Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 5 EMERGENCY ULTRASOUND38
18. What is the significance of
increased aortic diameter?
Longitudinal studies have shown that
patients with AAA have an increase in
aortic diameter of approximately
0.5 cm/year. Patients with an aortic
diameter of greater than 5 cm have a
25% chance of rupture within 5 years,
with larger aneurysms having a greater
chance of rupture. Aneurysms that
rupture have a mortality of greater than
80%, so ultrasound is an important
tool in the detection of AAA.
19. Describe the uses of cardiac
ultrasonography in the ED.
These are primary indications for cardiac ultrasonography in the ED (see Table 5-1):
a. It may be used during the trauma examination to detect pericardial effusions in patients
thought to have mechanisms of injury or clinical presentations consistent with pericardial
tamponade or cardiac rupture.
b. It may be used for detection of nontraumatic pericardial effusions (i.e., malignancy, uremic,
rheumatologic).
c. Another important indication includes the evaluation of patients presenting in cardiac
arrest. Contractility can be assessed in patients presenting in cardiac arrest when there is a
question of pulseless electrical activity. When there is no evidence of cardiac contractility
and other reversible causes of pulseless electrical activity have been ruled out, strong
consideration should be given to terminating the resuscitation.
d. Lastly, emergent echocardiography is starting to be used for detecting central venous
volume status.
20. What is the role of ultrasound in the evaluation of patients with suspected
renal colic?
By itself, ultrasound is only 64% to 75% sensitive for the identification of renal calculi and
even less sensitive for the evaluation of acute hydronephrosis. Studies that combined kidney,
ureter, and bladder radiographs and ultrasound in well-hydrated patients showed improved
ability to identify kidney stones and hydronephrosis. In the end, a noncontrast CT is a far
superior imaging tool for the patients presenting with suspected renal colic. If hydronephrosis
without an etiology is seen on ED ultrasound, further imaging should be pursued.
21. How is lower extremity venous ultrasound performed in the ED to diagnose
deep venous thrombosis (DVT)?
A linear transducer with a high frequency range is used. The examination should start
proximally with the vein in a transverse plane just below the inguinal ligament where the
common femoral vein can be visualized. Compression followed by no compression should
occur in 1-cm increments until the femoral vein dives into the adductor canal. Next the
popliteal region is visualized again in 1-cm increments. An examination is considered to be
negative when complete compression occurs to the point that the anterior and posterior walls
of the vein touch. In a positive study, the vessel walls will not touch; the clot echogenicity can
vary greatly from echogenic to non-echogenic. Recent studies show the sensitivity and
specificity of ED DVT studies to range from 70% to 95% and 89% to 95%, respectively. For
accurate diagnosis of DVT, additional components, such as pretest probability and the D-dimer
assay, may need to be considered.
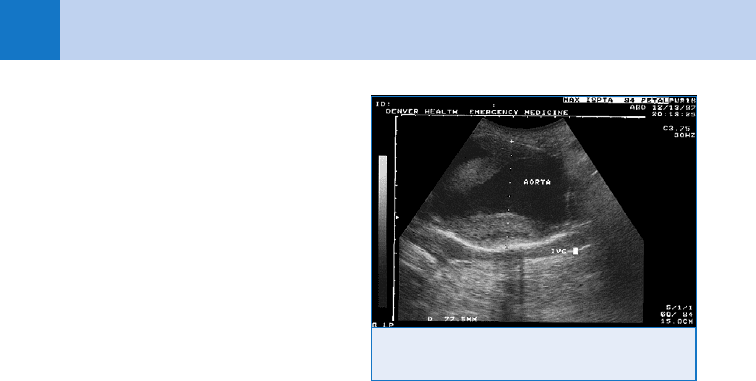
Figure 5-5. Long-axis view of a 7.75-cm diameter
abdominal aortic aneurysm.

Chapter 5 EMERGENCY ULTRASOUND 39
22. What are some future applications for emergency ultrasound?
Uses for emergency ultrasound continue to rapidly expand. This is clearly demonstrated in the
2008 American College of Emergency Physician’s clinical practice guidelines for ultrasound
that expands upon core applications. For instance, one of the fastest-growing applications is
to guide invasive procedures. This is not confined with vascular access but also other
procedures, such as localization and drainage of abscesses, nerve blocks, lumbar puncture,
placement of an intravenous pacer wire, and suprapubic bladder aspiration, to name a few.
Emergency ultrasound is tremendously useful in the evaluation of patients in cardiac arrest,
with undifferentiated hypotension or shock, suspected DVT, testicular torsion, or an
appendicitis diagnosis in the pediatric population.
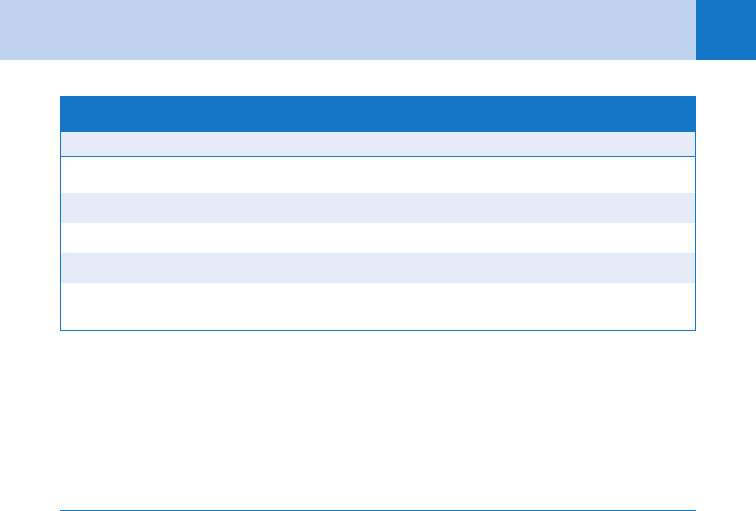
Established Applications Newer Applications
Abdominal Deep venous thrombosis evaluation
Aortic
Biliary Thoracic
Urinary tract Pleural effusion
Pneumothorax
Pelvic
Intrauterine pregnancy Musculoskeletal
Abscess incision and drainage
Trauma Fracture evaluation
Focused abdominal sonography for trauma
Ocular
Cardiac Retinal detachment
Emergent echocardiography Vitreous hemorrhage
Pericardial effusion
Tamponade Procedural
Contractility Pericardiocentesis
Thoracentesis
Procedural Foreign body and detection and removal
Central venous access Arthocentesis
Pacemaker placement
TABLE 5-1. EMERGENCY ULTRASOUND CORE APPLICATION
From American College of Emergency Physicians. ACEP emergency ultrasound guidelines—2008.
Ann Emerg Med 53(4):550–570, 2009.

Chapter 5 EMERGENCY ULTRASOUND40
23. Has the political environment changed with respect to emergency physicians
using ultrasound?
Yes, there have been many changes in recent years. Ultrasound use by emergency physicians
has gone from a novelty experience to something that is tested on emergency medicine
specialty boards and the national inservice examination, is recommended by the American
College of Emergency Physicians to be taught in all residency programs early in training, and
is widely used in clinical practice. As such, the question is no longer whether or not
ultrasound will be used by emergency physicians, but rather how it can be used for optimal
care of ED patients.
BIBLIOGRAPHY
1. Braffman BH, Coleman BG, Ramchandani P, et al: Emergency department screening for ectopic pregnancy: A
prospective US study. Radiology 190:797–802, 1994.
2. Branney SW, Moore EE, Cantrill SV, et al: Ultrasound based key clinical pathway reduces the use of hospital
resources for the evaluation of blunt abdominal trauma. J Trauma 42:1086–1090, 1997.
3. Burnside PR, Brown MD, Kline JA: Systematic review of emergency physician-performed ultrasonography for
lower-extremity deep vein thrombosis. Acad Emerg Med 15:555–557, 2008.
4. Holmes JF, Harris D, Battistella FD: Performance of abdominal ultrasonography in blunt trauma patients with
out-of-hospital or emergency department hypotension. Ann Emerg Med 43:354–361, 2004.
5. Kendall JL, Shimp RJ: Performance and interpretation of focused right upper quadrant ultrasound by
emergency physicians. J Emerg Med 21:7–13, 2001.
6. Kline JA, Omalley PM, Tayal VS, et al: Emergency clinician-performed compression ultrasonography for deep
venous thrombosis of the lower extremity. Ann Emerg Med 52:437–445, 2008.
7. Kuhn M, Bonnin RL, Davey MJ, et al: Emergency department ultrasound scanning for abdominal aortic
aneurysm: accessible, accurate and advantageous. Ann Emerg Med 36:219–223, 2000.
8. Ma OJ, Kefer MP, Mateer JR, et al: Evaluation of hemoperitoneum using a single- vs multiple-view
ultrasonographic examination. Acad Emerg Med 2:581–586, 1995.
9. Ralls PW, Colletti PM, Chandrasoma P, et al: Real-time sonography in suspected acute cholecystitis.
Radiology 155:767–771, 1985.
10. Tayal V, Graf CD, Gibbs MA: Prospective study of accuracy and outcome of emergency ultrasound for
abdominal aortic aneurysm over two years. Acad Emerg Med 10: 867–871, 2003.
41
CHAPTER 6
GERIATRIC EMERGENCY MEDICINE
Kenneth C. Jackimczyk, MD, FACEP
1. Why dedicate a chapter to geriatric emergency medicine?
Elderly persons are a rapidly growing segment of the population. In 2004, approximately 36
million people in the United States were older than age 65. By the year 2030, this number is
expected to double, and over the next 20 years the number of individuals older than age 85 will
grow three times faster than the general population. Patients older than 65 years account for
15% of all ED visits and more than 40% of in-patient admissions. Elderly patients stay in the ED
longer and require more diagnostic studies than younger patients.
Geriatric patients have unique medical and social characteristics. They often have multiple
comorbid conditions that complicate evaluation of the presenting complaint. Diseases often
present atypically in geriatric patients. These patients often have reduced functional reserves,
which make a careful assessment of the patient’s psychosocial environment essential prior to
making decisions about disposition.
2. What important physiologic changes occur with aging?
n
Musculoskeletal: Loss of muscle strength, impaired mobility, and decreased bone mass.
n
Cardiovascular: Decreased cardiac output and increased systolic blood pressure.
n
Pulmonary: Decreased vital capacity and decreased functional reserve.
n
Head, eye, ear, nose, and throat (HEENT): Impaired hearing and vision.
n
Renal: Decreased renal blood flow and glomerular filtration rate (GFR).
n
Immune system: Decreased cellular immunity and decrease antibody titers.
n
Dermatologic: Impaired thermoregulation and atrophy of skin.
KEY POINTS: PRINCIPLES OF GERIATRIC EMERGENCY MEDICINE
1. Vital signs can be normal in the elderly patient with serious illness.
2. Adverse medication reactions are common in elderly patients.
3. Atypical presentations of serious diseases are more common.
3. How can prehospital personnel facilitate the care of elderly patients?
Elderly patients account for more than one third of emergency medical services (EMS)
transports to the ED. Prehospital providers can obtain information from family or health care
workers at the scene regarding the patient’s social and physical environment, his or her
baseline functional and mental status, and the reason for EMS activation. Ambulance
personnel should obtain lists of medications the patient is using and any documentation
regarding living wills or advance directives.
4. What is the significance of fever in elderly patients?
Elderly patients presenting with fever have a significant risk of serious bacterial infection.
Conversely, because of their blunted fever response, bacteremic elderly patients may not be
febrile. Don’t be lulled into complacency by a lack of fever in an ill-appearing elderly patient
because nearly half of patients with serious infections will not have a fever.

Chapter 6 GERIATRIC EMERGENCY MEDICINE42
5. What are the four types of elder abuse?
a. Physical abuse: Nonaccidental force that results in bodily injury or pain (e.g., hitting,
biting, slapping, sexual assault, burns, or unreasonable restraint [physical, chemical]).
b. Psychological abuse: Threats made with the intent of causing emotional pain or injury.
c. Exploitation: Caretaker use of the resources of an elder for monetary or personal profit.
d. Neglect: Failure of the caretaker to provide the services necessary to avoid physical harm,
mental anguish, or mental illness. This neglect can be intentional or unintentional.
6. What red flags in the history should alert the physician to the possibility of
elder abuse?
n
Delay in presentation with injury.
n
Vague or implausible explanation for injury.
n
Repetitive injuries.
n
Missed appointments and noncompliance with medications.
n
No caregiver accompanying an impaired patient to the ED.
7. What red flags in the physical examination should alert the physician to the
possibility of elder abuse?
n
Subdued, oversedated, or withdrawn behavior.
n
Unkempt appearance or poor nutrition.
n
Multiple or unexplained bruises, abrasions, or lacerations.
n
Burns, bites, or pressure sores.
n
Occult fracture.
8. Why is it important to know the elderly patient’s current medications?
Adverse drug-related events are a significant cause of morbidity in elderly patients and are the
most common cause of iatrogenic illness in elderly patients. The average elderly person uses
more than four prescription drugs and more than two over-the-counter medications daily.
These numbers are even higher for institutionalized patients. Adverse reactions to medications
are directly proportional to the number of medications being taken.
9. What presenting complaints should lead me to suspect that the patient is
experiencing an adverse reaction to medications?
n
Altered level of consciousness.
n
Weakness.
n
Dizziness.
n
Syncope.
10. Don’t elderly patients always have abnormal laboratory values?
No. Most laboratory values in geriatric patients do not require different reference ranges from
traditional adult values, and the fact that the patient is elderly should not be used to justify
abnormal laboratory values. There are, however, some exceptions in patients older than age 65:
n
Elevated serum alkaline phosphatase (may be 2.5 times greater than the normal).
n
Elevated fasting blood glucose (135 to 150 mg/dL).
n
Elevated erythrocyte sedimentation rate (40 mm/hour).
n
Decreased hemoglobin (11.0 g/dL in women or 11.5 g/dL in men).
n
Elevated blood urea nitrogen (28 to 35 mg/dL).
11. Should I worry if a geriatric trauma victim has normal vital signs with
apparently minor injuries?
Yes. Vital signs in the elderly may remain normal until acute deterioration occurs. Geriatric
patients have a blunted tachycardic response to injury. A “normal” blood pressure of
120/80 mm Hg may represent relative hypotension in the elderly hypertensive patient. The elderly
patient’s diminished cardiovascular reserve, increased susceptibility to fractures, and the presence
of comorbid conditions such as coronary artery disease can result in significant morbidity, even

Chapter 6 GERIATRIC EMERGENCY MEDICINE 43
with injuries that appear to be minor. Elderly patients have the highest trauma mortality rate of
any age group, and normal vital signs or a low injury severity score should never put the
physician at ease.
12. Which presentations in geriatric trauma are associated with an extremely high
mortality rate?
n
Automobile-pedestrian accidents (.50% mortality).
n
Presenting systolic blood pressure less than 130 mm Hg.
n
Acidosis (pH ,7.35).
n
Multiple fractures.
n
Head injury (67% of unconscious elderly trauma patients die).
n
Pelvic fractures.
13. Aren’t falls a fact of life in elderly patients?
No. Any fall is a serious threat to the independence of the elderly patient. A fall should be
considered a significant symptom that warrants a full ED evaluation because 10% to 15% of
geriatric falls result in serious injury, and 50% of patients who require hospitalization die
within 1 year of their fall.
14. What is different about evaluating the elderly patient who falls?
It is essential to assess the cause of the fall as well as the injuries that have occurred. Falls
may result from either physiologic or environmental factors. Physiologic factors include
muscle weakness, gait and balance disorders, visual impairment, postural hypotension, and
syncope. Environmental disorders include dark hallways, loose rugs, and low-lying tables. The
evaluation for syncope should focus on acute cardiovascular causes (e.g., dysrhythmias,
myocardial infarction), neurologic events, hypovolemia, and adverse reactions to medications.
Use of psychotropic medications, such as benzodiazepines and other sedatives, are associated
with an increased risk of falls in the elderly.
15. Do emergency physicians have a role in prevention of recurrent falls in the
elderly?
Yes. Several studies have shown that risk factors can be identified in the ED (e.g., muscle
weakness, arthritis, cognitive impairment) and reported to the patient’s primary physician so
that interventions can be preformed. Psychotropic drugs may be discontinued or prescribed in
reduced doses. Educating the patient on simple changes that can be made in the home to
reduce falls has also been shown to be helpful.
KEY POINTS: FALLS IN GERIATRIC PATIENTS
1. Falls in elderly patients are a serious problem.
2. Check for both physiologic and environmental causes of the fall.
3. Consider syncope as the cause of the fall.
16. Can procedural sedation be performed safely in the geriatric patient?
Yes, but the physician must be aware of the altered pharmacokinetics and pharmacodynamics
in elderly patients. As the body ages, there is a reduction in lean body mass and total body
water and an increase in total body fat. There also is a decrease in renal and hepatic blood
flow. This has an effect on the metabolism and the distribution of medications administered to
an elderly patient. Elderly patients have increased central nervous system sensitivity to
analgesic and sedative medications. Remember: start low and go slow.
Chapter 6 GERIATRIC EMERGENCY MEDICINE44
17. Should I be concerned about atypical presentations of acute myocardial
infarction (AMI) in elderly patients?
Yes. AMI is the leading cause of death in elderly patients and atypical presentations are
actually typical for AMI in the elderly. Nearly 40% of elderly patients diagnosed with AMI did
not complain of chest pain on presentation, and similarly, 50% had no evidence of ischemia or
infarct on their presenting electrocardiogram (ECG). For these reasons, it is imperative that the
ED physician know the atypical presentations of AMI in elderly patients. The mnemonic
GRANDFATHERS refers to atypical presentations of AMI in elderly patients:
General malaise
Refers to a gastrointestinal complaint
Altered mental status
Neurologic deficits
Dyspnea
Falls or Flu symptoms
Atypical chest pain
Trouble walking
Hypotension
Exhaustion
Reverse in functional status
Syncope or presyncope
18. Should I resuscitate the elderly patient in cardiac arrest?
Yes. Resuscitation studies document no difference in the percentage of successful outcomes
across the age spectrum, and elderly patients who survive are no more likely to sustain
irreversible brain injury than younger patients. Unless there is a well-defined advance directive,
there should be no discrimination based on age in resuscitating elderly patients in cardiac arrest.
19. How does my approach to acute abdominal pain change in elderly patients?
Any complaint of abdominal pain in the elderly should be taken seriously. Elderly patients have
decreased pain perception and are more likely to have normal vital signs in the face of significant
intra-abdominal pathology. Older patients are also less likely to demonstrate peritoneal findings
because they lack well-developed abdominal musculature. These factors cause delays in
diagnosis, higher perforation rates, and higher mortality rates in abdominal diseases in the
elderly. Keep a broad differential diagnosis and consider the common disorders such as
appendicitis and cholecystitis but also remember diseases specific to older patients, such as
diverticulitis, volvulus, mesenteric ischemia, abdominal aortic aneurysm, and carcinomas. CT
scanning should be used liberally in older patients suspected of having a surgical process, but
do not delay surgical consultation waiting for laboratory results or imaging studies.
20. Which is more serious, dementia or delirium?
Delirium. Delirium is considered a medical emergency. The elderly patient may already have
dementia, but a sudden change in mental status may represent an acute organic process,
such as infection or an adverse reaction to a medication. To attribute a change in mental
status to worsening dementia, without searching for an organic cause, is a serious error.
21. How do I differentiate between delirium and dementia?
See Table 6-1.
22. What special concerns are there in discharging elderly patients?
n
Cognitive function: Does the patient understand the discharge instructions? Can the patient
still live independently and self-administer medications?
n
Physical function: Can the patient perform the activities of daily living (bathing, dressing,
feeding)? Does the patient require an assistance device such as a walker or wheelchair?
n
Physical environment: Can the patient safely return with his or her current cognitive or
functional status? Did the current environment contribute to the ED presentation?
Chapter 6 GERIATRIC EMERGENCY MEDICINE 45
n
Social environment: Will the caregiver or spouse be able to care for the patient? Is health
care supervision available?
n
Resources: Is a telephone available? Is money available for medicine or follow-up
appointments? Is there transportation to get to a follow-up appointment?
Delirium Dementia
Acute in onset Insidious in onset
Decreased level of consciousness Clear consciousness
Waxes and wanes Progressive decline
Reversible cause Usually irreversible cause
Irregular sleep-wake pattern Regular sleep-wake pattern
TABLE 6-1. DIFFERENTIATION BETWEEN DELIRIUM AND DEMENTIA
BIBLIOGRAPHY
1. D’Andrea CC: Geriatric trauma. In Ferrera PC, Colucciello SA, Marx JA, et al, editors: Trauma management: an
emergency medicine approach St. Louis, 2001, Mosby, pp 533–545.
2. Gazmuri RJ: Outcome after cardiopulmonary resuscitation: is age a factor Crit Care Med 27:2295–2296, 1999.
3. Gerson LW, Camargo CA, Wilber ST: Home modification to prevent falls in older ED patients. Am J Emerg
Med 23:295–298, 2005.
4. Hohl CM, Dankoff J, Colacone A, et al: Polypharmacy: adverse drug-related events and potential adverse drug
interactions in elderly patients presenting to an emergency department. Ann Emerg Med 38:666–671, 2001.
5. Kleinschmidt KC: Elder abuse: a review. Ann Emerg Med 30:463–472, 1997.
6. Mandavia D: Geriatric trauma. Emerg Med Clin North Am 16:257–274, 1998.
7. Martinez JP, Mattu A: Abdominal pain in the elderly. Emerg Med Clin North Am 24: 371–388, 2006.
8. Meldon SW, Ma OJ, Woolard R, editors: Geriatric emergency medicine, New York, 2004, McGraw-Hill.
9. Sanders AB: Emergency care of the elder person. St. Louis, 1996, Beverly Cracom Publications.
10. Wilber ST: Altered mental status in older emergency department patients. Emerg Med Clin North Am 24:
299–316, 2006.
46
SAFETY IN EMERGENCY MEDICINE
CHAPTER 7
Robert L. Wears, MD, MS
1. The ED has been described as a natural laboratory for the study of safety.
What makes it so?
The conditions of work in EDs typically detract from optimal human performance. These
might be divided into two types: Failure-producing conditions (FPCs) and violation-
producing conditions (VPCs). The former lead to what in folk wisdom are called human
errors, and the latter are conditions that lead people to deviate from formal procedures.
2. Define some basic safety terms.
n
An error is a term of historical interest only. It was originally defined as the failure of
a planned action to be completed as intended (i.e., error of execution) or the use of a
wrong plan to achieve an aim (i.e., error of planning). The concept of error has not
proven useful in creating safer systems of care, and in fact may be harmful, because
of its slipperiness and the pejorative baggage that it carries.
n
Active faults are those whose effects are seen immediately. They are most often
associated with those who perform on the front line (the ED is as front line as it gets).
n
A latent fault is one whose adverse consequences may lie dormant for some time,
only becoming evident when it combines with other factors to breach the system’s
defenses. Responsibility for latent faults can often be laid at the feet of those who
designed or manage the system.
n
Slips describe attentional or perceptual failures in the execution of an observable
action sequence. Covert internal events (generally associated with memory failures)
leading to a failure of execution are referred to as lapses. Both slips and lapses are
actions that deviate from an intended plan.
n
A mistake is a deficiency or failure in either the judgment or inferential process
involved in the selection of an objective, or in the specification of the means to
achieve it, irrespective of whether or not the actions directed by this decision-scheme
run according to plan.
n
An incident or near miss is a failure in some aspect of care that is either caught in
time, mitigated, or fortunately has no effect on the patient.
n
An accident or adverse event is a failure in some aspect of care that leads to injury.
n
Both incidents and accidents are typically judged according to their preventability, but
this is a fraught concept.
n
Negligent adverse events represent a subset of preventable adverse events that satisfy
legal criteria used in determining negligence (i.e., whether or not the care provided
failed to meet the standard of care reasonably expected of an average physician
qualified to take care of the patients in question).
3. Why don’t we use the term error anymore?
Error is a folk model for explaining performance. Errors are mental constructs that are
developed after-the-fact to explain outcomes. They are like optical illusions, simultaneously
convincing and misleading. If we could make health care safer but still committed errors,
we would be pleased, and if we eliminated errors but still had the same burden of adverse
events, we would not. The problem is not error; the problem is harm.

Chapter 7 SAFETY IN EMERGENCY MEDICINE 47
4. I’ve heard the term iatrogenic. Isn’t that when physicians make mistakes?
The term iatrogenic was originally used to describe “disorders induced in the patient by
autosuggestion based on the physician’s examination, manner, or discussion” but later gained
a broader definition as “the creation of additional problems or complications resulting from
treatment by a physician or surgeon” (Dorland’s Medical Dictionary, 25th edition, 1974).
Recently, it has come to be used in a more general sense to describe adverse outcomes that
result from a patient’s treatment within the health care system. A more appropriate term to
describe such error is comiogenic, proposed by Sharpe and Faden (1998). It has its origin in
the Greek root komein (to take care of), familiar to us in the term nosocomial, which describes
disease (Gr. nosos) that originates in the hospital. This new term has the advantage of
embracing the diverse sources of harm that can occur to patients in health care systems.
5. What’s the breakdown of safety problems in the ED?
We don’t really know because there haven’t been any systematic studies to date. Most of what
is known comes from incidental observations made in the major studies on hospitalized
patients who came through the ED, a few ED studies, and anecdotal observations. It appears
that the incident rate, especially of slips and lapses, is probably quite high, but that the
majority of these are corrected before they result in an adverse outcome. One thing appears
clear: the most costly and deadly problems generally result from mistakes associated with
delayed or missed diagnoses.
6. Am I likely to survive a career in emergency medicine without being involved
in a serious adverse event?
No. When you work in the jungle, you get bitten by snakes.
7. What’s the ratio of detected to undetected failures?
About 1:50
8. What proportion of adverse events is preventable?
About 70%
9. What are FPCs? Give examples in the ED.
An FPC is any factor or condition that increases the probability of failure in a given system.
There is no other area of medicine where this combination of FPCs exists so intensively. If you
hadn’t already realized it, your chosen career of emergency medicine is one of the most
difficult areas of medicine. Examples of FPCs are:
n
Diagnostic uncertainty.
n
High decision density.
n
High cognitive load.
n
Novel or infrequently occurring situations.
n
Time limitations for detection and correction of error.
n
Low signal-to-noise ratio.
n
Overcrowding/channel capacity overload (RACQITO).
n
Mismatch between real and perceived risk.
n
Poor feedback.
n
Poor quality of person-to-person information transfer.
n
Experience, training, and education limitations.
n
Disruption of circadian rhythms by shift-work.
n
Compromised task-pacing through interruptions or interventions.
n
High physical and emotional stress levels.
10. Most of these look self-evident, but what is meant by the low signal-to-noise
ratio FPC?
Signals are critical pieces of information that must not be missed. No signal is received in
isolation. All signals are accompanied by noise, which consists of distracting stimuli or pieces
of information that reduce the likelihood of detecting the signal. A low signal-to-noise ratio
