Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


SHOCK & RESUSCITATION
237
dopamine because the latter depletes myocardial norepineph-
rine stores. Dosage typically ranges from 5–15 μg/kg per
minute. Increased urine output also may be achieved after
dobutamine administration because of increased renal perfu-
sion from elevated cardiac output. Infusion is begun at a rate
of 2–5 μg/kg per minute and titrated to the desired effect.
Maximal benefit is usually achieved at levels between 10 and
15 μg/kg per minute.
3. Alpha-adrenergic agents—Despite adequate volume
resuscitation and improved cardiac output, blood pressure
may remain depressed. Phenylephrine and norepinephrine
are two agents commonly used to increase systemic vascular
resistance.
Norepinephrine is the biosynthetic precursor of epineph-
rine, and as such posses both α- and β-adrenergic activity. In
low doses, its major effect is β-adrenergic. It increases cardiac
contractility, conduction velocity, and heart rate. At higher
doses, both α- and β-adrenergic effects occur, which include
peripheral vasoconstriction, increased cardiac contractility, car-
diac work, and stroke volume. Norepinephrine causes splanch-
nic vasoconstriction, which may lead to end-organ ischemia.
The drug is cleared rapidly from the plasma with a half-life of
approximately 2 minutes. Initial infusion rates are 0.5–1
μg/min. The usual maximum dose is 1 μg/kg per minute.
4. Vasopressin—Vasopressin (antidiuretic hormone) is nor-
mally released by the hypothalamus and produces vasocon-
striction of vascular smooth muscle in addition to its
antidiuretic effect on the renal collecting system. At low plasma
concentrations it causes vasodilation of the coronary, cerebral,
and pulmonary vessels. Vasopressin levels increase in early sep-
tic shock and later fall as sepsis worsens. When given in doses
of 0.01–0.04 units/min, vasopressin infusion increases serum
vasopressin levels and decreases the need for other vasopres-
sors. At this dose, urinary output may increase, and pulmonary
vascular resistance may decrease. Doses higher than 0.04
units/min can cause undesirable vasoconstrictive effects.
5. Vasodilators—Because decreased vascular resistance is
the primary cause of hypotension in septic shock, further
pharmacologic vasodilation is contraindicated. Occasionally,
severe myocardial depression is accompanied by an increase
in systemic vascular resistance. This preterminal event puts
further strain on the left ventricle and may cause complete
hemodynamic collapse. Judicious use of vasodilators such as
nitroprusside may be tried. Nitroglycerin is probably an infe-
rior choice because it also reduces preload.
E. Antimicrobial Agents—Identification of the source of
sepsis is imperative. If the offending tissue bed is not drained
or if bacteremia is not treated, outcome will be adversely
affected. Evaluation of the patient’s history is essential to deter-
mine likely sources. Once the probable origin has been identi-
fied, appropriate antimicrobial therapy can be instituted to
provide coverage for organisms commonly encountered. The
details of diagnosis and therapy of infections are presented in
Chapters 15 and 16. When a likely source cannot be identified,
empirical broad-spectrum therapy should be instituted with
drugs known to be effective against gram-positive, gram-
negative, and anaerobic organisms. In surgical patients who
have had abdominal procedures, enteric gram-negative and
anaerobic organisms are of particular concern. Attention must
be given to dosing in these patients because alterations in renal
function may affect degradation and because an expanded
plasma volume affects the volume of distribution and there-
fore the size of the loading dose that must be given.
F. Glycemic Control—Hyperglycemia is defined as a blood
glucose concentration of greater than 110 mg/dL and is com-
mon in critically ill patients. Multiple factors contribute to
hypergylcemia, including increased levels of stress hor-
mones, peripheral insulin resistance, drugs, and exogenous
dextrose infusion. Hyperglycemia has a number of detrimen-
tal effects, including decreased leukocyte adhesion, impaired
neutrophil chemotaxis, and phagocytosis. Hypergylcemia
also may be prothrombotic.
Rigid control of hyperglycemia has been shown to
improve outcome, likely by reducing the incidence of sepsis-
induced multiple-organ failure. Additionally, tight control
has been shown to reduce the length of stay in the ICU, atten-
uate the inflammatory response, decrease antibiotic use,
reduce the incidence and duration of critical-illness polyneu-
ropathy, and reduce the number of ventilator days.
Glucose control may be provided with either a glucose
concentration–dependent dose (“sliding scale”) or a con-
stant infusion for higher serum glucose levels. Typically, glu-
cose levels should remain below 130 mg/dL.
G. Corticosteroids—While older studies demonstrated no
benefit to the use of supraphysiologic doses of corticos-
teroids, more recent work has found that lower physiologic
doses for longer periods of time may be beneficial. Patients
should undergo a Cortrosyn stimulation test. After obtaining
blood for a baseline concentration of serum cortisol, 250 μg
Cortrosyn is given intravenously, and blood for a repeat
serum cortisol assay is collected 30–60 minutes later. If there
is concern that the patients is hypoadrenal, 4 mg dexametha-
sone can be given prior because it does not interfere with the
test. If the increase after Cortrosyn is less than 9 μg/dL, there
is insufficient adrenal reserve, and 50 mg hydrocortisone
should be given every 6 hours for 7 days. This should be sup-
plemented with fludrocortisone 50 μg orally every day. It is
likely that all patients should be started on replacement cor-
ticosteroid until the results of the stimulation study are
known, at which time supplementation can be withdrawn
from those who responded to the stimulation test.
H. Drotrecogin Alfa—Drotrecogin alfa is a glycoprotein ana-
logue of protein C that is activated by thrombin. Activated
protein C inhibits coagulation, increases fibrin breakdown,
and possibly inhibits the synthesis of TNF. A large clinical
study of drotrecogin alfa found a reduction in mortality from
30.8% in patients treated with placebo to 24.7% in those
treated with the drug. The most important adverse effect of
CHAPTER 11
238
the drug is bleeding, which occurred in 3.5% of those treated
with the drug compared with 2% treated with placebo.
Although the incidence of bleeding did not reach statistical
significance, the drug is contraindicated in patients with active
or recent bleeding or a high risk of bleeding, an epidural
catheter, or intracranial hemorrhage. It should be used cau-
tiously in those at risk for bleeding. Drotrecogin alfa is admin-
istered intravenously at a continuous dose of 24 μg/kg per
hour for 96 hours. No alteration in the dose is required for
those with renal or hepatic compromise. The drug’s cost is
approximately $8000 for a 4-day regimen in a 70-kg patient.
I. Transfusion—The traditional transfusion threshold of 10
mg/dL has been challenged by the finding that patients are
not adversely affected by withholding transfusion until
hemoglobin concentration drops to between 7 and 9 g/dL.
Further, there may be some advantage to lower hemoglobin
concentrations in patients older than age 55. Such data come
from broad groups of patients, and specific conclusions can-
not be drawn. It is likely, however, that more restrictive
thresholds are not harmful and actually may reduce mortal-
ity. The availability of recombinant human erythropoietin
may be a useful adjunct to reducing the need for transfusion
in critically ill patients.
J. Other Modalities—Septic patients require multimodality
support, including gastrointestinal and renal. To this end,
proper prophylaxis against gastric stress ulceration should be
provided with either H
2
-receptor blockade or proton pump
inhibitors. Additionally, renal function must be monitored
closely, and appropriate support with either hemofiltration
and/or dialysis should be provided. Adequate prophylaxis
against deep venous thrombosis includes either unfraction-
ated or low-molecular-weight heparin. The dose of some
low-molecular-weight heparins needs to be adjusted or with-
held in patients with renal failure. Lower extremity compres-
sion stockings are valuable adjuncts.
Current Controversies and Unresolved Issues
A. Fluid Resuscitation—The choice of fluid for the initial
and continued resuscitation of septic patients is widely
debated. Proponents of balanced salt solutions claim that pul-
monary dysfunction is not worsened by judicious administra-
tion guided by endpoints such as ventricular filling pressure
and cardiac output. Colloids increase the circulating plasma
volume more effectively than do crystalloids, but they are
expensive. When pulmonary microvascular permeability is
increased, colloids actually may worsen respiratory function
by increasing the osmotic gradient favoring translocation of
fluid into the alveolar and pulmonary interstitial spaces.
Activated protein C (Xigris) for severe sepsis. Med Lett Drugs Ther
2002;44:17–18. [PMID: 11856952]
Bernard GR et al: Efficacy and safety of recombinant human acti-
vated protein C for severe sepsis. N Engl J Med 2001;344:
699–709. [PMID: 11236773]
Dellinger RP et al: Surviving Sepsis Campaign guidelines for man-
agement of severe sepsis and shock. Crit Care Med
2008;36:296–327. [PMID: 18158437]
Holcroft JW, Robinson MK: Shock: identification and manage-
ment of shock states. In: Care of the Surgical Patient. Scientific
American, 1992.
Holmes CL et al: Physiology of vasopressin relevant to manage-
ment of septic shock. Chest 2001;120:989–1002. [PMID:
11555538]
Howell G, Tisherman SA: Management of sepsis. Surg Clin North
Am 2006;86:1523–39. [PMID: 17116461]
Mecher CM et al: Unaccounted anion in metabolic acidosis during
septic shock in humans. Crit Care Med 1991;19:705–11. [PMID:
2026034]
Opal SM, Cross AS: Clinical trials for severe sepsis. Infect Dis Clin
North Am 1999;13:285–97. [PMID: 10340167]
Sihler KC, Nathens AB: Management of severe sepsis in the surgi-
cal patient. Surg Clin North Am 2006;86:1457–81. [PMID:
17116457]
Smith AL: Treatment of septic shock with immunotherapy.
Pharmacotherapy 1998;18:565–80. [PMID: 9620107]
Snell RJ, Parillo JE: Cardiovascular dysfunction in septic shock.
Chest 1991;99:1000–9.
Suffredini A et al: The cardiovascular response of normal humans
to the administration of endotoxin. N Engl J Med 1989;321:
280–86. [PMID: 2664516]
Vincent JL, Preiser JC: Inotropic agents. New Horizons 1993;1:
137–44. [PMID: 7922387]
Vercueil A, Grocott MPW, Mythen MG: Physiology, pharmacology,
and rationale for colloid administration for the maintenance of
effective hemodynamic stability in critically ill patients.
Transfusion Med Rev 2005;19:93–109.
Vincent JL, Herwig G: Fluid resuscitation in sevre sepsis and septic
shock: An evidence-based review. Crit Care Med 2004;32:451–4.
Anaphylactic Shock & Anaphylactoid
Reactions
ESSENTIALS OF DIAGNOSIS
Cutaneous flushing, pruritus.
Abdominal distention, nausea, vomiting, diarrhea.
Airway obstruction owing to laryngeal edema.
Bronchospasm, bronchorrhea, pulmonary edema.
Tachycardia, syncope, hypotension.
Cardiovascular collapse.
General Considerations
Anaphylactic shock and anaphylactoid reactions are due to
the sudden release of preformed inflammatory mediators
from mast cells and basophils. After exposure to the offend-
ing stimulus, initial symptoms may appear within seconds to
minutes or may be delayed as long as 1 hour. Anaphylactic
SHOCK & RESUSCITATION
239
shock is differentiated from anaphylactoid reactions in that
the former is a true anamnestic response in which a sensi-
tized individual comes in contact with an antigenic sub-
stance. This reaction stimulates membrane-bound IgE,
causing mast cells and basophils to release histamine and
PAF into the circulation. These mediators result in vasodila-
tion, bronchoconstriction, pruritus, bronchorrhea, platelet
aggregation, and increased vascular permeability. The latter
may lead to laryngeal edema that culminates in airway
obstruction. The frequency and outcome of anaphylactic
reactions are summarized in Table 11–6. Anaphylactoid reac-
tions occur when the offending agent causes the direct release
of these substances without mediation by IgE. This may
involve a number of pathways, including complement-
mediated reactions, nonimmunologic activation of mast
cells, and production of arachidonic acid mediators.
Reactions to nonsteroidal anti-inflammatory drugs
(NSAIDs) are particularly dangerous because NSAID inhibi-
tion of the cyclooxygenase pathway favors the formation of
lipoxygenase pathway mediators from arachidonic acid.
Some of these include leukotrienes C
4
,D
4
,E
4
(slow-reacting
substance of anaphylaxis), and B
4
. These leukotrienes and
their intermediate products (5-HETE and 5-HPETE)
increase vascular permeability and produce bronchocon-
striction. Leukotriene B
4
is an eosinophilic and neutrophilic
chemoattractant. If the cyclooxygenase pathway is activated
by the inciting agent, the production of prostaglandin D
2
furthers bronchoconstriction. The most common agents
causing anaphylactic shock and anaphylactoid reactions are
listed in Tables 11–7 and 11–8. Anaphylactoid reactions may
occur in up to 10% of patients. When an initial reaction
occurs after the infusion of radiocontrast agents, the risk of a
similar reaction on reexposure approaches 35%.
Clinical Features
A. Symptoms and Signs—The initial symptoms are often
complaints of pruritus and a sense of impending doom.
These can progress to overt signs over several seconds or may
be delayed for up to an hour. Respiratory symptoms may
start with complaints of a lump in the throat, progressing to
dyspnea, dysphonia, hoarseness, and cough. If pulmonary
edema develops as a result of increased capillary permeability,
dyspnea and cyanosis result. Cardiovascular findings begin
with symptoms of weakness and faintness that may be accom-
panied by palpitations. As shock progresses, tachycardia
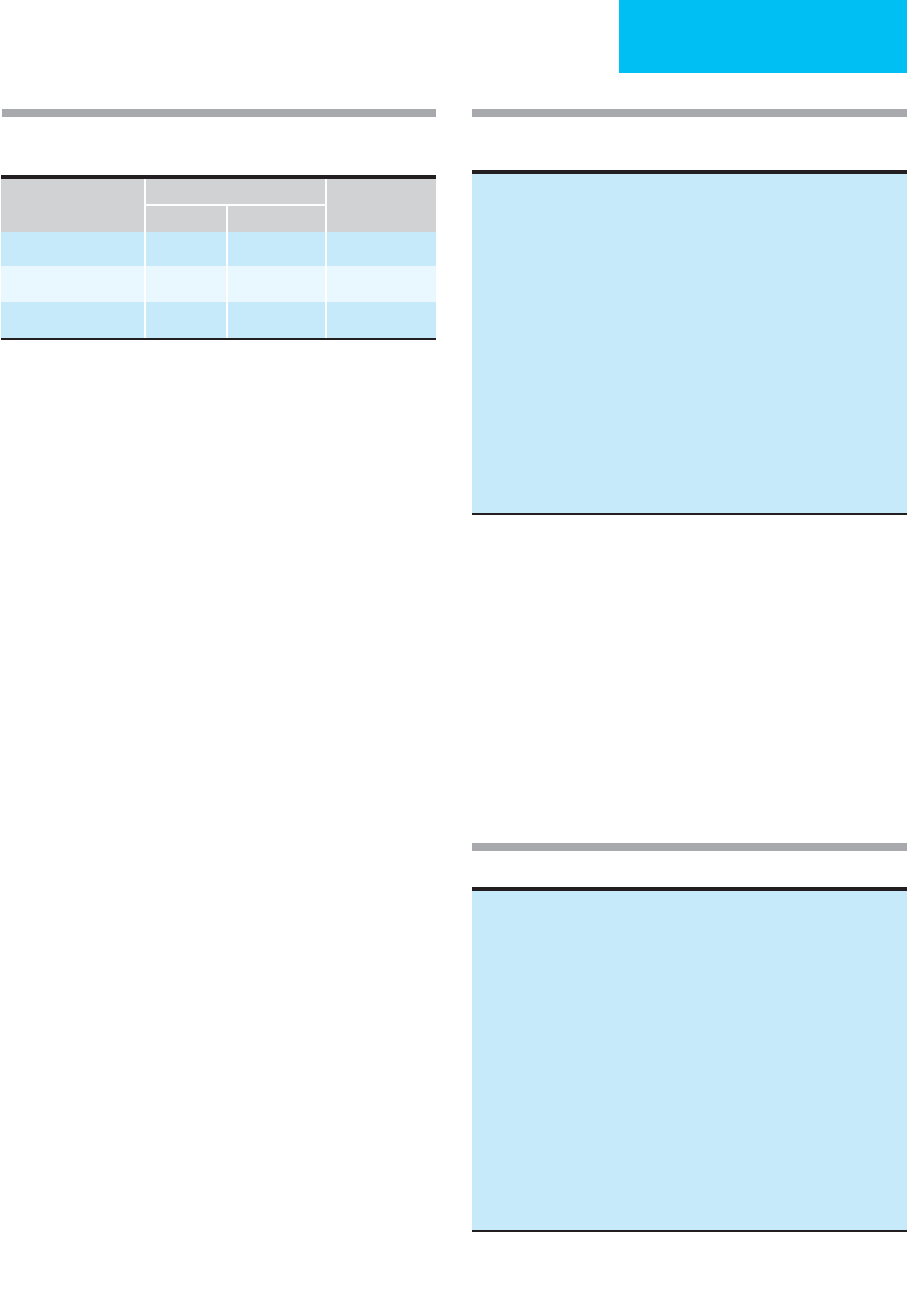
Agent
Frequency of Events
Mild Severe
Deaths per Year
(USA)
Penicillin 0.5–1% 0.04% 400–800
Hymenoptera stings 0.5% 0.05% ≥100
Contrast media 5% 0.10% 250–1000
From Lavine SJ, Shelhamer JH: Anapyhlaxis. In: Critical Care.
Civetta JM, Raylor RW, Kirby RR (editors). Lippincott, 1992.
Table 11–6. Frequency of anaphylactic events and
deaths.
Haptens Foods Venoms
Beta-lactam antibiotics Nuts Stinging insects,
Sulfonamides Shellfish especially
Nitrofurantoin Buckwheat Hymenoptera,
Demeclocycline Egg white fire ants
Streptomycin Cottonseed Hormones
Vancomycin Milk Insulin
Local anesthetics Corn Adrenocortico-tropic
Others Potato hormone
Serum products Rice Thyroid-stimulating
Immune globulin Legumes hormone
Immunotherapy for allergic Citrus fruits Enzymes
diseases Chocolate Chymopapain
Heterologous serum Others L-Asparaginase
Miscellaneous
Seminal fluid
Others
Modified from Austen KF: Systemic anaphylaxis in man. JAMA
1965;192:108; and from Kaliner M: Anaphylaxis. NER Allergy
Proceedings 1984;5:324.
Table 11–7. Etiologic agents responsible for anaphylactic
shock.
Complement-mediated reactions
Blood
Serum
Plasma
Plasmanate (not albumin)
Immunoglobulins
Nonimmunologic mast cell activators
Opioids
Radiocontrast media
Dextrans
Neuromuscular blocking agents
Others
Arachidonic acid modulators
Nonsteroidal anti-inflammatory drugs
Tartrazine (possibly)
Idiopathic
Most common conclusion after thorough evaluation
Adapted from Kaliner M: Anaphylaxis. NER Allergy Proceedings
1984;5:324.
Table 11–8. Etiologic agents for anaphylactoid reactions.

CHAPTER 11
240
appears along with arrhythmias, conduction disturbances, and
myocardial ischemia. Cutaneous symptoms include flushing
and pruritus that progress to urticaria, angioedema, and
diaphoresis. Patients may complain of abdominal pain or
bloating, cramps, and nausea. These progress to emesis, diar-
rhea, and occasionally hematemesis and hematochezia.
Other signs include syncope, seizures, conjunctival injection,
lacrimation, rhinorrhea, and nasal congestion.
B. Laboratory Findings—An increased hematocrit is found
commonly as a result of hemoconcentration from vascular
permeability. Serum mast cell tryptase is usually elevated.
Differential Diagnosis
Several common disorders seen in the ICU may be confused
with anaphylactic shock and anaphylactoid reactions:
myocardial ischemia and infarction, cardiac arrhythmias,
hypovolemic shock, septic shock, pulmonary embolism, aspi-
ration of feedings, bronchitis, acute exacerbation of chronic
obstructive pulmonary disease (COPD), seizure disorder,
hypoglycemia, and cerebrovascular accidents. Relationship to
administration of medications, blood, and new intravenous
solutions should suggest the possibility of anaphylaxis.
Treatment
A. Airway—The first mandate is to ensure a secure airway. If
the patient was intubated prior to the reaction, one should
take care that the endotracheal or nasotracheal tube does not
become dislodged during resuscitation. If the patient was not
intubated, emergency airway control by bag and mask or
intubation probably will be necessary. It is far better to intu-
bate these patients before laryngeal edema develops because
subsequent intubation is extremely difficult. Some clinicians
recommend the use of inhaled racemic epinephrine (0.3 mL
in 3 mL of saline administered by nebulizer) if upper airway
compromise occurs because of edema. It is far safer to intu-
bate the patient.
B. Circulatory Support—Most patients who develop ana-
phylactic shock or an anaphylactoid reaction in the ICU will
already have intravenous access. However, this catheter may
be small and will not permit the administration of large vol-
umes of fluid over a short period of time. Large-bore peripheral
intravenous lines are mandatory for fluid and drug adminis-
tration. Do not attempt central line placement in a hypoten-
sive patient who is hypovolemic. Collapse of the large veins
normally used for central catheter placement increases the
risk of a life-threatening complication.
1. Epinephrine—Drug therapy should begin with epineph-
rine (1:1000), 0.3–0.5 mL subcutaneously. The dose of epi-
nephrine may be repeated every 5–10 minutes as needed. If
the patient does not respond to the initial dose—or if severe
laryngospasm or frank cardiovascular collapse is present—
5–10 mL of epinephrine (1:10,000) may be administered
intravenously. If intravenous access is not available, either
0.5 mL of a 1:1000 dilution may be given intramuscularly or
10 mL of a 1:10,000 dilution may be instilled into the endo-
tracheal tube. When epinephrine is given intravenously,
severe tachycardia, myocardial ischemia, vasospasm, and
hypertension may result. Epinephrine decreases mediator
synthesis by increasing intracellular concentrations of cAMP.
Furthermore, it counteracts many of the deleterious effects of
the mediators of anaphylaxis.
2. Histamine antagonists—Histamine antagonists should
be administered as early as possible. Diphenhydramine
(1 mg/kg intravenously) and ranitidine (50 mg intravenously
over 5 minutes) are the preferred drugs. Cimetidine must be
used with extreme caution because rapid intravenous admin-
istration may result in hypotension or asystole.
3. Pressors—If hypotension persists after the repeated
administration of epinephrine and histamine antagonists,
aggressive fluid resuscitation is required. If this fails,
dopamine may be started at an initial dose of 5 μg/kg per
minute and increased until the dose reaches 20 μg/kg per
minute. A plateau effect occurs above this dose, requiring
that a second pressor be used if an adequate response has not
yet been achieved. Because of the extreme vasodilation, nor-
epinephrine should be started in the range of 3–4 μg/min
and titrated until a mean arterial pressure between 60 and
80 mm Hg is reached. The patient should be weaned from
pressors as quickly as possible.
C. Other Measures—Continued observation in the ICU is
indicated. An arterial catheter should be inserted for pressure
monitoring and to aid in securing blood gas samples for ven-
tilator management. In patients who remain unstable or who
require continuing pressor infusion, a pulmonary artery
catheter should be placed. Biphasic anaphylaxis may occur in
up to 25% of patients. Life-threatening reactions reappear
after an asymptomatic interval of up to 8 hours following
resuscitation. Hydrocortisone, 100–250 mg intravenously
every 6 hours, may help to prevent the late manifestations of
biphasic anaphylaxis. Steroids probably have no role in the
immediate treatment of acute anaphylaxis.
Patients who are receiving beta-blockers at the time of an
anaphylactic reaction may be resistant to the effects of
administered epinephrine. Atropine and glucagon may be
useful adjuncts to reverse the cardiac manifestations of
anaphylaxis in these patients.
Prognosis
The patient’s overall medical condition, the delay between
exposure to the antigen and the onset of anaphylaxis, and the
severity of symptoms all influence the outcome.
Anderson JA: Allergic reactions to drugs and biological agents.
JAMA 1992;268:2844–57. [PMID: 1433700]
Atkinson TP, Kaliner MA: Anaphylaxis. Med Clin North Am
1992;76:841–55. [PMID: 1614236]
SHOCK & RESUSCITATION
241
Goust JM: Immediate hypersensitivity. Immunol Ser 1993;
58:343–59. [PMID: 8424982]
Levine SJ, Shelhamer JH: Anaphylaxis. In: Civetta JM, Taylor RW,
Kirby RR (eds), Critical Care. Philadelphia: Lippincott, 1992.
Levy JH, Levi R: Diagnosis and treatment of anaphylactic/
anaphylactoid reactions. Monogr Allergy 1992;30:145–55.
[PMID: 1280764]
Marone G, Stellato C: Activation of human mast cells and basophils
by general anesthetic agents. Monogr Allergy 1992;30:54–73.
Raper RF, Fisher MM: Profound reversible myocardial depression
after anaphylaxis. Lancet 1988;1:386–9. [PMID: 2893192]
White MV: The role of histamine in allergic disease. J Allergy Clin
Immunol 1990;86:599–605. [PMID: 1699987]
Neurogenic Shock
ESSENTIALS OF DIAGNOSIS
Preceded by trauma or spinal anesthesia.
Hypotension with tachycardia.
Cutaneous warmth and flushing in the denervated area.
Venous pooling.
General Considerations
Neurogenic shock is produced by loss of peripheral vasomo-
tor tone as a result of spinal cord injury, regional anesthesia,
or administration of autonomic blocking agents. Blood
becomes pooled in the periphery, venous return is decreased,
and cardiac output falls. If the level of interruption is below
the midthorax, the remaining adrenergic system above the
level of injury is activated, resulting in increased heart rate
and contractility. If the cardiac sympathetic outflow is
affected, bradycardia results. Blood pressure can decrease to
extremely low levels as blood pools peripherally in the
venous reservoir. All patients who have sustained spinal
trauma should be assumed to have hypovolemic shock from
associated injuries until proved otherwise.
Clinical Features
A. Symptoms and Signs—Patients may be alert and
responsive if head injuries are absent. Extremities are warm
above the level of injury and cool below. Blood pressure may
be extremely low, with a very rapid heart rate. Skeletal mus-
culature is affected after trauma. Loss of the peripheral
venous muscular pump may further decrease venous return.
Signs and symptoms of spinal cord injury and spinal shock
will be present.
B. Laboratory Findings—Laboratory studies are not helpful
in diagnosis. Because capillary permeability is normal,
plasma leaks do not occur. Prior to volume resuscitation,
hematocrit is usually normal.
C. Imaging Studies—Radiographs of the cervical, thoracic,
and lumbosacral spine are important to determine whether
fractures are present that may be unstable. These typically
will have been completed before the patient was admitted to
the ICU, but the intensivist must review the films so that
patient manipulations will not cause further spinal cord
injury. CT and MRI may be useful to determine whether
fragments within the spinal canal may be causing cord com-
pression. When present, they may be amenable to neurosur-
gical decompression.
Differential Diagnosis
Trauma patients considered for admission to a critical care
unit after spinal injury must have thorough surgical and neu-
rosurgical evaluation before transfer. The presence of con-
comitant hypovolemic shock from unrecognized bleeding
sites within the abdomen, chest, and extremities must be
excluded. Isolated head injury does not cause shock. Rather,
it may increase the blood pressure while slowing the heart
rate (Cushing’s reflex).
Treatment
A. Supportive Measures—A secure airway and adequate
intravenous access are urgent priorities. If intubation is
required and there is concern regarding the stability of the
cervical spine, fiberoptic or nasotracheal intubation may be
required. A diligent search must be made for other injuries in
trauma patients. When neurogenic shock arises from a spinal
anesthetic procedure in which the level of blockade has
become too high, intubation also may be necessary because
of compromise of the muscles of respiration.
Depending on the level of the injury, patients may have
loss of bladder function. A Foley catheter should be
inserted to decompress the bladder and aid in monitoring
urine output.
B. Fluid Resuscitation—Effective circulating blood volume
decreases dramatically because of venous pooling. Fluid
resuscitation is usually necessary and typically begins with
several liters of balanced salt solution. In some patients, this
may be all that is required to increase blood pressure.
C. Pharmacologic Support—If volume infusion fails to
restore the blood pressure, infusion of an alpha-adrenergic
agent is required to provide direct vasoconstriction. Either
phenylephrine or norepinephrine may be used. These drugs
are started in low doses and increased slowly until just suffi-
cient to restore blood pressure to a mean between 60 and
80 mm Hg. Weaning usually can be achieved fairly quickly, so
central venous or pulmonary artery catheterization is not
often required.
D. Surgery—If spinal cord transection is complete, the only
role for surgery is stabilization of vertebral fractures to pre-
vent further injury. If a foreign body is present, removal may
promote return of function if the cord is intact.
CHAPTER 11
242
E. Rehabilitation—After the acute stage has passed and the
patient has been stabilized, planning should be undertaken
to provide long-term care. This is the most difficult part of
the management of these patients. Demands on nursing and
support personnel are extreme in order to prevent pressure
ulcers and urinary and respiratory tract infections and to
provide nutritional support. Early consultation with a psy-
chiatrist is recommended to help the patient adjust to com-
plete and permanent loss of function.
CARDIAC SHOCK
Cardiac shock occurs when the heart fails to adequately
pump the blood volume presented to it. There are two gen-
eral categories: cardiogenic shock and cardiac compressive
shock. Cardiogenic shock develops when the heart loses its
ability to function as a pump. Cardiocompressive shock is
due to compression of the great veins and cardiac chambers,
restricting their normal filling and emptying.
Cardiogenic Shock
ESSENTIALS OF DIAGNOSIS
Decreased urine output.
Impaired mental function.
Cool extremities.
Distended neck veins.
Hypotension with evidence of peripheral and pul-
monary venous congestion.
General Considerations
Cardiogenic shock occurs most commonly either after
relentless progression of cardiac disease or after an acute
event such as myocardial infarction or rupture of a cardiac
valve or septum. These causes are summarized in Table 11–9.
The absolute amount of myocardium involved is probably
the most important prognostic factor. When more than 45%
of the left ventricular myocardium is necrotic, cardiogenic
shock becomes evident clinically.
Bradycardia and arrhythmias may underlie cardiogenic
shock. Heart rates less than about 50 beats/min may be inad-
equate to support cardiac output. Similarly, arrhythmias may
significantly alter cardiac filling patterns and prevent ade-
quate pumping.
A staging system has been developed for the classification
of cardiogenic shock that develops on a chronic basis.
A. Stage I (Compensated Hypotension)—The decreased
cardiac output and resulting hypotension invoke compensa-
tory mechanisms able to restore blood pressure and tissue
blood flow to normal levels. These reflexes are mediated by
the arterial baroreceptors, which increase the systemic vascu-
lar resistance.
B. Stage II (Decompensated Hypotension)—Cardiac
output falls below that which enables the peripheral vascula-
ture to maintain blood pressure by vasoconstriction. Blood
pressure and tissue perfusion fall.
C. Stage III (Irreversible Shock)—Profound reduction in
flow activates ischemic mediators such as the complement
cascade. Membrane injury develops that further aggravates
the ischemic insult. Irreversible myocardial and peripheral
tissue damage occur.
Clinical Features
A. Symptoms and Signs—When cardiogenic shock occurs
as a result of an acute event, pain may be a prominent find-
ing. Details of diagnosis and management of acute myocar-
dial infarction are presented in Chapter 22. When shock is an
acute exacerbation of a relentless process or the result of
another disease, symptoms may be less pronounced.
Physical examination will reveal signs consistent with the
underlying pathophysiologic mechanism of decreased car-
diac output and absolute hypervolemia. Blood pressure is
less than 90 mm Hg. The heart rate may be extremely high
and exceed the maximum aerobic limit (230––the patient’s
age in years). When decompensation occurs, bradycardia
usually develops. Neck veins are distended, and pulsations
frequently can be observed more than 4 cm above the clavi-
cle with the patient in the semierect position. Peripherally,
the extremities are cool, reflecting inadequate perfusion.
Abdominal examination may reveal a congested and dis-
tended liver that is tender to palpation. Rales are detected on
auscultation of the lungs in a patient who has a normal right
ventricle. With biventricular failure or pulmonary hyperten-
sion, pulmonary auscultation may be normal. Cardiac exam-
ination typically reveals a third heart sound, and there may
be a murmur characteristic of valvular disease.
B. Hemodynamic Effects—Virtually all patients with car-
diogenic shock will require a pulmonary artery catheter for
monitoring and evaluation of the response to therapy. The
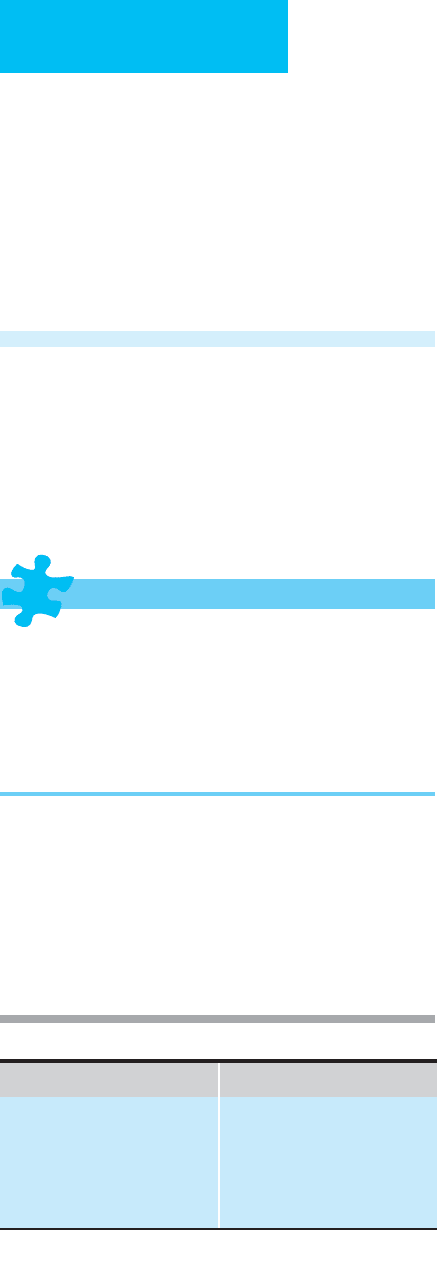
Nonmechanical Causes Mechanical Causes
Acute myocardial infarction
Low cardiac output syndromes
Right ventricular infarction
End-stage cardiomyopathy
Rupture of septum or free wall
Mitral or aortic insufficiency
Papillary muscle rupture or
dysfunction
Critical aortic stenosis
Pericardial tamponade
From Farmer JA: Cardiogenic Shock. In: Critical Care. Civetta JM,
Taylor RW, Kirby RR (editors). Lippincott, 1992.
Table 11–9. Causes of cardiogenic shock.

SHOCK & RESUSCITATION
243
usual findings are elevation of central venous and pul-
monary capillary wedge pressures and a cardiac index less
than about 1.8 L/min/m
2
.
C. Laboratory Findings—If acute myocardial infarction is
the precipitating cause, elevated cardiac bands of creatine
kinase will be observed. Plasma drug levels of medications
the patient has been receiving should be measured to deter-
mine whether they are in the toxic or subtherapeutic ranges.
A routine chemistry panel is required to evaluate K
+
and
HCO
3
–
. Serum lactate may be elevated when shock has been
prolonged. Hematocrit and hemoglobin should be deter-
mined to evaluate the need for transfusion.
D. Imaging Studies—Chest radiography often will reveal a
pattern of pulmonary edema. Radionuclide ventriculogra-
phy may be helpful in evaluating ventricular ejection frac-
tion. Echocardiography is also useful in the evaluation of
valvular and ventricular function. If pericardial tamponade
is suspected, echocardiography is the examination of choice
to establish that diagnosis.
Differential Diagnosis
Cardiogenic shock should be suspected in patients with
chronic myocardial disease who experience a sudden wors-
ening of symptoms. Acute myocardial infarction may be
complicated by ventricular septal rupture, papillary muscle
rupture, and papillary muscle dysfunction, which can lead to
cardiogenic shock. Constrictive pericarditis and rupture of a
cardiac ventricular aneurysm may lead to cardiac compres-
sive shock. Rupture of an abdominal aortic aneurysm in a
patient with coronary artery disease may cause diagnostic
confusion. Abdominal pain owing to rupture of the
aneurysm may simulate the pain of acute myocardial infarc-
tion. Electrocardiography typically reveals myocardial
ischemia. The absence of distended neck veins is the critical
distinguishing feature. Myocardial contusion after blunt
trauma may cause severe cardiogenic shock.
Treatment
A. General Measures—Patient comfort and relief of anxi-
ety should be addressed immediately. Opioids not only
relieve pain and provide sedation—but they also block
adrenergic discharge and lessen cardiac stress. Intravenous
morphine should be given starting with a bolus of 2–4 mg.
Dosing should be titrated to both subjective response and
effect on blood pressure. Because morphine is a vasodilator,
it may decrease right ventricular filling and adversely affect
blood pressure in a hypovolemic patient. An arterial catheter
and a pulmonary artery flotation catheter usually are
mandatory to manage these patients effectively.
When cardiogenic shock is the result of acute myocardial
infarction, early efforts should be directed at controlling the
infarct size. An imbalance between oxygen delivery and
increased oxygen consumption prompted by changes in
heart rate, blood pressure, and contractility may extend the
size of the infarction. If therapy is begun within 3 hours of
myocardial infarction, the incidence of cardiogenic shock is
4%. However, if therapy is delayed, cardiogenic shock occurs
in up to 13% of patients. Intravenous nitroglycerin and beta-
blockers are the main features of early treatment.
Nitroglycerin reduces right ventricular preload and
decreases left ventricular afterload. The reduction in after-
load decreases end-diastolic pressure and reduces wall stress
and myocardial oxygen consumption. Furthermore, it dilates
epicardial vessels and may improve oxygen delivery to
ischemic areas. The early use of nitroglycerin both decreases
infarct size and reduces early mortality. The possibility of
right ventricular infarction and pericardial tamponade must
be excluded before therapy with nitroglycerin is begun.
Beta-blockers decrease myocardial oxygen demand,
antagonize circulating catechols, and have antiarrhythmic
activity. A particular benefit may accrue when beta-blockers
are combined with thrombolytic agents. Beta-blockers are
best started within 2 hours of infarction. Calcium channel
blockers also have been investigated for this purpose but have
failed to demonstrate efficacy in acute situations. The mor-
tality rate may be increased if calcium channel blockers are
used in patients with pulmonary edema.
B. Resuscitation—Although cardiogenic shock may occur
in patients with whole body fluid overload, they may be
effectively hypovolemic. If PCWP is less than 10–12 mm Hg,
balanced salt solution should be administered in an attempt
to increase filling pressures. Cardiac output should be meas-
ured after each change of 2–3 mm Hg in PCWP. Filling pres-
sures near 20 mm Hg may be required before cardiac output
increases.
If laboratory studies reveal that the patient is hypoxemic,
supplemental oxygen should be provided. Oxygen delivery
should be maximized by ensuring complete arterial hemo-
globin saturation. Intubation with PEEP may be required to
accomplish this when pulmonary edema is present. Judicious
use of PEEP is required because it adversely affects ventricu-
lar preload and cardiac output.
C. Pharmacologic Support—Once volume status has been
optimized, support of the failing myocardium is often neces-
sary. Inotropes, vasodilators, and diuretics all may be used.
1. Inotropes—
a. Dobutamine—Dobutamine is the inotropic drug of
choice for the management of congestive heart failure and
cardiogenic shock. It is a β
1
-adrenergic agonist that has min-
imum chronotropic and peripheral vasoconstrictive effects.
It has a significant advantage over dopamine in that it does
not cause the release of norepinephrine. Furthermore, it does
not require the presence of norepinephrine at the nerve ter-
minals for effect. Because of its minimum chronotropic
effect, dobutamine can improve ventricular performance
without significantly increasing myocardial oxygen demand.
Dobutamine’s greatest potential is realized in patients with
reduced cardiac indices and increased filling pressures.

CHAPTER 11
244
Because it is a vasodilator, dobutamine reduces filling pres-
sures and wall tensions in patients with dilated ventricles.
This permits better myocardial nutrient flow during diastole.
A recent study found a 33% improvement in cardiac index, a
decrease in systemic vascular resistance, and no change in
heart rate or systemic blood pressure when dobutamine was
given in doses that averaged 8.5 μg/kg per minute. The drug
may be given in doses up to 40 μg/kg per minute without sig-
nificantly increasing heart rate. When three-vessel coronary
artery disease is present, dobutamine may create a steal and
direct blood away from ischemic areas.
b. Dopamine—The effects of dopamine depend on the
dose administered. In lower doses (<4 μg/kg per minute),
dopamine increases renal blood flow by stimulating
dopaminergic (D
1
) receptors in the kidney and causes
peripheral vasodilation through D
2
receptors that inhibit the
release of norepinephrine. At intermediate dosages (5–10
μg/kg per minute), dopamine improves cardiac function and
increases blood pressure without elevating myocardial oxy-
gen consumption. Systemic vascular resistance is usually not
increased. At higher doses (>10 μg/kg per minute),
dopamine elevates systemic vascular resistance by stimulat-
ing alpha-adrenergic receptors and heart rate by stimulating
beta-adrenergic receptors. A recent study found that an aver-
age dose of 17 μg/kg per minute was needed to optimize
coronary perfusion pressure in a group of patients that
developed cardiogenic shock after myocardial infarction.
Dopamine at such high levels increases myocardial oxygen
demand, produces tachycardia, and may limit renal perfusion.
It should be used with caution in patients with cardiogenic
shock because it may adversely influence the balance of
myocardial oxygen delivery and consumption.
c. Digoxin—Although digitalis preparations have modest
inotropic effects, they are probably of little importance in the
treatment of cardiogenic shock except for the treatment of
atrial fibrillation with rapid ventricular response. Small
intravenous doses of digoxin may improve diastolic filling
time and increase cardiac output in these situations.
d. Isoproterenol—This agent causes tachycardia, increased
myocardial contractility, and decreased peripheral vascular
resistance through its stimulation of both α
1
and β
2
receptors.
Myocardial oxygen consumption is increased dramatically.
Although isoproterenol increases coronary blood flow, it actu-
ally may shunt blood away from ischemic areas and increase
the infarct size. Highly restricted indications include the pres-
ence of bradycardia and severe aortic valvular insufficiency.
Intravenous administration is started at a dose of 0.01 μg/kg
per minute and increased until the desired effect is obtained.
e. Norepinephrine—Norepinephrine has both alpha- and
beta-adrenergic effects. At low doses, it causes beta stimula-
tion of the heart and increases blood pressure and cardiac
output. At higher doses, it primarily affects the alpha-
adrenergic receptors and supports blood pressure by increas-
ing systemic vascular resistance. At higher doses it also tends
to produce tachycardia, arrhythmias, and peripheral visceral
ischemia. Norepinephrine should be used with extreme caution
because at higher doses it increases left ventricular afterload
and may worsen myocardial ischemia. If cardiogenic shock
proves resistant to both dobutamine and dopamine, norepi-
nephrine may be started at doses of 1–2 μg/min and
increased until blood pressure increases. Of particular con-
cern are the visceral and renal vasoconstrictive effects that
may produce end-organ ischemia in the face of apparently
satisfactory blood pressure.
f. Other agents—Amrinone is a weak inotrope that increases
contractility independently of the catechol pathways. Although
its exact mechanism of action is not known, it increases intra-
cellular cAMP and calcium concentrations. The increased
cAMP concentration in smooth muscle decreases peripheral
and pulmonary vascular resistance and dilates coronary arter-
ies. Amrinone increases stroke volume without increasing heart
rate. The usual loading dose is 0.75 mg/kg over 3–5 minutes,
followed by a second bolus 30 minutes later. The boluses are
followed by a continuous intravenous infusion of 5–10 μg/kg
per minute. The total daily dose should not exceed 10 mg/kg.
After the bolus is given, effects are seen within several minutes.
Glucagon increases cardiac contractility and decreases
peripheral vascular resistance. The onset of action is
extremely rapid. A test dose of 4–6 mg should be given intra-
venously to determine whether any effect is produced. If suc-
cessful, this is followed by a constant infusion of 4–12 mg/h.
The agent appears to be useful for the treatment of cardio-
genic shock and left ventricular failure. It probably merits
consideration in patients who have failed to respond to other
agents or when dysrhythmias develop. It may be helpful when
left ventricular dysfunction is a result of treatment with beta-
blockers. Hyperglycemia is a side effect of the drug.
2. Vasodilators—Vasodilators are used to lower left ven-
tricular afterload, which decreases myocardial oxygen con-
sumption. Their use is limited by their hypotensive effect,
which may compound the difficulties associated with
peripheral oxygen delivery.
a. Nitroprusside—Nitroprusside decreases both afterload
and preload. When nitroprusside is used optimally, the
increase in left ventricular ejection fraction partially offsets
the decrease in systemic vascular resistance. Therapy begins
with a dose of 5–10 μg/min and is advanced in increments of
2.5–5 μg/min every 10 minutes until an increase in cardiac
output is noted. The dose should be reduced if systolic blood
pressure falls below 90 mm Hg. Nitroprusside may produce
an intracoronary steal that may aggravate areas of ischemia.
The drug is metabolized to cyanide and subsequently to thio-
cyanate. Doses above 3 μg/min may lead to toxicity, especially
when the drug is used for more than 3 days. Free cyanide ions
combine with cytochromes, leading to anaerobic metabolism
and increased lactate levels. This results in a metabolic acido-
sis that eventually culminates in confusion, hyperreflexia,
and coma. Thiocyanate levels should be monitored and not
permitted to rise above 10 mg/dL. Prophylactic infusion of
hydroxocobalamin may avert toxicity by combining with
cyanide to form cyanocobalamin.

SHOCK & RESUSCITATION
245
b. Nitroglycerin—Nitroglycerin is a nitrate derivative
whose greatest effect is preload reduction, which reflexly
decreases left ventricular filling. It has the additional advan-
tage of dilating the coronary vasculature and is the drug of
choice when cardiogenic shock is due to ischemia.
Nitroglycerin is also effective in the treatment of acute valvu-
lar incompetence. Care must be exercised to ensure that
patients are not hypovolemic prior to its administration
because the increased venous capacity will decrease venous
return and further lower the cardiac output. The normal
starting dose is 10 μg/min, which can be increased by 10 μg/min
every 5–10 minutes to a total dose of 50–100 μg/min. Doses
as high as 400 μg/min can be tolerated for several days.
D. Other Modalities—The management of acute myocar-
dial infarction is discussed in Chapter 22. Newer modalities
available to improve cardiac function after infarction include
thrombolytic therapy, percutaneous angioplasty, balloon
pumping, and left ventricular assist devices. Emergency
coronary artery bypass grafting is an option for patients who
fail to respond to other forms of treatment.
Prognosis
Fulminant cardiogenic shock continues to carry a mortality
rate of 90% when only pharmacologic therapy is used.
Application of percutaneous transluminal coronary angio-
plasty, left ventricular assist devices, and early surgical revas-
cularization may help to improve this outcome.
Farmer JA: Cardiogenic shock. In: Civetta JM, Taylor RW, Kirby RR
(eds), Critical Care. Philadelphia: Lippincott, 1992.
Handler CE: Cardiogenic shock. Postgrad Med J 1985;61:705–12.
[PMID: 3898054]
Holcroft JW, Wisner DH: Shock and acute pulmonary failure in
surgical patients. In: Way LW (ed), Current Surgical Diagnosis &
Treatment, 9th ed. Stanford, CT: Appleton & Lange, 1991.
Mueller HS: Inotropic agents in the treatment of cardiogenic
shock. World J Surg 1985;9:3–10. [PMID: 3885584]
Cardiac Compressive Shock
ESSENTIALS OF DIAGNOSIS
Hypotension with tachycardia.
Oliguria.
Mental status changes.
Distended neck veins.
General Considerations
Cardiac compressive shock is a low-output state that occurs
when the heart or great veins are compressed. Compression
either impedes the return of blood to the heart or prevents
effective pumping action of the heart itself. Pericardial tam-
ponade is due to fluid within the pericardial sac that con-
stricts the cardiac chambers and prevents them from filling
properly. This may occur acutely after penetrating trauma
with laceration of a coronary artery, or it may be progressive
with chronic diseases such as uremia and connective tissue
disorders. Distention of the abdomen with elevation of the
diaphragm compresses the heart and may produce a form of
shock. PEEP used with mechanical ventilation increases the
intrathoracic pressure, which both collapses the superior and
inferior venae cavae and reduces the transmural pressure
gradient, thereby decreasing cardiac filling. In similar fash-
ion, tension pneumothorax increases the intrathoracic pres-
sure and decreases venous return.
Clinical Features
A. Symptoms and Signs—Signs associated with poor
peripheral perfusion such as hypotension, tachycardia, cool
extremities, oliguria, and altered mental status are usually
present. The presence of distended neck veins is central to the
diagnosis, although they may be absent if the patient is hypo-
volemic. When tension pneumothorax is the cause, hyperres-
onance is noted on thoracic percussion, breath sounds are
absent on the affected side, and the mediastinum is shifted
away from the involved chest. Displacement of the trachea in
association with distended neck veins is pathognomonic of
tension pneumothorax. For patients who are breathing spon-
taneously, inspiration increases the degree of venous disten-
tion (Kussmaul’s sign). Paradoxic pulse also may occur with
spontaneous breathing and consists of a decrease in systolic
pressure of more than 10 mm Hg with inspiration.
When cardiac compressive shock occurs after injury, pen-
etrating trauma to the chest is usually present. Pericardial
tamponade is uncommon after blunt injuries. Patients
admitted for exacerbations of chronic disease often have a
history of pericardial effusion. When mechanical ventilation
is used, cardiac compressive shock occurs because (1) the
inflated lungs compress the superior and inferior venae
cavae, (2) the right atrium and ventricle are compressed, and
(3) expansion of the lungs compresses the pulmonary vascu-
lature and increases the resistance to right ventricular ejec-
tion. Hypotension and tachycardia worsen in these patients
as PEEP is increased. The correlation between the two may
not be apparent at first, although careful examination of the
patient’s flowsheet will reveal changes in hemodynamics that
correspond to ventilator manipulations.
B. Hemodynamic Monitoring—Central venous pressure is
increased, as are pulmonary artery and pulmonary capillary
wedge pressures. Equalization of central venous pressure,
pulmonary artery, and pulmonary capillary wedge pressures
strongly suggests pericardial tamponade.
C. Imaging Studies—Upright posteroanterior chest radi-
ographs may show an enlarged cardiac shadow, but this is
nonspecific. If tension pneumothorax is suspected, treatment

CHAPTER 11
246
must not be delayed while x-rays are obtained. If an inciden-
tal chest radiograph is available, it will reveal hyperlucency of
one or both hemithoraces with displacement of the mediasti-
nal structures to the contralateral side. Transesophageal two-
dimensional echocardiography is very sensitive and can be
used to establish the diagnosis in nonemergent situations.
Treatment of suspected decompensated traumatic pericar-
dial tamponade should never be postponed while awaiting
imaging studies.
Differential Diagnosis
Primary cardiogenic shock without compression presents
the major differential dilemma because both types present
with low cardiac output and high venous pressure. An acute
myocardial infarction or progressive deterioration in a criti-
cally ill patient suggests cardiogenic shock. Most patients
who develop tension pneumothorax or pericardial tampon-
ade after injury will have had the diagnosis established and
therapy instituted before arrival in the critical care unit.
Missed injuries occur occasionally and must be differentiated
from traumatic air embolism to the coronary arteries. The
latter usually causes severe dysrhythmias and a rapid down-
hill course.
Treatment
A. Fluid Resuscitation—Rapid fluid infusion may tran-
siently compensate for the decrease in ventricular filling.
Central venous pressure cannot be used to guide such infu-
sion because central venous pressure always will be elevated
prior to the administration of fluid.
B. Operative Treatment—Surgical decompression of the
offending site is indicated. For tension pneumothorax,
immediate insertion of a large-bore intravenous catheter into
the affected hemithorax will rapidly release the increased
pressure. After pulse and blood pressure return to normal,
this small catheter can be replaced with a larger tube thora-
costomy connected to a chest evacuation device. Placement
of the smaller catheter never should be delayed pending pro-
curement and placement of a more definitive thoracostomy
tube. If cardiac compression is due to gastric distention,
placement of a nasogastric tube may be helpful. When dis-
tention is due to other causes, surgical exploration is usually
warranted. Pericardial decompression should be performed
for pericardial tamponade. Reduction of ventilatory pres-
sures and augmentation of the circulating blood volume, if
possible, usually correct compression resulting from the use
of PEEP.
