Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.


228 Section III • The Esophagus
STEP 4: POSTOPERATIVE CARE
◆ After recovery from anesthesia, the patient can be taken to a fl oor bed.
◆ The patient should be encouraged to ambulate as early as postoperative day 1. Incentive
spirometry and good pulmonary physiotherapy are essential.
◆ The nasogastric tube may be removed on the second postoperative day, and jejunostomy
tube feedings are started. Sips of clear liquids may be allowed when bowel function normal-
izes. Between postoperative days 5 and 7, a barium swallow should be performed to evalu-
ate the anastomosis. If the anastomosis is intact, a soft diet is started. As diet is advanced,
bulky food and carbonated beverages should be avoided.
STEP 5: PEARLS AND PITFALLS
◆ When using a jejunal graft, one should be prepared to substitute a colonic graft if the jeju-
num is inadequate, either because the length is insuffi cient to replace the full length of the
esophagus or because the blood supply is damaged during harvesting.
◆ Studies comparing the quality of life of patients after esophagectomy with age-matched con-
trols demonstrated no signifi cant differences in outcomes between the populations.
SELECTED REFERENCES
1. Meneshian A, Heitmiller RF: Surgical management of esophageal cancer. In Yuh D (ed): Johns Hopkins
Manual of Cardiothoracic Surgery. New York, McGraw-Hill, 2007, pp 273-294.
2. Deschamps C, Nichols FC III, Cassivi SD, et al: Long-term function and quality of life after esophageal
resection for cancer and Barrett’s. Surg Clin North Am 2005;85:649-656.
3. Linden PA, Swanson SJ: Esophageal resection and replacement. In Sellke F (ed): Sabiston & Spencer:
Surgery of the Chest. Philadelphia, Elsevier, 2005, pp 627-651.
229
STEP 1: SURGICAL ANATOMY
◆ A comprehensive understanding of the anatomy of the thorax and esophagus is critical
before undertaking surgical procedures on the esophagus.
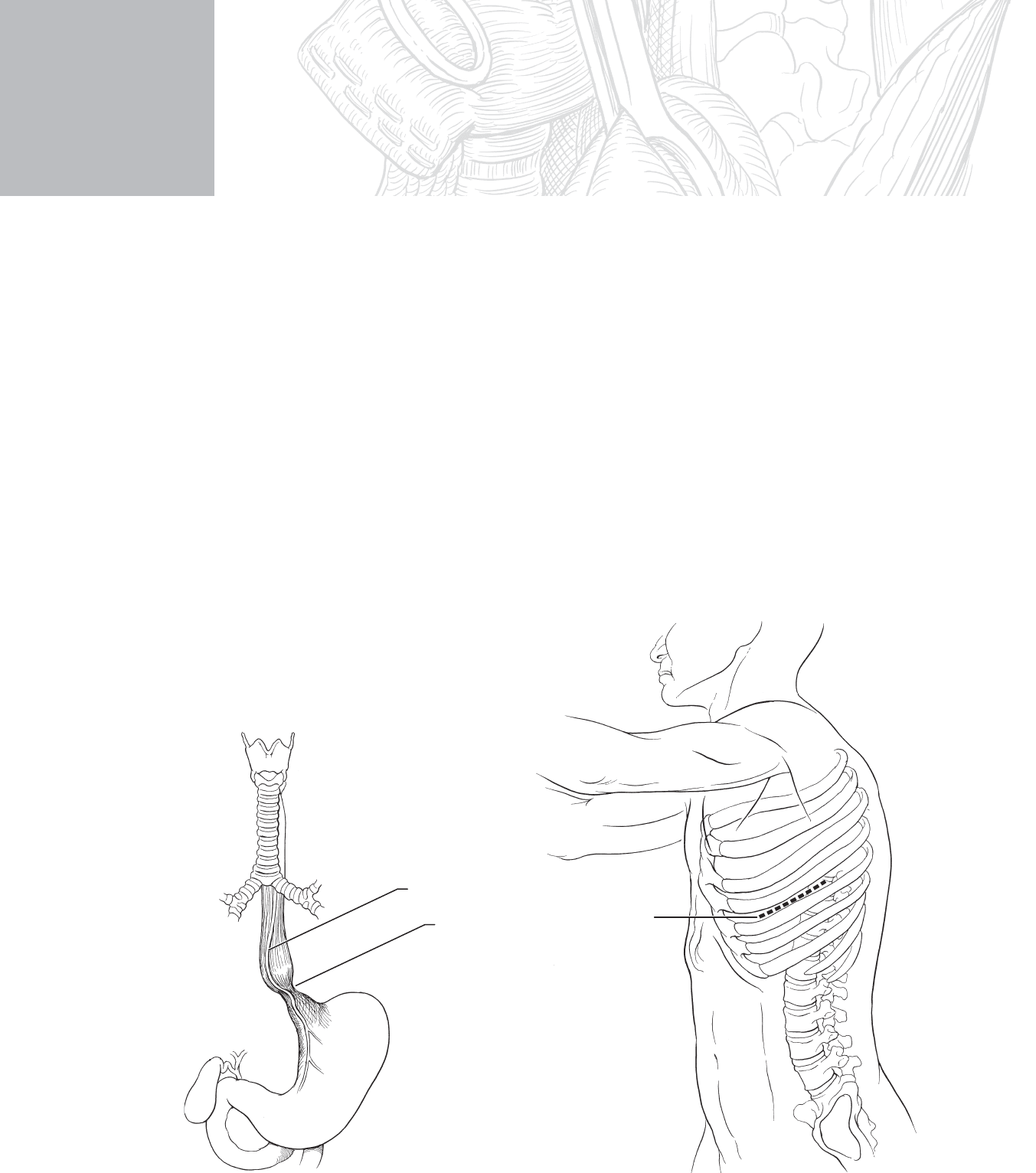
◆ Figure 19-1, A, demonstrates key anatomic structures that must be considered in an open
Heller myotomy.
Anterior vagus nerve
Stenotic distal
esophagus
MC
A
Incision
B
FIGURE 19 –1
CHAPTER
19
Open Heller Myotomy
David B. Loran and Joseph B. Zwischenberger

230 Section III • The Esophagus
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ The word achalasia means “failure to relax,” which characterizes the pathophysiologic
dysfunction of the lower esophageal sphincter in this disease. The sustained high-pressure
zone is believed to be due to denervation or dysfunction of the nerves in Auerbach’s plexus,
which leads to the loss of inhibitory effects of these ganglia on the muscles of the lower
esophageal sphincter. Initiation of swallowing is normal; however, the esophagus cannot
empty properly, which leads to varying degrees of dysphagia. Typical symptoms include
odynophagia, foul breath, regurgitation of undigested food, and the patient describing a
sensation of food “getting stuck” in his or her lower chest. Late symptoms result from the
sequelae of continued aspiration and include hoarseness, pneumonitis, pneumonia, and
lung abscess.
◆ Diagnosis is based on patient symptoms and objective testing. Barium esophagram will
show a mild to severely dilated esophageal body with a characteristically smooth “bird-
beak” tapering at the distal esophagus. Manometry is the gold standard for diagnosis of
achalasia and will show a loss of propulsive contractions in the esophageal body. Resting
pressures at the lower esophageal sphincter can be normal to elevated with incomplete or
completely absent relaxation upon swallowing. Esophagoscopy with biopsy is sometimes
needed to rule out distal esophageal stricture due to esophagitis or carcinoma, which can
mimic achalasia.
◆ Once the diagnosis of achalasia is made, treatment usually begins with nonsurgical thera-
pies. Botulinum toxin injected via an endoscope into the area of the lower esophageal
sphincter can relieve symptoms in 50% to 65% of patients for as long as 18 months. Most
have recurrence of symptoms beyond this time. Pneumatic or forceful bougie dilation of
the lower esophageal sphincter has a long-term success rate approaching 70%. The gold
standard for treatment of achalasia is surgical myotomy, with long-term success rates of
90% to 95%. Patients are usually treated with one or two attempts of nonsurgical therapies
before being referred to a surgeon for myotomy. Those who are poor surgical candidates can
be treated nonsurgically indefi nitely.
◆ Informed consent is obtained from the patient who is given nothing by mouth 8 hours
before the procedure.
◆ General endotracheal anesthesia is administered for this procedure.
◆ The patient is placed in the lateral decubitus position with the right side down and secured
to the operating table. The bed can be bent at the seventh to eighth intercostal space to
facilitate exposure.
◆ The skin is prepped with povidone-iodine (Betadine), from the top of the shoulder
superiorly to the iliac crest inferiorly, then between the midline anteriorly and spinous
processes posteriorly.

CHAPTER 19 • Open Heller Myotomy 231
STEP 3: OPERATIVE STEPS
1. INCISION
◆ A muscle-sparing minithoracotomy incision measuring 8 to 10 cm is placed in the seventh
intercostal space (Figure 19-1, B). The serratus anterior muscle is separated to expose the
intercostal muscles, which are removed from the superior aspect of the eighth rib to enter
the chest. A rib retractor is placed.
2. DISSECTION
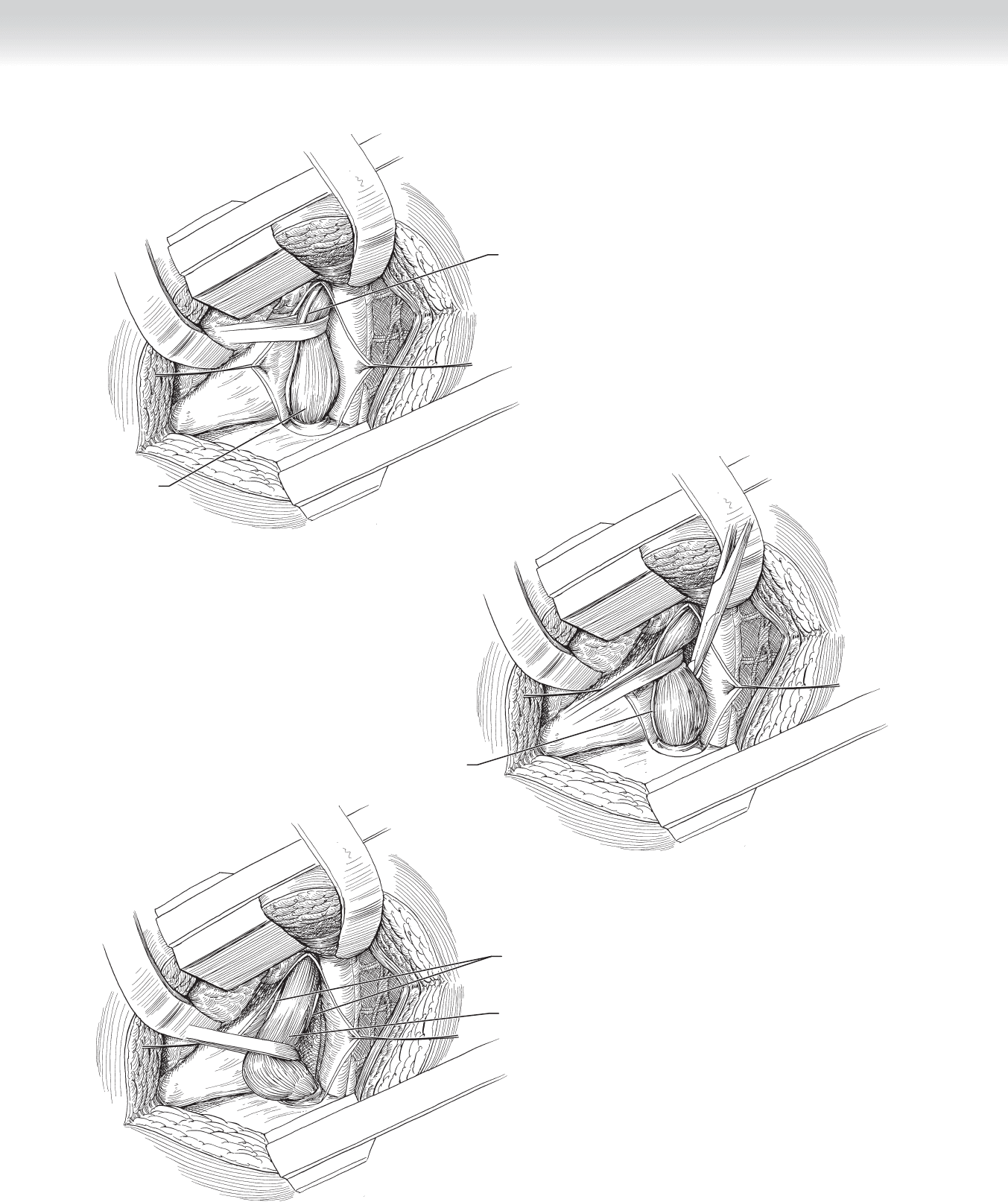
◆ A size 40F to 44F bougie or Maloney dilator is placed by the anesthesiologist to facilitate
dissection. The inferior pulmonary ligament is divided and the lung is retracted cephalad. The
mediastinal pleura overlying the esophagus is incised from the gastroesophageal junction to
the inferior pulmonary vein to expose the esophagus. This segment of esophagus is mobilized
anteriorly if only a myotomy is planned or is completely mobilized and encircled with a
Penrose drain if an antirefl ux procedure is added to the myotomy (Figure 19-2).
◆ Care should be taken during this dissection not to injure either vagus nerve located at the
lateral margins of the distal esophagus. Usually the vagus nerves are adherent and should
not be mobilized (see Figure 19-2, B-C).
232 Section III • The Esophagus
Anterior/posterior
vagus nerve
Esophagus mobilized
C
FIGURE 19 –2
Anterior
vagus nerve
B
Anterior vagus
nerve
Bulge in
esophagus
A
CHAPTER 19 • Open Heller Myotomy 233
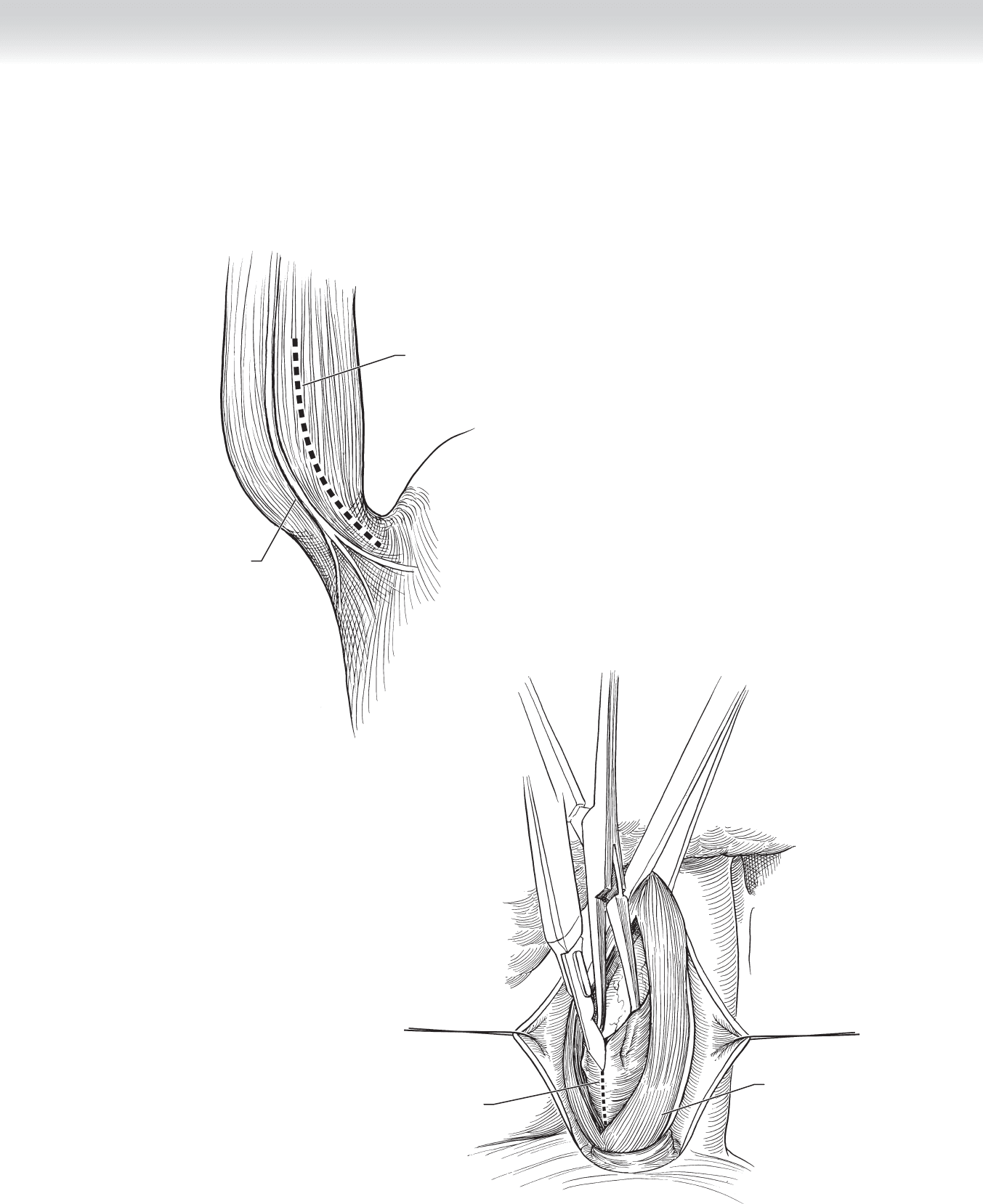
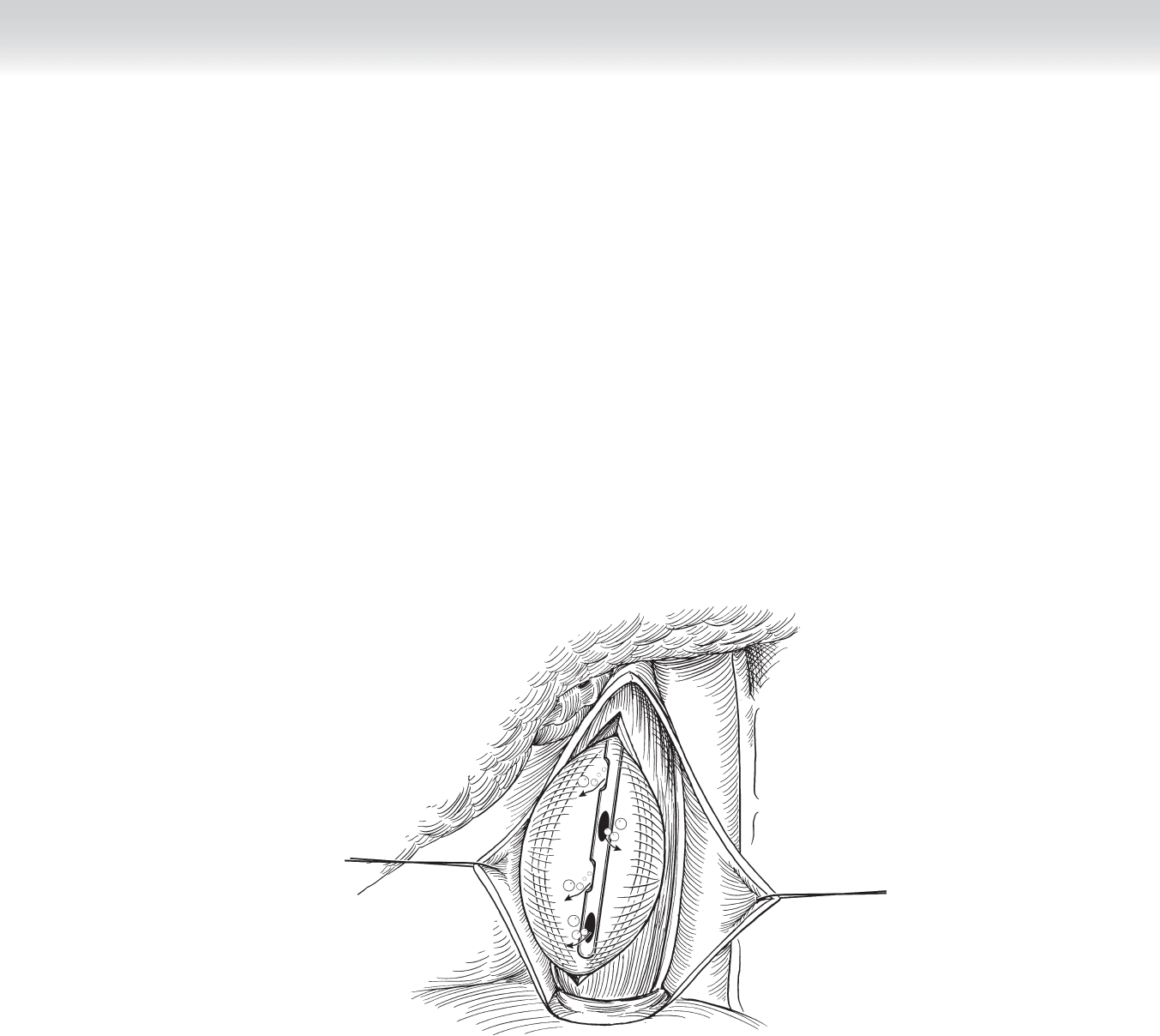
◆ The esophageal musculature is incised from the inferior pulmonary vein to the esopha-
geal hiatus and extended onto the cardia of the stomach for approximately 1 to 2 cm
(Figure 19-3).
Longitudinal muscle
B
Incision through circular muscle
Incision
Anterior vagus
nerve
A
FIGURE 19 –3
234 Section III • The Esophagus
◆ The esophageal muscle is gently divided longitudinally until the mucosa is seen to bulge
from underneath (Figure 19-4).
◆ A right-angle clamp or peanut dissector is used to raise the muscular wall from the mucosa
over approximately 50% of the esophageal circumference. Care must be taken not to enter
the esophageal lumen through the mucosa.
Submucosa
A
Submucosa
B
Circular
muscle
Longitudinal
muscle
FIGURE 19 –4
CHAPTER 19 • Open Heller Myotomy 235
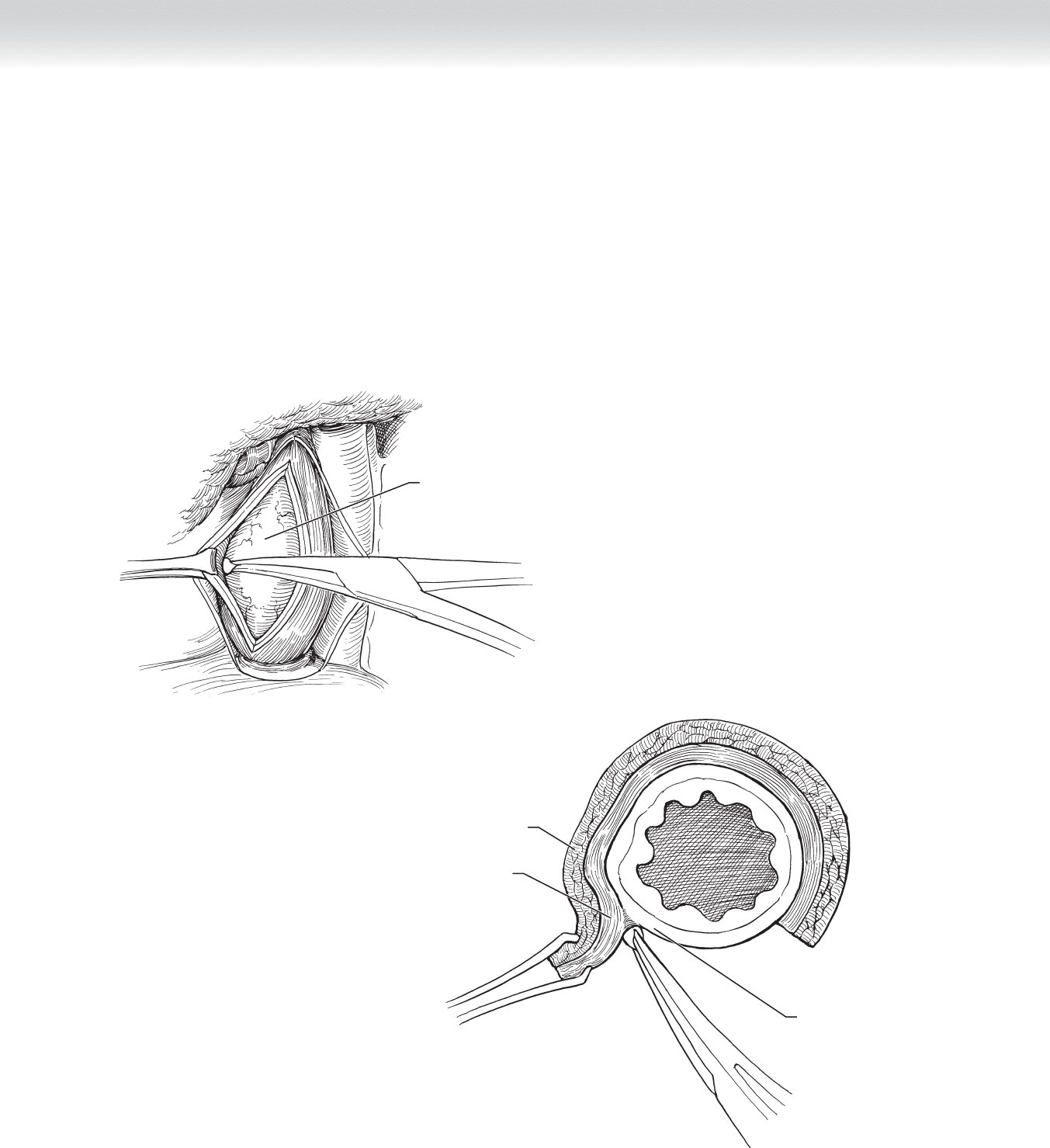
◆ For the surgeon to inspect mucosal integrity, the bougie can be removed from the esopha-
gus upon completion of the myotomy and replaced by a nasogastric (NG) tube. The chest
cavity is fi lled with saline irrigation while the anesthesiologist gently injects air through the
NG tube and the surgeon looks for air bubbles. If no air bubbles are seen, the Penrose drain
is removed and the esophagus returns to its normal position (Figure 19-5). If the mucosa
has been violated, the defect should be closed primarily with absorbable suture reapproxi-
mating the muscle fi bers. An opposite site is then used for the myotomy.
◆ Following completion of the myotomy, a chest tube is placed in the pleural space and
exited through a separate incision in the lateral chest wall.
FIGURE 19 –5
236 Section III • The Esophagus
FIGURE 19 –6
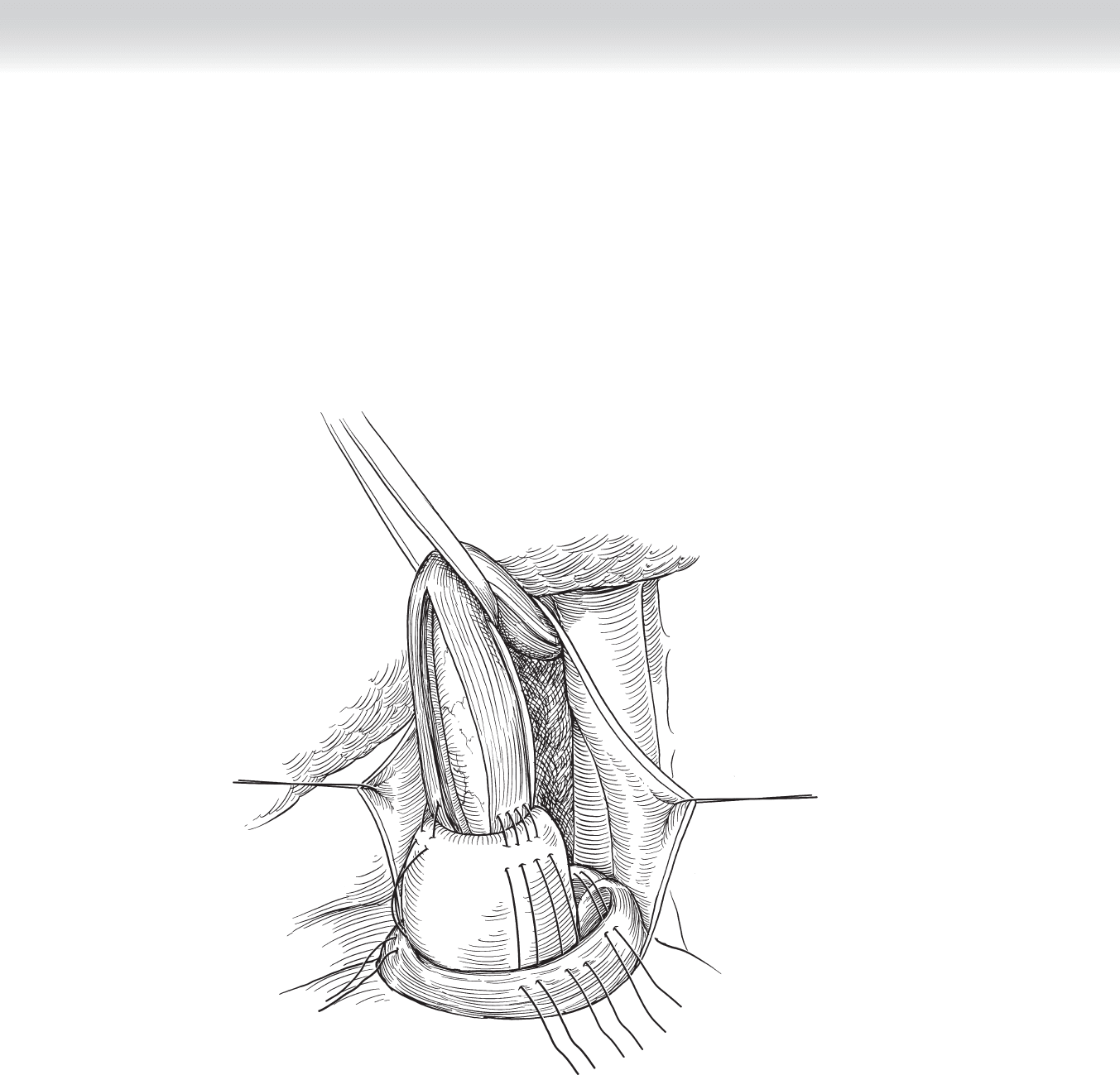
◆ Antirefl ux procedure, if added, is either a Belsey Mark IV (270 degree), Nissen (360 degree),
or Dor (180 degree). Most surgeons add an antirefl ux procedure but no individual technique
has proven superior (Figure 19-6).
CHAPTER 19 • Open Heller Myotomy 237
3. CLOSING
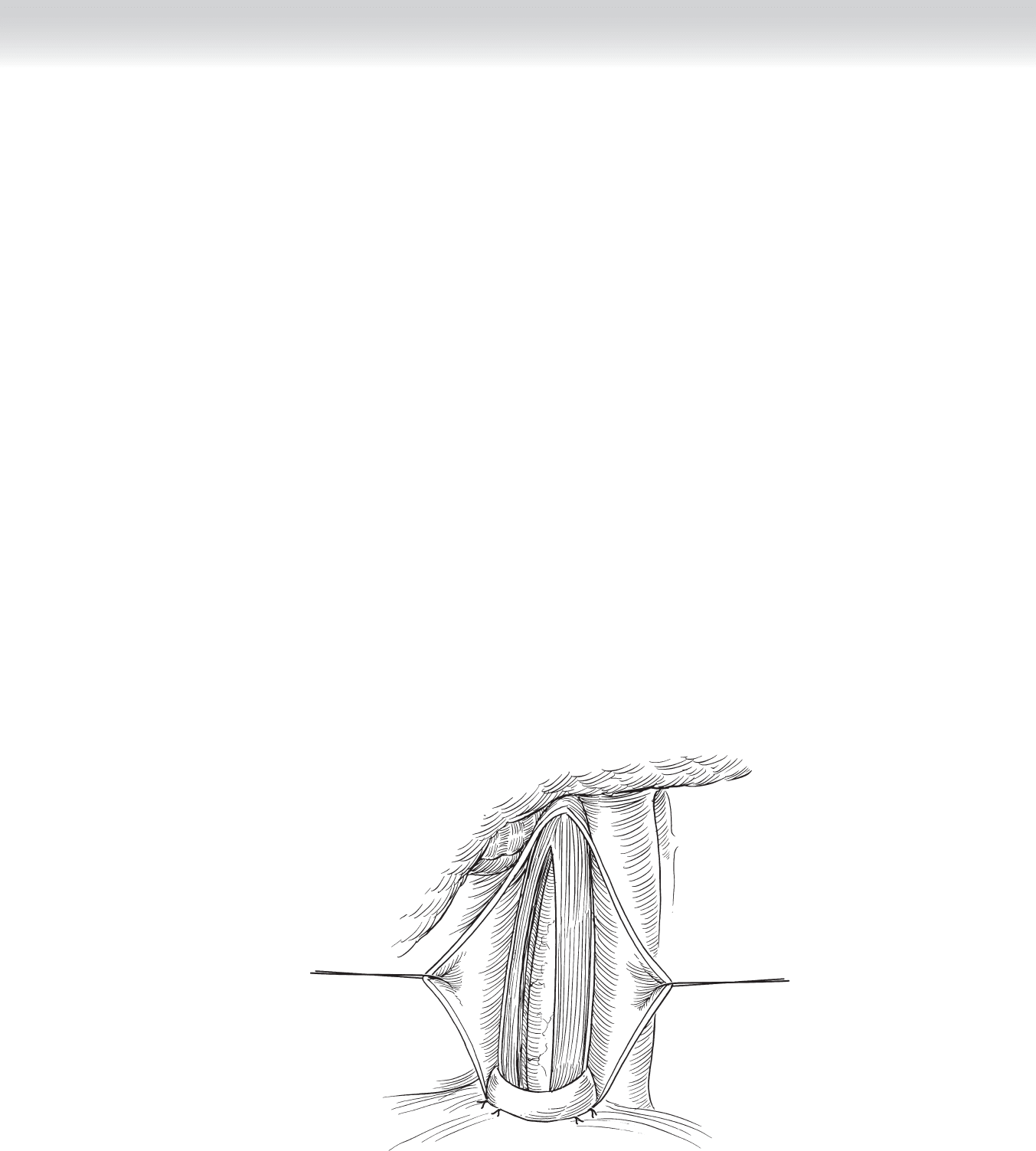
◆ The rib retractor is removed, and interrupted 0 Vicryl sutures are placed around the sev-
enth and eighth ribs for closure of the chest cavity. Muscle layers are reapproximated with
running 2-0 absorbable suture. The skin is closed with staples or a running 4-0 absorbable
stitch. The chest tube is secured with a 2-0 silk drain stitch (Figure 19-7).
STEP 4: POSTOPERATIVE CARE
◆ After recovery from anesthesia, the patient can be taken to a fl oor bed.
◆ The chest tube should initially be placed to 15 to 20 cm H
2
0 wall suction and the patient
kept NPO.
◆ On the second postoperative day, a contrast esophagram is obtained to ensure there is no
leak from the myotomy site. With no leak present, a diet is initiated. If no esophageal leak
is found, the lung is fully expanded. If there is no air leak present in the chest tube, the
tube is removed. Patients are usually ambulatory by the second postoperative day and dis-
charged to home by the third postoperative day.
FIGURE 19 –7
