Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 17 SEIZURES118
A transiently (,1 hour) raised anion gap is good evidence that a grand mal seizure has
occurred. This is determined by blood samples drawn as close to the time of seizure as
possible. Field blood samples are ideal for this study. If there is no anion gap acidosis, one
may presume that the patient did not have a major motor seizure.
KEY POINTS: ANCILLARY LABORATORY TESTING IN PATIENTS
WITH SEIZURES
1. Usually not indicated for patients with recurrent seizures unchanged from prior episodes.
2. Should be limited to those tests designed to find underlying causes of seizures.
3. Include blood chemistries (i.e., sodium, calcium, magnesium), blood sugar, appropriate drug
screen, kidney function, and liver function.
11. And if the patient does not have a history of seizures?
Routine screening laboratory tests in a patient with new onset seizure who has returned to
baseline have low yield. In general, it is recommended that these patients have a blood sugar
and blood sodium determination. If the patient is a woman of child-bearing years, a pregnancy
test can be useful because it may affect choice of antiepileptic therapy and/or disposition.
The routine use of lumbar puncture in new onset seizure patients is not supported by the
literature. Additional testing (i.e., calcium, magnesium, drug screening, and kidney and liver
function testing) should be obtained if clinically indicated.
12. What about imaging studies?
In the patient with a first-time seizure, emergent noncontrast head CT is recommended for
patients in whom a structural lesion is suspected. This includes patients with new focal
deficits, persistent altered mental status, fever, recent head trauma, persistent headache,
history of cancer, or presence of a coagulopathy or platelet disorder; patients who are on
anticoagulation therapy; and patients who are HIV positive or otherwise immunosuppressed.
Emergent neuroimaging should also be considered in the patient with first-time seizure who is
older than 40 years or who has a partial seizure.
13. What should be the disposition of the patient who presents with a seizure?
Patients who present with any of the following should be considered for emergent admission
to the hospital for inpatient evaluation and therapy: persistent altered mental status, CNS
infection, new focal abnormality, new intracranial lesion, underlying correctable medical
problem (e.g., significant hypoxia, hypoglycemia, hyponatremia, dysrhythmia, and significant
alcohol withdrawal), acute head trauma, status epilepticus, and eclampsia. If the patient has a
history of seizure and has a simple seizure and a subtherapeutic anticonvulsant level, then this
should be addressed prior to discharge.
Patients with new onset seizures who have normal work-ups in the ED and are medically
stable may be considered for discharge. In this case, follow up with the patient’s primary care
physician or a consulting neurologist must be arranged. The patient should be informed via
ED discharge instructions on the possibility of another seizure and be advised to avoid
working with hazardous machines, driving an automobile, and doing any other activities that
can result in serious injury if the patient has another seizure. Also, most states have laws that
require reporting a patient with seizures, if the patient has a driver’s license.
Chapter 17 SEIZURES 119
KEY POINTS: EMERGENT NEUROIMAGING RECOMMENDATIONS
FOR PATIENTS WITH SEIZURES
1. Seizure with focal neurological deficits, persistent altered mental status, fever, recent trauma,
persistent headache, history of cancer, history of anticoagulation, HIV positive (AIDS), and
when timely follow-up cannot be ensured.
2. Urgent imaging for patients who have completely recovered from their seizure and for whom
no clear-cut cause has been identified to help identify a possible structural cause.
3. Patients with first-time seizures who are older than 40 years or have partial onset seizure.
4. Patients with prior history of seizures who have a new or different seizure pattern.
WEBSITES
American College of Emergency Physicians: http://www.acep.org
BIBLIOGRAPHY
1. Duvivier E, Pollack C: Seizures. In Marx JA, Hockberger RS, Walls RM, et al, editors: Rosen’s emergency
medicine: concepts and clinical practice, ed 7, New York, 2009, Mosby.
2. Lowenstein DH, Aldredge BK: Status epilepticus. N Engl J Med 338:970, 1998.
3. Millikan D, Rice B, Silbergleit R: Emergency treatment of status epilepticus: current thinking. Emerg Med Clin
North Am 27:101–110, 2009.
4. Schachter SC: Seizure disorders. Med Clin North Am 93(2) 343–351, 2009.
5. St. Louis EK, Granner MA: Seizures and epilepsy in adolescents and adults. In Rakel RE, Bope ET: Conn’s
Current Therapy 2009, Philadelphia, 2008, Saunders.
6. Trescher WH, Lesser RP: The epilepsies. In Bradley WG, Daroff RB, Fenichel GM, et al, editors: Neurology in
clinical practice, ed 5, Philadelphia, 2008, Butterworth Heinemann.
14. Should I start the patient with a new seizure on antiepileptic medication prior
to discharge?
This decision is best made in consultation with the patient’s primary care physician or neurologist.
Most patients with a single new onset seizure who can be discharged do not need to be started
on anticonvulsants until seen in follow-up and further testing (i.e., electroencephalogram [EEG])
is completed.
15. What is a pseudoseizure?
Pseudoseizures are functional events that may mimic seizures in their motor activity or
behavior. They are not caused by abnormal electrical discharges in the brain. In general, patients
with pseudoseizures have underlying anxiety or hysterical/histrionic personality disorders.
Pseudoseizures are sometimes difficult to diagnose in the ED. Some maneuvers that may be
of benefit include suggesting to the patient that the seizure will stop soon or attempting to
distract the patient with loud noises or bright lights during the seizure activity. Patients who
show asynchronous extremity movements, forward thrusting movement of the pelvis, and eyes
deviated toward the ground no matter what the head position are more likely to be having
pseudoseizures. Simultaneous video and EEG monitoring can help to differentiate true seizures from
pseudoseizures. In addition, a serum prolactin level drawn within 20 minutes of seizure activity
should be elevated in the patient with true seizure. A normal anion gap on serum electrolytes drawn
immediately after the grand mal seizure supports the diagnosis of a pseudoseizure.
120
CHAPTER 18
ANAPHYLAXIS
Vincent J. Markovchick, MD, FAAEM, FACEP,
and Nadia S. Markovchick, MD
1. What is anaphylaxis?
A serious allergic reaction that is immunoglobulin E (IgE) mediated, rapid in onset, and
may cause death after exposure to an allergen in a previously sensitized individual within
minutes to hours of allergen exposure. The three diagnostic criteria include skin and
mucosal edema, respiratory compromise, and hypotension and/or gastrointestinal
symptoms.
2. What is an anaphylactoid reaction?
A potentially fatal syndrome clinically similar to anaphylaxis, which is not an IgE-mediated
response and may follow a single first-time exposure to certain agents, such as radiopaque
contrast media, salicylates, and opioids.
3. Name the most common causes of anaphylaxis.
Ingestion, inhalation, or parenteral injection of antigens that sensitize predisposed
individuals. Common antigens include:
n
Drugs (e.g., penicillin)
n
Foods (e.g., shellfish, nuts, or egg whites)
n
Insect stings (hymenoptera) and bites (snakes)
n
Diagnostic agents (ionic contrast media)
n
Physical and environmental agents (e.g., latex, exercise, and cold)
Idiopathic anaphylaxis is a diagnosis of exclusion that is made when no identifiable
cause can be determined.
4. How do I make the diagnosis clinically?
Involvement of at least two of the following must be present:
n
Cutaneous manifestations (e.g., urticaria or rash)
n
Mucous membranes (angioedema)
n
Upper respiratory tract (e.g., edema and hypersecretions)
n
Lower respiratory tract (bronchoconstriction)
n
Gastrointestinal symptoms (e.g., nausea, vomiting, or abdominal cramping)
n
Cardiovascular system (vasodilation and cardiovascular collapse)
5. What are the most common signs and symptoms?
The clinical presentation ranges from mild to life-threatening. Mild manifestations that
occur in most people include urticaria and dermal angioedema. Life-threatening
manifestations involve the respiratory and cardiovascular systems. Respiratory signs
and symptoms include acute upper airway obstruction presenting with stridor or lower
airway manifestations of bronchospasm with diffuse wheezing. Cardiovascular collapse
presents in the form of syncope, hypotension, tachycardia, and dysrhythmias.
6. What is the role of diagnostic studies?
There is no immediate role for diagnostic studies in the ED because diagnosis and
treatment are based solely on presenting clinical signs and symptoms. However, if there
is a question about the diagnosis, serum tryptase and plasma and urine histamine levels
Chapter 18 ANAPHYLAXIS 121
are elevated for up to 6 hours after an allergic reaction and can be measured in the ED if there
is a question about the diagnosis. There is a role for skin testing either before administration
of an antigen or in follow-up referral to determine the exact allergens involved.
7. What is the differential diagnosis?
Hereditary angioedema, septic and cardiogenic shock, asthma, croup and epiglottitis,
vasovagal syncope, and any acute cardiovascular or respiratory collapse of unclear origin.
8. What is the most common form of anaphylaxis, and how is it treated?
Urticaria, either simple or confluent, is the most benign and the most common clinical
manifestation. This is thought to be due to a capillary leak mediated by histamine release.
It may be treated by the administration of antihistamines (i.e., orally, intramuscularly, or
intravenously) or epinephrine (i.e., subcutaneously or intramuscularly).
9. What is hereditary angioedema? How is it related to anaphylaxis?
Angioedema is edema of subcutaneous tissue, most often involving the face, tongue, lips
larynx, gastrointestinal tract and, in men, the genitals. When angioedema occurs with
urticaria, it is likely an allergic reaction. If angioedema occurs without urticaria, it may be
hereditary angioedema.
10. How does the treatment of hereditary angioedema differ from that of
anaphylaxis?
Hereditary angioedema is a genetic condition, usually presenting first in adolescence,
involving a deficiency or absence of C1 esterase inhibitors. In adults, the condition can
present as an acquired C1 esterase deficiency; angiotensin-converting enzyme (ACE) inhibitors
have been implicated as a trigger. Regardless of the cause, it is not IgE mediated;
antihistamines and steroids are not as effective as in anaphylaxis. Because the initial diagnosis
of C1 esterase deficiency is often unknown at the time of ED presentation, treat as an allergic
reaction. If there is minimal or no response to therapy, consider intravenous (IV) fresh frozen
plasma (which contains C1 esterase inhibitor) or C1 esterase inhibitor concentrate.
11. Summarize the initial treatment for life-threatening forms of anaphylaxis.
a. Upper airway obstruction with stridor and edema is treated with high-flow nebulized
oxygen, racemic epinephrine, and IV epinephrine. If airway obstruction is severe or
increases, perform endotracheal intubation or cricothyroidotomy.
b. Acute bronchospasm is treated with epinephrine. Mild-to-moderate wheezing in patients
with normal blood pressure may be treated with 0.01 mg/kg of 1:1000 epinephrine
administered intramuscularly. If the patient is in severe respiratory distress or has a silent
chest, administer IV epinephrine via a drip infusion: 1 mg of epinephrine in 250 mL of D
5
W
at an initial rate of 1 mg/min with titration to desired effect. Bronchospasm refractory to
epinephrine may respond to a nebulized b-agonist, such as albuterol sulfate or
metaproterenol.
c. Cardiovascular collapse presenting with hypotension is treated with a constant infusion of
epinephrine, titrating the rate to attain a systolic blood pressure of 100 mm Hg or mean
arterial pressure of 80 mm Hg.
d. For patients in full cardiac arrest, administer 1:10,000 epinephrine, 1 mg slow IV push or
via endotracheal tube. Immediate endotracheal intubation or cricothyroidotomy should be
performed.
Chapter 18 ANAPHYLAXIS122
12. What are the adjuncts to initial epinephrine and airway management?
If intubation is unsuccessful and cricothyroidotomy is contraindicated, percutaneous
transtracheal jet ventilation via needle cricothyroidotomy should be considered, especially in
small children. IV diphenhydramine (1 mg/kg up to 50 mg) should be given to all patients.
Simultaneous administration of an H
2
blocker, such as cimetidine, 300 mg intravenously, may
be helpful. Aerosolized bronchodilators, such as metaproterenol, are useful if bronchospasm
is present. For refractory hypotension, pressors, such as norepinephrine or dopamine, may be
administered. Glucagon, 1 mg intravenously every 5 minutes, may be helpful in epinephrine-
resistant patients who are on long-term b-adrenergic blocking agents, such as propranolol.
Corticosteroids have limited benefit because of the delayed (4–6 hours) onset of action, but
may be beneficial in patients with prolonged bronchospasm or hypotension.
13. What are the complications of bolus IV epinephrine administration?
When epinephrine 1:10,000 is administered via IV push in patients who have an obtainable
blood pressure or pulse, there is significant potential for overtreatment and the potentiation of
hypertension, tachycardia, ischemic chest pain, acute myocardial infarction, and ventricular
dysrhythmias. Extreme care must be exercised in elderly patients and in patients with
underlying coronary artery disease. It is much safer to give IV epinephrine by a controlled
titratable drip infusion with continuous monitoring of cardiac rhythm and blood pressure.
14. What is biphasic anaphylaxis? How common is it?
A recurrence of the symptoms of anaphylaxis after the initial symptoms resolve. This may
occur anywhere from several hours to as long as 72 hours. This may be caused by
persistence of the allergen or immune mediators relative to the duration of the therapy.
The reported incidence is between 1% and 23% of all anaphylactic reactions. Some risk
factors that may make biphasic anaphylaxis more likely are:
n
A history of biphasic anaphylaxis
n
Delays in onset of initial symptoms, in initial treatment, or in resolution of symptoms with
proper therapy
n
Severe reactions involving hypotension or laryngeal edema
n
Patients taking b-blockers
15. Is there a role for prophylactic treatment in anaphylaxis? How is this
performed?
When the potential benefits of treatment or diagnosis outweigh the risks (e.g., administration
of an antivenom for life-threatening or limb-threatening snake bites), informed consent should
be obtained if the patient is competent. Pretreat with IV diphenhydramine (Benadryl) and
corticosteroids and prepare an IV epinephrine infusion drip. The patient should be in an
intensive care unit (ICU) setting with continuous monitoring of blood pressure, cardiac
rhythm, and oxygen saturation; have full intubation and cricothyroidotomy equipment at the
bedside. Under the supervision of a physician capable of immediately administering IV
epinephrine and managing the airway, administration of the antigen (e.g., the antivenom)
should be started. Nonionic contrast medium for diagnostic imaging studies should be given
to patients with a history of anaphylaxis to ionic contrast material.
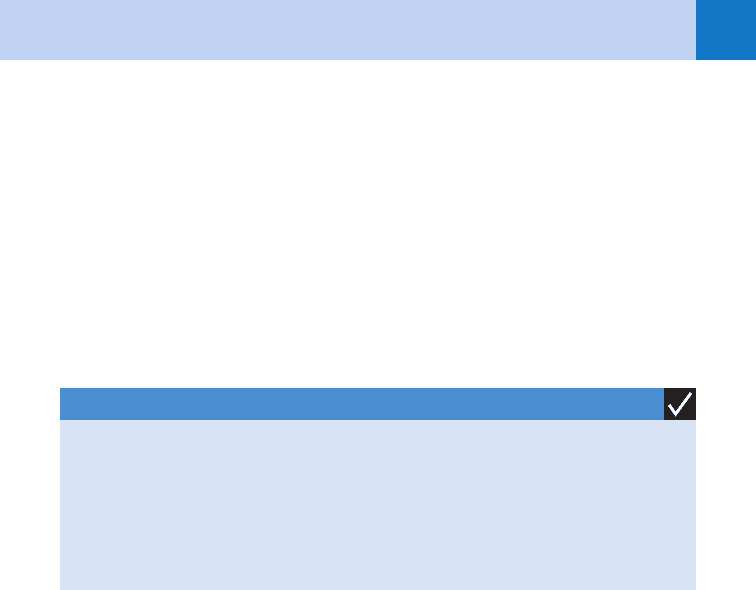
KEY POINTS: ANAPHYLAXIS
1. Life-threatening target organs are the upper airway mucosa, bronchiole smooth muscle,
and the cardiovascular system.
2. Hypotension is the indication for IV epinephrine.
3. Administer IV epinephrine as a drip, not as a bolus, in the noncardiac arrest situation.
Chapter 18 ANAPHYLAXIS 123
16. What about steroids?
Because corticosteroids have an onset of action of approximately 4 to 6 hours after
administration, they have limited to no benefit in the initial acute treatment of anaphylaxis.
The administration of hydrocortisone (250–1,000 mg intravenously) or methylprednisolone
(125–250 mg intravenously), followed by a tapering dose over 7 to 10 days, is an acceptable
regimen after the resolution of the initial anaphylactic episode.
17. What is the disposition of a patient who initially responds to aggressive
treatment?
Although most patients become asymptomatic after early, aggressive treatment, all patients
with true anaphylactic reactions should be admitted to either an ED or hospital observation
unit for 2 to 4 hours minimum. Patients who rebound or continue to have life-threatening
symptoms (e.g., bronchospasm, hypotension, or upper airway obstruction) should be
admitted.
18. What follow-up instructions are given to patients treated for anaphylaxis?
Patients who have had a moderate-to-severe anaphylactic reaction (anything other than
isolated urticaria) should be prescribed and educated in the self-administration of epinephrine
into the muscles of the thigh with an autoinjector at the first sign of anaphylactic symptoms.
Self-administration of oral diphenhydramine is indicated to treat mild reactions, such as
urticaria or concomitant with the administration of epinephrine.
19. Is there an advantage of intramuscular (IM) over a subcutaneous epinephrine
injection?
Yes, if injected into the thigh. A recent study has demonstrated higher peak plasma levels
when epinephrine is injected into the muscles of the lateral thigh over subcutaneous or deltoid
muscle injections.
BIBLIOGRAPHY
1. Cuniowski PA, Hunter CJ: Would you recognize this patient’s biphasic anaphylaxis? Emerg Med 41(1):30–34,
2009.
2. Horak A, Raine R, Opie LH, et al: Severe myocardial ischemia induced by intravenous adrenaline. BMJ
286:519, 1983.
3. Peavy R, Metcalfe D: Understanding the mechanisms of anaphylaxis. Curr Opin Allergy Clin Immunol 8(4):
310–314, 2008.
4. Runge JW, Martinez JC, Cavuti EM: Histamine antagonists in the treatment of acute allergic reactions. Ann
Emerg Med 21:237–242, 1992.
5. Salzberg P, Singer E: Anaphylaxis, when seconds count. Emerg Med, May 2007. 18–24.
6. Simons FER, Gu X, Simons KJ: Epinephrine absorption in adults: intramuscular versus subcutaneous
injection. J Allergy Clin Immuno 108(5):871–873, 2001.
7. Smit DeV, Cameron PA, Rainer TH: Anaphylaxis presentations to an emergency department in Hong Kong:
incidence and predictors of biphasic reactions. J Emerg Med 28:381–388, 2005.
8. Tran PT, Muelleman RL: Allergies, allergic disease and anaphylaxis. In Adams JG, Barton E, Collings J, et al:
Emergency medicine, Philadelphia, 2008, Saunders, pp 1142–1147.
9. Tran, PT, Muellman RL: Allergy, hypersensitivity and anaphylaxis. In Marx JA, Hockberger RS, Walls RM,
et al: Rosen’s emergency medicine: concepts and clinical practice, ed 7, Philadelphia, 2010, Mosby,
pp 1511–1528.
10. Volcheck GW, Li JT: Exercise-induced urticaria and anaphylaxis. Mayo Clin Proc 72:140–147, 1997.
124
CHAPTER 19
LOW BACK PAIN
Kevin Andruss, MD, and Robert Hockberger, MD
1. Can I skip this chapter?
Not if you anticipate a career that involves caring for adults. Low back pain (LBP) is the
second most common cause of physician visits, following upper respiratory symptoms.
Approximately 70% to 85% of all people experience LBP during their lives. It is the most
common cause of activity limitation in people younger than 45 years and the third most
common cause in people older than 45 (after heart disease and arthritis). The cost of
diagnosis, treatment, disability, lost productivity, and litigation due to LBP exceeds
$50 billion annually, making it the third most expensive medical disorder in the
United States, after heart disease and cancer.
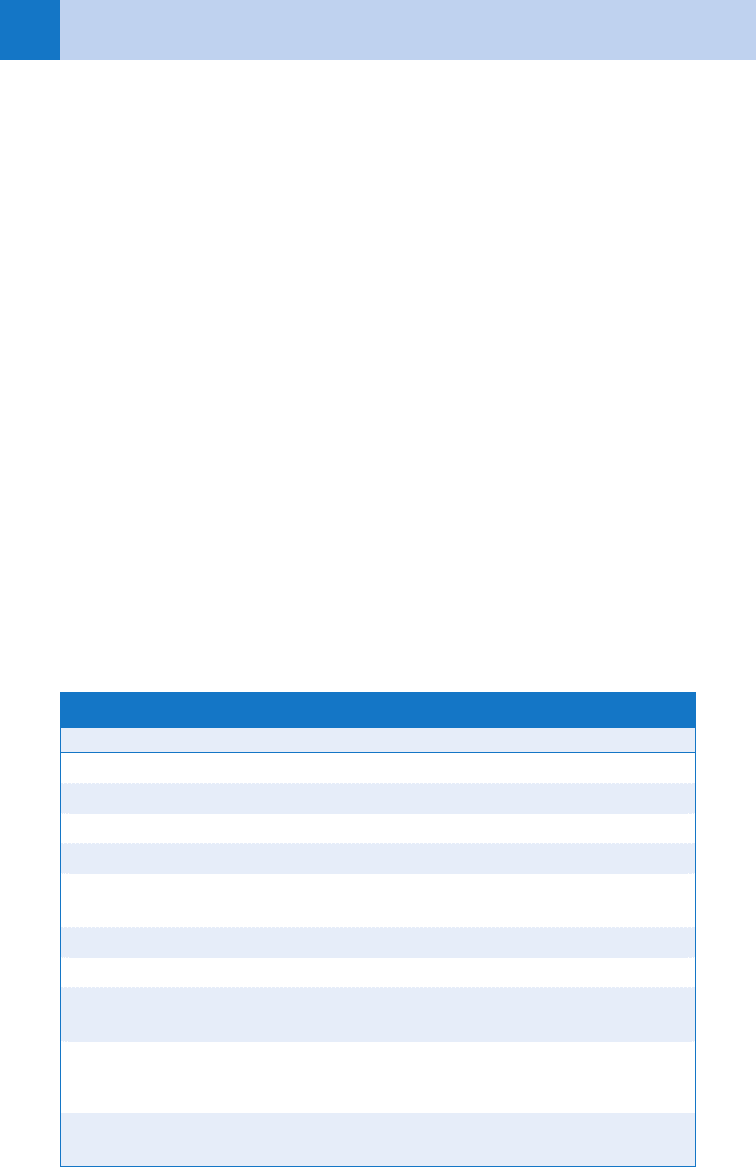
2. What are the causes of LBP?
Roughly 97% of LBP cases are caused by mechanical spine disorders. Only 3% of cases
are caused by nonmechanical spine disorders (especially spinal malignancy and
infection) or visceral disease (particularly abdominal aortic aneurysm); however, these
are medically significant causes of LBP that should not be missed. (See Table 19-1.)
3. What should I ask when taking the patient’s history?
The goal of the history is to distinguish medically significant causes of LBP from the
much more common mechanical spine disorders.
n
Spinal infection should be suspected in children, immunocompromised patients, and
intravenous drug users who present with localized spinal tenderness and fever
(although only 50% of patients will have fever at the time of presentation).
n
Spinal malignancy should be suspected in patients with a history of cancer or recent
weight loss and in patients older than 50 years with progressive LBP lasting more
than 1 month.
n
Occult spinal fracture should be suspected in the elderly and in patients with known
malignancy or osteoporosis (from steroid use or inactivity) who present with LBP of
unclear cause.
n
Visceral causes of LBP are usually distinguished by associated signs and symptoms.
4. How should I focus my physical examination?
All patients with LBP should get a complete neurologic examination, focusing on lower
extremity strength, sensation, and reflexes (see Table 19-2). Mechanical spine disorders,
with the exception of herniated lumbar disks or severe spondylolisthesis, should not
compromise neurologic function.
n
Rectal tone and sensation should be assessed if there is any concern for cord
compression or sacral lesions. Localized spinal tenderness is suggestive of fracture,
infection, or malignancy.
n
A straight leg raise (SLR) test should be performed in patients with leg symptoms
(see Question 6).
n
An abdominal examination is important to assess for visceral disease including an
abdominal aortic aneurysm.

Chapter 19 LOW BACK PAIN 125
5. What does it mean when a patient with LBP also has leg pain?
Patients with LBP and leg pain (termed sciatica) may have one of two syndromes.
n
Referred pain is caused by inflammation of the sciatic nerve. It is usually dull and poorly
localized, does not radiate distal to the knee, and is not associated with a positive SLR test
or neurologic impairment.
n
Radicular pain is usually caused by nerve root impingement from a herniated lumbar disk
or the narrowing of a vertebral foramen from spinal stenosis, but it may also occur with
epidural metastases or abscesses in high-risk patients. It is sharp and well localized,
frequently (but not always) radiates distal to the knee, invariably is associated with a
positive SLR test, and may be associated with neurologic impairment.
TABLE 19-1. DIFFERENTIAL DIAGNOSIS OF LOW BACK PAIN
Mechanical Spine
Disorders
Nonmechanical
Spine Disorders
Visceral
Disease
Lumbar strain Malignancy Abdominal aortic
Degenerative disk/facet disease Multiple myeloma Aneurysm
Metastatic cancer Pelvic organs
Herniated disk Spinal column or
cord cancer
PID
Spinal stenosis Lymphoma Prostatitis
Spondylolysis Infection Renal disease
Spondylolisthesis Septic discitis Pyelonephritis
Congenital spinal disease Osteomyelitis Nephrolithiasis
Traumatic fracture Epidural abscess Gastrointestinal disorders
Osteoporotic compression fracture Shingles Pancreatitis
Inflammatory arthritis Penetrating ulcer
Cholecystitis
PID, pelvic inflammatory disease.
TABLE 19-2. CLINICAL FEATURES OF LUMBAR DISK HERNIATION
Disk L4 L5 S1–2
Pain Front of leg Side of leg Back of leg
Weakness Knee extension Great toe
dorsiflexion
Foot plantar flexion
Sensory loss Knee and medial foot Side of calf, web
of great toe
Back of calf and
lateral foot
Reflex loss Knee jerk None Ankle jerk
Chapter 19 LOW BACK PAIN126
6. How do I perform an SLR test? How do I interpret the results?
To perform an SLR test, have the patient lie supine while you slowly raise the involved leg
(flexing the hip while keeping the knee extended) until the patient complains of discomfort.
A positive SLR test occurs when leg elevation between 30 and 70 degrees results in pain that
radiates down the involved leg; merely evoking pain confined to the low back or hamstrings
does not count as a positive test. The SLR test is 91% sensitive but only 26% specific for a
herniated disk; a crossed-SLR test, in which raising the uninvolved leg evokes pain radiating
down the involved leg, is only 29% sensitive but 88% specific for disk herniation.
7. What Red Flag signs and symptoms should prompt further work-up?
Table 19-3 lists the high-risk signs and symptoms (and associated causes of LBP) that should
prompt spinal imaging: lumbosacral radiographs, computed tomography (CT), or magnetic
resonance imaging (MRI).
8. In addition to imaging, what other tests should I consider?
When spinal infection or malignancy is suspected, an erythrocyte sedimentation rate (ESR)
should be obtained. An elevated ESR (usually greater than 60–80 mm/hr) should lead to
further investigation, usually with a spinal CT or MRI. These tests should be obtained
emergently in patients whenever there is evidence of acute neurologic compromise
(e.g., loss of bowel or bladder function, motor weakness, or sensory changes).
9. What should I know about children who present with back pain?
Back pain is rare in children. LBP that interferes with activities previously enjoyed by a child
may be indicative of serious underlying pathology. Spondylolysis and spondylolisthesis due to
sports are the most common causes of LBP in children (see question 10). Scoliosis does not
usually cause back pain, but conditions that cause scoliosis (e.g., cancer, fracture, limb length
discrepancy, infection, or tumors) may cause pain. Although every attempt should be made to
limit gonadal radiation in pediatric patients, children with LBP that is not clearly mechanical in
TABLE 19-3. RED FLAG FEATURES OF LOW BACK PAIN
Red Flag Features Possible Cause Imaging
Age .50 years Fracture, malignancy LS-spine X-ray
Trauma Fracture LS-spine X-ray
Fever, intravenous drug use, recent infection Infection MRI or CT
Unexplained weight loss, history of cancer Metastases LS-spine X-ray
Urinary retention, motor deficits at multiple levels,
fecal incontinence, saddle anesthesia
Cauda equina
syndrome
MRI
Progressive motor weakness Myelopathy MRI
Failure to improve after 1 month Fracture, malignancy LS-spine X-ray
Immunosuppression or steroid use Fracture, infection LS-spine X-ray,
MRI, or CT
Midline spinal tenderness Fracture, infection,
malignancy
LS-spine X-ray
CT, computed tomography; LS, lumbosacral; MRI, magnetic resonance imaging.
Chapter 19 LOW BACK PAIN 127
nature should be imaged. An ESR may prove helpful when infection or malignancy is
suspected.
10. Is there a difference between spondylosis, spondylolysis, and
spondylolisthesis?
Yes. The terminology is confusing. The prefix spondylo- means vertebrae.
n
Spondylosis is a nonspecific term for degenerative spine disease.
n
Spondylolysis implies severe degeneration with a resulting fracture of the pars
interarticularis, which is the portion of the lateral mass of the vertebrae between the
superior and inferior articular processes.
n
When spondylolysis occurs bilaterally, anterior slippage of one vertebral body on another
can occur, termed spondylolisthesis. Severe spondylolisthesis can cause neurologic
impairment.
KEY POINTS: MEDICALLY SIGNIFICANT CAUSES OF LBP
1. Abdominal aortic aneurysm
2. Cauda equina syndrome
3. Lumbar disk herniation with severe neurologic compromise
4. Spinal malignancy
5. Spinal infection
11. Who should be hospitalized for treatment?
With the exception of previously discussed patients who require emergent CT or MRI, there
are no standard indications for hospitalization. Patients with suspected disk herniation who
are in significant physical distress or exhibit evidence of severe motor impairment of the lower
extremities are often admitted for pain control and strict bed rest because failure to respond to
aggressive conservative management may necessitate surgical intervention.
12. How should patients be treated in the ED?
Quickly. There is no need to await definitive diagnosis before providing pain relief. Oral or
parenteral nonsteroidal anti-inflammatory drugs (NSAIDs) and application of superficial heat
are first-line agents. Parenteral narcotics may be necessary to provide adequate analgesia.
13. How should patients with musculoskeletal LBP be treated as outpatients?
Bed rest is not recommended in patients with acute LBP. Patients who remain active have less
pain and are better able to perform everyday activities than those who rest in bed. Most
patients benefit from oral NSAIDs, but some require opioids to produce adequate analgesia
during the first few days. Sedatives and muscle relaxants may be effective in treating LBP, but
given the side effects (i.e., drowsiness and dizziness) and risk of long-term dependence, these
should not be used as first-line agents.
14. What aftercare instructions should I give my patients?
Patients with suspected disk disease and patients with symptoms that don’t improve within
1 to 2 weeks should be seen by a physician for follow-up evaluation. All patients should be
instructed to return immediately if they develop worsening symptoms, particularly bowel or
bladder dysfunction or progressive weakness.
