Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

RESPIRATORY FAILURE
277
with 37% who did not develop nosocomial pneumonia.
Although this difference in mortality rate was not statistically
significant, VAP did increase the time spent in the ICU. The
diagnosis of VAP is very difficult. Presence or absence of
fever, leukocytosis, or purulent sputum are not sensitive
or specific for VAP. The combination of new infiltrates
plus two of fever, leukocytosis, or purulent sputum has a
likelihood ratio of 2.8. The absence of new infiltrates low-
ers the likelihood of VAP (likelihood ratio = 0.35). Some
investigators have recommended that patients undergo
invasive diagnostic testing using fiberoptic bronchoscopy
(eg, protected brush catheters with quantitative bacterial
cultures); others suggest that these data do not improve
diagnostic accuracy. Decreasing the frequency of ventila-
tor circuit changes is associated with fewer episodes of
nosocomial pneumonia. Attention to careful suctioning,
frequent draining of condensate in the ventilator circuit,
judicious use of antibiotics (including shorter courses),
and avoiding prolonged mechanical ventilation decrease
the risk of VAP.
Discontinuation of Mechanical Ventilation
(“Weaning”)
Mechanical ventilation can be discontinued easily and safely
in the majority of patients, that is, those who do not have
severe lung disease or neuromuscular weakness or who are
electively placed on mechanical ventilation for surgery. In
other patients—especially those with lung disease—mechanical
ventilation usually must be discontinued with careful moni-
toring using a variety of techniques. A gradual reduction in
ventilatory support has led to the use of the term weaning
from the mechanical ventilator as the patient resumes spon-
taneous ventilation, but there is growing evidence that many
patients in the ICU do not need slow withdrawal of
mechanical ventilation. Discontinuation of mechanical ven-
tilation should be distinguished from discontinuation of
endotracheal intubation or tracheostomy. Although the
terms intubation and ventilation are often used synony-
mously, there are some patients in whom intubation is
necessary but mechanical ventilation is not (eg, those with
upper airway obstruction).
In may ICUs, discontinuation of mechanical ventilation is
facilitated by protocols directing physicians, nurses, and res-
piratory therapists. These evidence-based protocols have
been successful in decreasing duration of mechanical venti-
lation and maximizing patient understanding and comfort
during the process. However, not all studies demonstrate that
such protocols are necessary.
A. Physiologic Assessment—For mechanical ventilation to
be discontinued, the patient must have a sustained ventila-
tory capacity that equals or exceeds the ventilatory require-
ment. For most patients who fail, the ventilatory requirement
(ie, how much minute ventilation is needed to maintain
Pa
CO
2
) is high relative to ventilatory capacity (how much
minute ventilation the patient is capable of providing
without assistance)(Table 12–11). The ventilatory require-
ment is a function of the metabolic rate (CO
2
production),
the set point for Pa
CO
2
, and the efficiency of lung gas
exchange (dead space:tidal volume ratio). Ventilatory capac-
ity is determined primarily by the interaction of ventilatory
drive, respiratory system mechanics, and inspiratory muscle
strength and endurance.
Disuse of respiratory muscles leads to atrophy, earlier and
easier fatigue, and possibly discoordination. In patients with
increased airway resistance or decreased lung or chest wall
compliance, respiratory muscles must generate relatively
greater pressure for a given tidal volume. Often these patients
have an increased ventilatory requirement and, therefore, an
increased pressure-time product—an index of muscle work
and potential for fatigue. Factors associated with decreased
muscle strength and endurance include electrolyte abnor-
malities (eg, hypokalemia and hypophosphatemia), critical
illness polymyopathy and polyneuropathy, high-dose corti-
costeroid therapy, malnutrition, and recent use of nondepo-
larizing muscle relaxants.
B. Predicting Successful Weaning—The underlying disease
that caused a need for mechanical ventilation must be cor-
rected first. The patient should have adequate gas exchange, as
evidenced by an only moderate supplemental oxygen require-
ment (Pa
O
2
/F
IO
2
>200), PEEP of less than 5–8 cm H
2
O, and
V
D
/V
T
of less than 0.50. The ventilatory requirement is gen-
erally the minute ventilation (
.
V
E
) provided during mechani-
cal ventilation. If gas exchange and the metabolic rate do
not change, the patient will have to provide this amount of
.
V
E
to maintain Pa
CO
2
at the preweaning level. Weaning is
usually unsuccessful when the
.
V
E
requirement is greater
than 10–12 L/min, or about twice the resting
.
V
E
in normal
adults. Adequate ventilatory capacity is encouraged by ensur-
ing normal plasma electrolytes (especially phosphorus,
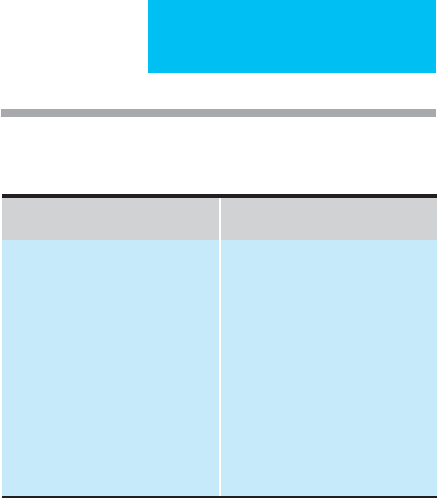
Increased Ventilatory
Requirement
Decreased Sustained
Ventilatory Capacity
Fever
Infection
Increased ventilatory drive
Metabolic acidosis
Excessive hyperalimentation
(especially with carbohydrate?)
Liver disease
Respiratory muscle fatigue
Hypokalemia
Hypophosphatemia
Decreased ventilatory drive
Bronchospasm
Airway secretions
Decreased lung or chest wall
compliance
Neuromuscular weakness
Malnutrition
Small endotracheal tube
Increased resistance of endotra-
cheal tube or ventilator circuit
Table 12–11. Factors contributing to difficult weaning:
Increased ventilatory requirement or decreased
ventilatory capacity.

CHAPTER 12
278
magnesium, and potassium), discontinuing sedatives, and
minimizing abnormal lung mechanics by treatment with
bronchodilators and suitable patient positioning.
Ventilatory capacity is assessed using a variety of weaning
parameters, some of which are shown in Table 12–12. Vital
capacity, negative inspiratory pressure, spontaneous
.
V
E
measured for 1 minute, and maximum voluntary ventilation
measured for 8–10 seconds estimate short-term ventilatory
capacity. These variables have excellent predictive value in
patients recovering from short-term general anesthesia, but
their predictive value is only marginal in patients with acute
or chronic lung diseases. This is largely because these param-
eters assess only ventilatory capacity and do not take into
account the ventilatory requirement and work of breathing.
In one study in which 58% of patients were weaned success-
fully, the following variables were found to be most closely
correlated with success:days of mechanical ventilation before
the weaning trial, respiratory frequency:tidal volume ratio,
maximal inspiratory pressure, maximal expiratory pressure,
and vital capacity. There were important differences between
groups with COPD, neurologic respiratory failure, and other
causes of respiratory failure; positive predictive values for
successful weaning ranged from 74–94%.
Indices that combine estimates of ventilatory require-
ment, work of breathing, and ventilatory capacity may be
useful. For example, a spontaneous respiratory rate:tidal vol-
ume ratio (f/V
T
) of less than 100/min/L may predict success-
ful weaning because it is an index of requirement and
capacity. This ratio, termed the rapid shallow breathing index,
proved to have greater sensitivity and specificity than other
variables for prediction of weaning. However, a report of
52 patients undergoing weaning from mechanical ventilation
indicated that 12 of 13 patients with a f/V
T
of more than
105/min/L were weaned successfully, whereas only one
patient who failed extubation had a ratio that high. One
interpretation is that very low f/V
T
ratios have a high positive
predictive value for successful weaning, whereas very high
ratios predict unsuccessful weaning well. On the other hand,
ratios of between 70 and 110/min/L are less useful.
Nevertheless, current predictors and clinical judgment of
successful weaning are poor. Because of this, a clinical trial of
patients who have marginal or low likelihoods of successful
weaning may be indicated. In an important study, all patients
using mechanical ventilation had a daily spontaneous
breathing trial unless contraindicated (eg, apnea, hypopnea,
severe hypoxemia, or high oxygen or minute ventilation
requirements). Surprisingly, a number of patients were dis-
continued successfully from mechanical ventilation who
would not have been predicted to do so by their clinicians. In
fact, patients who tolerate a spontaneous breathing trial of
30–120 minutes should be considered for immediate extuba-
tion in the absence of contraindications.
C. Weaning Methods—Patients who are easily weaned from
mechanical ventilation are easily weaned regardless of the
specific method used. Those who are difficult to wean for any
reason are difficult no matter which method is used. An
explanation of the weaning procedure, including descriptions
of possible discomfort and an assurance of close monitoring,
should be provided to the patient before weaning is started.
Once mechanical ventilatory support is being withdrawn,
slowly or rapidly, signs that should lead to restarting
mechanical ventilation or slowing the process include
tachypnea, tachycardia (HR >120 beats/min), hypotension,
severe anxiety, hypoxemia, respiratory acidosis (pH <7.30),
arrhythmias, chest pain, or other signs of hemodynamic
compromise. A study of a small number of patients showed
that a fall in gastric intramural pH, suggesting tissue
ischemia, was found in patients who failed weaning, whereas
those who were successful had no change in gastric intramu-
ral pH. In any patient who has difficulty being weaned from
mechanical ventilation, reassessment of ventilatory require-
ments and ventilatory capacity is indicated.
There are no conclusive studies demonstrating superior-
ity of any weaning method for patients with difficulty having
mechanical ventilation discontinued. Recent studies, how-
ever, suggest that spontaneous breathing trials followed by
extubation in suitable patients reduces length of ICU stay
and duration of mechanical ventilation. Although attractive,
noninvasive PPV in those with postextubated respiratory
distress has not been shown to benefit these patients.
Evidence that intermittent mandatory ventilation helps in
difficult patients is lacking.
1. T tube—The ventilator circuit is disconnected from the
endotracheal tube, and humidified oxygen is supplied by a
tube connected across the endotracheal tube connection
(T tube) while the patient breathes spontaneously. The
patient is observed carefully for signs of respiratory failure,
discomfort, severe dyspnea, or other intolerance.
If the T tube is used for a spontaneous breathing trial and
the patient tolerates the procedure for 30–120 minutes, then
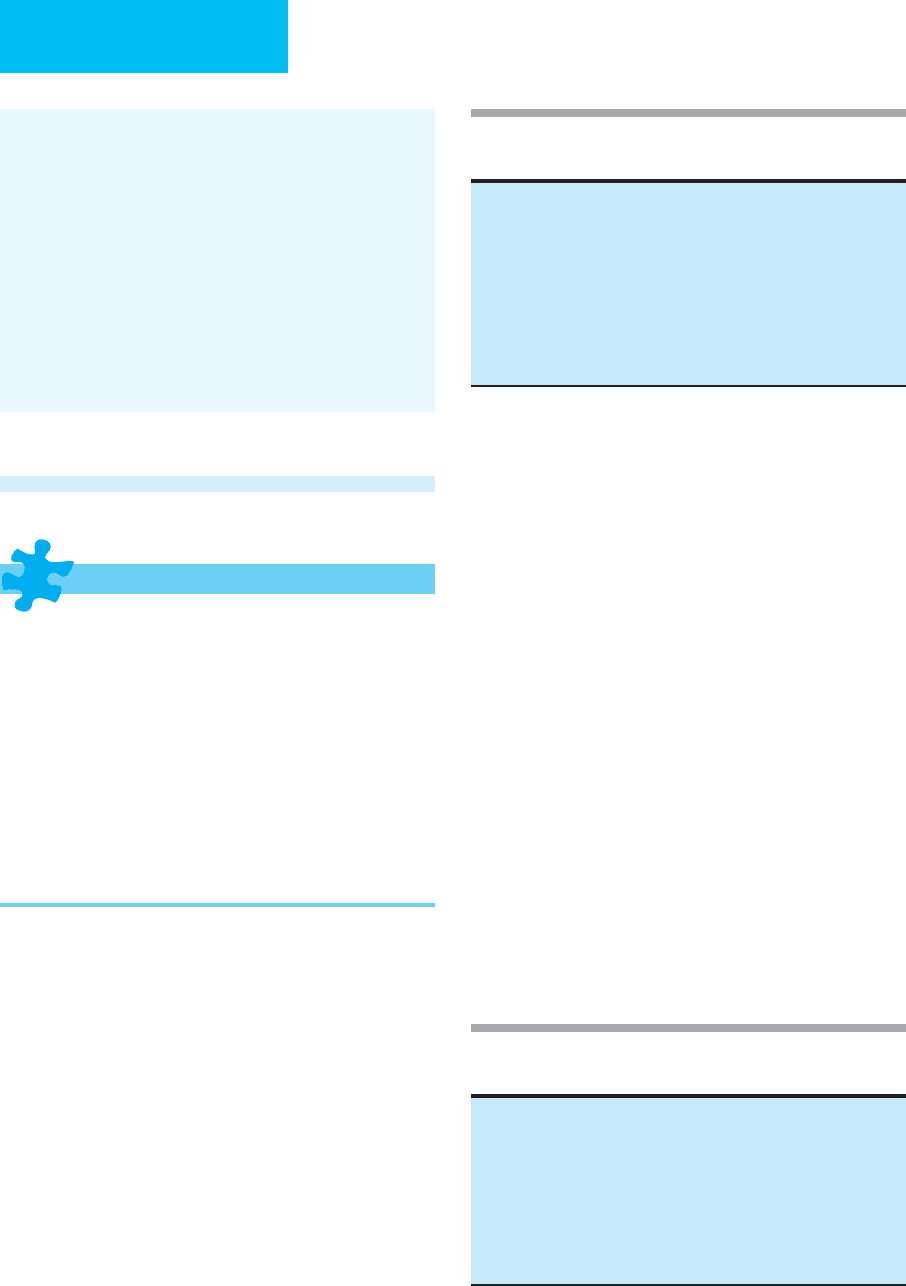
Table 12–12. Some variables used to predict success
during weaning from mechanical ventilation.
Ventilatory capacity
.
V
E
(on ventilator) <10 L/min and
.
V
E
(spontaneous) =
.
V
E
(on ventilator)
V
T
>5 mL/kg; VC >10–15 mL/kg
Spontaneous f <25/min
Maximum negative inspiratory pressure <–25 cm H
2
O
Maximal voluntary ventilation (MVV) >2 x
.
V
E
(ventilator)
Ventilatory requirement
Pa
O
2
>60 mm Hg with F
IO
2
<0.50
V
D
/V
T
<0.50
Combined indices
<100 breaths/min/L
Successful 30-minute spontaneous breathing trial
f breaths/min
V
T
(L)
RESPIRATORY FAILURE
279
the patient can be extubated. Otherwise, the duration of T-
tube sessions is increased depending on the patient’s
response. In between sessions, the patient is reconnected to
the mechanical ventilator in the assist-control mode. In some
patients, a T-tube session may be as short as 5–10 minutes at
first, with very gradual lengthening. The sessions may be
repeated two to four times daily depending on patient toler-
ance. It is important to strike a balance between excessive res-
piratory muscle fatigue during the sessions and adequate time
for the patient to assume some of the work of breathing.
A variation of the T-tube weaning method uses the venti-
lator circuit and ventilator to provide the air-oxygen mixture
during spontaneous breathing rather than a separate T tube.
This method allows for monitoring and warning of low
spontaneous tidal volume. However, some ventilator circuits
during spontaneous ventilation require much more patient
effort than the conventional T tube. Some mechanical venti-
lators provide gas mixtures to spontaneously breathing
patients with minimal work and effort by using continuous
flow or bypass circuits.
2. Intermittent mandatory ventilation (IMV)—This
mode was described earlier. The number of mechanical ven-
tilator breaths each minute is decreased gradually over hours
or days while the patient provides a progressively increasing
share of the breaths taken each minute. The IMV mode in
some mechanical ventilators requires that the patient do
excessive work during the spontaneous breaths, and for this
reason, patients may tire easily. Despite encouraging data
when IMV was first used in the 1970s, there is no evidence
that IMV facilitates weaning in patients with lung disease or
in those who are difficult to wean. IMV has the advantage of
providing good monitoring of the patient during weaning,
with breath-by-breath spontaneous tidal volume and rate
displayed by most ventilators.
3. Pressure-support ventilation—The theoretic advan-
tages of PSV were outlined earlier. During weaning by this
technique, the pressure-support pressure is chosen initially
to achieve a tidal volume of 6–8 mL/kg and a respiratory rate
less than about 20 breaths/min. Pressure-support pressure
then is decreased gradually until the patient’s own tidal vol-
ume without pressure support is adequate. Mechanical ven-
tilation usually can be discontinued when the pressure
support is less than 7–10 cm H
2
O.
When it is desired to rest the inspiratory muscles tem-
porarily, either pressure-support pressure can be increased
until tidal volume reaches the desired level with little or no
patient effort or using conventional mechanical ventilation.
A few studies comparing PSV to T-tube weaning and IMV
have been completed, and T-tube weaning and PSV are sim-
ilarly more successful than IMV weaning. It is likely that PSV
and T-tube weaning will both be useful depending on patient
selection and clinician preference.
4. Noninvasive positive-pressure ventilation—
Noninvasive positive-pressure ventilation has potential benefits
in the weaning process after the patient is extubated. Some
studies have suggested that patients who are marginal wean-
ing candidates (eg, those with COPD with high ventilatory
requirements or low ventilatory capacity) may be extubated
successfully with the assistance of face-mask noninvasive
positive-pressure ventilation. The advantages might be
decreased duration of intubation, fewer complications, and
shorter hospital stays. Other studies have found that patients
who have failed weaning or extubation might be temporarily
supported using noninvasive positive-pressure ventilation
rather than reintubation. Recent studies have not shown par-
ticular benefit in selected and unselected patients. Further
studies are necessary to determine the precise role and out-
come of noninvasive positive-pressure ventilation in wean-
ing. If used, however, candidates should be selected carefully
and monitored closely.
5. Other methods—Facilities that specialize in manage-
ment and weaning of long-term ventilator-dependent
patients may be a less costly alternative than the ICU in
selected patients. A number of specialized centers have
reported considerable success in weaning patients after very
prolonged mechanical ventilation.
Anzueto A et al: Incidence, risk factors and outcome of baro-
trauma in mechanically ventilated patients. Intensive Care Med
2004;30:612–9. [PMID: 14991090]
Boles JM et al: Weaning from mechanical ventilation. Eur Respir J
2007;29:1033–56. [PMID: 17470624]
Branson R: Understanding and implementing advances in ventila-
tor capabilities. Curr Opin Crit Care 2004;10:23–32. [PMID:
15166846]
Conti G et al: A prospective, blinded evaluation of indexes pro-
posed to predict weaning from mechanical ventilation.
Intensive Care Med 2004;30:830–6. [PMID: 15127195]
Esteban A et al: Noninvasive positive-pressure ventilation for
respiratory failure after extubation. N Engl J Med 2004;350:
2452–60. [PMID: 15190137]
Girou E et al: Association of noninvasive ventilation with nosoco-
mial infections and survival in critically ill patients. JAMA
2000;284:2361–7. [PMID: 11066187]
Haitsma JJ: Physiology of mechanical ventilation. Crit Care Clin
2007;2:117–34. [PMID: 17368160]
Jonson B: Elastic pressure-volume curves in acute lung injury and
acute respiratory distress syndrome. Intensive Care Med
2005;31:205–12. [PMID: 15605228]
Kallet RH, Branson RD: Do the NIH ARDS Clinical Trials Network
PEEP/F
IO
2
tables provide the best evidence-based guide to bal-
ancing PEEP and F
IO
2
settings in adults? Respir Care
2007;52:461–75. [PMID: 17417980]
Klompas M: Does this patient have ventilator-associated pneumo-
nia? JAMA 2007;297:1583–93. [PMID: 17426278]
MacIntyre NR et al: Evidence-based guidelines for weaning and
discontinuing ventilatory support: A collective task force facili-
tated by the American College of Chest Physicians, the
American Association for Respiratory Care, and the American
College of Critical Care Medicine. Chest 2001;120:375–95S.
[PMID: 11742959]
CHAPTER 12
280
Myers TR, MacIntyre NR: Does airway pressure release ventilation
offer important new advantages in mechanical ventilator sup-
port? Respir Care 2007;52:452–8. [PMID: 17417979]
Ni Chonghaile M, Higgins B, Laffey JG: Permissive hypercapnia:
Role in protective lung ventilatory strategies. Curr Opin Crit
Care 2005;11:56–62. [PMID: 15659946]
Peigang Y, Marini JJ: Ventilation of patients with asthma and
chronic obstructive pulmonary disease. Curr Opin Crit Care
2002;8:70-6. [PMID: 12205409]
Rothaar RC, Epstein SK: Extubation failure: Magnitude of the
problem, impact on outcomes, and prevention. Curr Opin Crit
Care 2003;9:59–66. [PMID: 12548031]
Vitacca M et al: Assessment of physiologic variables and subjective
comfort under different levels of pressure support ventilation.
Chest 2004;126:851–9. [PMID: 15364766]
ACUTE RESPIRATORY FAILURE FROM SPECIFIC
DISORDERS
Neuromuscular Disorders
ESSENTIALS OF DIAGNOSIS
May present with decreased ventilation owing to respi-
ratory muscle weakness (usually high respiratory rate
with low tidal volume) or decreased ventilatory drive
(low respiratory rate and tidal volume).
PaCo
2
>50 mm Hg.
VC <55% of predicted or less than 1500 mL may be
associated with hypercapnia.
Neuromuscular disorders often lead to atelectasis, aspi-
ration, pneumonia, hypoxemia, and poor cough reflex.
Suspect respiratory muscle weakness in all patients
with neuromuscular weakness; general muscle strength
does not always correlate with respiratory function.
General Considerations
Respiratory failure from neuromuscular diseases results from
respiratory muscle weakness or abnormal control of ventila-
tion. Muscle weakness or paralysis can result from disease in
any part of the nervous system involved with motor activity.
Problems with control of ventilation are seen in diseases that
affect the O
2
and CO
2
chemoreceptors, their connections to
the CNS, or the integrative and autonomic parts of the brain
stem, primarily the medulla.
In addition to respiratory failure, neuromuscular disease
can be associated with a number of other respiratory mani-
festations (Table 12–13). For critically ill patients, complica-
tions of nonneurologic diseases and treatment may include
neuromuscular weakness (eg, electrolyte abnormalities, cor-
ticosteroid myopathy, hypothyroidism, and peripheral neu-
ropathy) and depressed ventilatory drive (eg, sedatives and
opioid analgesics).
Pathophysiology
Respiratory failure in neuromuscular disease is due to weak-
ness of the intercostal muscles and the diaphragm. However,
other factors contribute to abnormal gas exchange
(Table 12–14). Acute weakness of inspiratory and expiratory
muscles results in a rapidly progressive decrease in vital
capacity and alveolar hypoventilation with hypoxemia. In
most cases, the mechanical properties of the chest wall are
altered, but the lungs are normal unless complications occur.
On the other hand, chronic neuromuscular disease may alter
the lungs and chest wall. Other factors that contribute to dif-
ferences in the presentation of respiratory failure include the
age of the patient at onset of disease, the distribution of mus-
cle weakness, a chronic or relapsing course, and the presence
of underlying lung or heart disease.
A. Normal Respiratory Muscles—Respiratory muscles
include the diaphragm, the intercostal muscles, muscles in the
neck that can generate additional respiratory effort, and mus-
cles of the abdominal wall. Other muscles play a key part in
ventilation, including muscles in the upper airway and the
smooth muscles of the lower airways. Respiratory muscles can
be divided into inspiratory and expiratory muscles, although
some are used during both parts of the respiratory cycle. The
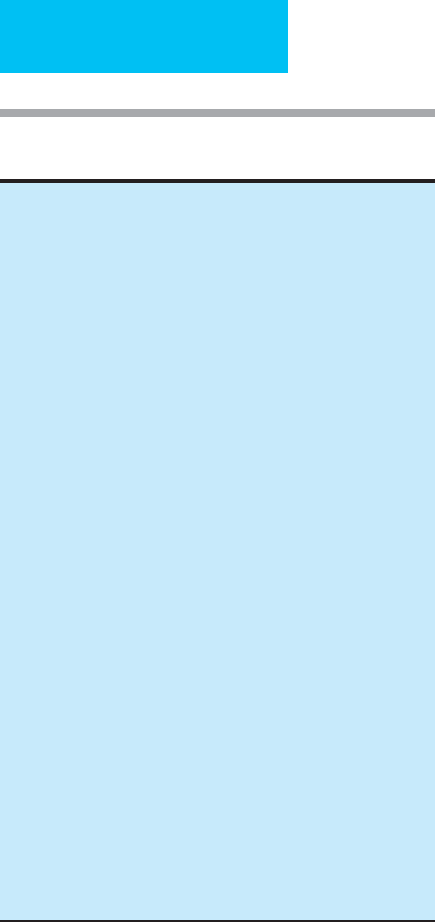
Table 12–13. Respiratory complications of neuromuscular
disease.
Hypercapnic respiratory failure
Hypoxemia
Pneumonia
Aspiration of gastric contents
Pulmonary edema
Abnormal ventilatory pattern
Upper airway obstruction
Atelectasis
Respiratory alkalosis
Pulmonary embolism
Table 12–14. Physiologic consequences of neuromuscu-
lar disease.
Decreased lung volumes
Alveolar hypoventilation
Decreased lung compliance
Increased chest wall compliance (acute weakness)
Decreased chest wall compliance (chronic spastic paralysis)
Abnormal abdominal wall mechanics
Ventilation-perfusion maldistribution
Atelectasis
Impaired cough effectiveness

RESPIRATORY FAILURE
281
diaphragm generates negative intrathoracic pressure during
contraction by pulling downward toward the abdomen.
However, if abdominal wall muscles contract simultaneously
with the diaphragm, the net effect is rather to pull the lower
margins of the rib cage upward and outward, thereby expand-
ing the thoracic volume. Muscles in the neck assist inspiratory
efforts, especially when the work of breathing is increased,
high ventilation is needed, the lungs are hyperinflated, or the
diaphragm becomes fatigued. These accessory muscles include
the sternocleidomastoids and scalenes.
Exhalation is usually passive, but normal subjects can
increase expiratory flow by contracting expiratory muscles
and generating higher positive intrathoracic pressures. Even
passive exhalation depends on respiratory muscles, however,
because passive expiratory flow is proportionate primarily to
airway caliber and lung elastic recoil; both these factors are
maximized at high lung volume, which requires good inspi-
ratory muscle strength to achieve.
B. Lung Volumes in Neuromuscular Disorders—Vital
capacity (VC) and inspiratory capacity (IC) are diminished
because of decreased ability to expand the lungs and chest wall
against passive inward recoil of those structures. While
decreased IC contributes to decreased total lung capacity
(TLC), the other component of TLC is the functional residual
capacity (FRC), often considered to be determined by the pas-
sive balance between inward recoil of the lung and outward
recoil of the chest wall at end expiration. But FRC does change
with the onset of neuromuscular weakness. For example, nor-
mal volunteers given submaximal doses of muscle relaxants
had about a 10% decrease in VC and TLC, but FRC decreased
about 20% as a result of decreased stiffness of the chest wall.
In patients with myasthenia gravis given pyridostigmine, an
increase in FRC correlating with an increase in respiratory
muscle strength was found. A study of stable patients with
moderate respiratory muscle weakness found that VC aver-
aged about 50% of predicted from height and age, TLC about
67% of predicted, and FRC about 79% of predicted.
In chronic neuromuscular disease, both altered chest wall
compliance and reduced lung compliance contribute further
to decreased FRC. Chest wall compliance in patients with
spinal cord injury and spastic paralysis of chest wall muscles
may be only 70% of normal. Small tidal volumes reduce lung
compliance, adversely affecting surfactant distribution and
perhaps stiffening and shortening lung fibrous and elastic
tissues from chronically reduced lung expansion.
C. Inadequate Cough—Inadequate cough, with retention of
secretions and increased tendency to pneumonia and atelec-
tasis, is the most common and important problem seen in
patients with neuromuscular weakness. Coughs are most
effective in removing secretions from airways if large shear
forces are generated by high-velocity gas movement in the
airways. In normal individuals, coughs are initiated at high
lung volumes, depend on vigorous contraction of expiratory
muscles to compress airways and generate high positive
intrathoracic pressures, and are released explosively. The
patient with neuromuscular weakness cannot produce effec-
tive cough if these three components are compromised.
The combination of low lung volume, impaired cough,
and accumulation of secretions leads to atelectasis. At low
lung volumes, alveoli are strongly influenced by surface forces
generated at the interface between the alveolar gas and the
wetted surface of the alveoli. This surface tension increases
the tendency of the alveoli to collapse. Airway secretions also
contribute to atelectasis by obstructing inward airflow and
allowing alveolar gas to be absorbed into the blood.
D. Abnormal Control of Ventilation—As described earlier,
alveolar ventilation in normal individuals is adjusted to regu-
late Pa
CO
2
. Hypoxemia also stimulates respiration but does not
play an active role in normal individuals at sea level. Neurologic
disorders that affect the central or peripheral chemoreceptors,
the integrative centers in the brain stem, or the primary outputs
to the respiratory muscles (phrenic nerves) may lead to inap-
propriate ventilation for the metabolic requirements of the
patient. Both hypoventilation and hyperventilation may be
seen depending on the site of the neurologic problem.
Clinical Features
Symptoms, signs, and laboratory findings depend on the
type of neuromuscular disorder leading to respiratory failure
(Table 12–15). Common to all forms of respiratory failure in
neuromuscular diseases are hypoxemia, hypercapnia, atelec-
tasis, poor cough, and risk of development of pneumonia
and other complications. Deep venous thrombosis and pul-
monary embolism are common in immobilized patients.
Occasionally, patients who have difficulty in weaning from
mechanical ventilation are found to have an unsuspected pri-
mary or secondary neuromuscular disorder.
A. Disorders of Ventilatory Control—Impaired ventilatory
control owing to a primary neurologic disorder is a relatively
unusual cause of respiratory failure. Patients present with low
respiratory rate and tidal volume, fluctuating uncoordinated
breathing patterns, or markedly periodic breathing. Diseases
that affect the medullary centers, including poliomyelitis and
cerebrovascular disease, as well as depression by CNS drugs or
hypothyroidism, can suppress the respiratory rhythm and out-
put from the autonomic nervous system. In patients with
impaired ventilatory control, clinical findings are related pri-
marily to the effects of respiratory failure on gas exchange in
addition to the consequences of the underlying disease. If CNS
depression from opioid or sedative drugs is present, patients
often will be lethargic or comatose. Other manifestations of
autonomic dysfunction such as hypertension or hypotension
and bradycardia or tachycardia can be seen in medullary
infarction. Furthermore, infarction or ischemia of the medulla
often results in characteristic effects on other neurologic path-
ways, including motor and sensory long tracts. A largely
reversible disorder of ventilatory control may be seen in
patients who have intermittent and transient hypoxemia, such
as seen in those with severe sleep-disordered breathing or
obstructive sleep apnea syndrome.
CHAPTER 12
282
B. Neuromuscular Weakness—Respiratory failure from
neuromuscular diseases that leave ventilatory control mech-
anisms intact usually presents with low tidal volume and,
because of the response to hypoxemia, hypercapnia, and lung
and chest wall mechanoreceptors, increased respiratory fre-
quency. There are some differences between the clinical pic-
tures depending on the particular disorder.
1. Muscle disease—Primary muscle diseases can be con-
genital or acquired. All can result in respiratory failure
when severe, including the congenital muscular dystro-
phies, inflammatory muscle disorders such as polymyositis
and dermatomyositis, drug-induced muscle weakness from
such agents as corticosteroids, and muscle weakness caused
by electrolyte and metabolic disturbances, including
hypokalemia, hypophosphatemia, hypothyroidism, hyper-
thyroidism, and chronic renal failure. Muscle weakness may
not affect all muscle groups equally. Proximal muscles may
be more severely affected in some muscular dystrophies, and
even when respiratory failure is developing, there may be
poor correlation between the strength of the extremity mus-
cles and that of the respiratory muscles. Myotonic dystrophy,
a rare disorder presenting with weakness and myotonic phe-
nomena including impaired muscular relaxation, imposes
the additional burden of a stiff chest wall and increased work
of breathing.
The myopathic effects of corticosteroids can exacerbate
the effects of the underlying disease for which the drug is
administered, and corticosteroid-induced weakness in
patients with asthma or interstitial pneumonitis can con-
tribute substantially to respiratory impairment. A syndrome
associated with use of neuromuscular junction blocking
agents and corticosteroids can cause weakness and failure to
wean from mechanical ventilation. In some of these patients,
both evidence of myopathic changes on muscle biopsy and
neuropathic changes evidenced by nerve conduction studies
have been found. Hypokalemia and hypophosphatemia also
may precipitate respiratory failure in ICU patients.
Myxedema is associated with muscle weakness and elevated
plasma creatine kinase. Muscle weakness seen in thyroid dis-
ease is generally correlated with the severity of thyroid dis-
ease and corrects with treatment.
Patients with a variety of critical illnesses can develop a
syndrome called critical illness myopathy. This disorder has
been associated with critical illness polyneuropathy but may
occur alone. Clinically, these patients develop muscle weak-
ness during treatment for serious illness, although no specific
cause of muscle injury can be identified. Histopathologic
changes may include variation in muscle fiber size, fiber atro-
phy, angulated fibers, fatty degeneration, fibrosis, and single-
fiber necrosis, but there are no inflammatory changes. There
are structural differences between patients who receive corti-
costeroids and those whose muscles are affected by some
combination of cytokines and myotoxic substances.
Common predisposing conditions include ARDS, pneumo-
nia, liver and lung transplantation (possibly related to corti-
costeroids), liver failure, and acidosis. Because of common
predisposing conditions, critical illness polyneuropathy
should be distinguished from this syndrome. Both are asso-
ciated with difficulty in weaning from mechanical ventilation
and sometimes are not suspected until this stage of respira-
tory failure.
Primary muscle disorders often can be distinguished
from peripheral neuropathy by the absence of sensory find-
ings and by electromyography.
2. Peripheral neuropathies—Peripheral nervous system
disorders can be divided into those that affect the neuromus-
cular junction and those that affect the peripheral nerves.
Peripheral neuropathies, although seen in many disorders
such as vasculitis, diabetes mellitus, vitamin deficiencies,
Table 12–15. Neuromuscular diseases associated with
respiratory failure.
Medullary center injury or depression
Poliomyelitis
Cerebral vascular disease
Hypothyroidism
Narcotic and sedative drug overdosage
Primary muscle diseases
Muscular dystrophy
Myotonic dystrophy
Polymyositis, dermatomyositis
Drugs: corticosteroids
Hypokalemia, hypophosphatemia
Critical illness myopathy
Peripheral nerve diseases
Peripheral neuropathies
Guillain-Barré syndrome
Vasculitis
Diabetes
Vitamin deficiency
Toxin exposure
Infection
Infiltrative diseases
Critical illness polyneuropathy
Neuromuscular junction diseases
Myasthenia gravis and cholinergic crisis
Botulism
Tick paralysis
Drugs: paralyzing agents, aminoglycosides
Spinal cord injury and disease
Trauma
Poliomyelitis
Amyotrophic lateral sclerosis
Malignancy
Paraspinous or parameningeal abscess
Diaphragmatic paralysis
Cerebral cortical diseases
Stroke
Extrapyramidal disorders
Neurogenic pulmonary edema

RESPIRATORY FAILURE
283
toxin exposure (eg, lead), infections, and infiltrative diseases,
cause respiratory failure only rarely. For ICU patients, the
most important disorders are acute polyradiculoneuritis
(Guillain-Barré syndrome) and critical illness polyneuropa-
thy. Guillain-Barré syndrome is a demyelinating disease that
is seen most often several weeks after nonspecific viral or
other infectious illnesses, although the primary illness may
be asymptomatic or difficult to pinpoint. Some variants have
a strong association with prior Campylobacter jejuni infec-
tion. Clinical findings include ascending paralysis and sen-
sory involvement initially of the lower extremities. In
patients whose disease progresses over the course of about
2–4 weeks, involvement of the respiratory muscles, upper
extremities, and trunk may contribute to respiratory failure.
Autonomic instability may further complicate diagnosis and
management. Variants of Guillain-Barré syndrome may have
different patterns of involvement, making diagnosis more
difficult. About 5% of Guillain-Barré syndrome patients ini-
tially have ataxia, ophthalmoplegia, and aflexia with less
striking extremity weakness (Miller-Fisher variant). Other
variants have purely motor or sensory involvement only.
Critical illness polyneuropathy is associated with sepsis
and multiple-organ failure. Manifestations include muscle
weakness and wasting and findings suggestive of peripheral
neuropathy. Patients have flaccid weakness and loss of deep
tendon reflexes. There is no evidence that metabolic or nutri-
tional factors or inflammation play a major role. The histo-
logic appearance of primary axonal degeneration and
denervation is consistent with widespread primary nerve
injury. It has been speculated that the association with failure
of other organ systems indicates that peripheral neuropathy is
another marker of severe systemic illness. Critical illness
polyneuropathy is associated with respiratory failure and dif-
ficulty in weaning from mechanical ventilation. As many as
70% of patients with sepsis and multiple-organ failure have
primary axonal degeneration of motor and sensory fibers,
and 30% have difficulty in weaning from mechanical ventila-
tion, limb muscle weakness, or diminished muscle reflexes.
Electrophysiologic studies show reduction or absence of mus-
cle and sensory action potentials, but slowing of nerve con-
duction or nerve conduction blocks is absent. Clinically,
patients with critical illness polyneuropathy should be evalu-
ated for botulism, Guillain-Barré syndrome, prolonged effects
of muscle relaxants, and critical illness myopathy. Some inves-
tigators do not make a distinction between critical illness
polyneuropathy and myopathy; the disorders are part of a
continuum of associated complications of critical illness.
3. Neuromuscular junction disorders—Neuromuscular
junction disorders include myasthenia gravis, an immuno-
logic disease caused by antibodies to acetylcholine receptors;
botulism, in which a specific neurotoxin produced by
Clostridium botulinum is ingested; and drug-induced disor-
ders, including pharmacologic blockade of the neuromus-
cular junction by paralyzing agents or inadvertent blockade
by aminoglycosides and other drugs. Myasthenia gravis
occasionally has gone unrecognized until it was severe
enough to present with respiratory failure. Botulism should
be suspected if there is descending paralysis and an appropri-
ate clinical history. On occasion, botulism results from toxin
produced by organisms infecting a wound, often in associa-
tion with parenteral drug abuse. Weakness or difficulty in
weaning in ICU patients should prompt a review of medica-
tions that can affect the neuromuscular junction. Rarely,
these include calcium channel blockers, quinidine, pro-
cainamide, and lithium.
4. Spinal cord disorders—Acute cervical spinal cord
injury resulting in quadriplegia may cause near-total respira-
tory muscle paralysis if above the C3 level, but some function
of neck muscles still may be present. If injury is below C3–4,
diaphragmatic activity may be preserved, but respiratory
failure may develop. In this setting, rib cage movement may
be paradoxical, with inspiratory effort causing the chest wall
to move inward because of flaccid paralysis of intercostal
muscles. The mechanical efficiency of the diaphragm is also
diminished as a result of flaccid paralysis of abdominal wall
muscles, and cough effectiveness is greatly reduced. With
time, the chest wall and abdominal wall become less compli-
ant as muscles become spastic. In some patients, these
changes may allow spontaneous efforts to become sufficient
to maintain ventilation.
Other spinal cord diseases presenting with respiratory
failure include poliomyelitis and amyotrophic lateral sclero-
sis. Poliomyelitis has a variable prognosis, with both weak-
ness and inability to protect the upper airway contributing
to potential respiratory failure. Amyotrophic lateral sclero-
sis is progressive, and respiratory failure is inevitable and
irreversible.
5. Diaphragmatic paralysis—Diaphragmatic paralysis
from bilateral phrenic nerve injury or disease is rare. Vital
capacity is usually less than 50% of predicted and worsens
when supine. The abdominal wall moves paradoxically
inward during inspiration, increasing the work of breathing
and making ventilation particularly inefficient for the other
muscles of inspiration. Unilateral diaphragmatic paralysis is
often well tolerated unless there is underlying lung disease or
a requirement for increased work of breathing or minute
ventilation during illness.
C. Diseases of the Cerebral Cortex—Patients with strokes
have upper motor neuron paralysis but rarely present with
primary respiratory failure. However, respiratory problems
are the most common complications of stroke, including
aspiration and lung infection owing to generalized weakness,
immobility, and aspiration. More recently, the respiratory
complications of extrapyramidal disorders such as
Parkinson’s disease have become appreciated. The increased
stiffness of the chest wall increases the work of breathing,
and there are increased respiratory complications from
immobilization. Isolated closed head injury of any kind
requiring mechanical ventilation is commonly associated

CHAPTER 12
284
with pneumonia. In one study, 41% of these patients devel-
oped pneumonia and had a longer ICU stay compared with
those without pneumonia.
A rare complication of cerebral injury is neurogenic pul-
monary edema, seen in association with head injury, stroke,
status epilepticus, and cerebral hypoxia. Although it can be
indistinguishable from other forms of pulmonary edema,
neurogenic pulmonary edema may appear and disappear
rapidly despite causing severe gas-exchange disturbances.
The mechanism of neurogenic pulmonary edema is
unknown but may be related to extreme changes in pul-
monary vascular tone in response to autonomic stimuli.
Both increased lung epithelial permeability and increased
regional lung hydrostatic pressures cause pulmonary edema.
Among critically ill patients, abnormal neurologic status
is a major factor leading to prolonged mechanical ventila-
tion, with reduced level of consciousness the most common
cause. However, the underlying neurologic problem is more
likely a systemic illness (eg, drug toxicity or metabolic
encephalopathy) rather than a primary CNS disease.
D. Laboratory Findings—Hypoxemia is common, and a
Pa
O
2
of less than 70 mm Hg on room air is likely. Hypercapnia
with acute respiratory acidosis is the key marker of respira-
tory failure owing to neuromuscular weakness or decreased
ventilatory drive. Other laboratory findings are not particu-
larly useful, but abnormal plasma electrolytes, including
decreased potassium, magnesium, calcium, and phosphorus,
may contribute to muscle dysfunction. In patients with unex-
plained neuromuscular weakness, elevated plasma creatine
kinase suggests myopathy or myositis. Thyroid function tests
may be useful even if the patient lacks the usual signs of
hypothyroidism or hyperthyroidism. Diagnosis of specific
neuromuscular disorders may be helped by electromyogra-
phy, nerve conduction studies, or nerve biopsy.
E. Imaging Studies—Complications of neuromuscular dis-
eases may be seen on chest x-ray. Atelectasis is a common
finding—either as macroatelectasis, with focal linear,
rounded, or other opacities visible on chest x-ray or evidence
of segmental, lobar, or other collapse, or in some cases with no
chest x-ray findings but only hypoxemia and an increased
P(
A
–a)
O
2
. In one study, 95% of patients with neuromuscular
disease requiring mechanical ventilation had atelectasis at some
time, most often as lobar atelectasis in the dependent lungs.
Aspiration pneumonia is another common respiratory compli-
cation of neuromuscular diseases. Although dependent areas of
the lungs are involved most often, new alveolar or interstitial
infiltrates anywhere in the lungs suggest pneumonia.
When assessing neurologic disorders associated with res-
piratory failure, CT scanning is not often useful in evaluating
the brain stem and has variable usefulness for spinal cord
abnormalities. MRI is highly effective for imaging these
areas, but patients cannot undergo MRI while being sup-
ported with mechanical ventilation.
F. Assessing Respiratory Muscle Strength—Prediction of
respiratory failure in these disorders involves assessment of
respiratory muscle strength. Adequate respiratory muscle
function requires both inspiratory and expiratory strength,
but neither maximum inspiratory pressure nor expiratory
pressure strongly correlates with general muscle strength. In
patients with polymyositis or other proximal muscle
myopathies presenting with generalized weakness, mean
maximum inspiratory and expiratory airway pressures aver-
aged about 50% of normal in one study, whereas at the same
time the average of maximum inspiratory and maximum
expiratory pressures were less than 70% of predicted in
about two-thirds of patients. Pa
CO
2
was inversely correlated
with both respiratory muscle strength and VC expressed as a
percentage of predicted. Hypercapnia was especially likely
when VC was less than 55% of predicted. In a study of
patients with Guillain-Barré syndrome, one-half of patients
developed respiratory failure. These had a mean VC when
intubation was required of about 15 mL/kg compared with
more than 40 mL/kg for nonintubated patients.
In patients with progressive neuromuscular weakness
who are at risk of respiratory failure, a reasonable approach
is to follow VC daily or more often if necessary. If VC falls
below about 20 mL/kg, is less than 55% of predicted, or
decreases below 1500 mL in an adult, respiratory failure
should be anticipated and arterial blood gases measured.
Intubation and mechanical ventilation (or noninvasive ven-
tilation if rapid reversal is expected) may be necessary if there
is progressive hypercapnia. Although some investigators rec-
ommend using the mean or sum of maximum inspiratory
and expiratory pressures rather than VC measurements, VC
is usually obtained more easily in the ICU.
Treatment
In most cases, treatment of respiratory failure owing to neu-
romuscular disease is supportive, including airway protec-
tion and mechanical ventilation. The exceptions are the few
diseases for which specific treatment is available, including
electrolyte abnormalities, myasthenia gravis, botulism, thy-
roid disease, and corticosteroid myopathy. It is essential to
prevent respiratory complications when possible and to rec-
ognize and treat them promptly when they occur.
A. General Care—Patients with neuromuscular disorders
should have attention to airway protection, including exami-
nation of the swallowing mechanism and gag reflex, alteration
of diet if necessary, careful feeding, and attention to body posi-
tioning. Feeding by mouth or by enteral feeding tubes should
be monitored closely, especially because some neuromuscular
diseases can affect gastric emptying and intestinal motility. In
all neuromuscular disorders—even when stable—respiratory
failure can be precipitated by stress from conditions such as
pulmonary or other infections, concurrent illness such as
heart failure, major surgery, medications, or electrolyte distur-
bances. General measures such as prophylaxis for gastritis and
prevention of deep venous thrombosis should be instituted.
Prevention of atelectasis by mechanical means is contro-
versial. Incentive spirometry is not as helpful in patients with
RESPIRATORY FAILURE
285
neuromuscular weakness as in those with normal strength.
Intermittent positive-pressure breathing (IPPB) seems
attractive as a way of overcoming low lung volume during
tidal breathing. However, results of studies have been mixed.
Continuous positive airway pressure (CPAP) and bilevel
noninvasive positive-pressure ventilation also have been
tried without clear success. Some studies have shown that
rotational therapy using special beds is helpful in decreasing
atelectasis and pneumonia in immobile patients.
B. Treatment of Respiratory Failure—Treatment of respi-
ratory failure in patients with neuromuscular disease
includes airway maintenance, oxygen, bronchodilators if
necessary, and use of incentive spirometry to avoid atelecta-
sis. Respiratory failure is usually of the hypercapnic variety
unless there is atelectasis or consolidation from pneumonia.
Mechanical ventilation is often necessary to perform the
work of breathing in the patient with muscle weakness who
develops hypercapnia.
If respiratory drive is inadequate, the assist-control mode is
used with volume-preset ventilation. There is little rationale
for IMV or pressure-control ventilation, and pressure-support
ventilation cannot be used unless the patient can initiate and
sustain inspiratory efforts. Lung compliance and resistance are
normal in the absence of secondary pulmonary complications.
Unless and until ventilation-perfusion maldistribution devel-
ops, high concentrations of supplemental oxygen are not
needed. As in patients with obstructive or interstitial lung dis-
ease, tidal volumes should be limited to 6–8 mL/kg of ideal
body weight. PEEP may be quite helpful in decreasing atelec-
tasis and for reducing the sense of dyspnea in some patients.
Patients with specific neuromuscular diseases may pres-
ent with different needs. If respiratory muscle weakness is the
primary problem but ventilatory control is intact, pressure-
support ventilation may be suitable. In some disorders, it
may be desirable to rest the respiratory muscles entirely. The
assist mode does not “rest” inspiratory muscles as much as
the control mode—that is, if the patient initiates the breath,
the inspiratory muscles continue to contract throughout
inspiration, whereas if the ventilator initiates the breath,
inspiration is completely passive on the patient’s part.
Pressure-support ventilation, although the inspiratory mus-
cles are not completely rested, may have potential advantages
of allowing some work to be done but with less effort.
In some patients, positive-pressure ventilation is needed
only for some part of the day eg, (at night), and the patient can
breathe well for long periods of time. Tracheostomy may be
necessary to attach the ventilator at night, or noninvasive ven-
tilation may be tried for intermittent use.
Bednarik J, Lukas Z, Vondracek P: Critical illness polyneuromy-
opathy: the electrophysiological components of a complex
entity. Intensive Care Med 2003;29:1505–14. [PMID: 12879242]
De Jonghe B et al: Critical illness neuromuscular syndromes. Crit
Care Clin 2007;23:55–69. [PMID: 17307116]
Laghi F, Tobin MJ: Disorders of the respiratory muscles. Am J
Respir Crit Care Med 2003;168:10–48. [PMID: 12826594]
MacDuff A, Grant IS: Critical care management of neuromuscular
disease, including long-term ventilation. Curr Opin Crit Care
2003;9:106–12. [PMID: 12657972]
Mellies U, Dohna-Schwake C, Voit T: Respiratory function assess-
ment and intervention in neuromuscular disorders. Curr Opin
Neurol 2005;18:543–7. [PMID: 16155437]
Polkey MI, Moxham J: Clinical aspects of respiratory muscle dys-
function in the critically ill. Chest 2001;119:926–39. [PMID:
11243977]
Rabinstein AA, Wijdicks EF: Warning signs of imminent respira-
tory failure in neurological patients. Semin Neurol
2003;23:97–104. [PMID: 12870111]
Simonds AK: Recent advances in respiratory care for neuromuscu-
lar disease. Chest 2006;130:1879–86. [PMID: 17167012]
Thoracic Wall Disorders
ESSENTIALS OF DIAGNOSIS
Chest wall anatomic deformity, chest wall stiffness, or
severe obesity.
Massive ascites, late-stage pregnancy, recent abdomi-
nal or thoracic surgery, thoracic and abdominal trauma,
and large abdominal or pelvic masses sometimes may
present with respiratory failure.
Paco
2
>50 mm Hg, usually with hypoxemia.
Low tidal volume; usually increased respiratory frequency.
Primary lung disease absent but secondary complications
frequent.
General Considerations
Thoracic wall abnormalities other than those owing to neu-
romuscular disease are relatively rare causes of respiratory
failure. However, acquired and congenital abnormalities may
result in distortion of the chest wall, mechanical disadvan-
tage of the respiratory muscles, increased work of breathing,
or limitation of chest wall expansion. Patients usually have
chronic respiratory failure with hypoxemia, hypercapnia,
and cor pulmonale but also may present with acute deterio-
ration or exacerbations. The most common chronic disor-
ders leading to respiratory failure are severe obesity of the
chest wall and abdomen, kyphoscoliosis and scoliosis, and
ankylosing spondylitis. Massive ascites, late-stage pregnancy,
recent abdominal or thoracic surgery and trauma, and
myotonic dystrophy may cause respiratory failure in a simi-
lar manner.
Pathophysiology
Thoracic cage abnormalities restrict lung expansion. Vital
capacity and total lung capacity are decreased. Functional
residual capacity (FRC) is usually decreased except in most
patients with spondylitis. Because of overall reduction in
lung volumes, FEV
1
is also usually low, but the ratio of FEV
1

CHAPTER 12
286
to VC is normal in the absence of obstructive lung disease.
Respiratory failure results from a combination of increased
work of breathing and ventilation-perfusion maldistribution
owing to restriction of expansion of the lungs and chest wall.
The mechanics of the chest wall and the diaphragm are
altered in ways unique to the type of disorder and the loca-
tion of the abnormalities.
A. Chest Wall Deformity—Scoliosis and kyphosis may be
idiopathic or due to poliomyelitis, tuberculosis, or other iden-
tifiable causes. Patients with scoliosis have an inverse relation-
ship between the severity of scoliotic deformity and the
compliance of the thoracic cage. Those who develop respira-
tory failure have the most severe thoracic deformity and low-
est chest wall compliance. Patients with scoliosis breathe at low
tidal volumes, presumably to minimize the work of breathing.
Kyphosis alone rarely is associated with respiratory failure, but
when seen together with scoliosis, it may contribute to
increased work of breathing and other abnormalities.
Ankylosing spondylitis limits rib cage expansion, and
patients tend to breathe primarily by diaphragmatic move-
ment as the thoracic cage becomes increasingly immobile.
The contribution of thoracic cage expansion to tidal breath-
ing falls as minute ventilation increases. The position of the
thoracic cage at end expiration often becomes fixed at a vol-
ume larger than in normal subjects. The chest wall therefore
exerts a greater than normal outward pull on the lungs, result-
ing in a normal or increased FRC despite low VC and TLC.
A flail chest results from severe blunt trauma outside the
hospital but occasionally from cardiopulmonary resuscita-
tion. The flail is the paradoxical inward movement of the
chest wall during inspiration, making ventilation inefficient
and worsening respiratory mechanics. Chest pain and
underlying lung contusions contribute to respiratory failure.
B. Obesity
1. Severe obesity—Severe obesity—in particular, predomi-
nantly central or truncal obesity—puts a heavy mechanical
burden on the chest wall and the diaphragm during inspira-
tion. Increased weight causes the end-expiratory position of
the chest wall and diaphragm to be more inward than nor-
mal. Thus the amount of gas that can be further expired from
the end-expiratory position (expiratory reserve volume
[ERV]) is reduced. On the other hand, the inspiratory
capacity—the maximal amount of gas that can be inspired
from the resting end-expiratory point—is normal or
increased, at least in young obese adults with no underlying
diseases. The work of breathing is increased, especially when
minute ventilation increases. The larger mass of the chest
wall and abdominal wall must be accelerated at each breath,
and additional energy is expended to move them during tidal
breathing. Small tidal volumes are usually selected by these
patients, and the ability to increase minute ventilation can be
limited and associated with severe dyspnea. It is likely that
obesity associated with more peripheral distribution of
added adipose tissue (eg, buttocks and extremities) has less
effect on respiratory function, but this has not been studied.
Obese patients are more prone to develop obstructive
sleep apnea because of a greater redundant soft tissue in the
upper airway, potentiating airway obstruction during sleep-
associated relaxation of upper airway muscles. A syndrome
of obesity-hypoventilation has been described. The mecha-
nism of this central hypoventilation is unclear but is proba-
bly associated with increased work of breathing, decreased
responsiveness of the respiratory center, and chronic hypox-
emia. These patients have daytime hypercapnia from
depressed chemoresponsiveness, increased work of breath-
ing, and abnormal pulmonary function. Patients with
obesity-hypertension syndrome often have pulmonary
hypertension and cor pulmonale.
C. Limitation of Diaphragmatic Excursion—Patients with
massive ascites, late stage of pregnancy, recent abdominal or
thoracic surgery or trauma, severe hepatomegaly, or large
pelvic or abdominal tumors may present occasionally with
respiratory problems. Most often they have basilar atelecta-
sis, low tidal volumes, and mild hypoxemia. If diaphragmatic
excursion is severely limited, these patients may develop
hypercapnia. The underlying condition may contribute to
additional problems. For example, patients with liver disease,
ascites, or tumors also may have pleural effusions, further
compromising lung function. Those with recent surgery or
trauma may be unable or unwilling to take deep inspirations
because of pain.
D. Gas Exchange and Pulmonary Hypertension—
Patients with all types of chest wall abnormalities may have
ventilation-perfusion maldistribution contributing to
hypoxemia and hypercapnia. In obesity and limited
diaphragmatic excursion, this finding has been attributed
primarily to atelectasis at the bases of the lungs because of
elevation of the diaphragm and low FRC. This is supported
by observations that obese subjects have better gas exchange
when standing than when supine and improvement in
hypoxemia and reduced P(
A
–a)
O
2
during exercise. Patients
with ascites and abdominal tumors would be expected to be
similar. In scoliosis and spondylitis, regional differences in
ventilation can be explained by differences in expansion
owing to local chest wall stiffness in spondylitis or asymmet-
ric deformity in scoliosis.
The combination of chronic hypoxemia and respiratory
acidosis along with anatomic deformity of pulmonary vessels
explains the pulmonary hypertension and cor pulmonale
seen in some patients with severe chest wall abnormalities.
For reasons that are not clear, cor pulmonale is seen more
often in chronic respiratory failure from scoliosis, sometimes
in the absence of severe gas-exchange abnormalities; it may
be related to anatomic deformity or arrested development of
pulmonary vessels.
Clinical Features
Some patients with thoracic wall abnormalities have chronic
respiratory failure with chronic hypoxemia and hypercapnia.
