Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.


238 Section III • The Esophagus
STEP 5: PEARLS AND PITFALLS
◆ Without fundoplication, approximately 60% of patients report symptoms of refl ux, most of
which can be managed medically. Most surgeons therefore add an antirefl ux procedure to
the myotomy. No technique has proven superior, but most avoid a 360-degree fundoplica-
tion because of its higher rate of dysphagia.
◆ In prospective studies, laparoscopic Heller myotomy has been shown to achieve comparable
outcomes with open surgery, with longer operative time and shorter hospital stay. Long-
term follow-up has demonstrated satisfactory outcomes in 80% to 90% of cases.
◆ Patients with esophageal dilation of up to 6 cm have had patient satisfaction of greater than
90% from laparoscopic Heller myotomy.
◆ Patients with a sigmoid esophagus should be considered for myotomy fi rst, then esophagec-
tomy if symptoms do not resolve. Studies have demonstrated good to excellent patient sat-
isfaction in 54% to 71% of patients at 7 to 11 years follow-up with myotomy of the
sigmoid esophagus.
SELECTED REFERENCES
1. Tsiaoussis J, Athanasakis E, Pechlivanides G, et al: Long-term functional results after laparoscopic surgery
for esophageal achalasia. Am J Surg 2007;193:26-31.
2. Constantini M, Zaninotto G, Guirroli E, et al: The laparoscopic Heller-Dor operation remains an effective
treatment for esophageal achalasia at a minimum 6-year follow-up. Surg Endosc 2005;19:345-351.
3. Bonatti H, Hinder RA, Klocker J, et al: Long-term results of laparoscopic Heller myotomy with partial
fundoplication for the treatment of achalasia. Am J Surg 2005;190:874-878.
4. Douard R, Gaudric M, Chaussade S, et al: Functional results after laparoscopic Heller myotomy for
achalasia: A comparative study to open surgery. Surgery 2004;136:16-24.
5. Gaissert HA, Lin N, Wain JC: Transthoracic Heller myotomy for esophageal achalasia: Analysis of long-
term results. Ann Thorac Surg 2006;81:2044-2049.

240
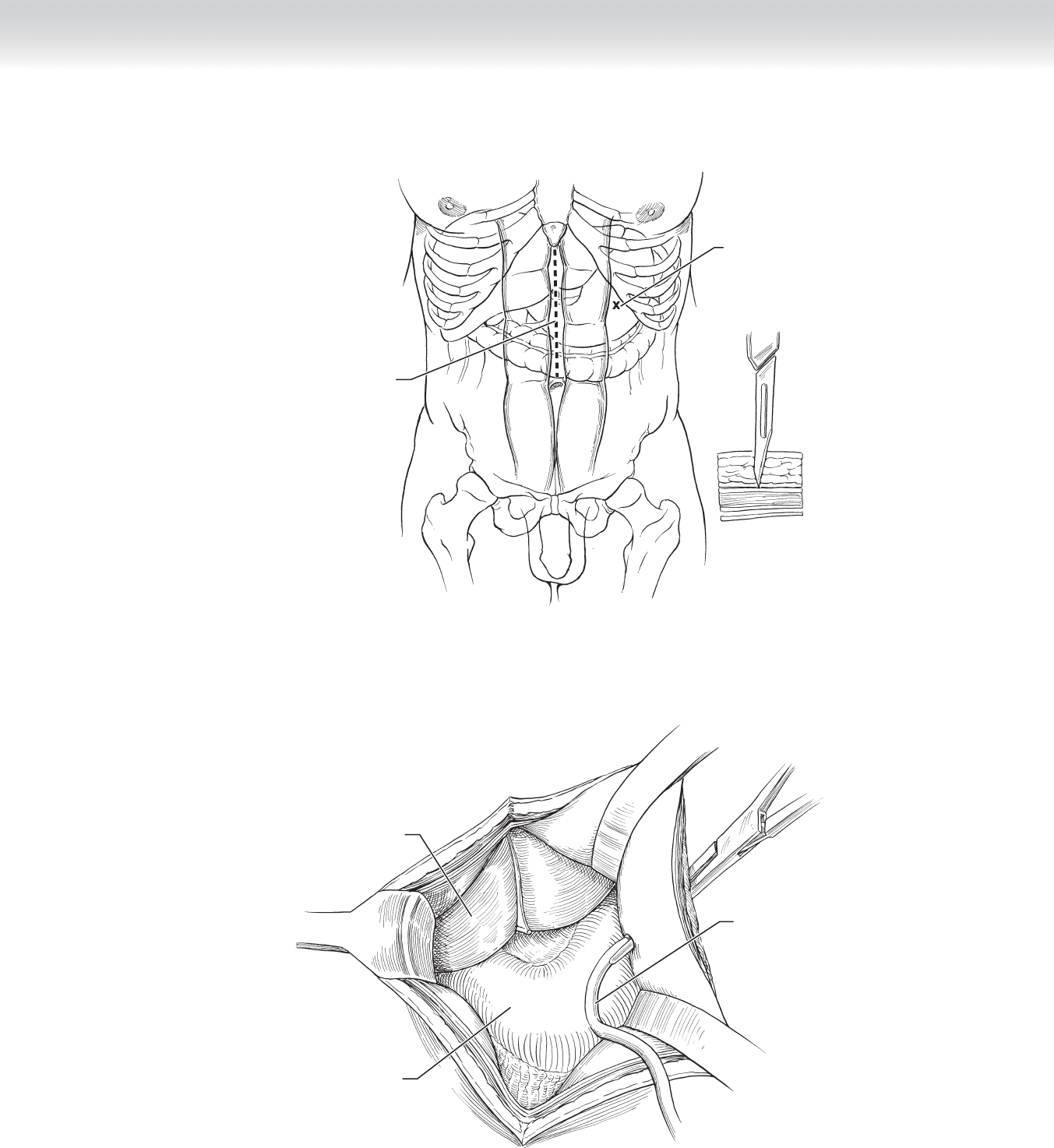
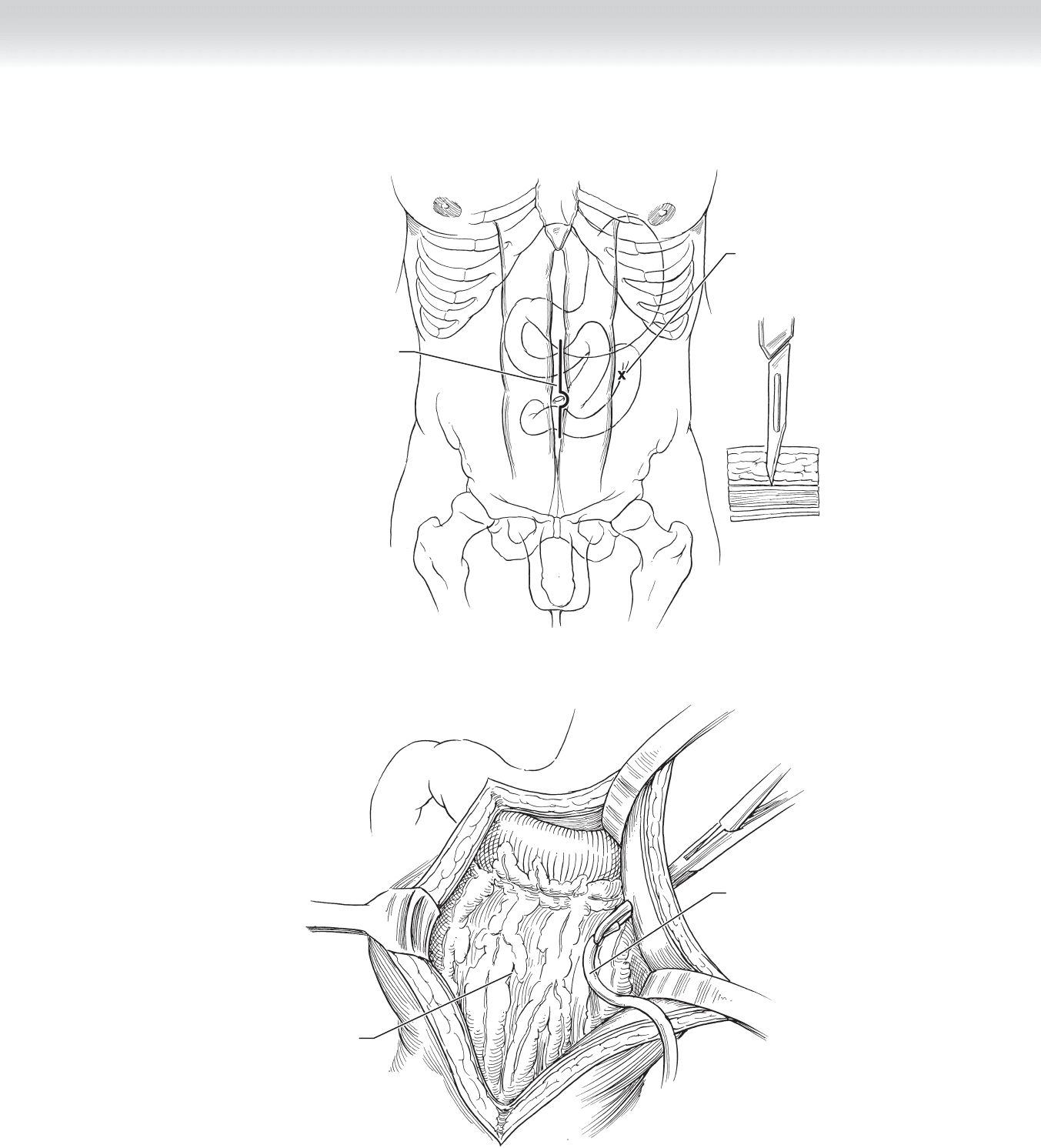
STEP 1: SURGICAL ANATOMY
◆ Allows gastric decompression
◆ Access for enteral feeding (Figure 20-1)
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Anesthesia: general
◆ Position: supine
STEP 3: OPERATIVE STEPS
1. INCISION
◆ Incision and exposure: upper midline
◆ Use scalpel to create stab wound through skin and anterior fascia just lateral to rectus abdo-
minus muscle left of midline (see Figure 20-1).
2. DISSECTION
◆ With retraction and visualization, the surgeon should use forceps through the stab wound
to enter through the peritoneum and into the abdomen.
◆ The surgeon should use the same forceps to grasp a mushroom catheter (12F) and retract
the external end of the catheter through the stab wound (Figure 20-2).
CHAPTER
20
Stamm Gastrostomy
Dennis C. Gore
CHAPTER 20 • Stamm Gastrostomy 241
Liver
Stomach
Mushroom
catheter
FIGURE 20 –2
Upper midline
incision
Exit site
2 cm or more
below costal
margin
MC
FIGURE 20 –1
242 Section IV • The Abdomen
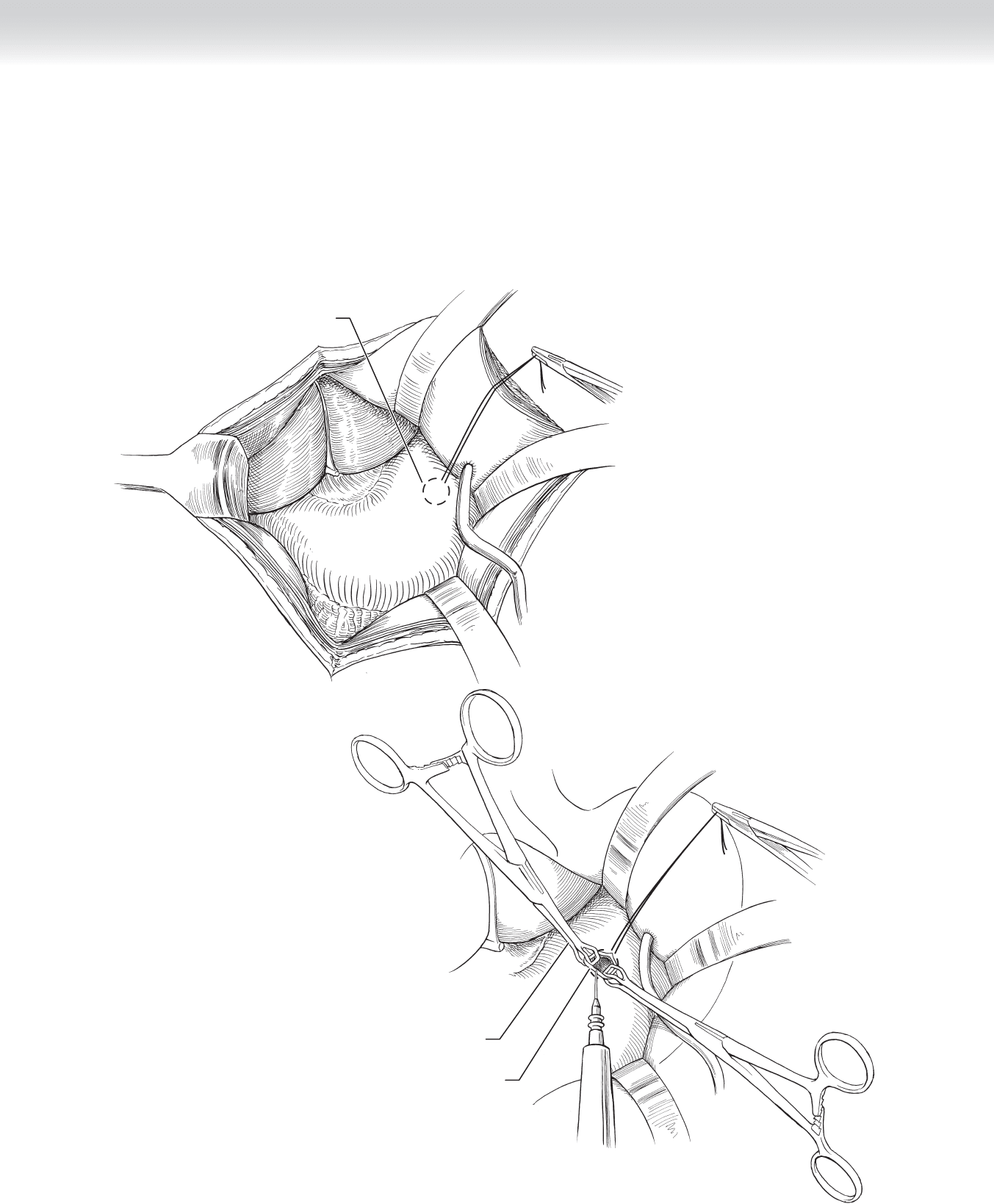
◆ Place 2-0 silk purse-string suture to the anterior wall of the stomach (Figure 20-3).
◆ Using two Babcock clamps for traction, the surgeon uses the cautery to create gastrotomy
within the purse-string suture (Figure 20-4).
First purse-string suture
FIGURE 20 –3
Babcock clamp
Gastrotomy
FIGURE 20 –4
◆ Two Babcock clamps are used for traction and forceps are used to stent the mushroom
catheter tip, which is placed through gastrotomy (Figure 20-5, A).
◆ The fi rst purse-string suture is secured around the catheter (Figure 20-5, B).
B
Second purse-string suture
Mushroom catheter
A
First purse-string suture
FIGURE 20 –5
CHAPTER 20 • Stamm Gastrostomy 243
244 Section IV • The Abdomen
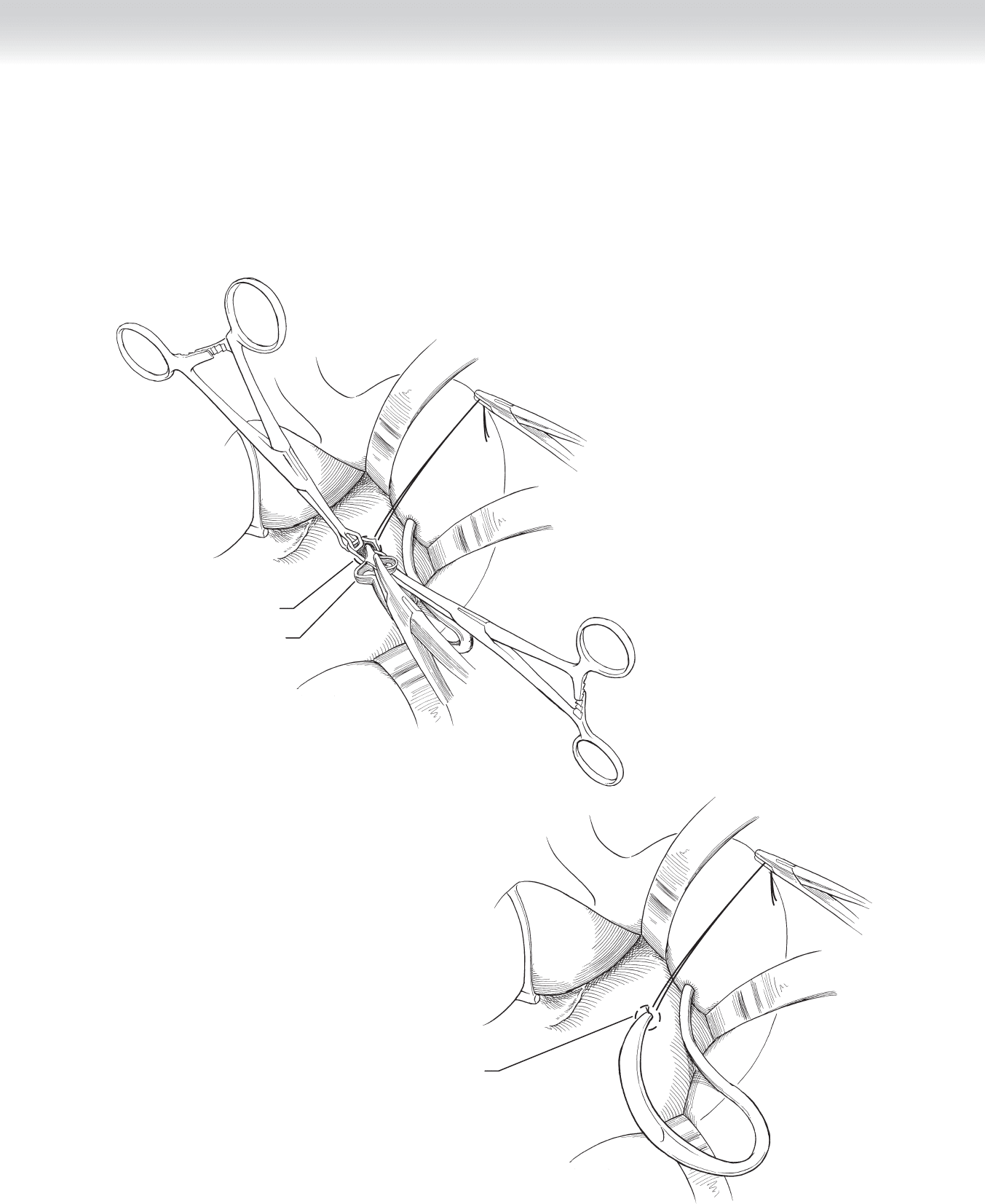
◆ The second purse-string of 2-0 silk sutures is placed around the tube and secured
(Figure 20-6).
◆ 2-0 silk sutures are used to anchor the anterior wall of the stomach to the peritoneum in
simple, interrupted fashion (Figure 20-7).
◆ The mushroom catheter is retracted to approximate the anterior stomach wall with the
peritoneum, then secured, and silk sutures are tied.
Mushroom catheter
Transversalis muscle
Parietal
peritoneum
Stomach
FIGURE 20 –6
Anchor
sutures
FIGURE 20 –7

CHAPTER 20 • Stamm Gastrostomy 245
3. CLOSING
◆ Closure of fascia with suture
◆ Closure of skin
STEP 4: POSTOPERATIVE CARE
◆ Routine
STEP 5: PEARLS AND PITFALLS
◆ Two Babcock clamps grasping the edges of the gastrotomy along with a forceps inserted
into the tip of the mushroom catheter and then held under tension provide an excellent
means of retraction for placing the mushroom catheter within the stomach.
◆ The catheter should remain in place until the gastrostomy tract and the anterior stomach
wall are securely healed to the peritoneal surface, which usually takes 10 days.
◆ First place all the sutures from the stomach to the peritoneum, then retract the catheter to
approximate the anterior surface of the stomach to the peritoneum and secure ligatures.
This sequence allows good visualization and room for placing sutures.
SELECTED REFERENCES
1. Zollinger RM Jr, Zollinger RM: Atlas of Surgical Operations. New York, MacMillan, 1983, p 30.

246
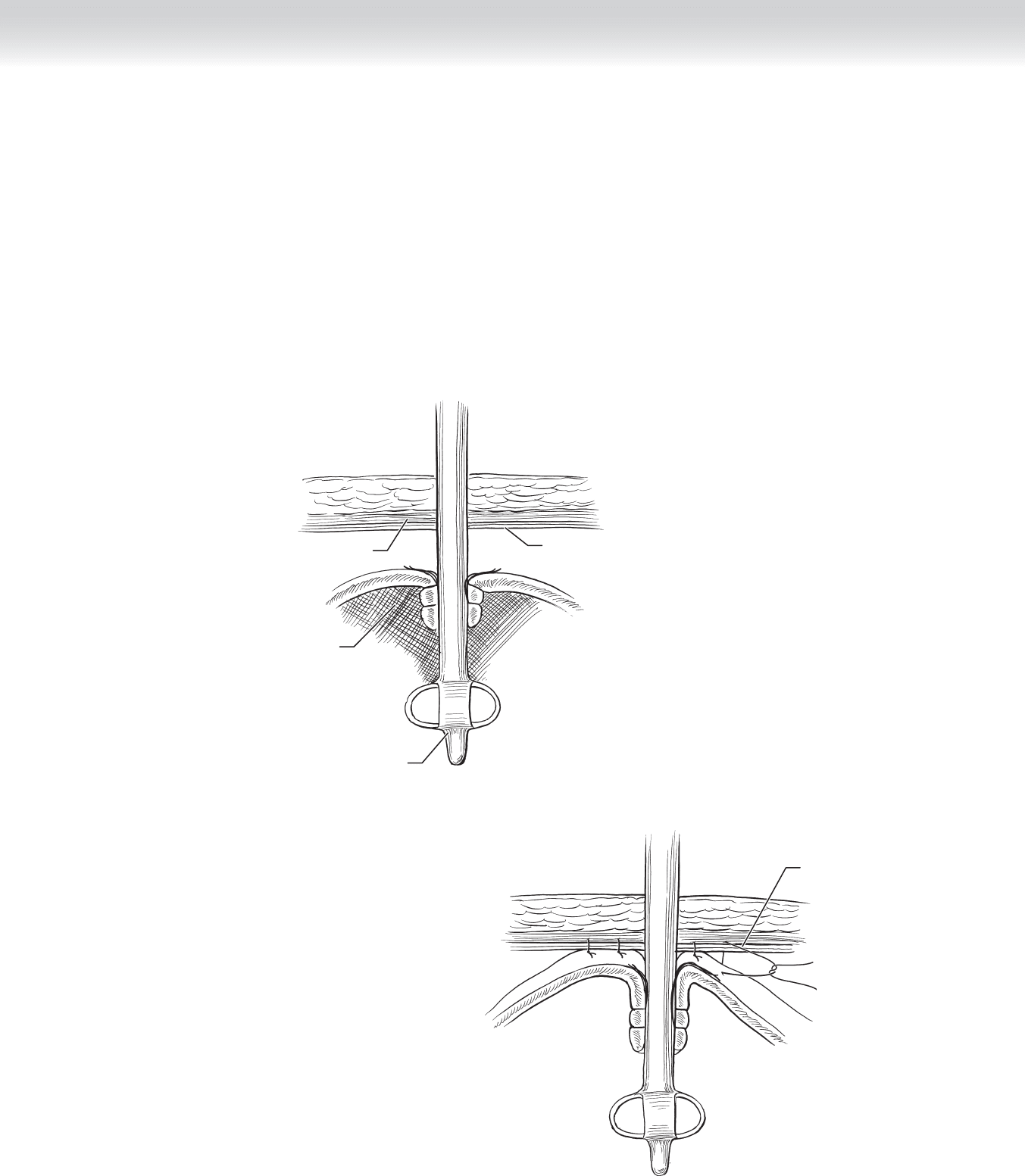
STEP 1: SURGICAL ANATOMY
◆ See Figure 21-1.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Indication: access for enteral feeds
◆ Anesthesia: general
◆ Position: supine
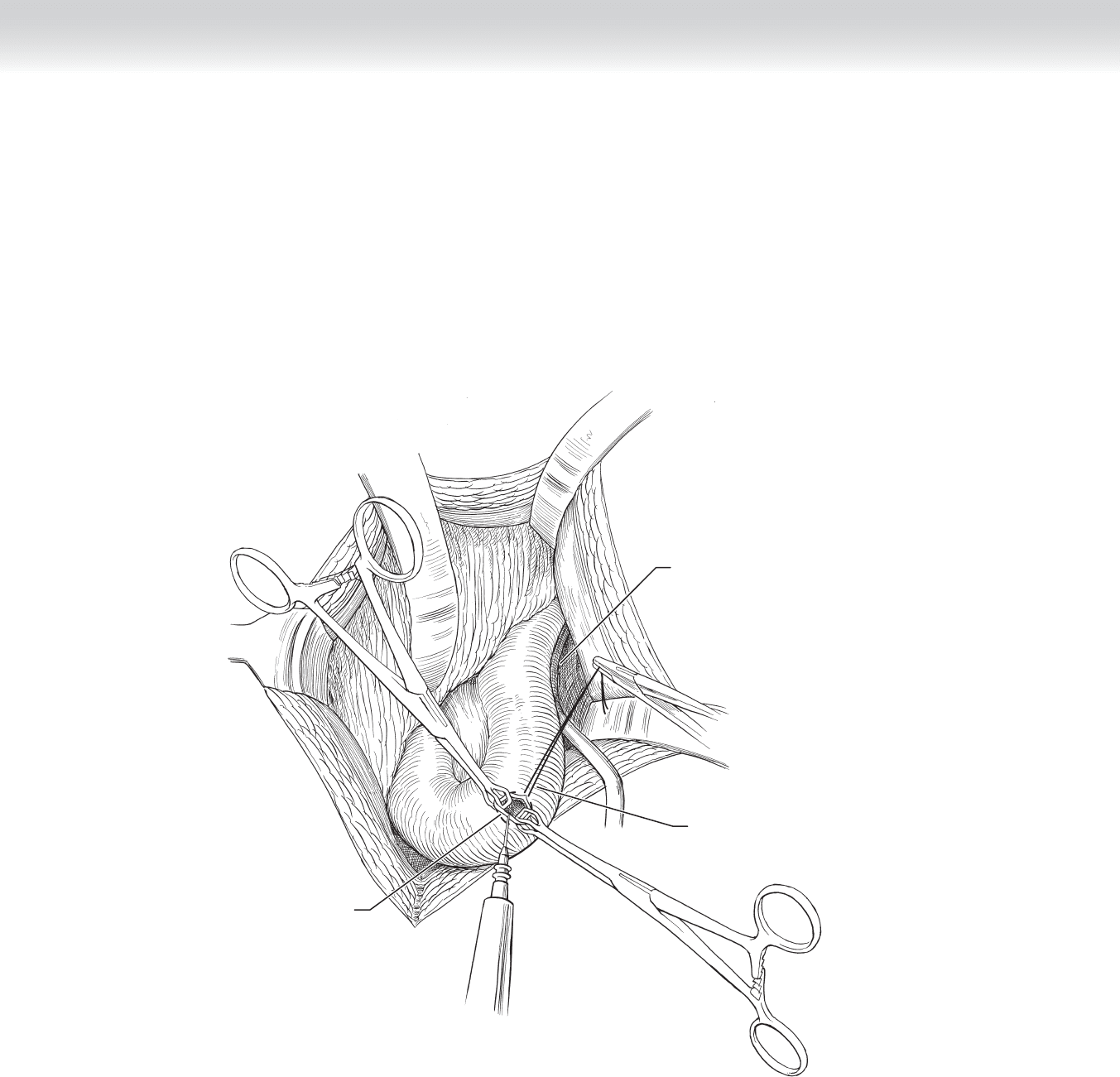
STEP 3: OPERATIVE STEPS
1. INCISION
◆ Periumbilical midline laparotomy (Figure 21-1).
2. DISSECTION
◆ After entering the peritoneal cavity, use scalpel to create stab wound through skin and ante-
rior fascia, just lateral to rectus abdominus muscle, usually to the left (see Figure 21-1).
◆ With retraction and visualization, use forceps through stab wound to enter through
peritoneum and into abdomen (Figure 21-2).
◆ Use this same forceps to grasp mushroom catheter (20F) and retract external end of
catheter through stab wound.
CHAPTER
21
Witzel Jejunostomy
Dennis C. Gore
Omentum
Mushroom
catheter
Periumbilical midline
laparotomy incision
Exit site of
tube through
abdominal wall
(stab wound)
MC
FIGURE 2 1–1
FIGURE 2 1–2
CHAPTER 21 • Witzel Jejunostomy 247
248 Section IV • The Abdomen
◆ Place 3-0 silk suture as purse string into antimesenteric wall of selected jejunum, usually
approximately 30 cm distal to ligament of Treitz yet with suffi cient mobility to reach
peritoneum at the site of the catheter exit (Figure 21-3).
◆ Using two Babcock clamps for traction, use cautery to create enterotomy within purse
string (Figure 21-3).
Enterotomy
within jejunum
Mushroom
catheter
First purse-string
suture
FIGURE 2 1–3
