Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

198 Section III • The Esophagus
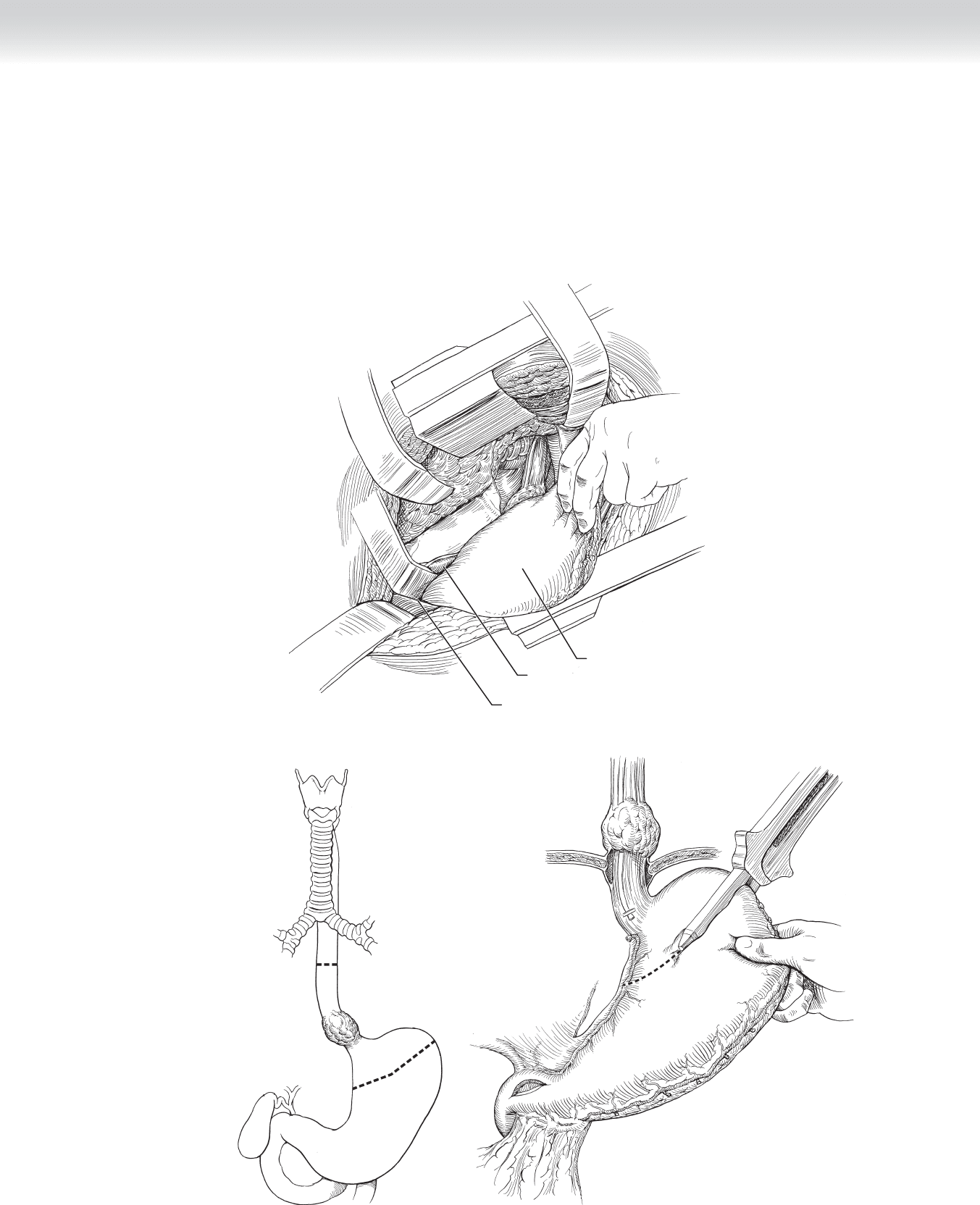
◆ The stomach, which has been previously mobilized, should be gently elevated into the
chest (Figure 17-5).
◆ An endoscopic gastrointestinal anastomosis (GIA) stapling device is used to resect the cardia
and proximal fundus along the lesser curve with at least a 5-cm margin. This staple line can
be oversewn with interrupted 3-0 silk Lembert stitches (Figure 17-6).
Liver
Cut edge of diaphragm
Stomach
FIGURE 17 –5
B
A
FIGURE 17 –6
CHAPTER 17 • Esophagectomy—Transthoracic (Ivor Lewis) 199
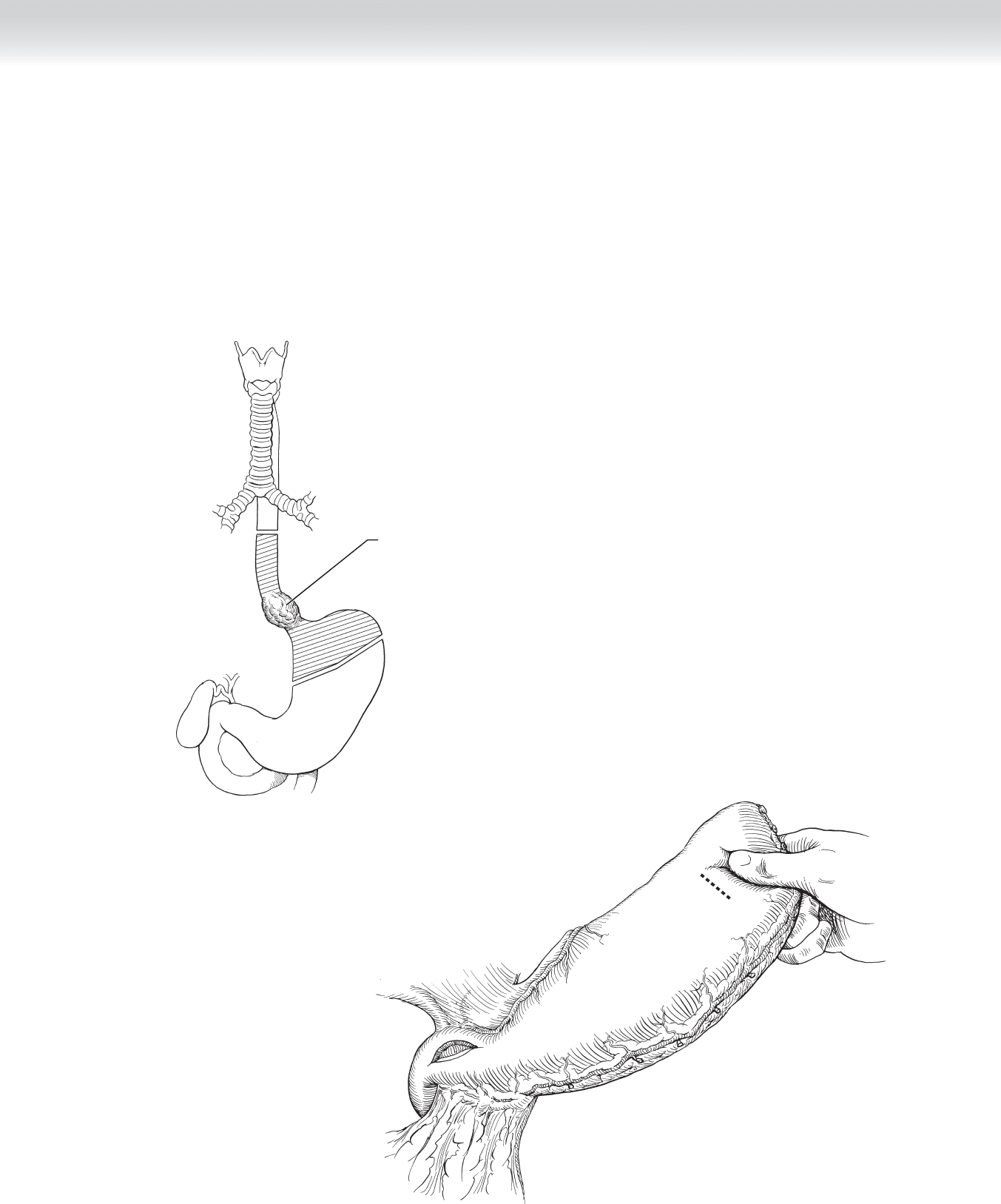
◆ The stomach is placed as high in the chest cavity as possible to avoid undue tension at the
anastomotic site. A stapled anastomosis using an end-to-end anastomosis (EEA) stapling
device can be used via a 1.0- to 1.5-cm gastrotomy or, alternatively, a hand-sewn
anastomosis can be performed. The hand-sewn anastomosis is performed in two layers.
First, the posterior row of interrupted 3-0 silk stitches is placed between the posterior wall
of the esophagus, approximately 0.5 to 1.0 cm proximal to the cut end of the esophagus
and the fundus of the stomach (Figures 17-7 and 17-8).
Tumor removed along
with portions of esophagus
and fundus of stomach
FIGURE 17 –7
FIGURE 17 –8
200 Section III • The Esophagus
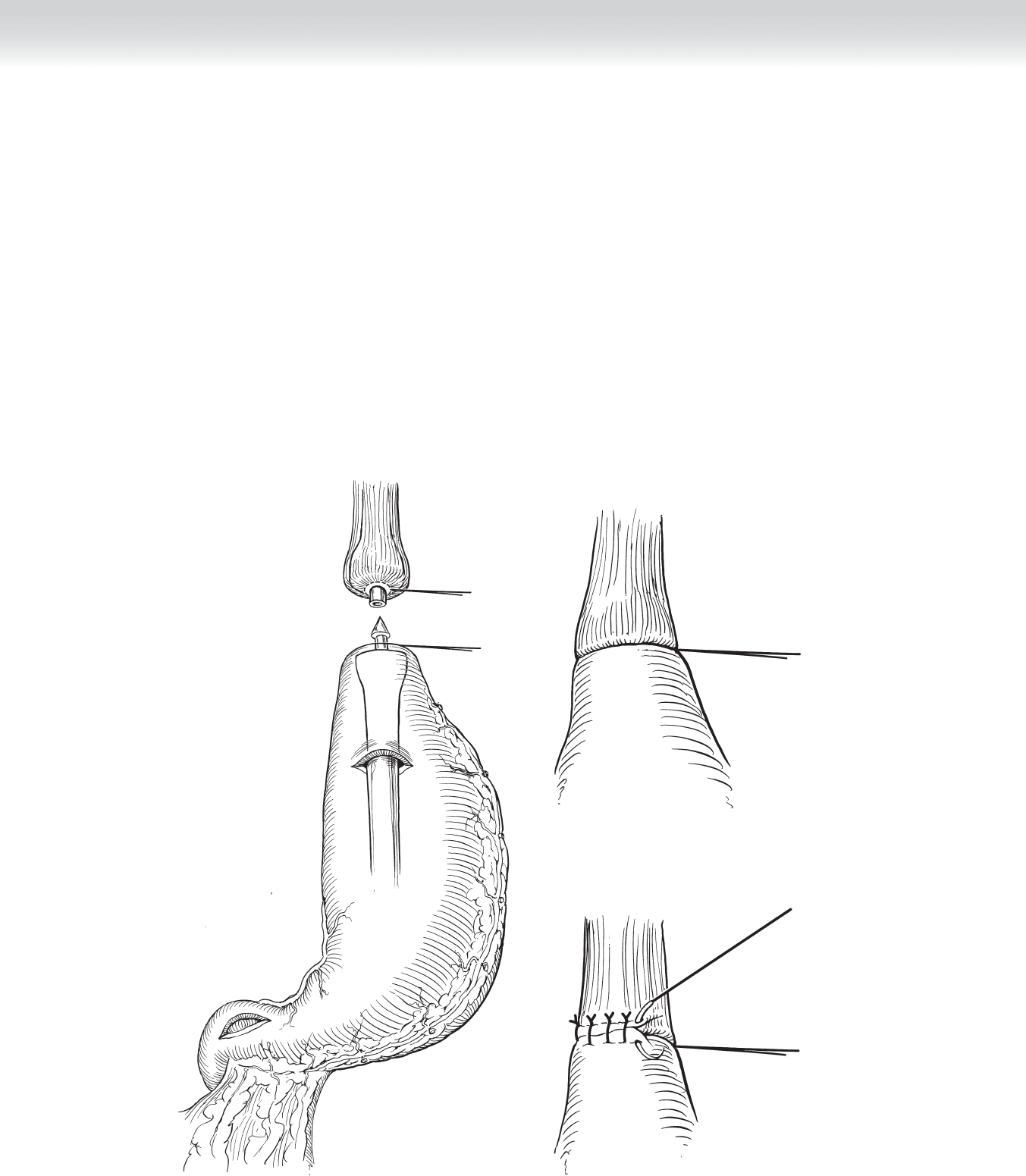
◆ At this point, the anesthesiologist places a nasogastric tube as the surgeon guides it from the
esophagus, through the gastrotomy, and into the stomach. A running 4-0 absorbable suture
is used to perform the mucosa-mucosa anastomosis. An anterior row of interrupted 3-0 silk
Lembert stitches completes the anastomosis (Figure 17-9).
◆ The stomach should be tacked to the prevertebral fascia and esophageal hiatus with inter-
rupted 3-0 silk stitches once the anastomosis is complete. A 36F chest tube is placed into
the right side of the chest and exited through a separate stab incision below the thoracotomy.
A
B
C
FIGURE 17 –9
CHAPTER 17 • Esophagectomy—Transthoracic (Ivor Lewis) 201
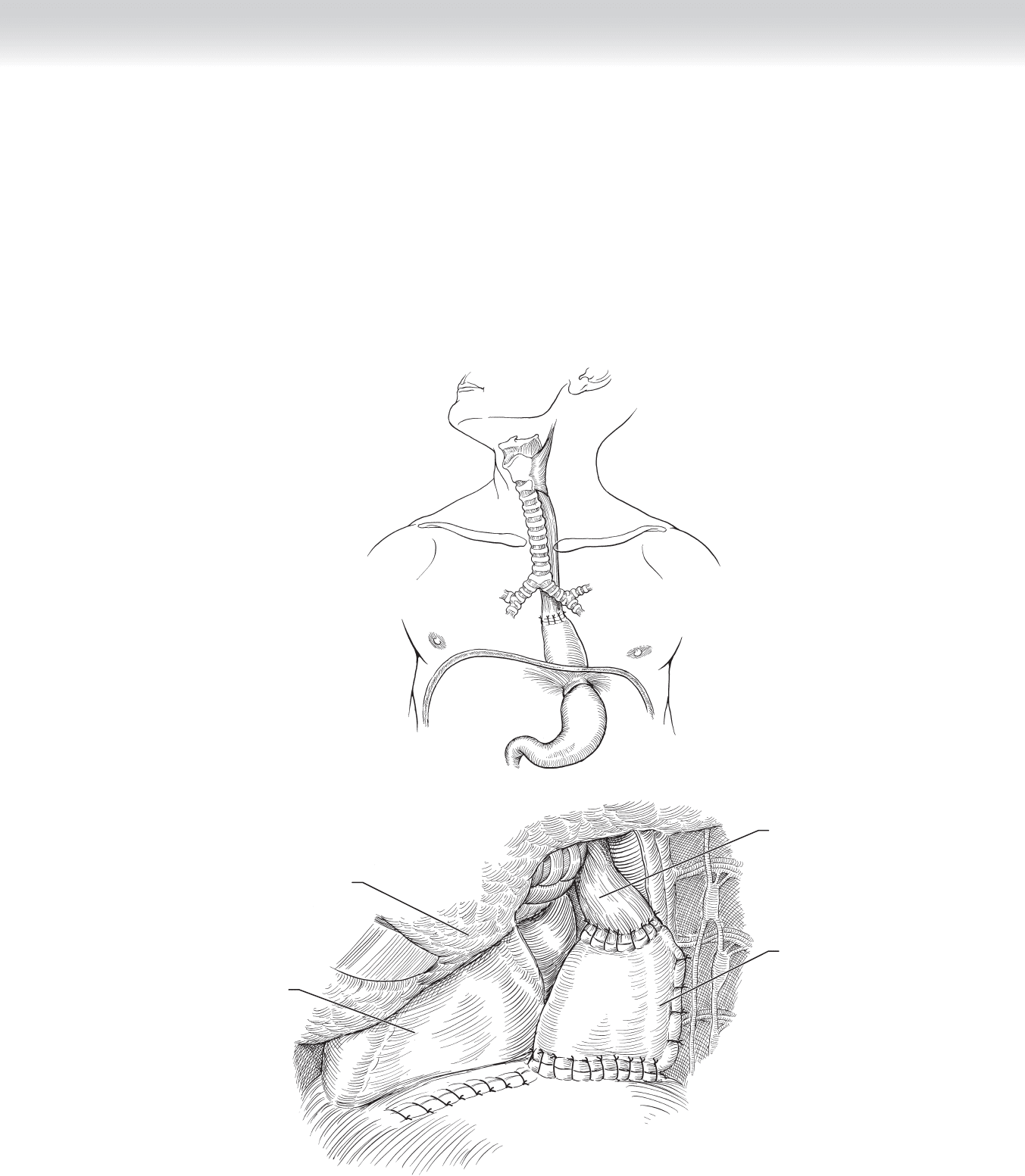
3. CLOSING
◆ The abdominal incision is closed according to surgeon preference. The fascia is usually
closed with a no. 0 or no. 1 interrupted or running absorbable monofi lament suture, and
skin is closed with staples. The thoracotomy is closed with interrupted no. 1 or no. 2
Vicryl fi gure-of-eight stitches. Muscle layers are individually reapproximated with running
2-0 Vicryl suture, and the skin is closed with staples or running 4-0 absorbable suture.
Sterile dressings are applied (Figure 17-10).
A
B
Stomach
Esophagus
Left lung
Heart
FIGURE 17 –10

202 Section III • The Esophagus
STEP 4: POSTOPERATIVE CARE
◆ Routine intensive care unit monitoring is not mandatory following transthoracic esophagec-
tomy, but the decision is made for each individual based on length of operation, surgeon
preference, patient comorbidities, and blood loss. On postoperative day 4 or 5, a contrast
esophageal swallow study is performed to evaluate the anastomosis for leak. If no leak is
present, a diet is initiated and output from the chest tube is monitored. Assuming no
increase in output with feeding and a fully expanded lung and drained right hemithorax,
the chest tube can be removed. Ambulation and chest physiotherapy should be initiated on
postoperative day 1 and continued until discharge.
STEP 5: PEARLS AND PITFALLS
◆ Identify and preserve the right gastric and right gastroepiploic arteries when mobilizing the
stomach.
◆ Test the esophagogastric anastomosis under water before closing to ensure no gross anasto-
motic dehiscence is present.
◆ Avoid injury to the posterior membranous trachea during esophageal mobilization.
◆ Act quickly to ensure adequate drainage of the thorax and mediastinum if signs of anasto-
motic leak occur in the postoperative period.
SELECTED REFERENCES
1. Junginger T, Gockel I, Heckhoff S: A comparison of transhiatal and transthoracic resections on the prog-
nosis in patients with squamous cell carcinoma of the esophagus. Eur J Surg Oncol 2006;32:749-755.
2. Hulscher JB, van Sandick JW, de Boer AG, et al: Extended transthoracic resection compared with limited
transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med 2002;347:1662-1669.
203
CHAPTER
18
Esophagogastrectomy
Joseph B. Zwischenberger and Edward Y. H. Chan
STEP 1: SURGICAL ANATOMY
◆ A comprehensive understanding of the anatomy of the thorax, esophagus, stomach, and
abdomen is critical before undertaking surgical procedures on the esophagus and stomach.
STEP 2: PREOPERATIVE CONSIDERATIONS
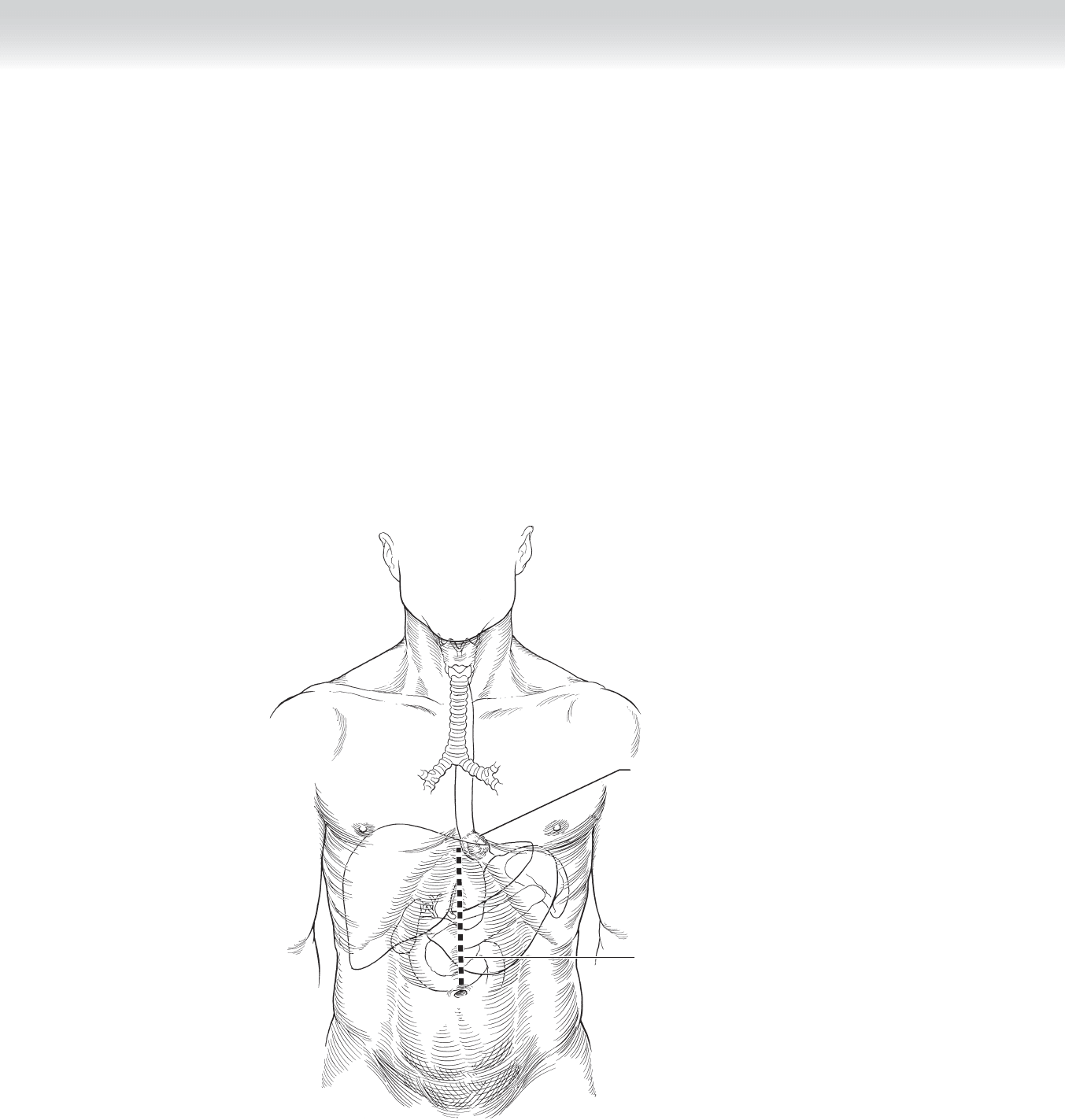
◆ Indications: Indications for esophagogastrectomy include malignant tumor of the lower
esophagus or esophagogastric junction, which precludes a clear tumor margin to allow use
of the stomach for esophageal reconstruction. Malignancies of the esophagogastric junction
are most commonly adenocarcinomas of gastric origin (Figure 18-1).
◆ A left thoracoabdominal approach is indicated if the tumor location necessitates resection
of the distal esophagus and proximal stomach and when a Roux-en-
Y anastomosis is to be
used to reconstruct the resected stomach. If removal of the proximal stomach only is re-
quired to obtain adequate surgical margins, an anastomosis may be made between the
distal stomach and the esophagus in the chest. However, this reconstructive approach
may be associated with refl ux esophagitis and dysphagia. Some surgeons prefer the alter-
native of a total resection of the stomach and distal esophagus with a Roux-en-
Y jejunal
interposition with an end-to-end anastomosis with the remaining esophagus. For a total
esophagogastrectomy, a colon interposition is required. A double-contrast barium enema
and colonoscopy will aid selection of the right (preferred), transverse, or left colon.
During the procedure, length and blood supply also infl uence colon selection.
◆ Preoperative planning: Informed consent is obtained and the patient is made nothing-by-
mouth status at least 8 hours before the procedure. A bowel preparation is necessary the
day before the procedure in case the colon is needed as a reconstruction conduit. In the
operating room, a radial artery catheter should be used for continuous blood pressure
monitoring. Central venous access is not routinely necessary; however, if access is needed,
the right neck veins should be used to allow the surgeon complete access to the left side of
the neck during operation. A double-lumen endotracheal tube is used to defl ate and retract
either lung to facilitate dissection. If a colonic interposition is planned, mesenteric angiography
should be performed on patients with risk factors for atherosclerotic disease.
204 Section III • The Esophagus
◆ Anesthesia: General endotracheal anesthesia is mandatory for this procedure.
◆ Position: The patient is placed in the right lateral (left thoracoabdominal) position.
◆ Operative preparation: The skin over the entire neck, chest, and abdomen should be
prepped with povidone-iodine (Betadine).
Tumor in
distal esophagus
Incision
MC
FIGURE 18 –1
CHAPTER 18 • Esophagogastrectomy 205
STEP 3: OPERATIVE STEPS
1. INCISION
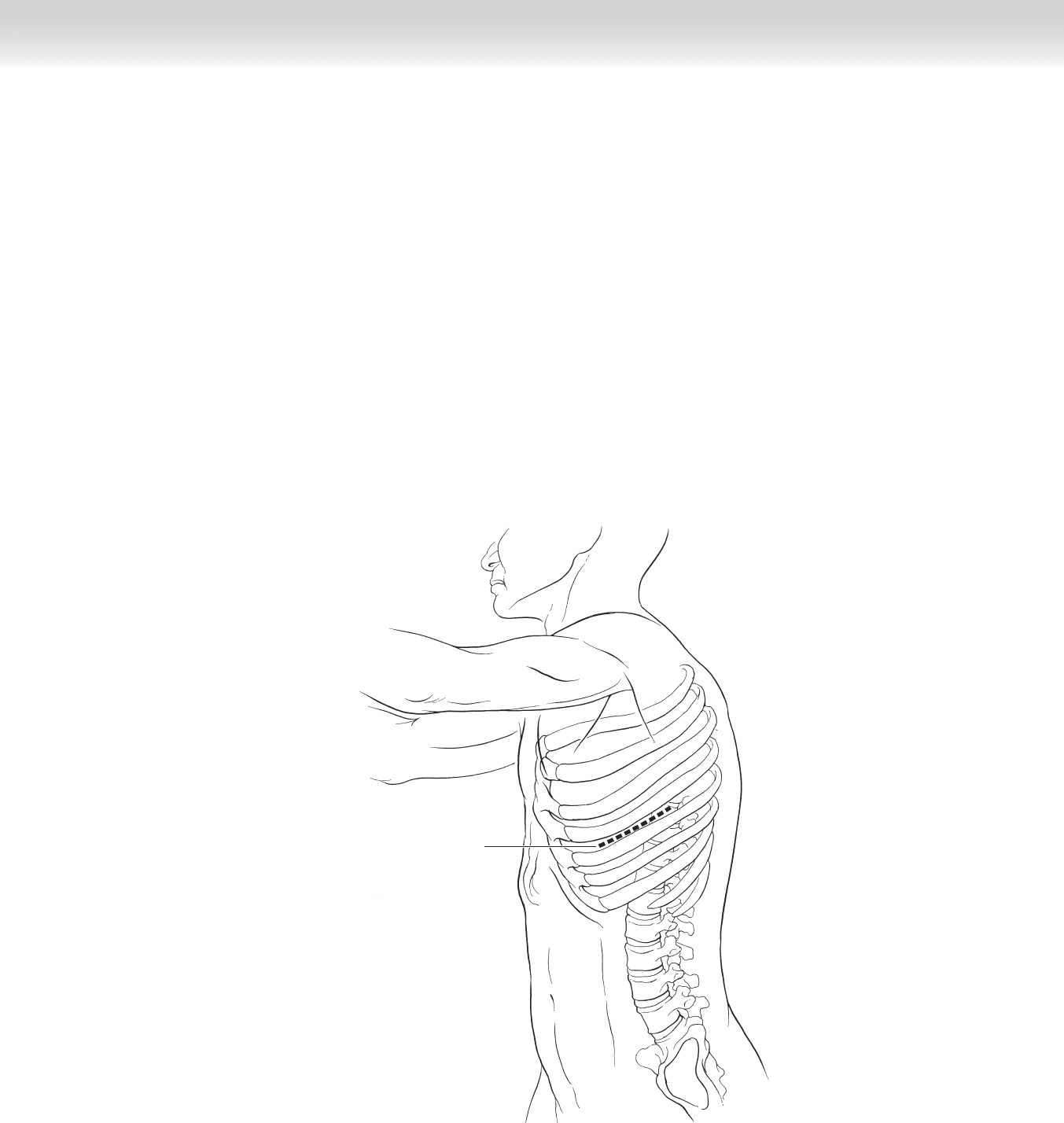
◆ Incision and exposure: A left thoracotomy is performed between the sixth and seventh
ribs. The serratus anterior muscle is separated to expose the intercostal muscles, which are
removed from the superior aspect of the seventh rib to enter the chest (Figure 18-2).
◆ A thoracoabdominal incision may provide greater exposure. However, this approach leads
to longer operative time and may result in an unstable costal arch, chondritis, or persistent
pain. A separate midline abdominal incision is often better tolerated (see Figure 18-1).
Incision
FIGURE 18 –2

206 Section III • The Esophagus
2. DISSECTION
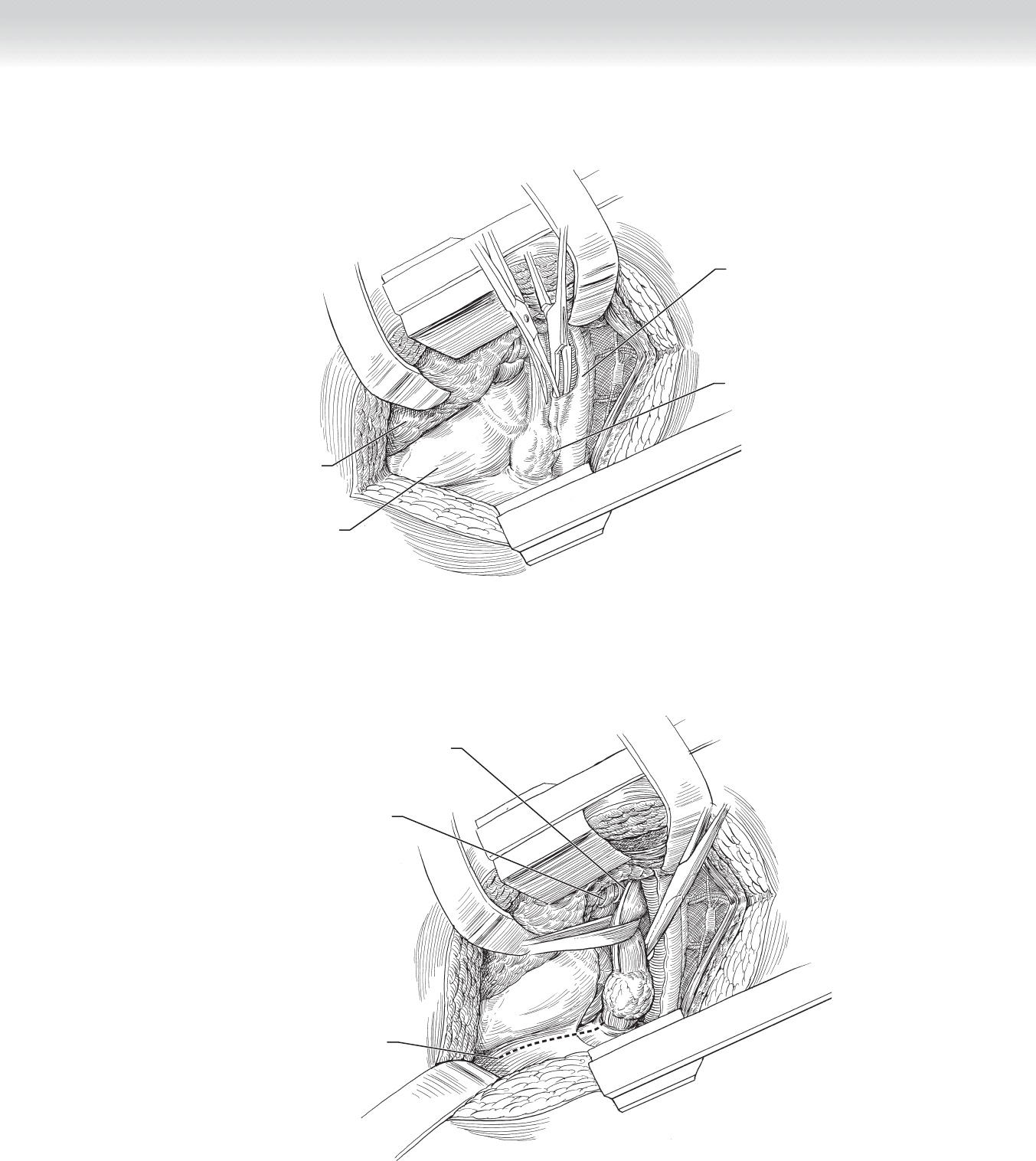
◆ Diaphragm incision: The left thorax is entered and a semilunar incision is made in the
diaphragm near the costal arch, 2 cm from the costal margin. Retraction of the cut edge
of the diaphragm exposes the left lobe of the liver and the left upper abdomen. Radial
incisions may be made to expose and resect the adjacent diaphragm to achieve tumor-free
margins when the tumor invades the crus. Crural resection has a greater risk of diaphrag-
matic paralysis postoperatively (Figures 18-3 and 18-4).
◆ The abdomen should be carefully examined for peritoneal or hepatic metastases. The cardia
of the stomach should be palpated through the lesser sac, and the mobility of the tumor
should be assessed. If there are metastases or the tumor is fi xed to the aorta or spine, the
tumor is not resectable.
◆ Esophageal mobilization: The pleura of the mediastinum is opened with visualization
of the esophagus and the esophageal tumor. Mobilization of the esophagus from the aorta is
achieved and the esophagus proximal to the tumor is encircled by a Penrose drain. The
surgeon must identify the anterior vagus nerve and the left bronchus and pulmonary vein.
The esophageal vessels should be dissected, ligated, and divided. To provide local clearance
of the tumor, the surgeon should take 1 cm of the crura in continuity with the
tumor (see Figure 18-4).
CHAPTER 18 • Esophagogastrectomy 207
Tumor in
distal esophagus
Esophageal tumor
Left lung
Heart
FIGURE 18 –3
Incision in diaphragm
Anterior vagus nerve
Left bronchus and
pulmonary vein
FIGURE 18 –4
