Voet D., Voet Ju.G. Biochemistry
Подождите немного. Документ загружается.

671
+
4
⋅
GDP
GDP
GTP
GTP
γ
ββ
γ
H
2
O
G
sα
⋅ GDP
+ P
i
R
S
sα sα
671
CHAPTER 19
Signal Transduction
1 Hormones
A. Quantitative Measurements
B. Pancreatic Islet Hormones
C. Gastrointestinal Hormones
D. Thyroid Hormones
E. Control of Calcium Metabolism
F. Epinephrine and Norepinephrine
G. Steroid Hormones
H. Control of Endocrine Function: The Hypothalamus
and Pituitary Gland
I. Control of the Menstrual Cycle
J. Growth Hormone and Its Receptor
K. Opioid Peptides
L. The Hormonal Function of Nitric Oxide
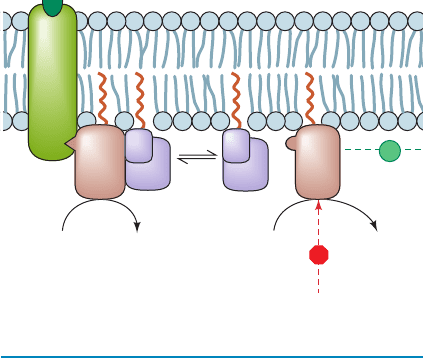
2 Heterotrimeric G Proteins
A. Overview
B. G Protein-Coupled Receptors
C. Heterotrimeric G Proteins: Structure and Function
D. Adenylate Cyclases
E. Phosphodiesterases
3 Tyrosine Kinase–Based Signaling
A. Receptor Tyrosine Kinases
B. Cancer: The Loss of Control of Growth
C. Relaying the Signal: Binding Modules, Adaptors,
GEFs, and GAPs
D. MAP Kinase Signaling Cascades
E. Tyrosine Kinase–Associated Receptors
F. Protein Phosphatases
4 The Phosphoinositide Cascade
A. Ca
2
, Inositol Trisphosphate, and Diacylglycerol Are
Second Messengers
B. The Phospholipases C
C. The Protein Kinases C
D. The Phosphoinositide 3-Kinases
E. Inositol Polyphosphate Phosphatases
F. Epilog: Complex Systems and Emergent Properties
Living things coordinate their activities at every level of
their organization through complex chemical signaling sys-
tems. Intercellular signals occur through the mediation of
chemical messengers known as hormones and, in higher
animals, via neuronally transmitted electrochemical im-
pulses. Intracellular communications are maintained by the
synthesis or alteration of a great variety of different sub-
stances that are often integral components of the processes
they control. For example, metabolic pathways, as we have
seen, are regulated by the feedback control of allosteric en-
zymes by metabolites in those pathways or by the covalent
modification of these enzymes. In this chapter we consider
chemical signaling and how these signals are mediated.We
begin by discussing the functions of the major human hor-
mone systems. We then discuss the three major pathways
whereby intercellular signals are transduced (converted) to
intracellular signals, namely, those that utilize (1) het-
erotrimeric G proteins, (2) receptor tyrosine kinases, and
(3) phosphoinositide cascades. Neurotransmission is
discussed in Section 20-5.
1 HORMONES
Hormones are classified according to the distance over
which they act (Fig. 19-1):
1. Endocrine hormones act on cells distant from the site
of their release. Endocrine hormones, for example, insulin
and epinephrine, are synthesized and released in the blood-
stream by specialized ductless endocrine glands.
2. Paracrine hormones (alternatively, local mediators)
act only on cells close to the cell that released them. For ex-
ample, an essential element of the immune response is ini-
tiated when a white blood cell known as a macrophage that
has encountered a specific antigen binds a so-called T cell
specific for that antigen. The macrophage thereupon re-
leases a protein growth factor named interleukin-1 (IL-1)
that stimulates the bound T cell to proliferate and differen-
tiate (Section 35-2Aa).
3. Autocrine hormones act on the same cell that released
them. For example, the response of a T cell to interleukin-1
is enhanced by the T cell’s autostimulatory release of the
protein growth factor interleukin-2 (IL-2).
We are already familiar with certain aspects of hor-
monal control. For instance, we have considered how epi-
nephrine, insulin, and glucagon regulate energy metabo-
lism through the intermediacy of cAMP (Sections 18-3E
and 18-3G). In this section we extend and systematize this
information. Before we do so, you should note that bio-
chemical communications are not limited to intracellular
and intercellular signals. Many organisms release sub-
stances called pheromones that alter the behavior of other
organisms of the same species in much the same way as
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 671
672 Chapter 19. Signal Transduction
hormones. Pheromones are commonly sexual attractants
but some have other functions in species, such as ants, that
have complex social interactions.
The human endocrine system (Fig. 19-2) secretes a wide
variety of hormones (Table 19-1) that enable the body to:
1. Maintain homeostasis (e.g., insulin and glucagon
maintain the blood glucose level within rigid limits during
feast or famine).
2. Respond to a wide variety of external stimuli (such as
the preparation for “fight or flight” engendered by epi-
nephrine and norepinephrine).
3. Follow various cyclic and developmental programs
(for instance, sex hormones regulate sexual differentiation,
maturation, the menstrual cycle, and pregnancy; Sections
19-1Gb and 19-1I).
Most hormones are either polypeptides, amino acid deriva-
tives, or steroids, although there are important exceptions
to this generalization. In any case, only those cells with a
specific receptor for a given hormone will respond to its
presence even though nearly all cells in the body may be ex-
posed to the hormone. Hormonal messages are therefore
quite specifically addressed.
In this section, we outline the hormonal functions of the
various endocrine glands. Throughout this discussion keep
in mind that these glands are not just a collection of inde-
pendent secretory organs but form a complex and highly
interdependent control system. Indeed, as we shall see, the
secretion of many hormones is under feedback control
through the secretion of other hormones to which the
original hormone-secreting gland responds. Much of our
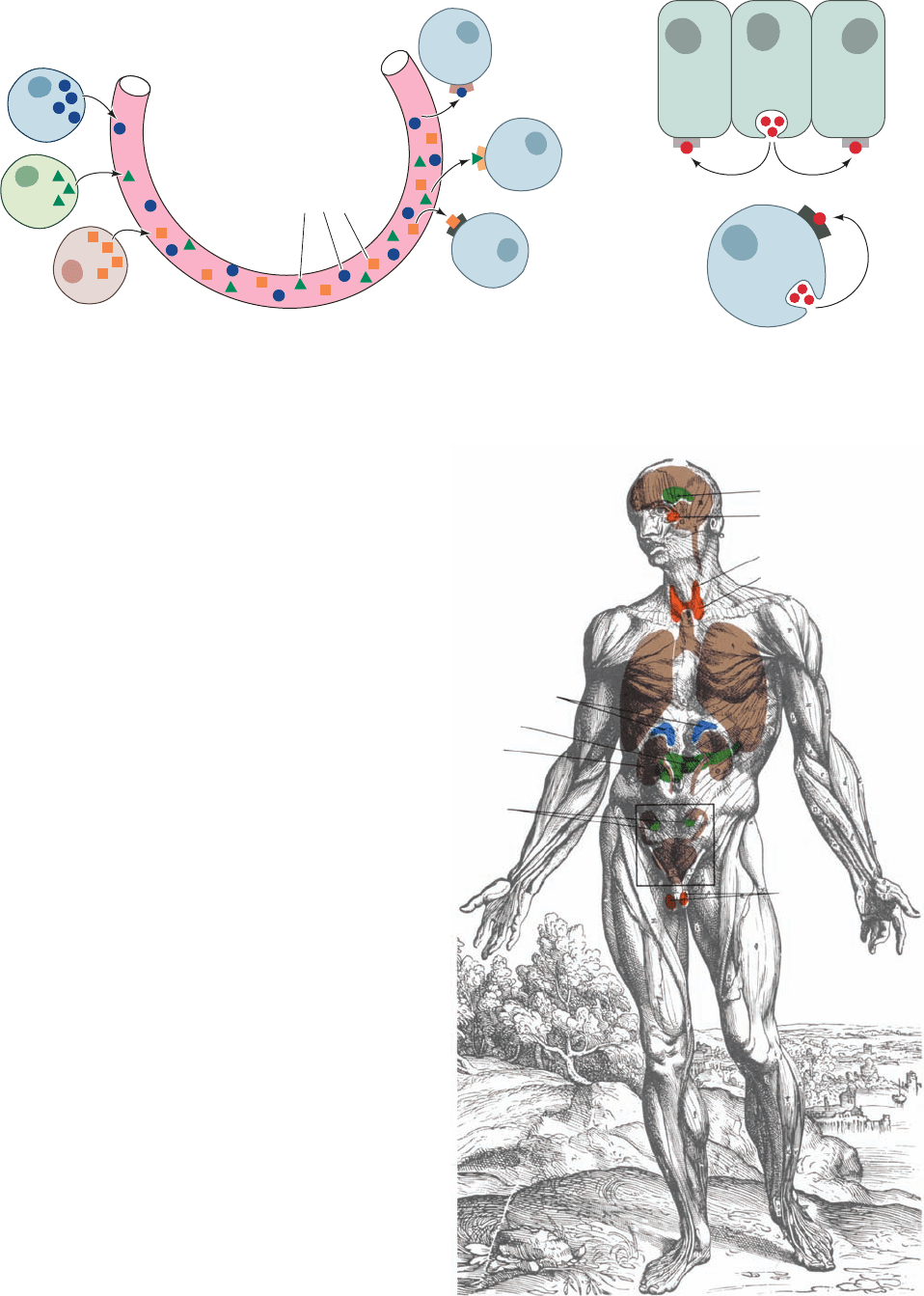
Figure 19-1 Classification of hormones. Hormonal
communications are classified according to the distance over
which the signal acts: (a) endocrine signals are directed at distant
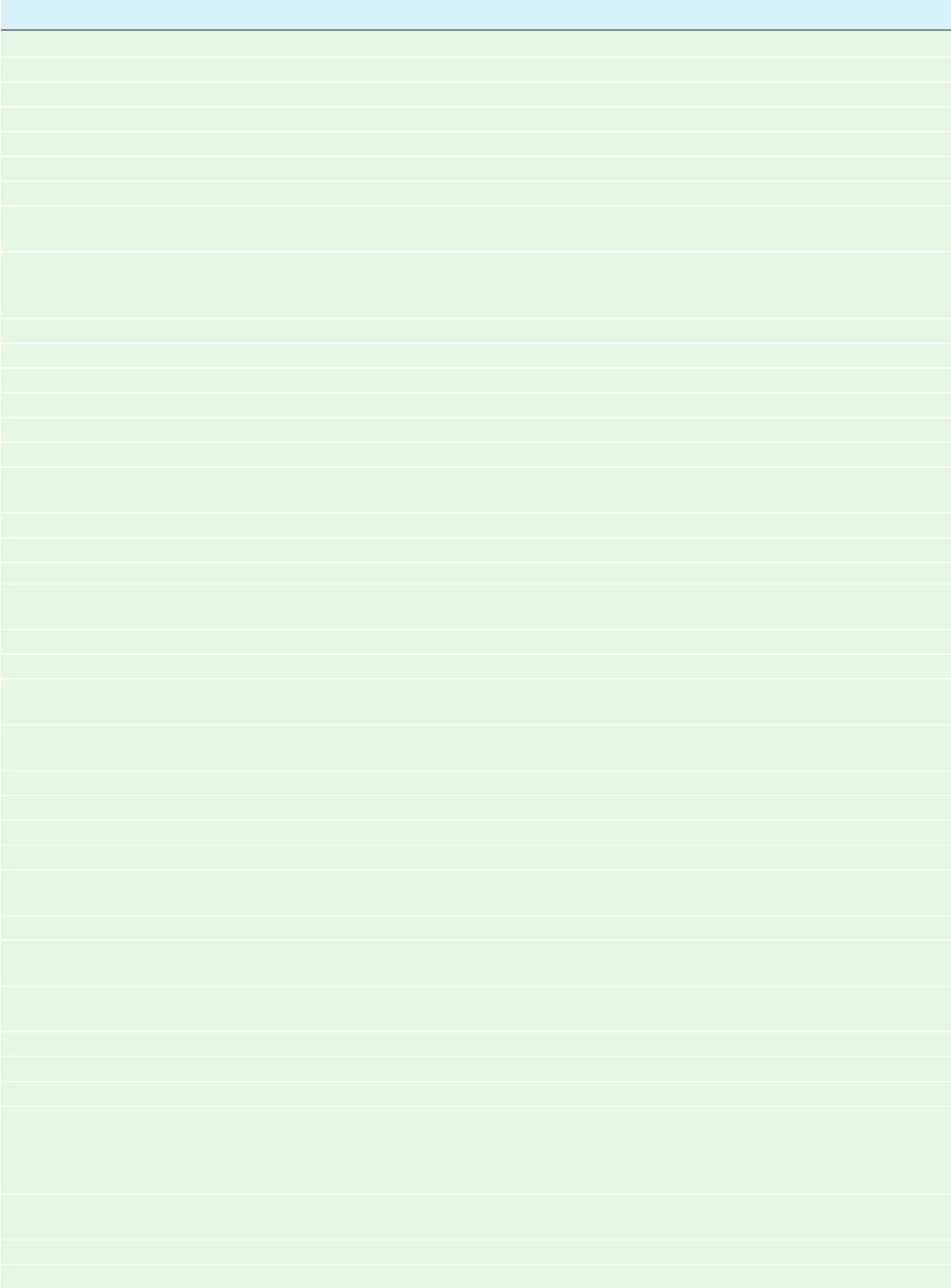
Figure 19-2 Major glands of the human endocrine system.
Other tissues, the intestines, for example, also secrete endocrine
hormones.
(c)
(b)
Autocrine
Paracrine
(a) Endocrine
Endocrine
cells
Bloodstream
Target
cells
Hormone
molecules
cells through the intermediacy of the bloodstream, (b) paracrine
signals are directed at nearby cells, and (c) autocrine signals are
directed at the cell that produced them.
Adrenal glands
Hypothalamus
Pituitary
Parathyroid
Thyroid
Testes
Pancreas
Ovaries
Kidney
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 672
Section 19-1. Hormones 673
Table 19-1 Some Human Hormones
Hormone Origin Major Effects
Polypeptides
Corticotropin-releasing factor (CRF) Hypothalamus Stimulates ACTH release
Gonadotropin-releasing factor (GnRF) Hypothalamus Stimulates FSH and LH release
Thyrotropin-releasing factor (TRF) Hypothalamus Stimulates TSH release
Growth hormone-releasing factor (GRF) Hypothalamus Stimulates growth hormone release
Somatostatin Hypothalamus Inhibits growth hormone release
Adrenocorticotropic hormone (ACTH) Adenohypophysis Stimulates the release of adrenocorticosteroids
Follicle-stimulating hormone (FSH) Adenohypophysis In ovaries, stimulates follicular development, ovulation, and
estrogen synthesis; in testes, stimulates spermatogenesis
Luteinizing hormone (LH) Adenohypophysis In ovaries, stimulates oocyte maturation and follicular
synthesis of estrogens and progesterone; in testes,
stimulates androgen synthesis
Chorionic gonadotropin (CG) Placenta Stimulates progesterone release from the corpus luteum
Thyrotropin (TSH) Adenohypophysis Stimulates T
3
and T
4
release
Somatotropin (growth hormone) Adenohypophysis Stimulates growth and synthesis of somatomedins
Met-enkephalin Adenohypophysis Opioid effects on central nervous system
Leu-enkephalin Adenohypophysis Opioid effects on central nervous system
-Endorphin Adenohypophysis Opioid effects on central nervous system
Vasopressin Neurohypophysis Stimulates water resorption by kidney and increases blood
pressure
Oxytocin Neurohypophysis Stimulates uterine contractions
Glucagon Pancreas Stimulates glucose release through glycogenolysis and
stimulates lipolysis
Insulin Pancreas Stimulates glucose uptake through gluconeogenesis,
protein synthesis, and lipogenesis
Gastrin Stomach Stimulates gastric acid and pepsinogen secretion
Secretin Intestine Stimulates pancreatic secretion of HCO
3
Cholecystokinin (CCK) Intestine Stimulates gallbladder emptying and pancreatic secretion
of digestive enzymes and HCO
3
Gastric inhibitory peptide (GIP) Intestine Inhibits gastric acid secretion and gastric emptying;
stimulates pancreatic insulin release
Parathyroid hormone Parathyroid Stimulates Ca
2
uptake from bone, kidney, and intestine
Calcitonin Thyroid Inhibits Ca
2
uptake from bone and kidney
Somatomedins Liver Stimulates cartilage growth; have insulinlike activity
Steroids
Glucocorticoids Adrenal cortex Affect metabolism in diverse ways, decrease inflammation,
increase resistance to stress
Mineralocorticoids Adrenal cortex Maintain salt and water balance
Estrogens Gonads Maturation and function of secondary sex organs,
particularly in females
Androgens Gonads Maturation and function of secondary sex organs,
particularly in males; male sexual differentiation
Progestins Ovaries and placenta Mediate menstrual cycle and maintain pregnancy
Vitamin D Diet and sun Stimulates Ca
2
absorption from intestine, kidney, and bone
Amino Acid Derivatives
Epinephrine Adrenal medulla Stimulates contraction of some smooth muscles and
relaxes others, increases heart rate and blood pressure,
stimulates glycogenolysis in liver and muscle, stimulates
lipolysis in adipose tissue
Norepinephrine Adrenal medulla Stimulates arteriole contraction, decreases peripheral
circulation, stimulates lipolysis in adipose tissue
Triiodothyronine (T
3
) Thyroid General metabolic stimulation
Thyroxine (T
4
) Thyroid General metabolic stimulation
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 673

understanding of hormonal function has come from careful
measurements of hormone concentrations, the effects of
changes of these concentrations on physiological functions,
and measurements of the affinities with which hormones
bind to their receptors. We begin, therefore, with a consi-
deration of how physiological hormone concentrations
are measured and how receptor–ligand interactions are
quantified.
A. Quantitative Measurements
a. Radioimmunoassays
The serum concentrations of hormones are extremely
small, generally between 10
12
and 10
7
M, so they usually
must be measured by indirect means. Biological assays
were originally employed for this purpose but they are gen-
erally slow, cumbersome, and imprecise. Such assays have
therefore been largely supplanted by radioimmunoassays.
In this technique, which was developed by Rosalyn Yalow,
the unknown concentration of a hormone, H, is determined
by measuring how much of a known amount of the ra-
dioactively labeled hormone, H*, binds to a fixed quantity
of anti-H antibody in the presence of H. This competition
reaction is easily calibrated by constructing a standard
curve indicating how much H* binds to the antibody as a
function of [H].The high ligand affinity and specificity that
antibodies possess gives radioimmunoassays the advan-
tages of great sensitivity and specificity.
b. Receptor Binding
Receptors, as do other proteins, bind their correspon-
ding ligands according to the laws of mass action:
Here R and L represent receptor and ligand, and the reac-
tion’s dissociation constant is expressed:
[19.1]
where the total receptor concentration,[R]
T
[R] [R L].
Equation [19.1] may be rearranged to a form analogous to
the Michaelis–Menten equation of enzyme kinetics (Sec-
tion 14-2A):
[19.2]
where Y is the fractional occupation of the ligand-binding
sites. Equation [19.2] represents a hyperbolic curve (Fig.
19-3a) in which K
L
may be operationally defined as the lig-
and concentration at which the receptor is half-maximally
occupied by ligand.
Although K
L
and [R]
T
may, in principle, be determined
from an analysis of a hyperbolic plot such as Fig. 19-3a, the
analysis of a linear form of the equation is a simpler proce-
dure. Equation [19.1] may be rearranged to:
[19.3]
[R L]
[L]
([R]
T
[R L])
K
L
Y
[R L]
[R]
T
[L]
K
L
[L]
K
L
[R][L]
[R L]
([R]
T
[R L])[L]
[R L]
R L Δ R L
Now, in keeping with customary receptor-binding nomen-
clature, let us redefine [R L] as B (for bound ligand), [L]
as F (for free ligand), and [R]
T
as B
max
. Then Eq. [19.3]
becomes:
[19.4]
A plot of B/F versus B, which is known as a Scatchard plot
(after George Scatchard, its originator), therefore yields a
straight line of slope 1/K
L
whose intercept on the B axis
is B
max
(Fig. 19-3b). Here, both B and F may be determined
by filter-binding assays as follows. Most receptors are insol-
uble membrane-bound proteins and may therefore be sep-
arated from soluble free ligand by filtration (receptors that
have been solubilized may be separated from free ligand
by filtration, for example, through nitrocellulose since
proteins nonspecifically bind to nitrocellulose). Hence,
through the use of radioactively labeled ligand, the values
of B and F ([R L] and [L]) may be determined, respec-
tively, from the radioactivity on the filter and that remain-
ing in solution.The rate of R L dissociation is generally so
slow (half-times of minutes to hours) as to cause insignifi-
cant errors when the filter is washed to remove residual
free ligand.
c. Competitive-Binding Studies
Once the receptor-binding parameters for one ligand
have been determined, the dissociation constant of other
ligands for the same ligand-binding site may be determined
through competitive-binding studies.The model describing
this competitive binding is analogous to the competitive in-
hibition of a Michaelis–Menten enzyme (Section 14-3A):
R
K
I
K
L
R L No binding
I
LRL
+
+
+
•
I
•
B
F
(B
max
B)
K
L
1
K
L
B
B
max
K
L
674 Chapter 19. Signal Transduction
Figure 19-3 Binding of ligand to receptor. (a) A hyperbolic
plot. (b) A Scatchard plot. Here B ⬅ [R L], F ⬅ [L], and
B
max
⬅ [R]
T
.
1.0
(a) (b)
0.5
[L] B
K
L
1
Slope = –
B
F
[R
• L]
[R]
T
B
max
B
max
K
L
K
L
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 674
where I is the competing ligand whose dissociation con-
stant with the receptor is expressed:
[19.5]
Thus, in direct analogy with the derivation of the equation
describing competitive inhibition:
[19.6]
The relative affinities of a ligand and an inhibitor may
therefore be determined by dividing Eq. [19.6] in the pres-
ence of inhibitor with that in the absence of inhibitor:
[19.7]
When this ratio is 0.5 (50% inhibition),the competitor con-
centration is referred to as [I
50
] in analogy with the [IC
50
] of
drugs that inhibit enzymes (Section 15-4Aa). Thus, solving
Eq. [19.7] for K
I
at 50% inhibition:
[19.8]
B. Pancreatic Islet Hormones
The pancreas is a large glandular organ, the bulk of which
is an exocrine gland dedicated to producing digestive en-
zymes such as trypsin, RNase A, -amylase, and phospholi-
pase A
2
that it secretes via the pancreatic duct into the
small intestine. However, ⬃1 to 2% of pancreatic tissue
consists of scattered clumps of cells known as islets of
Langerhans, which comprise an endocrine gland that func-
tions to maintain energy metabolite homeostasis. Pancre-
atic islets contain three types of cells, each of which se-
cretes a characteristic polypeptide hormone:
1. The cells secrete glucagon (29 residues; Section
18-3Ea).
2. The cells secrete insulin (51 residues; Fig. 9-4).
3. The cells secrete somatostatin (14 residues).
Insulin, which is secreted in response to high blood glucose
levels, primarily functions to stimulate muscle, liver, and
adipose cells to store glucose for later use by synthesizing
glycogen, protein, and fat (Section 27-2). Glucagon, which
is secreted in response to low blood glucose, has essentially
the opposite effects: It stimulates liver to release glucose
through glycogenolysis (Section 18-3E) and gluconeogene-
sis (Section 23-1) and it stimulates adipose tissue to release
fatty acids through lipolysis. Somatostatin, which is also se-
creted by the hypothalamus (Section 19-1H), inhibits the
release of insulin and glucagon from their islet cells and is
K
I
[I
50
]
1
[L]
K
L
[R L]
I
[R L]
0
K
L
[L]
K
L
a1
[I]
K
I
b [L]
[R L]
[R]
T
[L]
K
L
a1
[I]
K
I
b [L]
K
I
[R][I]
[R I]
therefore thought to have a paracrine function in the
pancreas.
Polypeptide hormones, as are other proteins destined
for secretion, are ribosomally synthesized as preprohor-
mones, processed in the rough endoplasmic reticulum and
Golgi apparatus to form the mature hormone, and then
packaged in secretory granules to await the signal for their
release by exocytosis (Sections 12-4B, 12-4C, and 12-4D).
The most potent physiological stimuli for the release of in-
sulin and glucagon are, respectively, high and low blood
glucose concentrations, so that islet cells act as the body’s
primary glucose sensors. However, the release of these hor-
mones is also influenced by the autonomic (involuntary)
nervous system and by hormones secreted by the gastroin-
testinal tract (Section 19-1C).
C. Gastrointestinal Hormones
The digestion and absorption of nutrients are compli-
cated processes that are regulated by the autonomic nerv-
ous system in concert with a complex system of polypep-
tide hormones. Indeed, gastrointestinal peptide hormones
are secreted into the bloodstream by a system of special-
ized cells lining the gastrointestinal tract whose aggregate
mass is greater than that of the rest of the endocrine sys-
tem. Over 20 gastrointestinal hormones have been de-
scribed. Four of the better characterized gastrointestinal
hormones are:
1. Gastrin (17 residues), which is produced by the gastric
mucosa, stimulates the gastric secretion of HCl and
pepsinogen (the zymogen of the digestive protease pepsin).
Gastrin release is stimulated by amino acids and partially
digested protein as well as by the vagus nerve (which inner-
vates the stomach) in response to stomach distension.
Gastrin release is inhibited by HCl and by other gastroin-
testinal hormones.
2. Secretin (27 residues), which is produced by the mu-
cosa of the duodenum (upper small intestine) in response
to acidification by gastric HCl, stimulates the pancreatic se-
cretion of so as to neutralize this acid.
3. Cholecystokinin (CCK; 8 residues), which is pro-
duced by the duodenum, stimulates gallbladder emptying,
the pancreatic secretion of digestive enzymes and
(and thus enhances the effect of secretin), and inhibits gas-
tric emptying. CCK is released in response to the products
of lipid and protein digestion, that is, fatty acids, monoacyl-
glycerols, amino acids, and peptides.
4. Gastric inhibitory peptide (GIP, also known as glucose-
dependent insulinotropic polypeptide; 42 residues), which
is produced by specialized cells lining the small intestine, is
a potent inhibitor of gastric acid secretion, gastric mobility,
and gastric emptying. However, GIP’s major physiological
function is to stimulate pancreatic insulin release. Indeed,
the release of GIP is stimulated by the presence of glucose
in the gut, which accounts for the observation that, after a
meal, the blood insulin level increases before the blood
glucose level does.
HCO
3
HCO
3
Section 19-1. Hormones 675
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 675
These gastrointestinal hormones form families of related
polypeptides: The C-terminal pentapeptides of gastrin and
CCK are identical; secretin, GIP, and glucagon are closely
similar. Two other gastrointestinal peptide hormones are
discussed in Section 27-3C.
D. Thyroid Hormones
The thyroid gland produces two related hormones, tri-
iodothyronine (T
3
) and thyroxine (T
4
),
NH
3
H
X H Triiodothyronine (T
3
)
X I Thyroxine (T
4
)
OC
+
X
COO
–
CH
2
HO
I
II
that stimulate metabolism in most tissues (adult brain is a
conspicuous exception). The production of these unusual
iodinated amino acids begins with the synthesis of thy-
roglobulin, a 2748-residue protein. Thyroglobulin is post-
translationally modified in a series of biochemically unique
reactions (Fig. 19-4):
1. Around 20% of thyroglobulin’s 140 Tyr residues are
iodinated in a thyroperoxidase (TPO)-catalyzed reaction
forming 2,5-diiodotyrosyl residues.
2. Two such residues are oxidatively coupled to yield T
3
and T
4
residues.
3. Mature thyroglobulin itself is hormonally inactive.
However, some five or six molecules of the active hor-
mones, T
3
and T
4
, are produced by the proteolysis in the
lysosome of thyroglobulin on hormonal stimulation of the
thyroid (Section 19-1H).
How do thyroid hormones work? T
3
and T
4
, being non-
polar substances, are transported by the blood in complex
676 Chapter 19. Signal Transduction
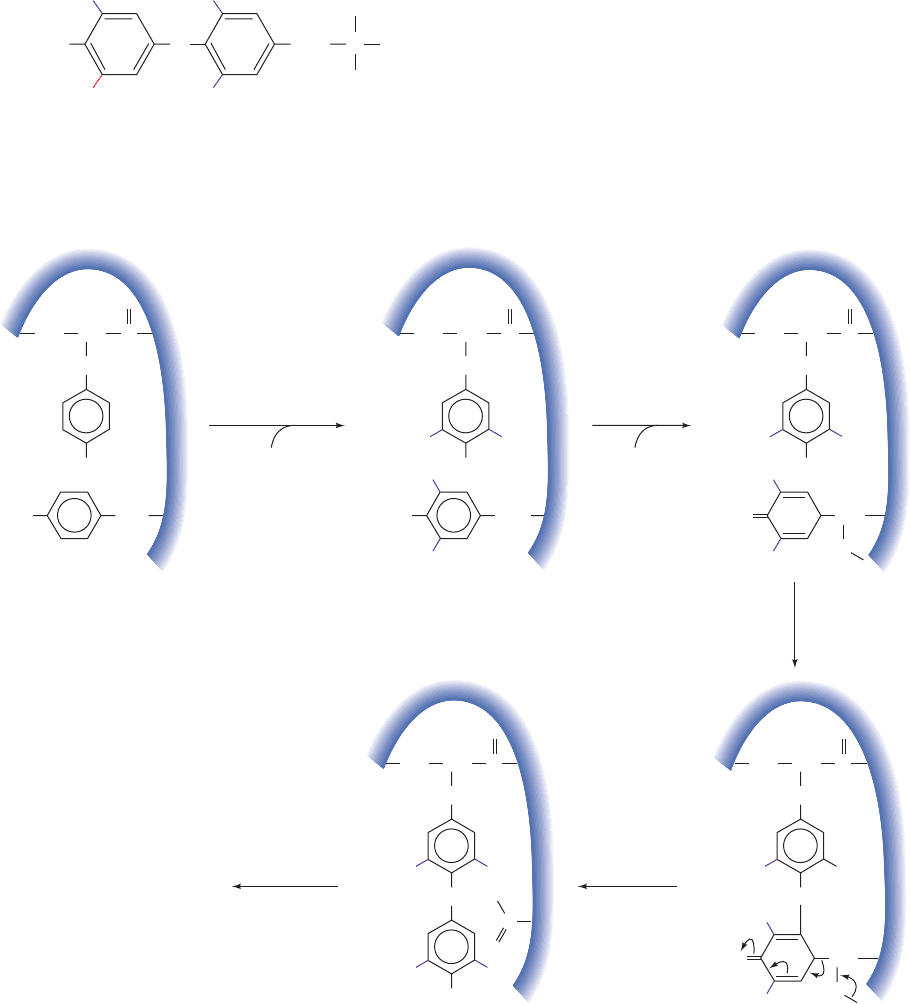
Figure 19-4 Biosynthesis of T
3
and T
4
in the thyroid gland.
The pathway involves the iodination, coupling, and hydrolysis
HO CH
2
Tyr
OH
CH
2
CH CNH
O
Tyr
Thyroglobulin
HO CH
2
OH
CH
2
CH CNH
O
1
thyroperoxidase
I
H
2
O
2
2
H
2
O
2
2
3
proteolysis
I
II
I
OCH
I
I
I
I
O
CH
2
CH CNH
O
I
I
I
C
O
CH
2
CH CNH
O
O
II
OH
II
T
3
T
4
O
O
CH
2
CH CNH
O
H
OCH
O
H
H
H
•
•
(proteolysis) of thyroglobulin Tyr residues. The relatively scarce
I
is actively sequestered by the thyroid gland.
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 676
with plasma carrier proteins, primarily thyroxine-binding
globin, but also prealbumin and albumin. The hormones
then pass through the cell membranes of their target cells
into the cytosol,where they bind to a specific protein. Since
the resulting hormone–protein complex does not enter the
nucleus, it is thought that this complex acts to maintain an
intracellular reservoir of thyroid hormones. The true thy-
roid hormone receptor is a chromosomally associated pro-
tein and therefore does not leave the nucleus. The binding
of T
3
, and to a lesser extent T
4
, activates this receptor as a
transcription factor (Section 5-4Aa), resulting in increased
rates of expression of numerous metabolic enzymes. High
affinity thyroid hormone–binding sites also occur on the
inner mitochondrial membrane (the site of electron trans-
port and oxidative phosphorylation; Section 22-1), suggest-
ing that these receptors may directly regulate O
2
consump-
tion and ATP production.
Abnormal levels of thyroid hormones are common
human afflictions. Hypothyroidism is characterized by
lethargy, obesity, and cold dry skin, whereas hyperthy-
roidism has the opposite effects. The inhabitants of areas
in which the soil has a low iodine content often develop
hypothyroidism accompanied by an enlarged thyroid
gland, a condition known as goiter. The small amount of
NaI usually added to commercially available table salt
(“iodized” salt) easily prevents this iodine deficiency dis-
ease. Young mammals require thyroid hormone for nor-
mal growth and development: Hypothyroidism during the
fetal and immediate postnatal periods results in irre-
versible physical and mental retardation, a syndrome
named cretinism.
E. Control of Calcium Metabolism
Ca
2
forms hydroxyapatite, Ca
5
(PO
4
)
3
OH, the major min-
eral constituent of bone, and is an essential element in
many biological processes including the mediation of hor-
monal signals as a second messenger,the triggering of mus-
cle contraction, the transmission of nerve impulses, and
blood clotting. The extracellular [Ca
2
] must therefore be
closely regulated to keep it at its normal level of ⬃1.2 mM.
Three hormones have been implicated in maintaining Ca
2
homeostasis (Fig. 19-5):
1. Parathyroid hormone (PTH), an 84-residue polypep-
tide secreted by the parathyroid gland, which increases
serum [Ca
2
] by stimulating its resorption from bone and
kidney and by increasing the dietary absorption of Ca
2
from the intestine.
2. Vitamin D, a group of steroidlike substances that act
in a synergistic manner with PTH to increase serum
[Ca
2
].
3. Calcitonin, a 33-residue polypeptide synthesized by
specialized thyroid gland cells, which decreases serum
[Ca
2
] by inhibiting the resorption of Ca
2
from bone and
kidney.
We shall briefly discuss the functions of these hormones.
a. Parathyroid Hormone
The bones, the body’s main Ca
2
reservoir, are by no
means metabolically inert. They are continually “remod-
eled” through the action of two types of bone cells: os-
teoblasts which synthesize the collagen fibrils that form
the bulk of bone’s organic matrix,the scaffolding on which
its Ca
5
(PO
4
)
3
OH mineral phase is laid down; and osteo-
clasts, which participate in bone resorption (Section 15-
4Ab). PTH inhibits collagen synthesis by osteoblasts and
stimulates bone resorption by osteoclasts.The main effect of
PTH, however, is to increase the rate at which the kidneys
excrete phosphate,the counterion of Ca
2
in bone.The con-
sequent decreased serum [P
i
] causes Ca
5
(PO
4
)
3
OH to
leach out of bone through mass action and thus increase
serum [Ca
2
]. In addition, PTH stimulates the production
of the active form of vitamin D by the kidney, which, in
turn, enhances the transfer of intestinal Ca
2
to the blood
(see below).
b. Vitamin D
Vitamin D is a group of fat-soluble dietary substances
that prevent rickets, a disease of children characterized by
stunted growth and deformed bones stemming from insuf-
ficient bone mineralization (vitamin D deficiency in adults
is known as osteomalacia, a condition characterized by
weakened, demineralized bones). Although rickets was
first described in 1645, it was not until the early twentieth
century that it was discovered that animal fats, particularly
fish liver oils, are effective in preventing this deficiency dis-
ease. Moreover, rickets can also be prevented by exposing
children to sunlight or just UV light in the wavelength
range 230 to 313 nm, regardless of their diets.
The D vitamins, which we shall see are really hormones,
are sterol derivatives (Section 12-1E) in which the steroid
B ring is disrupted at its 9,10 position. The natural form of
the vitamin,vitamin D
3
(cholecalciferol), is nonenzymatically
Section 19-1. Hormones 677
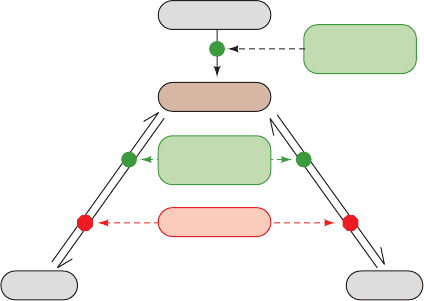
Figure 19-5 Roles of PTH, vitamin D, and calcitonin in
controlling Ca
2
metabolism.
Intestines
Blood [Ca
2+
]
PTH (+)
Vitamin D (+)
KidneyBone
PTH (+)
Vitamin D (+)
Calcitonin (–)
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 677
These various nonpolar substances are transported in the
bloodstream in complex with vitamin D-binding protein.
1,25(OH)
2
D acts to increase serum [Ca
2
] by promoting
the intestinal absorption of dietary Ca
2
and by stimulating
Ca
2
release from bone. Intestinal Ca
2
absorption is stim-
ulated through increased synthesis of a Ca
2
-binding pro-
tein, which functions to transport Ca
2
across the intestinal
mucosa. 1,25(OH)
2
D binds to cytoplasmic receptors in in-
testinal epithelial cells that, on transport to the nucleus,
function as transcription factors for the Ca
2
-binding pro-
tein. The maintenance of electroneutrality requires that
Ca
2
transport be accompanied by that of counterions,
mostly P
i
, so that 1,25(OH)
2
D also stimulates the intestinal
absorption of P
i
. The observation that 1,25(OH)
2
D, like
PTH, stimulates the release of Ca
2
and P
i
from bone
seems paradoxical in view of the fact that low levels of
1,25(OH)
2
D result in subnormal bone mineralization. Pre-
sumably the increased serum [Ca
2
] resulting from
1,25(OH)
2
D-stimulated intestinal uptake of Ca
2
causes
bone to take up more Ca
2
than it loses through direct hor-
monal stimulation. In addition, vitamin D has been shown
to modulate the immune response, provide protection
against certain types of cancers, and has been implicated in
preventing/reversing heart disease.
Vitamin D, unlike the water-soluble vitamins, is retained
by the body, so that excessive intake of vitamin D over long
periods causes vitamin D intoxication (although note that
most individuals, particularly the elderly and those with
limited sun exposure, have less than the recommended lev-
els of vitamin D in their blood). The consequent high
serum [Ca
2
] results in aberrant calcification of a wide va-
riety of soft tissues. The kidneys are particularly prone to
calcification, a process that can lead to the formation of
kidney stones and ultimately kidney failure. In addition, vi-
tamin D intoxication promotes bone demineralization to
the extent that bones are easily fractured. The observation
that the level of skin pigmentation in indigenous human
populations tends to increase with their proximity to the
equator is explained by the hypothesis that skin pigmenta-
tion functions to prevent vitamin D intoxication by filter-
ing out excessive solar radiation.
c. Calcitonin
Calcitonin has essentially the opposite effect of PTH; it
lowers serum [Ca
2
]. It does so primarily by inhibiting os-
teoclastic resorption of bone. Since PTH and calcitonin
both stimulate the synthesis of cAMP in their target cells
(Section 19-2A), it is unclear how these hormones can op-
positely affect osteoclasts. Calcitonin also inhibits kidney
from resorbing Ca
2
, but in this case the kidney cells that
calcitonin influences differ from those that PTH stimulates
to resorb Ca
2
.
d. Osteoporosis
Osteoporosis (Section 15-4Ab) is a degenerative bone
disease that results in an increased risk of bone fracture
due to bone demineralization as well as changes in the
amounts and variety of noncollagenous bone proteins. It is
most common in postmenopausal women, although it also
formed in the skin of animals through the photolytic action
of UV light on 7-dehydrocholesterol:
Vitamin D
2
(ergocalciferol), which differs from vitamin D
3
only by a side chain double bond and methyl group, is
formed by the UV irradiation of the plant sterol ergosterol.
Since vitamins D
2
and D
3
have essentially identical biolog-
ical activities, vitamin D
2
is commonly used as a vitamin
supplement, particularly in milk.
Vitamins D
2
and D
3
are hormonally inactive as such;
they gain biological activity through further metabolic pro-
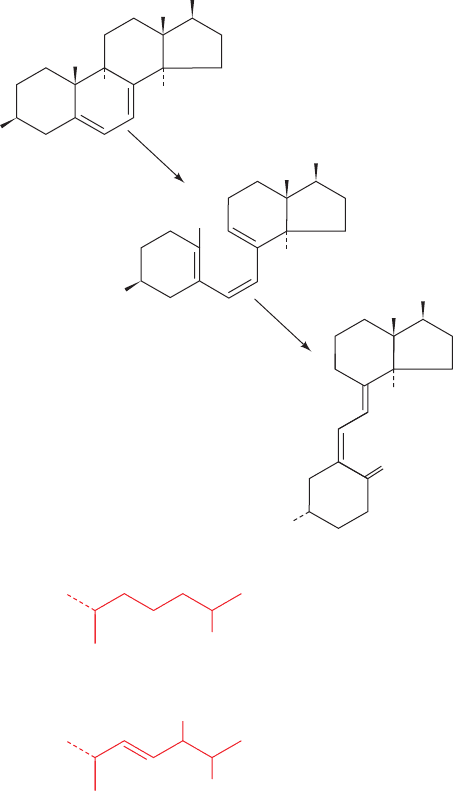
cessing, first in the liver and then in the kidney (Fig. 19-6):
1. In the human liver, vitamin D
3
is hydroxylated to
form 25-hydroxycholecalciferol in an O
2
-requiring reaction
catalyzed by either of two cytochrome P450’s (Section
15-4Bc), CYP27A1 and CYP2R1.
2. The 25-hydroxycholecalciferol is transported to the
kidney, where it is further hydroxylated by CYP27B1 to
yield the active hormone 1,25-dihydroxycholecalciferol
[1,25(OH)
2
D]. CYP27B1 is activated by PTH, so this reac-
tion is an important control point in Ca
2
homeostasis.
678 Chapter 19. Signal Transduction
H
3
C
H
3
C
CH
2
CH
3
CH
3
CH
3
H
3
C
CH
3
CH
3
H
3
C
HO
R
R X 7-Dehydro-
cholesterol
R Y Ergosterol
R X Vitamin D
3
(cholecalciferol)
R Y Vitamin D
2
(ergocalciferol)
UV
radiation
spontaneous
X
Y
A
10
9
B
CD
H
3
C
R
H
3
C
R
H
3
C
H
H
H
H
HO
HO
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 678
occurs in elderly men and as a consequence of certain hor-
monal disorders or the long-term administration of gluco-
corticoids (Section 19-1G).
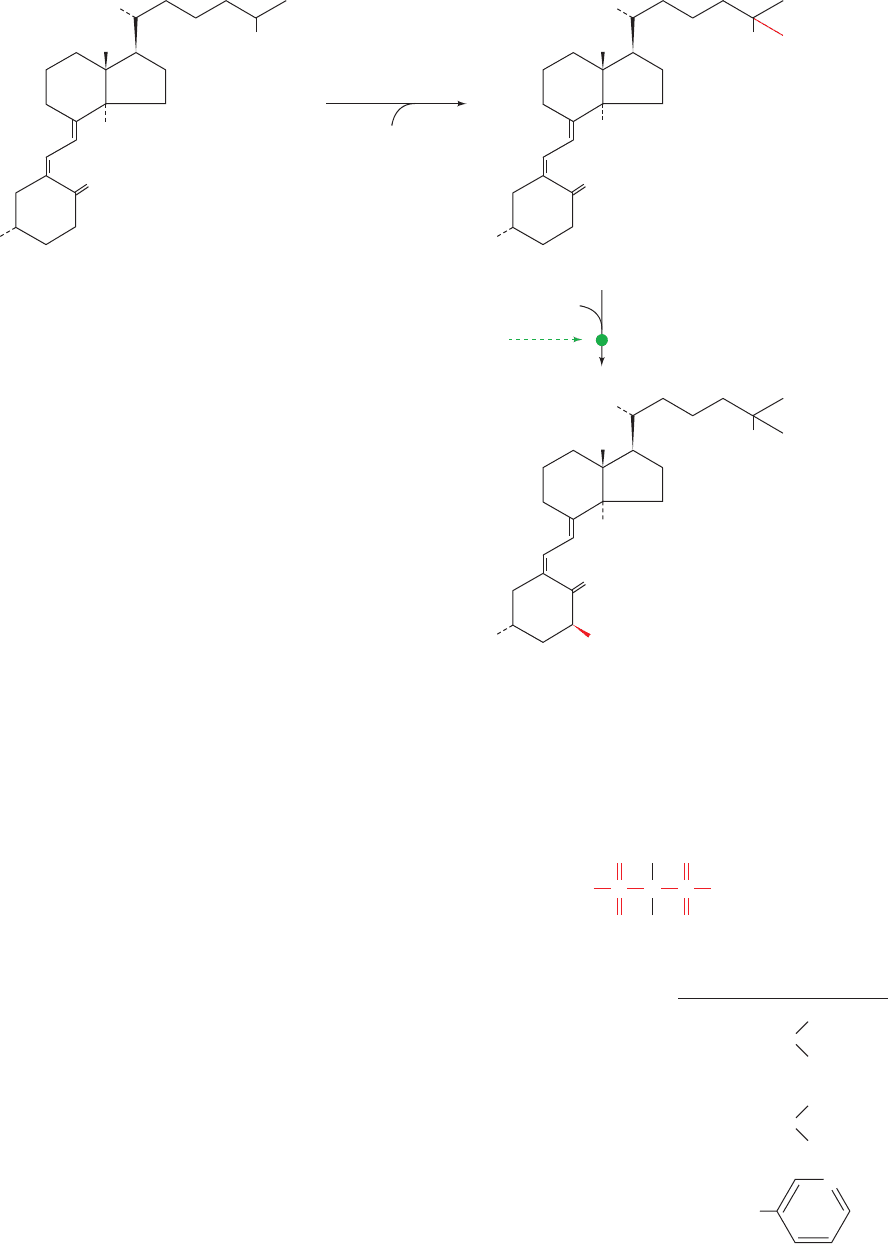
Osteoporosis is most commonly treated by the admin-
stration of bisphosphonates (Fig. 19-7).These drugs bind to
bone tissue from which they are absorbed by osteoclasts.
There they inhibit prenyltransferase (Section 25-6Ac), an
enzyme in the pathway forming the prenyl groups that an-
chor certain proteins to the cell membrane (Section 12-3Ba).
This disrupts the contact region between the osteoclast and
the bone surface, thus decreasing bone resorption. Bisphos-
phonate treatment is usually accompanied by calcium and
vitamin D supplements and by load-bearing exercise.
F. Epinephrine and Norepinephrine
The adrenal glands consist of two distinct types of tissue:
the medulla (core), which is really an extension of the sym-
pathetic nervous system (a part of the autonomic nervous
system), and the more typically glandular cortex (outer
layer). Here we consider the hormones of the adrenal
medulla; those of the cortex are discussed in the following
subsection.
Section 19-1. Hormones 679
Figure 19-6 Activation of vitamin D
3
as a hormone in liver
and kidney. Vitamin D
2
(ergocalciferol) is similarly activated.
Cholecalciferol
(Vitamin D
3
)
(inactive)
25-Hydroxycholecalciferol
1,25-Dihydroxycholecalciferol
[1,25(OH)
2
D]
(active)
CYP27A1
CYP2R1
(liver)
O
2
O
2
CYP27B1 (kidney)
PTH ()
CH
2
CH
3
CH
3
H
3
C
H
3
C
1
25
HO
H
H
CH
2
CH
3
CH
3
H
3
C
OH
H
3
C
HO
H
CH
2
CH
3
CH
3
H
3
C
OH
OH
H
3
C
HO
R
1
R
2
O
COP
O
––
O
OP
O
R
1
R
2
OH
(CH
2
)
2
N
CH
3
CH
3
OH
A
lendronate (Fosamax
TM
)
Ibandronate (Boniva
TM
)
Risedronate (Actonel
TM
)
(CH
2
)
2
N
CH
3
(CH
2
)
4
CH
3
OH
N
CH
2
Figure 19-7 Some bisphosphonates that are in clinical use
against osteoporosis. Each drug has both a generic (chemical)
name and proprietary trade name, here in parentheses, under
which it is marketed.
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 679
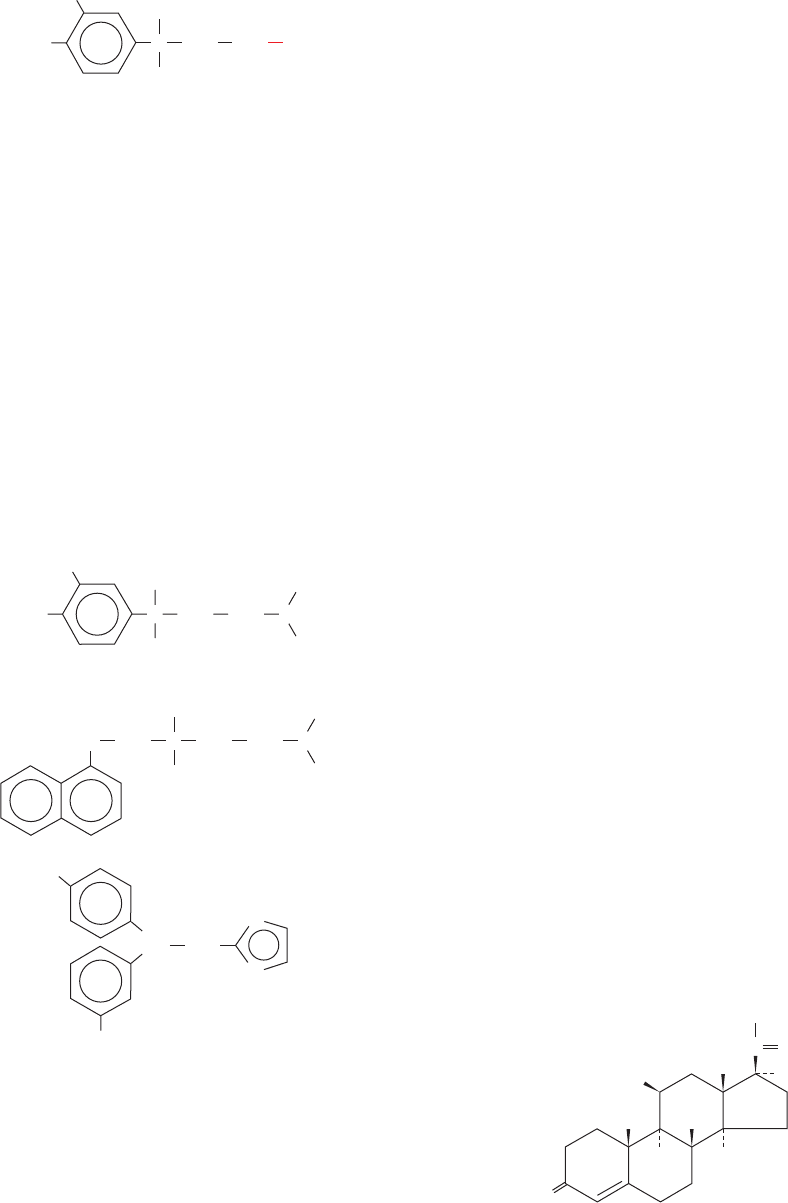
The adrenal medulla synthesizes two hormonally active
catecholamines (amine-containing derivatives of catechol,
1,2-dihydroxybenzene), norepinephrine (noradrenaline)
and its methyl derivative epinephrine (adrenaline):
These hormones are synthesized from tyrosine, as is de-
scribed in Section 26-4B, and stored in granules to await
their exocytotic release under the control of the sympa-
thetic nervous system.
The biological effects of catecholamines are mediated
by two classes of plasma transmembrane receptors, the
- and the -adrenergic receptors (also known as adreno-
receptors). These TM glycoproteins were originally identi-
fied on the basis of their varying responses to certain agonists
(substances that bind to a hormone receptor so as to evoke
a hormonal response) and antagonists (substances that
bind to a hormone receptor but fail to elicit a hormonal
response, thereby blocking agonist action). The - but not
the -adrenergic receptors, for example, are stimulated by
isoproterenol but blocked by propranolol, whereas - but
not -adrenergic receptors are blocked by phentolamine:
The - and -adrenergic receptors, which occur in sepa-
rate tissues in mammals, generally respond differently and
often oppositely to catecholamines. For instance,-adrenergic
receptors, which activate adenylate cyclase, stimulate gly-
cogenolysis and gluconeogenesis in liver (Sections 18-3Ea
and 18-3G), glycogenolysis and glycolysis in skeletal muscle,
OH
Phentolamine
CH
2
H
3
C
NH
N
N
H
+
Isoproterenol
HO
HO C
OH
H
CH
2
CH
3
CH
3
NH
2
CH
+
Propranolol
OH
O
H
CH
2
CH
3
CH
3
CHCCH
2
NH
2
+
HO
HO C
H
OH
CH
2
NH
2
R
R H Norepinephrine (noradrenaline)
R CH
3
Epinephrine (adrenaline)
+
lipolysis in adipose tissue, the relaxation of smooth
(involuntary) muscle in the bronchi and the blood vessels
supplying the skeletal (voluntary) muscles, and increased
heart action. In contrast, -adrenergic receptors, whose in-
tracellular effects are mediated either by the inhibition of
adenylate cyclase (
2
adrenergic receptors; Section 19-2D)
or via the phosphoinositide cascade (
1
adrenergic receptors;
Section 19-4A), stimulate smooth muscle contraction in
blood vessels supplying peripheral organs such as skin and
kidney, smooth muscle relaxation in the lung and gastroin-
testinal tract, and blood platelet aggregation. Most of these
diverse effects are directed toward a common end: the mobi-
lization of energy resources and their shunting to where they
are most needed to prepare the body for sudden action.
The varying responses and tissue distributions of the -
and -adrenergic receptors and their subtypes to different
agonists and antagonists have important therapeutic conse-
quences. For example, propranolol is used for the treatment
of high blood pressure and protects heart attack victims
from further heart attacks, whereas epinephrine’s bron-
chodilator effects make it clinically useful in the treatment
of asthma, a breathing disorder caused by the inappropri-
ate contraction of bronchial smooth muscle.
G. Steroid Hormones
a. The Adrenocortical Steroids Mediate a Wide
Variety of Metabolic Functions
The adrenal cortex produces at least 50 different adreno-
cortical steroids (whose synthesis is outlined in Section
25-6C). These have been classified according to the physio-
logical responses they evoke:
1. The glucocorticoids affect carbohydrate, protein, and
lipid metabolism in a manner nearly opposite to that of in-
sulin and influence a wide variety of other vital functions,
including inflammatory reactions and the capacity to cope
with stress.
2. The mineralocorticoids largely function to regulate
the excretion of salt and water by the kidney.
3. The androgens and estrogens affect sexual develop-
ment and function. They are made in larger quantities by
the gonads.
Glucocorticoids, the most common of which are cortisol
(also known as hydrocortisone) and corticosterone, and
the mineralocorticoids, the most common of which is aldos-
terone, are all C
21
compounds:
Cortisol (hydrocortisone)
O
HO
OH
CO
CH
2
OH
20
21
1
2
4
3
CH
3
5
10
6
7
8
12
11
9
17
13
14
15
16
19
CH
3
18
H
H
H
680 Chapter 19. Signal Transduction
JWCL281_c19_671-743.qxd 3/16/10 7:16 PM Page 680
