Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 24 MENINGITIS168
WEBSITE
Infectious Diseases Society of America: www.idsociety.org.
BIBLIOGRAPHY
1. Attia J, Hatala R, Cook DJ, et al: Does this adult patient have acute meningitis? JAMA 282:175–181, 1999.
2. Chaudhuri A: Adjunctive dexamethasone treatment in acute bacterial meningitis. Lancet Neurol 3:54–62, 2004.
3. Edlow JA: Headache. In Wolfson AB, editor: Hardwood-Nuss’ clinical practice of emergency medicine, ed 4,
Philadelphia, 2005, Lippincott Williams & Wilkins, pp 94-100.
4. Euerle B: Spinal puncture and cerebrospinal fluid examination. In Roberts JR, Hedges JR editors: Clinical
procedures in emergency medicine, ed 4, Saunders, 2004, pp 1197–1222.
5. Quagliarello VJ, Scheld WM: Treatment of bacterial meningitis. N Engl J Med 336:708–716, 1997.
6. Sadoun T, Singh A: Adult acute bacterial meningitis in the United States: 2009. update. Emergency Medicine
Practice 11(9): 1–25, 2009.
7. Talan DA: New concepts in antimicrobial therapy for emergency department infections. Ann Emerg Med
34:503–516, 1999.
8. Ziai WC, Lewin III JJ: Update in the diagnosis and management of central nervous system infections.
Neurologic Clinics 26: 427–468, 2008.
169
V. RESPIRATORY SYSTEM
CHAPTER 25
BREATHING AND VENTILATION
John L. Kendall, MD, and Ryan Paterson, MD
1. How useful is the respiratory rate in the evaluation of a patient?
The respiratory rate is invaluable as a vital sign. Normal respiratory rate in children varies
with age, whereas adults typically breathe 12 to 16 times per minute. As a testament to its
usefulness, the respiratory rate can be helpful in the diagnosis of many conditions other
than those with primary pulmonary pathology. For example, it is elevated in patients with
anemia, arteriovenous fistula, pregnancy, cyanotic heart disease, metabolic acidosis, febrile
illness, central nervous system pathology, anxiety, and those at high altitude. It is important
that the respiratory rate be counted carefully for at least 30 seconds. The respiratory rate is
often incorrectly estimated from a short period of observation.
2. Which breathing patterns are associated with pathologic conditions?
n
Kussmaul respirations are deep, rapid breaths that are associated with metabolic
acidosis.
n
Cheyne-Stokes breathing comprises respirations that wax and wane cyclically so that
periods of deep breathing alternate with periods of apnea. Causes include congestive
heart failure (CHF), hypertensive crisis, hyponatremia, high altitude illness, and head
injury.
n
Ataxic breathing is characterized by unpredictable irregularity. Breaths may be
shallow or deep and may stop for short periods. Causes include respiratory
depression and brain stem injury at the level of the medulla.
3. Which pulmonary function tests are commonly used in the ED?
Other than the respiratory rate, the most useful pulmonary function test for ED patients
is the peak expiratory flow rate. It is measured by having a patient exhale at a maximum
rate through a peak flowmeter. Normal values range from 350 to 600 L/min in adults.
Lower levels are characteristic of increased airway resistance as commonly seen in
asthma and chronic obstructive pulmonary disease (COPD) exacerbations. Patients who
present with values of less than 100 L/min have severe airflow obstruction. Comparing a
patient’s current peak expiratory flow rate to his or her personal best can provide good
insight into the severity of respiratory distress and necessary treatment. Serial
measurements are helpful for objectively quantifying response to treatment. A less
commonly used test is the forced end-expiratory volume at 1 second, which helps
quantify the severity of obstructive and restrictive lung disease.
4. How does pulse oximetry work?
Pulse oximetry is based on a combination of spectrophotometry and plethysmography.
n
Spectrophotometry is based on the Beer-Lambert law, which holds that optical
absorbance is proportional to the concentration of a substance and the thickness of the
medium. Using this principle, the absorbance of light within a pulsatile vascular bed is
used to distinguish between oxyhemoglobin (O
2
Hb) and reduced hemoglobin (Hb).
n
Plethysmography measures the tissue displacement caused by an arterial pulse. This
allows for assessment of the increase in light absorption caused by local arterial flow
compared with the background of composite tissues and venous blood.
Plethysmography also allows determination of the heart rate.
Chapter 25 BREATHING AND VENTILATION170
Pulse oximeters function by placing a pulsatile vascular bed between a light-emitting diode
(LED) and a detector. Light is transmitted through the tissue at two wavelengths, 660 nm
(primarily absorbed by O
2
Hb) and 940 nm (primarily absorbed by Hb), allowing differentiation
of O
2
Hb from Hb. The detector compares the concentration of O
2
Hb and Hb and displays the
result as a percent saturation.
5. How can pulse oximetry be useful? In which situations can it yield false
readings?
Pulse oximetry is useful when monitoring arterial O
2
Hb saturation in cardiopulmonary
disorders; monitoring oxygen saturation during conscious sedation, airway management, or in
patients with a decreased level of consciousness; or quantifying the arterial O
2
Hb saturation
response to therapeutic interventions. Situations in which the usefulness of pulse oximetry is
limited include vasoconstriction, excessive movement, low O
2
Hb saturations (,83%),
intravascular dyes, exposure of the measuring sensor to ambient light sources, and when nail
polish is present. Oxygen saturation measurements may be falsely elevated in the presence of
carboxyhemoglobin and falsely decreased in the presence of methemoglobin.
KEY POINTS: PULSE OXIMETRY
1. Pulse oximetry measures oxygenation, not ventilation.
2. Poor peripheral perfusion is a frequent reason pulse oximeters provide unreliable readings.
6. Why can a good pulse oximetry reading be falsely reassuring?
Clinicians often rely on the pulse oximeter as part of monitoring a patient’s respiratory status,
particularly when using procedural sedation. The pulse oximeter only measures oxygenation
and provides no information regarding CO
2
exchange and thus does not assess for adequate
ventilation. A preoxygenated patient can be apneic for several minutes without an appreciable
decrease in oxygen saturation, while significant hypercarbia is developing. Although the pulse
oximeter has become indispensable, the clinician must always remember that it only assesses
one part of a patient’s respiratory status.
7. What is end-tidal CO
2
(EtCO
2
) and when is its monitoring useful?
EtCO
2
is another monitoring device used to evaluate ventilation, and when combined with the
pulse oximeter, it provides a more complete evaluation of the patient’s respiratory status.
EtCO
2
monitors exhaled CO
2,
displaying its concentration in both numerical and graphical
format. The CO
2
concentration in the breath correlates directly with the concentration of CO
2
in the alveoli. The CO
2
in the alveoli is dependent on the ventilation/perfusion (V/Q)
relationship, which is influenced by a number of physiologic and pathologic states. A CO
2
increase or decrease may represent the earliest change in a patient’s ventilation and perfusion
states. EtCO
2
is currently being used in a number of ways:
n
During conscious sedation
n
In patients with sepsis to monitor perfusion status
n
During cardiopulmonary resuscitation (CPR) to monitor effectiveness of compressions
n
For monitoring airway response to treatment in patients with COPD and asthma
n
To monitor for tube placement or dislodgement by emergency medical services (EMS)
during intubation and transport
8. What percentage of fraction of inspired oxygen (FiO
2
) corresponds with the
various types of oxygen delivery systems?
The three primary means of oxygen delivery are nasal cannula, simple facemask, and
facemask with an oxygen reservoir. A nasal cannula can be used to deliver oxygen at rates of

Chapter 25 BREATHING AND VENTILATION 171
1 to 6 L/min. With a nasal cannula, every 1 L/min of flow increase causes the FiO
2
to rise by
4%. As a result, a nasal cannula can deliver a FiO
2
between 25% and 45%. A simple facemask
relies on an oxygen flow of 5 to 10 L/min with a resulting FiO
2
ranging from 35% to 50%.
A facemask with an oxygen reservoir has a constant flow of oxygen so that higher
concentrations of oxygen can be achieved. A properly fitted facemask with an oxygen
reservoir with a 15 L/min flow rate can deliver up to 85% FiO
2
.
9. What is noninvasive ventilation?
It is a means of delivering positive-pressure ventilation without placing a nasotracheal or
endotracheal tube. As such, ventilatory assistance is possible without the risks of intubation
and mechanical ventilation. Careful selection of patients can make noninvasive ventilation a
useful tool to the emergency physician. Any patient who does not have an appropriate mental
status, is unable to protect the airway, or is unable to develop an adequate respiratory rate
would not be a good candidate for noninvasive ventilation.
10. What forms of noninvasive ventilation are available to emergency physicians?
The two most useful forms are mask continuous positive airway pressure (CPAP) ventilation
and bilevel positive airway pressure (BiPAP). Each method involves placing a tight-fitting mask
over the patient’s face and delivering breaths by positive pressure.
n
CPAP delivers a continuous amount of positive airway pressure during and after inspiration
and expiration.
n
BiPAP not only provides a set positive pressure during exhalation but also delivers a set
inspiratory pressure when the patient initiates a breath. The inspiratory pressure is always
set higher than the expiratory pressure, can be sustained for various periods, and stops
when the patient ceases to inhale or begins to exhale.
11. In what circumstances would noninvasive ventilation be preferred over
standard invasive ventilation?
Noninvasive ventilation has been shown to be useful in many conditions, including pulmonary
edema, pneumonia, asthma, COPD, and nocturnal hypoventilation. In properly selected
patients, CPAP is particularly useful in the treatment of pulmonary edema and BiPAP in
respiratory distress due to COPD. Patients with COPD are notoriously difficult to wean from
mechanical ventilators, and noninvasive ventilation can frequently be used to turn around
COPD patients in moderate respiratory distress who would otherwise have required standard
invasive ventilation. Lastly, some patients with advance directives forbidding mechanical
ventilation can benefit from the respiratory support provided by noninvasive ventilation.
12. How do I determine the initial ventilator settings in someone who has just
been intubated?
Ventilator settings must take into account the patient’s oxygenation status and his or her
ventilation or acid-base status. The primary method for affecting the oxygenation of a patient
is to alter the FiO
2
and positive end-expiratory pressure (PEEP). Initially, intubated patients
should be given 100% oxygen or an FiO
2
of 1.00. Subsequently, if arterial blood gas analysis
reveals that the PaO
2
is high, the FiO
2
and PEEP may be lowered incrementally.
The main factors determining a patient’s ventilatory status are tidal volume and respiratory
rate. Changes in each are reflected by the CO
2
from arterial blood gas analysis. High
respiratory rates and large tidal volumes decrease the carbon dioxide level, whereas the
converse elevates the carbon dioxide level. Initially, the tidal volume can be estimated to be
8 to 10 mL/kg; for a 70-kg patient, that is 560 to 700 mL.
The initial respiratory rate varies depending on the clinical situation. On average, the rate
should be set between 10 and 16 breaths per minute.
13. Are ventilator settings always the same?
No. When you intubate a patient you must remember that you have now placed a bet that you
can do a better job directing that patient’s ventilation than his or her brain. Keep in mind that
Chapter 25 BREATHING AND VENTILATION172
your patient’s respiratory center has millions of years of evolution backing it up compared
with your measly few years of experience. Imagining how your patient’s respiratory center
would respond to the clinical situation and where the failure has occurred will help you to
determine the best ventilator settings for your patient. For example, a patient with an
obstructive condition such as asthma does best with small tidal volumes, high respiratory
rates, and low levels of PEEP. In contrast, a patient with a COPD exacerbation requires lower
respiratory rates, higher tidal volumes, no PEEP, and a prolonged expiratory time. Following
EtCO
2
and pulse oximetry can provide real-time feedback of the adequacy of your settings.
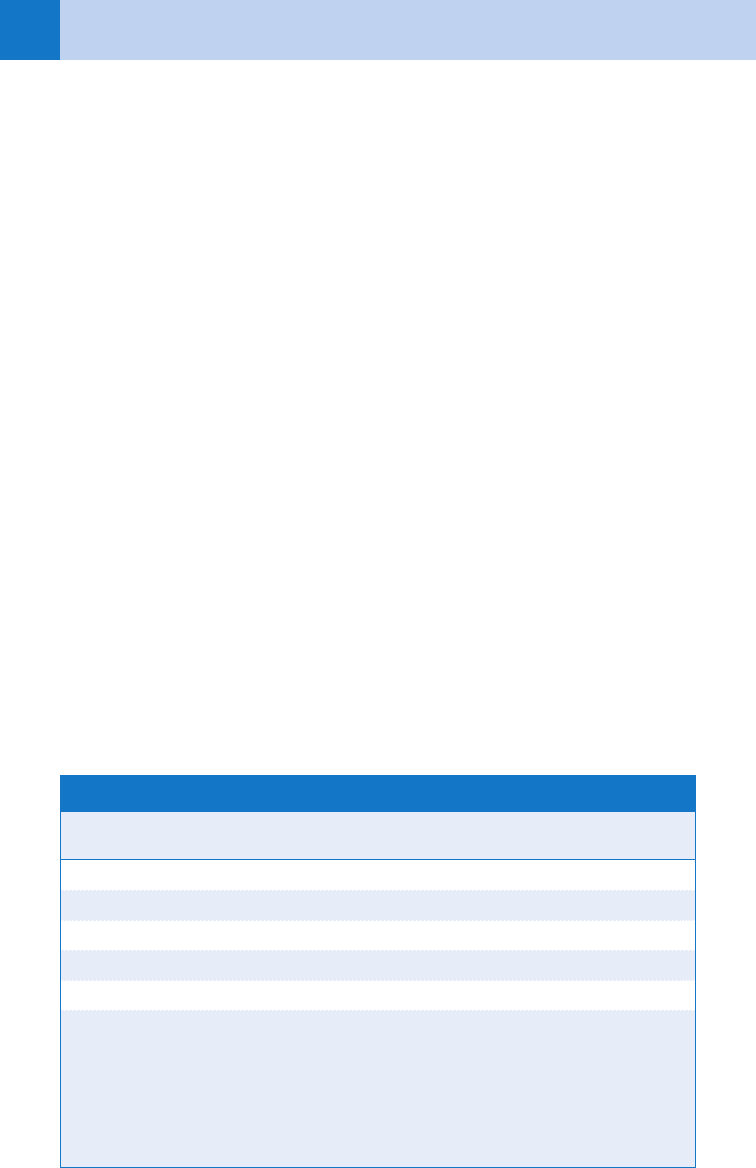
Other common ventilator settings for patients with closed head injury, CHF, metabolic
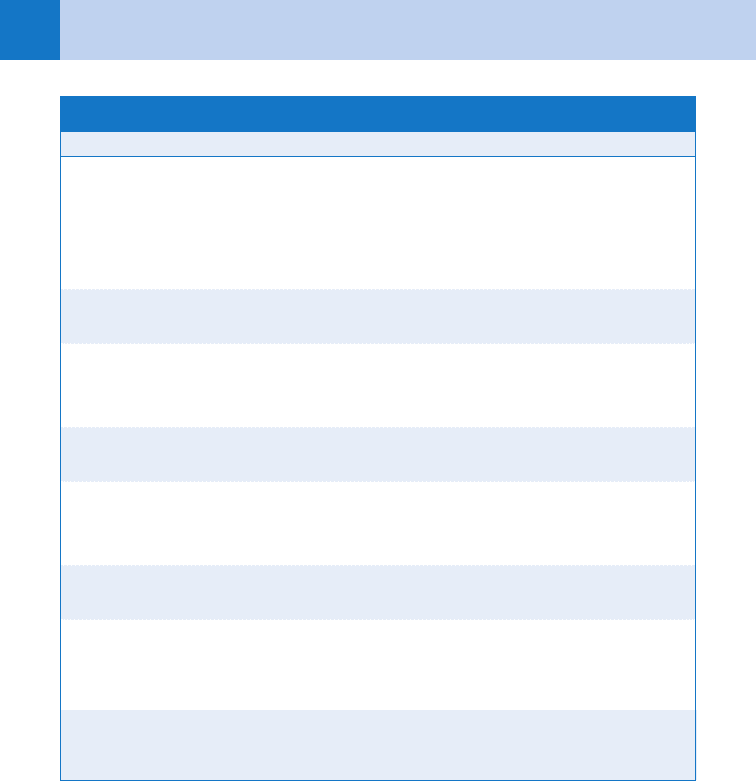
acidosis, and sepsis are shown in Table 25-1.
14. What are the different ventilator modes?
The main modes of ventilation are controlled mechanical ventilation (CMV), assist control
(AC), intermittent mandatory ventilation (IMV), and synchronized intermittent mandatory
ventilation (SIMV). In the CMV mode, the ventilator delivers a certain volume or pressure at a
preset rate, regardless of any ventilatory effort by the patient. AC is similar to CMV in that the
tidal volume or inspiratory pressure and minimum respiratory rate are set. It differs from CMV
by allowing patients to trigger the ventilator over a set minimum respiratory rate. IMV allows
the patient to breathe spontaneously without having a preset tidal volume or pressure. A set
rate similar to the CMV mode is in place. This allows the patient to breathe spontaneously,
while ensuring a set respiratory rate and tidal volume. SIMV differs from IMV in that the
ventilator senses the patient’s spontaneous respirations and does not deliver a breath if the
patient has already triggered the ventilator. This prevents stacking of respirations, which can
be a component of the IMV mode.
15. What is PEEP?
PEEP is pressure applied during expiration. PEEP prevents collapse of alveoli at end-expiration
leading to an increase in functional residual capacity. The end result is improved V/Q matching
in the pulmonary circulation, improving oxygenation. On the flip-side, PEEP can induce
barotrauma, diminish venous return to the heart, and elevate intracranial pressure. PEEP is
usually set at 2.5 or 5.0 cm H
2
O.
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; FiO
2
, fraction of inspired oxygen;
PEEP, positive end-expiratory pressure.
American Heart Association: Pediatric Advanced Life Support Provider Manual, Dallas, 2002, American Heart
Association, p 109.
Condition
Tidal Volume
(mL/kg)
Respiratory Rate
(breaths per minute) FiO
2
PEEP
(cm H
2
O)
Asthma 5–10 10–16 100% 2.5–10
COPD 8–12 6–8 100% None
Head injury 12–15 14–20 100% None
CHF 8–12 8–12 100% 5–10
Metabolic acidosis 8–12 14–20 100% 2.5–5
Sepsis 6 10–16 100% 2.5–5
TABLE 25-1. VENTILATOR SETTINGS ACCORDING TO CONDITION
Chapter 25 BREATHING AND VENTILATION 173
16. What is auto-PEEP?
Auto-PEEP develops when a positive-pressure breath is delivered before complete exhalation
of the previous breath. As a result, air becomes trapped and pressure within the lungs
increases. This leads to increased airway pressures, diminished venous return to the right
heart, and consequently hypotension. The increased airway pressures can lead to barotrauma,
pneumothorax, and inaccurate pulmonary artery catheter measurements. Auto-PEEP can be a
particular problem in the mechanical ventilation of COPD and asthmatic patients. The
immediate solution is to disconnect the ventilator circuit and allow a full exhalation followed
by appropriate changes to the ventilator settings.
17. What are the most common complications of mechanical ventilation?
The most common direct complication seen in the ED is barotrauma. High pressure can lead
to rupture of the alveolar wall, which can lead to pneumomediastinum, pneumothorax, tension
pneumothorax, pneumoperitoneum, and subcutaneous emphysema. Pneumonia leads the list
of ventilator complications overall, followed by sinusitis, tracheal necrosis, local trauma to the
nares and mouth, increased intracranial pressure, renal failure, hyponatremia, and fluid
retention.
18. How do I approach a patient on a ventilator with acutely worsening
oxygenation or ventilation?
A systematic approach to this situation will serve you well. The DOPE mnemonic taught in
pediatric life support can be helpful in remembering the approach:
n
First remove the patient from the ventilator and have an assistant hand ventilate the patient.
Many problems involving a $30,000 ventilator can be solved with a $15 resuscitation bag.
n
Displacement: Confirm the endotracheal tube is in the proper place by using some
combination of auscultation, CO
2
exchange, radiography, and direct visualization.
n
Obstruction: Confirm that the endotracheal tube is patent by passing suction catheter.
Sometimes an endotracheal tube can become kinked simply due to patient positioning.
n
Pneumothorax: Confirm that there is no evidence of barotrauma, usually by a combination
of physical examination and a chest radiograph.
n
Equipment: Confirm that the ventilator circuit and ventilator itself are functioning properly.
KEY POINTS: VENTILATOR MANAGEMENT
1. Each clinical situation calls for a different approach to ventilator management.
2. Tidal volume and respiratory rate affect the patient’s ventilation and pCO
2
.
3. FiO
2
and PEEP affect the patient’s oxygenation and pO
2
.
4. Oxygenation and ventilation problems in patients on mechanical ventilators can be managed
by removing them from the ventilator and following the DOPE mnemonic.
174
CHAPTER 26
ASTHMA, CHRONIC OBSTRUCTIVE
PULMONARY DISEASE, AND PNEUMONIA
Rita K. Cydulka, MD, MS, and Scott Felten, MD, FACEP
ASTHMA
1. What is asthma and what are the presenting symptoms of asthma
exacerbation?
Asthma is a chronic inflammatory disorder of the airways, resulting in recurrent
episodes of wheezing, breathlessness, chest tightness, and coughing. The airway
inflammation contributes to airway hyperreactivity, airflow obstruction, and chronic
disease.
2. In addition to asthma, what should be included in the differential
diagnosis of wheezing?
Chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), foreign
body aspiration, anaphylaxis, epiglottitis, tracheobronchitis, reactive airway disease, viral
respiratory infections, and vocal cord dysfunction.
3. Which aspects of the asthmatic’s history are important to the current
exacerbation?
Ask questions regarding exposure to common precipitants, such as viral upper
respiratory tract infections, allergens, cold, exercise, and possible aspirin or
nonsteroidal anti-inflammatory drug use. Also important are duration and severity of
symptoms, past history and frequency of sudden exacerbations, prior hospitalizations
and intubations, number of recent ED visits, current medications, worsening of
symptoms while on or if weaning off corticosteroids, and other comorbidities.
Non-Caucasian race and lower socioeconomic standing are also risk factors for severity
requiring hospitalization.
4. Are there any helpful ancillary diagnostic tests?
Bedside spirometry provides a rapid, objective assessment of patients and serves as a
guide to the effectiveness of therapy. The forced expiratory volume in 1 second (FEV
1
)
and the peak expiratory flow rate (PEFR) directly measure the degree of large airway
obstruction.
n
FEV
1
or PEFR >70% of predicted (or personal best) indicates mild obstruction
n
FEV
1
or PEFR 40%–69% of predicted (or personal best) indicates moderate
obstruction
n
FEV
1
or PEFR ,40% of predicted (or personal best) indicates severe obstruction
Pulse oximetry is a useful and convenient method for assessing oxygenation and
monitoring oxygen saturation during treatment. Most other tests, including arterial blood
gases, complete blood counts, and electrocardiograms, are not useful in the
management of asthma except in cases of active or impending respiratory failure. Chest
X-ray may be helpful if the patient does not respond to initial treatment or if a pulmonary
complication, such as foreign body obstruction, pneumonia, pneumomediastinum,
pneumothorax, or CHF, is suspected.
Chapter 26 ASTHMA, CHRONIC OBSTRUCTIVE PULMONARY DISEASE, AND PNEUMONIA 175
5. What are the key objectives when treating an asthma exacerbation? How are
they achieved?
The key objectives include correction of significant hypoxemia, rapid reversal of airflow
obstruction, and reduction of the likelihood of recurrence of severe airflow obstruction.
First-line treatment includes b
2
-agonists and corticosteroids in moderate exacerbations,
and oxygen if needed. Ipratropium should be added when treating severe exacerbations. Relief
of airflow obstruction (bronchoconstriction) is usually accomplished by administration of
either intermittent or continuous doses of aerosolized b
2
-agonists. Studies contain mixed
conclusions as to whether there is any added clinical benefit to levalbuterol in comparison to
racemic formulations. Current evidence does not suggest an improved benefit from
intravenous b
2
-agonists compared to aerosol. Early administration of systemic corticosteroids
addresses the inflammatory component of acute asthma and has been demonstrated to
prevent some hospitalization, although beneficial effects of corticosteroids are often not noted
until several hours after administration. High-dose inhaled corticosteroids may have some
benefit in the acute setting and can be continued safely by patients already on inhaled
steroids. Aerosolized ipratropium should be added if FEV
1
or PEFR is ,40% of predicted
because studies reveal that they increase pulmonary function modestly and decrease need for
hospitalization in these patients. Hypoxemia is usually corrected by administration of
supplemental oxygen with a goal of oxygen saturation of 90% to 95%. (See Table 26-1.)
Epinephrine or terbutaline may be administered subcutaneously to patients unable to
coordinate aerosolized treatments. Theophylline is not recommended in the acute setting.
6. How can I determine if my patients are improving?
Ask them how they feel, re-examine them, and obtain objective measures of pulmonary
function. Either FEV
1
or PEFR (the best of three attempts) should be obtained on presentation
and after treatment and compared with the patient’s percent predicted (or personal best) FEV
1
or PEFR, if known, to determine the need for more aggressive therapy or hospitalization.
7. What measures are available if my patient isn’t responding as expected?
Magnesium, heliox, ketamine, and continuous positive-pressure ventilation may offer some
benefits when all other treatment modalities have failed and patients remain in severe status
after conventional therapy. Magnesium sulfate has been noted to help reverse bronchospasm
in conjunction with standard therapy if PEFR is 25% or less of predicted but is not useful in
patients with mild or moderate obstruction. Although widely discussed in the literature, the
data for ketamine, heliox, and continuous positive-pressure ventilation are less compelling.
There are no absolute indications for intubation except for respiratory arrest and coma.
Possible indication for intubation includes exhaustion, worsening respiratory distress,
persistent or increasing hypercarbia, and changes in mental status. Intubate semielectively,
before the crisis of respiratory arrest, because intubation is difficult in patients, who have
asthma.
8. How should I decide whether a patient can be discharged or requires
hospitalization?
Disposition of patients is usually determined by clinical response after three doses of
aerosolized b
2
-agonist therapy; ipratropium (if used); and corticosteroids. If patients have
clear breath sounds, are no longer dyspneic or are back to baseline, and have an FEV
1
or
PEFR 70% of predicted, they may be discharged home. Patients with an incomplete response
to treatment, that is, FEV
1
between 50% and 70% of predicted and mild dyspnea, can be
considered for discharge after assessing their individual circumstances. Patients with a poor
response to bronchodilators, that is, FEV
1
,50% of predicted and who have moderate to
severe symptoms after treatment, require hospitalization. If an ED observation capability
exists, observation for 4 to 6 hours poststeroid administration will decrease the number of
inpatient admissions.
Chapter 26 ASTHMA, CHRONIC OBSTRUCTIVE PULMONARY DISEASE, AND PNEUMONIA176
9. What should be considered at time of discharge?
Patients who received corticosteroids acutely should continue oral steroid therapy at home for
3 to 10 days. For courses of less than 1 week, there is no taper required. For a 10-day course,
there remains no need to taper if the patients are concurrently taking inhaled formulations.
Dosing parameters are controversial, so choose a moderate regimen (about 40–50 mg
prednisone per day); Patients not already on controller medications who have mild persistent
asthma should be started on low-dose inhaled corticosteroids or oral leukotriene modifiers, such
as zafirlukast or montelukast. Long-acting b-agonists, such as salmeterol, should be added to
the regimen of patients with moderate persistent asthma who are inadequately controlled on
inhaled corticosteroids. All patients should be advised to use their short-acting b-agonists on a
regularly scheduled basis for a few days and then as needed. Patient education should be
provided at discharge, as well as an appointment for a follow-up visit within several weeks.
10. Does pregnancy change the management of acute asthma?
No. It is important to treat pregnant asthmatics aggressively to prevent maternal hypoxia and
subsequent fetal morbidity and mortality. Patients should not be undertreated because of fear
of teratogenicity; the risks from respiratory failure and severe acute asthma are greater than
from therapy with standard medications. The standard therapy and dosages are the same.
COPD, chronic obstructive pulmonary disease.
*Exercise extreme caution in patients with known coronary artery disease.
Medications Dosage and Route
Inhaled short-acting b
2
–agonists
Albuterol Nebulizer solution (5 mg/mL) 2.5–5 mg every 20 minutes for three doses,
then 2.5–10 mg every 1–4 hours as needed,
or 10–15 mg/hour continuously or
7.5 mg bolus
MDI (90 mg/puff): must be used with
spacer device
Four to eight puffs every 20 minutes up to
4 hours, then every 1–4 hours as needed
Systemic (injected) b
2
-agonists*
Epinephrine 1:1000 (1 mg/mL) 0.3–0.5 mg every 20 minutes for three
doses subcutaneously
Terbutaline (1 mg/mL) 0.25 mg every 20 minutes for three doses
subcutaneously
Inhaled anticholinergics
Ipratropium bromide nebulizer solution
(0.25 mg/mL)
0.5 mg every 30 minutes for three doses
then every 2–4 hours as needed
MDI (18 mg/puff): must be used with
spacer device
Four to eight puffs as needed
Systemic corticosteroids
Prednisone or prednisolone
Methylprednisolone
40–60 mg by mouth
125 mg intravenously
TABLE 26-1. MEDICATIONS USED TO TREAT ASTHMA AND COPD EXACERBATIONS
Chapter 26 ASTHMA, CHRONIC OBSTRUCTIVE PULMONARY DISEASE, AND PNEUMONIA 177
KEY POINTS: EMERGENCY TREATMENT OF ASTHMA
1. Relieve significant hypoxemia: oxygen.
2. Reverse airflow obstruction: b-agonists 1 ipratropium.
3. Reduce the likelihood of recurrence: corticosteroids.
4. Provide objective measure of improvement: PEFR or FEV1.
5. Adequate discharge planning includes education, medications, and follow-up.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
11. What is COPD and what are the presenting symptoms of a COPD exacerbation?
COPD is a disease characterized by chronic airflow limitation that is not fully reversible, is
progressive, and is associated with an abnormal inflammatory response to noxious particles
or gases. It is a combination of small airway disease and parenchymal destruction. It includes
emphysema and chronic bronchitis and can coexist with asthma. The characteristic symptoms
of COPD are cough, sputum production, and dyspnea on exertion. Exacerbations are
characterized by increased dyspnea, often accompanied by wheezing and chest tightness,
increased cough and sputum, change in color or thickness of sputum, and fever. Smoking,
exposure to occupational dusts and chemicals, and air pollution are the most common causes
of COPD.
12. In addition to COPD, what should be included in the differential diagnosis?
n
In patients who present with wheezing, the differential diagnosis includes asthma, CHF,
pneumonia, cardiogenic pulmonary edema, and bronchitis.
n
In those who present with dyspnea, the differential diagnosis includes myocardial ischemia,
pericardial effusion, pneumothorax, pulmonary embolism, pneumonia, asthma, acute
respiratory distress syndrome (ARDS), bronchiectasis, pulmonary fibrosis, pleural effusion,
tuberculosis, and metabolic disturbances, acidosis and shock.
13. Which diagnostic tests are helpful in the management of COPD?
Pulse oximetry should be used in every patient with COPD. Oxygen saturation less than 90%
indicates severe hypoxia. Arterial blood gas measurements often can identify patients with
increased and continuing hypoxia, hypercarbia, and respiratory acidosis, especially if
compared with the patient’s baseline values. Check theophylline levels if indicated. Chest
radiographs are appropriate in COPD exacerbations to help manage complications and
concomitant disease. In patients with cor pulmonale, continuous cardiac monitoring may
identify any associated arrhythmias. The use of B-type natriuretic peptide (BNP) does not
substitute for clinical judgment when trying to differentiate COPD from CHF as a numeric
cut-off value that differentiates between the two diseases remains elusive. In contrast to
asthma, acute pulmonary function tests are less helpful in the emergency setting because of
the difficulty that sick patients with COPD have in performing these tests properly.
Differentiation of mild, moderate, and severe COPD relies on the FEV
1
and the ratio of FEV
1
/
forced vital capacity (FVC) ,70%. Making this calculation without formal pulmonary function
tests (PFTs) is generally not possible in the ED.
14. What are the key objectives when treating a COPD exacerbation and how are
they achieved?
The key objectives are to relieve hypoxemia, alleviate reversible bronchospasm, and treat the
underlying etiology of the exacerbation. The cornerstone of initial management is treating the
hypoxia with supplemental oxygen with a goal of oxygen saturation of 90% or greater. Despite
