Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


RESPIRATORY FAILURE
307
dead space and achieve improved gas exchange with lower
tidal volume and pressure. As such, it may be an adjunct to
low-tidal-volume methods.
A more radical method of ventilation is partial liquid
ventilation (PLV), in which the lungs are filled with a per-
fluorocarbon, a substance in which oxygen is highly solu-
ble. Conventional volume-preset ventilation is used, but
gas movement through the lungs is almost entirely by dif-
fusion. PLV has the potential advantages of overcoming
loss of surfactant, recruiting lung units without increased
airway pressure, and avoiding further lung injury. Multiple
randomized trials of PLV have failed to show improved
outcome.
D. Supportive Care—Patients with ARDS often require pro-
longed mechanical ventilation and long duration of stay in
the ICU, putting them at risk for complications of ICU mon-
itoring and therapy, infection, and prolonged bed rest.
Attention must be paid to maintaining nutrition, preventing
deep venous thrombosis and GI bleeding, and preventing
other complications. However, recognizing that deaths in
patients with ARDS often result from infection and nonres-
piratory system failure, supportive care focuses especially on
minimizing cardiovascular compromise and preventing
infection.
E. Treatment and Prevention of Infection—Infection is
a major prognostic factor in ARDS, either as the primary
cause of ARDS or secondarily as a cause of death. In one
study, the mortality rate was 78% in patients who developed
ARDS during bacteremia and 60% in those who develop
nosocomial pneumonia. In another study, infection was
absent in two-thirds of survivors but present in two-thirds
of nonsurvivors. The major infection sites were the lungs or
pleura, the abdomen, soft tissues, and other locations, and
about 5% had multiple sites of infection. Gram-negative
bacilli made up 57% of 177 isolates causing infection in
ARDS in one series, whereas gram-positive cocci were found
in 36% and other organisms in 7%. Among pneumonias,
gram-negative organisms were found in 58% and were
related to endotracheal intubation and prolonged need for
ventilatory support. The finding of gram-negative pathogens
in ARDS patients with pneumonia assumes particular
importance because those patients had only a 12% survival
rate despite appropriate in vitro sensitivity of bacteria to
administered antibiotics, whereas patients with ARDS asso-
ciated with gram-negative bacillary abdominal infections
had a 59% survival rate.
Sepsis or severe pneumonia should be suspected as the
cause of ARDS in all patients unless a highly likely alternative
is present. A primary infection site may be easily identified,
but in doubtful cases, occult lung and abdominal sources
must be investigated. Antibiotics should be selected on the
basis of clinical findings and epidemiologic data. Some
important considerations include the likelihood of gram-
negative bacilli, staphylococci, and candidemia in hospitalized
patients; previous antibiotic use; the possibility of infection
with anaerobic organisms; immunologic competence of the
patient; gastric antacid administration; and other host and
local ICU factors. Ventilator-associated pneumonia is a com-
mon complication of ARDS with prolonged mechanical ven-
tilation. The diagnosis is difficult to confirm, but new or
changing infiltrates, fever, purulent sputum, and worsening
gas exchange are usually to make the diagnosis.
F. Pharmacologic Therapy—There are at present no estab-
lished pharmacologic therapies for ARDS. Many studies have
attempted to intervene in the early stages of ALI by interrup-
tion of cytokine pathways (eg, antagonists and receptor
antagonists), inhibition of endotoxin (eg, monoclonal anti-
bodies), reduction of nonspecific inflammation (eg, corti-
costeroids and prostaglandin and leukotriene inhibitors),
and prevention of oxidant damage (eg, antioxidants such as
acetylcysteine, vitamin C, and superoxide dismutase). None
has proved to be successful.
Nitric oxide is a potent endogenous vasodilator. When
given by inhalation in low concentration, it selectively dilates
pulmonary vessels in well-ventilated regions of the lung, and
it is rapidly inactivated before reaching the systemic circula-
tion. Clinical trials have shown improvement in gas exchange
probably because of improved distribution of pulmonary
perfusion. No large study has concluded that nitric oxide
improves clinical outcome.
Diuretics such as furosemide should be given to ARDS
patients who show evidence of volume overload and are judged
to have adequate systemic intravascular volume. Diuretics
should be used judiciously to avoid volume depletion and com-
promise of right and left ventricular filling. ARDS patients
often have increased airway resistance, so inhaled β-adrenergic
agonists may be helpful as bronchodilators. These drugs also
stimulate sodium and water transport by alveolar epithelial
cells, perhaps helping to resolve pulmonary edema.
Corticosteroids have been attractive in ARDS because of
potential roles for cytokine- and inflammation-mediated
lung injury, and these drugs are potent anti-inflammatory
agents. However, a large study found no difference in overall
mortality despite some improvement in gas exchange in
patients with ARDS for at least 7 days given large doses of
corticosteroids. The role of nonsteroidal anti-inflammatory
drugs, antioxidants, and other drugs such as ketoconazole
and pentoxifylline remains unclear despite small studies
showing potential benefit. Synthetic surfactants of different
types and components have been the subject of several stud-
ies in ARDS. In most, gas exchange improves, at least tran-
siently, but survival is not improved.
Prognosis
In the first description of the syndrome of ARDS, 12 patients
were described, of whom 7 died. Despite improvement in
care, the mortality rate has changed only slightly.
Nevertheless, recent studies have been encouraging. In one

CHAPTER 12
308
study from Seattle, mortality was 50–60% in the mid-1980s
but fell to 30–40% in the late 1990s. The large National
Institutes of Health (NIH)–sponsored trial using low tidal
volumes reported mortality of 30–40%.
A. Respiratory Failure and Outcome—Previously,
patients with ARDS often died early in the course of the dis-
ease from intractable hypoxemic respiratory failure.
Hypoxemia could not be corrected adequately by adminis-
tration of high concentrations of oxygen, and survival was
often less than 3 days after onset. Accordingly, treatment
focused on reversing hypoxemia with positive end-
expiratory pressure, changes in ventilator management, and
extracorporeal membrane oxygenation. Despite signifi-
cantly improved hypoxemia, these measures have had little
or no effect on outcome. One retrospective study found that
unmatched patients who did not receive PEEP had no
higher mortality than those who were given PEEP, although
the PEEP group died later in their course. Other studies
indicate that the severity of respiratory failure at the onset of
ARDS correlates poorly with mortality rate. In another
analysis, the number of neutrophils and lack of acidosis
were associated with survival, whereas the severity of respi-
ratory failure and lung mechanics, response to PEEP, wedge
pressure, blood pressure, and cardiac output were not pre-
dictive. On the other hand, a few studies do find a correla-
tion between outcome and severity of respiratory failure,
but more closely with initial response to therapy. That is,
those patients who have a marked improvement in oxygena-
tion with initial therapy (oxygen and PEEP) at 24 hours do
significantly better than those with a poorer response. More
recently, high dead space:tidal volume ratio has been shown
to correlate with poor outcome in ARDS.
B. Nonrespiratory Organ Failure and Outcome—In one
study, death associated with ARDS was due to irreversible
respiratory failure in only 16%, and most of these died in
the first 3 days. In contrast, of the deaths in this series, most
were due to sepsis, with others resulting from cardiac, CNS,
and hepatic failure. In another study, multiple-organ-
system dysfunction was found in almost all patients with
sepsis and ARDS but much less frequently in those with
ARDS who showed no evidence of infection. The kidneys
were the most commonly affected nonpulmonary organ in
ARDS, with renal failure developing and contributing to
morbidity and mortality data in 30–50%. In a European
multicenter report, the overall ARDS mortality rate was
59%, but death occurred in 38% of cases of ARDS follow-
ing trauma and 68% of those with intraabdominal sepsis.
Probably because of decreased organ-system reserve,
patients over age 70 in this report had a mortality rate of
82%. A study of the importance of multiple-organ-system
failure in ARDS found that nonsurvivors had more severe
thrombocytopenia than survivors, as well as lower blood
pH, more liver dysfunction, and higher plasma creatinine
concentrations.
Current Controversies and Unresolved Issues
A. Fluid Management—Whether intravascular volume
should be reduced in ARDS remains a controversial issue.
Because of increased lung permeability, pulmonary edema is
maintained at pulmonary capillary hydrostatic pressures
that are normal or low. It is argued that resolution of pul-
monary edema would be facilitated by lowering microvascu-
lar hydrostatic pressure with diuretics and fluid restriction.
On the other hand, there is concern about oxygen delivery to
the tissues in the face of intravascular volume depletion.
Positive-pressure ventilation and PEEP reduce cardiac out-
put and oxygen delivery, and cardiac output is maintained
by ensuring adequate intravascular fluid volume. Sepsis and
shock, major factors in ARDS, often require massive fluid
administration because of hypotension and decreased tissue
perfusion. These factors suggest that volume expansion may
be needed and that diuretics and negative fluid balance
should be avoided.
Retrospective evidence indicates that net negative fluid
balance is desirable in ARDS. Reduction of pulmonary
microvascular pressure decreases lung water despite severe
lung injury, and cumulative net negative fluid balance and
weight loss are significantly higher in survivors compared
with nonsurvivors of ARDS. These trials have the problem
of self-selecting patients with better prognoses, but they
nonetheless suggest that fluid balance may be an important
determinant of outcome. In one study, better survival in
ARDS was found in those who had at least a 25% reduction
in pulmonary capillary wedge pressure compared with those
who did not. Survivors of ARDS had lower wedge pressures
and body weights compared with nonsurvivors, and the mean
number of days of mechanical ventilation and days of ICU
care were less in those who gained less than 1 L of fluid over
the first 36 hours. There was no detrimental effect on nonpul-
monary organ system function despite low fluid intake.
Two prospective studies shed light on this problem. In
one, a more “conservative” strategy of fluid replacement was
compared with a more liberal one. Using central venous
pressure (CVP) or pulmonary artery wedge pressure (PAWP)
for guidance, as well as urine output and mean arterial pres-
sure, ALI patients were managed according to protocols.
Over the first 7 days, there was a very small negative cumula-
tive fluid balance for the conservative protocol; the liberal
protocol resulted in a mean positive fluid balance of nearly
7000 mL. There was no difference in 60-day mortality, but
the conservative strategy resulted in shorter duration of
mechanical ventilation and duration of ICU stay. There were
no additional complications.
In the other study, randomization of ALI patients to
insertion and use of a pulmonary artery catheter or central
venous catheter showed no difference in 60-day survival or
organ dysfunction. There were more arrhythmias seen with
the pulmonary artery catheter, but no differences in incidence
of renal failure or use of vasopressors, diuretics, or dialysis.
RESPIRATORY FAILURE
309
B. Periodic Lung Recruitment—The PV curve of the
lungs, both in normal individuals and in those with ARDS,
shows hysteresis, or a different curve during inflation and
deflation. Because the inflation limb requires higher pres-
sures at the same lung volume than the deflation limb, a
relatively high transpulmonary pressure may be needed
initially to “open” lung units. For subsequent breaths, the
pressure needed for inflation is considerably smaller. This
finding has led to the recommendation for periodic
“recruitment maneuvers” superimposed on conventional
ventilatory techniques.
One kind of recruitment maneuver consists of increasing
airway pressure to 30–45 cm H
2
O and holding pressure con-
stant for 30 seconds or more while ventilator cycling is inhib-
ited. This can be done by using the continuous positive
airway pressure (CPAP) mode, with the patient heavily
sedated or paralyzed. Successful recruitment is marked by a
subsequent increase in lung compliance (lower inspiratory
plateau pressure at the same tidal volume) and lower oxygen
requirements. The frequency, magnitude, safety, and clinical
benefit of aggressive lung recruitment are not established.
These maneuvers might be considered in patients with
refractory hypoxemia, but routine use is not supported by
current evidence.
C. Prone Positioning—A number of investigators have
advocated placing the ARDS patient into the prone position.
Several studies have demonstrated improvement in Pa
O
2
in
50–75% of patients turned from supine to prone, with some
patients having prolonged benefit. The mechanism of prone
positioning appears to be the smaller volume of lung that is
compressed by the abdominal contents and heart in the
prone position and by more uniform lung ventilation.
Hypoxemia is more likely to improve during early-stage
ARDS with pulmonary edema than after significant fibrosis
develops. Because the prone position may allow adequate gas
exchange with lower values of PEEP, tidal volume, and F
IO
2
,
this technique also might be considered a lung-protective
strategy.
Recent studies vary the daily duration of prone position-
ing, use changes in Pa
CO
2
to predict benefit, and compare
prone position with PEEP and recruitment maneuvers.
While there is general agreement that Pa
O
2
increases, current
evidence does not support a survival benefit.
D. Routine Use of PV Curves—PV curves have been recom-
mended for determining optimal PEEP and tidal volume lev-
els to avoid ventilator-associated lung injury. There is no
doubt that careful PV curve analysis has been instrumental in
enhancing our understanding of lung and chest wall mechan-
ics in ARDS, but routine use is not practical for a combina-
tion of technical and clinical reasons. Of interest, some
investigators have shown that current recommendations for
minimal PEEP, optimal tidal volume, and target plateau pres-
sure match very well with data derived from PV curves.
Adhikari N, Burns K, Meade M: Pharmacologic therapies for
adults with acute lung injury and acute respiratory distress syn-
drome. Cochrane Database Syst Rev 2004;4:CD004477. [PMID:
15495113]
Brower RG et al and National Heart, Lung, and Blood Institute
ARDS Clinical Trials Network: Higher versus lower positive
end-expiratory pressures in patients with the acute respiratory
distress syndrome. N Engl J Med 2004;351:327–36. [PMID:
10793162]
Brower RG et al: Higher versus lower positive end-expiratory pres-
sures in patients with the acute respiratory distress syndrome.
N Engl J Med 2004;351:327–36. [PMID: 15269312]
Frutos-Vivar F, Ferguson ND, Esteban A: Epidemiology of acute
lung injury and acute respiratory distress syndrome. Semin
Respir Crit Care Med 2006;27:327–36. [PMID: 16909367]
Gattinoni L et al: Lung recruitment in patients with the acute res-
piratory distress syndrome. N Engl J Med 2006;354:1775–86.
[PMID: 16641394]
Gattinoni L et al: Lung recruitment in patients with the acute res-
piratory distress syndrome. N Engl J Med 2006;354:1775–86.
[PMID: 16641394]
Girard TD, Bernard GR: Mechanical ventilation in ARDS: A state-
of-the-art review. Chest 2007;131:921–9. [PMID: 17356115]
Lee-Chiong T Jr, Matthay RA: Drug-induced pulmonary edema
and acute respiratory distress syndrome. Clin Chest Med
2004;25:95–104. [PMID: 15062601]
MacIntyre N: Ventilatory management of ALI/ARDS. Semin
Respir Crit Care Med 2006;27:396–403. [PMID: 16909373]
Marini JJ: Advances in the understanding of acute respiratory dis-
tress syndrome: Summarizing a decade of progress. Curr Opin
Crit Care 2004;10:265–71. [PMID: 15258498]
National Heart, Lung, and Blood Institute Acute Respiratory
Distress Syndrome (ARDS) Clinical Trials Network: Efficacy
and safety of corticosteroids for persistent acute respiratory dis-
tress syndrome. N Engl J Med 2006;354:1671–84.
National Heart, Lung, and Blood Institute Acute Respiratory
Distress Syndrome (ARDS) Clinical Trials Network:
Comparison of two fluid-management strategies in acute lung
injury. N Engl J Med 2006;354:2564–75. [PMID: 16714767]
National Heart, Lung, and Blood Institute Acute Respiratory
Distress Syndrome (ARDS) Clinical Trials Network:
Pulmonary-artery versus central venous catheter to tuide treat-
ment of acute lung injury. N Engl J Med 2006;354:2213–24.
[PMID: 16714768]
Nuckton TJ et al: Dead-space fraction as a risk factor for death in
the acute respiratory distress syndrome. N Engl J Med
2002;346:1281–6. [PMID: 11973365]
Silliman CC: The two-event model of transfusion-related acute
lung injury. Crit Care Med 2006;34:S124–31. [PMID: 16617256]
Steinberg KP, Kacmarek RM: Should tidal volume be 6 mL/kg
predicted body weight in virtually all patients with acute
respiratory failure? Respir Care 2007;52:556–67. [PMID:
17484788]
Terragni PP et al: Tidal hyperinflation during low tidal volume
ventilation in acute respiratory distress syndrome. Am J Respir
Crit Care Med 2007;175:160–6. [PMID: 17038660]
Wheeler AP, Bernard GR: Acute lung injury and the acute respiratory
distress syndrome: A clinical review. Lancet 2007;369:1553–64.
[PMID: 17482987]
CHAPTER 12
310
Obstructive Sleep Apnea &
Obesity-Hypoventilation Syndrome
ESSENTIALS OF DIAGNOSIS
Excessive daytime somnolence with evidence of upper
airway obstruction during sleep (obstructive sleep
apnea syndrome).
Impaired ventilatory response to CO
2
and hypoxemia
(obesity-hypoventilation syndrome).
May have right-sided heart failure with cor pulmonale,
hypertension, and left ventricular dysfunction.
General Considerations
The obstructive sleep apnea-hypopnea syndrome is a com-
mon condition affecting 5% of adult men and approximately
half that number of women. This syndrome is closely associ-
ated with snoring and is characterized by repeated episodes
of upper airway collapse during sleep with resulting acute
hypercapnia, hypoxemia, sleep disruption, hemodynamic
alterations, and impairment of daytime functioning. Severely
affected individuals may develop respiratory failure and be
admitted to the ICU with marked hypercapnia, poly-
cythemia, altered mental status, and pulmonary hyperten-
sion with cor pulmonale. Alternatively, obstructive sleep
apnea may be observed in ICU patients admitted for other
indications (eg, unstable angina pectoris or cardiogenic pul-
monary edema); in such cases, the recognition and treatment
of the sleep-disordered breathing may be a critical compo-
nent of the overall ICU therapy. It should be noted, however,
that most patients with obstructive sleep apnea do not have
daytime hypoventilation and therefore do not have respira-
tory failure in the usual sense.
A. Normal Breathing during Sleep—For the purpose of
this chapter, sleep may be separated into two main types,
rapid eye movement (REM) sleep and non–rapid eye move-
ment (NREM) sleep, which differ considerably in their
effects on breathing and on upper airway resistance.
Although REM and NREM sleep stages alternate throughout
the night, the majority of REM sleep is normally concen-
trated during the latter half of the sleep period.
In normal awake individuals, the control of breathing is
influenced not only by chemical and mechanical stimuli but
also by inputs from higher cortical centers. With the transi-
tion to sleep (usually light NREM sleep), volitional influ-
ences are lost, and in addition, the responsiveness of the
central respiratory center to increasing Pa
CO
2
is blunted rel-
ative to the awake state. Upper airway caliber is also reduced
owing to both gravitational effects related to the supine posi-
tion and a decrease in the tonic activity of upper airway dila-
tor muscles, which, during wakefulness, prevent inspiratory
narrowing owing to negative intraairway pressures. The net
effects of these changes in ventilatory drive and airway cal-
iber are a slight increase in inspiratory upper airway resist-
ance and mild hypoventilation (Pa
CO
2
= 42–44 mm Hg at sea
level) relative to the awake state.
During REM sleep, respirations are irregular, and ventila-
tion appears to be, in part, under the control of behavioral
processes activated during this dreaming state. Ventilatory
responsiveness to chemical stimuli is markedly reduced, and
there is a profound suppression of skeletal muscle tone,
including the intercostal muscles and other accessory mus-
cles of respiration, but excluding the diaphragm and extraoc-
ular muscles. Although brief central apneas and hypopneas
can result in transient mild arterial oxygen desaturations,
these are clinically unimportant in normal individuals.
B. Obstructive Sleep Apnea Syndrome—In contrast to
mild narrowing of the upper airway found in normal persons,
an exaggerated response is seen in obstructive sleep apnea
syndrome, with episodic partial (hypopnea) or complete
(apnea) obstruction of the upper airway during sleep. These
events may last from 10–90 seconds and are terminated by an
arousal from sleep, resulting in sleep fragmentation. The site
of obstruction can occur at any point along the airway above
the level of the glottis, and often more than one site is
involved. A strong association of obstructive sleep apnea with
obesity in men suggests that small upper airway caliber is an
important predisposing factor, although obstructive sleep
apnea is found in nonobese individuals as well. Other poten-
tial factors include adenotonsillar hypertrophy or other
anatomic abnormalities, increased collapsibility of the upper
airway, inflammation or edema of these structures, and
abnormal neural reflexes. The degree of respiratory drive
plays a role, as does the amount of nasal airway resistance;
both these factors tend to increase the amount of intralumi-
nal negative pressure and, thereby, the tendency to collapse
the pharyngeal airway during inspiration.
Patients with obstructive sleep apnea syndrome tend to
experience most of their problems during the wake-to-sleep
transition (when ventilatory control is relatively unstable) and
during REM sleep (when respiratory muscle hypotonia and
chemical insensitivity combine to produce frequent and pro-
longed apneas). Because the threshold for arousal is relatively
low during lighter NREM sleep (stages 1 and 2), patients with
obstructive sleep apnea may alternate between these sleep
stages and wakefulness throughout the entire night and never
reach the more restorative deeper NREM stages 3 or 4. For
similar reasons, REM sleep is also typically fragmented and
reduced in quantity. While the severity of daytime sleepiness
generally correlates with the frequency of obstructive breath-
ing events, some patients may have minimal sleepiness despite
severe disruption of breathing during sleep (defined as more
than 30 apneas or hypopneas per hour).
Hemodynamic abnormalities during sleep are common
in patients with obstructive sleep apnea. Hypoxemia and
high levels of circulating catecholamines contribute to both
increased systemic and pulmonary vascular resistance. Blood

RESPIRATORY FAILURE
311
pressure peaks immediately after an arousal occurs after an
obstructive event, when a sudden increase in cardiac output
meets these high vascular resistances. The markedly negative
intrathoracic pressures during obstructed inspiratory efforts
raise the transmural myocardial pressure, further increasing
both right and left ventricular afterload. In addition to
apnea-related fluctuations in blood pressure, obstructive
sleep apnea increases the risk of daytime hypertension. This
effect has been shown to be independent of obesity, age, and
gender and is thought to be related to a “resetting” of the
carotid baroreceptors as a result of repeated hypoxemia and
repetitive bursts of catecholamines with each obstructive
event that remodels vascular tone. Left ventricular hyper-
trophy is common in patients with obstructive sleep apnea,
and left ventricular diastolic dysfunction (more often than
systolic abnormalities) may result in cardiogenic pul-
monary edema in these patients. Increased myocardial oxy-
gen requirements combined with apnea-related hypoxemia
can precipitate myocardial ischemia and present as noctur-
nal angina in patients with underlying coronary artery dis-
ease. Cardiac arrhythmias, including bradycardias and
pauses up to 13 seconds during apneas and ventricular
ectopy associated with severe desaturation, may be seen in
the most severe cases.
Obstructive sleep apnea also has been strongly associated
with coronary artery disease and stroke, although a direct
causal relationship has yet to be definitively demonstrated.
Suggested pathophysiologic mechanisms include the hemo-
dynamic abnormalities described earlier, as well as increases
in platelet activation and plasma fibrinogen that have been
reported in patients with untreated obstructive sleep apnea.
C. Obesity-Hypoventilation Syndrome—Obesity-
hypoventilation syndrome is an uncommon condition in
which usually morbidly obese individuals develop hypercapnic
respiratory failure from a combination of depressed response
to CO
2
and hypoxia, increased work of breathing, and possibly
abnormal heart and lung function. Obesity-hypoventilation
syndrome has a variable relationship to obstructive sleep apnea
perhaps because of the association of each with obesity, but
most obesity-hypoventilation syndrome patients have some
degree of obstructive sleep apnea. Obesity-hypoventilation
patients have daytime hypercapnia and decreased responsive-
ness to hypercapnia, in contrast to the majority of obstructive
sleep apnea patients, who, while awake, maintain normal Pa
CO
2
and have a normal ventilatory response to CO
2
. Patients with
obesity-hypoventilation syndrome often have pulmonary
hypertension leading to cor pulmonale.
Clinical Features
A. Symptoms and Signs—Patients with obstructive sleep
apnea may complain of daytime hypersomnolence, a history
of heavy snoring, awaking gasping for breath, and unrefresh-
ing sleep. Bed partners, if available, often provide more reli-
able information and will describe repeated periods of apnea
terminated by loud snorts and gasping. Systemic hypertension
is common. These patients may be seen occasionally in the
ICU for severe nocturnal hypoxemia, arrhythmias, cardiac
ischemia, heart failure, or altered mental status. Patients with
obesity-hypoventilation syndrome often have severe right-
and left-sided heart failure with dyspnea and pulmonary and
peripheral edema.
On examination of the obstructive sleep apnea patient,
periodic breathing may be noted during sleep. Unlike the
Cheyne-Stokes breathing pattern seen in severe heart failure,
however, the patient with obstructive sleep apnea will have
little or no airflow despite the increasing respiratory efforts.
After a time varying from seconds to minutes, the patient
arouses, may awaken briefly, and opens the airway to the
accompaniment of snoring and upper respiratory noises.
During the apnea, the patient may demonstrate use of acces-
sory muscles, intercostal retractions and paradoxical inspira-
tory chest wall movements, and movement of the neck
toward the thoracic inlet during inspiratory maneuvers.
These findings are characteristic of obstruction of the upper
airway while respiratory efforts are being made. Pulsus para-
doxus is not uncommon during apneic events.
Those with respiratory failure associated with obstructive
sleep apnea or those with obesity-hypoventilation syndrome
may have acute respiratory acidosis, which may be severe
enough to cause lethargy or coma. Other patients may seek
medical attention primarily for severe peripheral edema and
massive weight gain because of right ventricular failure from
pulmonary hypertension. Dyspnea or wheezing suggests a
component of obstructive lung disease or pulmonary edema.
Most, but not all, patients with severe sleep apnea will show
evidence of daytime hypersomnolence.
B. Laboratory Findings—Most patients with obstructive sleep
apnea have few abnormal laboratory findings when awake.
Erythrocytosis is unusual in obstructive sleep apnea alone and
suggests superimposed obesity-hypoventilation or other causes
of sustained hypoxemia. In patients seen in the ICU who pres-
ent with respiratory failure, hypercapnia and hypoxemia are
seen. Chronic CO
2
retention leads to a compensatory elevation
of plasma bicarbonate. Electrocardiography may show evi-
dence of left-sided or biventricular hypertrophy, tachycardia
or bradycardia in association with apneic events, and, rarely,
ventricular ectopy. The chest x-ray may confirm cardiomegaly,
pulmonary edema from left ventricular failure, or enlarged
pulmonary arteries in patients with pulmonary hypertension.
Patients with obesity-hypoventilation syndrome have abnor-
mally low ventilatory response to CO
2
and hypoxia.
C. Confirmatory Testing—Traditionally, confirmation of
obstructive sleep apnea has been made by polysomnography.
Measurements made during sleep demonstrate episodic
upper airway obstruction by showing periods of absence of
airflow despite evidence of inspiratory effort. Arterial
hypoxemia or O
2
desaturation proves that obstruction is
causing significant gas-exchange abnormalities. In the
sleep laboratory, the number, nature, severity, and duration of
sleep-disordered breathing events (ie, apneas and hypopneas)

CHAPTER 12
312
are carefully measured and counted. Other measurements
include electroencephalography and electrocardiography.
Portable cardiorespiratory recorders (four to six channels
including, at a minimum, airflow, respiratory effort, satura-
tion, and heart rate) are better suited for use in the ICU and
generally provide the information needed to guide treat-
ment. In some critically ill patients, diagnostic testing may
not be feasible, and a presumptive diagnosis of obstructive
sleep apnea may have to be made prior to confirmatory test-
ing. In these patients, direct observation of the sleeping
patient and pulse oximetry trends demonstrating an episodic
(sawtooth) pattern of desaturations in the ICU can be used
to initiate and titrate therapy.
Differential Diagnosis
Obstructive sleep apnea syndrome may coexist with other lung
diseases. Both obstructive sleep apnea and COPD are common
in men, and these diseases complicate each other. Severe car-
diomyopathy and CNS disease may present with periodic
breathing, dyspnea, and hypersomnolence. Obesity is associ-
ated with hypoxemia from atelectasis. Weight gain, edema,
heart failure, and hypoventilation may be seen with hypothy-
roidism. Thyroid function should be determined in all patients
considered to have obesity-hypoventilation syndrome.
Treatment
A. Mild Obstructive Sleep Apnea—Patients with mild
obstructive sleep apnea are unlikely to be seen in the ICU for
this problem alone, but this syndrome is common and may
be seen in those admitted with other diseases. In these
patients, apneic episodes occur relatively infrequently during
sleep onset and REM sleep, and daytime hypercapnia is not a
problem. Treatment is directed at weight reduction, absti-
nence from alcohol and cigarette use, treatment of nasal dis-
ease (if present), and avoidance of a supine body position
during sleep. Nocturnal nasal CPAP can be used if necessary.
Additional treatment options include mouthpieces that dis-
place the mandible anteriorly during sleep (thereby pulling
the tongue away from the posterior pharyngeal wall), and
rarely, pharyngeal surgery. Successful management should
result in reduced daytime somnolence and improvement of
such neuropsychiatric symptoms.
B. Severe Obstructive Sleep Apnea—Severe obstructive
sleep apnea may require aggressive relief of nocturnal upper
airway obstruction. Tracheostomy is very effective because of
unequivocal reversal of upper airway obstruction, but this is
very rarely required.
1. Nasal CPAP—Nasal continuous positive airway pressure
(CPAP) has become the treatment of choice for this disorder.
By providing positive pressure to the collapsible portion of
the upper airway during sleep, nasal CPAP effectively pre-
vents airway obstruction during inspiration.
Nasal CPAP is generally provided by a blower attached to
flexible tubing leading to a small mask placed over the nose or
small soft nasal prongs. A sufficient continuous flow of air is
blown into the system, and via a controllable vent, continuous
positive pressure of up to 20 cm H
2
O can be maintained. The
appropriate level of nasal CPAP is best determined during
polysomnography; however, rough approximations may be
made in the ICU by direct observation of the patient during
sleep, with upward titration of pressure until apneas, snoring,
and desaturations are eliminated. Newer “autotitrating”
devices that adjust pressure based on the shape of the inspira-
tory flow profile also can help to identify optimal pressures.
Most patients in whom it is tried, at least for the short term,
tolerate nasal CPAP, but not all patients can be managed suc-
cessfully in this way. For those unable to tolerate the required
continuous pressures, bilevel nasal ventilation may be more
comfortable and effective while allowing a high inspiratory
and a lower expiratory pressure level.
Nasal CPAP has a variable role in patients with obstructive
sleep apnea who present with respiratory failure to the ICU. In
many, nasal CPAP is sufficient to restore and maintain upper
airway patency and normalize gas exchange during sleep.
These patients probably have only mild respiratory center
depression from hypoxemia and hypercapnia. Some patients
are improved by the combination of nasal CPAP and oxygen.
On the other hand, some obstructive sleep apnea patients with
respiratory failure have little immediate response to nasal
CPAP, which suggests that upper airway obstruction is no
longer the only factor. In these patients, nasal CPAP can be
tried, but if satisfactory results are not obtained quickly, more
definitive efforts at restoring ventilation and oxygenation must
be made using mechanical ventilation.
Effective treatment with nasal CPAP is often accompa-
nied by a “rebound” of sleep, which gradually returns to
more normal quantities over several days. A spontaneous
diuresis is also seen commonly and is the result of a reduc-
tion in hypoxia-induced pulmonary vasoconstriction and a
lowering of left ventricular afterload. Hypertension may
improve or even resolve with effective nasal CPAP therapy.
2. Oxygen—Oxygen, alone or given in combination with
noninvasive positive-pressure ventilation, is given to correct
hypoxemia in the setting of respiratory failure with obstruc-
tive sleep apnea. Hypoxemia is a serious complication of this
syndrome, with potential for arrhythmias, altered mental
status, and further deterioration of ventilatory drive.
However, oxygen therapy alone typically prolongs apnea
duration, resulting in worsening hypercapnia and respiratory
acidosis.
In patients with acute respiratory failure, however, hypox-
emia is often very severe and may cause hypoxic inhibition of
central respiratory neural output and marked hypoxia of the
brain, heart, and other organs. The goal is to raise Pa
O
2
to at least
60 mm Hg for at least several days. Oxygen should be given with
careful monitoring of mental status, vital signs, respiratory rate,
and arterial blood gases. Increased hypercapnia indicating
RESPIRATORY FAILURE
313
worsening of respiratory failure with oxygen administration
should suggest the need for initiating or increasing ventilatory
support rather than discontinuing oxygen.
3. Other treatment—Endotracheal intubation or tra-
cheostomy is highly effective. In patients with localized
obstruction owing to adenotonsillar hypertrophy or nasal
polyps, surgical excision may be curative but should not be
done until the patient has been stabilized medically. Other
surgical treatments (including uvulopalatopharyngoplasty
and mandibular osteotomy with hyoid suspension) have
even less of a role in the actual setting because these proce-
dures tend only to reduce the severity of the obstruction, and
the results are difficult to predict. Diuretic administration
may be helpful if elimination of obstructive breathing events
and desaturations is insufficient to induce a spontaneous
diuresis. Pulmonary edema is often the result of left ventric-
ular diastolic dysfunction, and β-blockers may be more effec-
tive than afterload-reducing medications. There is no role for
respiratory stimulants or carbonic anhydrase inhibitors in
the treatment of obstructive sleep apnea syndrome. The use
of sedative-hypnotic agents is contraindicated in these
patients because they suppress the arousal response and
therefore tend to lengthen apneas and cause more severe O
2
desaturations.
C. Obesity-Hypoventilation Syndrome—These patients
often benefit from diuresis in response to oxygen and diuret-
ics. Because of coexisting obstructive sleep apnea, mainte-
nance of upper airway patency is essential. Mechanical
ventilation may be necessary. Left ventricular failure is
treated with diuretics with β-blockers or afterload reduction
added as indicated clinically based on estimates or objective
measures of left ventricular function.
Mechanical ventilation should not be withheld until gas
exchange becomes severely abnormal. More often, mechani-
cal ventilation is required as a temporizing measure while
oxygen and other treatment correct the acute physiologic
derangement. Mechanical ventilation is sometimes necessary
so that oxygen can be given safely in patients who have
decreased ventilatory drive. After a few days of improved
Pa
O
2
, many patients will have improved ventilatory drive and
marked attenuation of hypercapnia. Patients often will
regain significant ventilatory responsiveness to CO
2
.
Some patients can be ventilated successfully using nonin-
vasive nasal ventilation with bilevel positive-pressure
ventilation. This procedure requires careful monitoring and
observation because minute ventilation and airway patency
cannot be guaranteed as with conventional mechanical ven-
tilation using an endotracheal tube. Bilevel positive-pressure
ventilation is much like inspiratory pressure-support ventila-
tion, with increased pressure maintained at a preset level
throughout inspiration. Although backup rates can be added
(similar to pressure-controlled IMV), they generally add lit-
tle to spontaneous ventilation in these patients owing to the
limited ability of inspiratory pressure applied noninvasively
to counteract forces produced by the weight of the chest and
abdomen.
Medroxyprogesterone acetate may have a beneficial effect
in patients with chronic obesity-hypoventilation syndrome,
but its usefulness in acute respiratory failure is unclear. In the
long term, weight loss is of substantial benefit because stud-
ies have shown that even a 10% reduction in weight can
improve gas-exchange derangements.
Arzt M et al: Suppression of central sleep apnea by continuous
positive airway pressure and transplant-free survival in heart
failure: A post hoc analysis of the Canadian Continuous Positive
Airway Pressure for Patients with Central Sleep Apnea and
Heart Failure Trial (CANPAP). Circulation 2007;115:3173–80.
[PMID: 17562959]
BaHammam A, Syed S, Al-Mughairy A: Sleep-related breathing
disorders in obese patients presenting with acute respiratory
failure. Respir Med 2005;99:718–25. [PMID: 15878488]
Bradley TD et al: Continuous positive airway pressure for central
sleep apnea and heart failure. N Engl J Med 2005;353:2025–33.
[PMID: 16282177]
Caples SM, Kara T, Somers VK: Cardiopulmonary consequences of
obstructive sleep apnea. Semin Respir Crit Care Med
2005;26:25–32. [PMID: 16052415]
Dincer HE, O’Neill W: Deleterious effects of sleep-disordered
breathing on the heart and vascular system. Respiration
2006;73:124–30. [PMID: 16293956]
Giles TL et al: Continuous positive airways pressure for obstructive
sleep apnea in adults. Cochrane Database Syst Rev
2006;3:CD001106. [PMID: 16855960]
Kushida CA et al: Practice parameters for the use of continuous
and bilevel positive airway pressure devices to treat adult
patients with sleep-related breathing disorders. Sleep
2006;29:375–80. [PMID: 16553024]
Yaggi HK et al: Obstructive sleep apnea as a risk factor for stroke
and death. N Engl J Med 2005;353:2034–41. [PMID:
16282178]
314
00
Acute Renal Failure
Acute renal failure can be defined as a precipitous impair-
ment of kidney function without regard to etiology or mech-
anism. It can occur as a result of many causes, but clinical
findings, complications, and some forms of treatment are the
same in all cases. The causes can be divided into three main
groups: prerenal, resulting from rapidly reversible renal
hypoperfusion; postrenal, owing to obstruction to urine flow;
and intrinsic, owing to lesions directly involving the renal
parenchyma. In most patients, intrinsic renal failure can be
considered a diagnosis of exclusion once pre- and postrenal
causes are eliminated.
Clinical Features
Investigations useful in determining the cause and severity of
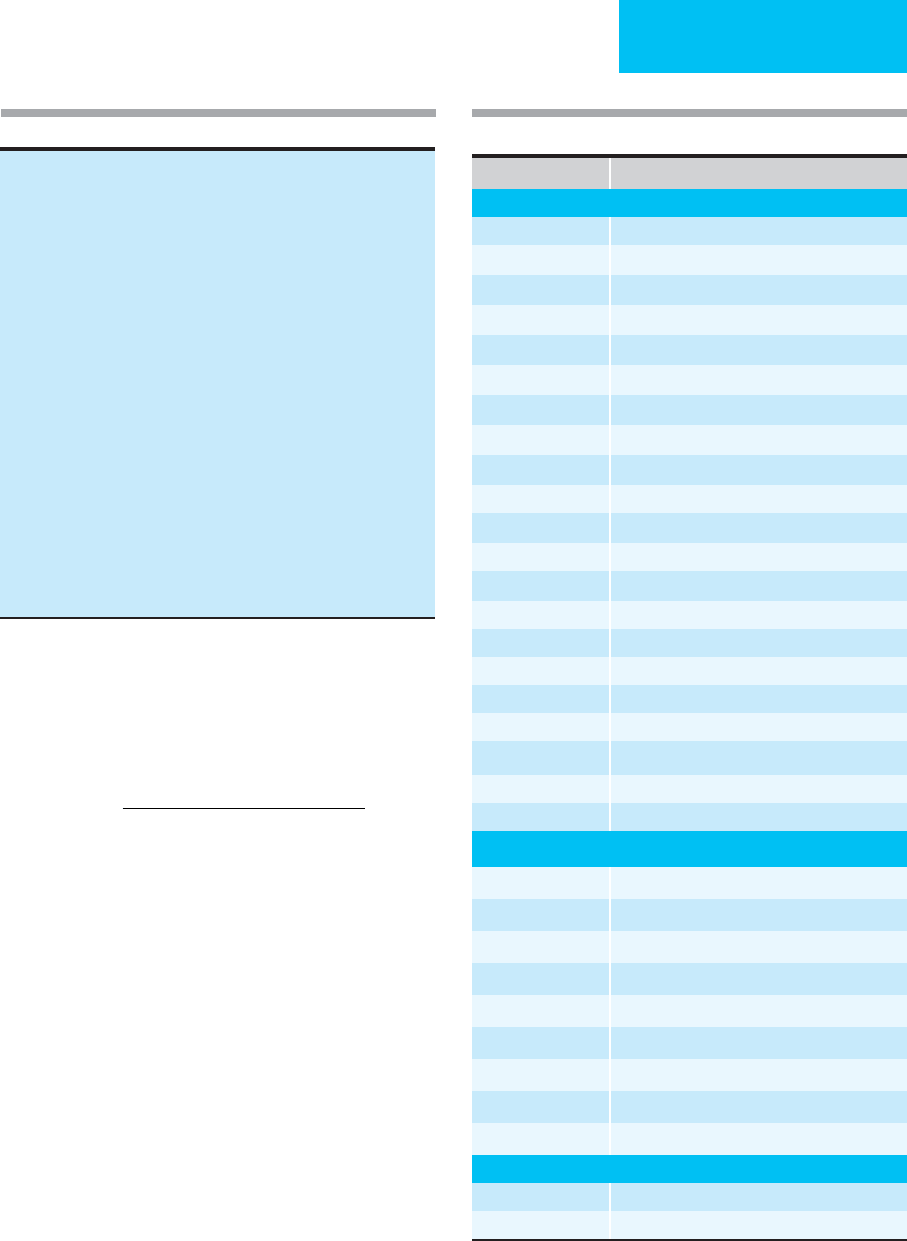
acute renal failure are listed in Table 13–1.
A. History—Noting the time of onset of renal problems
helps to differentiate between acute renal failure and the nat-
ural progression of chronic renal disease. The most com-
mon causes of chronic renal failure are diabetes,
hypertension, chronic glomerulonephritis, and polycystic
kidney disease. The patient’s drug history should seek to
identify medications known to cause renal dysfunction,
including nonsteroidal anti-inflammatory drugs (NSAIDs),
angiotensin-converting enzyme (ACE) inhibitors, and
antibiotics (Table 13–2). Exposure to hydrocarbons (car-
bon tetrachloride), ethylene glycol (antifreeze), or radio-
logic contrast agents also can cause acute renal failure.
B. Symptoms and Signs—Acute renal failure is rarely asso-
ciated with flank pain or dysuria, exceptions being condi-
tions characterized by severe renal inflammation,
crystalluria, acute obstruction, intrarenal hemorrhage, and
arterial embolization. Most of the symptoms associated with
acute renal failure are the result of renal dysfunction. Salt and
water overload, resulting in edema, hypertension, and pul-
monary congestion, is most often the result of inadequate
diuresis. Manifestations associated with acute retention of
uremic toxins include anorexia, nausea, hiccupping, vomit-
ing, hematemesis, impaired hemostasis, neuromuscular irri-
tability, asterixis, lethargy, coma, and seizures. Conditions
seen more often after prolonged uremia include pruritus,
pericarditis, and anemia. Spontaneous bone fractures owing
to secondary hyperparathyroidism and altered vitamin D
metabolism are not associated with acute renal failure, and
their presence argues strongly for chronic uremia as the
cause. Hyperkalemia owing to impaired renal excretion can
cause cardiac arrhythmias. Uremic acidosis may elicit
Kussmaul respirations.
Evaluation of intravascular volume status and degree of
hydration should include measurement of orthostatic blood
pressure and heart rate, assessment of mucosal hydration
and skin turgor, and inspection for the presence or absence
of edema (peripheral and sacral), jugular venous distention,
pulsus paradoxus, cardiac rubs or gallops, pulmonary rales,
or effusions and ascites. Equally informative are signs of
associated morbidity, including those of congestive heart
failure, cirrhosis, or systemic vasculitis.
C. Laboratory Findings—
1. Serum creatinine and glomerular filtration rate—
Creatinine is made in the muscle and released into the circu-
lation at a rate of 15–25 mg/kg per day for a middle-aged
man and 10–20 mg/kg per day for a middle-aged woman.
Under conditions of severe muscle damage (rhabdomyoly-
sis), leakage of creatinine into the serum can exceed the pre-
ceding estimates. Creatinine is excreted primarily by
glomerular filtration, with only a small percentage (10%)
secreted by the tubules and virtually none reabsorbed. The
normal glomerular filtration rate (GFR) must be reduced by
about half before there is a substantial increase in serum cre-
atinine levels (>1 mg/dL). As a result, serum creatinine is not
a reliable guide to modest decreases in renal function. In con-
trast, preexisting increases in serum creatinine support the
diagnosis of chronic renal disease.
13
Renal Failure
Andre A. Kaplan, MD
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
RENAL FAILURE
315
When creatinine levels are relatively stable over several
days, a crude estimate of the prevailing GFR can be made
using the following formula:
The result (in mL/min) is multiplied by 0.85 for a female.
This calculation is useful in providing a quick estimate of
renal function but is potentially misleading if there are sub-
sequent changes in the serum creatinine level. In order to val-
idate the calculation, a 24-hour urine collection for
creatinine is required.
During bouts of severe renal failure, serum creatinine
increases by 1–2 mg/dL per day. More rapid increases in
serum creatinine suggest rhabdomyolysis. Spurious increases
in serum creatinine can occur without declines in GFR when
certain cephalosporins or ketones (acetoacetate) interfere
with the colorimetric reaction used for its identification.
Likewise, cimetidine and trimethoprim-sulfamethoxazole
can compete for tubular secretion and result in increases in
serum creatinine unrelated to decreased GFR.
2. Urea—Urea is the major nitrogen-containing metabolite
of protein catabolism and is excreted primarily by the kid-
neys. Normally, 35–50% of filtered urea is reabsorbed by the
tubules. Under conditions of decreased renal blood flow,
GFR
age][wt (kg)]
Serum creatinine (
=
−
×
[140
72
mmg/dL)
Table 13–1. Renal assessment.
History
Physical examination
Serum chemistries
Urea, creatinine, electrolytes, abnormal serologic tests (see text)
Urine chemistries
Na, FE
Na
, urea, FE
urea
, creatinine
24-hour clearance: creatinine, urea, protein
Urinalysis
Dipstick determinations
Microscopy
Sulfosalicylic acid
Urine culture/Gram stain
Hemodynamic monitoring
Ultrasound imaging
Radiography
KUB, IVP, tomography, CT scan, MRI
Invasive radiography
Renal arteriography (selective, digital subtraction)
Retrograde pyelography
Percutaneous antegrade pyelography
Nuclear scanning
Split function studies and renal flow (DTPA, MAG-3)
Gallium scan
Renal biopsy
Drug Mechanism of Nephrotoxicity
Antimicrobial Agents
Abacavir AIN
Acyclovir Crystalluria
Aminoglycosides ATN; electrolyte-wasting
Amphotericin B ATN; electrolyte-wasting, renal tubular acidosis
Cephalosporins AIN, spurious increased creatinine
Cidofovir ARF
Ciprofloxacin AIN
Dapsone ATN
Foscarnet ATN, electrolyte-wasting, hypocalcemia
Ganciclovir ARF
Indinavir Nephrolithiasis, crystalluria, pyuria, obstruction
Meropenem ARF
Penicillins AIN
Pentamidine ATN
Polymyxin B ATN (may occur when given orally)
Quinolones AIN?
Rifampin AIN
Sulfadiazine ARF, crystalluria
Sulfamethoxazole AIN, crystals, decreased creatinine secretion
Sulfisoxazole Crystalluria
Valacyclovir ARF
Immunosuppressive Agents
Cisplatin ATN, HUS, Glomerular capillary thrombosis
Cyclosporine Intrarenal vasoconstriction
Daclizumab ATN, renal dysfunction?
Ifosfamide ARF
Interferon Prerenal azotemia? ATN?
Interleukin-2 Shock-like syndrome, prerenal azotemia
Methotrexate Crystalluria (high-dose IV)
Mitomycin HUS
Tacrolimus Intrarenal vasoconstriction
Diuretics
All Prerenal azotemia
Mannitol Osmotic nephrosis
Table 13–2. Drugs associated with acute renal failure.
(
continued
)

CHAPTER 13
316
tubular reabsorption of urea can increase to 90% or more.
Since creatinine is not reabsorbed, serum urea increases
more rapidly than serum creatinine under these conditions,
as seen in prerenal renal failure. In general, when measured
as blood urea nitrogen (BUN) in milligrams per deciliter, the
normal ratio of BUN to serum creatinine is 10:1. If it rises to
levels of 20:1 or more, one should suspect prerenal azotemia.
In addition to variations in renal handling, blood urea con-
centrations are also subject to the state of protein catabolism.
Thus 6 g of protein yields approximately 1 g of urea nitrogen.
Under most clinical conditions, there is a direct relationship
between the amount of protein ingested and urea nitrogen
production. Under conditions of stress, inadequate caloric
intake, or corticosteroid administration, endogenous protein
catabolism results in enhanced urea production. GI hemor-
rhage and the resulting absorption of blood proteins—
approximately 200 g of protein in 1 L of whole blood—also
can increase urea production.
3. Plasma electrolytes—Abnormalities of plasma
sodium, potassium, bicarbonate, calcium, magnesium, and
phosphate are common in acute renal failure, and their
determination and monitoring are an integral part of the
diagnosis and management of acute renal failure.
4. Serologic markers—A search for abnormal serologic
markers, such as various autoantibodies, is part of the basic
workup of immunologically mediated renal disease, includ-
ing glomerulonephritis.
5. Urine electrolytes—Evaluation of random urine sam-
ples provides quick information about the current state of
renal function. The fractional excretion of sodium (FE
Na
) is
the best means of differentiating between prerenal azotemia
and acute tubular necrosis and can be calculated as follows:
In the context of oliguria (urine output <500 mL/day), a
FE
Na
of less than 1% is most commonly associated with pre-
renal azotemia, but it also may be seen with acute glomeru-
lonephritis. Under similar oliguric conditions, a FE
Na
of
greater than 1% is probably related to acute tubular necrosis.
Unfortunately, the potential usefulness of this test is often
lost if diuretics are given prior to collection of the urine sam-
ple.
The fractional excretion of urea (FE
urea
) also can be use-
ful and is similarly calculated as follows:
Normal values in well-hydrated individuals are between
50% and 65%. Values below 35% are most compatible with
renal hypoperfusion and are not affected by loop diuretics
FE
urine Ur (mg/dL)
urine Cr (mg/dL)
ser
urea
=×
uum Cr (mg/dL)
serum Ur (mg/dL)
FE
urine Na (meq/L)
urine Cr (mg/dL)
serum
Na
=×
Cr (mg/dL)
serum Na (meq/L)
Drug Mechanism of Nephrotoxicity
Antihypertensives
ACE inhibitors Hemodynamic compromise (most common
with bilateral renal artery stenosis), AIN
Angiotensin receptor
blockers
Hemodynamic compromise (most common
with bilateral renal artery stenosis)
Anti-Inflammatory Drugs
Celecoxib AIN
Diclofenac AIN
Fenoprofen AIN, nephrotic syndrome
Ibuprofen AIN
Indomethacin AIN, nephrotic syndrome
Ketorolac AIN
Nabumetone AIN
Naproxen AIN, nephrotic syndrome
NSAIDs (all) Prerenal azotemia (especially in CHF, cirrho-
sis, nephrosis, chronic renal failure, volume
depletion), ATN
Rofecoxib AIN
Sulindac AIN, nephrotic syndrome
Tolmetin AIN
Antiplatelet Agents
Clopidogrel HUS
Ticlopidine Nephrotic syndrome, HUS
MIscellaneous Agents
Allopurinol AIN
Cimetidine AIN, decreased creatinine secretion
Disopyramide Obstructive uropathy
Intravenous immune
globulin
Prerenal azotemia with filtration failure due
to hyperoncotic plasma
Lithium AIN
Omeprazole AIN
Phenindione AIN
Phenytoin AIN
Ranitidine AIN
Radiocontrast Agents
All ATN (especially with volume depletion or
advanced diabetic nephropathy)
Key: ACE = angiotension-converting enzyme, AIN = allergic intersti-
tial nephritis, ATN = acute tubular necrosis, CHF = congestive heart
failure, HUS = hemolytic uremic syndrome, NSAID = nonsteriodal
anti-inflammatory drug. (See Table 13–6.)
Table 13–2. Drugs associated with acute renal failure.
(continued)
