Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 8 HOW TO CRITICALLY REVIEW EMERGENCY MEDICINE LITERATURE58
12. Should I read reviews on clinical topics?
This depends on many factors:
n
Are you looking for basic knowledge or understanding of a disease process? If so, a clinical
review may be sufficient and can provide the foundation for you to continue your reading
on the topic.
n
Are you looking for the latest information? Clinical reviews may be outdated by the time of
publication because the literature on which they are based was written before the review.
n
Is it a narrative or systematic review? In narrative reviews, the author selects the articles to
include in the review and summarizes the topic based in part on his or her experience. In a
systematic review, the author identifies articles through a search and includes or excludes
the articles based on predefined criteria and summarizes the topic based on strength of the
evidence from the included articles.
13. How do I practice evidence-based medicine?
Critically reviewing the medical literature and applying the best evidence to your practice is
evidence-based medicine. After reading this chapter, you should be able to read research
studies and determine the strength of the studies and their findings.
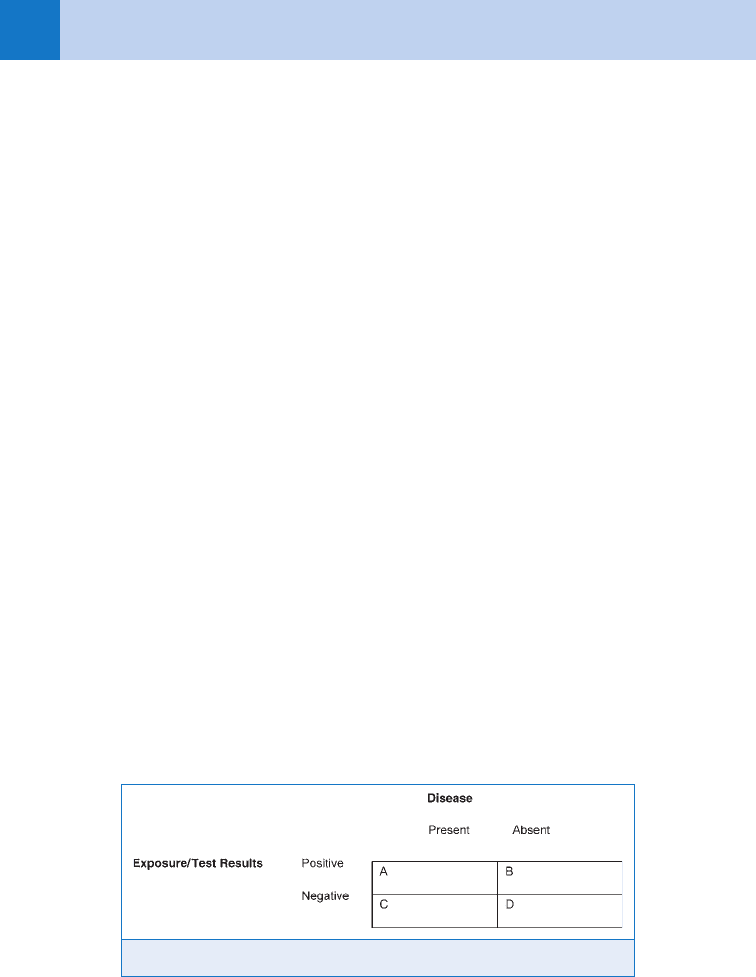
14. What are some of the statistical terms I should be familiar with?
n
Relative risk: The risk of developing a disease after an exposure compared with individuals
without an exposure: A/(A 1 B) 4 C/(C 1 D)
n
Odds ratio: The odds of developing a disease after an exposure compared with those
without an exposure: (AD)/(BC)
n
Sensitivity: The proportion of people with a positive test result who truly have the disease:
A/(A 1 C)
n
Specificity: The proportion of people with a negative test result who do not have the
disease: D/(B 1 D)
n
Positive predictive value: The likelihood that a person with a positive test result actually
has the disease: A/(A 1 B)
n
Negative predictive value: The likelihood that a person with a negative test result does not
have the disease: D/(C 1 D)
See Figure 8-1 for reference.
Figure 8-1. Disease versus exposure grid.
Chapter 8 HOW TO CRITICALLY REVIEW EMERGENCY MEDICINE LITERATURE 59
BIBLIOGRAPHY
1. Barratt A, Wyer PC, Hatala R, et al: Tips for learners of evidence-based medicine: 1. Relative risk reduction,
absolute risk reduction, and number needed to treat. Can Med Assoc J 171:353–358, 2004.
2. Davidoff F, DeAngelis CD, Drazen JM, et al: Sponsorship, authorship, and accountability. JAMA 286:1232–
1234, 2001.
3. Gallagher EJ: P, 0.05: Threshold for decerebrate genuflection. Acad Emerg Med 6:1084–1087, 1999.
4. Gilbert EH, Lowenstein SR, Koziol-McLain J, et al: Chart reviews in emergency medicine: Where are the
methods? Ann Emerg Med 27:305–308, 1996.
5. Jones JB: Research fundamentals: statistical considerations in research design: a simple person’s approach.
Acad Emerg Med 7:194–199, 2000.
6. Sackett DL: How to read clinical journals: Why to read them and how to start reading them critically. Can Med
Assoc J 124:555–558, 1981.
60
EVIDENCE-BASED RATIONAL USE
OF DIAGNOSTIC IMAGING
CHAPTER 9
Ronald R. Townsend, MD, MA, and Stephen V. Cantrill, MD
1. What does evidence-based rational use of imaging mean?
Evidence-based imaging is the application of evidence-based medicine methodology to
decisions regarding the use of diagnostic imaging or interventional image-guided
procedures. A rational decision is made regarding use of imaging in a particular clinical
situation based upon knowledge of the results of published research on the use of
imaging for the problem at hand, the clinical expertise of the provider(s), and the
patient’s values and preferences. Such an analysis may lead to a decision to perform a
specific imaging study or no study at all. Use of evidence-based imaging is motivated by
desires to provide optimal quality patient care and avoid costs and radiation exposure
associated with examinations that will not benefit the patient.
2. Describe the evidence-based approach.
The evidence-based medicine approach incorporates five steps in the determination of a
specific patient scenario:
n
Ask an answerable question.
n
Search the literature for current best evidence.
n
Appraise the retrieved evidence.
n
Apply the findings.
n
Evaluate your success with the process.
Crucial to the process are narrow definitions of the question, complete retrieval of
current literature, and critical analysis of the validity and relevance of the available
research.
3. How is the evidence used by the clinician?
The clinician must decide what, if any, imaging is appropriate based on integration of the
details of the patient’s history, symptoms, and signs with the available evidence. The
unique nature of a given patient’s presentation may make an examination inappropriate,
even if its use is generally supported by evidence.
4. When should I consult a radiologist prior to ordering an imaging study?
For many clinical problems, the appropriate evidence-based imaging may be well known
to the clinician. Especially for complex questions or for patients with recurrent visits to
the ED, consultation with a radiologist prior to any imaging may help optimize the
patient’s care.
5. How can I apply evidence-based imaging in my clinical practice?
Although education regarding use of evidence-based medicine (and its application to
imaging) in medical schools, residencies, and in postgraduate settings is increasing,
most practitioners are overwhelmed by the concept of doing a complete analysis
themselves. Fortunately, there are many resources available to aid the physician in
determining what the evidence suggests will be useful imaging for some common
clinical problems.
Many specialty societies have developed guidelines or appropriateness criteria that
include analyses of application of imaging in many emergency situations (e.g., ACR

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING 61
From Mettler FA, Huda W, Yoshizumi TT, et al: Effective doses in radiology and diagnostic nuclear medicine:
a catalog. Radiology 248:254–263, 2008.
Appropriateness Criteria). These range from opinion papers (not evidence-based) to true
attempts at rigorous evidence-based analysis. Review of the materials accompanying these
guidelines can help clarify their nature, but they may be a useful conduit to the literature in
any case.
6. Are clinical prediction rules helpful?
Evidence-based clinical prediction rules are widely available validated tools to guide
emergency imaging for many scenarios. They typically define specific history, physical
findings, and/or laboratory parameters that accurately predict the utility or lack of utility of
specific imaging.
7. Is radiation exposure from X-rays and CT used in ED patients dangerous?
When evidence-based imaging is performed, the benefit of the diagnostic information obtained
will generally far outweigh any small risk associated with radiation exposure. For example, a
victim of major trauma should not be denied a CT and the potential of image-directed life-
saving treatment, even if she may be pregnant.
However, as of 2007, medical radiation is the largest source of exposure to the U.S.
population, surpassing background radiation. The medically related radiation exposure of the
U.S. population has increased substantially in recent years, related primarily to increased use
of newer diagnostic studies (especially CT, interventional procedures, and nuclear medicine).
Diagnostic radiographs (X-rays or plain films) have relatively low associated radiation, so less
risk. Some examples of average adult effective dose for some imaging procedures are given
below. Newer CT scanning technology may use lower radiation doses for many examinations,
which helps minimize risk (see Table 9-1).
8. Which patients are at highest risk from imaging-related radiation exposure?
Young patients and those who receive many CT scans. The primary concern related to
significant patient radiation exposure is risk of development of neoplasm. The lifetime risk is
highest for children. The patients placed at highest risk as a result of medical imaging are
those who receive multiple high-dose examinations (e.g., CT of multiple body parts),
especially when done repeatedly over months or years. Again, the benefit may substantially
Examination
Average Effective
Dose (mSv)
Range of Values
Reported (mSv)
PA chest radiograph 0.02 0.007–0.050
Pelvis radiograph 0.6 0.2–1.2
Head CT 2 0.9–4.0
Chest CT for pulmonary embolism 15 13–40
Abdomen CT 8 3.5–25
Pelvis CT 6 3.3–10
IR-pelvic vein embolization 60 44–78
Background (annual) 3 Geographic variation
TABLE 9-1. ADULT EFFECTIVE DOSES FOR IMAGING PROCEDURES
mSv, milli-Sieverts (1 mSv 5 100 mrem).

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING62
9. What question should be asked when ordering diagnostic imaging studies in
young patients?
For young patients with chronic problems, an important question to consider: Is there an
evidence-based imaging approach that can address the patient’s need without use of ionizing
radiation? This often involves use of ultrasound or magnetic resonance imaging (MRI).
Consultation with a radiologist should be considered in planning the approach to such patients.
10. What else should be considered when ordering diagnostic imaging?
Unnecessary imaging contributes to the high cost of health care that ultimately is a burden to
society. A CT of the chest, abdomen, and pelvis, for example, may result in charges of more
than $5,000. For the individual patient, an incidental finding at imaging may result in wasted
time and money to work up the finding, which most often proves not significant. There is the
potential for substantial morbidity or even mortality if this leads to biopsy or surgery. This
may be viewed as unavoidable if the initial imaging was clearly indicated but is even more
tragic if it was not.
11. Should a cervical spine CT be obtained in all trauma patients?
No. Many trauma victims have virtually no likelihood of clinically significant cervical spine injury.
An evidence-based approach would be to utilize one of the published clinical prediction rules to
determine who should be imaged. The NEXUS criteria and Canadian C-spine rule define patients
in whom no imaging is necessary (see Chapter 82). There is no clear evidence to favor one of
these rules over the other and not enough data to confirm validity in children. In patients who
are at high risk of cervical spine injury, CT is more sensitive and specific than plain radiography.
12. Which patients should get a cervical spine CT without cervical spine X-ray?
A validated rule (referred to as the Harborview high-risk cervical spine criteria) defines a
subgroup of patients who meet NEXUS or Canadian C-Spine rule criteria who may be
effectively managed with CT as the initial cervical spine imaging. This includes adults with any
one of these parameters (who would typically be getting head CT contemporaneously):
Injury mechanism parameters:
n
High-speed (.35 mph combined impact) motor vehicle accident (MVA)
n
Crash with death at scene of MVA
n
Fall from height .10 ft.
Clinical parameters:
n
Significant closed head injury (or intracranial hemorrhage seen on CT)
n
Neurologic symptoms or signs referred to the cervical spine
n
Pelvic or multiple extremity fractures
KEY POINTS: RISKS OF IMAGE-RELATED RADIATION
1. Risk benefit analysis clearly favors the performance of evidence-based imaging in the ED.
2. Patients who receive multiple high-dose imaging examinations (especially CT) are at highest
risk of long-term consequences.
3. Young patients are at higher risk than older patients.
outweigh the risk for patients with clearly indicated examinations. Nevertheless, before
ordering any examinations, it is prudent to carefully review the imaging history of a patient
who frequently presents to the ED with recurrent problems such as chest pain, abdominal
pain, or renal colic. For example, does a young woman with recurrent kidney stones need
another CT to evaluate her stones or can she be effectively managed with ultrasound?

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING 63
13. Should all chest pain patients get a CT to exclude pulmonary embolism?
No. Such an approach would be expensive, subject many patients to unnecessary radiation,
and potentially contribute to missed diagnoses of pathology not evident on CT. A clinical
prediction rule can be used to distinguish patients who may benefit from imaging for possible
pulmonary embolism from those unlikely to have embolism (See Chapter 27).
14. When should patients with clinical suspicion of kidney stones get a
noncontrast CT of the abdomen and pelvis (CT-KUB)?
Evidence does support CT as the most accurate examination in the diagnosis of urinary stone
disease. It clearly has the highest sensitivity and specificity of all imaging modalities for
ureterolithiasis. It can facilitate management decisions by accurately assessing stone size and
number and the degree of collecting system dilatation. However, many patients with prior CT
documentation of urinary stone disease present to the ED on multiple occasions, and it may
not be necessary or prudent to perform another CT-KUB at each visit.
15. What imaging other than CT-KUB should be considered for patients who
frequently present to the ED with symptomatic urinary stone disease?
Many patients with recurrent urinary calculi may be managed with symptomatic treatment.
If any imaging is necessary to facilitate management, ultrasound may provide the necessary
information. Ultrasound may detect hydronephrosis as a sign of obstruction. The low
sensitivity of ultrasound for ureteral calculi limits its utility in the initial evaluation of patients
with possible stone disease.
16. Is CT or MRI ever appropriate to evaluate extremity trauma?
In the vast majority of clinical situations, the presence or absence of fracture in an extremity is
accurately determined by physical examination with or without plain radiography. Evidence-
based rules defining which trauma patients need and which do not need radiography are well
validated for some body parts (e.g., Ottawa ankle, foot, and knee rules).
Some patients may have persistent symptoms, but no radiographic confirmation of
fracture. The appropriate imaging approach to these patients depends on the anatomic site
involved and specific symptoms and signs. In some situations, additional radiographic views
(e.g., obliques) may define an injury. Many of these situations are uncommon enough that
strong evidence to guide practice is limited. For many non–weight-bearing bones, persistent
clinical suspicion of nondisplaced fracture can be addressed with 10-day follow-up
radiography, at which time a healing fracture may become evident.
Evaluation of possible occult, lower extremity fracture in a patient who is unable to
ambulate, especially with symptoms related to the hip, may require additional urgent imaging.
CT, MRI, and bone scan all have been utilized to diagnose radiographically occult hip fracture.
CT with multiplanar reconstructions is most useful to diagnose subtle cortical disruption, but
MRI has the advantage of better assessing soft tissue (e.g., cartilage).
There is strong evidence to support the use of MRI in assessing soft-tissue injuries in the
knee, but this is rarely required during an ED visit. Emergent CT to further define some
fractures may be needed to plan treatment. This is most common for fractures of the hind and
mid foot and intra-articular fractures about the knee, ankle, or elbow. When clinical findings
lead to suspicion of vascular injury associated with extremity fracture or fracture-dislocation,
further evaluation with catheter angiography or CT angiography may be appropriate. Strong
evidence to support the use of CT angiography for this purpose is lacking for some vessels,
however.
17. Does the evidence support use of CT or plain films for facial fracture
imaging?
CT (especially thin section multidetector CT with multiplanar reconstruction) has higher
sensitivity and specificity than plain radiography in diagnosis of many types of facial fractures.
Complex facial fractures are almost all managed based on CT findings. In general practice,

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING64
most practitioners use CT as the initial and only examination in evaluating patients with
definite fractures clinically and those felt to have high probability of fractures. (The exception
is nasal bone fractures, which usually require no imaging for diagnosis or treatment.)
However, there is a lack of strong evidence to support specific imaging algorithms for specific
patient groups.
18. What are the indications for emergent MRI for ED patients?
MRI is usually the best examination for patients with acute atraumatic myelopathy, who may
be at risk for progressive neurologic deficit related to spinal cord compression by tumor,
abscess, or hematoma. The urgency of the examination cannot be completely defined by
evidence but requires clinical judgment.
Acute focal neurologic deficits referable to intracranial pathology often require emergent
imaging. Either CT or MRI (either examination often requiring contrast) may be supported by
evidence in some circumstances. Patient-specific factors (i.e., history, details of deficit, time
course) and local imaging equipment capability/availability may be important factors in
deciding on CT or MRI. Consultation with the local radiologist should be considered.
Evidence supports use of contrast-enhanced CT in patients with clinical suspicion of aortic
dissection. However, intravenous (IV) contrast administration may be contraindicated in
patients with severe allergy or acute renal failure. MRI with contrast (contraindicated with
renal failure) or without contrast may be appropriate in some patients. Transesophageal
ultrasound may be an alternative in institutions where that is available.
19. What imaging should be done when appendicitis is suspected clinically?
No imaging should be done if management will not be changed (e.g., the surgeon is clinically
convinced the patient has appendicitis and will operate no matter what is found at imaging).
CT of the abdomen and pelvis has the best accuracy in diagnosis of appendicitis and
differentiating it from other causes of right lower quadrant pain. Use of oral and/or rectal
contrast for the examination is largely a matter of institutional experience or preference. IV
contrast has been used in most studies evaluating CT for appendicitis, but accuracy is similar
in other studies without it. Use of IV contrast may improve definition of associated abscess or
other pathology causing right lower quadrant pain.
Compression ultrasound is less sensitive than CT for appendicitis but may be most useful
in the effort to avoid radiation exposure in pregnant or other high-risk patients. MRI has been
used to diagnose appendicitis in pregnant patients, but there is little evidence regarding its
accuracy. Consultation with a radiologist should be considered regarding local experience with
ultrasound or MRI if use of those examinations for diagnosis of appendicitis is considered.
20. What imaging should be performed for a clinical diagnosis of acute
pancreatitis?
With a patient’s first diagnosis of acute pancreatitis, ultrasound is appropriate to evaluate for
gallstones as a possible cause of the pancreatitis. If biliary dilatation is identified on that
examination, further evaluation may be required. CT with IV contrast is most useful to evaluate
complications of pancreatitis (e.g., necrosis, pseudocyst) but usually not appropriate at the
time of initial diagnosis in the ED.
21. What imaging should be performed to evaluate a palpable abdominal or pelvic
mass?
The patient’s demographics (e.g., gender, age) and location of the palpable mass affect
imaging choice.
A palpable pelvic mass in a woman, most often related to uterine or ovarian pathology, is
best evaluated with pelvic ultrasound (transabdominal and transvaginal), including Doppler.
A pulsatile midline abdominal mass in an older adult may be well evaluated with
ultrasound of the abdominal aorta to identify any aneurysm and determine its size and extent.
If ultrasound is technically limited (e.g., obese patient), CT can be used to evaluate for

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING 65
aneurysm or another cause of the mass. In a patient with acute symptoms suspicious for
aneurysm rupture, the patient’s condition should determine whether imaging is advisable
before intervention, but ultrasound cannot accurately determine presence or absence of blood
leaking from an aneurysm. CT with IV contrast is best for that assessment.
In an adult, a palpable abdominal mass not clearly related to any organ by examination is
best evaluated by CT. There is a paucity of data comparing imaging approaches for abdominal
masses, however. When a palpable mass may be an enlarged organ (e.g., liver or spleen),
ultrasound may confirm that diagnosis without requiring use of ionizing radiation.
In an infant, palpable masses often relate to kidneys or the biliary tree, with best initial
evaluation with ultrasound.
22. What is appropriate evidence-based imaging for right upper quadrant pain?
Abdominal ultrasound is highly accurate in the diagnosis of cholelithiasis and should be the
first imaging study when that is the primary question. Ultrasound and clinical and/or
laboratory parameters together allow accurate diagnosis of acute cholecystitis in most patients
without additional imaging. In problematic cases (especially possible acalculous cholecystitis),
cholescintigraphy (nuclear medicine examination of the gallbladder) may be useful to diagnose
acute cholecystitis, but it is not often required for management of patients in the ED.
Cholescintigraphy does have a higher sensitivity than ultrasound in the diagnosis of acute
cholecystitis. One advantage of ultrasound is its ability to identify nonbiliary causes of right
upper quadrant pain in these patients (e.g., disease in the liver or right kidney).
KEY POINTS: EVIDENCE-BASED IMAGING
1. Base imaging choices on patient symptoms and signs. Avoid shotgun imaging.
2. Only perform imaging studies that will affect patient management. Abdominal radiographs
are generally wasteful if CT or ultrasound will be performed, regardless of findings on the
radiograph.
23. What imaging should be done for suspected small bowel obstruction?
Abdominal radiographs have limited sensitivity for detection of small bowel obstruction and
limited ability to determine etiology of any obstruction present. If management decisions are
not to be made based on results of the radiographs, they should not be obtained (e.g., if the
patient will get and be managed based on results of CT whether the radiographs are positive
or negative). CT of the abdomen and pelvis with IV (but not oral or rectal) contrast may best
define presence of obstruction, its cause, and any evidence of secondary compromise of
bowel. Ultrasound can also identify findings of small bowel obstruction, but it is probably not
as sensitive as CT (little evidence).
24. What is appropriate evidence-based imaging for left lower quadrant pain?
When diverticulitis is the primary clinical concern, CT of the abdomen and pelvis with IV and
oral (with or without rectal) contrast best defines the presence and extent of diverticulitis. It
defines presence or absence of complications, such as perforation or abscess formation,
which are important in patient management. Other conditions that can mimic diverticulitis
clinically (e.g., epiploic appendigitis) can be diagnosed with CT. Compression ultrasound can
be used for diagnosis of diverticulitis, but it appears less accurate than CT (limited data).
25. What imaging is appropriate for suspected abdominal abscess?
CT of the abdomen and pelvis with IV and enteric (oral and/or rectal) contrast can effectively
evaluate for abdominal abscess in patients with abdominal pain and fever or other history,
symptoms, and signs causing suspicion of abscess. If there are localizing symptoms and

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING66
signs, a targeted ultrasound may be effective (e.g., clinical question of pericholecystic abscess
or question of abdominal wall abscess along a surgical wound), but there is little data
comparing alternative imaging approaches in this context. For possible pelvic abscess related
to infections of gynecologic origin, transabdominal and transvaginal pelvic ultrasound with
Doppler should be considered.
26. When is imaging appropriate for patients with scrotal pain?
When the cause of acute scrotal pain is not evident clinically, scrotal ultrasound with Doppler
evaluation of testicular blood flow is the most accurate examination in diagnosis of testicular
torsion and distinguishing torsion from other pathologies. It should be performed emergently
to optimize the chance of testicular salvage if torsion is present. Radionuclide perfusion
studies can be utilized for diagnosis of torsion but may have limited specificity and are usually
less available than ultrasound.
27. Should a head CT be performed in all trauma patients?
No. Many patients will not benefit from a head CT. History, symptoms, and signs can be used
to identify patients at significant risk of intracranial injury post trauma (see Chapter 83). The
New Orleans Criteria for patients with a minor head injury and a Glasgow Coma scale score of
15 limits CT to patients with one of seven findings: headache, vomiting, age older than 60 years,
drug or alcohol intoxication, deficits in short-term memory, physical evidence of trauma above
the clavicles, or seizure. In other patient populations (patients with a coagulopathy) other rules
or guidelines may be useful.
28. How about a head CT on anticoagulated trauma patients?
There are data that anticoagulated trauma patients are at greater risk to develop a traumatic
brain injury, and when it occurs, the injury will be more severe with a higher fatality rate. For
this reason, the threshold for obtaining a head CT on an anticoagulated trauma patient should
be very low. These patients may also require closer monitoring and potential repeat head CT
because of the possible development of a delayed acute subdural hematoma.
29. Should patients with closed head injury routinely receive a CT of the abdomen
and pelvis at time of head CT?
The clinical threshold for obtaining a CT of the abdomen and pelvis in trauma patients with
head injuries is reduced at many centers. It is clear that occult injuries may be identified in
such patients. There is a lack of strong evidence, however, regarding which patients benefit
from this approach.
WEBSITES
ACR Appropriateness Criteria: www.acr.org/SecondaryMainMenuCategories/quality_safety/app_
criteria.aspx
Canadian C-spine Rule: www.aafp.org/afp/20040615/tips/17.html
Harborview High-risk Cervical Spine Criteria: www.ajronline.org/cgi/reprint/174/3/713.pdf
NEXUS Criteria: www.aafp.org/afp/20060515/poc.html

Chapter 9 EVIDENCE-BASED RATIONAL USE OF DIAGNOSTIC IMAGING 67
BIBLIOGRAPHY
1. Christopher Study Investigators: Effectiveness of managing suspected pulmonary embolism using an algorithm
combining clinical probability, d-dimer testing, and computed tomography. JAMA 295:172—179, 2006.
2. Hanson JA, Blackmore CC, Mann FA, et al: Cervical spine injury: a clinical decision rule to identify high-risk
patients for helical CT screening. AJR 174:713–717, 2000.
3. Haydel MJ, Preston CA, Mills TJ, et al: Indications for computed tomography in patients with minor head
injury. N Engl J Med 343:100–105, 2000.
4. Medina LS, Blakemore CC: Evidence-based imaging: optimizing imaging in patient care. New York, 2006,
Springer, pp 1–569.
5. Mettler FA, Huda W, Yoshizumi TT, et al: Effective doses in radiology and diagnostic nuclear medicine: a
catalog. Radiology 248: 254–263, 2008.
6. Self MA, Blake A-M, Whitley M, et al: The benefit of routine thoracic, abdominal, and pelvic computed
tomography to evaluate trauma patients with closed head injuries. Am J Surg 186:609–614, 2003.
7. Smits M, Dippel DWJ, de Hann GG, et al: External validation of the Canadian CT head rule and the New Orleans
Criteria for CT scanning in patients with minor head injury. JAMA 294:1519–1525, 2005.
8. Staunton, M: Evidence-based radiology: steps 1 and 2. Asking answerable questions and searching for
evidence. Radiology 242:23–31, 2007.
