminal gallstones and sludge, pericholecystic
fluid and focal tenderness over gallbladder (sono-
graphic Murphy’s sign).
CT: Nearly 100% of gallstones visualized. Distended
gallbladder with thickened wall, rim enhancement,
pericholecystic fat stranding, gas in lumen or wall in
emphysematous cholecystitis.
Hepatobiliary scintigraphy: Uptake of iminodiacetic acid
analogues into liver but nonvisualization of gallbladder
within 60 minutes of injection.
General Considerations
In acute calculous cholecystitis, cystic duct obstruction
results from a lodged gallstone in almost 95% of cases. The
gallbladder distends, with resulting mucosal inflammation
and edema from bile stasis. Both distention and mural edema
may lead to venous obstruction and subsequent mural
ischemia and possible perforation.
Clinical parameters are of limited utility in the critical
care setting. There is a significant clinical overlap among a
variety of conditions, such as acute pancreatitis, perforated
peptic ulcer, pyelonephritis, and thoracic abnormalities such
as pneumonia and myocardial infarction.
Figure 7–33. Complicated pancreatitis. CT demon-
strates a large pseudocyst in the head of the pancreas.
CHAPTER 7
182
Radiographic Features
A. Plain Abdominal Radiographs—Plain radiographs can
detect the 15% of gallstones that are radiopaque. In emphy-
sematous cholecystitis, typically seen in diabetics, gas within
the gallbladder wall and lumen may be seen. Plain films also
may be useful to distinguish other causes of right upper
quadrant pain, such as a perforated viscus or pneumonia.
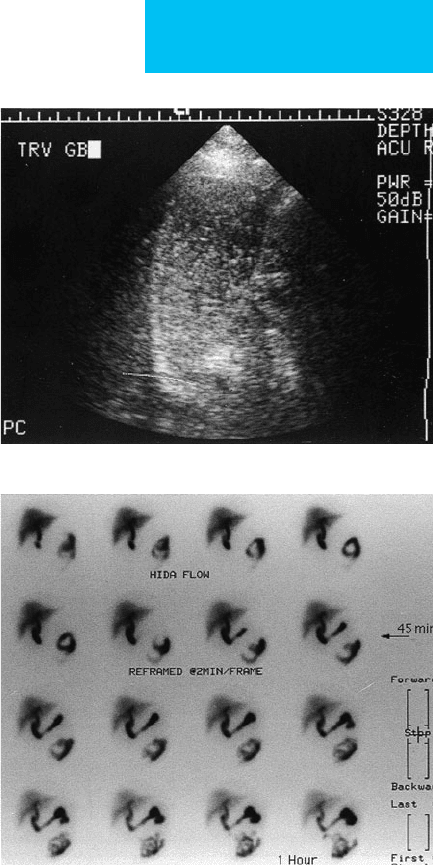
B. Ultrasound—Ultrasound should be the test of choice for
rapid diagnosis of acute cholecystitis at the bedside. Features
highly suggestive of acute calculous cholecystitis include a
thick-walled, distended gallbladder with gallstones, perichole-
cystic fluid, and focal tenderness overlying the gallbladder
(sonographic Murphy’s sign)(Figure 7–34). However, in
patients who have been in the ICU for a few days or longer,
the gallbladder tends to look abnormal on sonography, usu-
ally having a thickened wall and internal echoes. In these
patients, a reliable sonographic Murphy’s sign should be
absent. Sonography also may be limited by body habitus,
overlying bowel gas, gangrenous cholecystitis, or overlying
dressings. Pericholecystic fluid is an unreliable sign in patients
with ascites. Gallbladder wall thickening alone in the absence
of other findings may have many causes, including acute hep-
atitis, HIV cholangiopathy, IL-2 therapy, and anasarca.
C. Scintigraphy—In patients with equivocal signs and
sonography, scintigraphy may provide complementary infor-
mation in acute calculous cholecystitis. Technetium (
99m
Tc)
iminodiacetic acid–derived agents have been shown to have
high sensitivity and specificity for the diagnosis of acute
cholecystitis. These agents are injected intravenously, and
sequential imaging is performed over the liver with a SPECT
camera. Sequential liver uptake and excretion into the biliary
tree and intestine are imaged for up to 1 hour after injection.
Normally, the gallbladder should fill with the radiotracer
within 1 hour. Lack of filling confirms the diagnosis of acute
calculous cholecystitis. However, lack of filling is also seen
with intrinsic gallbladder dysfunction.
Although scintigraphy is an excellent test, it is cumber-
some to perform at the bedside in the ICU compared with
sonography. An accurate test requires that the patient fast
for at least 2–4 hours prior to the procedure, and delayed
images up to 4 hours may be needed. Scintigraphy has high
negative predictive value; filling of the gallbladder within
1 hour excludes the diagnosis of acute calculous cholecystitis.
However, many causes can prevent radiotracer flow into the
cystic duct, and false-positive examinations have been
reported in up to 40% of severely ill or debilitated patients.
The most common causes of false-positive tests are bile sta-
sis, bile hyperviscosity, and gallbladder distention. Specific
causes include chronic cholecystitis, hyperalimentation,
severe jaundice, hepatic dysfunction, pancreatitis, prolonged
fasting, and recent nonfasting state. Causes of false-negative
tests include pancreatitis and poor hepatic function.
Hepatobiliary scintigraphic agents also may be used to con-
firm complications such as total common duct obstruction
or bile leak.
Acalculous Cholecystitis
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Ultrasound: Gallbladder wall is thickened; no intralumi-
nal stones; sonographic Murphy’s sign usually present.
CT: Mural thickening and inflammatory infiltration of
the pericholecystic fat.
A
B
Figure 7–34. Acute cholecystitis. A. Ultrasound demon-
strates a stone at the gallbladder neck with thickening of
the gallbladder wall, pericholecystic fluid, and tenderness
on compression (sonographic Murphy’s sign). In combination,
these features are highly specific for acute cholecystitis. B. In
another patient, abdominal CT shows distended gallbladder
with gallstones and surrounding infiltration of the fat.
IMAGING PROCEDURES
183
General Considerations
Acalculous cholecystitis is associated with a variety of clinical
conditions, including chronic debilitation, prolonged intuba-
tion, nasogastric suction and hyperalimentation, burns, and
pancreatitis. Although comprising 10–15% of all cases of chole-
cystitis, acalculous cholecystitis predominates in the postopera-
tive and posttraumatic patient population, accounting for up to
90% of all cholecystitis cases seen in that group. Mechanisms are
poorly understood and probably multifactorial. Bile stasis, bile
hyperconcentration, and edema with pressure in the gallbladder
wall leading to progressive ischemia have been linked to the
pathogenesis of this disorder. In addition, reflux of pancreatic
juices through biliary enteric anastomoses and pancreatitis have
been suggested. The clinical presentation of acalculous chole-
cystitis is similar to that of calculous cholecystitis. However, typ-
ical symptoms may be masked by concomitant problems.
Radiographic Features
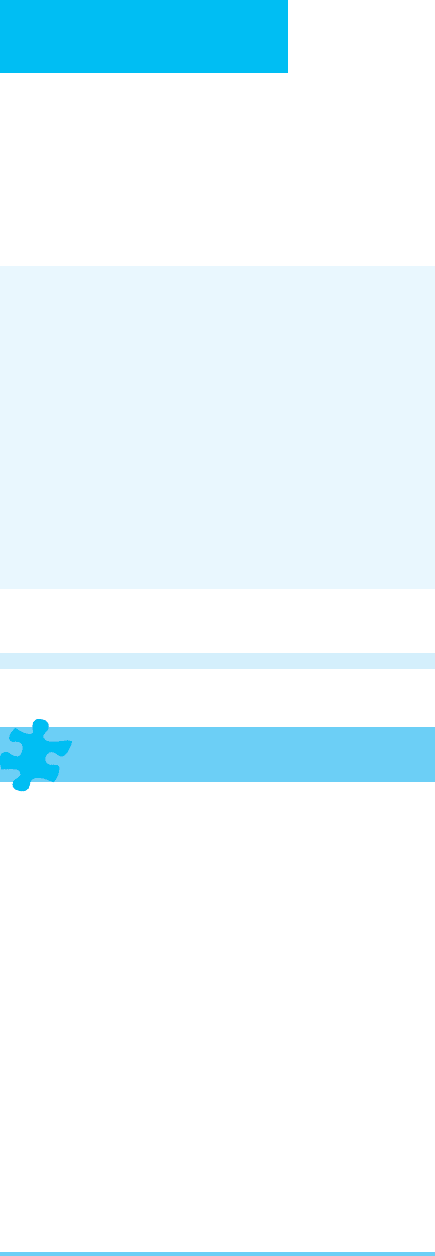
As with the clinical diagnosis, the radiologic diagnosis is also
difficult. In the patient population most prone to acalculous
cholecystitis, intrinsic functional and morphologic abnor-
malities of the gallbladder limit the specificity of both scintig-
raphy and sonography (Figure 7–35). Scintigraphy relies on
technetium (
99m
Tc) iminodiacetic acid to fill the gallbladder,
and scans often are done with pharmacologic intervention to
improve accuracy. Morphine may cause contraction of the
sphincter of Oddi, resulting in increased back pressure; chole-
cystokinin can be used to first empty the gallbladder. Although
the sensitivity of scintigraphy has been reported to be as high
as 95%, specificity is significantly lower than in calculous
cholecystitis. This is so because of the high number of false neg-
atives resulting from coexisting conditions such as prolonged
intubation, nasogastric suction, and hyperalimentation.
Sonographic features suggesting cholecystitis are simi-
larly compromised in these patients. They may have mild
wall thickening from edema and mild contraction. Often,
right upper quadrant tenderness mimicking a sonographic
Murphy sign is present in these patients in the absence of
acalculous cholecystitis. Although the sensitivity of sonogra-
phy is high, specificity is poor.
If results are equivocal, both scintigraphy and ultrasound
may be necessary, or a CT scan may be performed. Using IV
contrast–enhanced CT, mural thickening, mucosal enhance-
ment, and subtle pericholecystic inflammatory changes may
improve specificity.
Treatment
In patients with uncomplicated acute cholecystitis, IV antibi-
otics contain the inflammatory response and suppress further
inflammation, allowing patients to undergo less invasive surgery
with fewer complications. Although percutaneous aspiration
usually can be performed in patients with acute cholecystitis, its
role is debated because there is a high incidence of false-negative
sterile aspirates resulting from effective antibiotic treatment.
Temporary gallbladder decompression by percutaneous
cholecystostomy is beneficial in patients with acute cholecys-
titis who are at high surgical risk. The procedure is performed
with sonographic and fluoroscopic guidance in most institu-
tions, but it may be performed with CT guidance. It also can
be performed with sonographic guidance alone at the bed-
side. Complications, including bile leak, hemobilia, and vagal
reaction, have been reported in 5–10% of patients—less than
the complication rate associated with surgery (24%). Other
A
B
Figure 7–35. Acalculous cholecystitis. A. Ultrasound
demonstrates diffuse echoes throughout the gallbladder,
a marginally thickened wall, and positive sonographic
Murphy’s sign. B. HIDA (hepatobiliary iminodiacetic acid)
scan. The gallbladder does not fill with tracer by 60 minutes
despite provocative maneuvers.
CHAPTER 7
184
indications for percutaneous drainage include decompres-
sion of the biliary tract in cases of distal common duct
obstruction with only mild dilation of the intrahepatic ducts.
Some have advocated performing percutaneous cholecys-
tostomy in critically ill patients as a means of diagnosing and
treating acute cholecystitis. With this approach, in one study,
58% of critically ill patients improved.
Akhan O, Akinci D, Ozmen MN: Percutaneous cholecystostomy.
Eur J Radiol 2002;43:229–36. [PMID: 12204405]
Bennett GL, Balthazar EJ: Ultrasound and CT evaluation of emer-
gent gallbladder pathology. Radiol Clin North Am
2003;41:1203–16. [PMID: 14661666]
Bortoff GA et al: Gallbladder stones: Imaging and intervention.
Radiographics 2000;20:751–66. [PMID: 10835126]
Mariat G et al: Contribution of ultrasonography and cholescintig-
raphy to the diagnosis of acute acalculous cholecystitis in inten-
sive care unit patients. Intensive Care Med 2000;26:1658–63.
[PMID: 11193273]
Menu Y, Vuillerme MP: Non-traumatic abdominal emergencies:
Imaging and intervention in acute biliary conditions. Eur
Radiol 2002;12:2397–406. [PMID: 12271380]
Ziessman HA: Acute cholecystitis, biliary obstruction, and biliary
leakage. Semin Nucl Med 2003;33:279–96. [PMID: 14625840]
IMAGING IN EMERGENT & URGENT
GENITOURINARY CONDITIONS
Acute Renal Failure
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Ultrasound: In obstructive uropathy, dilation of the calices
and renal pelvis with visualization of echogenic calculi; in
intrinsic renal disease, increased cortical echogenicity
correlates with chronic medical renal disease.
CT: In obstructive uropathy, signs of acute obstruction
on CT include dilation of the collecting system, a source
of obstruction such as stone, swollen kidney with
increased stranding in the perinephric space; CT urogra-
phy (noncontrast helical CT) provides a rapid method of
detecting renal calculi and obstructive nephropathy
from a passing stone.
MR urography: Rapid assessment of cause and level of
obstruction; with gadolinium enhancement, differential
rates of enhancement permit assessment of renal
perfusion.
Renal scintigraphy: Technetium-99m MAG 3 scan per-
mits rapid assessment of differential renal function,
including flow, uptake, and excretion. Especially valuable
in transplanted kidneys to assess for a vascular occlusion
from intrinsic renal abnormality.
General Considerations
The workup of acute renal failure traditionally has been
focused on identifying prerenal, intrinsic renal, and postre-
nal causes. Prerenal causes (eg, cardiac or liver failure) and
systemic hypotension account for 75% of all causes of renal
failure. Intrinsic causes such as acute tubular necrosis and
glomerulonephritis account for 20%, and postrenal causes
such as obstructive nephropathy account for less than 5% of
cases. Imaging is used mainly to exclude an obstructive cause
of acute renal failure. These causes include obstruction from
a lower urinary tract source such as bladder tumor, prostatic
enlargement, or urethral stricture. Concomitant reflux also
may decrease renal function. Ureteral causes of obstruction
include luminal stones, tumors, blood clots, fungus balls, and
sloughed papillae, as well as extraluminal causes such as
mural strictures or extramural causes such as retroperitoneal
fibrosis, lymphadenopathy, or inadvertent ureteral ligation.
Radiographic Features
Azotemia due to obstruction is usually easily and rapidly
treatable. Cross-sectional imaging allows rapid identification
of hydronephrosis and its causes, as well as clues to evaluate
pyonephrosis, pyelonephritis, or abscess.
Sonography is the imaging method of choice to evaluate
hydronephrosis in the critically ill patient. It may be per-
formed at the bedside. Since it detects the presence of a
dilated collecting system, pitfalls in interpretation may be
present. In acute hydronephrosis, sonography may be normal
in 50% of patients because dilation is suboptimal, especially
in the first 72 hours. In subacute situations, a ruptured calix
may decompress the collecting system, leading to a false-
negative diagnosis if perinephric fluid is minimal or absent. A
volume-depleted patient may also have poor distention of the
collecting system due to low urine output. Patients with
retroperitoneal fibrosis or neoplastic encasement of the
ureters may have only minimally distended collecting sys-
tems. Conversely, patients with vesicoureteral reflux, para-
pelvic cysts, or prior episodes of inflammation may receive a
false-positive diagnosis of hydronephrosis. Sonography may
suggest the diagnosis of pyonephrosis or renal bleeding by the
presence of echoes in the collecting system.
In a large series of patients with azotemia undergoing renal
sonography, hydronephrosis was detected in 29% of those
known to be at high risk (ie, pelvic malignancy, palpable
abdominal or pelvic mass, renal colic, known nephrolithiasis,
bladder outlet obstruction, recent pelvic surgery, or sepsis).
However, in patients without these risk factors, hydronephro-
sis was detected in only 1%. Sixty-five percent of patients in
the low-risk group had medical renal disease compared with
36% of high-risk patients. The simplicity and relatively low
cost of a sonogram must be weighed against a typically nega-
tive result in the vast majority of patients and the risk of miss-
ing an obstructive cause of renal failure.
IMAGING PROCEDURES
185
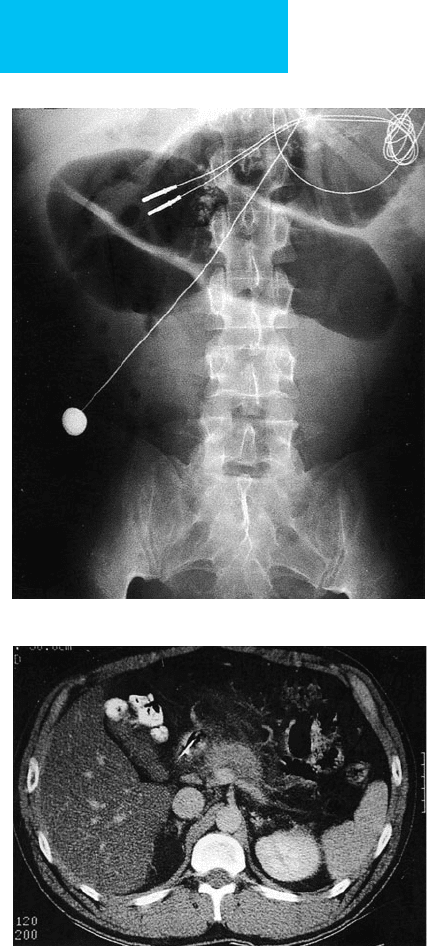
Helical noncontrast CT has emerged over the past few
years as the imaging procedure of choice for the evaluation
of renal colic (Figure 7–36). Helical CT detects over 99% of
all types of calculi—with the exception of the stones caused
by crystallization of the antiretroviral protease inhibitor
indinavir. Helical CT images stones not only in the renal col-
lecting system but also in the ureters, bladder, and posterior
urethra. CT also images the retroperitoneum and pelvis,
allowing detection of processes such as retroperitoneal fibro-
sis and lymphadenopathy. CT is excellent for the detection of
perirenal abscesses and abscesses in other areas of the
abdomen and pelvis.
When a potentially obstructing stone is found in the uri-
nary tract, the specific signs of obstruction include
hydronephrosis and hydroureter to the level of obstruction,
unilateral infiltration of perirenal and periureteral fat, and a
swollen kidney. Hydronephrosis may not be distinguishable
from pyonephrosis. However, high-density debris or, espe-
cially, gas within the collecting system suggests pyonephrosis.
MRI is emerging as a tool for evaluating urinary tract dis-
ease. However, it is currently impractical in critically ill
patients.
Urinary Tract Infection
ESSENTIALS OF RADIOLOGIC
DIAGNOSIS
Ultrasound: Usually normal in uncomplicated pyelonephri-
tis. However, the kidneys may be enlarged, with variable
echogenicity. Focal nephritis may appear as a solid renal
mass. A renal abscess appears as a complex cystic or
hypoechoic mass.
CT: Pyelonephritis is typically associated with nonspe-
cific findings. Kidneys may be enlarged, with peri-
nephric stranding. With IV contrast material, a striated
nephrogram may be seen with delayed function in
infected areas. Focal nephritis appears as an ill-
defined region of low attenuation in a lobar distribu-
tion. Renal abscesses are well-defined masses, often
with an enhancing rim, increased attenuation of the
adjacent perirenal fat, and thickening of the renal
fascia.
General Considerations
Pyelonephritis is typically a clinical diagnosis. Imaging is
helpful to detect complications of pyelonephritis or urosep-
sis or in patients who have failed to respond to standard
medical therapy. Complications of pyelonephritis include
pyonephrosis, renal or perirenal abscess, or other conditions
requiring surgical or percutaneous intervention.
A
B
C
Figure 7–36. Obstructive uropathy. A. Ultrasound shows
moderate hydronephrosis of the left kidney. B. CT scan
demonstrates moderate left hydronephrosis with
hydroureter. C. There is a tiny calculus obstructing the left
ureterovesical junction.

CHAPTER 7
186
Radiographic Features
Sonography is relatively insensitive and nonspecific in diag-
nosing acute pyelonephritis. It is useful to exclude
hydronephrosis and possibly pyonephrosis, as well as renal or
perirenal abscess. However, sonography cannot diagnose
changes in the perinephric fat or inflammatory thickening of
the perirenal fascia.
Barrozzi L et al: Renal ultrasonography in critically ill patients. Crit
Care Med 2007;35:S198–205. [PMID: 17446779]
Colistro R et al: Unenhanced helical CT in the investigation of
acute flank pain. Clin Radiol 2002;57:435–41. [PMID:
12069457]
Dalrymple NC et al: Pearls and pitfalls in the diagnosis of
ureterolithiasis with unenhanced helical CT. Radiographics
2000;20:439–47. [PMID: 10715342]
Demertzis J, Menias CO: State of the art: Imaging of renal infec-
tions. Emerg Radiol 2007;14:13–22. [PMID: 17318482]
Noble VE, Brown DF: Renal ultrasound. Emerg Med Clin North
Am 2004;22:641–59. [PMID: 15301843]
Rao PN: Imaging for kidney stones. World J Urol 2004;22:323–7.
[PMID: 15290203]
Sandhu C, Anson KM, Patel U: Urinary tract stones: I. Role of radi-
ological imaging in diagnosis and treatment planning. Clin
Radiol 2003;58:415–21. [PMID: 12788310]
Tamm EP et al: Evaluation of the patient with flank pain and pos-
sible ureteral calculus. Radiology 2003;228:319–29. [PMID:
12819343]
