Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 13 ABDOMINAL PAIN88
5. What is the relationship of peritoneal inflammation to loss of appetite?
Anorexia, nausea, and vomiting are directly proportional to the severity and extent of
peritoneal irritation. The presence of appetite does not rule out a surgically significant
inflammatory process, such as appendicitis. A retrocecal appendicitis with limited peritoneal
irritation may be associated with minimal gastrointestinal (GI) upset, and one third of all
patients with acute appendicitis do not report anorexia on initial presentation.
6. Discuss the pitfalls in evaluating elderly patients with acute abdominal pain.
Advanced age may and often does blunt the manifestations of acute abdominal disease. Pain
may be less severe; fever often is less pronounced, and signs of peritoneal inflammation, such
as muscular guarding and rebound tenderness, may be diminished or absent. Elevation of the
white blood cell (WBC) count is also less sensitive. Cholecystitis, intestinal obstruction, and
appendicitis are the most common causes for acute surgical abdomen in the elderly. Because
of atypical clinical presentations, additional screening tests, such as amylase, liver function
studies, and alkaline phosphatase, and the liberal use of ultrasound or computed tomography
(CT) scan may be useful in this age group.
7. What other factors should be sought in the history that may alter significantly
the presentation of patients with abdominal pain?
Symptoms and physical findings in patients with schizophrenia and diabetes may be muted
significantly. The prior use of steroids or antibiotics may alter signs and laboratory results
substantially.
KEY POINTS: APPENDICITIS
1. The most sensitive findings are right lower quadrant tenderness, nausea, and anorexia.
2. Clinical scoring systems are useful for risk stratification but not for excluding the diagnosis.
3. Ultrasound, CT, and magnetic resonance imaging (MRI) are most useful in equivocal cases
or patient groups with multiple possible alternative diagnoses.
8. What is the significance of obstipation?
Obstipation is the inability to pass either stool or flatus for more than 8 hours despite a
perceived need, and is highly suggestive of intestinal obstruction.
9. What vital sign is associated most closely with the degree of peritonitis?
Tachycardia is virtually universal with advancing peritonitis. The initial pulse is less important
than serial observations. An unexplained rise in pulse may be an early clue that early surgical
exploration is indicated. However, this response may be blunted or absent in elderly patients.
10. Does the duration of abdominal pain help in categorizing cause?
Severe abdominal pain persisting for 6 or more hours is likely to be caused by surgically
correctable problems. Patients with pain of more than 48 hours’ duration have a significantly
lower incidence of surgical disease than do patients with pain of shorter duration.
11. Name the two most commonly missed surgical causes of abdominal pain.
Appendicitis and acute intestinal obstruction.
12. Is there a place for narcotic analgesics in the management of acute abdominal
pain of uncertain cause?
For fear of masking vital symptoms or physical findings, old, conventional surgical wisdom
proscribes the use of narcotic analgesics until a firm diagnosis is established. Increasingly,

Chapter 13 ABDOMINAL PAIN 89
however, studies have demonstrated that pain medication may be given to selected patients
with stable vital signs because the analgesic effect may be reversed readily at any time by the
administration of naloxone. In a review article, Ranji et al found that pain control with opiates
may alter the physical examination findings, but these changes result in no significant increase
in management errors. Although inconclusive, a growing body of data suggests that evaluation
of acute abdominal disease may be facilitated when severe pain has been controlled and the
patient can cooperate more fully.
13. Which are the most useful preliminary laboratory tests to order?
A complete blood count with differential and urinalysis are generally recommended. The
initial hematocrit helps to define antecedent anemia. An elevated WBC count suggests
significant pathology but is nonspecific. Elevated urinary specific gravity reflects
dehydration, and an increased urinary bilirubin in the absence of urobilinogen points
toward total obstruction of the common bile duct. Pyuria, hematuria, and a positive
dipstick for glucose and ketones may reveal nonsurgical causes for abdominal pain. For
patients with epigastric or right upper quadrant pain, lipase and liver function studies are
advised. Any woman with childbearing capability should receive a pregnancy test. Serum
electrolytes, glucose, blood urea nitrogen, and creatinine are indicated if there is clinical
dehydration or other reason to suspect abnormality such as renal failure, diabetes, or a
metabolic acidosis.
14. Are plain radiographs always indicated?
No. Plain films of the abdomen have the highest yield when used in the evaluation of patients
with suspected bowel obstruction, intussusception, ileus, and free air secondary to a
perforated viscus. They have much less utility in detecting intra-abdominal mass, renal calculi,
diverticulitis, gallbladder disease, and abdominal aortic aneurysms. If these disorders are
suspected, other studies such as ultrasound or abdominal CT are more appropriate.
Conversely, among patients with uncomplicated peptic ulcer disease or massive hematemesis,
pain present for more than 1 week, strangulated abdominal wall hernias, or other obvious
clinical indications for laparotomy, plain radiographs add little.
15. Which plain films are most useful?
Traditional teaching holds that plain abdominal films should include a supine view, plus either
an upright view or a left lateral decubitus view (if unable to stand).
The supine view of the abdomen is the most informative and worthwhile abdominal film.
The upright film is superior for visualizing air-fluid levels associated with ileus, obstruction, or
biliary air. The erect chest radiograph is most sensitive for detection of free intraperitoneal air
and may show basal pneumonia, ruptured esophagus, elevated hemidiaphragm, air-fluid levels
associated with subdiaphragmatic or hepatic abscess, pleural effusion, and pneumothorax. In
the evaluation of patients with abdominal pain, the upright chest film, taken alone, has been
shown to be more useful than films of the abdomen itself.
16. Are air-fluid levels within the intestine always abnormal?
No. It is commonly taught that air-fluid levels when seen on an upright abdominal film are
pathognomonic for small bowel obstruction. A study of 300 normal patients by Gammill
and Nice showed, however, that the average number of air-fluid levels was four per patient,
with some films showing 20. Although typically less than 2.5 cm in length, some were 10
cm. Most of the air-fluid levels were found in the large bowel; only 14 of 300 normal patients
studied showed air-fluid levels in the small bowel. The authors suggested that before air-fluid
levels are used as the sole criterion for the diagnosis of paralytic ileus or mechanical
obstruction, one should see more than two air-fluid levels within dilated loops of the small
bowel.

Chapter 13 ABDOMINAL PAIN90
17. A 7-year-old child presents with acute abdominal pain with a history of
several similar bouts over the past 5 months. Physical examination is
unremarkable. What is the most likely cause?
In children older than age 5, abdominal pain that is intermittent and of more than 3 months’
duration is functional in greater than 95% of cases, especially in the absence of objective
findings such as fever, delayed growth patterns, anemia, GI bleeding, or lateralizing pain and
tenderness.
KEY POINTS: COMMON DISEASES THAT CAN SIMULATE
ACUTE ABDOMEN
1. DKA
2. Food poisoning
3. Pneumonia
4. Pelvic inflammatory disease
WEBSITES
www.emedicine.medscape.com
Acute appendicitis: www.emedicine.medscape.com/article/773895-overview
18. A patient with severe abdominal pain is found to be in diabetic ketoacidosis
(DKA). How do I decide whether the abdominal pain is a manifestation of the
DKA or whether a surgical condition has precipitated DKA?
Patients with established DKA often present to the ED with severe abdominal pain. Although
the precise mechanism of abdominal pain and ileus in patients with DKA is not well
understood, hypovolemia, hypotension, and a total body potassium deficit probably
contribute. An acute surgical lesion may initiate DKA; nevertheless, most patients in DKA have
no such pathology. Abdominal symptoms characteristically resolve as medical treatment
restores the patient to biochemical homeostasis. Treatment of the DKA must precede any
surgical intervention because of the extremely high intraoperative mortality among patients
not so stabilized. If symptoms persist despite adequate correction of DKA, then an underlying
surgical pathology becomes more likely.
19. Is a rectal examination necessary in the patient with suspected acute
appendicitis?
The literature is inconsistent as to its usefulness in aiding the diagnosis; however, failure to
perform a rectal examination is cited frequently in successful malpractice claims. Some other
diseases may be effectively diagnosed only by rectal examination (e.g., prostatitis or occult GI
bleed).
20. Is there a reliable diagnostic test that will either rule in or rule out
appendicitis?
No, not yet anyway. Kentsis et al, have shown that high-accuracy mass spectrometry urine
proteome profiling allowed identification of diagnostic markers of acute appendicitis. These
biomarkers may add significantly to the diagnostic accuracy of appendicitis in the near future.
Chapter 13 ABDOMINAL PAIN 91
BIBLIOGRAPHY
1. American College of Emergency Physicians (ACEP): Clinical policy: critical issues for the initial evaluation and
management of patients presenting with a chief complaint of nontraumatic acute abdominal pain. Ann Emerg
Med 36:406–415, 2000.
2. Bickerstaff LK, Harris SC, Leggett RS, et al: Pain insensitivity in schizophrenic patients. Arch Surg 123:49–51,
1988.
3. Brewer RJ, Golden GT, Hitch DC, et al: Abdominal pain: An analysis of 1,000 consecutive cases in a university
hospital emergency room. Am J Surg 131:219–233, 1976.
4. Gammill SL, Nice CM: Air fluid levels: Their occurrence in normal patients and their role in the analysis of
ileus. Surgery 71:771–780, 1972.
5. Greene CS: Indications for plain radiography in the emergency department. Ann Emerg Med 15:257–260,
1986.
6. Jaffe BM, Berger DH: The appendix. In Brunicardi CF, Anderson DK, Billiar TR, et al, editors: Schwartz’s
principles of surgery, ed 8, New York, 2005, McGraw-Hill, pp 1119–1137.
7. Kentsis A, Lin YY, Kurek K, et al: Discovery and validation of urine markers of acute pediatric appendicitis
using high-accuracy mass spectrometry. Ann Emerg Med 55(1):62–70, 2010.
8. Markle GB: Heel-drop jarring test for appendicitis [letter]. Arch Surg 120:243, 1985.
9. McHale PM, LoVecchio F: Narcotic analgesia in the acute abdomen. A review of prospective trials.
Eur J Emerg Med 8:131–136, 2001.
10. Parker LJ, Vukov LF, Wollan PC: Emergency department evaluation of geriatric patients with acute
cholecystitis. Acad Emerg Med 4:51–55, 1997.
11. Ranji SR, Goldman LE, Simel DL, et al: Do opiates affect the clinical evaluation of patients with acute
abdominal pain? JAMA 296:1764–1774, 2006.
12. Rothrock SG, Green SM, Dobson M, et al: Misdiagnosis of appendicitis in nonpregnant women of childbearing
age. J Emerg Med 13:1–8, 1995.
13. Silen W, editor: Cope’s early diagnosis of the acute abdomen, ed 21, New York, 2005, Oxford University
Press.
14. Wagner JM, McKinney WP, Carpenter JL: Does this patient have appendicitis? JAMA 276:1589–1594, 1996.
92
NAUSEA AND VOMITING
CHAPTER 14
Juliana Karp, MD
1. Vomiting? Do I really need to read this chapter when there are so many
more interesting chapters in this book?
Yes! One of the most common and harmful mistakes made in the ED is assuming that
nausea and vomiting are the result of gastroenteritis without thinking of and ruling out
more serious causes. In addition, vomiting is one of the most common presenting
complaints in the ED.
2. What causes vomiting?
The act of vomiting is a highly complex act involving a vomiting center in the medulla.
This center may be excited in four ways:
n
Via vagal and sympathetic afferents from the peritoneum; gastrointestinal, biliary, and
genitourinary tracts; pelvic organs; heart; pharynx; head; and vestibular apparatus.
n
By impulses converging at the nucleus tractus solitarius in the medulla.
n
Via the chemoreceptor trigger zone located in the floor of the fourth ventricle.
n
Via the vestibular or vestibulocerebellar system (motion sickness and some
medication-induced emesis).
3. Can vomiting itself lead to potential complications?
Yes. Some of these are life-threatening:
n
Esophageal perforation or Mallory-Weiss tear
n
Severe dehydration
n
Metabolic alkalosis
n
Severe electrolyte depletion (particularly sodium, potassium, and chloride ions)
n
Pulmonary aspiration
n
Esophageal or gastric bleeding
4. List the common gastrointestinal disorders that cause vomiting.
n
Gastroenteritis
n
Gastric outlet obstruction
n
Gastric retention
n
Alcoholic gastritis
n
Pancreatitis
n
Hepatitis
n
Small bowel obstruction
n
Appendicitis
n
Cholecystitis
n
Diabetic gastroparesis
KEY POINTS: CHARACTERISTICS OF GASTROENTERITIS
1. True abdominal or pelvic tenderness is not usually present in gastroenteritis.
2. Gastroenteritis usually consists of both vomiting and diarrhea.
3. Gastroenteritis is usually a self-limited disorder, but IV rehydration and electrolyte
replacement may be necessary.
Chapter 14 NAUSEA AND VOMITING 93
5. Are there different gastrointestinal causes of vomiting in children?
Yes, particularly during the first year of life. These include gastrointestinal atresia, malrotation,
volvulus, Hirschsprung’s disease, gastroesophageal reflux, pyloric stenosis, intussusception,
and inguinal hernia. (Vomiting in children presents considerations not covered in this chapter.
See Chapter 63.)
6. List the common causes of vomiting other than gastrointestinal disorders.
n
Infections
n
Pneumonia
n
Meningitis
n
Sepsis
n
Metabolic disturbances (e.g., diabetic ketoacidosis, uremia, or hypercalcemia)
n
Toxicologic (e.g., digoxin, theophylline, aspirin, or iron)
n
Cancer chemotherapy
n
Neurologic (e.g., hydrocephalus, cerebral edema, or migraine headache)
n
Renal calculi
n
Ovarian or testicular torsion
n
Pregnancy
n
Ruptured ectopic pregnancy
n
Labyrinthine disorders
n
Myocardial ischemia
n
Psychiatric
7. Can the character of the vomit help you to make a diagnosis?
Sometimes, especially with gastrointestinal disorders. In acute gastritis, vomit is usually
stomach contents mixed with a little bile. In biliary or ureteral colic, the vomit is usually
bilious. In sympathetic shock (acute torsion of abdominal or pelvic organ), it is common for
the patient to retch frequently but vomit only a little. In intestinal obstruction, the character of
vomit varies—first gastric contents, then bilious material, with progression to brown feculent
material that is pathognomonic of distal small or large bowel obstruction. Vomiting of blood is
a whole different story (see Chapter 33).
8. What else do I need to ask the patient?
n
Associated signs and symptoms, such as pain, fever, jaundice, and bowel habits. Think of
hepatitis or biliary obstruction with jaundice. Always remember that gastroenteritis is
uncommon without diarrhea.
n
Relationship of vomiting to meals. Vomiting that occurs soon after a meal is common
with gastric outlet obstruction from peptic ulcer disease. Vomiting after a fatty meal is
common with cholecystitis. Vomiting of food eaten more than 6 hours earlier is seen with
gastric retention.
n
Do not always focus on the gastrointestinal system. Ask about medications and possible
drug use, headache and other neurologic symptoms, and last menstrual period and
possibility of pregnancy. Inquire about cardiac risk factors, especially in older patients.
9. What do I look for on the physical examination?
Physical examination is helpful but can be unreliable. Look for signs of dehydration,
particularly in children. Check for bowel sounds, which are increased in gastroenteritis and
absent with obstruction or serious abdominal infections. Abdominal tenderness may be
present in a variety of disorders, but a rigid abdomen points to peritonitis, a surgical
emergency. Women of childbearing age with vomiting and abdominal or pelvic pain require a
pelvic examination and pregnancy test. Always remember the neurologic examination if there
are any associated neurologic symptoms, such as headache or vertigo.
Chapter 14 NAUSEA AND VOMITING94
10. Are laboratory tests indicated?
This question must be answered on an individual basis. In general, tests should be ordered
based on the history and physical examination. Diabetics and elderly patients can hide serious
infections and metabolic disturbances. Be careful with these patients.
11. When should I order radiographs?
This must be judged on an individual basis. Abdominal radiography is usually nonspecific but
may show free air with perforation of an abdominal viscus or dilated bowel with obstruction.
A chest film can be useful in cases of protracted vomiting to rule out aspiration or
pneumomediastinum. Lobar pneumonia with diaphragmatic irritation may cause vomiting with
abdominal pain and few respiratory symptoms.
KEY POINTS: DIAGNOSIS OF THE VOMITING PATIENT
1. Always consider etiologies other than gastrointestinal disorders.
2. Take a thorough history, especially in the young and elderly.
3. Always consider accidental ingestions in children and medication side effects or
toxicities in adults.
4. Laboratory testing and radiographs are seldom useful in gastroenteritis but may be
helpful to identify other causes of vomiting.
12. How should I treat the vomiting patient?
a. Always remember to protect the airway. Patients with altered mental status should be
placed on their side to prevent aspiration. Intubate early when necessary.
b. Intravenous (IV) fluids usually are indicated for rehydration; normal saline or lactated
Ringer solution is preferred.
c. Nasogastric suction can be therapeutic and diagnostic and is always indicated when there
is a suspicion of a gastrointestinal bleed or small bowel obstruction.
d. Medications to relieve nausea and vomiting must be used judiciously, especially in patients
with altered mental status, hypotension, or uncertain diagnosis.
e. Determine and, if possible, treat the underlying cause.
13. What medications should I use?
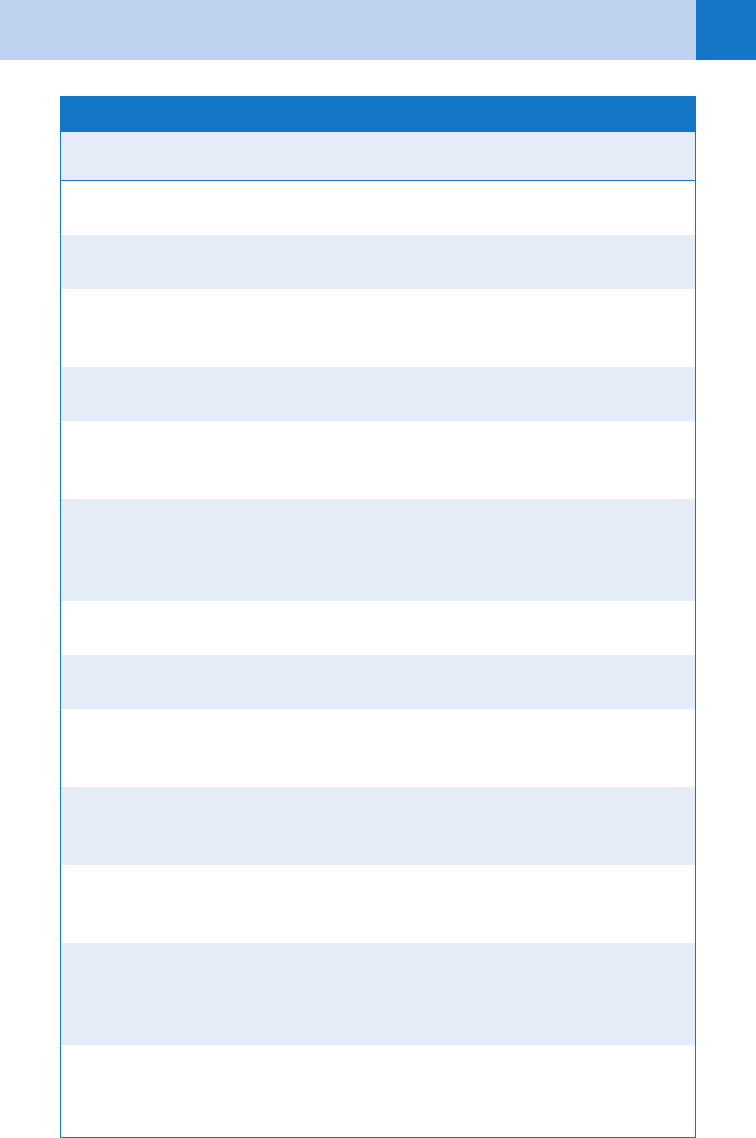
See Table 14-1.
WEBSITES
www.fda.gov/safety/medwatch
Chapter 14 NAUSEA AND VOMITING 95
Generic Name
Trade
Name Indication Dose
Palonosetron Aloxi Vomiting with
chemotherapy
0.25 mg IV prior to
chemotherapy
Meclizine Antivert Vertigo and motion
sickness
25 mg PO qid
Dolasetron
mesylate
Anzemet Vomiting associated with
anesthesia or
chemotherapy
12.5–100 mg PO or IV
single dose
Hydroxyzine Atarax Nausea, vomiting, anxiety 25–100 mg PO or IM tid
or qid
Diphenhydramine
Nabilone
Benadryl
Cesamet
Motion sickness
Nausea and vomiting with
chemotherapy
25–50 mg PO or IV qid
1–2 mg PO bid
Prochlorperazine
Dimenhydrinate
Compazine
Dramamine
Nausea, vomiting, anxiety
Nausea, motion sickness
10 mg PO, IM, or IV qid,
25 mg PR bid
50–100mg PO, IM,
or IV qid
Aprepitant Emend Nausea and vomiting,
with chemotherapy
125 mg PO on day 1, 80
mg PO on days 2 and 3
Phosphorated
carbohydrate
Emetrol Nausea and vomiting, 1–2 tbs PO every 15 min
(not to exceed 5 doses)
Droperidol Inapsine Nausea and vomiting 0.625–2.5 mg IV or 2.5 IM
(black box warning: QT
prolongation)
Granisetron Kytril Nausea and vomiting with
chemotherapy
10 mg/kg IV or 1 mg PO
bid (only on day of
chemotherapy)
Dronabinol Marinol Refractory nausea and
vomiting with
chemotherapy
5 mg PO tid or qid
Promethazine Phenergan Nausea, vomiting, motion
sickness, anxiety
12.5–50 mg PO, PR, or IV
qid (black box warning:
children younger than
2 years old)
Metoclopramide Reglan Nausea, vomiting, gastro-
esophageal reflux,
gastroparesis
5–10 mg PO or IV dosage
varies (box warning,
tardive dyskinesia)
TABLE 14-1. ANTIEMETIC MEDICATIONS
Continued
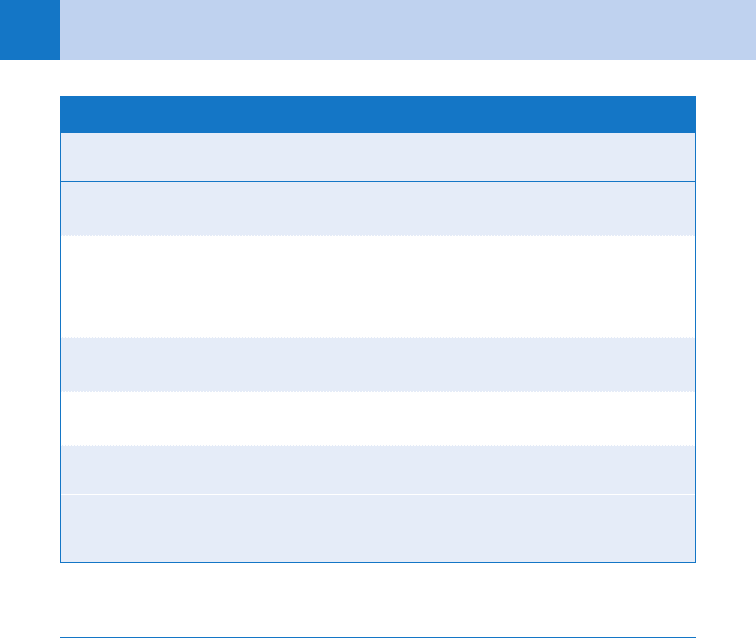
Chapter 14 NAUSEA AND VOMITING96
Generic Name
Trade
Name Indication Dose
Chlorpromazine Thorazine Nausea, vomiting, anxiety 10–25 mg PO qid, 25 mg
IM, or qid 100 mg PR qid
Trimethobenzamide
Thiethylperazine
Torecan
Tigan
Nausea and vomiting
Nausea and vomiting
250 mg PO tid or qid , 200
mg PR tid or qid , 200 mg
IM tid or qid
Dosage varies
Scopolamine Transderm
Scop
Nausea, vomiting, motion
sickness
1 patch every 3 days
Hydroxyzine
pamoate
Vistaril Nausea, vomiting, anxiety 25–100 mg PO or IM tid
or qid
Ondansetron Zofran Nausea and vomiting 4 mg IV or IM
TABLE 14-1. ANTIEMETIC MEDICATIONS—cont’d
bid, twice a day; IM, intramuscularly; IV, intravenously; PO, per os (by mouth); PR, per rectum; qid, four times
a day; tid, three times a day.
BIBLIOGRAPHY
1. Ernst A: Prochlorperazine versus promethazine for uncomplicated nausea and vomiting in the emergency
department: a randomized, double-blind clinical trial. Ann Emerg Med 36:89–94, 2000.
2. Wolfson, AB, Hendey, GW, Hendry PL, et al, editors: Harwood-Nuss’ clinical practice of emergency medicine,
ed. 4, Philadelphia, 2005, Lippincott Williams & Wilkins.
3. Marx JA, Hockberger RS, Walls RM, editors: Rosen’s emergency medicine: concepts and clinical practice, ed 7,
St. Louis, 2010, Mosby.
4. Silen W, editor: Cope’s early diagnosis of the acute abdomen, ed 21, New York, 2005, Oxford University Press.
97
CHAPTER 15
HEADACHE
Jonathan A. Edlow, MD, FACEP
1. How common are headaches and what percentage of ED patients have
headache as a chief complaint?
Nearly everyone has a headache at some point in their lives; migraine headache is found
in about 12% of the general population. Most patients do not seek medical care,
certainly not in the ED. Overall, approximately 2% of all ED visits are for headaches.
Of those who come to the ED with headache, only about 5% will have a serious cause.
2. When someone has a headache, what exactly is it that hurts?
The brain, the pia and arachnoid mater, the skull, and the choroid plexus are not the
source of headache pain. The structures in the head that are pain sensitive include the
scalp; skin; vessels; scalp muscles; parts of the dura mater; dural arteries; intracerebral
arteries; cranial nerves V, VI, and VII; and the cervical nerves. Irritation, inflammation,
distention, or traction of any of these may result in a headache.
3. Name the most common headaches for which patients seek treatment.
Muscle contraction (tension) and vascular (migraine) headaches are by far the most
common, even in an acuity-skewed ED population. These are often referred to as
primary headache disorders. Although painful, these disorders do not have life-
threatening sequelae. There are a number of cannot miss causes of headache that,
although less common, are crucial for emergency physicians to diagnose correctly.
4. What causes of headache are cannot miss?
True emergencies, or cannot miss causes of headaches, are conditions that threaten life, limb,
brain, or eye and treatable (see Table 15-1). Headaches that are true emergencies include:
n
Intracranial bleeding (subarachnoid hemorrhage; SAH)
n
Subdural or epidural hematoma
n
Intraparenchymal hemorrhage
n
Ischemic cerebrovascular accident (CVA)
n
Dissection of a carotid or vertebral artery
n
Hypertensive encephalopathy
n
Brain tumor
n
Giant cell arteritis (temporal arteritis) and other vasculitides
n
Central nervous system infections (meningitis and abscess)
n
Pseudotumor cerebri
n
Cerebral venous sinus thrombosis
n
Narrow angle glaucoma
n
Spontaneous intracranial hypotension
5. What are some clinical clues to distinguish primary headaches from
cannot miss headaches?
By definition, tension and migraine headaches are recurrent episodes; these episodes
are usually similar to one another in any one individual patient. Therefore, any first
severe headache can never be definitively diagnosed as tension or migraine. A headache
that is described as a first or worst headache, or even substantially different from prior
