Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

0010 Cardiac risks Alcoholics are at increased risk for
three different clinical cardiac complications. The
‘holiday heart syndrome’ refers to potentially lethal
arrhythmias secondary to the excessive consumption
of alcohol over a short period of time. Alcoholic
cardiomyopathy is caused by the toxic effects of alco-
hol and/or acetaldehyde or increased circulating fatty
acids on mitochondrial respiration in cardiac muscle
cells, and results in low-output left-sided heart
failure. ‘Wet beriberi’ represents high-output heart
failure secondary to thiamin deficiency in chronic
alcoholism and, since thiamin is integral to many
carbohydrate and ketoacid reactions, may be trig-
gered or exacerbated by acute fall in thiamin stores
following the administration of intravenous glucose
in severely malnourished alcoholics.
0011 Pancreatitis and pancreatic insufficiency Chronic
alcoholism is the leading cause of acute and recurrent
attacks of pancreatitis in developed countries,
resulting in anatomic distortion and progressive de-
struction of the pancreas. Loss of more than 90% of
pancreatic function results in pancreatic insufficiency,
a condition characterized by glucose intolerance due
to destruction of pancreatic beta cells and to de-
creased production of pancreatic digestive enzymes,
resulting in malabsorption of dietary protein, lipid,
and lipid-soluble vitamins A, D, E, and K. The net
clinical picture is that of late-onset chronic steator-
rhea (diarrhea due to excessive unabsorbed fat in the
stool), with malnutrition, diabetes, and signs of fat-
soluble vitamin deficiencies.
0012 Anemia Anemia is common in chronic alcoholism
due to frequent episodes of bleeding from alcohol-
associated gastritis or bleeding esophageal varices
and to nutritional causes. A study of more than one
hundred anemic chronic alcoholics admitted to a
large urban hospital found mixed and combined
causes, including iron deficiency consistent with epi-
sodic blood loss in about one-quarter, megaloblastic
bone marrow consistent with folate deficiency in one-
third, and sideroblastic bone marrow changes con-
sistent with pyridoxine deficiency in one-quarter of
the patients.
0013Neurological effects of excessive alcohol The
neurological effects of alcohol consumption can
be categorized as those related directly to alcohol,
those that are related to alcoholic liver disease,
and those that are secondary to the effects of alcohol
consumption on specific micronutrients. The direct
toxic effects of excessive alcohol consumption on
the brain include intoxication, coma, head injury,
and withdrawal syndromes. Intoxication is associated
with lowered inhibition, euphoria, poor memory and
judgment, and decreased reaction time, which is the
principal cause of motor vehicle accidents and other
alcohol-related trauma. About half of all motor
vehicle accidents involve innocent or intoxicated
pedestrians. Legal intoxication in most localities in
the USA occurs at blood levels above 0.08 g dl
1
or
0.019 mol l
1
. Severe intoxication resulting in coma
and death can occur at levels above 0.4 g dl
1
or
0.095 mol l
1
. Intoxication is often the background
for falls that can result in head injury, such as sub-
dural hematoma, that, if unrecognized, can lead to
progressive loss of consciousness and death. Alcohol
withdrawal syndromes occur after prolonged con-
sumption of excessive amounts of alcohol, usually in
binge drinkers who are forced through illness or other
circumstances to abruptly stop drinking. The several
potential signs of alcohol withdrawal depend upon
the length of time after the last drink and are all
characterized by hyperexcitability. For example,
tremulousness occurs within hours, a general seizure
may occur within the first 24 h, and delirium tremens
with auditory or visual hallucinations may occur 2–5
days after the last drink. These withdrawal syn-
dromes can be forestalled by reinstitution of alcohol
and gradual lowering of intake or by specific anti-
anxiety benzodiazepine drugs.
0014Hepatic encephalopathy represents a disturbance
in consciousness that occurs in patients with end-
stage alcoholic liver disease. This syndrome is caused
by nitrogenous substances, in particular ammonia,
that originate through intestinal bacterial digestion
of protein, bypass their hepatic site of metabolism
due to liver scarring and diversion of blood flow
from the portal-splanchnic circulation to the systemic
circulation, and then cross the blood–brain barrier
tbl0003 Table 3 Clinical toxic effects of alcohol
Cancers of oropharynx, esophagus, breast and colon (see folate)
Cardiac risk
Arrhythmias: ‘holiday heart syndrome’
Cardiomyopathy: low-output failure
Wet beri-beri: high-output failure (see thiamin)
Anemia due to iron, folate, and/or pyridoxine deficiencies
Pancreatitis and pancreatic insufficiency with malabsorption of
fat and fat-soluble vitamins
Alcoholic liver disease
Fatty liver: reversible
Alcoholic hepatitis: inflammation, steatonecrosis
Alcoholic cirrhosis: portal hypertension with risk of ascites,
renal failure, ruptured esophageal varices, and hepatic
encephalopathy
Neurological disorders:
Wernicke–Korsokoff syndrome (see thiamin)
Peripheral neuropathy (see thiamin, pyridoxine)
Intoxication: trauma, automobile accidents
Alcohol withdrawal syndromes
114 ALCOHOL/Metabolism, Beneficial Effects, and Toxicology

into the brain. Elevations in blood ammonia levels
typically occur in patients with severe cirrhosis of the
liver after ingestion of excessive animal protein or
after acute intestinal bleeding. If untreated, the stages
of consciousness proceed from normal to confusion
to somnolence to coma to death. Treatment consists
of avoidance of excessive dietary animal protein, pre-
vention or prompt treatment of intestinal bleeding,
and administration of substances that reduce ammo-
nia levels in the intestine.
0015 Neurologic disorders that are based on micronutri-
tent deficiencies include the Wernicke–Korsokoff
syndrome of thiamin deficiency and peripheral
neuropathies of thiamin or pyridoxine deficiency,
and are described separately below.
0016 Alcoholic liver disease The risk of developing alco-
holic liver disease is dependent upon the amount and
duration of alcohol consumed. While alcoholic fatty
liver is common and reversible with abstinence,
alcoholic hepatitis or inflammation of the liver with
steatonecrosis of hepatocytes carries a significant
mortality and is the precursor of chronic scarring or
cirrhosis of the liver. Both alcoholic hepatitis and
cirrhosis can result in portal hypertension, which is
associated with diversion of portal-splanchnic blood
flow through collateral veins to the systemic circula-
tion, and is characterized clinically by increased risk
of abdominal fluid accumulation known as ascites,
renal failure, acute hemorrhage from esophageal
varices, and hepatic encephalopathy.
0017 Retrospective European and American population
studies found that the chronic consumption of at least
six drinks per day was the threshold for developing
alcoholic cirrhosis over time, whereas the statistical
risk of developing cirrhosis develops with as little as
three drinks per day. A German study of well-to-do
corporate executives found a direct relationship be-
tween the amount and duration of alcohol consump-
tion and the incidence of cirrhosis by liver biopsy,
such that the average daily consumption of 160 g of
alcohol (11 drinks, equivalent to 440 ml or a pint of
whiskey) over 15 years resulted in a 50% likelihood
of cirrhosis. Worldwide, the mortality from alcoholic
liver disease increases in direct proportion to the
national per capita consumption of alcohol, with the
greatest number of cirrhosis-related deaths occurring
in Russia and eastern European countries, followed
by countries with a high daily cultural wine consump-
tion such as France and Italy. These statistics, to-
gether with results from alcohol-fed animal models,
support the notion that the pathogenesis of alcoholic
liver disease is related mainly to the toxic effects of
alcohol and its acetaldehyde metabolite that trigger
oxidative and cytokine responses. These responses
result in hepatic inflammation, hepatocellular necro-
sis, collagen production, and cirrhosis. More recent
data point to an important role of abnormal hepatic
methionine metabolism during excessive alcohol
consumption – in particular, decreased hepatic
S-adenosylmethionine – that is associated with abnor-
mal antioxidative mechanisms and altered hepato-
cellular DNA metabolism associated with necrosis
and apoptosis of hepatocytes.
Nutrient Deficiencies
0018While alcoholic liver disease is mainly due to the
toxicity of alcohol, its presence has profound effects
on nutrient metabolism (Table 4). There are essen-
tially three overall etiologies of malnutrition in
chronic alcoholism: decreased dietary intake due to
anorexia and/or economic deprivation combined
with alcohol addiction, decreased intestinal absorp-
tion, and abnormal nutrient metabolism with in-
creased nutrient excretion in the bile or urine. With
the exception of beer as a source of folate, alcoholic
beverages are essentially devoid of micronutrients
and of protein, carbohydrate, and lipid sources of
energy. Abnormal nutrient absorption of dietary
energy from fat and of soluble vitamins is magnified
by pancreatic insufficiency due to decreased pancre-
atic lipase secretion and by alcoholic liver disease due
to decreased secretion of bile acids that are required
for the micellar solubilization of dietary lipids.
0019Thiamin Chronic alcoholism is the principal cause
of thiamin deficiency in the developed world, and low
serum levels of thiamin have been described in 80%
of patients with alcoholic liver disease. The etiologies
of thiamin deficiency include poor diet and intestinal
tbl0004Table 4 Micronutrient deficiences associated with chronic
alcoholism
Micronutrient Deficiency signs
Thiamin Wernicke–Korsokoff syndrome
Peripheral neuropathy
Folate Macrocytic anemia
Diarrhea
Colon and breast cancer
Hyperhomocysteinemia
Pyridoxine Peripheral neuropathy
Sideroblastic anemia
Vitamin A Night blindness
Increased cancer risk
Vitamin D Osteoporosis
Zinc Night blindness
Abnormal taste
Hypogonadism
Abnormal cellular immunity
Iron Microcytic anemia
ALCOHOL/Metabolism, Beneficial Effects, and Toxicology 115

malabsorption secondary to alcohol inhibition of
the Na, K-ATPase pump in the basolateral membrane
of the intestinal epithelial absorbing enterocytes.
The clinical features of the Wernicke–Korsokoff syn-
drome of thiamin deficiency include progressive cere-
bral, thalamic, and cerebellar defects that result in
cognitive defects, ophthalmoplegia, and a wide-
based gait. The Korsokoff syndrome refers to irre-
versible confabulation, confusion, and profound loss
of recent memory. Chronic alcoholics are also prone
to develop wet or dry beriberi. Wet beriberi is one of
the cardiomyopathies of chronic alcoholism, is char-
acterized by high-output cardiac failure, and can be
precipitated by intravenous administration of glucose
to severely malnourished patients, with marginal
thiamin stores. Dry beriberi represents progressive
peripheral neuropathy mainly of the lower extrem-
ities and may be associated with painful hypersensi-
tivity of the plantar surfaces of the feet that makes
walking difficult.
0020 Folate deficiency and abnormal methionine metabo-
lism Folate deficiency occurs in about 50% of
patients with alcoholic liver disease and results from
combinations of poor diet, malabsorption secondary
to alcohol inhibition of the intestinal reduced folate
carrier, abnormal hepatobiliary metabolism, in-
creased urine excretion, and acetaldehyde-triggered
oxidation of the folate molecule. While macrocytic
anemia is the overt clinical sign of folate deficiency
induced by chronic excessive alcohol ingestion, more
subtle signs include chronic diarrhea due to abnormal
enterocyte function and hyperhomocysteinemia when
more than two alcoholic drinks are consumed per
day. The combined effects of folate deficiency and
chronic alcohol intake may contribute to abnormal
hepatic methionine and DNA metabolism. Studies in
animal models found that chronic exposure to alco-
hol impairs the activities of methionine synthase and
methyl adenosyl transferase, resulting in hyperhomo-
cysteinemia and S-adenosylmethionine deficiency,
which in turn impairs the synthesis of the antioxidant
glutathione and contributes to the development of
alcoholic liver disease. As indicated, impaired DNA
metabolism may account for the increased risk for
colon and breast cancer found in excessive alcohol
consumers with dietary inadequacy of folate.
0021 Vitamin B
12
The standard Schilling test for vitamin
B
12
absorption is abnormal in chronic alcoholic pa-
tients secondary to low uptake of the vitamin by the
absorbing ileal enterocytes. However, whereas hep-
atic levels of vitamin B
12
are low in patients with
alcoholic liver disease, serum vitamin B
12
levels are
typically normal or elevated in chronic alcoholism
and correlate with changes in serum enzymes that
reflect alcoholic liver injury. This dichotomy may
relate to failure of liver uptake and/or increased re-
lease of vitamin B
12
and its analogs from damaged
hepatocytes. Owing to the metabolic interaction of
vitamin B
12
and folate in the methionine synthase
reaction, the clinical effects of liver vitamin B
12
defi-
ciency cannot be readily distinguished from those of
folate deficiency. Thus, the degree to which liver vita-
min B
12
deficiency contributes to macrocytic anemia
and hyperhomocysteinemia in chronic alcoholic
patients with liver disease has not been established.
0022Pyridoxine Pyridoxine, or vitamin B
6
, deficiency in
chronic alcoholism results from poor diet and the
effects of the alcohol metabolite acetaldehyde on hep-
atic pyridoxal phosphate that releases it from its pro-
tein binder and enhances its urinary excretion. The
effects of pyridoxine deficiency include sideroblastic
anemia, peripheral neuropathy, and a relative de-
crease in serum alanine transaminase activity that
results in decreased ratio of this hepatic enzyme
compared with aspartate transaminase during the
development of alcoholic liver disease.
0023Vitamin A While serum levels are unreliable, hep-
atic vitamin A deficiency, according to measurements
in liver biopsies, increases in relationship to the sever-
ity of alcoholic liver disease and is essentially univer-
sal in alcoholic cirrhosis. The causes of vitamin A
deficiency include malabsorption secondary to de-
creased secretion of pancreatic lipase and of bile
acids and increased catabolism due to alcohol induc-
tion of microsomal enzymes that convert retinol to
polar metabolites that are rapidly excreted in bile, as
well as enhanced metabolism of retinol to retinalde-
hyde by alcohol dehydrogenase. The effects of vita-
min A deficiency in chronic alcoholics include
decreased dark visual adaptation, which may enhance
the risk of automobile accidents, and abnormal epi-
thelial cell turnover, which may enhance the risk of
esophageal cancer. Chronic alcoholics have an in-
creased risk of vitamin A toxicity during supplemen-
tation of vitamin A at relatively low levels (e.g., 5000
IU per day), resulting in more rapid progression of
alcoholic liver injury. Supplementation of chronic al-
coholics with b-carotene contributes to a similar dele-
terious effect on the liver as well as an enhanced risk
of lung cancer when smoking is combined with exces-
sive alcohol consumption.
0024Vitamin D and metabolic bone disease Chronic
alcoholics frequently have low circulating levels
of 25-hydroxy vitamin D, especially following the
development of alcoholic liver disease. The potential
116 ALCOHOL/Metabolism, Beneficial Effects, and Toxicology

causes of vitamin D deficiency in alcoholic liver dis-
ease include poor diet, decreased sun exposure, de-
creased intestinal absorption secondary to inadequate
bile secretion, decreased hepatic 25-hydroxylation,
and increased degradation by alcohol induced micro-
somal enzymes. Vitamin D deficiency is compounded
by decreased calcium absorption as a pathway to
decreased bone accretion. However, moderate alco-
hol consumption may be protective against bone dis-
ease, since alcohol use also raises estrogen levels in
women and is associated with decreased secretion of
parathyroid hormone.
0025 Zinc Low serum zinc levels are common in chronic
alcoholics and are low in about 50% of liver speci-
mens obtained at all stages of alcoholic liver disease.
Zinc deficiency is caused by inadequate dietary inges-
tion of zinc-rich proteins, decreased production of
zinc-rich pancreatic enzymes, abnormal transport
through absorbing enterocytes, and enhanced urine
excretion due to decreased binding to serum albumin.
Among alcoholics, zinc deficiency contributes to
night blindness since zinc is a cofactor for retinol
dehydrogenase, impaired alcohol metabolism due to
decreased activity of gastric alcohol dehydrogenase,
altered taste that may contribute to anorexia, de-
creased testosterone production and hypogonadism
that may contribute to osteoporosis, and altered
cellular immune function contributing to enhanced
infection risk.
0026 Iron Iron deficiency in chronic alcoholic patients is
due to frequent episodes of gastrointestinal bleeding,
and was found in about one-quarter of consecutive
anemic patients admitted to a large urban hospital.
The causes of bleeding among alcohol consumers
include acute gastritis, esophageal tears due to
retching and vomiting (Mallory–Weiss syndrome),
and episodic ruptured esophageal varices. Contrary
to popular opinion, the incidence of peptic ulcer is
no greater in alcoholics than in nonconsumers of
alcohol.
Energy Metabolism in Chronic Alcoholism
0027 Alcohol consumers may be severely malnourished,
at normal weight, or obese. In moderate drinkers,
alcohol-induced thermogenesis accounts for 15% of
alcohol metabolism, and preprandial alcohol con-
sumption increases the amount of nonalcohol calories
consumed in a meal. However, other studies have
shown that women moderate drinkers may become
underweight due to the substitution of alcohol
calories for carbohydrate. Among excessive alcohol
drinkers, the substitution of alcohol for nonalcohol
calories decreases body weight due to the energy con-
suming effect of alcohol metabolism by inducible
hepatic microsomal CYP2E1. Conversely, weight
gain and obesity may occur when alcohol is added
to a typical high-fat diet, potentially due to promo-
tion of fat storage that results from the inhibitory
effect of alcohol on oxidation of lipids in the liver
(Table 5).
Effects of Alcoholic Liver Disease on Energy and
Protein Metabolism
0028Extensive multicenter clinical studies have estab-
lished the universality of protein calorie malnutrition
in patients with alcoholic hepatitis and cirrhosis
(Table 6). Several studies that used anthropometric
techniques found that body fat stores were decreased
in derelict chronic alcoholics, whereas those who de-
veloped alcoholic liver disease had a significant deple-
tion of skeletal muscle as well. Protein calorie
malnutrition scores based on anthropometry, urinary
creatinine excretion, serum albumin, transferrin, and
retinol bound protein, and anergy by skin testing
correlated with disease severity and mortality in
over 500 male patients with alcoholic liver disease.
Retrospective studies showed that malnourished ex-
cessive alcohol consumers limit their intakes of non-
alcohol calories, whereas prospective studies of
hospitalized patients with alcoholic liver disease
found significant anorexia with voluntary consump-
tion of less than half the diet offering, which correl-
ated with disease severity and was predictive of
mortality risk. On the basis of measured lean body
mass or body cell mass, resting energy expenditure by
indirect calorimetry is either normal, low, or high in
patients with alcoholic cirrhosis. Stable and abstinent
cirrhotics tend to have a normal or low energy ex-
penditure if muscle and visceral protein stores are
normal or decreased. However, patients with active
tbl0005 Table 5 Energy metabolism during alcohol consumption
Moderate drinkers Excessive drinkers
Increase in body weight Appetite stimulation or disinhibition Increase in fat stores through inhibition of lipid
oxidation
Decrease in body weight Substitution of alcohol for carbohydrate in diet
(women)
Substitution of alcohol for nonalcohol calories
Energy wasting of CYP2E1 metabolism
ALCOHOL/Metabolism, Beneficial Effects, and Toxicology 117
alcoholic hepatitis tend to have increased energy ex-
penditure, insulin resistance, and increased urinary
excretion of total nitrogen and creatinine, consistent
with ongoing inflammatory processes in the liver.
Malnourished nonhospitalized patients with stable
cirrhosis have normal carbohydrate metabolism but
decreased glycogen stores with a greater tendency to
utilize fatty acids as a fuel source. Many clinical trials
have approached the question of whether improving
protein calorie malnutrition by oral, enteral, or par-
enteral nutrition support will reduce the morbidity
and mortality from alcoholic liver disease. Although
most trials have found an improvement in parameters
of malnutrition, none have shown that correction of
malnutrition by nutritional support alters the course
of this disease. However, a recent European multi-
center clinical trial showed that provision of oral
S-adenosylmethionine for 2 years decreased the mor-
tality from active alcoholic liver disease by one half.
See also: Alcohol: Properties and Determination; Alcohol
Consumption; Anemia (Anaemia): Iron-deficiency
Anemia; Other Nutritional Causes; Cancer:
Epidemiology; Coronary Heart Disease: Etiology and
Risk Factor; Folic Acid: Properties and Determination;
Iron: Properties and Determination; Physiology; Liver:
Structure and Function; Thiamin: Properties and
Determination; Physiology; Vitamin B
6
: Properties and
Determination; Physiology; Zinc: Deficiency
Further Reading
Bode JC, Hanisch P, Henning H et al. (1988) Hepatic zinc
content in patients with various stages of alcoholic liver
disease and in patients with chronic active and chronic
persistent hepatitis. Hepatology 8: 1605–1609.
Colditz G, Giovannucci E, Rimm EB et al. (1991) Alcohol
intake in relation to diet and obesity in women and men.
American Journal of Clinical Nutrition 54: 49–55.
Doll R (1993) Alcoholic beverages and cancers of the di-
gestive tract and larynx. In: Verschuren PM (ed.) Health
Issues Related to Alcohol Consumption, pp. 125–166.
Washington, DC: ILSI Press.
Giovannucci E, Rimm EB, Ascherio A et al. (1995) Alcohol,
low-methionine/low-folate diets, and risk of colon
cancer in men. Journal of the National Cancer Institute
87: 265–273.
Gronbaek M, Deis A, Sorensen TI et al. (1995) Mortality
associated with moderate intakes of wine, beer, or
spirits. British Medical Journal 310: 1165–1169.
Halsted CH (1995) Alcohol and folate interactions: clinical
implications. In: Bailey LB (ed.) Folate in Health and
Disease, pp. 313–327. New York: Marcel Dekker.
Hultberg B, Berglund M, Andersson A and Frank A (1993)
Elevated plasma homocysteine in alcoholics. Alcohol-
ism, Clinical and Experimental Research 17: 687–689.
Jacques PF, Bostom AG, Wilson PW et al. (2001) Determin-
ants of plasma total homocysteine concentration in the
Framingham Offspring cohort. American Journal of
Clinical Nutrition 73: 613–212.
Klatsky AL (1994) Epidemiology of coronary heart disease
– influence of alcohol. Alcoholism, Clinical and Experi-
mental Research 18: 88–96.
Kondrup J and Muller MJ (1997) Energy and protein re-
quirements of patients with chronic liver disease. Journal
of Hepatology 27: 239–247.
Lelbach WK (1975) Cirrhosis in the alcoholic and its rela-
tion to the volume of alcohol abuse. Annals of the New
York Academy of Sciences 252: 85–105.
Leo MA and Lieber CS (1999) Alcohol, vitamin A, and
b-carotene: adverse interactions, including hepatotoxi-
city and carcinogenicity. American Journal of Clinical
Nutrition 69: 1071–1936.
Lieber CS (1995) Medical disorders of alcoholism [see
comments]. New England Journal of Medicine 333:
1058–1065.
Mato JM, Camara J, Fernandez de Paz J et al. (1999)
S-Adenosylmethionine in alcoholic liver cirrhosis: a ran-
domized, placebo-controlled, double-blind, multicenter
clinical trial. Journal of Hepatology 30: 1081–1089.
Mendenhall C, Roselle GA, Gartside P and Moritz T (1995)
Relationship of protein calorie malnutrition to alcoholic
liver disease: a reexamination of data from two Veterans
Administration Cooperative Studies. Alcoholism, Clin-
ical and Experimental Research 19: 635–641.
National Institute on Alcohol Abuse and Alcoholism (2000)
Tenth Special Report to the U.S. Congress on Alcohol
and Health. Rockville, MD: US Department of Health
and Human Services.
Renaud S and de Lorgeril M (1992) Wine, alcohol, plate-
lets, and the French paradox for coronary heart disease.
Lancet 339: 1523–1526.
Savage D and Lindenbaum J (1986) Anemia in alcoholics.
Medicine (Baltimore) 65: 322–338.
Sellers TA, Kushi LH, Cerhan JR et al. (2001) Dietary folate
intake, alcohol, and risk of breast cancer in a prospective
study of postmenopausal women. Epidemiology 12:
420–428.
tbl0006 Table 6 Effect of alcoholic liver disease on energy and protein
metabolism
Protein calorie
malnutrition
Universal in advanced liver disease
Decreased dietary intake due to anorexia
Increased protein catabolism in active
disease
Abnormal energy
metabolism
Active disease: hypermetabolic
Inactive disease or stable cirrhosis
Normal or hypometabolic
Prefer fatty acids as fuel source
Decreased glycogen storage
Fat malabsorption due to low pancreatic
enzyme and bile secretion
Nutritional support Improves nutritional status
Not proven to alter the course of disease
118 ALCOHOL/Metabolism, Beneficial Effects, and Toxicology
Alcohol Consumption
A Sierksma and K F A M Hulshof, TNO Nutrition and
Food Research, The Netherlands
D E Grobbee, University Medical Center Utrecht,
Utrecht, The Netherlands
H F J Hendriks, TNO Nutrition and Food Research,
The Netherlands
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001 Alcohol-containing beverages play a prominent role
in many societies. For centuries, alcohol (ethanol)
formed a part of our diet. Even in the first Bible,
wine consumption and drunkenness are mentioned.
In the early middle ages, alcoholic beverages (beer)
became of great importance as there was a lack of
clean drinking water.
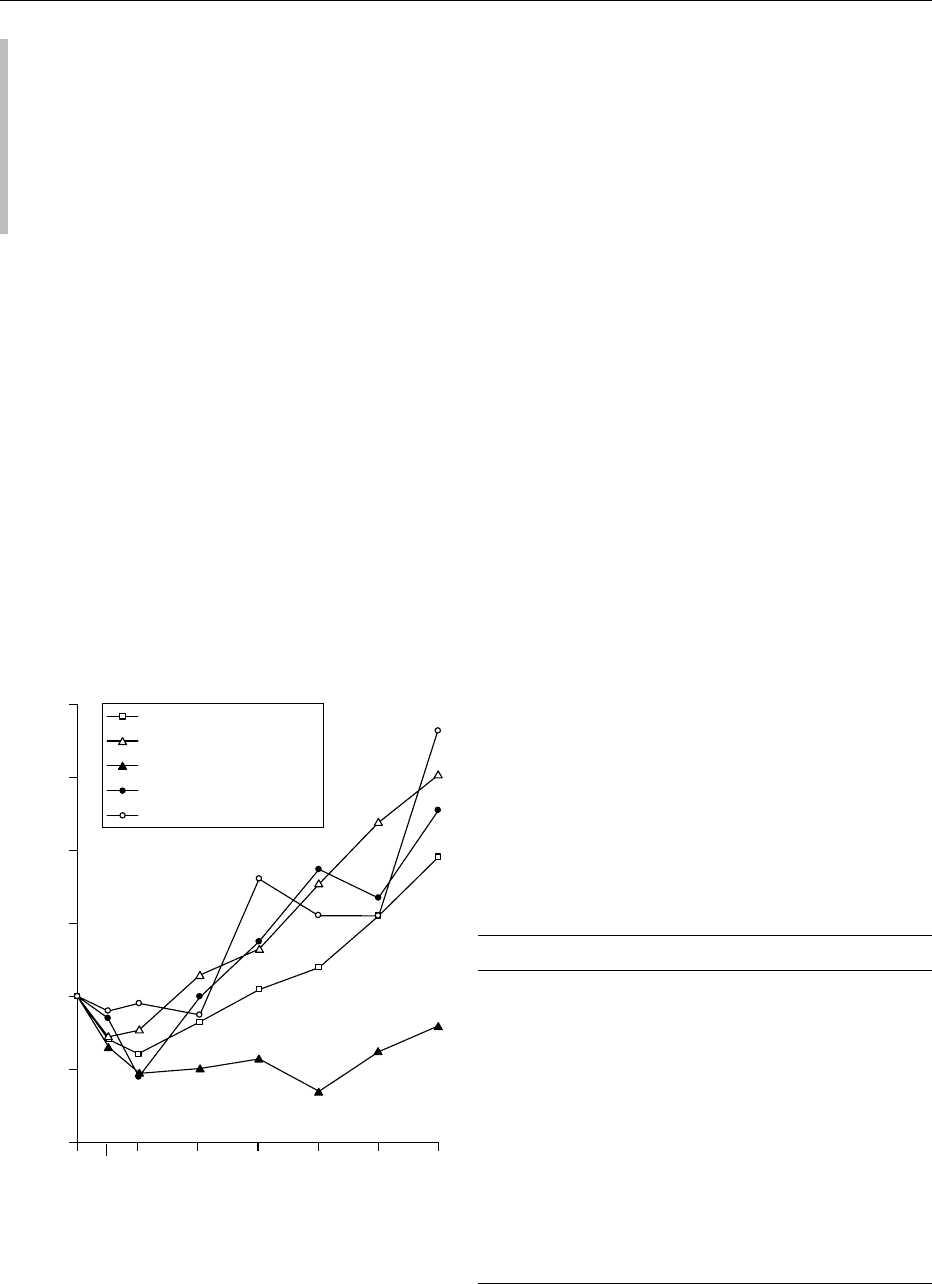
0002 Abundant epidemiological and clinical evidence
shows that there is a J-shaped relationship between
alcohol intake and total mortality, with increases
in death from cirrhosis, accidents, cancer, and cere-
brovascular disease in heavier drinkers (Figure 1).
Alcohol is consumed according to various patterns.
It is becoming increasingly clear that certain drinking
patterns may have widely varying effects on health
and may lead to social problems. This chapter dis-
cusses various aspects of alcohol consumption. First,
data on trends in alcohol consumption are given,
drinking patterns and their health effects are pre-
sented, followed by an overview of the most fre-
quently used methods for the assessment of alcohol
intake and their suitability for different purposes.
Then, the terms ‘moderate and excessive drinking’
and ‘standard drink’ are discussed, and finally, differ-
ent alcohol control policies and their effectiveness are
summarized.
Trends in Alcohol Consumption
Historical Trends
0003Economic changes, such as those brought about by
depression and war, cause fluctuations in the per-
capita alcohol consumption. During World War I
and II, alcohol consumption was low, and in the
mid-1970s after the OPEC oil crisis, per-capita alco-
hol consumption declined in some countries. In other
countries, such a decline occurred in the early 1980s,
when unemployment increased, and income stopped
rising. Table 1 shows the total alcohol consumption
per inhabitant in various developed countries in
1973, 1983, and 1999. Developing countries show
increases in alcohol consumption, but these countries
still have lower rates of consumption than those in
Europe and North America.
Drinks per day
0
0.60
Rate ratio
0.80
1.00
1.20
1.40
1.60
1.80
1
Occas.
23456+
All causes
All cancers
Accidents
Coronary heart disease
Cerebrovascular disease
fig0001 Figure 1 Relationship between alcohol intake and total mortal-
ity and death from cirrhosis, accidents, cancer, coronary heart
disease, and cerebrovascular disease. From Boffetta P and
Garfinkel L (1990) Alcohol drinking and mortality among men
enrolled in an American Cancer Society prospective study. Epi-
demiology 1: 342–348, with permission.
tbl0001Table 1 Total alcohol consumption per liter of pure alcohol per
capita in various countries in 1973, 1983, and 1999
Country 1973 1983 1999
Australia 8.6 9.5 7.5
Austria 12.2 10.2 9.3
Canada 7.2 8.2 6.3
Denmark 8.4 10.4 9.5
Finland 5.6 6.4 7.3
France 16.2 14.0 10.7
Germany 11.0 11.0 10.6
Hungary 9.5 11.4 9.7
Italy 13.9 11.4 7.7
Japan 4.9 5.8 6.6
Netherlands 7.6 8.9 8.2
New Zealand 8.8 9.2 7.4
Spain 13.7 12.8 9.9
United Kingdom 6.5 7.2 8.1
USA 7.3 8.1 6.7
Data adapted from World Drink Trends 2000. International Beverage
Consumption and Production Trends: Henley-on-Thames, UK. NTC
Publications, Commodity Board for the Distilled Spirits Industry.
ALCOHOL/Alcohol Consumption 119
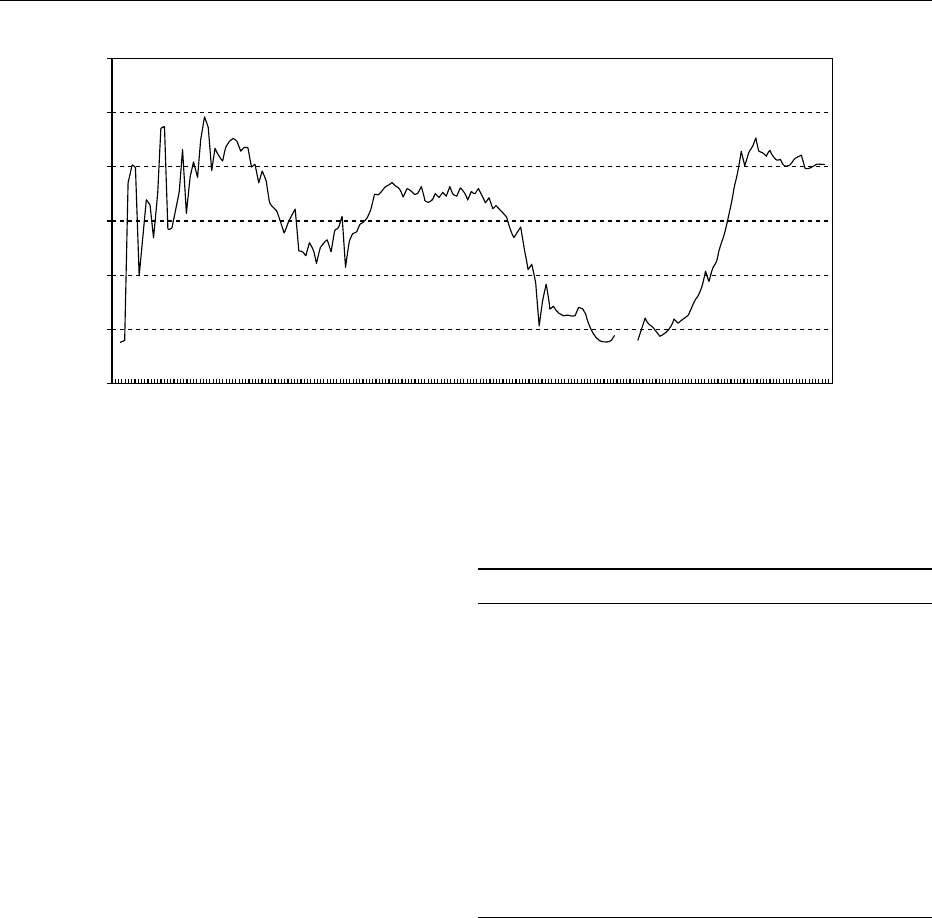
0004 In The Netherlands, alcohol consumption has been
quite stable since 1979, with an average intake of 8 l
of pure alcohol per inhabitant per year (Figure 2). The
Dutch National Food Consumption Survey over the
last 10 years showed that the proportion of alcohol
users increased among those aged 13–16 and 16–19
years and that alcohol consumption increased among
males aged 16–19 and 19–22 years. Above these age
groups, alcohol consumption is somewhat decreased.
Beverage Preference
0005 Wine is the predominant beverage in Mediterranean
and Latin American societies. In these regions, wine
is commonly consumed with meals. Spirits are the
beverages of choice in Nordic and some Eastern
European countries, where the drinking pattern is
characterized by a low overall consumption and
binge-drinking. Beer is the beverage of choice in
many parts of Europe, North America, and Australia.
In these countries, beer is mainly drunk in leisure time
and usually not with a meal. Wine-drinking has
become more popular in beer-drinking countries,
and beer-drinking in wine-drinking countries. In
spirit-drinking countries, both beer and wine con-
sumption have become popular. So differences in
beverage preference among preference appear to di-
minish over time. Table 2 shows the recent consump-
tion figures for alcoholic beverages in various
countries.
Drinking Patterns
0006 Drinking patterns refer to several aspects of drinking
behavior, including the quantity and frequency of
consumption, personal characteristics of the drinkers,
types of beverage consumed, temporal variations in
drinking, settings where drinking takes place, and the
activities associated with drinking. These patterns are
important determinants of both the positive and
negative consequences of drinking.
Quantity and Frequency
0007The importance of quantity follows from extensive
epidemiological research. Light to moderate alcohol
consumption is associated with a reduced risk for
coronary heart disease, as well as for ischemic stroke
tbl0002Table 2 Consumption by beverage type per liter per capita in
various countries in 1999
Country Spirits
a
Beer Wine
Australia 3.9 91.2 19.3
Austria 4.0 108.9 30.9
Canada 5.1 68.0 8.9
Denmark 3.2 101.9 29.9
Finland 6.4 80.1 17.5
France 6.9 38.7 57.2
Germany 5.7 127.5 22.9
Hungary 8.6 65.0 30.0
Italy 1.4 27.1 51.5
Japan 7.1 48.0 2.5
Netherlands 4.8 84.2 18.6
New Zealand 4.1 80.7 16.3
Spain 6.9 68.8 33.7
UK 4.3 99.0 14.5
USA 5.3 84.4 7.7
a
Liters of spirits was calculated, assuming that spirits contain 35 vol%
alcohol. Data adapted from World Drink Trends 2000. International
Beverage Consumption and Production Trends. Henley-on-Thames, UK.
NTC Publications, Commodity Board for the Distilled Spirits Industry.
1800 1820 1840 1860 1880 1900 1920 1940 1960 1980 2000
0
2
4
6
8
10
12
Litre pure alcohol per inhabitant per year
fig0002 Figure 2 Alcohol consumption in The Netherlands (liters of pure alcohol per inhabitant per year) since 1820. From Statistics
Netherlands, with permission.
120 ALCOHOL/Alcohol Consumption

and possibly for type 2 diabetes. Epidemiological
and physiological data are in favor of a causal rela-
tionship. Proposed protective mechanisms include
the stimulation of high-density lipoprotein (HDL)-
mediated processes and improvement of hemostatic
processes and vascular wall functioning. Excessive
alcohol consumption and alcohol abuse may lead to
alcoholism or alcohol dependence, with negative
effect on almost all parts of the body, including the
liver, brain, pancreas, cerebrovascular system, and
immune system, and are also associated with prema-
ture death.
0008 Both the average amount of alcohol consumed and
how drinkers decide to spread the consumption of
alcohol over the hours and situations available for
drinking are important. Although very little is known
about the effects of drinking frequency, intuitively, it
seems clear that variations in frequency may have
widely varying effects on health and social problems.
Binge-drinking, for example, is associated with
intoxication, hangover, and injuries.
Individual Characteristics
0009 Drinking is generally associated with particular per-
sonal characteristics, like genetics, personality traits,
age, gender, and religion.
0010 Genetics Alcohol dependence is a result of an inter-
action between biological and environmental factors.
Twin and adoption studies have shown that there is a
genetic factor in the etiology of alcohol dependence,
but the exact mechanism of transmission is not
known.
0011 Up to about 50% of some Asian groups have in-
herited deficiencies of the enzyme aldehyde (acetylde-
hyde) dehydrogenase, inducing relatively high blood
levels of acetaldehyde, which causes symptoms such
as flushing, nausea, vomiting, palpitations, and hyper-
tension. Deficiency of this enzyme deters the individ-
ual from drinking alcohol and reduces the risk of
alcohol dependence. About 5–10% of the British and
German populations and up to 20% of the Swiss
population are reported to have atypical forms of the
enzyme alcohol dehydrogenase, which causes more
rapid elimination of alcohol.
0012 Personality traits Personality traits such as chronic
anxiety, a sense of inferiority, self-indulgent tenden-
cies, antisocial personality disorder, aggressive and
impulsive personality, particularly in adolescents,
and borderline personality have been linked with
alcohol abuse.
0013 Age Young people are more likely to abuse alcohol
than older people. They have higher risks of incurring
such complications associated with acute intoxication
such as accidents, violence, and alcohol poisoning.
Physical changes in older people, like increased sus-
ceptibility to the depressant effects of alcohol, de-
creased rates of alcohol catabolism in the liver and
decreased percentage of body water, tend to limit
excessive alcohol consumption.
0014Gender Use, abuse, and dependence of alcohol are
much more common in males than in females. Social
disapproval or prohibition tends to restrict alcohol
consumption by females, but it may also promote a
different pattern of use, such as drinking at home or
in private. The lower percentage of body water and
the slower metabolism of alcohol in women may
influence the use of alcohol by women and may also
be a reason for the increased risk of alcohol problems.
Females tend to start abusive drinking much later in
life than males and probably also develop alcohol
problems later. The inverse association between
moderate alcohol consumption and coronary heart
disease has been documented in both men and
women. Benefits for women are mostly associated
with lower quantities of alcohol and appear to be
most pronounced in postmenopausal women. This
is not surprising since this age group, like men over
the age of 50, has a marked increase in cardiovascular
risk.
0015Religion Religion and religiosity are among the
most powerful predictors of drinking. The vast
majority of persons in Muslim countries abstain
from alcohol. Also, among Mormons, Adventists,
and various other religious communities, alcohol
drinking is not allowed. In countries where drinking
is relatively common, attendance at religious services
is a powerful predictor of whether and how much a
person drinks.
Beverage Type
0016Some reports have suggested that the type of beverage
may be important in coronary heart disease risk. Red
wine has received much attention as a potential con-
tributor of antioxidant activity, because of its natural
antioxidant compounds, i.e., polyphenols. However,
observational and experimental studies on the
consumption of beer, wine, and spirits in relation to
the risk of coronary heart disease indicate that
moderate consumption of all three alcohol-contain-
ing beverages is linked with a lower risk. Thus, a
substantial portion of the benefit is connected with
the alcohol component, rather than with specific non-
alcohol components present in the different types of
beverages.
ALCOHOL/Alcohol Consumption 121

Temporal Variations
0017 Drinking is strongly related to leisure time, which is
why drinking generally tends to be greatest during
nonworking hours and at weekends. Temporal pat-
terns of drinking vary considerably in different cul-
tures and social groups. The term ‘alcohol culture’
has been used to denote similarities between particu-
lar aspects of drinking patterns in different countries.
‘Dry’ and ‘wet’ drinking cultures refer to the rela-
tively low or high social acceptance of drinking. In
‘wet’ cultures, like the Mediterranean area and Latin
American societies, drinking with meals and during
the day is a common pattern. In ‘drier’ Northern
European cultures, drinking during the day is less
accepted and less common. It has been argued that
drinking problems are manifested differently in ‘dry’
cultures: fewer people incur problems, but those who
do suffer more severe individual consequences.
Settings and Activities
0018 Another dimension of drinking patterns concerns
the settings and activities associated with drinking.
Drinking may occur in connection with social or reli-
gious rituals or may be related to particular work
activities. Drinking can take place in private homes,
with or without a meal, or in public places, such as
bars, cafe
´
s, restaurants, or beer gardens.
0019 Drinking alcoholic beverages leads to a rapid
increase in blood alcohol concentration (BAC).
After reaching a maximum value, the BAC returns
slowly to the base level. The course of the alcohol
concentration with time depends on drinking condi-
tions such as the dose and concentration of the alco-
holic beverage consumed and whether alcohol is
consumed with or without a meal. Studies have shown
that BACs after moderate alcohol consumption
together with a meal remained half as high as those
with moderate alcohol consumption without a meal.
Assessment of Alcohol Consumption
0020 It is very difficult to assess alcohol intake accurately.
Although alcohol is part of the normal diet, it is not
considered a normal food constituent. It has a highly
symbolic value, and its consumption is influenced by
cultural differences and social norms.
0021 Methods for determining alcohol intake can be
divided into nonintrusive and intrusive estimates.
Nonintrusive estimates such as sales figures and col-
lateral reports are less threatening and more object-
ive, because respondents are not aware of them.
Intrusive estimates are based on self-reports or bio-
logical markers. Unfortunately, a ‘gold standard’ for
alcohol intake assessment is lacking.
Sales Figures
0022To determine alcohol availability in a population, per-
capita sales figures can be used. However, these do
not provide information about alcohol consumption
in certain groups or individuals. Another drawback is
that sales reports do not include untaxed alcohol
(duty-free shops), home-brewed alcohol, and export
sale.
Self-reports
0023Methods based on self-reports include face-to-face
or telephone interviews, self-administered question-
naires, and diaries. Most of these self-reports can be
applied very easily and are relatively cheap. Self-
reports are suitable for use in small studies and in
large-scale surveys for epidemiological research and
can provide beverage-specific information. The qual-
ity of the data collected is determined by the order
and structure of the questions asked and by the mode
of the report and characteristics of the respondent,
such as age and culture.
0024Questions about drinking are threatening and may
easily yield socially desirable answers. In population
surveys, the average extent of underestimation of
alcohol intake can vary between 29 and 83% of the
actual intake. When the degree of underestimation is
not linked to the actual level of intake, it will not
affect the conclusions, and only the quantitative def-
inition of moderate or optimal level of alcohol use
will be unrealistic. However, some studies indicate
that heavy drinkers underestimate their alcohol
intake more than light drinkers do, and in this case,
conclusions about dose–response relationships are
unreliable. Underestimation may be partly prevented
by an anonymous questionnaire. The memory cap-
acity of the respondents may be a limiting factor as
well. Common errors in assessing alcohol intake in
surveys include selection bias, nonresponse, incom-
plete time sampling, under- or overestimation of
portion size, and recall bias.
Collateral Reports
0025Collateral reports are provided by a significant ‘other
person’ (e.g., a spouse or friend). The accuracy of
these reports is affected by the subject’s daily routine
making behavior more or less predictable and
the frequency of contact between the subject and the
collateral. Collateral reports are often used as a refer-
ence method.
Biological Markers
0026The advantage of biological markers is that they are
an objective measurement of intake, not affected
by socially desirable answers or interviewer effects.
122 ALCOHOL/Alcohol Consumption

However, they are not suitable for assessing actual
level of intake, drinking patterns, or beverage prefer-
ences. They can only be used to rank individuals
according to their intake. Table 3 gives an overview
of the biological markers of alcohol presented in the
literature, their purpose and estimated sensitivity
(proportion of positives that are correctly identified
by the test), and their specificity (proportion of nega-
tives that are correctly identified by the test).
0027 Biological markers of alcohol use are not suitable
for assessing habitual low or moderate drinking
levels: they can only be used for clinical studies of
alcoholics to monitor change in drinking patterns of
patients or to check abstinence.
Alcohol Consumption: Moderate and
Excessive
Moderate and Excessive Drinking
0028 The literature contains widely different applications
of the term ‘moderate.’ A comparison of average daily
amounts defined as light, moderate, and heavy in a
sample of recent publications shows that the lower
limit of moderate alcohol intakes ranges from 4.5 to
50 g per day, and the upper limit ranges from about 24
to 80 g per day. Table 4 shows some recommenda-
tions on drinking levels published by governments or
learned bodies.
0029 On a population basis, for the average adult man,
the optimal level may be in the range of 10–19 g of
alcohol per day, and the noninjurious level may be
approximately 30–40 g per day. For a woman, these
levels may be < 10 g per day and approximately
10–20 g per day. However, the individual differences
in body size, age, and special situations that can in-
crease the degree of risk (pregnancy, driving, diseases,
and medications) should also be taken into account.
0030Light and frequent drinking is suggested to be
beneficial, whereas large amounts drunk infrequently
are harmful with respect to coronary heart disease.
What is a ‘Standard Drink’?
0031Research outcomes are often confusing when moder-
ate and excessive drinking are expressed in ‘standard
drinks.’ The term ‘standard drink’ was originally
intended to apply to drinks of ‘standard’ strengths.
However, the alcohol content varies among different
beers, wines, and distilled spirits, and interpretations
differ across countries as to how much alcohol there
is in a standard drink (see Table 4). There may also be
differences in the standard serving sizes within a given
country, depending on the type of beverage served, so
the amount of alcohol may be different between the
different beverages. Another problem is a lack of
uniformity in the definition in which the alcohol con-
tent is measured – grams versus ounces of ethanol,
American versus British fluid ounces, or measures of
alcohol content as a percentage by weight or by
volume. The size of drinks poured in serving estab-
lishments may not be the same as that defined by the
standard drink, and there are significant levels of
alcoholic beverage consumption in homes and other
private settings where drinks are rarely measured in
standard units. These wide discrepancies and vari-
ations make any form of international comparison
tbl0003 Table 3 Characteristics of biological markers of alcohol use
Marker Purpose Estimatedsensitivity (sens.) and specificity (spec.)
Ethanol in serum, breath, or urine Recent intake (2–6 h) Sens. 25%
Spec. 100%
Methanol in body fluids or breath Recent (5–15 h) and chronic intake Higher sensitivity than ethanol
MCV of erythrocytes Chronic intake Sens. 35%
Spec. 40–90%
Erythrocyte acetaldehyde in plasma Recent intake (several days) Low sensitivity
Transferases (GGT, ASAT, ALAT)
in serum
Chronic intake, screening GGT: sens. 45%,
spec. 75% ASAT and ALAT:
lower than for GGT
5-Hydroxytryptophol in urine Recent intake (6–15 h) Sens. 70%
Spec. 95%
HDL in serum Recent and chronic, moderate and
high intake
Sens. 30%
FAEE in serum Recent intake (24 h) Higher sensitivity than ethanol
CDT in serum Chronic excessive intake, screening Sens. 75%
Spec. 90%
AANB in serum Chronic intake, monitoring Low sensitivity
AANB, a-amino-N-butyric acid; ALAT, alanine aminotransferase; ASAT, aspartate aminotransferase; CDT, carbohydrate-deficient transferrin; FAEE, fatty
acid ethyl esters; GGT, g-glutamyltransferase; HDL, high-density lipoprotein. MCV, mean corpuscular volume.
Data adapted from MacDonald I (ed.) (1999) Health Issues Related to Alcohol Consumption. Brussels: ILSI Europe.
ALCOHOL/Alcohol Consumption 123
