Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


28
Jason S. Haukoos, MD, MSc
SHOCK
CHAPTER 4
1. Define shock.
A clinical syndrome characterized by widespread inadequate oxygenation and supply of
nutrients to tissues and organs resulting in cellular dysfunction.
2. How common is shock?
Although the prevalence is not precisely known, it is thought that shock constitutes
approximately 1% of all ED visits.
3. What is the overall mortality rate of patients who develop shock?
The mortality rate exceeds 20% for patients across all categories of shock.
4. List the five categories of shock and provide examples of each.
n
Hypovolemic: Examples: Trauma; gastrointestinal bleeding; ruptured ectopic
pregnancy; ruptured abdominal aortic aneurysm; and diabetic ketoacidosis.
n
Cardiogenic: Examples: acute myocardial infarction; cardiomyopathy; and valvular
dysfunction.
n
Distributive: Examples: sepsis; anaphylaxis; and spinal cord injury.
n
Obstructive: Examples: pulmonary embolism; cardiac tamponade; and tension
pneumothorax.
n
Toxic/Metabolic: Examples: carbon monoxide; cyanide; b-blocker; calcium channel
blocker; adrenal insufficiency; and thyroid storm.
5. How do you identify a patient in shock?
The successful treatment of an acutely ill patient with a high risk of death is predicated
on early recognition and treatment. A patient in shock will generally appear ill. Shock is a
clinical syndrome that reflects hypoperfusion. A brief focused history and targeted
physical examination will help determine if shock is present and its underlying etiology.
Examples of system-based symptoms and signs include:
n
Central nervous system: altered mental status.
n
Cardiovascular: decreased cardiac output; tachycardia; hypotension; and weak rapid
pulses.
n
Pulmonary: tachypnea; and hyperpnea.
n
Renal: decreased urine output.
n
Skin: delayed capillary refill; cool and mottled in the setting of hypovolemic or
cardiogenic shock, and warm and moist in the setting of distributive shock.
6. How should urine output be used during resuscitation of a patient in
shock?
Patients in shock should have a Foley catheter placed to accurately measure urine
output. Urine output is an excellent indicator of organ perfusion, assuming the patient
had normal renal function at baseline. A normal urine output is .1.0 mL/kg/hour, a
reduced urine output ranges from 0.5 to 1.0 mL/kg/hour, and a severely reduced urine
output is ,0.5 mL/kg/hour. During resuscitation, targeted therapy should additionally
focus on improving or normalizing urine output.

Chapter 4 SHOCK 29
7. Describe compensated and decompensated shock.
Shock initiates a sequence of stress responses intended to preserve perfusion to vital organs.
Compensated shock occurs soon after the onset of shock and is marked by the maintenance
of tissue perfusion pressures. Such patients typically have evidence of a stress response
(e.g., tachycardia and tachypnea) but also have a normal or high blood pressure and normal
or mildly elevated serum lactate concentrations. If left untreated, compensated shock will
progress to decompensated shock, which is characterized by profound global tissue
hypoperfusion, elevated serum lactate concentration, and hypotension.
8. What is the initial management of a patient who presents in shock?
Management of patients in shock begins with the ABCs (i.e., airway, breathing, and
circulation). Due to poor delivery and uptake of oxygen, all patients should be placed on either
15 L of oxygen by nonrebreather mask or intubated. Simultaneously, all patients should have
large-bore intravenous access and be placed on a cardiac monitor.
9. Define oxygen delivery.
DO
2
5 CaO
2
3 CO
DO
2
, oxygen delivery
CaO
2
, arterial oxygen concentration
CO, cardiac output
CaO
2
5 (1.34 3 Hgb 3 SaO
2
) 1 (0.003 3 PaO
2
)
Hgb, hemoglobin
SaO
2
, arterial oxygen saturation
PaO
2
, arterial oxygen partial pressure
Oxygen delivery is the product of the cardiac output and arterial oxygen concentration.
Arterial oxygen concentration is defined by the hemoglobin level, the arterial oxygen saturation,
and the arterial oxygen partial pressure. Maximizing cardiac output, hemoglobin, arterial oxygen
saturation, and the arterial partial pressure of oxygen will maximize oxygen delivery.
10. How useful are vital signs in assessing and treating someone in shock?
Vital signs are vital. Heart rate, respiratory rate, blood pressure, and pulse oximetry should
be monitored closely in patients in shock. Physiologic compensation and decompensation
(see Question 7) are commonly reflected in a patient’s vital signs. Additionally, normalization
of abnormal vital signs is one indicator of a patient’s response to resuscitation.
11. If a patient has normal vital signs, should I be reassured?
No. A patient’s heart rate and blood pressure may be normal in the setting of severe illness. In
the setting of shock, heart rate and blood pressure correlate poorly with cardiac output and
often underestimate the severity of systemic hypoperfusion.
12. Are orthostatic vital signs a sensitive indicator of hypovolemia? What
determines a positive orthostatic test?
To know what is abnormal, you first must know what is normal. Studies on healthy euvolemic
people showed an average increase in pulse of 13 to 18 beats per minute with a large
standard deviation. A pulse increase of 20 beats per minute as a determinant for hypovolemia
is nonspecific because many normal individuals fall within this range. However, an increase of
30 beats per minute in heart rate is more specific. A 20% volume loss is required to produce
this change in heart rate, making this an insensitive test at best. The development of
symptoms (e.g., lightheadedness on standing) does not occur in healthy euvolemic individuals
upon standing and should be considered abnormal. Patients in shock should not be allowed to
stand to assess changes in vital signs.

Chapter 4 SHOCK30
13. Are there other signs that are helpful in assessing an acutely ill patient?
Yes. Besides vital signs, components of the physical examination (e.g., level of consciousness,
capillary refill, and urinary output), you should pay close attention to the patient’s serum
lactate, central venous pressure (CVP), and central venous (ScvO
2
) or mixed venous (SvO
2
)
oxygen saturation.
14. How should I use and interpret a serum lactate?
Serum lactate is a commonly used marker to assess the extent of systemic hypoperfusion and
the degree to which a patient may be responding to resuscitation. In fact, it is an early marker of
systemic hypoperfusion and is often elevated prior to overt changes in a patient’s vital signs.
Therefore, liberal use of this marker may help identify patients earlier in their disease processes.
A serum lactate concentration .4 mEq/L is associated with the highest mortality rates.
15. What is the Lactate Clearance Index, and how can it be used during
resuscitation of a patient in shock?
The Lactate Clearance Index refers to measuring serum lactate concentrations at two or more
times during the course of the resuscitation. If after 1 hour of the beginning of resuscitation
efforts, the serum lactate concentration has not decreased by 50%, additional steps should be
undertaken to improve systemic perfusion.
16. What is a normal CVP and how is it measured?
A normal CVP ranges from 5 to 10 cm H
2
O. Central venous pressure is measured by attaching
an electronic pressure transducer or a water manometer to the end of an intravenous line
placed into the central venous system. The zero reference point for measuring a CVP is at the
point that bisects the fourth intercostals space and the midaxillary line in a supine patient,
corresponding to the position of the right atrium.
17. How is CVP used during resuscitation of a patient in shock?
The guiding principal for using the CVP is to normalize or supranormalize its value. The target
CVP should range from 10 to 15 cm H
2
O to maximize cardiac preload. In many shock states,
the heart becomes stiff and its function depressed. A supranormal CVP thus allows for
improved cardiac filling.
18. What is venous oxygen saturation, and what is the difference between a
ScvO
2
and SvO
2
?
Venous oxygen saturation provides a measure of tissue oxygenation (i.e., the balance between
oxygen supply [DO
2
] and demand [VO
2
]). SvO
2
is measured using a pulmonary artery catheter
and includes deoxygenated blood returning to the heart from the body, as well as
deoxygenated blood from the heart via the coronary sinus. It normally ranges between 65%
and 75%. ScvO
2
, on the other hand, is measured using a central venous catheter and
consistently overestimates (albeit to a small degree) venous oxygen saturation because it does
not include sampling of blood mixed with blood returning from the heart.
19. How do I use a ScvO
2
or a SvO
2
during resuscitation?
An ScvO
2
,65% suggests decreased oxygen supply or increased demand. In response,
attempt to improve oxygen delivery by increasing arterial oxygen saturation (SaO
2
) and/or
arterial oxygen partial pressure (PaO
2
) via oxygen supplementation; hemoglobin concentration
via transfusion; and/or cardiac output via inotropic support.
20. What is early goal-directed therapy?
Goal-directed therapy refers to the practice of resuscitating patients to defined physiological
endpoints (e.g., mean arterial pressure, CVP, urine output, serum lactate concentration,
cardiac output, hemoglobin level, and SvO
2
), indicating that systemic tissue perfusion and
vital organ function have been restored. This has only been rigorously studied in patients with
sepsis; however, it has recently been evaluated in postcardiac arrest. It is likely that early

Chapter 4 SHOCK 31
goal-directed therapies will be evaluated in other forms of shock in the future, thus guiding
emergency physicians’ abilities to improve resuscitation endpoints and survival.
21. List the primary resuscitation goals in patients suffering from shock.
n
Maximize oxygenation.
n
Establish adequate ventilation.
n
Improve hemodynamic dysfunction.
n
Treat the underlying etiology.
22. What is the Trendelenburg position? What purpose(s) does it serve?
Trendelenburg refers to the patient placed in a supine, approximately 45-degree, head-down
position. The purposes of this position have been reported to include improving blood
pressure, redistributing circulating blood volume, placing central lines, and improving the
sensitivity of abdominal ultrasound for intra-abdominal fluid. Although commonly used for the
purpose of improving hemodynamic parameters, several studies have not demonstrated its
utility in significantly improving blood pressure or redistribution of blood volume.
23. Define systemic inflammatory response syndrome (SIRS).
SIRS is defined by two or more of the following:
n
Temperature .38°C or 36°C.
n
Heart rate .90 beats per minute.
n
Respiratory rate .20 breaths per minute or partial pressure of carbon dioxide (PaCO
2
)
,32 mm Hg.
n
Serum white blood cell count .12,000 mm
3
or ,4,000 mm
3
or 10% band forms.
It is important to note that this definition, although standardized, is not specific for
defining serious illness. Although most commonly related to sepsis, SIRS may result from a
variety of noninfectious insults, including trauma, burns, pancreatitis, and overdose.
24. Define sepsis, severe sepsis, and septic shock, and discuss their specific
therapies.
See Chapter 47.
25. How do I treat cardiogenic shock?
The treatment of cardiogenic shock should focus on improving myocardial contractility and
overall pump function. Provide oxygen and ventilatory support, including the judicious use of
noninvasive positive-pressure ventilation when pulmonary edema is present. Initiate inotropic
support using dobutamine or dopamine, and identify the etiology and administer specific
treatment (e.g., thrombolysis or percutaneous coronary intervention in the setting of acute
coronary syndrome). Consider intra-aortic balloon counterpulsation or cardiopulmonary
bypass for patients with refractory shock.
26. Explain the mechanism of dobutamine.
Dobutamine is a synthetic catecholamine with primarily b
1
-receptor (cardiac stimulation) and
mild b
2
-receptor (vasodilation) agonism.
27. Explain the mechanism of dopamine.
Dopamine is an endogenous catecholamine that when administered intravenously produces a
dose-dependent activation of adrenergic and dopaminergic receptors. When given in low doses
(e.g., 5 mg/kg/min), dopamine preferentially activates dopaminergic receptors, producing
vasodilatation in renal, mesenteric, and cerebral circulations. When given in intermediate doses
(e.g., 5 to 10 mg/kg/min), dopamine stimulates b-receptors, thus increasing cardiac output.
When given in high doses (e.g., .10 mg/kg/min), dopamine activates a-receptors, producing a
dose-dependent increase in systemic vascular resistance. It is important to note that dopamine
has modest inotropic characteristics when compared to dobutamine and that tachyphylaxis
may result from its use if used for a prolonged period of time.

Chapter 4 SHOCK32
28. How do I treat shock due to anaphylaxis?
See Chapter 18.
29. Explain the mechanism of epinephrine.
Similar to dopamine, epinephrine is a primary b-receptor agonist at low doses and an
a-receptor agonist at high doses. However, epinephrine is significantly more potent than
dopamine.
30. How do I treat shock due to pulmonary embolism (PE)?
Massive PE causes shock by reducing the cross-sectional area of the pulmonary outflow tract,
thus increasing right-sided heart pressures, reducing blood flow to the left side of the heart,
all of which results in a hemodynamic compromised state. Treatment centers on provision of
oxygenation and ventilation, hemodynamic support using crystalloids and vasopressors, as
necessary, and use of thrombolytics or surgical embolectomy in the setting of refractory
shock.
31. How do I treat shock due to cardiac tamponade?
As always, ensure adequate oxygenation and ventilation. Similar to other forms of obstructive
shock (e.g., PE), administration of intravenous fluids may help overcome increased cardiac
filling pressures. However, the principal therapies for cardiac tamponade are
pericardiocentesis or pericardiotomy.
32. What is neurogenic shock and how is it treated?
Neurogenic shock is a form of distributive shock resulting from spinal cord injury in which
central or peripheral sympathetic tone is lost. Such patients are commonly hypotensive with
either a normal or low heart rate. Administer intravenous fluids to normalize intravascular
volume. If hypotension persists, several vasopressor options exist, although intravenous
phenylephrine (0.15 to 0.75 mg/kg/min) is considered the classic first-line agent.
33. Explain the mechanism of phenylephrine.
Phenylephrine is a pure and potent a-agonist. Administration of this agent can induce a reflex
bradycardia, resulting in decreased cardiac output.
KEY POINTS: SHOCK
1. Shock is defined as a clinical syndrome characterized by widespread inadequate
oxygenation and supply of nutrients to tissues and organs, resulting in cellular dysfunction.
2. The five categories of shock are hypovolemic, cardiogenic, distributive, obstructive, and
toxic/metabolic.
3. Serum lactate is a commonly used marker to assess the extent of systemic hypoperfusion
and the response to resuscitation.
4. The primary resuscitation goals in patients suffering from shock are to maximize oxygen-
ation, establish adequate ventilation, improve hemodynamic distribution, and treat the under-
lying cause.
Chapter 4 SHOCK 33
BIBLIOGRAPHY
1. Abramson D, Scalea TM, Hitchcock R, et al: Lactate clearance and survival following injury. J Trauma 35:
584–588, 1993.
2. Bell RM, Krantz BE: Initial assessment. In Mattox KL, Feliciano DV, Moore EE, editors: Trauma, ed 4,,
New York, 2000, McGraw-Hill, pp 153–170.
3. Bone R: American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference:
definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med
20:864–874, 1992.
4. Gaieski DF, Band RA, Abella BS, et al: Early goal-directed hemodynamic optimization combined with therapeutic
hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation 80:418–424, 2009.
5. Kline JA: Shock. In Marx J, editor: Rosen’s emergency medicine: concepts and clinical practice, ed 5,
St. Louis, 2002, Mosby, pp 33–47.
6. Marino PL: The ICU book, ed 2, Baltimore, 1998, Williams & Wilkins.
7. Nguyen HB, Rivers EP, Knoblich BP, et al: Early lactate clearance is associated with improved outcome
in severe sepsis and septic shock. Crit Care Med 32:1637–1642, 2004.
8. Rivers EP, Amponsah D: Shock. In Wolfson AB, editor: Harwood-Nuss’ clinical practice of emergency
medicine, ed 4, Philadelphia, 2005, Lippincott Williams & Wilkins, pp 36–43.
9. Rivers EP, Nguyen B, Havstad S, et al: Early goal-directed therapy in the treatment of severe sepsis and septic
shock. N Engl J Med 8:1368–1377, 2001.
10. Shapiro NI, Howell MD, Talmor D, et al: Serum lactate as a predictor of mortality in emergency department
patients with infection. Ann Emerg Med 45:524–528, 2005.
34
CHAPTER 5
EMERGENCY ULTRASOUND
John L. Kendall, MD, FACEP, and Catherine Erickson, MD
1. What is ED ultrasound all about?
An ultrasound probe in the hands of the clinician has historically been considered the
stethoscope of the 21st century. Extending beyond this definition, the technology of
ultrasound is increasingly considered to be an integral part of the evaluation and
management of ED patients.
2. Why should ultrasound be performed in the ED?
Focused ultrasound examinations performed by ED physicians allow for more timely,
less invasive, and safer evaluations of patients. Ectopic pregnancy and biliary colic may
be evaluated rapidly, intra-abdominal traumatic hemorrhage may be diagnosed without
the invasiveness of diagnostic peritoneal lavage or the delay of a computed tomography
(CT) scan, and patients with major trauma or suspected abdominal aortic aneurysm
(AAA) may be evaluated quickly in the safety of the ED.
3. How does emergency ultrasound differ from ultrasound performed by the
radiology department?
Emergency ultrasound is meant to be a focused, goal-directed examination. Specific
findings, such as the presence of intraperitoneal fluid in blunt abdominal trauma;
intrauterine pregnancy (IUP) in suspected ectopic pregnancy; gallstones, wall thickness,
or sonographic Murphy’s sign in right upper quadrant pain; aortic dilation in suspected
AAA; and pericardial fluid in patients with possible pericardial tamponade, are used to
guide patient care. In contrast, a radiologist-performed ultrasound is more
comprehensive in that all structures viewed are evaluated.
4. How about some basic ultrasonography physics?
Ultrasound images are generated as sound waves at various frequencies (MHz) that
reflect off tissue interfaces. The higher the ultrasound frequency, the greater the
resolution but at the expense of reduced tissue penetration. Dense tissues, such as
bone or gallstones, appear bright because most of the ultrasound energy is absorbed
or reflected. Solid organs, such as the liver or spleen, show a gray scale of tissue
architecture. All of the ultrasound energy passes through fluid or blood, leaving a black
(anechoic) area on the screen. Ultrasound energy does not propagate well through air.
Thus, lung, hollow viscous structures, and air trapped within soft tissues are difficult to
visualize. In general, abdominal and cardiac examinations utilize a 3.5- to 5-MHz probe,
transvaginal ultrasound examinations a 7.5- to 10-MHz probe, and vascular studies a
10- to 12-MHz specialized probe.
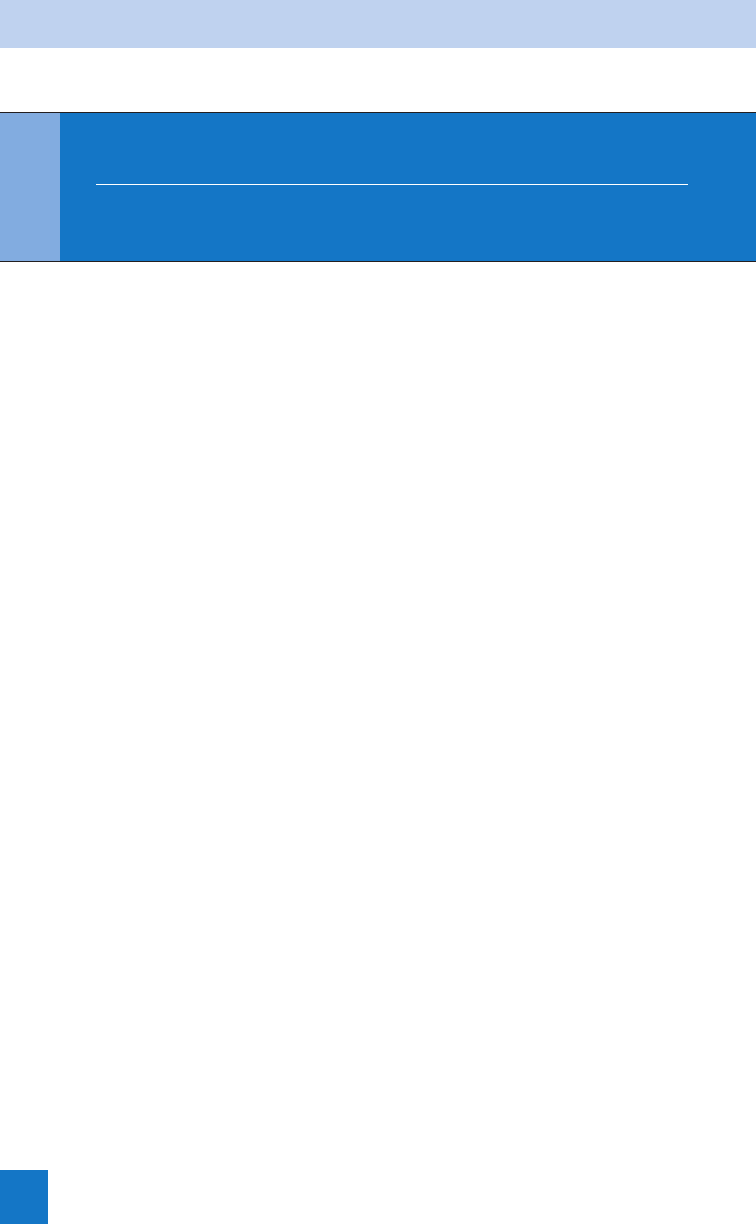
5. Describe the basics of the trauma ultrasound examination.
The trauma ultrasound examination (also known as the focused assessment with
sonography for trauma [FAST]) is done rapidly at the patient’s bedside during the
secondary survey. The primary goal is to detect free intraperitoneal fluid, which appears
as anechoic areas within the peritoneal cavity. Sites in the abdomen that are evaluated
are the potential spaces that occur at dependent sites within the peritoneal cavity. These
include the hepatorenal recess or Morison’s pouch (Fig. 5-1), splenorenal recess,
retrovesicular recess (pouch of Douglas in females), and both pericolic gutters. Oblique

Chapter 5 EMERGENCY ULTRASOUND 35
views of the right and left chest are
obtained to search for hemothorax, and
a subxiphoid or left parasternal cardiac
image is obtained to locate pericardial
effusion (Fig. 5-2).
6. Where is the best place to look
for intraperitoneal fluid?
The sonographic examination should
include all sites previously mentioned.
The sensitivity increases from
approximately 60% if one site is
viewed to almost 90% if all are used.
7. How does ultrasound compare
with traditional means of
evaluating the traumatic
abdomen?
Physical examination is only 50% to
60% sensitive for detecting abdominal
injuries after blunt trauma. Diagnostic
peritoneal lavage is 95% sensitive but
is not specific, resulting in unnecessary
laparotomies. CT is sensitive for
detecting abdominal injuries (.95%)
but is costly, is time consuming, and
requires the patient to leave the ED.
Prospective studies of ultrasound
showed an 83% to 90% sensitivity for
the detection of hemoperitoneum, with
sensitivity approaching 100% in
patients who were hypotensive from an abdominal source. The accuracy of ultrasound to
detect the underlying parenchymal lesion varies widely.
8. How should I use ultrasound in my evaluation of blunt trauma patients?
Consider patient scenarios based on vital signs and ultrasound findings:
a. Stable vital signs, negative ultrasound
b. Stable vital signs, positive ultrasound
c. Unstable vital signs, negative ultrasound
d. Unstable vital signs, positive ultrasound
KEY POINTS: PRIMARY CHARACTERISTICS
OF THE EMERGENCY ULTRASOUND EXAMINATION
1. Performed for a defined indication
2. Focused, not complete
3. Easily learned and quickly performed
4. Directed toward one or two easily recognizable findings
5. Directly impacts clinical decision making
6. Performed at the bedside
Figure 5-2. Subxiphoid cardiac view shows a
pericardial effusion.
Figure 5-1. View of Morison’s pouch showing
intraperitoneal fluid.
Chapter 5 EMERGENCY ULTRASOUND36
Patients with stable vital signs and a negative ultrasound who have no other significant
injuries, have normal mental status, and are not intoxicated can be managed with observation,
serial physical examinations, and serial ultrasound studies. Patients with stable vital signs and
a positive ultrasound warrant an abdominal CT scan. If the vital signs are unstable and
ultrasound is negative or indeterminate, a bedside diagnostic peritoneal lavage can be done
and other etiologies of hypotension considered. If the vital signs are unstable and the
ultrasound is positive for free fluid, the patient should go directly to laparotomy.
9. Can I tell how much intraperitoneal fluid is present based on the ultrasound
image?
No, conflicting data exist. No study has yet shown an accurate means of quantifying the
amount of intraperitoneal fluid that is present based on its sonographic appearance.
10. What are some of the pitfalls I may encounter during a trauma ultrasound
examination of the abdomen?
Although relatively rare, one of the
more concerning aspects of emergency
ultrasound is the false-negative study.
In terms of abdominal trauma, clotted
blood is the finding that mimics a
negative study the closest. An example
of clotted blood found in Morison’s
pouch is shown in Fig. 5-3. It initially
was interpreted to be liver parenchyma
because of a similar echogenic pattern.
False-positive findings that simulate
hemoperitoneum can occur in the
setting of ascites, urine from a ruptured
bladder, bowel contents from bowel
perforation, perinephric fat, and
fluid-filled stomach or bowel.
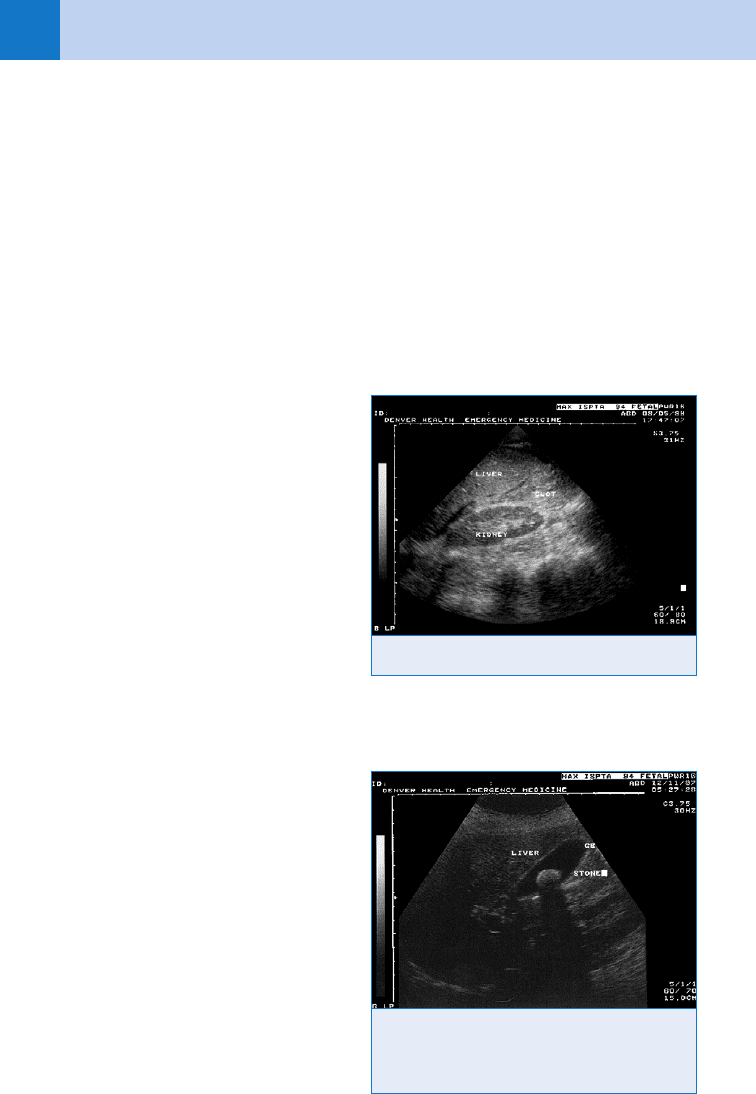
11. What is the sonographic appearance of the gallbladder and related
structures?
The gallbladder is cystic, so the
sonographic appearance is a pearlike
structure that is anechoic. Surrounding
this anechoic area is a ring of
midechogenicity that corresponds to the
gallbladder wall. Normally, it is less than
4 mm wide, but can be thicker
immediately after eating or if in
edematous states, such as liver failure,
ascites, congestive heart failure, renal
disease, or AIDS. Stones are typically
circular in nature, can be of any size, and
are bright, or hyperechoic, on their
proximal side. Ultrasound does not
penetrate stones well, so distal to the
stone there is a shadow (Fig. 5-4). This
also is called the headlight sign,
signifying the presence of a calcified
gallstone. Sludge is a collection of the precipitants of bile that layers within the gallbladder and
appears sonographically as mildly echogenic material without any shadowing.
Figure 5-3. Clotted blood in Morison’s pouch.
Figure 5-4. Long-axis view of the gallbladder
shows a gallstone. The gallstone is represented
by an echogenic proximal surface and distal
attenuation shadow.

Chapter 5 EMERGENCY ULTRASOUND 37
12. What findings are suggestive of acute cholecystitis?
The primary findings of the emergency gallbladder ultrasound are the presence of gallstones
and a sonographic Murphy’s sign (defined as maximal tenderness over an ultrasound-detected
gallbladder). The presence of these primary findings has a 92% positive predictive value and a
95% negative predictive value for the presence of cholecystitis. Other findings, such as wall
thickening (.4 mm), ductal dilation (.6 mm), pericholecystic fluid, sludge, and an
emphysematous gallbladder, are considered to be secondary findings and are less reliably
seen by emergency sonographers. Ultrasound is insensitive at detecting choledocholithiasis.
13. What are the indications for pelvic ultrasonography in the ED?
Ultrasonography is the imaging study of choice for evaluating abdominal pain or bleeding in
pregnant patients in the first or second trimester. The goal of ED ultrasound is to establish the
presence of an IUP, so as to effectively rule out an ectopic pregnancy. Ectopic pregnancy is
the second leading cause overall of maternal mortality and the number one cause of maternal
mortality during the first trimester.
14. How early can an IUP be detected using ultrasound? What value of b-human
chorionic gonadotropin (HCG) does this correspond to?
An IUP may be detectable as early as 4.5 weeks by transvaginal ultrasound at a b-HCG level
of 1,000 to 2,000 mIU/mL (6 weeks or greater with a b-HCG of 5,000 mIU/mL using
transabdominal ultrasound). The discriminatory zone, or level of b-HCG at which one would
expect to see evidence of an IUP, depends on the institution where the patient is being seen.
A gestational sac is seen at approximately 4-5 weeks gestational age and cardiac activity can
be measured as early as 6 weeks gestational age.
15. How sensitive is ultrasound for the evaluation of ectopic pregnancy?
Several studies have shown that 75% to 80% of patients have a diagnostic ultrasound
(i.e., either an IUP or a demonstrable ectopic pregnancy). The problem is that in the remaining
20% of patients with nondiagnostic ultrasounds, nearly one fourth have ectopic pregnancies.
This increase in ectopic pregnancy among patients with nondiagnostic ultrasound suggests
that this group should have thorough evaluation, including an obstetric-gynecologic
consultation in the ED.
16. Describe the pitfalls in pelvic ultrasonography.
For emergency physicians, the goal of pelvic ultrasonography is to determine whether an IUP
is present. It is not clear how well emergency physicians evaluate the adnexa, pelvic free fluid,
or ovaries. Cornual pregnancies may be mistaken for an IUP, with an attendant risk of rupture
and hemorrhage. The question of heterotopic pregnancies (i.e., simultaneous IUP and ectopic
pregnancy) must be considered. In populations without risk factors for ectopic pregnancy, the
risk of a heterotopic gestation is approximately 1 in 30,000 pregnancies. The incidence
increases markedly, however, in patients with preexisting pelvic inflammatory disease or
scarring and is greatest for patients receiving medical fertility assistance, in whom the
incidence is estimated to be 1 in 100 to 1 in 400 pregnancies. A pseudosac can be seen in
20% of ectopic pregnancies. It is formed in response to the b-HCG produced by the abnormal
pregnancy. It consists of a single-ringed structure in the endometrial cavity, and it can be
mistaken for a true gestational sac, which consists of two concentric rings.
17. What other abdominal structures can be evaluated by emergency ultrasound?
Evaluation of the abdominal aorta can be useful in elderly patients who present with a pulsatile
abdominal mass, nontraumatic abdominal pain or flank pain, hypotension of unknown cause,
or unexplained pulseless electrical activity. AAA is manifested by aortic diameter greater than
3 cm with most symptomatic aneurysms being greater than 5 cm (Fig. 5-5). Studies by
emergency physicians showed sensitivity of 100% and a specificity of 98% for the detection
of AAA. Studies showed a 90% correlation of ultrasound-determined aortic diameter to
pathologic specimens.
