Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 22 DENTAL AND ORAL SURGICAL EMERGENCIES148
5. When should an avulsed tooth be
replanted? How is it stabilized?
An avulsed tooth should be replanted
within 1 to 2 hours of injury. Teeth should
not be replanted if more than 2 hours
have passed since avulsion. Stabilization
of replanted teeth is indicated provided
that there is not extensive caries,
periodontal disease, or large alveolar
housing fractures. Deciduous teeth should
not be replanted. Teeth are stabilized by
physiologic splinting with dental
composite and ligature wire for 7 to
10 days.
6. What are alveolar housing
fractures? How are they treated?
Fractures of the alveolar ridge
encompassing the dentition of the maxilla
or mandible. The usual treatment involves
the manual reduction of the fracture and
rigid splint fixation with an Erich arch bar
for 4 to 6 weeks.
7. Should antibiotics be prescribed
for an alveolar housing fracture or
reimplanted tooth?
Yes. A 5-day course of penicillin is
recommended. The oral dose of penicillin V is 500 mg four times a day for adults and 25 to
50 mg/kg/day in four divided doses for children. In penicillin-allergic patients, clindamycin is
preferred. The oral dose of clindamycin is 300 mg four times a day for adults and 10 to
20 mg/kg/day in four divided doses for children.
8. What are the concerns with electrical and thermal burns to the mouth?
n
Electrical burns are deceptive. The ultimate extent of tissue damage is greater than is
present on initial examination, and the full extent of the injury may not be appreciated for
4 to 7 days. Wound contracture may produce microstomia. Close observation is warranted
due to the possibility of delayed arterial hemorrhage.
KEY POINTS: PROCESS USED TO PREPARE AND APPLY
CALCIUM HYDROXIDE PASTE (DYCAL)
1. Isolate and dry tooth with gauze.
2. Dispense equal volume of base and catalyst paste onto a mixing pad.
3. Stir immediately using an applicator (the wooden end of a cotton-tipped applicator will
suffice) for 10 seconds until a uniform mixture occurs.
4. Quickly apply the mixed material onto the tooth and cover any exposed dentin or pulp.
5. Wait. The mixed material will set in about 2 minutes.
6. Remove excess paste with a sharp instrument. Be sure to check bite.
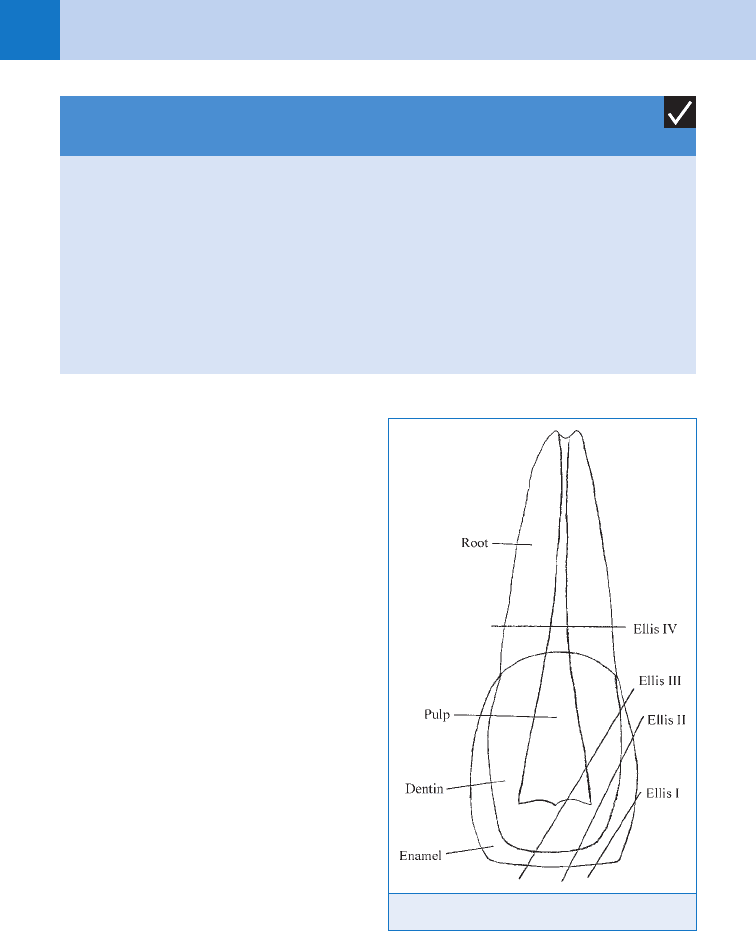
Figure 22-1. Ellis classification of tooth fractures.
Chapter 22 DENTAL AND ORAL SURGICAL EMERGENCIES 149
n
Thermal burns are typically treated with antibiotic ointment and topical steroids. Both
electrical and thermal burn contractures may need to be treated with skin grafts and
splinting.
9. How should a tongue laceration with profuse bleeding be treated?
Initially, packing with gauze and applying pressure should allow visualization of the source of
bleeding. Securing the airway may be necessary with some tongue lacerations due to
expanding hematoma and possible compromise of the airway. A silk traction suture placed
into the tip of the tongue can aid in visualization of the laceration. Injection of a local
anesthetic with 1:100,000 epinephrine aids with vasoconstriction. Clamping, ligating, or
electrocautery helps to control the larger bleeders when the site can be identified clearly. If
minor bleeding persists, the laceration should be closed in a layered fashion using resorbable
sutures for deep approximation and Vicryl or Dexon for surface approximation.
10. How should a through-and-through lip laceration be closed?
Initial debridement of the wound may require surgical and saline debridement. Wound
exploration and possible soft-tissue radiographs to rule out foreign body (e.g., tooth
fragments, metal, etc.) should be considered. Mucosal preparation with hexachlorophene
(pHisoHex) is recommended. The mucosa is closed with 3-0 plain gut suture. Skin preparation
with chlorhexidine following mucosal closure is recommended. A layered closure of the lip,
using 4-0 Vicryl suture for deep tissue/muscle approximation and 5-0 or 6-0 nylon for skin,
should be used. If the laceration involves the vermillion border, this should be approximated
first because any misalignment is extremely noticeable. Care should also be taken to align the
orbicularis oris muscle to avoid any deformity. Prophylactic antibiotic coverage with penicillin
for 5 days is recommended.
11. How should human or animal bites to the mouth be treated?
Human bites are managed best with copious irrigation, surgical debridement, tetanus
prophylaxis, and prophylactic antibiotics. The drug of choice is amoxicillin with clavulanic
acid. Wounds should be closed primarily if possible, although delayed primary closure is an
option in some cases. Animal bites are handled in a similar way. Antibiotics are recommended
and may vary depending on species. Patients bitten by animals with suspected rabies must be
treated aggressively, including irrigation with chlorhexidine solution followed by copious saline
irrigation and rabies postexposure prophylaxis.
12. When should antibiotics be used in management of dental infections?
An acute dentoalveolar abscess usually requires antibiotic therapy, with penicillin being the
drug of choice. Adjunctive therapy should include root canal treatment or extraction of the
offending tooth with incision and drainage. The patient should be followed closely, usually
within 24 hours.
13. List some nonodontogenic sources of orofacial pain.
n
Temporomandibular joint
n
Muscles of mastication
n
Salivary glands
n
Nose and paranasal sinuses
n
Blood vessels (arteritis)
n
Nerves
n
Oral ulcers
n
Cardiac ischemia can occasionally present with jaw pain
14. When should a patient with a dental abscess be admitted to the hospital?
Admission criteria should be based on history and physical findings: size and location of
swelling, rapidity of onset, dysphagia, dyspnea, fever, malaise, trismus, age, state of
hydration, laboratory evaluation, and immune status of the patient. Urgent admission for
Chapter 22 DENTAL AND ORAL SURGICAL EMERGENCIES150
airway concerns, as well as intravenous (IV) antibiotics and fluid resuscitation, may be
necessary.
15. Name the risks of dental local anesthesia.
Local anesthetic toxicity including seizures, allergy, syncope, trismus, needle tract infection,
intra-arterial or IV injection, paresthesia, hematoma, and transient Bell’s palsy from accidental
injection into the area of the parotid gland affecting cranial nerve VII. Broken needles rarely
occur.
16. What is the best way to perform local dental anesthesia?
Prior to all dental injections, the injection site should be cleansed with gauze and topical
anesthetic applied if desired. The most predictable way to provide anesthesia to the maxilla is
to infiltrate the buccal and palatal (painful injection) mucosa above the offending tooth with a
27-gauge short or long needle.
For the mandible, an inferior alveolar nerve block is the best way to provide anesthesia for
lower teeth on the affected side along with infiltration. To perform an inferior alveolar nerve
block, a 25- or 27-gauge long needle with an aspirating syringe is needed. Using the
nondominant hand, grasp the anterior mandible with your thumb intraorally near the
ascending ramus at the level of the teeth. Aim the needle at the external auditory canal while
inserting the needle in mucosa about 0.5 to 1 cm above the plane of teeth (bisecting your
thumbnail) while approaching from the opposite mandibular premolars. The needle tip should
enter the mucosa at the fold between the pharynx and buccal mucosa (pterygomandibular
raphe). The needle tip should be advanced approximately 1.5 to 2 cm until the medial side of
the mandible is felt, and then the needle is withdrawn a few millimeters. After aspirating,
approximately 1.8 mL of local anesthetic should have a therapeutic effect.
17. What is acute necrotizing ulcerative gingivitis (ANUG)? How is it treated?
ANUG is an acute infection of the gingiva that can be precipitated by psychological stress,
smoking, and poor oral hygiene. ANUG typically presents with blunted interdental papilla,
which represents areas of necrosis, gingival bleeding, pain, fetor oris, gingival swelling, and
lymphadenopathy. ANUG responds well to local debridement and irrigation. Oral rinses with
chlorhexidine are necessary. Antibiotics should be used only in refractory cases, and penicillin
is the drug of choice.
18. Why is a lateral pharyngeal abscess of great concern?
This infection is potentially life threatening because of airway obstruction and requires urgent
incision and drainage. This abscess occurs between the pharyngeal mucosa and the superior
constrictor muscle. Presenting symptoms usually include dysphagia, pain, trismus, and fever.
Medial bulging of the lateral pharyngeal wall frequently occurs, causing displacement of the
uvula to the opposite side. This complication is usually secondary to mandibular third molar
extractions and/or needle tract infections.
19. What is Ludwig angina?
An emergent infection of the submandibular, sublingual, and submental spaces bilaterally;
if untreated, airway compromise is inevitable. A dental cause is present in 90% of cases.
Treatment consists of maintaining the airway, removal of the offending tooth with incision and
drainage, antibiotics and IV hydration.
20. How are aphthous ulcers and herpetic lesions differentiated in the oral cavity?
Recurrent aphthous ulcers, also known as canker sores, occur as a single circular ulcer and
are usually less than 1 cm in diameter. The lesion has a central yellow area surrounded by a
prominent band of erythema. Herpetic lesions usually present as clusters of small vesicles
that eventually coalesce. Recurrent aphthous ulcers may occur anywhere in the oral cavity
except the lips, hard palate, and attached gingiva. Recurrent herpes occurs exclusively in the
lips, hard palate, and attached gingiva. Both of these types of lesions can be quite painful.
Chapter 22 DENTAL AND ORAL SURGICAL EMERGENCIES 151
21. How are oral cavity ulcers treated?
Recurrent aphthous ulcers are treated many different ways, including topical corticosteroids,
antibiotics, and anesthetic mouth rinses. An attapulgite (Kaopectate), diphenhydramine
(Benadryl), and lidocaine (Xylocaine)—KBX—suspension has been shown to provide relief in
cases of multiple recurrent aphthous ulcers. The treatment of herpes simplex virus is aimed at
palliation of pain. Topical acyclovir, when used during the prodromal stage, has been shown to
decrease size of lesions and duration of symptoms. Children may become dehydrated and
require admission.
22. How is postextraction hemorrhage evaluated and treated?
The patient’s past medical history and current medications should be thoroughly reviewed.
Clinical inspection must include good lighting and suction to evaluate the alveolus for a
bleeding source. Application of a gauze dressing maintained with firm digital pressure over the
extraction site stops most bleeding episodes.
Some hemostatic agents such as gelatin sponges (Gelfoam), absorbable knitted fabric
(Surgicel), and topical thrombin may also be useful. Injecting the area with a local anesthetic
containing a vasoconstrictor can also be effective. A carefully placed suture aids hemostasis.
Refractory bleeding should be evaluated further with appropriate laboratory studies.
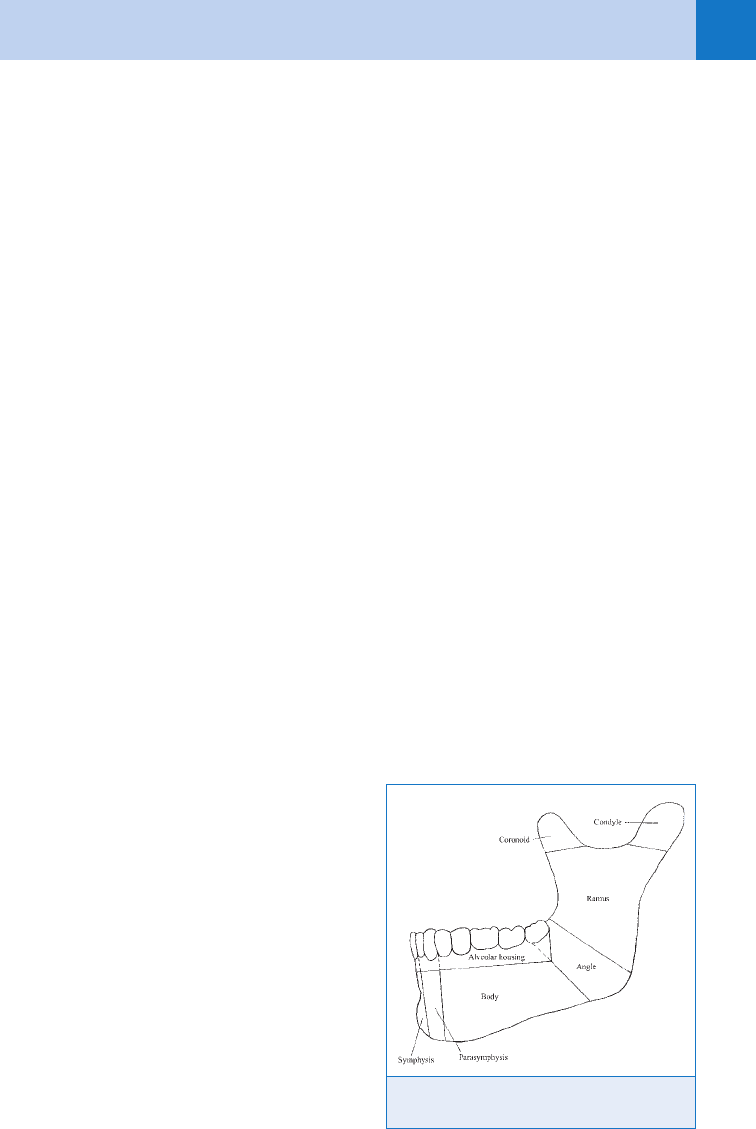
23. What is the classification of mandibular fractures?
The best clinical classification is by anatomic region: symphysis, parasymphysis, body, angle,
ramus, condyle, and alveolar housing. These fractures may be further described by the
specific type of fracture: simple, compound, comminuted, multiple, greenstick, or pathologic.
(See Fig. 22-2.)
24. List different ways to radiologically examine a patient for a mandible fracture.
Panoramic radiograph, computed tomography, mandible series (i.e., Towne’s views,
posteroanterior, and lateral oblique right and left), dental periapical radiographs.
25. How do you clinically examine a patient for a mandibular fracture?
The main diagnostic criteria are a history of trauma, abnormal mandibular movements elicited
by bimanual palpation, step deformities or changes in the occlusion, loose teeth, and soft-
tissue trauma including laceration or hematoma.
26. Describe a lasso ligature.
A 24-, 25-, or 26-gauge wire that is
placed around one or two teeth adjacent
to a fracture to approximate fragments of
a mandible fracture. The wire is tightened
as the patient’s occlusion is maintained to
bring the fracture into closer alignment.
This helps to relieve pain, stop bleeding,
and prevent the continued contamination
of saliva into the fracture site.
27. Are antibiotics indicated for a
mandibular fracture?
Antibiotics are indicated in all open
mandibular fractures and all fractures
involving teeth are considered open
fractures. Fractures of the subcondylar/
condylar region that do not communicate
with the external auditory canal are
closed and are not treated with
antibiotics.
Figure 22-2. Clinical classification of mandibular
fractures by anatomic region.
Chapter 22 DENTAL AND ORAL SURGICAL EMERGENCIES152
28. List the immediate clinical problems associated with a fractured mandible.
n
Airway compromise
n
Bleeding
n
Pain
n
Fracture displacement
n
Displaced or aspirated teeth
n
Lacerations
n
Trismus
n
Subcutaneous emphysema
29. What is a mandible contrecoup fracture?
A fracture distant from the site of trauma. A classic example is trauma to the symphysis or
parasymphysis area with unilateral or bilateral subcondylar fractures.
30. Describe the treatment of dry socket (alveolar osteitis).
Dry socket is treated by gently irrigating the extraction site and placing a sedative dressing
(BIPS and gauze or Alvogyl) into the socket. Local anesthetic may be necessary for pain relief
during application of the dressing. Follow-up is needed to ensure pain relief and absence of
infection. Multiple treatments are sometimes necessary.
KEY POINTS: COMMON CHARACTERISTICS OF DRY SOCKET
(ALVEOLAR OSTEITIS)
1. Extraction 2 to 3 days prior to onset of pain
2. No purulence
3. No fever
4. No clot in extraction site (exposed bone)
5. No trismus
31. What oral complication is being seen with the use of bisphosphonates in the
treatment of malignancy?
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is associated with IV
bisphosphonate or oral bisphosphonate usage, usually following dentoalveolar surgery or in
areas of bony protuberances and presents as an area of necrotic bone with or without pain or
infection. It is treated with chlorhexidine 0.12% mouth rinses, analgesics, antibiotics,
hyperbaric oxygen therapy, and surgery, depending on the severity.
KEY POINTS: BRONJ
1. Area of necrotic bone present for more than 8 weeks.
2. May or may not have pain or infection.
3. Occurs in the mandible 2:1 over maxilla.
4. Use of bisphosphonates for treatment of cancer-related conditions or osteoporosis.
Chapter 22 DENTAL AND ORAL SURGICAL EMERGENCIES 153
BIBLIOGRAPHY
1. American Association of Oral & Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis
of the jaws. J Oral Maxillofac Surg 65:369–367, 2007.
2. Flynn TR, Halpern LR: Antibiotic selection in head and neck infections. Oral Maxillofac Surg Clin North Am
15:17–38, 2003.
3. Fonseca R, Walker R, editors: Oral and maxillofacial trauma, ed 3, St. Louis, 2005, Elsevier Saunders.
4. Ghali GE, Larsen PE, Waite PD: Peterson’s principles of oral and maxillofacial surgery, ed 2, London, 2004,
BC Decker.
5. Kaban L, Pogrel M, editors: Complications in oral and maxillofacial surgery, Philadelphia, 1997, W. B.
Saunders.
6. Malamed A: Handbook of local anesthesia, St. Louis, 1996, Mosby.
7. Marx R. Stern D, editors: Oral and maxillofacial pathology, Chicago, 2003, Quintessence Publishing, pp 53–54.
8. Mehrotra B, Rosenberg TJ, Engroff SL: Osteonecrosis of the jaws associated with the use of bisphosphonates:
a review of 63 cases. J Oral Maxillofac Surg 62:527–534, 2004.
9. Topazian R, Goldberg M, editors: Oral and maxillofacial infections, 4th ed. Philadelphia, 2002, W. B. Saunders,
pp 177–185.
155
IV. CENTRAL NERVOUS SYSTEM
CHAPTER 23
TRANSIENT ISCHEMIC ATTACK
AND CEREBROVASCULAR ACCIDENT
Michael M. Liao, MD
1. Define cerebrovascular accident (stroke)?
Stroke is any vascular injury that impairs or blocks cerebral blood flow to a specific
region of the brain, resulting in ischemic injury to brain cells. Stroke is the third most
common cause of mortality in the United States and the leading cause of adult disability.
2. What are the major types of acute stroke?
The two major types are ischemic and hemorrhagic. The critical diagnostic study to
differentiate between the two is a noncontrast head computed tomography (CT).
3. What are the causes of ischemic stroke?
Ischemic stroke causes 80% of all strokes.
n
Thrombotic: atherosclerosis, vasculitis, lacunar
n
Embolic: atrial fibrillation, mechanical heart valve, low cardiac ejection fraction,
endocarditis, atrial septal defects, cervical artery dissection (i.e., carotid or vertebral
arteries)
4. What are the causes of hemorrhagic stroke?
Hemorrhagic stroke causes 20% of all strokes. These can be either intracerebral or
subarachnoid hemorrhage.
5. What are the potential mimics of acute stroke?
Postictal Todd’s palsy, hypoglycemia, complex migraine, conversion disorder, Bell’s
palsy, acute spinal cord compression, brain tumor, systemic infection, and multiple
sclerosis.
6. Define transient ischemic attack (TIA)?
The classic definition of TIA has been time-based (i.e., ,24 hours of symptoms), yet
most TIAs will resolve within 1 hour. However, up to 67% of classic TIAs will have
evidence of acute ischemic lesions on diffusion-weighted magnetic resonance imaging
(MRI). Because no time cutoff can reliably determine if underlying ischemic infarction
has occurred, in 2009 the American Heart Association and American Stroke Association
(AHA/ASA) transitioned to a tissue-based definition of TIA (i.e., transient symptoms with
lack of tissue injury confirmed by neuroimaging).
7. Why be concerned about a TIA?
Just as acute coronary syndrome can be a harbinger of myocardial infarction, TIAs are
associated with a high risk of early acute stroke (up to 10% within the first 2 days).
The ABCD
2
score may be useful in predicting 2-day stroke risk (Table 23-1). Evidence
suggests that rapid evaluation and initiation of preventative measures within 24 hours
may significantly reduce the risk of recurrent stroke.
8. How do I differentiate between TIA and stroke?
If a TIA or stroke presents acutely, it may be impossible to differentiate between them
without MRI. Both should be emergently managed as a possible acute stroke.

Chapter 23 TRANSIENT ISCHEMIC ATTACK AND CEREBROVASCULAR ACCIDENT156
9. How do I approach a patient with acute stroke symptoms?
Initial triage should be emergent. As with all acute patients, airway, breathing, and
circulation (ABCs), intravenous (IV) access, oxygen, and monitoring are the critical first
steps. Early management must also include a fingerstick glucose test, noncontrast head CT,
electrocardiogram (ECG), and immediate notification of a stroke team, if available. History is
critical to stroke assessment and must include time of onset, evidence of preceding seizure,
anticoagulation use, and potential associated trauma. A complete neurologic examination is
essential. Abnormal blood pressures (BP) are important to recognize, but management will
depend on if the stroke is hemorrhagic or ischemic.
10. How do I determine the onset time for an acute stroke?
Symptom onset is critical to determine eligibility for thrombolytic therapy and must be
documented for every patient. Unless the symptom onset is clearly witnessed or known by the
patient, the time when the patient was last seen to be normal is used. If the patient awakens
from sleep with stroke-like symptoms, then the last time the patient was awake and normal is
considered the time of onset.
11. When should I consider extracranial arterial dissection as a cause of acute
stroke?
Dissection of the extracranial carotid and vertebral arteries (also called cervical arteries) is an
important etiology of acute ischemic stroke. Injury to these vessels can cause stroke from
either thrombus embolization or vessel occlusion. Consider this etiology in those with neck
trauma (including even minor trauma); cervical spine fractures; young patients (,45 years
old); and those with neck pain.
BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic
blood pressure; TIA, transient ischemic attack.
• Age 60 1 point
• BP: Initial SBP 140 or DBP 90 1 point
• Clinical features:
Unilateral weakness 2 points, or
Speech impairment without weakness 1 point, or
Other 0 points
• Duration of TIA:
60 min 2 points, or
10–59 min 1 point, or
,10 min 0 points
• Diabetes 1 point
2-day stroke risk:
• High: total 6–7 pts (8.1% risk)
• Mod: total 4–5 pts (4.1%)
• Low: total 0–3 pts (1.0%)
TABLE 23-1. ABCD
2
SCORE

Chapter 23 TRANSIENT ISCHEMIC ATTACK AND CEREBROVASCULAR ACCIDENT 157
12. What is a primary stroke center?
In 2003, The Joint Commission launched a Primary Stroke Center Certification Program in
collaboration with AHA/ASA. To obtain Primary Stroke Center Certification, a hospital must
address 11 major aspects of acute stroke care, including acute stroke teams, written care
protocols, and multidisciplinary integration.
13. Who is on the stroke team?
The optimal management of stroke requires a multidisciplinary collaboration among
the emergency medical service (EMS), ED, neurology, neurosurgery, neuroradiology,
interventional neuroradiology (if available), laboratory services, and critical care. In a
primary stroke center, an acute stroke team, consisting of at least two healthcare providers
experienced in diagnosing and treating acute stroke, is on call 24/7 to evaluate a patient
within 15 minutes.
14. What role do emergency medical technicians (EMTs) play?
Besides acute stabilization, EMTs are tasked with early recognition of potential acute stroke
and the rapid communication of these findings with the receiving hospital. This allows early
activation of the acute stroke team and preparation of CT/MRI, which can save precious
minutes in the early evaluation of acute stroke.
15. When do I activate the acute stroke team?
As soon as you suspect the patient of having an acute stroke within the window period for
therapy, you should activate the acute stroke team immediately.
16. What is the window for systemic thrombolytics?
The publication of European Cooperative Acute Stroke Study (ECASS) III in 2008 has extended
the potential window for thrombolytics from 3 hours to 4.5 hours.
17. What is the evidence for tissue plasminogen activator (tPA) in acute ischemic
stroke?
Alteplase (also called tPA) is the only thrombolytic currently approved by the Food and Drug
Administration (FDA) for acute stroke. In 1995, the National Institute of Neurological Disorders
and Stroke (NINDS) trial showed that tPA improved functional outcome at 3 months (i.e.,
modified Rankin scale <1) if given within 3 hours of symptom onset, with a number needed
to treat (NNT) 6 and number needed to harm (NNH) 17. In 2008, ECASS III showed similarly
improved functional outcome within the 3- to 4.5-hour timeframe (NNT 14, NNH 47; NNH 23
with NINDS definition). NNH represents symptomatic intracerebral hemorrhage, and NNT
represents modified Rankin scale <1 at 3 months.
18. What is the risk of tPA?
The primary risk of tPA is systemic bleeding, particularly intracerebral hemorrhage (ICH).
Angioedema may occur in 1% to 5% of patients. For the NINDS trial, ICH with tPA was 6.4%
versus 0.6% for the nontreatment group. For ECASS III, ICH with tPA was 2.4% versus 0.2%
(7.9% versus 3.5% if original NINDS definitions were used). The factors that appear
associated with increased risk of hemorrhage are older age, brain edema or mass effect on
CT, and higher baseline stroke severity.
19. What is the importance of the National Institutes of Health stroke scale
(NIHSS)?
The NIHSS is the most commonly used objective measure of acute stroke severity. It ranges
from 0 to 42, involves 13 questions, and requires the use of standardized pictures, sentences,
and words. A booklet and standardized template are free online at www.strokecenter.org/trials/
scales/nihss.html.
